Abstract
Background
Patient safety is a fundamental value of healthcare to avoid patient harm. Non‐compliance with patient safety standards may result in patient harm and is therefore a global concern. A Self‐assessment Instrument for Perioperative Patient Safety (SIPPS) monitoring and benchmarking compliance to safety standards was validated in a multicentre pilot study.
Methods
A preliminary questionnaire, based on the Dutch perioperative patient safety guidelines and covering international patient safety goals, was evaluated in a first digital RAND Delphi round. The results were used to optimize the questionnaire and design the SIPPS. For measurement and benchmarking purposes, SIPPS was categorized into seven main patient safety domains concerning all care episode phases of the perioperative trajectory. After consensus was reached in a face‐to‐face Delphi round, SIPPS was pilot‐tested in five hospitals for five characteristics: measurability, applicability, improvement potential, discriminatory capacity and feasibility.
Results
The results of the first Delphi round showed moderate feasibility for the preliminary questionnaire (81·6 per cent). The pilot test showed good measurability for SIPPS: 99·8 per cent of requested information was assessable. Some 99·9 per cent of SIPPS questions were applicable to the selected respondents. With SIPPS, room for improvement in perioperative patient safety compliance was demonstrated for all hospitals, concerning all safety domains and all care episode phases of the perioperative trajectory (compliance 76·1 per cent). SIPPS showed mixed results for discriminatory capacity. SIPPS showed good feasibility for all items (range 91·9–95·7 per cent).
Conclusion
A self‐assessment instrument for measuring perioperative patient safety (SIPPS) compliance meeting international standards was validated. With SIPPS, improvement areas for perioperative patient safety and best practices across hospitals could be identified.
Introduction
Patient safety is a fundamental value of healthcare to avoid patient harm. Non‐compliance with patient safety standards may result in permanent injury, increased length of stay in healthcare facilities or even death, and is a major global concern. Therefore, ensuring the safety of patient care is to be given the highest priority. Since the launch of the WHO patient safety programme in 2004, more than 140 countries have taken the challenge to identify risks in patient safety and improve safety performance, to prevent avoidable harm1. It is commonly reported that around one in ten hospitalized patients are harmed as a result of adverse events; at least 50 per cent of these events are considered preventable2. Most adverse events are related to surgical procedures (40 per cent) and medication errors (15 per cent)2.
National audits3, 4, 5 by the Dutch Health Care Inspectorate (IGZ) in the period 2007–2009 showed that perioperative care in the Netherlands could be improved with regard to information transfer, clinical documentation, teamwork and coordination. In response to the IGZ recommendations, national perioperative safety guidelines6, 7, 8 were developed in 2010–2012. These guidelines are in line with international patient safety goals (IPSGs)9 (Table 1), and are applicable to both surgical and non‐surgical interventions performed in hospitals. Adherence to evidence‐based guidelines is associated with safer perioperative care and improved outcome10, 11, 12, 13.
Table 1.
Definitions of international patient safety goals9
| IPSG no. | Goal | Standard |
|---|---|---|
| 1 | To identify patients correctly | The hospital develops and implements a process to improve the accuracy of patient identification |
| 2 | To improve effective communication | The hospital develops and implements a process to improve the effectiveness of verbal and/or telephone communication among caregivers |
| 3 | To improve the safety of high‐alert medications | The hospital develops and implements a process to improve the safety of high‐alert medications |
| 4 | To ensure correct‐site, correct‐procedure, correct‐patient surgery | The hospital develops and implements a process for ensuring correct‐site, correct‐procedure, correct‐patient surgery |
| 5 | To reduce the risk of healthcare‐associated infection | The hospital adopts and implements evidence‐based hand hygiene guidelines to reduce the risk of healthcare‐associated infections |
| 6 | To reduce the risk of patient harm resulting from falls | The hospital develops and implements a process to reduce the risk of patient harm resulting from falls |
ISPG, international patient safety goal.
To support hospitals in their efforts to improve patient safety, the non‐profit Dutch Safe Curative Care Association (VVCZ; http://www.vvcz.nl) was established in 2011. Within the VVCZ, 15 Dutch hospitals cooperate to improve patient safety by exchanging knowledge, best practices and well designed tools. To facilitate monitoring and benchmarking, the VVCZ developed and introduced an integrated PeriOperative Patient Safety audit (iPOPS). iPOPS examines the extent to which current perioperative patient safety performances meet (inter)national standards of care, and facilitates hospitals and departments to improve areas that are currently below standards. In this way, iPOPS helps staff to improve continuously the organization's perioperative patient safety performance. The iPOPS audit consists of four elements that are complementary to one another, each focusing on a different aspect of perioperative care; used together, they provide a complete assessment of the perioperative practice performance in daily healthcare (Fig. 1). This assessment includes the following four parts: a prospective Self‐assessment Instrument for Perioperative Patient Safety (SIPPS) by means of a questionnaire, conducted by professionals working in the perioperative trajectory; observations of perioperative practice performance in the workplace by peers, using the Surgical Patient safety Observation Tool (SPOT)14; assessment of locally used protocols based on (inter)national guidelines; and interviews with professionals directly involved in perioperative care.
Figure 1.
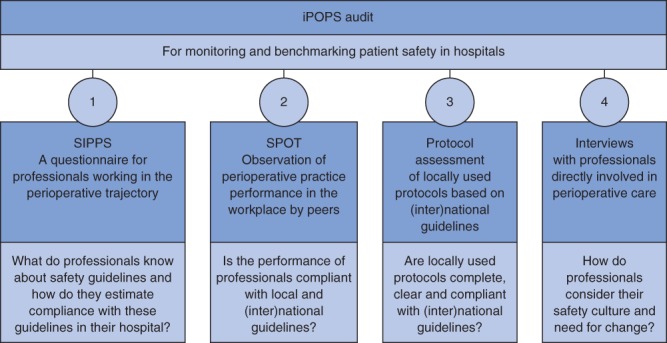
Components of the Integrated PeriOperative Patient Safety audit (iPOPS). SIPPS, Self‐assessment Instrument for Perioperative Patient Safety; SPOT, Surgical Patient safety Observation Tool
The aim of the present multicentre pilot study was to evaluate and optimize SIPPS as one of the four iPOPS core elements for further improvement and scientific validation of the instrument. The pilot study included testing of SIPPS in five hospitals to assess the clinimetric characteristics in line with previous studies14, 15, 16, 17, 18, 19.
Methods
The study consisted of two parts (Fig. 2): evaluating and improving the preliminary questionnaire by means of a RAND‐modified Delphi consensus procedure20 21; and validating SIPPS by pilot‐testing the instrument on its clinimetric characteristics in five hospitals14, 15, 16, 17, 18, 19 (Table 2). The self‐assessment questionnaire is a translation of the content of the perioperative guidelines into questions answered by a preselected group of healthcare providers working in the perioperative trajectory. This questionnaire was originally developed in Dutch and translated into English by an official translating agency. For measuring and benchmarking purposes, SIPPS was categorized into both seven patient safety domains (Table 3) and four perioperative care episode phases. Questions concerning safety culture were added to ascertain whether the organizational culture encouraged individual staff members to report concerns about safety or quality of care without retaliatory action from the hospital. These additional questions were excluded from the present study, because they were not based on the Dutch perioperative guidelines and international patient safety goals. Ethical approval was not required as no patients were involved.
Figure 2.
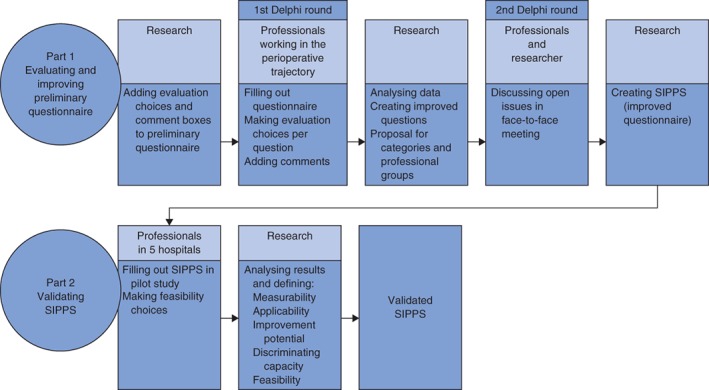
Evaluation and validation steps for a validated Self‐assessment Instrument for Perioperative Patient Safety (SIPPS)
Table 2.
| Criterion | Definition | Score |
|---|---|---|
| Measurability | Questions are measurable | Good: at least 80 per cent of questions are answered |
| Moderate: more than 20 to less than 80 per cent of questions are answered | ||
| Poor: 20 per cent or less of questions are answered | ||
| Applicability | Questions are applicable to the selected respondents | Good: at least 80 per cent of questions are applicable |
| Poor: less than 80 per cent of questions are applicable | ||
| Improvement potential | Room for improvement of current practice (topic level) | Good: compliance with the standard is less than 90 per cent |
| Poor: compliance with the standard is at least 90 per cent | ||
| Discriminatory capacity for comparison | Discrimination of practice performance (compliance with the standards) between different topics and between departments or hospitals | Good: more than 20 per cent variation between lowest and highest scores |
| Poor: 20 per cent or less variation between lowest and highest scores | ||
| Feasibility | The questionnaire is clear, applicable and easy to use | Good: at least 90 per cent of respondents agree |
| Moderate: 50–89 per cent of respondents agree | ||
| Poor: less than 50 per cent of respondents agree |
Table 3.
Definitions of patient safety domains covered by the Self‐assessment Instrument for Perioperative Patient Safety (SIPPS)
| Domain | Definition |
|---|---|
| Verification | The process of checking the validity and completeness of a clinical or other requirement from the source that issued the requirement |
| Medical record | A written account by healthcare professionals of a variety of patient health information, such as assessment findings, treatment details, progress notes and discharge summary |
| Behaviour | Demonstrated (non)compliance with standards by healthcare professionals |
| Organization | Demonstration of the standards that are organized according to what is done directly and indirectly to provide for a safe, effective and well managed organization |
| Transfer | The formal shifting of responsibility for the care of a patient from: one care unit to another; one clinical service to another; one healthcare provider to another (also known as handover); or one organization to another |
| Patient communication | Standards that are organized according to what is done directly or indirectly to inform the patient |
| Standard operating procedure | A (combination of) protocol, procedure or process documentation |
| Protocol: a scientific medical treatment plan or study outline for a procedure or treatment | |
| Procedure: a written document describing how a task is performed, usually including step‐by‐step instructions | |
| Process: a definition of a task that needs to be done and by whom |
Evaluating and improving the preliminary questionnaire
Part 1 of the study (Fig. 2) was performed between January 2015 and July 2017 during iPOPS audits conducted in VVCZ member hospitals, in two Delphi rounds.
Based on the existing perioperative self‐assessment questionnaire used during iPOPS audits, the respondents of VVCZ‐audited hospitals (professionals working in the perioperative trajectory) were invited to comment on the content of this questionnaire. For this reason, in addition to each question, respondents could choose between four simple evaluation statements: ‘question is good’, ‘question is unclear’, ‘question is not relevant’ and ‘question is not applicable to my work’. Supplementary comments could be added to each question.
Results from the first Delphi round were analysed and prepared to present in a face‐to‐face VVCZ members' meeting, to reach consensus on the content of an optimized self‐assessment instrument, called SIPPS.
Validating SIPPS
In part 2 of the study (Fig. 2), SIPPS was pilot‐tested on five clinimetric characteristics: measurability, applicability, improvement potential, discriminating capacity and feasibility (Table 2). To evaluate SIPPS on the first four characteristics, the respondents could choose between five answers for each question: ‘yes’, meaning ‘we are 90–100 per cent compliant with this standard’; ‘partly’, meaning ‘we are 50–89 per cent compliant with this standard’; ‘no’, meaning ‘we are less than 50 per cent compliant with this standard’; ‘unknown’, meaning ‘I do not know the answer to this question’; or ‘not applicable’, meaning ‘this question is not applicable to my job’. Supplementary comments could be added to each question.
To evaluate the fifth characteristic (the feasibility of SIPPS), respondents were invited to comment according to a six‐point scale, varying from ‘totally agree’ to ‘totally disagree’ on four statements after completing SIPPS: ‘the questions were clearly formulated’, ‘the questions were relevant to my work’, ‘the answering categories provided enough possibilities to give the answer(s) I had in mind’ and ‘the time to complete the self‐evaluation SIPPS was acceptable’.
Results
Evaluating and improving the preliminary questionnaire
In the period from April to December 2016, respondents of the preliminary questionnaire commented on the instrument. Thirteen VVCZ member hospitals participated in this first Delphi round, and digitally and anonymously filled out 345 self‐assessment questionnaires and additional evaluation questions. All respondents were professionals working in the perioperative trajectory: anaesthesia nurses (31), anaesthetists (21), pharmacists (13), nurses working in the preanaesthesia care unit (17), nurses working in the admissions department (18), operating room (OR) managers (25), quality and safety managers (14), medical technologists (19), anaesthesiology employees working in the outpatient clinic (25), OR planners (27), surgical physicians (16), OR nurses (28), employees working in the polyclinic department with the exception of anaesthesia (15), postanaesthesia care nurses (25), surgical ward nurses (19), medical technology employees (14) and logistics employees (18). In total, 12 139 evaluating answers and 495 comments were received. The results of the first Delphi round showed moderate feasibility for the preliminary questionnaire (81·6 per cent) (Table 4).
Table 4.
Results of the first Delphi round for evaluation of the preliminary questionnaire
| Evaluation statement | Score |
|---|---|
| Question is not applicable to my work | 1243 (10·2) |
| Question is not relevant | 129 (1·1) |
| Question is unclear | 861 (7·1) |
| Question is good | 9906 (81·6) |
| Total score | 12 139 (100) |
Values in parentheses are percentages.
A single researcher processed and analysed the results and suggestions from the first Delphi round, and then compared the questions with the perioperative guidelines in detail, translating the items resulting from the first Delphi round into clear questions for specific groups of professional caregivers. Existing categories of the preliminary questionnaire were considered and proposals made for adaptations. This researcher also studied the existing categories of the preliminary questionnaire and made proposals for adaptations. Subsequently, consensus was reached in a face‐to‐face VVCZ members' meeting on three remaining issues: combining or renaming certain employee groups and adding ICU employees (both nurses and physicians) to the list of professionals; adding a perioperative phase to the pre‐existing preoperative, intraoperative and postoperative phases (for questions concerning the total perioperative trajectory); and adding culture‐related questions to SIPPS.
SIPPS was then developed in a web‐based application. SIPPS contains 118 questions with 0–10 subquestions. Table 5 gives examples of SIPPS questions, categorization and professionals addressed. The complete SIPPS questionnaire is provided in Table S1 (supporting information).
Table 5.
Examples of SIPPS questions and categorization
| Question* | Care episode phase | Safety domain | Professionals |
|---|---|---|---|
| Do you obtain the following information from the referring specialist: reason for admission, relevant medical history, medication, specific details? | Preoperative | Transfer | Surgeon |
| Is anaesthesia induced with no background noise in the OR? | Intraoperative | Behaviour | Anaesthetist, anaesthesia nurse, OR nurse |
| Do at least two people transport the patient after leaving the OR? | Postoperative | Organization | Anaesthetist, anaesthesia nurse, OR nurse, postanaesthesia care nurse |
| Do you have access at all times to the patient data you require to work in a patient‐safe manner? | Perioperative | Medical record | Anaesthetist, anaesthesia nurse, pharmacist, ICU nurse, ICU physician, OR anaesthesia care manager, OR surgical care manager, OR nurse, planning employee, postanaesthesia care nurse, preanaesthesia care nurse, surgeon, surgical ward nurse |
Answering categories: yes, partly, no, not known, not applicable, not answered. OR, operating room.
Validating SIPPS
Between March and June 2017, iPOPS audits were performed in five Dutch VVCZ hospitals (2 tertiary care and 3 regional care hospitals). During these audits, a total of 140 SIPPS questionnaires were digitally and anonymously filled out by professionals working in the perioperative trajectory: anaesthesia nurses (11), anaesthetists (10), pharmacists (5), medical technicians (6), preanaesthesia care nurses (9), ICU ward nurses (6), ICU physicians (5), OR anaesthesia care managers (8), OR surgical care managers (9), OR planners (10), quality and safety staff members (11), physicians (16), OR nurses (11), postanaesthesia care nurses (9) and surgical ward nurses (14).
Results with respect to measurability, applicability, improvement potential, discriminating capacity and feasibility of SIPPS are shown in Tables 6, 7 and 8. Feasibility results of SIPPS are shown in Table 9. Based on these results, five measurable characteristic results of SIPPS were defined.
Table 6.
SIPPS results per hospital per safety domain
| Safety domain | Response | Yes | Partly | No | Not known | Not applicable | No response |
|---|---|---|---|---|---|---|---|
| Hospital 1 | |||||||
| Verification | 205 | 181 (88·2) | 14 (6·9) | 4 (1·8) | 6 (3·0) | 0 (0) | 0 (0) |
| Medical record | 272 | 223 (82·0) | 26 (9·7) | 5 (1·7) | 17 (6·2) | 0 (0) | 1 (0·4) |
| Behaviour | 63 | 53 (84) | 5 (8) | 3 (5) | 2 (3) | 0 (0) | 0 (0) |
| Organization | 369 | 288 (78·0) | 46 (12·4) | 14 (3·9) | 21 (5·7) | 0 (0) | 0 (0) |
| Transfer | 94 | 71 (75) | 11 (12) | 9 (9) | 3 (3) | 0 (0) | 0 (0) |
| Patient communication | 70 | 49 (70) | 10 (15) | 9 (13) | 0 (0) | 0 (0) | 1 (1) |
| SOP | 139 | 103 (74·3) | 12 (8·9) | 10 (7·2) | 12 (8·9) | 0 (0) | 1 (0·7) |
| Total | 1212 | 968 (79·9) | 125 (10·3) | 53 (4·4) | 62 (5·1) | 0 (0) | 3 (0·3) |
| Hospital 2 | |||||||
| Verification | 112 | 109 (97·0) | 2 (1·5) | 0 (0) | 1 (1·1) | 0 (0) | 0 (0) |
| Medical record | 179 | 144 (80·2) | 20 (11·0) | 5 (2·6) | 10 (5·6) | 0 (0) | 1 (0·6) |
| Behaviour | 51 | 44 (85) | 7 (13) | 0 (0) | 1 (2) | 0 (0) | 0 (0) |
| Organization | 271 | 212 (78·1) | 34 (12·6) | 9 (3·1) | 15 (5·6) | 0 (0) | 2 (0·6) |
| Transfer | 95 | 73 (77) | 8 (9) | 7 (8) | 6 (6) | 0 (0) | 0 (0) |
| Patient communication | 26 | 19 (72) | 3 (13) | 3 (12) | 1 (4) | 0 (0) | 0 (0) |
| SOP | 68 | 57 (83) | 3 (4) | 2 (3) | 5 (8) | 0 (0) | 1 (1·5) |
| Total | 802 | 656 (81·8) | 77 (9·6) | 26 (3·2) | 40 (5·0) | 0 (0) | 4 (0·4) |
| Hospital 3 | |||||||
| Verification | 141 | 121 (86·1) | 11 (7·7) | 3 (1·9) | 6 (4·3) | 0 (0) | 0 (0) |
| Medical record | 218 | 169 (77·4) | 19 (8·8) | 7 (3·0) | 22 (10·3) | 0 (0) | 1 (0·5) |
| Behaviour | 55 | 42 (75) | 12 (22) | 1 (2) | 1 (1) | 0 (0) | 0 (0) |
| Organization | 406 | 305 (75·0) | 59 (14·6) | 15 (3·8) | 27 (6·7) | 0 (0) | 0 (0) |
| Transfer | 117 | 89 (76·4) | 9 (7·6) | 12 (10·5) | 2 (2·1) | 4 (3·4) | 0 (0) |
| Patient communication | 38 | 23 (60) | 9 (23) | 0 (0) | 6 (16) | 0 (0) | 0 (0) |
| SOP | 147 | 101 (68·4) | 13 (8·6) | 5 (3·1) | 29 (19·6) | 0 (0) | 1 (0·3) |
| Total | 1122 | 849 (75·7) | 132 (11·7) | 42 (3·8) | 93 (8·3) | 4 (0·4) | 2 (0·1) |
| Hospital 4 | |||||||
| Verification | 78 | 69 (88) | 4 (6) | 5 (6) | 0 (0) | 0 (0) | 0 (0) |
| Medical record | 109 | 81 (74·6) | 18 (16·6) | 5 (4·6) | 5 (4·2) | 0 (0) | 0 (0) |
| Behaviour | 32 | 22 (69) | 8 (25) | 2 (6) | 0 (0) | 0 (0) | 0 (0) |
| Organization | 192 | 113 (59·0) | 40 (20·8) | 15 (7·9) | 24 (12·5) | 0 (0) | 0 (0) |
| Transfer | 54 | 37 (69) | 5 (9) | 12 (22) | 0 (0) | 0 (0) | 0 (0) |
| Patient communication | 15 | 11 (71) | 2 (15) | 2 (13) | 0 (0) | 0 (0) | 0 (0) |
| SOP | 66 | 37 (56) | 3 (4) | 9 (13) | 17 (26) | 0 (0) | 0 (0) |
| Total | 546 | 370 (68·0) | 81 (14·8) | 49 (9·0) | 46 (8·4) | 0 (0) | 0 (0) |
| Hospital 5 | |||||||
| Verification | 101 | 76 (75·0) | 14 (14·1) | 8 (7·5) | 3 (2·6) | 1 (0·9) | 0 (0) |
| Medical record | 164 | 121 (74·0) | 28 (17·1) | 4 (2·4) | 11 (6·6) | 0 (0) | 0 (0) |
| Behaviour | 45 | 31 (69) | 11 (24) | 2 (4) | 1 (2) | 0 (0) | 0 (0) |
| Organization | 330 | 233 (71·0) | 60 (18·0) | 11 (3·3) | 26 (7·8) | 0 (0) | 1 (0·3) |
| Transfer | 90 | 54 (60) | 20 (22) | 8 (9) | 8 (9) | 0 (0) | 0 (0) |
| Patient communication | 17 | 14 (82) | 2 (13) | 0 (0) | 1 (6) | 0 (0) | 0 (0) |
| SOP | 108 | 81 (75·2) | 5 (4·6) | 2 (2·2) | 19 (18·0) | 0 (0) | 0 (0) |
| Total | 855 | 610 (71·0) | 140 (16·3) | 35 (4·1) | 69 (8·0) | 1 (0·1) | 1 (0·1) |
Values in parentheses are percentages; due to rounding, values and percentages may not sum or calculate correctly. ‘Yes’ indicates 90–100 per cent compliance with this standard; ‘partly’ indicates 50–89 per cent compliance; ‘no’ indicates less than 50 per cent compliance; ‘not known’ indicates the answer to the question was unknown; ‘not applicable’ means the question was not applicable to the person's job. SIPPS, Self‐assessment Instrument for Perioperative Patient Safety; SOP, standard operating procedure.
Table 7.
SIPPS results per hospital per care episode phase in the perioperative trajectory
| Care phase | Response | Yes | Partly | No | Not known | Not applicable | No response |
|---|---|---|---|---|---|---|---|
| Hospital 1 | |||||||
| Perioperative | 528 | 408 (77·3) | 65 (12·2) | 18 (3·4) | 36 (6·9) | 0 (0) | 1 (0·2) |
| Preoperative | 137 | 125 (91·0) | 12 (8·7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Intraoperative | 312 | 258 (82·6) | 26 (8·3) | 14 (4·5) | 13 (4·2) | 0 (0) | 1 (0·3) |
| Postoperative | 235 | 178 (75·6) | 23 (9·8) | 21 (9·0) | 12 (5·1) | 0 (0) | 1 (0·5) |
| Total | 1212 | 968 (79·9) | 125 (10·3) | 53 (4·4) | 62 (5·1) | 0 (0) | 3 (0·3) |
| Hospital 2 | |||||||
| Perioperative | 362 | 267 (73·7) | 52 (14·3) | 12 (3·3) | 29 (7·9) | 0 (0) | 3 (0·8) |
| Preoperative | 42 | 37 (88) | 3 (7) | 1 (2) | 1 (2) | 0 (0) | 0 (0) |
| Intraoperative | 223 | 201 (90·3) | 10 (4·5) | 7 (3·3) | 4 (1·8) | 0 (0) | 0 (0) |
| Postoperative | 175 | 150 (86·0) | 12 (7·0) | 5 (3·1) | 6 (3·6) | 0 (0) | 1 (0·3) |
| Total | 802 | 656 (81·8) | 77 (9·6) | 26 (3·2) | 40 (5·0) | 0 (0) | 4 (0·4) |
| Hospital 3 | |||||||
| Perioperative | 593 | 439 (74·0) | 81 (13·6) | 18 (3·1) | 54 (9·1) | 0 (0) | 2 (0·3) |
| Preoperative | 55 | 44 (81) | 6 (11) | 2 (4) | 2 (4) | 0 (0) | 0 (0) |
| Intraoperative | 271 | 210 (77·5) | 31 (11·6) | 19 (6·9) | 7 (2·6) | 4 (1·5) | 0 (0) |
| Postoperative | 203 | 156 (76·8) | 13 (6·5) | 3 (1·7) | 30 (14·9) | 0 (0) | 0 (0) |
| Total | 1122 | 849 (75·7) | 132 (11·7) | 42 (3·8) | 93 (8·3) | 4 (0·4) | 2 (0·1) |
| Hospital 4 | |||||||
| Perioperative | 269 | 174 (65·0) | 44 (16·4) | 12 (4·6) | 38 (14·2) | 0 (0) | 0 (0) |
| Preoperative | 34 | 23 (68) | 4 (11) | 7 (20) | 0 (0) | 0 (0) | 0 (0) |
| Intraoperative | 144 | 111 (77·0) | 13 (8·8) | 16 (11·0) | 4 (2·9) | 0 (0) | 0 (0) |
| Postoperative | 99 | 61 (62) | 20 (20) | 14 (14) | 4 (4) | 0 (0) | 0 (0) |
| Total | 546 | 370 (68·0) | 81 (14·8) | 49 (9·0) | 46 (8·4) | 0 (0) | 0 (0) |
| Hospital 5 | |||||||
| Perioperative | 469 | 318 (68·0) | 88 (18·8) | 14 (3·1) | 48 (10·2) | 0 (0) | 1 (0·2) |
| Preoperative | 39 | 28 (71) | 6 (15) | 3 (7) | 2 (5) | 1 (2) | 0 (0) |
| Intraoperative | 215 | 157 (73·0) | 35 (16·3) | 17 (7·8) | 7 (3·1) | 0 (0) | 0 (0) |
| Postoperative | 132 | 108 (82·0) | 11 (8·1) | 1 (1·1) | 12 (9·0) | 0 (0) | 0 (0) |
| Total | 855 | 610 (71·0) | 140 (16·3) | 35 (4·1) | 69 (8·0) | 1 (0·1) | 1 (0·1) |
Values in parentheses are percentages; due to rounding, values and percentages may not sum or calculate correctly. ‘Yes’ indicates 90–100 per cent compliance with this standard; ‘partly’ indicates 50–89 per cent compliance; ‘no’ indicates less than 50 per cent compliance; ‘not known’ indicates the answer to the question was unknown; ‘not applicable’ means the question was not applicable to the person's job. SIPPS, Self‐assessment Instrument for Perioperative Patient Safety.
Table 8.
Yes (compliant) scores per safety domain and perioperative care phase for hospitals 1–5
| Total response | Hospital yes score | Total yes | Range (%) | Difference (%)* | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |||||
| Safety domain | |||||||||
| Verification | 637 | 181 (88·2) | 109 (97·0) | 121 (86·1) | 69 (88) | 76 (75·0) | 555 (87·2) | 75·0–97·0 | 22 |
| Medical record | 942 | 223 (82·0) | 144 (80·2) | 169 (77·4) | 81 (74·6) | 121 (74·0) | 738 (78·3) | 74·0–82·0 | 8 |
| Behaviour | 246 | 53 (84) | 44 (85) | 42 (75) | 22 (69) | 31 (69) | 191 (77·6) | 69–85 | 16 |
| Organization | 1568 | 288 (78·0) | 212 (78·1) | 305 (75·0) | 113 (59·0) | 233 (71·0) | 1150 (73·3) | 59·0–78·1 | 19 |
| Transfer | 450 | 71 (75) | 73 (77) | 89 (76·4) | 37 (69) | 54 (60) | 325 (72·1) | 60–77 | 17 |
| Patient communication | 166 | 49 (70) | 19 (72) | 23 (60) | 11 (71) | 14 (82) | 115 (69·5) | 60–82 | 22 |
| SOP | 528 | 103 (74·3) | 57 (83) | 101 (68·4) | 37 (56) | 81 (75·2) | 379 (71·8) | 56–83 | 27 |
| Total | 4537 | 968 (79·9) | 656 (81·8) | 849 (75·7) | 370 (68·0) | 610 (71·0) | 3453 (76·1) | 68·0–81·8 | 14 |
| Perioperative care phase | |||||||||
| Perioperative | 2221 | 408 (77·3) | 267 (73·7) | 439 (74·0) | 174 (65·0) | 318 (68·0) | 1606 (72·3) | 65·0–77·3 | 12 |
| Preoperative | 307 | 125 (91·0) | 37 (88) | 44 (81) | 23 (68) | 28 (71) | 257 (83·7) | 68–91·0 | 23 |
| Peroperative | 1165 | 258 (82·6) | 201 (90·3) | 210 (77·5) | 111 (77·0) | 157 (73·0) | 937 (80·4) | 73·0–90·3 | 17 |
| Postoperative | 844 | 178 (75·6) | 150 (86·0) | 156 (76·8) | 61 (62) | 108 (82·0) | 653 (77·4) | 62–86·0 | 24 |
| Total | 4537 | 968 (79·9) | 656 (81·8) | 849 (75·7) | 370 (68·0) | 610 (71·0) | 3453 (76·1) | 68·0–81·8 | 14 |
Values in parentheses are percentages; due to rounding, values and percentages may not sum or calculate correctly.
Maximum minus minimum range value. SOP, standard operating procedure.
Table 9.
Evaluation of feasibility of the SIPPS
| Evaluation statement | Responded | Did not respond | Agreed totally | Agreed | Agreed slightly | Disagreed slightly | Did not agree | Disagreed totally | Total agreed | Total disagreed |
|---|---|---|---|---|---|---|---|---|---|---|
| The questions were clearly formulated | 137 | 3 | 6 | 104 | 18 | 8 | 0 | 1 | 128 (93·4) | 9 (6·6) |
| The questions were relevant to my work | 136 | 4 | 12 | 89 | 24 | 9 | 2 | 0 | 125 (91·9) | 11 (8·1) |
| The answering categories provided me enough possibilities to give the answers I had in mind | 138 | 2 | 14 | 94 | 24 | 5 | 1 | 0 | 132 (95·7) | 6 (4·3) |
| The time to complete the self‐evaluation SIPPS was acceptable | 136 | 4 | 16 | 106 | 8 | 4 | 2 | 0 | 130 (95·6) | 6 (4·4) |
| Total | 547 | 13 | 48 | 393 | 74 | 26 | 5 | 1 | 515 (94·1) | 32 (5·9) |
Values in parentheses are percentages. SIPPS, Self‐assessment Instrument for Perioperative Patient Safety.
Measurability
SIPPS showed good measurability: 99·8 per cent (4527 of 4537) of the requested information was provided by the respondents (Tables 6 and 7).
Applicability
SIPPS showed good applicability: 99·9 per cent (4532 of 4537) of the questions were answered by the preselected respondents (Tables 6 and 7).
Improvement potential
Table 8 shows the patient safety compliance results (the total ‘yes’ scoring answers of the questionnaire of the five participating hospitals). Both in total and at an individual hospital level, the 90 per cent score was not reached: 76·1 (range 67·8–81·8) per cent. Room for improvement in perioperative practice performance is indicated by the SIPPS results, in all five pilot hospitals.
Discriminating capacity
Table 8 shows the discriminating capacity of SIPPS – the compared differences between the total ‘yes’ (compliant) results of the participating hospitals. For patient safety, good variation (more than 20 per cent) in compliance between hospitals was shown for three domains: 75– 97 per cent for the domain verification; 60–82 per cent for patient communication; and 56–83 per cent for standard operating procedure. The domains organization, transfer, behaviour and medical record showed poor variation (20 per cent or less): 19, 17, 16 and 8 per cent respectively. For the care episode phase, variation between hospitals was good with respect to comparison for the preoperative and postoperative phases (23 and 24 per cent respectively). Variation within intraoperative and total perioperative phases was 17 and 12 per cent respectively.
Feasibility
SIPPS showed good feasibility for all four quality criteria (94·1 per cent): clear formulation (93·4 per cent), relevance (91·9 per cent), good answering possibility (95·7 per cent) and acceptable time effort (95·6 per cent) (Table 9).
Discussion
SIPPS, a comprehensive self‐assessment instrument to measure perioperative patient safety, was pilot‐tested and validated for prospective monitoring, benchmarking and improving perioperative safety performance. SIPPS was evaluated by means of a RAND‐modified Delphi consensus procedure and pilot‐tested on its clinimetric characteristics.
The present study resulted in a validated and feasible measurement instrument for perioperative patient safety performance in daily clinical practice. All perioperative patient safety questions appeared to be easily measurable with SIPPS and were generally applicable to surgical procedures. The overall improvement potential appeared to be good. SIPPS also helped to identify patient safety domains with room for improvement. A good discriminatory capacity of the tool was shown for several topics, whereas the total hospital scores showed lower variation in the pilot period. These results indicate there is no need to adapt the content of SIPPS.
Based on the pilot SIPPS results, benchmarking of best practices between hospitals and different departments or phases in the perioperative trajectory is facilitated. For instance, hospital 4 could learn from the best practice performance of hospital 2, especially for the domains ‘organization’ and ‘standard operating procedure’ (Fig. 3), and in the preoperative and postoperative care episode phase (Fig. 4). SIPPS is currently used in all VVCZ member hospitals, as part of iPOPS. The iPOPS audit team consists of an audit leader together with two expert professionals in perioperative care (1 physician and 1 non‐physician). The hospitals use iPOPS results to support internal perioperative patient safety improvement initiatives. Results are anonymized and then used for benchmarking between VVCZ member hospitals. SIPPS is complementary to the previously evaluated SPOT14, which shows the results of observable patient safety topics. Together with protocol insight (judging clarity, currency and conformity with perioperative guidelines) and interviews with caregivers, a comprehensive perioperative audit is provided for Dutch hospitals, in a safe setting by and for professionals themselves. To the authors' knowledge, no similar self‐assessment tool is currently available to characterize perioperative patient safety. As well as surgical disciplines, SIPPS is also suitable for other medical specialties and activities with an interventional character, such as radiology, cardiology, bronchoscopy and endoscopy.
Figure 3.
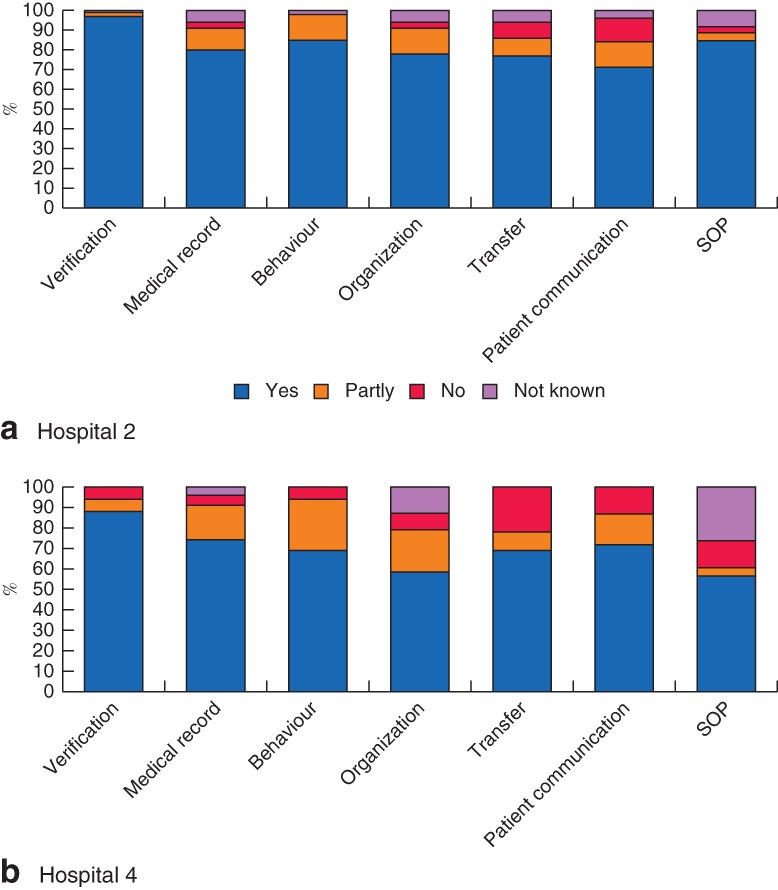
Self‐assessment Instrument for Perioperative Patient Safety (SIPPS) results for compliance at the safety domain level in a hospital 2 and b hospital 4. ‘Yes’ indicates 90–100 per cent compliance with the standard; ‘partly’ indicates 50–89 per cent compliance; ‘no’ indicates less than 50 per cent compliance; ‘not known’ indicates the answer to the question was unknown. SOP, standard operating procedure
Figure 4.
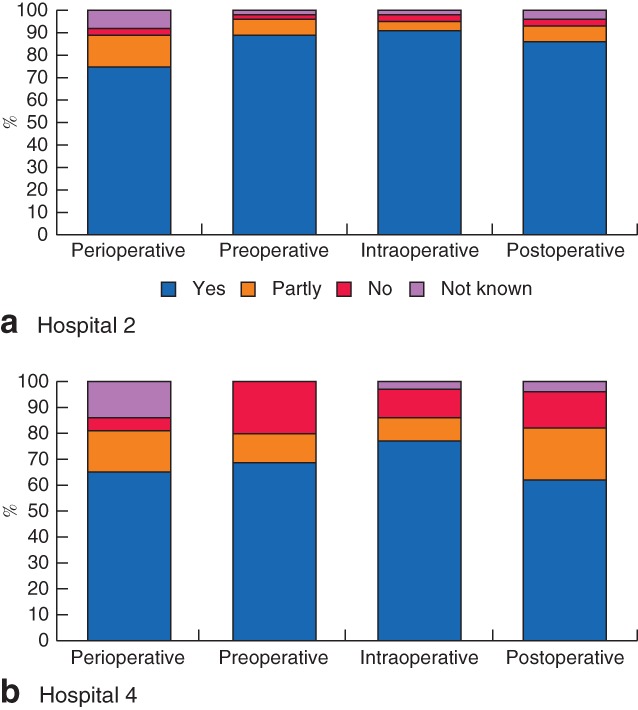
Self‐assessment Instrument for Perioperative Patient Safety (SIPPS) results for compliance at care episode level in a hospital 2 and b hospital 4. ‘Yes’ indicates 90–100 per cent compliance with the standard; ‘partly’ indicates 50–89 per cent compliance; ‘no’ indicates less than 50 per cent compliance; ‘not known’ indicates the answer to the question was unknown.
Worldwide, patient safety programmes are designed to measure and improve safety in order to control risks and minimize potentially avoidable patient harm, by systems and teamwork approaches22. These programmes are intended not only to prevent adverse events and complications, but also to develop a ‘culture of safety’ within hospitals, setting up an infrastructure for surveillance and management of preventable patient harm13. New insights into the mechanisms by which compliance with safety and quality measures lead to improvements in patient outcomes suggest that hospitals taking steps to implement comprehensive sets of safe practices may benefit from improvements in the management of complications among higher‐risk surgical patients13. These findings highlight the importance of hospitals having systems to identify and treat surgical complications. Nonetheless, it remains difficult to evaluate the impact of hospital safety initiatives on patient outcomes, as the effectiveness may depend on the cumulative effect of many different coordinated care systems and safety interventions.
Extensive guidelines are transformed into a comprehensive and feasible self‐assessment instrument for professional caregivers, to measure perioperative patient safety performance. Perioperative experts from various hospitals participated in the present study, which resulted in broad support for the instrument. SIPPS offers a structured method for measuring and monitoring perioperative compliance and risks in order to improve patient safety. The pilot test showed that SIPPS is a suitable and easy‐to‐use tool for identifying patient safety risk areas throughout the perioperative process. Spreading this standardized validated assessment tool across institutions can be used to provide ongoing, comparable data to maintain and improve safety standards.
This SIPPS study has limitations. The evaluation characteristics used to validate the instrument were based on measurable clinical characteristics. Although the results showed good ability to identify opportunities for improvement of patient safety performance, results in outcome and/or quality of care cannot be measured by SIPPS. Because only a small number of representatives participated, the results do not provide a full representation of all those working in the perioperative trajectory. It is therefore suggested that hospitals use the tool regularly to stimulate a broad response. Greater attention needs to be focused on understanding the hospital's ability to improve patient outcomes through safety programmes and practices. Finally, the current English version of the questionnaire has some limitations because it has not been translated back into the original Dutch language by an independent person, to ensure that no meanings have been altered.
Supporting information
Table S1. SIPPS questions and categories
Acknowledgements
The authors thank C. Joosten, designer for medical innovations at design studio Panton, for support in processing the data.
Disclosure: The authors declare no conflict of interest.
Funding information No funding
References
- 1.WHO. 10 Facts on Patient Safety http://www.who.int/features/factfiles/patient_safety/en/ [accessed 15 December 2017].
- 2. de Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ, Boermeester MA. The incidence and nature of in‐hospital adverse events: a systematic review. Qual Saf Health Care 2008; 17: 216–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inspectie voor de Gezondheidszorg (IGZ). [Preoperative Process Lacks a Multidisciplinary and Standardized Approach and Teambuilding.] IGZ: The Hague, 2007.
- 4.Inspectie voor de Gezondheidszorg (IGZ).[Standardization is Essential for Risk Reduction in the Operative Process] IGZ: The Hague, 2008.
- 5.Inspectie voor de Gezondheidszorg (IGZ). [Postoperative Care in Hospitals Partly Sufficient, But Still Contains Too Many Risks.] IGZ: The Hague, 2009.
- 6.Nederlandse Vereniging voor Anesthesiologie (NVA), Nederlandse Vereniging voor Heelkunde (NVH). [Guideline: The Preoperative Care Process.] NVA, NVH: Utrecht, 2010.
- 7.Nederlandse Vereniging voor Anesthesiologie (NVA), Nederlandse Vereniging voor Heelkunde (NVH). [Guideline: The Peroperative Care Process.] NVA, NVH: Utrecht, 2011.
- 8.Nederlandse Vereniging voor Anesthesiologie (NVA), Nederlandse Vereniging voor Heelkunde (NVH). [Guideline: The Postoperative Care Process.] NVA, NVH: Utrecht, 2012.
- 9.Joint Commission International (JCI). Joint Commission International Accreditation Standards for Hospitals (5th edn). JCI: Oakbrook Terrace, 2014.
- 10. Baines R, Langelaan M, de Bruijne M, Spreeuwenberg P, Wagner C. How effective are patient safety initiatives? A retrospective patient record review study of changes to patient safety over time. BMJ Qual Saf 2015; 24: 561–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. de Vries EN, Prins HA, Crolla RM, den Outer AJ, van Andel G, van Helden SH et al; SURPASS Collaborative Group . Effect of a comprehensive surgical safety system on patient outcomes. N Engl J Med 2010; 363: 1928–1937. [DOI] [PubMed] [Google Scholar]
- 12. van Klei WA, Hoff RG, van Aarnhem EE, Simmermacher RK, Regli LP, Kappen TH et al Effects of the introduction of the WHO ‘Surgical Safety Checklist’ on in‐hospital mortality: a cohort study. Ann Surg 2012; 255: 44–49. [DOI] [PubMed] [Google Scholar]
- 13. Brooke BS, Dominici F, Pronovost PJ, Makary MA, Schneider E, Pawlik TM. Variations in surgical outcomes associated with hospital compliance with safety practices. Surgery 2012; 151: 651–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Heideveld‐Chevalking AJ, Calsbeek H, Emond YJ, Damen J, Meijerink WJHJ, Hofland J et al Development of the Surgical Patient safety Observation Tool (SPOT). BJS Open 2018; 2: 119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McGlynn EA. Choosing and evaluating clinical performance measures. Jt Comm J Qual Improv 1998; 24: 470–479. [DOI] [PubMed] [Google Scholar]
- 16. Rubin HR, Pronovost P, Diette GB. From a process of care to a measure: the development and testing of a quality indicator. Int J Qual Health Care 2001; 13: 489–496. [DOI] [PubMed] [Google Scholar]
- 17. Hermens RP, Ouwens MM, Vonk‐Okhuijsen SY, van der Wel Y, Tjan‐Heijnen VC, van den Broek LD et al Development of quality indicators for diagnosis and treatment of patients with non‐small cell lung cancer: a first step toward implementing a multidisciplinary, evidence‐based guideline. Lung Cancer 2006; 54: 117–124. [DOI] [PubMed] [Google Scholar]
- 18. Emond YE, Stienen JJ, Wollersheim HC, Bloo GJ, Damen J, Westert GP et al Development and measurement of perioperative patient safety indicators. Br J Anaesth 2015; 114: 963–972. [DOI] [PubMed] [Google Scholar]
- 19. Fava GA, Tomba E, Sonino N. Clinimetrics: the science of clinical measurements. Int J Clin Pract 2012; 66: 11–15. [DOI] [PubMed] [Google Scholar]
- 20. Boulkedid R, Abdoul H, Loustau M, Sibony O, Alberti C. Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLoS One 2011; 6: e20476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ogden SR, Culp WC Jr, Villamaria FJ, Ball TR. Developing a checklist: consensus via a modified Delphi technique. J Cardiothorac Vasc Anesth 2016; 30: 855–858. [DOI] [PubMed] [Google Scholar]
- 22. McCulloch P, Morgan L, New S, Catchpole K, Roberston E, Hadi M et al Combining systems and teamwork approaches to enhance the effectiveness of safety improvement interventions in surgery: the Safer Delivery of Surgical Services (S3) program. Ann Surg 2017; 265: 90–96. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. SIPPS questions and categories


