Abstract
Objective
The aim of this study was to evaluate the value of technetium-99m methoxyisobutylisonitrile (99mTc-MIBI) imaging and ultrasound in preoperative localization of parathyroid adenoma (PA) and parathyroid hyperplasia (PH).
Participants and methods
A retrospective study of 99mTc-MIBI double-phase scintigraphy (DPS) was performed in 187 hyperparathyroidism cases with pathologically diagnosed PA or PH. Of these patients, 167 cases underwent ultrasound, and 146 cases underwent 99mTc-MIBI single-photon emission computed tomography/computed tomography (SPECT/CT). The sensitivity and diagnostic accuracy of ultrasound, 99mTc-MIBI DPS, and SPECT/CT were compared between PA and PH. Differences in 99mTc-MIBI DPS, serum parathyroid hormone (PTH), serum calcium and phosphorus, as well as the weight and longest diameter of lesion between PA and PH were also compared.
Results
As per patient-based analysis, the sensitivity of ultrasound, 99mTc-MIBI DPS, and SPECT/CT was 90.70% (39/43), 95.56% (43/45), and 100.00% (30/30), respectively, for PA, and 93.55% (116/124), 90.85% (129/142), and 93.10% (108/116), respectively, for PH. There were no significant differences in sensitivity of these three imaging methods between PA and PH. However, per lesion-based analysis, the accuracy of ultrasound, 99mTc-MIBI DPS, and SPECT/CT in detecting PA was 78.43% (40/51), 86.79% (46/53) and 96.88% (31/32), respectively, and the accuracy of 99mTc-MIBI DPS was higher than that of ultrasound (χ2=6.507, P=0.011), and for PH, it was 49.69% (160/322), 40.71% (171/420), and 43.80% (152/347), respectively. The accuracy of ultrasound was higher than that of 99mTc-MIBI DPS (χ2=5.940, P=0.015). The accuracy of a combination of all three examinations of ultrasound+99mTc-MIBI DPS, ultrasound+99mTc-MIBI SPECT/CT, 99mTc-MIBI DPS+SPECT/CT, and ultrasound+99mTc-MIBI DPS+99mTc-MIBI SPECT/CT was 51.51% (154/299), 53.85% (161/299), 50.17% (150/299), and 54.18% (162/299), respectively, which was higher than that of ultrasound (χ2=5.273, P=0.022; χ2=8.226, P=0.004; χ2=3.880, P=0.049; χ2=8.702, P=0.003, respectively). Serum levels of PTH and phosphorus were lower in patients with PA than in patients with PH (P<0.001), and serum calcium level, the weight, and the longest diameter of lesion and early uptake rate of 99mTc-MIBI DPS were higher in patients with PA than in patients with PH (P<0.01). Serum PTH level is often less than 1000 pg/ml in PA, but usually more than 1000 pg/ml in PH.
Conclusion
Ultrasound, 99mTc-MIBI DPS, and SPECT/CT all have a higher value in the diagnosis of PA than PH. 99mTc-MIBI SPECT/CT should be optimal for detecting PA, and early SPECT/CT scan might be better than delayed scan. Compared with 99mTc-MIBI DPS and SPECT/CT, ultrasound has a slight advantage in localization of PH lesions. The combination of ultrasound and 99mTc-MIBI DPS or SPECT/CT imaging could improve the accuracy in localization of PH lesions and should be considered as the first-line method for detecting PH.
Keywords: adenoma, dual-phase, hyperplasia, parathyroid, single-photon emission computed tomography/computed tomography, technetium-99m methoxyisobutylisonitrile, ultrasound
Introduction
Hyperparathyroidism (HPT) is a series of clinical syndromes resulting in the disorder of parathyroid hormone (PTH), which leads to the disorder of calcium and phosphorus metabolism. Multiple organs and systems are often involved in the disease. Its clinical manifestations are complex and diverse, which often results in misdiagnosis and mistreatment of HPT. HPT could be divided into three types: primary hyperparathyroidism (PHPT), secondary hyperparathyroidism (SHPT), and tertiary hyperparathyroidism (THPT).
HPT is diagnosed through symptoms and blood tests, including serum PTH, serum calcium, serum phosphorus, urinary calcium, and serum alkaline phosphatase. The clinical diagnosis of PHPT is mainly based on hypercalcemia, hypophosphatemia, elevated urinary calcium (24 h Ca>200 mg), and elevated PTH.
HPT is usually caused by parathyroid adenoma (PA) and parathyroid hyperplasia (PH) and rarely by parathyroid carcinoma or cysts. Parathyroidectomy or minimally invasive parathyroidectomy is the most effective treatment for most HPT patients. The accurate preoperative location of lesion(s) causing PHPT is very important and necessary for successful surgical intervention.
There are several invasive and noninvasive techniques used for preoperative localization of hyperfunctioning parathyroid glands in patients with HPT. The invasive techniques, including arteriography, and PTH measurement in ultrasound-guided puncture fluid of parathyroid lesions or selective sampling from the jugular vein, are not commonly used to assist in preoperative planning. The noninvasive techniques include ultrasound, computed tomography (CT), MRI, and radionuclide scintigraphy and are often used for preoperative localization diagnosis. Previous studies have shown that CT and MRI, as anatomical techniques, have little clinical value in positioning diagnosis before parathyroidectomy. Ultrasound, as a simple and convenient method, has some advantages and may have clinical values in preoperative localization and diagnosis. Some researchers proposed that ultrasound should be the first choice because of its high sensitivity in locating PHPT 1,2. A meta-analysis showed that the sensitivity and positive predictive values of ultrasound for patients with PHPT were 76.1% [95% confidence interval (CI): 70.4–81.4%] and 93.2% (95% CI: 90.7–95.3%), respectively 2. Radionuclide scintigraphy, as a functional imaging technique, plays an important role in preoperative parathyroid localization, especially in ectopic HPT.
During the past few decades, radionuclide scintigraphy became a widely accepted technique for preoperative localization of HPT, and it has experienced several improvements constantly. In early 1960s, cobalt-60 vitamin B12 was used for parathyroid imaging. Digiulino and colleagues demonstrated that selenium-75 methionine (75Se-MET) could be used as a parathyroid imaging agent to locate ectopic parathyroid glands. Further research showed that 56.52% (13/23) of PA could be accurately located by 75Se-MET, and seven cases of PH were unable to be located 3–5. To date, parathyroid radionuclide scintigraphy included thallium-201 (201Tl)/technetium-99m methoxyisobutylisonitrile (99mTc-MIBI) subtraction scintigraphy,  /99mTc-MIBI subtraction scintigraphy, 99mTc-MIBI double-phase scintigraphy (DPS), 99mTc-MIBI single-photon emission computed tomography (SPECT), and 99mTc-MIBI SPECT/CT. Parathyroid 99mTc-MIBI scintigraphy is one of the most frequently used methods, and its mechanism involves uptake of 99mTc-MIBI by mitochondria-rich oxyphilic cells in PAs 6,7, and faster washing out of 99mTc-MIBI from normal parathyroid tissue compared with the lesion because of the higher expression of P-gp and GST-π in normal parathyroid tissue than in parathyroid lesion 8.
/99mTc-MIBI subtraction scintigraphy, 99mTc-MIBI double-phase scintigraphy (DPS), 99mTc-MIBI single-photon emission computed tomography (SPECT), and 99mTc-MIBI SPECT/CT. Parathyroid 99mTc-MIBI scintigraphy is one of the most frequently used methods, and its mechanism involves uptake of 99mTc-MIBI by mitochondria-rich oxyphilic cells in PAs 6,7, and faster washing out of 99mTc-MIBI from normal parathyroid tissue compared with the lesion because of the higher expression of P-gp and GST-π in normal parathyroid tissue than in parathyroid lesion 8.
Recent studies have found that fluorine-18-fluorodeoxyglucose, carbon-11-l-methionine, fluorine-18-choline, fluorine-18-fluorocholine PET, or PET/CT imaging could be used for the preoperative localization of PHPT 9–13. 99mTc-MIBI DPS was the most frequently used method to diagnose and position HPT and has shown a high sensitivity and specificity for PHPT, especially in ectopic HPT. A meta-analysis by Cheung et al. 2 showed that the sensitivity and positive predictive values of 99mTc-MIBI SPECT for patients with PHPT were 78.9% (95% CI: 64–90.6%) and 90.7% (95% CI: 83.5–96.0%), respectively.
Both PHPT and SHPT could be caused by PA or PH. Overall, 80–85% of PHPT cases are typically caused by a single-gland PA, less frequently in ~15–20% of cases by multigland PH, and rarely by parathyroid carcinoma 14. Many studies have focused on preoperative 99mTc-MIBI scintigraphy of PHPT or SHPT; however, there are conflicting reports on the accuracy of parathyroid 99mTc-MIBI scintigraphy in positioning HPT. The sensitivity and diagnostic accuracy of 99mTc-MIBI imaging in both a single lesion often caused by PA and multiple lesions often caused by PH were controversial 15–17. A meta-analysis including 471 patients from 24 studies declared that the pooled sensitivity and specificity of parathyroid 99mTc-MIBI scintigraphy in detecting PH in SHPT patients were 58% (95% CI: 52–65%) and 93% (95% CI: 85–100%), respectively 18. A recent study by Gordon et al. 19 including 54 patients showed that the sensitivity and specificity of 99mTc-MIBI scintigraphy in PH lesion positioning was 96 and 88%, respectively. However, Murphy and colleagues studied the radioactivity contained within excised neck tissues during radioguided parathyroidectomy in 320 patients with PA and 58 patients with PH, and according to the results, PA always contained an average of 56±9% (range: 18–136%) of background radioactivity, whereas PH had only 7.5±0.8% (range: 5.1–16%) 20. A study showed that 99mTc-MIBI imaging could distinguish PH from PA, because the sensitivity and specificity of 99mTc-MIBI imaging for PH were significantly lower than that for PA 21. Adalet and colleagues reported that the sensitivity of thallium-201/99mTc-MIBI subtraction imaging for PA was 71% (17/30), but for PH, the sensitivity was only 25% (6/20).
On the contrary, there were few studies focused on the differences in the value of preoperative localization of parathyroid 99mTc-MIBI scintigraphy between PA and PH. Therefore, the purpose of this retrospective study is to determine (a) whether there are differences in the accuracy and sensitivity of ultrasound, 99mTc-MIBI DPS, and 99mTc-MIBI SPECT/CT for the preoperative localization in patients with PA and PH, and (b) among ultrasound, 99mTc-MIBI DPS, and 99mTc-MIBI SPECT/CT, which technique has the highest accuracy for preoperative localization of lesion(s) causing HPT in patients with PH.
Participants and methods
Patients
Overall, 187 patients (76 males and 111 females) with biochemical evidence of HPT, who underwent a parathyroidectomy at our institute between July 2011 and May 2017, were included and analyzed retrospectively in this investigation. The average age of patients was 52.9±13.9 years (range: 10–83 years). For positioning the lesions, all patients underwent preoperative imaging; all 187 patients underwent 99mTc-MIBI DPS, 146 of them underwent 99mTc-MIBI SPECT/CT, 167 of them underwent high-resolution ultrasound, and 133 of them underwent all three examinations. According to the preoperative localization diagnosis and the results of operative exploration, subtotal included ablation of three glands and one-half of the fourth gland or total parathyroidectomy with implant was performed. The excised glands were sent for frozen sections, and on the basis of the histologic finding, 45 PA cases and 142 PH cases were confirmed. The width, length, and thickness of each lesion were recorded before histopathology examination, and then the volume of lesion was estimated according to the ellipsoid volume formula: lesion volume (ml)=π/6×width (cm)×length (cm)×depth (cm) 22. Lesion volume was assumed to represent lesion weight (1 ml equals 1 g) 23. The early uptake rate (EUR), delayed uptake rate (DUR), and the retention index (RI) of 99mTc-MIBI DPS, serum PTH, serum calcium and phosphorus, the weight, and the longest diameter of lesion between PA and PH was collected from individual medical case record/reports. This study was approved by the Ethics Committee of the First Affiliated Hospital of Xi’an Jiaotong University (Xi’an, China), and all participants provided written informed consent.
Parathyroid 99mTc-MIBI DPS and 99mTc-MIBI SPECT/CT
DPS of the head, neck, and chest area in anterior view was performed 15 min (early phase) and 120 min (delayed phase) after the intravenous injection of 740–1110 MBq (20–30 mCi) of 99mTc-MIBI (Beijing Atom High Tech Co. Ltd, Beijing, China), with 500 k counts/view. 99mTc-MIBI SPECT/CT was obtained 30 min after the 99mTc-MIBI injection. A Siemens Symbia T16 SPECT/CT scanner (Siemens, Erlangen, Germany) equipped with a dual-head low-energy high-resolution collimator was used for image acquisition, and 64 projections were acquired over 360° with an acquisition time of 30 s/view, a 20% energy window centered at a 140-keV photo peak, a 128×128 matrix, with a zoom factor of 1.45.
Ultrasound examination
Routine parathyroid ultrasound was performed using a Hitachi EUB-7500 HV ultrasound device (Hitachi Aloka Medical Ltd., Tokyo, Japan), preoperatively, with 6–13 MHz variable frequency linear probe. The patient is placed in a supine position. All parts of the anterior and lateral cervical area, the upper mediastinum, and the supraclavicular fossae should be evaluated at least in two orthogonal sections. The site, number, shape, size, boundary, echogenicity, and blood flow of the lesion(s) in parathyroid were noted.
Qualitative and semiquantitative analysis of 99mTc-MIBI DPS and 99mTc-MIBI SPECT/CT
The 99mTc-MIBI image and ultrasound were interpreted independently by two experienced nuclear medicine physicians or sonologists. Positive 99mTc-MIBI DPS result was a focal accumulation of the tracer in the early phase, which showed a fixed concentration or increasingly concentrated in the delayed phase (Fig. 1). For MIBI-positive parathyroid lesions, average counts of the diseased parathyroid gland and normal thyroid gland were obtained after a region of interest was drawn manually around each area; and for normal thyroid and that for MIBI false-negative parathyroid lesions, regions of interest were drawn in reference to the surgical findings. The parathyroid-to-thyroid counts ratio was determined using the average counts of the diseased parathyroid glands and normal thyroid glands 24. Then EUR, DUR, and RI of 99mTc-MIBI DPS were calculated: uptake ratio=average counts of the diseased parathyroid glands/average counts of normal thyroid glands, RI=(DUR−EUR)/EUR.
Fig. 1.
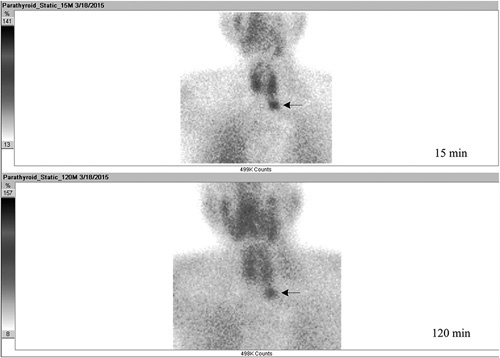
Positive 99mTc-MIBI DPS imaging. 15-min and 120-min 99mTc-MIBI DPS images showed an increasingly focal concentration in the left lower parathyroid glands (arrows). DPS, double-phase scintigraphy; 99mTc-MIBI, technetium-99m methoxyisobutylisonitrile.
Positive 99mTc-MIBI SPECT/CT result showed a fixed concentration in parathyroid, neck, or mediastinum on SPECT imaging, and an independent soft tissue mass in corresponding position was found on CT imaging (Fig. 2).
Fig. 2.
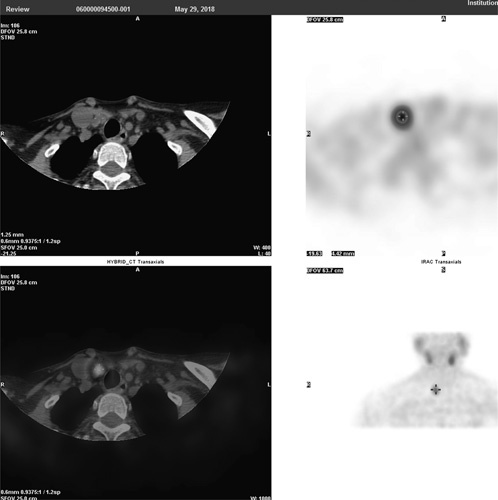
Positive 99mTc-MIBI SPECT/CT imaging. SPECT/CT transaxial slices imaging. CT showed a soft tissue density nodule localized in the right front of the trachea, and SPECT showed a focal uptake of 99mTc-MIBI in nodule. CT, computed tomography; DPS, double-phase scintigraphy; SPECT, single-photon emission computed tomography; 99mTc-MIBI, technetium-99m methoxyisobutylisonitrile.
Statistical analysis
Data were analyzed using SPSS, version 18.0 (SPSS Inc., Chicago, Illinois, USA). Continuous variables were expressed as mean±SD and analyzed by Student’s t-test. The χ2-test was used to compare categorical variables. Statistical significance was set at P less than 0.05.
Results
The sensitivity and accuracy of ultrasound, 99mTc-MIBI DPS, 99mTc-MIBI SPECT/CT, ultrasound+99mTc-MIBI DPS, ultrasound+99mTc-MIBI SPECT/CT, 99mTc-MIBI DPS+SPECT/CT, and ultrasound+99mTc-MIBI DPS+99mTc-MIBI SPECT/CT in PA
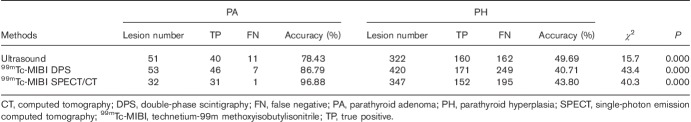
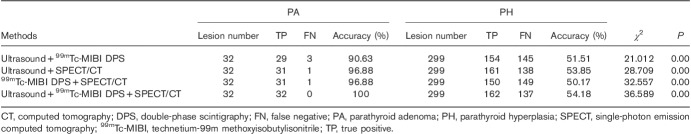
Per patient-based analysis in PA, the sensitivity of ultrasound, 99mTc-MIBI DPS, and 99mTc-MIBI SPECT/CT was 90.70% (39/43), 95.56% (43/45), and 100.00% (30/30), respectively (Table 1), and there was no significant difference between the three imaging methods for sensitivity. The sensitivity of ultrasound+99mTc-MIBI DPS, ultrasound+99mTc-MIBI SPECT/CT, 99mTc-MIBI DPS+SPECT/CT, and ultrasound +99mTc-MIBI DPS+SPECT/CT was 96.67% (29/30), 100.00% (30/30), 100.00% (30/30), and 100.00% (30/30) (Table 2), and there was no significant difference among the four groups.
Table 1.
On a per patient-based analysis, the sensitivity of 99mTc-MIBI DPS, 99mTc-MIBI SPECT/CT, and ultrasound in patients with PA and PH
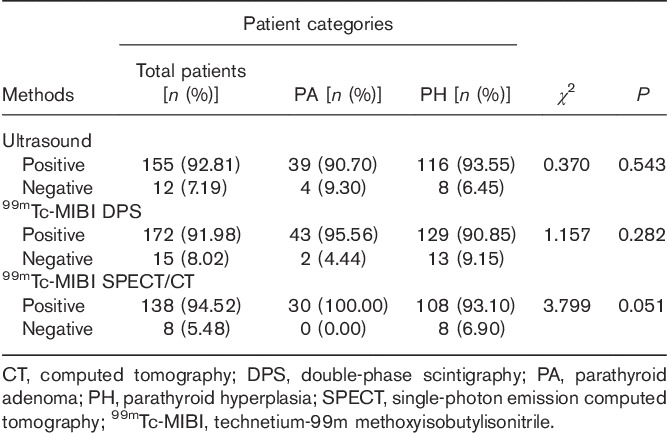
Table 2.
On a per patient-based analysis, the sensitivity of ultrasound+99mTc-MIBI DPS, ultrasound+99mTc-MIBI SPECT/CT, 99mTc-MIBI DPS+SPECT/CT, and ultrasound+99mTc-MIBI DPS+SPECT/CT with PA and PH in 133 cases who underwent all three examinations
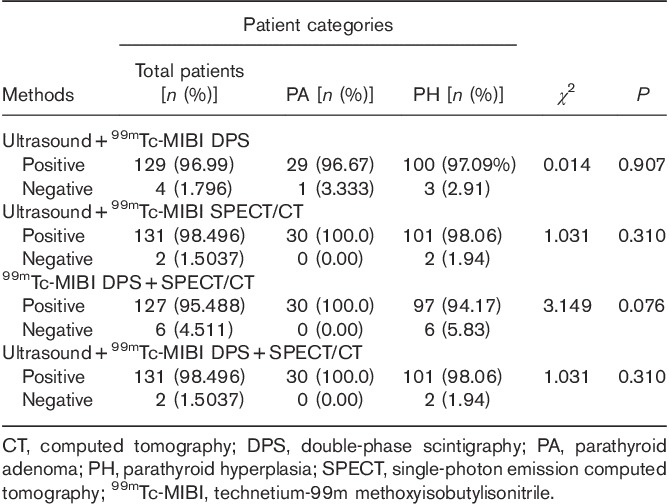
Per lesion-based analysis, the accuracy in PA of ultrasound, 99mTc-MIBI DPS, and 99mTc-MIBI SPECT/CT was 78.43% (40/51), 86.79% (46/53), and 96.88% (31/32), respectively (Table 3); the accuracy of SPECT/CT was higher than that of ultrasound (χ2=6.507, P=0.011), but there were no significant differences between 99mTc-MIBI DPS and UC (χ2=1.277, P=0.258), and between 99mTc-MIBI DPS and 99mTc-MIBI SPECT/CT (χ2=2.761, P=0.097). The accuracy in PA of ultrasound+99mTc-MIBI DPS, ultrasound +99mTc-MIBI SPECT/CT, 99mTc-MIBI DPS+SPECT/CT and ultrasound+99mTc-MIBI DPS+99mTc-MIBI SPECT/CT was 90.63% (29/32), 96.88% (31/32) and 96.88% (31/32), 100.00% (32/32) (Table 4), and there was no significant difference among the four groups.
Table 3.
On a per lesion-based analysis, the sensitivity of 99mTc-MIBI DPS, 99mTc-MIBI SPECT/CT, and ultrasound in patients with PA and PH
Table 4.
Per lesion-based analysis, the sensitivity of 99mTc-MIBI DPS, 99mTc-MIBI SPECT/CT, and ultrasound in patients with PA and PH in 133 cases who underwent all three examinations
The sensitivity and accuracy of ultrasound, 99mTc-MIBI DPS, 99mTc-MIBI SPECT/CT, ultrasound+99mTc-MIBI DPS, ultrasound+99mTc-MIBI SPECT/CT, 99mTc-MIBI DPS+SPECT/CT, and ultrasound+99mTc-MIBI DPS+99mTc-MIBI SPECT/CT in PH
Per patient-based analysis in PH, the sensitivity of ultrasound, 99mTc-MIBI DPS, and 99mTc-MIBI SPECT/CT was 93.55% (116/124), 90.85% (129/142), and 93.10% (108/116) in PH, respectively (Table 1), and no significant difference was found among the three methods for sensitivity in PH. The sensitivity of ultrasound+99mTc-MIBI DPS, ultrasound+99mTc-MIBI SPECT/CT, 99mTc-MIBI DPS+SPECT/CT, and ultrasound+99mTc-MIBI DPS+99mTc-MIBI SPECT/CT in PH was 97.09% (100/103), 98.06% (101/103), 94.17% (97/103), and 98.06% (101/103), respectively (Table 2), and no significant difference was found among the four groups.
Per lesion-based analysis in PH, the accuracy of ultrasound, 99mTc-MIBI DPS, and 99mTc-MIBI SPECT/CT was 49.69% (160/322), 40.71% (171/420), and 43.80% (152/347), respectively. The accuracy of ultrasound was higher than that of DPS (χ2=5.940, P=0.015), whereas no significant differences were found between 99mTc-MIBI DPS and 99mTc-MIBI SPECT/CT (χ2=0.744, P=0.388), and between SPECT/CT and ultrasound (χ2=2.325, P=0.127) (Table 3). The accuracy of ultrasound who underwent all three examinations was 42.14% (126/299). The accuracy of ultrasound+99mTc-MIBI DPS, ultrasound+99mTc-MIBI SPECT/CT, 99mTc-MIBI DPS+SPECT/CT and ultrasound+99mTc-MIBI DPS+99mTc-MIBI SPECT/CT was 51.51% (154/299), 53.85% (161/299), 50.17% (150/299), and 54.18% (162/299), respectively (Table 4), and it was higher than that of ultrasound (χ2=5.273, P=0.022; χ2=8.226, P=0.004; χ2=3.880, P=0.049; χ2=8.702, P=0.003, respectively).
As shown in Tables 3 and 4, ultrasound, 99mTc-MIBI DPS, SPECT/CT, ultrasound+99mTc-MIBI DPS, ultrasound+99mTc-MIBI SPECT/CT, 99mTc-MIBI DPS+SPECT/CT, and ultrasound+99mTc-MIBI DPS+99mTc-MIBI SPECT/CT all had better diagnostic accuracy for the preoperative localization of HPT lesion in patients with PA than in patients with PH.
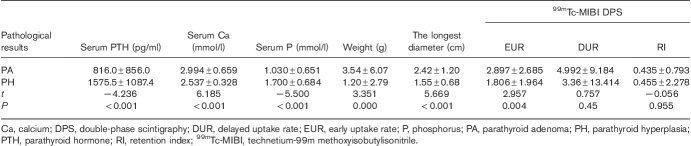
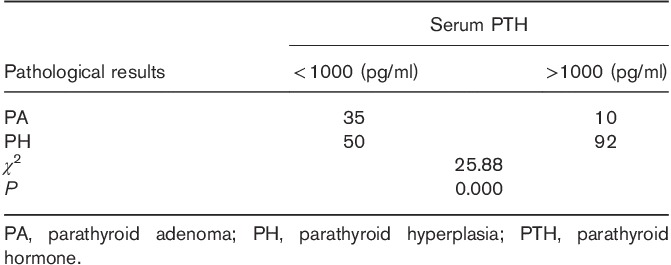
Comparison of serum PTH, calcium, phosphorus, lesion volume, and uptake of 99mTc-MIBI between PA and PH
Serum PTH and phosphorus levels were lower in patients with PA than in patients with PH (P<0.001), and the serum calcium level, the weight, and the longest diameter of lesion were significantly higher in PA than in PH (P<0.01). The EUR of 99mTc-MIBI in PA lesion was higher than that in PH lesion (P<0.05), but no statistically significant difference was found in DUR or RI of 99mTc-MIBI between PA and PH (P>0.05) (Table 5). Serum PTH level is often less than 1000 pg/ml in patients with PA, but usually more than 1000 pg/ml in patients with PH (Table 6).
Table 5.
Quantitative analysis of serum PTH, serum calcium, serum phosphorus, lesion size, and uptake of 99mTc-MIBI in PA and PH
Table 6.
Qualitative analysis of serum PTH in PA and PH
Discussion
This study showed that no matter on a per patient-based or lesion-based analysis, ultrasound, 99mTc-MIBI DPS, and 99mTc-MIBI SPECT/CT have high sensitivity and detection rate in presurgical positioning for patients with PA, and ultrasound and 99mTc-MIBI DPS have similar ability to localize PA lesions preoperatively. 99mTc-MIBI SPECT/CT is theoretically advantageous over other imaging methods because it provides the accurate location, the anatomy information, and functional status of parathyroid lesions. More importantly, radionuclide scintigraphy is considered as functional imaging, has high detection rate for HPT, and is superior to other preoperative parathyroid localization techniques, especially in ectopic HPT, so 99mTc-MIBI SPECT/CT should be the best method for preoperative localization in patients with PA or PHPT 25,26. Previous studies showed that PAs weighing more than 1.0 g have greater than 95% sensitivity 27, weighing more than 0.5 g have greater than 90% sensitivity 28, even adenomas as small as 210 mg correspond to a predicted correct localization of 80.2% (95% CI: 68.4–88.3%) for 99mTc-MIBI SPECT/CT 29.
A meta-analysis including 1236 PHPT patients indicated that no matter on a per patient-based analysis or on a per lesion-based analysis, the detection rate of 99mTc-MIBI SPECT/CT ranged from 64 to 100%, with a pooled estimate of 88% (95% CI: 84–92%) 26. Because of 80–85% of PHPT cases caused by PA, our finding is consistent with this review. Therefore, our results show clearly that ultrasound, 99mTc-MIBI DPS, and 99mTc-MIBI SPECT/CT all have a high value in the diagnosis of PA, and 99mTc-MIBI imaging is the best method for positioning PA, which was found in some PHPT studies 25.
There were a few studies focused on the lesion detection of 99mTc-MIBI imaging in patients with PH, and the sensitivity and accuracy of 99mTc-MIBI imaging was assessed, but the results of these studies were controversial. Some researchers demonstrated that 99mTc-MIBI imaging had a high sensitivity and specificity to locate PH lesions or multiple lesions 17,19,30–32, but others hold the opposite view 20,21,33–35. In our study, on a per patient-based analysis, ultrasound, 99mTc-MIBI DPS, and SPECT/CT showed high sensitivity in PH localization. It seems to indicate that all of the three methods had high clinical value for patients with PH. However, a patient with PH may have multiple lesions, for example, an average of 2.96 lesions in a patient with PH in our study. Therefore, the sensitivity and accuracy on a per lesion-based analysis could reflect the clinical value better than that on a per patient-based analysis (Fig. 3).
Fig. 3.
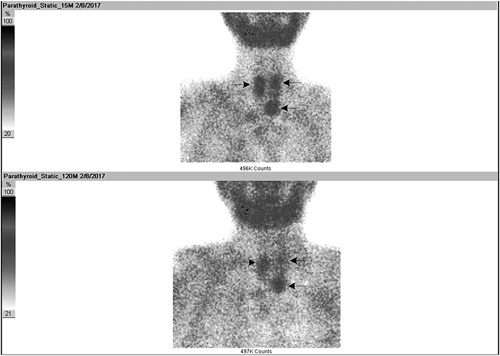
99mTc-MIBI DPS showed three lesions in a patient with PH. A 36-year-old male, presented with HPT. 15-min and 120-min 99mTc-MIBI DPS images showed three lesions in the left upper, left lower, and right upper parathyroid glands (arrows), and PH was further confirmed by surgery and pathology. DPS, double-phase scintigraphy; HPT, hyperparathyroidism; PH, parathyroid hyperplasia; 99mTc-MIBI, technetium-99m methoxyisobutylisonitrile.
Our study showed that the combination of ultrasound and 99mTc-MIBI DPS or SPECT/CT imaging could improve the accuracy in localization of PH lesions and should be considered as the first-line method for detecting PH. Although all of the three methods have an inadequate diagnostic accuracy for PH, the accuracy of ultrasound, 99mTc-MIBI DPS, and 99mTc-MIBI SPECT/CT in PH was only 49.69, 40.71, and 43.80%, respectively, and compared with 99mTc-MIBI DPS and 99mTc-MIBI SPECT/CT, ultrasound has better accuracy for the detection of PH. In additional, ultrasound has the advantage of being simple, cheap, and convenient, with no radioactivity.
Currently, the optimal imaging moment to perform parathyroid 99mTc-MIBI SPECT or SPECT/CT is still controversial 36–41. In the study, there was significant difference in EUR, but no difference in DUR and RI between PA and PH; it indicated that early 99mTc-MIBI SPECT/CT improved sensitivity and detection rate of locating HPT, and was better than delayed 99mTc-MIBI SPECT/CT.
In addition, serum PTH and phosphorus levels were lower in PA than in PH. Serum PTH was often less than 1000 pg/ml in PA, but usually more than 1000 pg/ml in PH. Serum calcium, glandular size, weight, and the longest diameter of lesion were higher in PA than in PH. These indexes could aid in the differential diagnosis of PA and PH. Increased serum PTH levels lower than 1000 pg/ml, large and single lesion, and positive 99mTc-MIBI imaging often suggest a PA lesion, whereas where the small and multilesions, increased serum PTH level more than 1000 pg/ml, and negative 99mTc-MIBI imaging finding are observed, the possibility of false-negative results of 99mTc-MIBI imaging caused by PH should be considered.
Limitations of this study
For a retrospective investigation study, surgery was done only after localization examinations, and the calculated sensitivity was affected, which were the limitations of this study.
Conclusion
Ultrasound, 99mTc-MIBI DPS, and SPECT/CT all have a high diagnostic value in PA. 99mTc-MIBI SPECT/CT is superior to other two techniques and should be optimal for detecting PA. Early SPECT/CT imaging is better than delayed imaging; the possible reason is that the uptake of 99mTc-MIBI was related to mitochondria-rich oxyphilic cells, and the washing out of 99mTc-MIBI was related to the higher expression of P-gp and GST-π in parathyroid lesion(s). The three methods have an inadequate accuracy for PH, but compared with 99mTc-MIBI DPS and SPECT/CT, ultrasound ultrasound has a slight advantage in localization of PH lesions. The combination of ultrasound and 99mTc-MIBI DPS or SPECT/CT imaging could improve the accuracy in localization of PH lesions and should be considered as the first-line method for detecting PH.
Acknowledgements
Conflicts of interest
There are no conflicts of interest.
Footnotes
*Jianjun Xue and Yan Liu contributed equally to the writing of this article.
References
- 1.Mihai R, Simon D, Hellman P. Imaging for primary hyperparathyroidism-an evidence-based analysis. Langenbeck Arch Surg 2009; 394:765–784. [DOI] [PubMed] [Google Scholar]
- 2.Cheung K, Wang TS, Farrokhyar F, Roman SA, Sosa JA. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol 2012; 19:577–583. [DOI] [PubMed] [Google Scholar]
- 3.Colella AC, Pigorini F. Experience with parathyroid scintigraphy. AJR 1970; 109:714–723. [DOI] [PubMed] [Google Scholar]
- 4.Digiulino W, Beierwaltes WH. Parathyroid scanning with selenium-75 labelled methionine. J Nucl Med 1964; 5:417–427. [PubMed] [Google Scholar]
- 5.Digiulio W, Morales JO. The Value of the selenomethionine se 75 scan in preoperative localization of parathyroid adenomas. JAMA 1969; 209:1873–1880. [PubMed] [Google Scholar]
- 6.Bénard F, Lefebvre B, Beuvon F, Langlois MF, Bisson G. Rapid washout of technetium-99m-MIBI from a large parathyroid adenoma. J Nucl Med 1995; 36:241–243. [PubMed] [Google Scholar]
- 7.Piñero A, Rodriguez JM, Martinez-Barba E, Canteras M, Stiges-Serra A, Parrilla P. Tc99m-sestamibi scintigraphy and cell proliferation in primary hyperparathyroidism: a causal or casual relationship? Surgery 2003; 134:41–44. [DOI] [PubMed] [Google Scholar]
- 8.Xue J, Liu Y, Yang D, Yu Y, Geng Q, Ji T, et al. Dual-phase 99mTc-MIBI imaging and the expression of P-gp, GST-π, and MRP1 in hyperparathyroidism. Nucl Med Commun 2017; 38:868–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neumann DR, Esselstyn CB, MacIntyre WJ, Chen EQ, Go RT, Kohse LM. Parathyroid adenoma localization by PET FDG. J Comput Assist Tomogr 1993; 17:976–977. [DOI] [PubMed] [Google Scholar]
- 10.Sundin A, Johansson C, Hellman P, Bergström M, Ahlström H, Jacobson GB, et al. PET and parathyroid l-[carbon-11]methionine accumulation in hyperparathyroidism. J Nucl Med 1996; 37:1766–1770. [PubMed] [Google Scholar]
- 11.Quak E, Lheureux S, Reznik Y, Bardet S, Aide N. F-18-choline, a novel PET tracer for parathyroid adenoma? J Clin Endocr Metab 2013; 98:3111–3112. [DOI] [PubMed] [Google Scholar]
- 12.Michaud L, Burgess A, Huchet V, Lefèvre M, Tassart M, Ohnona J, et al. Is 18F-fluorocholine positron emission tomography/computerized tomography a new imaging tool for detecting hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism? J Clin Endocr Metab 2014; 99:4531–4536. [DOI] [PubMed] [Google Scholar]
- 13.Thanseer N, Bhadada SK, Sood A, Mittal BR, Behera A, Gorla AKR, et al. Comparative effectiveness of ultrasonography, 99mTc-sestamibi, and 18F-fluorocholine PET/CT in detecting parathyroid adenomas in patients with primary hyperparathyroidism. Clin Nucl Med 2017; 42:e491–e497. [DOI] [PubMed] [Google Scholar]
- 14.Dugonjić S, Šišić M, Radulović M, Ajdinović B. Positive 99mTc-MIBI and the subtraction parathyroid scan are related to intact parathyroid hormone but not to total plasma calcium in primary hyperparathyroidism. Hell J Nucl Med 2017; 20:46–50. [DOI] [PubMed] [Google Scholar]
- 15.Nichols KJ, Tomas MB, Tronco GG, Rini JN, Kunjummen BD, Heller KS, et al. Preoperative parathyroid scintigraphic lesion localization: accuracy of various types of readings. Radiology 2008; 248:221–232. [DOI] [PubMed] [Google Scholar]
- 16.Elaraj DM, Sippel RS, Lindsay S, Sansano I, Duh QY, Clark OH, et al. Are additional localization studies and referral indicated for patients with primary hyperparathyroidism who have negative sestamibi scan results? Arch Surg 2010; 145:578–581. [DOI] [PubMed] [Google Scholar]
- 17.Berber E, Parikh RT, Ballem N, Garner CN, Milas M, Siperstein AE. Factors contributing to negative parathyroid localization: an analysis of 1000 patients. Surgery 2008; 144:74–79. [DOI] [PubMed] [Google Scholar]
- 18.Caldarella C, Treglia G, Pontecorvi A, Giordano A. Diagnostic performance of planar scintigraphy using 99mTc-MIBI in patients with secondary hyperparathyroidism: a meta-analysis. Ann Nucl Med 2012; 26:794–803. [DOI] [PubMed] [Google Scholar]
- 19.Gordon L, Burkhalter W, Mah E. Dual-phase 99mTc-sestamibi imaging: its utility in parathyroid hyperplasia and use of immediate/delayed image ratios to improve diagnosis of hyperparathyroidism. J Nucl Med Technol 2002; 30:179–184. [PubMed] [Google Scholar]
- 20.Murphy C, Norman J. The 20% rule: a simple, instantaneous radioactivity measurement defines cure and allows elimination of frozen sections and hormone assays during parathyroidectomy. Surgery 1999; 126:1028–1029. [DOI] [PubMed] [Google Scholar]
- 21.Johnston LB, Carroll MJ, Britton KE, Lowe DG, Shand W, Besser GM, et al. The accuracy of parathyroid gland localization in primary hyperparathyroidism using sestamibi radionuclide imaging. J Clin Endocr Metab 1996; 81:346–352. [DOI] [PubMed] [Google Scholar]
- 22.Gupta Y, Ahmed R, Happerfield L, Pinder SE, Balan KK, Wishart GC. P-glycoprotein expression is associated with sestamibi washout in primary hyperparathyroidism. Br J Surg 2007; 94:1491–1495. [DOI] [PubMed] [Google Scholar]
- 23.de Bruin TW, Croon CD, de Klerk JM, van Isselt JW. Standardized radioiodine therapy in Graves’ disease: the persistent effect of thyroid weight and radioiodine uptake on outcome. J Intern Med 1994; 236:507–513. [DOI] [PubMed] [Google Scholar]
- 24.Takebayashi S, Hidai H, Chiba T, Takagi Y, Nagatani Y, Matsubara S. Hyperfunctional parathyroid glands with 99mTc-MIBI scan: semiquantitative analysis correlated with histologic findings. J Nucl Med 1999; 40:1792–1797. [PubMed] [Google Scholar]
- 25.Hindié E, Zanotti-Fregonara P, Tabarin A, Rubello D, Morelec I, Wagner T, et al. The role of radionuclide imaging in the surgical management of primary hyperparathyroidism. J Nucl Med 2015; 56:737–744. [DOI] [PubMed] [Google Scholar]
- 26.Treglia G, Sadeghi R, Schalin-Jäntti C, Caldarella C, Ceriani L, Giovanella L, et al. Detection rate of 99mTc-MIBI single photon emission computed tomography (SPECT)/CT in preoperative planning for patients with primary hyperparathyroidism: a meta-analysis. HeadNeck 2016; 38:e2159–e2172. [DOI] [PubMed] [Google Scholar]
- 27.Vijayakumar V, Anderson ME. Detection of ectopic parathyroid adenoma by early Tc-99m sestamibi imaging. Ann Nucl Med 2005; 19:157–159. [DOI] [PubMed] [Google Scholar]
- 28.Gotthardt M, Lohmann B, Behr TM, Bauhofer A, Franzius C, Schipper ML, et al. Clinical value of parathyroid scintigraphy with technetium-99m methoxyisobutylisonitrile: discrepancies in clinical data and a systematic metaanalysis of the literature. World J Surg 2004; 28:100–107. [DOI] [PubMed] [Google Scholar]
- 29.Sandqvist P, Nilsson IL, Grybäck P, Sanchez-Crespo A, Sundin A. SPECT/CT’s advantage for preoperative localization of small parathyroid adenomas in primary hyperparathyroidism. Clinical Nuclear Medicine 2017; 42:e109–e114. [DOI] [PubMed] [Google Scholar]
- 30.Wong KK, Gandhi A, Viglianti BL, Fig LM, Rubello D, Gross MD. Endocrine radionuclide scintigraphy with fusion single photon emission computed tomography/computed tomography. World J Radiol 2016; 8:635–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wong KK, Chondrogiannis S, Bowles H, Fuster D, Sánchez N, Rampin L, et al. Hybrid-fusion SPECT/CT systems in parathyroid adenoma:technological improvements and added clinical diagnostic value. Rev Esp Med Nucl Imagen Mol 2016; 35:385–390. [DOI] [PubMed] [Google Scholar]
- 32.Mohebati A, Shaha AR. Imaging techniques in parathyroid surgery for primary hyperparathyroidism. Am J Otolaryngol 2012; 33:457–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Adalet I, Hawkins T, Clark F, Wilkinson R. Thallium–technetium-subtraction scintigraphy in secondary hyperparathyroidism. Eur J Nucl Med 1994; 21:509–513. [DOI] [PubMed] [Google Scholar]
- 34.Pattou F, Huglo D, Proye C. Radionuclide scanning in parathyroid diseases. Br J Surg 1998; 85:1605–1616. [DOI] [PubMed] [Google Scholar]
- 35.Milas M, Wagner K, Easley KA, Siperstein A, Weber CJ. Double adenomas revisited: nonuniform distribution favors enlarged superior parathyroids (fourth pouch disease). Surgery 2003; 134:995–1003. [DOI] [PubMed] [Google Scholar]
- 36.Hayakawa N, Nakamoto Y, Kurihara K, Yasoda A, Kanamoto N, Miura M, et al. A comparison between 11C-methionine PET/CT and MIBI SPECT/CT for localization of parathyroid adenomas/hyperplasia. Nucl Med Commun 2015; 36:53–59. [DOI] [PubMed] [Google Scholar]
- 37.Lezaic L, Rep S, Sever MJ, Kocjan T, Hocevar M, Fettich J. 18F-Fluorocholine PET/CT for localization of hyperfunctioning parathyroid tissue in primary hyperparathyroidism: a pilot study. Eur J Nucl Med Mol Imaging 2014; 41:2083–2089. [DOI] [PubMed] [Google Scholar]
- 38.Im HJ, Lee IK, Paeng JC, Lee KE, Cheon GJ, Kang KW, et al. Functional evaluation of parathyroid adenoma using 99mTc-MIBI parathyroid SPECT/CT: correlation with functional markers and disease severity. Nucl Med Commun 2014; 35:649–654. [DOI] [PubMed] [Google Scholar]
- 39.Keidar Z, Solomonov E, Karry R, Frenkel A, Israel O, Mekel M. Preoperative [99mTc]MIBI SPECT/CT interpretation criteria for localization of parathyroid adenomas-correlation with surgical findings. Mol Imaging Biol 2017; 19:1–6. [DOI] [PubMed] [Google Scholar]
- 40.Lavely WC, Goetze S, Friedman KP, Leal JP, Zhang Z, Garret-Mayer E, et al. Comparison of SPECT/CT, SPECT, and planar imaging with single-and dual-phase 99mTc-sestamibi parathyroid scintigraphy. J Nucl Med 2007; 48:1084–1089. [DOI] [PubMed] [Google Scholar]
- 41.García-Talavera P, Díaz-Soto G, Montes AA, Villanueva JG, Cobo A, Gamazo C, et al. Contribution of early SPECT/CT to 99mTc-MIBI double phase scintigraphy in primary hyperparathyroidism: diagnostic value and correlation between uptake and biological parameters. Rev Esp Med Nucl Imagen Mol 2016; 35:351–357. [DOI] [PubMed] [Google Scholar]