Abstract
Objective
We describe school performance and experience in children with inflammatory bowel disease (IBD) across Germany and Austria. Predictors of compromised performance and satisfaction were evaluated to identify subgroups of increased risk.
Design
This cross-sectional analysis was based on a postal survey in children aged 10–15 with Crohn’s disease, ulcerative colitis or unclassified IBD and their families. Multivariate regression analysis was used to assess influential factors on parental satisfaction with school, attending advanced secondary education (ASE), having good marks and having to repeat a class. Satisfaction was assessed based on the Child Healthcare–Satisfaction, Utilisation and Needs instrument (possible range 1.00–5.00).
Results
Of 1367 families contacted, 675 participated in the study (49.4%). Sixty-eight participants (10.2%) had repeated a year, 312 (46.2%) attended ASE. The median school satisfaction score was 2.67 (IQR 2.00–3.33). High socioeconomic status (SES) and region within Germany were predictive for ASE (OR high SES 8.2, 95% CI 4.7 to 14.2). SES, female sex and region of residence predicted good marks. Grade retention was associated with an active disease course (OR 2.7, 95% CI 1.4 to 5.3) and prolonged periods off school due to IBD (OR 3.9, 95% CI 1.8 to 8.6).
Conclusions
A severe disease course impacted on the risk of grade retention, but not on type of school attended and school marks. Low satisfaction of parents of chronically ill children with the school situation underlines the need for a more interdisciplinary approach in health services and health services research in young people.
Keywords: inflammatory bowel diseases, school, education
Summary box.
What is already known about this subject?
Crohn’s disease and ulcerative colitis are increasingly diagnosed in childhood and early adulthood.
These inflammatory bowel diseases (IBD) run a chronic course with potentially severe impact on quality of life.
There is concern that inflammatory bowel disease (IBD) may impact on education and job perspectives of affected children.
What are the new findings?
Parents showed low satisfaction with the disease-related situation at school, in particular in students with poor marks.
Children with severe disease course and longer periods of absence had a markedly increased risk of grade retention.
There was no association between disease related factors and type of school attended or marks received.
How might it impact on clinical practice in the foreseeable future?
More attention needs to be paid to training of teachers and communication about the disease at school in particular where students are lower performers. Also, solutions need to be discussed and implemented to help children catch up with school in periods of absence due to IBD.
Introduction
Growing up with chronic disease poses many challenges to all concerned—patients, parents, care givers and social environment.1 This is also true for the inflammatory bowel diseases (IBD), which comprise Crohn’s disease (CD), ulcerative colitis (UC) and colitis unclassified.2 These diseases are typically first diagnosed in young adults, but may occur at any age, including childhood.3 They are characterised by a chronically relapsing course with a large variety of potential complications.4 In children, the disease may interfere substantially with physical and psychosocial development.5 6 This can also imply difficulties in school, potentially compromising overall educational achievement and employability.7–9 Evidence of relevantly impaired educational outcomes of adolescents with IBD as compared to the general population is not consistent.10–13 In general, socioeconomic or psychological characteristics seem to have more impact on schooling success than the somatic condition as such, at least unless the disease course is severe.8 14 In a recent analysis from the Swiss IBD cohort, coping of affected children was described as excellent, including school performance.15 Still, high levels of dissatisfaction were reported in terms of disease-related communication with school staff and appropriate health and toilet facilities.12 16 17 School absenteeism is another frequently reported problem in chronic disease of childhood.9 18 Overall, there are few quantitative data from larger patient groups to help target or prevent perceived problems in those most likely to be concerned.
We recently performed a large survey in children with IBD to assess the current situation of medical care in this group.19 20 Preliminary analysis showed high satisfaction of parents relating to competence and communication of physicians (manuscript in preparation). In contrast, the situation at school received rather low scores. This is remarkable, as low patient satisfaction ratings are, in general, uncommon.21
The main focus of the current analysis was explorative, aiming at describing the experience with the situation in school from the perspective of children with IBD and their parents. In addition, we examined determinants of school performance as indicated by, on the positive side, receiving advanced secondary education (ASE) and receiving good marks, and, on the negative side, grade retention.
Methods
Design and setting, patient recruitment
A mailed survey was performed on the quality of care in paediatric IBD.20 22 Eligibility criteria included a physician confirmed diagnosis of CD, UC or colitis unclassified and age between 10 and 15 years. Recruitment was via the German language paediatric IBD registry CEDATA-GPGE,23 24 the associated Saxonian Epidemiological Paediatric IBD registry,25 IBD-related research mailing lists and the national patient organisation.
Data collection
Parents and patients received multimodular postal questionnaires. Validated assessment instruments were included wherever possible.26 School-related information included type of school and current class attended, prolonged periods away from school due to IBD (ever missing 2 weeks or more at a time—never/very rarely, occasionally, frequently), skipping or repeating a class, most recent term marks in Math and German and the general impression whether the disease leads to compromised school performance (no, minor/rarely, marked/frequently). Marks in Germany range from 6 to 1, with 5 and 6 corresponding to a fail mark and 1 and 2 to a good mark.
In Germany, secondary education starts following 4 years of elementary school and commonly entails the decision for a specific type of secondary school, depending on school performance, interest and preferences. Depending on the school type, we classified secondary education as basic (expected school leaving after 10 years of education), intermediate (expected education trail 10 years overall±additional non-academic job qualifying training) and advanced secondary education (ASE (grammar school, Gymnasium—education expected to lead to a university qualifying degree). Any others (eg, Waldorf, integrative schools) were classified as ‘other’.
Parents judged the child’s physical and mental development in comparison to other children of similar age (normal, ahead, behind). From quality of life measures, we present results for the school-related items (getting along at school, having missed time at school recently).27 28 Also, we asked the children whether they disclosed the disease at school.
Satisfaction with the situation at school was available as a subdomain of the internationally validated generic questionnaire on Child Healthcare–Satisfaction, Utilisation and Needs (CHC-SUN).29 30 Items relate to (1) the knowledge of teachers about the child’s disease, (2) the teachers’ attentiveness to the disease and (3) the health facilities available at school. For graphical display, we simplified the original five-point answer scales to no, moderate and high satisfaction, summary scores used the original 1–5 scale. The CHC-SUN school service subscore was calculated by estimating the mean value of all questions answered.
School-related free text comments are cited relating to the following questions: important life events (parents only), what else is considered important in care, good experiences, bad experiences, anything else you’d like to tell us (children and parents).
Sociodemographic variables
Information was collected on region of residence within Germany or Austria (seven regions based on neighbouring states), migration background (both parents born abroad OR German not primary language spoken at home), family type (single parent households, both parents or other) and number of siblings. Parental socioeconomic status (SES) was assessed based on level of education, occupation and income of the parents and was used in three categories based on quintiles (high: highest 20%, medium: middle 60%, low: lowest 20%).31 32
Disease-specific variables, health status and comorbidity
Type of disease included CD, UC and IBD not specified (IBD_NS) based on the questionnaire information. IBD_NS comprised IBD with unclear or inconsistent information, as well as unclassified IBD. Age at onset was classified as very early diagnosis (age 0 to <6), early (6–9) and adolescence (>10). For current health status, general information on current IBD-related well-being was used as reported by parents (global question, five categories collapsed to good, moderate and poor). Disease course during the preceding year (no relapse, one relapse, several relapses/persistent symptoms), having had resecting surgery and current and previous medical therapy were available to indicate severity of disease (parent information).
Statistical analysis
Description and exploration
Baseline description of the sample shows absolute numbers and percentages for categorical or categorised variables, stratified by age group for sociodemographic and disease type for health related variables.
In addition, school-related experience is reported in a descriptive way.
Regression analyses
Attending ASE school, having missed a class and recent marks in German and Math were used as indicators of school performance and thus represented outcomes in regression analysis, in addition to satisfaction with school as a measure of experience.
To model ASE and having repeated a class (grade retention), logistic regression was used. The median grade of math and German was analysed as an ordinal response variable with adjacent-category logistic models.33 Determinants of satisfaction measure by the CHC-SUN subscore were examined in linear regression analysis. All variables considered relevant as potential determinants of school performance tables 1–4 underwent bivariate analysis. Variables were then selected into multivariate models based on the Akaike’s information criterion (AIC). For every step, changes in estimators and SEs were monitored to possibly detect overfitting. We present all regression results of the bivariate analysis, the fully adjusted models and the selected parsimonious models, with coefficients transformed to ORs for the logistic and adjacent category models and 95% CIs for all estimates. For the adjacent-category models, the OR correspond to an improvement of the median grade by 1. OR <0.5 or OR >2.0 are considered strong associations and OR with 95% CI excluding 1.0 are considered statistically significant.
Table 1.
Determinants of attending ASE (logistic regression, OR and 95% CI)
| Bivariate | Full model | Parsimonious | |
| Sociodemographic variables | |||
| Being a girl | 0.99 (0.73 to 1.36) | 0.90 (0.61 to 1.31) | |
| Age at survey (vs 13–14) | |||
| ≤12 | 1.26 (0.86 to 1.84) | 1.09 (0.68 to 1.75) | |
| ≥15 | 0.83 (0.58 to 1.21) | 0.97 (0.61 to 1.53) | |
| Region of residence (vs North Rhine-Westphalia (largest state by inhabitants)) | |||
| North-west | 0.78 (0.46 to 1.31) | 0.90 (0.48 to 1.67) | |
| South-west | 0.73 (0.45 to 1.19) | 0.67 (0.37 to 1.23) | |
| Bavaria | 0.47 (0.27 to 0.82) | 0.46 (0.24 to 0.91) | |
| North-east | 0.54 (0.29 to 1.01) | 0.68 (0.32 to 1.45) | |
| Saxony, Thuringia | 0.57 (0.33 to 0.97) | 0.80 (0.42 to 1.53) | |
| Austria, other | 0.31 (0.12 to 0.81) | 0.34 (0.11 to 1.07) | |
| Parental socioeconomic status (vs middle) | |||
| Low | 0.31 (0.20 to 0.49) | 0.31 (0.19 to 0.52) | 0.30 (0.18 to 0.50) |
| High | 6.96 (4.14 to 11.68) | 7.95 (4.54 to 13.93) | 8.16 (4.7 to 14.16) |
| Family situation (vs ‘classic’ family) | |||
| Single parent | 0.32 (0.19 to 0.55) | 0.54 (0.28 to 1.02) | 0.52 (0.28 to 0.97) |
| Other or unknown | 0.61 (0.35 to 1.08) | 1.18 (0.61 to 2.28) | 1.21 (0.63 to 2.32) |
| Immigration background | 1.21 (0.59 to 2.47) | 2.88 (1.19 to 6.94) | 2.93 (1.23 to 6.97) |
| Single child | 1.25 (0.82 to 1.91) | 1.29 (0.77 to 2.15) | |
| School-related variables | |||
| Periods off school (vs never or very rarely) | |||
| Occasionally | 0.98 (0.69 to 1.41) | 1.05 (0.67 to 1.65) | 1.00 (0.66 to 1.53) |
| Often | 0.72 (0.44 to 1.18) | 0.63 (0.33 to 1.20) | 0.67 (0.37 to 1.20) |
| Perceived compromised by inflammatory bowel disease at school (vs not compromised) | |||
| Slightly, occasionally | 1.02 (0.73 to 1.43) | 0.93 (0.59 to 1.45) | |
| Substantially, frequently | 0.91 (0.57 to 1.45) | 0.95 (0.50 to 1.81) | |
| Health-related variables | |||
| Age diagnosis*disease duration (vs 10+, >2 years duration) | |||
| 0–5 versus 10+ | 0.91 (0.53 to 1.57) | 0.68 (0.33 to 1.42) | 0.75 (0.39 to 1.44) |
| 6–9 versus 10+ | 1.00 (0.66 to 1.50) | 0.93 (0.55 to 1.57) | 0.97 (0.61 to 1.55) |
| 10+,<2 years duration | 1.24 (0.82 to 1.88) | 1.15 (0.67 to 1.95) | 1.20 (0.73 to 1.97) |
| Poor or moderate current health status (vs good) | 0.90 (0.65 to 1.24) | 0.84 (0.54 to 1.30) | |
| Active disease course (vs remission during last year) | 1.14 (0.83 to 1.57) | 1.40 (0.90 to 2.19) | 1.36 (0.92 to 2.02) |
Table 2*.
Determinants of good marks (adjacent-category model, OR and 95% CI for an increase in median grades by 1)
| Bivariate | Full model | Parsimonious | |
| Sociodemographic variables | |||
| Being a girl | 1.29 (1.03 to 1.55) | 1.32 (1.00 to 1.64) | 1.33 (1.01 to 1.65) |
| Age at survey (vs 13–14) | |||
| ≤12 | 1.74 (1.31 to 2.17) | 1.70 (1.18 to 2.21) | 1.68 (1.17 to 2.18) |
| ≥15 | 0.74 (0.56 to 0.93) | 0.75 (0.53 to 0.97) | 0.78 (0.56 to 1.01) |
| Region of residence (vs North Rhine-Westphalia) | |||
| North-west | 0.99 (0.66 to 1.32) | 0.96 (0.58 to 1.33) | 1.00 (0.61 to 1.38) |
| South-west | 1.14 (0.78 to 1.49) | 1.11 (0.69 to 1.53) | 1.11 (0.70 to 1.52) |
| Bavaria | 0.71 (0.46 to 0.96) | 0.71 (0.41 to 1.00) | 0.72 (0.43 to 1.02) |
| North-east | 1.36 (0.83 to 1.90) | 1.34 (0.69 to 2.00) | 1.40 (0.74 to 2.06) |
| Saxony, Thuringia | 1.57 (1.03 to 2.10) | 1.89 (1.11 to 2.67) | 1.96 (1.17 to 2.76) |
| Austria, other | 1.69 (0.73 to 2.64) | 1.79 (0.60 to 2.98) | 1.76 (0.60 to 2.91) |
| Parental socioeconomic status (vs middle) | |||
| Low | 0.71 (0.53 to 0.89) | 0.83 (0.57 to 1.10) | 0.77 (0.54 to 1.00) |
| High | 1.80 (1.32 to 2.27) | 1.47 (1.00 to 1.94) | 1.51 (1.04 to 1.98) |
| Family situation (vs ‘classic’ family) | |||
| Single parent | 0.71 (0.49 to 0.93) | 0.90 (0.55 to 1.26) | |
| Other or unknown | 0.80 (0.51 to 1.09) | 1.09 (0.61 to 1.56) | |
| Immigration background | 0.55 (0.30 to 0.80) | 0.53 (0.22 to 0.85) | |
| Single child | 0.92 (0.68 to 1.16) | 0.81 (0.55 to 1.07) | |
| School-related variables | |||
| Advanced secondary education | 1.78 (1.40 to 2.17) | 1.60 (1.17 to 2.03) | 1.53 (1.13 to 1.94) |
| Periods off school (vs never or very rarely) | |||
| Occasionally | 1.24 (0.95 to 1.52) | 1.15 (0.82 to 1.48) | 1.21 (0.89 to 1.54) |
| Often | 0.82 (0.56 to 1.09) | 0.88 (0.52 to 1.24) | 0.78 (0.48 to 1.08) |
| Perceived compromised by inflammatory bowel disease at school (vs not compromised) | |||
| Slightly, occasionally | 1.10 (0.86 to 1.33) | 1.06 (0.77 to 1.36) | |
| Substantially, frequently | 0.77 (0.53 to 1.01) | 0.72 (0.42 to 1.01) | |
| Health-related variables | |||
| Age diagnosis/disease duration (vs 10+, >2 years duration)* | |||
| 0–5 versus 10+ | 2.03 (1.31 to 2.74) | 1.37 (0.75 to 2.00) | 1.37 (0.75 to 1.99) |
| 6–9 versus 10+ | 1.38 (1.01 to 1.75) | 0.94 (0.63 to 1.25) | 0.95 (0.64 to 1.25) |
| 10+,<2 years duration | 1.49 (1.09 to 1.90) | 1.16 (0.77 to 1.54) | 1.15 (0.77 to 1.53) |
| Poor or moderate current health status (vs good health) | 0.95 (0.75 to 1.15) | 1.24 (0.89 to 1.58) | 1.14 (0.84 to 1.44) |
| Active disease course (vs remission during preceding 12 months) | 0.99 (0.79 to 1.18) | 1.06 (0.76 to 1.36) | 1.02 (0.75 to 1.30) |
Due to the inclusion criteria, all children with early disease onset had long-standing disease. These variables were therefore combined to a single combination variable for multivariate analysis.
Table 3.
Determinants of grade retention (logistic regression, OR and 95% CI)
| Bivariate | Full model | Parsimonious | |
| Sociodemographic variables | |||
| Being a girl | 0.65 (0.40 to 1.06) | 0.67 (0.37 to 1.21) | |
| Age at survey (vs 13–14) | |||
| ≤12 | 0.56 (0.31 to 1.03) | 0.36 (0.15 to 0.84) | 0.37 (0.16 to 0.84) |
| ≥15 | 1.30 (0.77 to 2.18) | 1.41 (0.73 to 2.72) | 1.54 (0.82 to 2.87) |
| Region of residence (vs North Rhine-Westphalia) | |||
| North-west | 1.04 (0.50 to 2.17) | 1.19 (0.48 to 2.97) | |
| South-west | 0.80 (0.38 to 1.67) | 1.06 (0.41 to 2.76) | |
| Bavaria | 1.07 (0.49 to 2.33) | 1.08 (0.41 to 2.86) | |
| North-east | 0.78 (0.31 to 1.99) | 0.67 (0.19 to 2.41) | |
| Saxony, Thuringia | 0.93 (0.43 to 2.02) | 0.69 (0.25 to 1.90) | |
| Austria, other | 0.86 (0.23 to 3.17) | 0.91 (0.20 to 4.12) | |
| Parental socioeconomic status (vs middle) | |||
| Low | 2.24 (1.34 to 3.73) | 1.97 (1.03 to 3.76) | 1.94 (1.06 to 3.53) |
| High | 0.69 (0.35 to 1.39) | 1.12 (0.44 to 2.87) | 1.11 (0.45 to 2.75) |
| Family situation (vs ‘classic’ family) | |||
| Single parent | 2.92 (1.6 to 5.16) | 1.66 (0.77 to 3.54) | |
| Other or unknown | 1.74 (0.81 to 3.76) | 1.42 (0.55 to 3.65) | |
| Immigration background | 0.43 (0.10 to 1.81) | 0.38 (0.07 to 1.98) | |
| Single child | 0.92 (0.49 to 1.73) | 0.91 (0.41 to 2.05) | |
| School-related variables | |||
| Advanced secondary education | 0.26 (0.15 to 0.46) | 0.28 (0.14 to 0.58) | 0.28 (0.14 to 0.57) |
| Periods off school (vs never or very rarely) | |||
| Occasionally | 1.11 (0.61 to 2.02) | 1.29 (0.59 to 2.83) | 1.41 (0.69 to 2.87) |
| Often | 3.89 (2.00 to 7.54) | 5.04 (2.08 to 12.26) | 3.93 (1.79 to 8.62) |
| Perceived compromised by inflammatory bowel disease at school (vs not compromised) | |||
| Slightly, occasionally | 0.80 (0.47 to 1.35) | 1.22 (0.59 to 2.51) | |
| Substantially, frequently | 1.72 (0.93 to 3.17) | 0.66 (0.28, to1.57) | |
| Health-related variables | |||
| Age diagnosis*disease duration (vs 10+, >2 years duration) | |||
| 0–5 versus 10+ | 1.23 (0.61 to 2.48) | 2.14 (0.78 to 5.85) | 2.13 (0.81 to 5.61) |
| 6–9 versus 10+ | 0.85 (0.47 to 1.53) | 1.46 (0.70 to 3.08) | 1.31 (0.64 to 2.69) |
| 10+,<2 years duration | 0.49 (0.25 to 0.96) | 0.43 (0.18 to 1.01) | 0.52 (0.23 to 1.16) |
| Poor or moderate current health status (vs good health) | 1.08 (0.67 to 1.74) | 0.55 (0.28 to 1.08) | 0.6 (0.32 to 1.11) |
| Active disease course (vs remission during preceding 12 months) | 2.11 (1.26 to 3.53) | 3.18 (1.56 to 6.50) | 2.69 (1.37 to 5.26) |
Table 4.
Determinants of satisfaction (linear regression, OR and 95% CI for one unit increase in Child Healthcare Score)
| Bivariate | Full model | Parsimonious | |
| Sociodemographic variables | |||
| Being a girl | −0.05 (−0.21 to 0.11) | −0.13 (−0.30 to 0.04) | −0.15 (−0.32 to 0.02) |
| Age at survey (vs 13–14) | |||
| ≤12 | 0.02 (−0.17 to 0.21) | −0.15 (−0.36 to 0.06) | |
| ≥15 | 0.06 (−0.14 to 0.25) | 0.04 (−0.16 to 0.25) | |
| Region of residence (vs North Rhine-Westphalia) | |||
| North-west | 0.11 (−0.15 to 0.36) | 0.22 (−0.05 to 0.49) | 0.18 (−0.09 to 0.45) |
| South-west | 0.10 (−0.15 to 0.35) | 0.09 (−0.17 to 0.35) | 0.06 (−0.20 to 0.32) |
| Bavaria | 0.25 (−0.03 to 0.53) | 0.27 (−0.02 to 0.56) | 0.23 (−0.05 to 0.52) |
| North-east | 0.37 (0.06 to 0.68) | 0.44 (0.11 to 0.78) | 0.42 (0.09 to 0.76) |
| Saxony, Thuringia | 0.39 (0.12 to 0.67) | 0.31 (0.02 to 0.59) | 0.28 (0.00 to 0.57) |
| Austria, other | 0.48 (0.04 to 0.92) | 0.53 (0.06 to 1.00) | 0.51 (0.05 to 0.98) |
| Parental socioeconomic status (vs middle) | |||
| Low | 0.08 (−0.12 to 0.28) | 0.01 (−0.21 to 0.24) | 0.05 (−0.16 to 0.26) |
| High | 0.06 (−0.14 to 0.26) | 0.08 (−0.15 to 0.30) | 0.04 (−0.18 to 0.25) |
| Family situation (vs ‘classic’ family) | |||
| Single parent | 0.06 (−0.18 to 0.30) | 0.08 (−0.20 to 0.35) | |
| Other or unknown | 0.22 (−0.07 to 0.51) | 0.14 (−0.16 to 0.44) | |
| Immigration background | −0.18 (−0.54 to 0.17) | 0.10 (−0.29 to 0.5) | |
| Single child | −0.32 (−0.53 to –0.11) | −0.38 (−0.60 to −0.16) | −0.38 (−0.59 to −0.16) |
| School-related variables | |||
| Advanced secondary education | −0.09 (−0.25 to 0.07) | −0.13 (−0.32 to 0.05) | −0.13 (−0.32 to 0.05) |
| Grades (vs average student) | |||
| Mean two or better | 0.27 (0.09 to 0.46) | 0.32 (0.12 to 0.52) | 0.29 (0.09 to 0.49) |
| Mean worse than 3 | 0.32 (-0.53 to −0.12) | −0.35 (−0.57 to −0.14) | −0.34 (−0.55 to–0.13) |
| Periods off school (vs never or very rarely) | |||
| Occasionally | 0.11 (−0.07 to 0.30) | 0.07 (-0.13 to 0.26) | 0.06 (−0.14 to 0.25) |
| Often | −0.17 (−0.42 to 0.07) | −0.04 (−0.32 to 0.24) | −0.02 (−0.30 to 0.26) |
| Perceived compromised by inflammatory bowel disease at school (vs not compromised) | |||
| Slightly, occasionally | 0.28 (0.11 to 0.44) | 0.16 (−0.03 to 0.36) | 0.17 (−0.03 to 0.36) |
| Substantially, frequently | −0.31 (−0.54 to −0.08) | −0.12 (−0.4 to 0.16) | −0.14 (−0.41 to 0.14) |
| Health-related variables | |||
| Age diagnosis*disease duration (vs 10+, >2 years duration) | |||
| 0–5 vs 10+ | 0.15 (−0.12 to 0.42) | 0.24 (−0.08 to 0.55) | 0.14 (−0.15 to 0.43) |
| 6–9 vs 10+ | 0.14 (−0.07 to 0.35) | 0.15 (−0.08 to 0.38) | 0.08 (−0.13 to 0.29) |
| 10+,<2 years duration | 0.30 (0.08 to 0.51) | 0.23 (−0.01 to 0.47) | 0.18 (−0.04 to 0.41) |
| Poor or moderate current health status (vs good health) | −0.26 (-0.42 to –0.09) | −0.26 (−0.45 to −0.07) | −0.26 (−0.45 to −0.07) |
| Active disease course (vs remission during preceding 12 months) | −0.04 (-0.21 to 0.12) | 0.12 (-0.07 to 0.32) | 0.12 (-0.08 to 0.32) |
All comparisons were considered exploratory. Regression analyses were programmed in R V.3.4.4 (‘VGAM’ vs 1.0–5).34
Results
Response and sample description
Overall, 1367 families were contacted, of which 675 sent back sufficiently completed questionnaires (49.4%). The largest source were the CEDATA registry (n=276, 40.9% of participants) and the patient organisation mailing list (n=148, 21.9%). Baseline characteristics of the patients are shown in tables 5 and 6. Median age was 14 years. 404 (59.9%) had CD, 208 (30.8%) UC and 63 (9.3%) IBD_NS. Of all children, 438 (65.4%) were currently well, and 275 (41.2%) had been in stable remission over the preceding 12 months.
Table 5.
Patient characteristics by age group (age at survey)—sociodemographic data
| <14 years | 14+years | All | |
| Sex | |||
| Male | 189 (56.6%) | 210 (61.6%) | 399 (59.1%) |
| Female | 145 (43.4%) | 131 (38.4%) | 276 (40.9%) |
| Parental socioeconomic status | |||
| Lowest quintile (1) | 65 (19.6%) | 86 (25.6%) | 151 (22.6%) |
| Middle quintiles (2-4) | 180 (54.4%) | 193 (57.4%) | 373 (55.9%) |
| Highest quintile (5) | 86 (26.0%) | 57 (17.0%) | 143 (21.4%) |
| Region of residence | |||
| North-west | 56 (16.8%) | 61 (17.9%) | 117 (17.5%) |
| North Rhine-Westphalia | 61 (18.3%) | 68 (19.9%) | 129 (19.0%) |
| South-west and Middle | 70 (21.0%) | 69 (20.2%) | 139 (20.5%) |
| Bavaria | 44 (13.2%) | 49 (14.4%) | 93 (13.9%) |
| North-east | 35 (10.5%) | 31 (9.1%) | 66 (9.7%) |
| South-east | 52 (15.6%) | 53 (15.5%) | 105 (15.6%) |
| Austria, abroad, not known | 16 (4.8%) | 10 (2.9%) | 26 (3.9%) |
| Family situation | |||
| Single parent household | 33 (9.9%) | 52 (15.2%) | 85 (12.6%) |
| Type of school | |||
| Elementary | 33 (9.9%) | 0 (0%) | 33 (4.9%) |
| Basic | 26 (7.8%) | 17 (5.0%) | 43 (6.4%) |
| Intermediate | 77 (23.1%) | 127 (37.2%) | 204 (30.2%) |
| Advanced | 156 (46.7%) | 156 (45.7%) | 312 (46.2%) |
| Other, unclear, not reported | 42 (12.6%) | 41 (12.0%) | 83 (12.3%) |
| Migration status | |||
| Migration background | 18 (5.4%) | 16 (4.7%) | 34 (5.0%) |
| Number of siblings | |||
| Single child | 59 (17.7%) | 52 (15.2%) | 111 (16.4%) |
| One sibling | 185 (55.4%) | 175 (51.3%) | 360 (53.3%) |
| Two siblings | 69 (20.7%) | 85 (24.9%) | 154 (22.8%) |
| Three or more siblings | 21 (6.3%) | 29 (8.5%) | 50 (7.4%) |
| Total | 334 | 341 | 675 |
Table 6.
Patient characteristics type of disease—health-related information
| CD | UC | IBD_NS | All | |
| Age at diagnosis | ||||
| 0–5 years | 44 (11.1%) | 23 (11.3%) | 19 (30.6%) | 86 (13.0%) |
| 6–9 years | 139 (35.0%) | 73 (35.8%) | 19 (30.6%) | 231 (34.8%) |
| 10–13 years | 190 (47.9%) | 92 (45.1%) | 20 (32.3%) | 302 (45.6%) |
| >14 years | 24 (6.0%) | 16 (7.8%) | 4 (6.5%) | 44 (6.6%) |
| Course during last year | ||||
| Stable remission | 161 (40.4%) | 85 (41.3%) | 29 (46.0%) | 275 (41.2%) |
| One relapse | 116 (29.1%) | 49 (23.8%) | 20 (31.7%) | 185 (27.7%) |
| More relapses/chronically active | 122 (30.6%) | 72 (35.0%) | 14 (22.2%) | 208 (31.1%) |
| Current health status | ||||
| Good | 261 (65.1%) | 137 (66.5%) | 40 (63.5%) | 438 (65.4%) |
| Moderate | 115 (28.7%) | 46 (22.3%) | 19 (30.2%) | 180 (26.9%) |
| Poor | 25 (6.2%) | 23 (11.2%) | 4 (6.3%) | 52 (7.8%) |
| Disease duration | ||||
| <1 years | 57 (14.3%) | 29 (14.1%) | 11 (17.5%) | 97 (14.5%) |
| 1 to <2 years | 61 (15.3%) | 29 (14,1%) | 8 (12.7%) | 98 (14.7%) |
| 2 to <5 years | 167 (41.9%) | 84 (41.0%) | 17 (27.0%) | 268 (40.2%) |
| 5 years+ | 114 (8.5%) | 63 (30.7%) | 27 (42.9%) | 204 (30.7%) |
| Resecting surgery | ||||
| Has had surgery | 31 (7.7%) | 12 (5.8%) | 2 (3.2%) | 45 (6.7%) |
| Therapy | ||||
| Ever had corticosteroids | 284 (83.8%) | 153 (86.9%) | 36 (69.2%) | 473 (83.4%) |
| Ever had biological | 131 (32.4%) | 31 (14.9%) | 10 (15.9%) | 172 (25.5%) |
| Ever had immunomodulators | 334 (82.7%) | 137 (65.9%) | 27 (57.1%) | 498 (74.1%) |
| Total | 404 | 208 | 63 | 675 |
General school-related experience
A large majority of children reported they had generally gotten along well at school recently (38.8% reasonably well, 39.0% very well, overall n=555). Thirty-four (5.2%) children did not get on well, and 97 reported intermediate experience. Two hundred and eighty-five (42.2%) of the parents thought the child’s situation at school was not affected by the IBD; a similar proportion (288, 42.7%) reported occasional problems due to IBD, and 98 (14.5%) thought the school situation was substantially compromised due to the child’s IBD. Ninety-five children (14.1%) had not disclosed at school that they had the disease, 315 (46.7%) kept some secrecy (eg, restricted circle of persons or only certain aspects disclosed) and 260 (38.5%) were completely open about their IBD in school.
Asked about the current relative developmental stage of the child, 248 (36.7%) of the parents reported they perceived the child as physically lagging behind other children the same age. For the time before starting school, this proportion was reported as 15.9% (107 children). In contrast, there was no preschool-current time difference in the proportion of parents perceiving the children as below or behind in their mental development (same as other children of similar age: current: 511 (75.7%); preschool: 488 (72.3%).
Indicators of school performance and trajectory
Time missed from school
Within the preceding 2 weeks, 49 (7.3%) had missed 50% or more of classes and 130 (19.3%) had missed school for less than 50% of the classes. Repeated prolonged periods off school at any time during the course of the disease were reported for 100 children (14.8%). Slightly more than a quarter (187, 27.7%) had never had this problem.
Type of school attended
There were 33 children still at elementary school. Three hundred and twelve children (46.2%) attended ASE, 43 (6.4%) basic secondary and 204 (30.2%) intermediate schools. Attending ASE was more likely with high parental SES with an excessively high OR of 8.2 (95% CI 4.7 to 14.2) and less likely when parental SES was low (reference medium SES, table 1). Also, children from single parent families less often had ASE, as compared with those with both parents at home (OR 0.5, 95% CI 0.3 to 1.0). A migration background was more common in children in ASE, but this group was very small. Disease-related variables contributed to model fit, but none of them was associated with the outcome (table 1).
School marks, being a good student
Poor marks were rare: 21 and 4 of 675 children had failed Math and German respectively in the last term. In contrast, 189 (28.0%) had good marks in both subjects. Female sex, younger age, living in Saxony, high parental SES and attending ASE were all moderately associated with better marks, whereas disease-related factors had no impact (table 2).
Grade retention
Grade retention was reported in 84 children (12.4%). Seven had skipped a class and were subsequently combined with those with regular trajectory for analysis. There was a clear association with periods off school: Of 100 students who had experienced prolonged periods off schools, 28 (28.0%) had repeated a year (no or very rare periods: 9.1%) (OR 3.9, 95% CI 2.0 to 7.5). In the multivariate analysis, retention risk increased with low parental SES, time missed at school and an active disease course during the preceding year (table 3).
Satisfaction with the situation at school
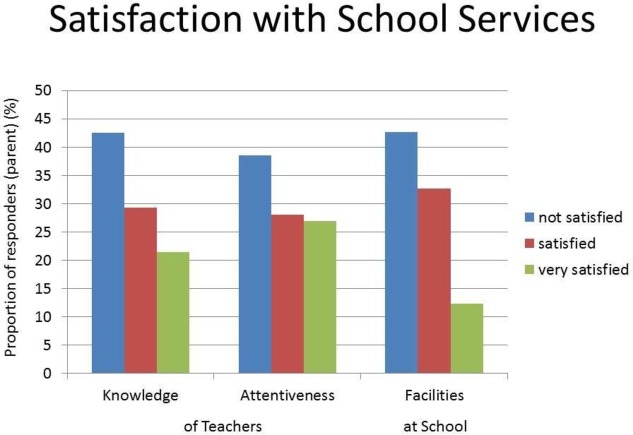
All items of the school services domain of the CHC-SUN showed low satisfaction in around 40%, and the lowest proportion of high satisfaction for health-related facilities (figure 1).
Figure 1.
Single item response—school services satisfaction.
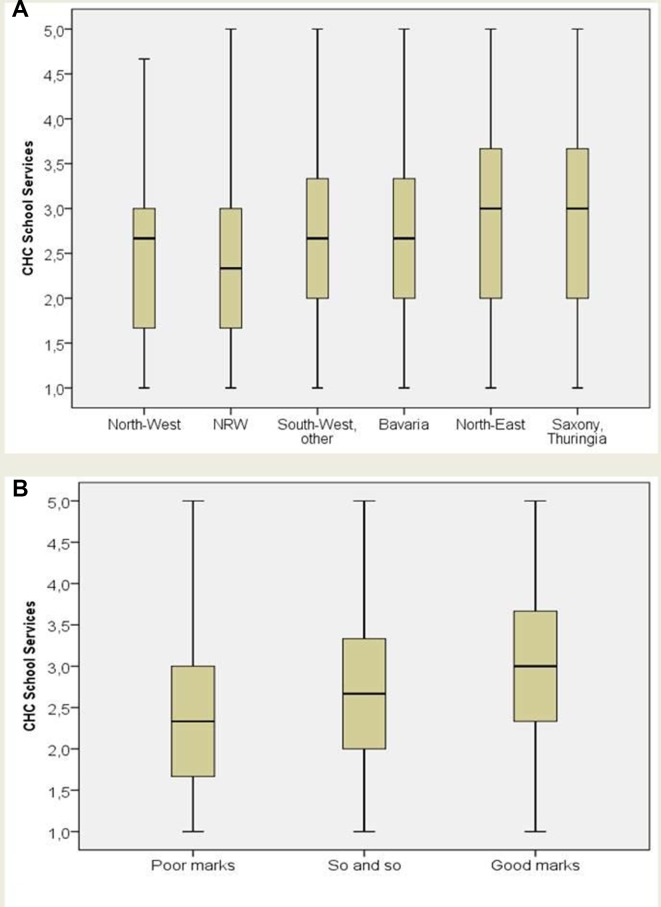
The summary score could be calculated for 630 persons. There was a clear trend of better scores with better school marks (figure 2). This was confirmed in the multivariate analysis (table 4). Also, satisfaction was higher in Eastern states as compared with West German regions. It was lower when the child was a single child, and when current health status was moderate or poor, as compared with good.
Figure 2.
Satisfaction score by (A) region and (B) school marks.
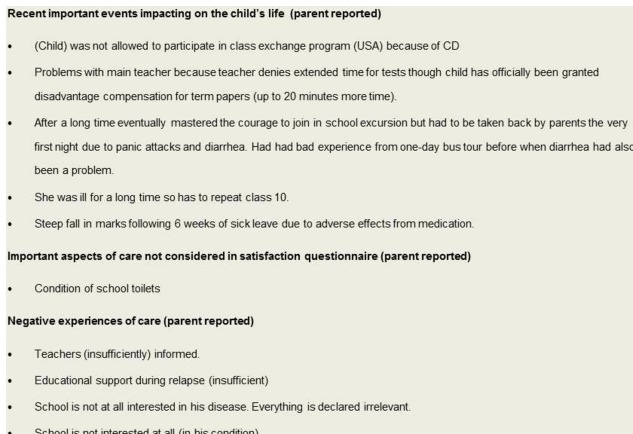
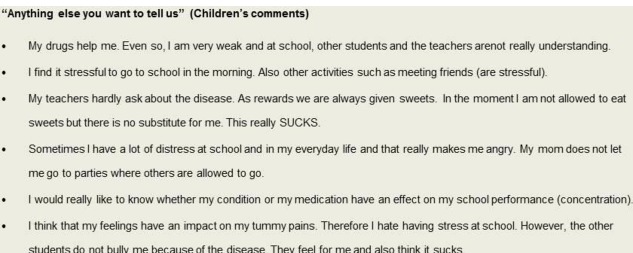
Anecdotal information, free text comments
All parental free text statements alluding directly to IBD at school are quoted in figure 3. In contrast to parents, many children used the occasion for last page comments. These often related to how they liked (or not liked) the questionnaire. All school-related children’s comments from this last question are listed in figure 4.
Figure 3.
Parents’ comments.
Figure 4.
Children’s comments.
Discussion
In this paper, we present data on school experience and performance from a large survey in German-speaking children with IBD. The most striking finding was the low satisfaction of parents with the situation at school. In contrast, of various indicators of school performance and trajectory, only grade retention was determined by disease-related variables. Around 15% of the children with IBD had repeatedly been off school in the past for prolonged periods of time due to the disease. For a similar proportion of children, parents felt the disease had a severe impact on school performance. Receiving ASE and getting good marks seemed to be unaffected by the disease, even if the course had been severe or many classes were missed.
Patient satisfaction scores are notoriously difficult to interpret due to the complex interplay between patient expectations and experience, or patient and provider characteristics, further confounded by a high variation in the way satisfaction is conceptualised and assessed.21 35 36 A common problem in satisfaction surveys are ceiling effects, in that high levels are commonly encountered even where quality of care is known to be deficient.37 Thus, the strikingly low school service satisfaction ratings, in particular in comparison with other domains of the instrument we used, are reason for concern. Stratification for various subgroups which might be particularly susceptible for lower quality school services did not render helpful results, as neither type of school nor severity of the disease showed convincing associations. Rather, it was the parents of children with poor marks who were particularly dissatisfied, while the parents of children with good marks were most satisfied. This may underline an impression that, as shown for health services research, in general, positive attitudes towards an organisation or provider will also lead to better satisfaction ratings, irrespective of other quality indicators.
Comparable data on school satisfaction in chronically ill children are scarce, and none had been available for IBD until recently. The parent-reported instrument we used has since been modified for self-report in German-speaking youth, based on a mixed sample of 182 chronically ill adolescents including 28 patients with gastrointestinal (GI) disease.38 In this study, 36% of patients in the GI group reported unmet needs relating to school or work, which was more than for any of the other disease groups (diabetes, multiple sclerosis, arthritis, skin disease, pulmonary conditions). With respect to the CHC-SUN, as in our survey, the school services subscore was lowest as compared with other domains in all patient groups, but in particular so for GI diseases. In fact, the mean score of 2.3 out of a maximum possible of 5 reported for this group was even lower than what was measured in our analysis. Thus, it seems that low satisfaction with school services is prevalent in chronically ill children, and in particular so in children with GI diseases.
It was not asked what exactly parents associate when asked about, for example, facilities at school, but there is reason to assume that the importance of clean and easy to reach toilets for persons with IBD may take effect in this point.12 39 Inappropriate provision and maintenance of lavatories in public schools in Germany has been the subject of public discussion for several years. A prominent online newspaper received, in 2015, 3000 parent letters relating to school services, of which a third reported their children avoided using toilets at school.40 It seems plausible that children with bowel disease would be even more sensitive to this issue. Similarly, embarrassment and privacy issues originating from insufficient knowledge of teachers are a particular concern. This is in concordance with the relatively low proportion of children who were completely open about the disease with teachers and fellow students (38.5%). In our survey, 15% kept the disease completely secret. Thus, there are specific challenges of suffering from bowel disease at school, reflected by the high proportion of reported unmet needs found by other investigators, even though this did not directly impact on educational success as measured by marks and ASE attendance, that is, expected type of school leaving degree.
Grade retention was the only indicator of school performance found to be associated with disease characteristics, hinting at a causal effect of having severe IBD. Most indicators of disease severity, as well as disease duration increased the risk for having to repeat a class. As an example, more than a quarter of those with a recent chronic active disease course had repeated a year. This was also related to prolonged periods off school. The absolute frequency is difficult to interpret. Retention policies vary by type of school, state within Germany, and over time. In some states, mark-based retention has been abolished altogether. In 2016/2017, Germany-wide, 2.3% of all children had to repeat a year, with state-specific proportions ranging from 1.3% in Berlin and Hamburg to 3.9% in Bavaria.41 Reliable cumulative rates are not available, but may well be higher than what we observed in children with less severe IBD in our study.
There is debate both nationally as in the international literature on the usefulness of having to repeat a class.42 43 In the context of long periods of missed time at school, getting more time may actually be considered beneficial by many children and their parents, in particular, as more than a third of the parents we surveyed reported their child with IBD to lag behind other children of similar age with respect to their physical development. Problems of self-esteem and social interaction deriving from delayed growth and puberty have been reported in the literature.44 45 We did not assess how the children felt about the retention. In any case, the mere fact of having to repeat a class is insufficient to judge whether this constitutes a problem to those concerned and whether it could have been avoided by appropriate support measures. We are currently performing a survey in children with IBD to find out more about any procedures in place to help students catch up with time missed from school, as well as their preferences.
For other indicators of school performance, specifically advanced schooling, beside state, parental SES was the most important influential factor of those available for evaluation in our survey. This association has been known and is generally interpreted as indicating social inequality within the German educational system.46 Also, the differences by state are not specific to IBD children, but reflect a known north-south gradient within Germany.41 From the perspective of caring for IBD, it is reassuring that disease related factors did not seem to have an impact.
It may seem unusual in our context of a clearly quantitative survey to narrate free text statements of patients. Of course, these constitute anecdotal evidence, expressed by a low number of single persons. The quotes cannot be considered in any way representative, and inference with respect to the relevance of the problems alluded to is not possible. They do, however, illustrate a few situations individual patients or parents considered particularly noteworthy and may help empathising with the special situation of being a child or adolescent (or his/her parent) with a chronic disease at school when planning and implementing further research, including interventions to improve the situation.
Our survey is strong in that it provides quantitative school related data from a large sample of young persons with IBD, using, wherever possible, validated instruments to collect information from both parents and children, with a focus on patient experience. There are a number of limitations. The most obvious derives from the fact that age appropriate schooling was one of several outcome indicators of quality of care in children, in a survey restricted to affected children. There were no healthy controls, so the actual burden afflicted by having the disease could not be quantified in absolute numbers. Moreover, while we appreciated the fact that good healthcare in chronically ill children is not just about physical health and vertical growth, we were in the end unprepared for the high importance parents placed on school-related issues. The endpoints chosen may insufficiently reflect how the school careers are affected by IBD, and we have now set up a study looking into support measures in more detail.
Generalisability may also be an issue. We have used a broad recruitment strategy in order to catch a wide spectrum of patients with IBD from different health contexts. Still, most patients were recruited via the paediatric specialist registry and the national patient organisation, both of which do not represent random samples of children with IBD. Rather, in combination with the response rate of around 50%, it is expected that we have surveyed parents with a particularly strong interest in the disease, better than average medical care and physician attachment, higher SES and higher compliance. This was also reflected by very low retention rates in patients with quiescent disease.
A specific challenge in examining school related factors is the very diverse German educational system. Education is organised on state level and has seen a number of major asynchronous structural changes over the last years comprominising comparability.46 47
Several factors could not be conclusively examined due to low numbers. This concerned, for example, residency in Austria, but also several vulnerable person groups, such as those a migration background. The unexpected positive association of migration background with ASE may be due to selection effects, in that underascertainment of non-German families was over-proportional in lower SES families.
Clinical studies typically use disease activity indices to describe disease severity, for which several items were not available to us.48 49 Recent disease course and parent global assessment of the child’s health may have been insufficiently sensitive to capture this aspect. We were in this survey generally focused on the patient perspective on the situation of care, thus dealing with perceptions. The degree to which what parents and children report would be substantiated by ‘objective’ measures remains questionable. However, in the end, it is the children who suffer the disease and have to live with the consequences, so even where findings remain vague and unexplained, there is reason for concern when a specific area of daily life is reported to represent a problem.
Conclusions
Our study shows, in accordance with the limited data in the literature, a high degree of dissatisfaction with health-related school services in parents of children with IBD. School trajectories in children with IBD take longer due to grade retention, but from our survey there is no indication that they will, in the end, result in poorer prospects on the job market, as school marks and type of school attended were not compromised. While school facilities and teachers’ knowledge and empathy seem the most obvious problems, more research is needed to identify promising targets and interventions for improvement. Our results may form a helpful basis in this respect.
Acknowledgments
We thank the team at BIPS, Bremen for support in organizing the survey, data editing and entry, data cleaning, plausibility testing and data management, Jan Thies Soller (Oldenburg) for support in preparing tables, Birgit Kaltz for providing input from the patient perspective, and all physicians contributing patients to this survey, including those associated with CEDATA-GPGE and the Saxonian Pediatric IBD registry. The German Crohn and Colitis Association (DCCV e.V.) for facilitating patient recruitment. All children and their parents sharing their experience by participating in this study.
Footnotes
Contributors: MF contributed to literature search, refinement of study questions, statistical analyses, first draft of the manuscript. AS contributed to statistics and non-standard multivariate analyses. SK and MC were consulting on the pediatric content of the study, pretesting of questionnaire, patient recruitment, review of manuscript. AB and MWL provided the pediatric expertise and contributed to the questionnaire development, patient recruitment and review of manuscript. JP was responsible for the coordination of survey and data collection, development and editing of questionnaires and data entry and review of manuscript. AT prepared the study concept and design; did the literature search, funding proposal, development of questionnaires; supervision of survey, statistical analysis and writing of manuscript. All authors contributed to and approved of the final manuscript.
Funding: This work was supported by a grant from the German Ministry of Education and Science (BMBF, Ripi Study, grant number FK 01GY1139).
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: Ethical approval was granted (Bremen University Ethics Committee, date of approval 12 March, 2013). Informed consent was secured after written information from parents or guardians, and the children.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data sharing is not possible due to patient consent excluding third party use of data. There are no additional unpublished data available.
References
- 1. Sawyer SM, Drew S, Yeo MS, et al. . Adolescents with a chronic condition: challenges living, challenges treating. Lancet 2007;369:1481–9. 10.1016/S0140-6736(07)60370-5 [DOI] [PubMed] [Google Scholar]
- 2. Rosen MJ, Dhawan A, Saeed SA. Inflammatory bowel disease in children and adolescents. JAMA Pediatr 2015;169:1053–60. 10.1001/jamapediatrics.2015.1982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kim SC, Ferry GD. Inflammatory bowel diseases in pediatric and adolescent patients: clinical, therapeutic, and psychosocial considerations. Gastroenterology 2004;126:1550–60. 10.1053/j.gastro.2004.03.022 [DOI] [PubMed] [Google Scholar]
- 4. Kugathasan S, Denson LA, Walters TD, et al. . Prediction of complicated disease course for children newly diagnosed with Crohn's disease: a multicentre inception cohort study. Lancet 2017;389:1710–8. 10.1016/S0140-6736(17)30317-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Duricova D, Fumery M, Annese V, et al. . The natural history of Crohn's disease in children: a review of population-based studies. Eur J Gastroenterol Hepatol 2017;29:125–34. 10.1097/MEG.0000000000000761 [DOI] [PubMed] [Google Scholar]
- 6. Fumery M, Duricova D, Gower-Rousseau C, et al. . Review article: the natural history of paediatric-onset ulcerative colitis in population-based studies. Aliment Pharmacol Ther 2016;43:346–55. 10.1111/apt.13478 [DOI] [PubMed] [Google Scholar]
- 7. Mackner LM, Greenley RN, Szigethy E, et al. . Psychosocial issues in pediatric inflammatory bowel disease: report of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr 2013;56:449–58. 10.1097/MPG.0b013e3182841263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Marri SR, Buchman AL. The education and employment status of patients with inflammatory bowel diseases. Inflamm Bowel Dis 2005;11:171–7. 10.1097/00054725-200502000-00011 [DOI] [PubMed] [Google Scholar]
- 9. Mackner LM, Bickmeier RM, Crandall WV. Academic achievement, attendance, and school-related quality of life in pediatric inflammatory bowel disease. J Dev Behav Pediatr 2012;33:1–11. 10.1097/DBP.0b013e318240cf68 [DOI] [PubMed] [Google Scholar]
- 10. Singh H, Nugent Z, Brownell M, et al. . Academic performance among children with inflammatory bowel disease: a population-based study. J Pediatr 2015;166:1128–33. 10.1016/j.jpeds.2014.12.010 [DOI] [PubMed] [Google Scholar]
- 11. Bernstein CN, Kraut A, Blanchard JF, et al. . The relationship between inflammatory bowel disease and socioeconomic variables. Am J Gastroenterol 2001;96:2117–25. 10.1111/j.1572-0241.2001.03946.x [DOI] [PubMed] [Google Scholar]
- 12. Schwenk HT, Lightdale JR, Arnold JH, et al. . Coping with college and inflammatory bowel disease: implications for clinical guidance and support. Inflamm Bowel Dis 2014;20:1618–27. 10.1097/MIB.0000000000000124 [DOI] [PubMed] [Google Scholar]
- 13. Ferguson A, Sedgwick DM, Drummond J. Morbidity of juvenile onset inflammatory bowel disease: effects on education and employment in early adult life. Gut 1994;35:665–8. 10.1136/gut.35.5.665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Calsbeek H, Rijken M, Bekkers MJ, et al. . School and leisure activities in adolescents and young adults with chronic digestive disorders: impact of burden of disease. Int J Behav Med 2006;13:121–30. 10.1207/s15327558ijbm1302_3 [DOI] [PubMed] [Google Scholar]
- 15. Rogler D, Fournier N, Pittet V, et al. . Coping is excellent in Swiss Children with inflammatory bowel disease: results from the Swiss IBD cohort study. J Crohns Colitis 2014;8:409–20. 10.1016/j.crohns.2013.10.004 [DOI] [PubMed] [Google Scholar]
- 16. Hummel TZ, Tak E, Maurice-Stam H, et al. . Psychosocial developmental trajectory of adolescents with inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2013;57:219–24. 10.1097/MPG.0b013e3182935474 [DOI] [PubMed] [Google Scholar]
- 17. Mayberry MK, Probert C, Srivastava E, et al. . Perceived discrimination in education and employment by people with Crohn's disease: a case control study of educational achievement and employment. Gut 1992;33:312–4. 10.1136/gut.33.3.312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Assa A, Ish-Tov A, Rinawi F, et al. . School attendance in children with functional abdominal pain and inflammatory bowel diseases. J Pediatr Gastroenterol Nutr 2015;61:553–7. 10.1097/MPG.0000000000000850 [DOI] [PubMed] [Google Scholar]
- 19. Timmer A, Schütte B, Peplies J. Versorgungsgerechtigkeit bei Kindern mit CED. Zwischeninformation zur Ripi-Befragungsstudie. Bauchredner 2015;1:63–6. [Google Scholar]
- 20. Timmer A, Stark R, Peplies J, et al. . Current health status and medical therapy of patients with pediatric-onset inflammatory bowel disease: a survey-based analysis on 1280 patients aged 10-25 years focusing on differences by age of onset. Eur J Gastroenterol Hepatol 2017;29:1276–83. 10.1097/MEG.0000000000000956 [DOI] [PubMed] [Google Scholar]
- 21. Crow R, Gage H, Hampson S, et al. . The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature. Health Technol Assess 2002;6:1–244. 10.3310/hta6320 [DOI] [PubMed] [Google Scholar]
- 22. Timmer A, Ahrens W. Regional inequality in paediatric inflammatory bowel disease: the effect of small area deprivation on outcomes in inflammatory bowel disease. Final Report of the RIPI-Study. Technische Informationsbibliothek 2015. [Google Scholar]
- 23. Scholz D, Behrens R, Claßen M. Patient registries as epidemiological tools. The Registry for Chronic Inflammatory Bowel Diseases CEDATA-GPGE] Kinder- und Jugendmedizin 2011;11:283–8. [Google Scholar]
- 24. Buderus S, Scholz D, Behrens R, et al. . Inflammatory bowel disease in pediatric patients: characteristics of newly diagnosed patients from the CEDATA-GPGE Registry. Dtsch Arztebl Int 2015;112:121–7. 10.3238/arztebl.2015.0121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Meier C, Thönneßen C, Rothe U. [Chronisch entzündliche Darmerkrankungen bei Kindern und Jugendlichen] Chronic inflammatory bowel disease in childhood and adolescence. Monatsschrift Kinderheilkunde 2006;154:1212–8. [Google Scholar]
- 26. Kurth BM, Kamtsiuris P, Hölling H, et al. . The challenge of comprehensively mapping children's health in a nation-wide health survey: design of the German KiGGS-Study. BMC Public Health 2008;8:196 10.1186/1471-2458-8-196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ravens-Sieberer U, Herdman M, Devine J, et al. . The European KIDSCREEN approach to measure quality of life and well-being in children: development, current application, and future advances. Qual Life Res 2014;23:791–803. 10.1007/s11136-013-0428-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Otley A, Smith C, Nicholas D, et al. . The IMPACT questionnaire: a valid measure of health-related quality of life in pediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2002;35:557–63. 10.1097/00005176-200210000-00018 [DOI] [PubMed] [Google Scholar]
- 29. Schmidt S, Thyen U, Chaplin J, et al. . Cross-cultural development of a child health care questionnaire on satisfaction, utilization, and needs. Ambul Pediatr 2007;7:374–82. 10.1016/j.ambp.2007.04.007 [DOI] [PubMed] [Google Scholar]
- 30. Schmidt S, Thyen U, Chaplin J, et al. . Healthcare needs and healthcare satisfaction from the perspective of parents of children with chronic conditions: the DISABKIDS approach towards instrument development. Child Care Health Dev 2008;34:355–66. 10.1111/j.1365-2214.2008.00815.x [DOI] [PubMed] [Google Scholar]
- 31. Jöckel KH, Babitsch B, Bellach BM. Measurement and quantification of sociodemographic characteristics in epidemiological studies. German Working Group on Epidemiological Methods of the GMDS and DGSMP 1997. [Google Scholar]
- 32. Winkler J, Stolzenberg H. Adjustment of the index of social class for application in the German Health Interview and Examination Survey for Children and Adolescents. Wismar Discussion Papers 2009. [Google Scholar]
- 33. Ananth CV, Kleinbaum DG. Regression models for ordinal responses: a review of methods and applications. Int J Epidemiol 1997;26:1323–33. 10.1093/ije/26.6.1323 [DOI] [PubMed] [Google Scholar]
- 34. Yee TW. Vector generalized linear and additive models: with an implementation in R. Springer, 2015. [Google Scholar]
- 35. Williams B. Patient satisfaction: a valid concept? Soc Sci Med 1994;38:509–16. 10.1016/0277-9536(94)90247-X [DOI] [PubMed] [Google Scholar]
- 36. Voutilainen A, Pitkäaho T, Vehviläinen-Julkunen K, et al. . Meta-analysis: methodological confounders in measuring patient satisfaction. J Res Nurs 2015;20:698–714. 10.1177/1744987115619209 [DOI] [Google Scholar]
- 37. Williams B, Coyle J, Healy D. The meaning of patient satisfaction: an explanation of high reported levels. Soc Sci Med 1998;47:1351–9. 10.1016/S0277-9536(98)00213-5 [DOI] [PubMed] [Google Scholar]
- 38. Schmidt S, Thyen U, Herrmann-Garitz C, et al. . The Youth Health Care measure-satisfaction, utilization, and needs (YHC-SUN)-development of a self-report version of the Child Health Care (CHC-SUN) proxy-measure. BMC Health Serv Res 2016;16:189 10.1186/s12913-016-1419-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pittet V, Vaucher C, Froehlich F, et al. . Patient self-reported concerns in inflammatory bowel diseases: a gender-specific subjective quality-of-life indicator. PLoS One 2017;12:e0171864 10.1371/journal.pone.0171864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Endres A, Erk E. [School toilets: use them here?]. ZEIT ONLINE - Die Zeit 2015:19.9.2015. [Google Scholar]
- 41. Hoffmann J, Malecki A. Schulen auf einen Blick In: Statistisches Bundesamt (Destatis), 2018. [Google Scholar]
- 42. Peixoto F, Monteiro V, Mata L, et al. . "To be or not to be Retained … That's the Question!" Retention, Self-esteem, Self-concept, Achievement Goals, and Grades. Front Psychol 2016;7:1550 10.3389/fpsyg.2016.01550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ehmke T, Sälzer C, Pietsch M, et al. . Competence development in the school year after PISA 2012: effects of grade retention. Zeitschrift für Erziehungswissenschaft 2017;20:99–124. [Google Scholar]
- 44. Mackner LM, Vannatta K, Crandall WV. Gender differences in the social functioning of adolescents with inflammatory bowel disease. J Clin Psychol Med Settings 2012;19:270–6. 10.1007/s10880-011-9292-x [DOI] [PubMed] [Google Scholar]
- 45. Greenley RN, Hommel KA, Nebel J, et al. . A meta-analytic review of the psychosocial adjustment of youth with inflammatory bowel disease. J Pediatr Psychol 2010;35:857–69. 10.1093/jpepsy/jsp120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Helbig M. Bildungsföderalismus und die ungleiche Verteilung von Bildungschancen. Wege aus dem Bildungsdilemma 2009;34. [Google Scholar]
- 47. Klemm K. Das Bildungssystem Deutschlands: Strukturen und Strukturreformen. Empirische Bildungsforschung: Springer, 2011: 153–64. [Google Scholar]
- 48. Ruemmele FM, Hyams JS, Otley A, et al. . Outcome measures for clinical trials in paediatric IBD: an evidence-based, expert-driven practical statement paper of the paediatric ECCO committee. Gut 2015;64:438–46. 10.1136/gutjnl-2014-307008 [DOI] [PubMed] [Google Scholar]
- 49. Siegel CA, Whitman CB, Spiegel BMR, et al. . Development of an index to define overall disease severity in IBD. Gut 2018;67:244–54. 10.1136/gutjnl-2016-312648 [DOI] [PubMed] [Google Scholar]