Abstract
Background
Patient complaints can provide valuable insights into the quality and safety of clinical care. Studies examining the epidemiology of complaints in out-of-hours general practice internationally are limited.
Aim
To characterise patient complaints in an out-of-hours general practice setting.
Design and setting
Retrospective cohort study of patient complaints to an out-of-hours service provider in Dublin, Ireland, over a 5-year period (2011–2016). This comprises nurse-led telephone triage and GP consultations for patients with urgent problems.
Method
A modified version of the UK Healthcare Complaints Analysis Tool (HCAT) was utilised to code complaints, which were reviewed independently in duplicate by two academic GPs.
Results
Of 445 598 telephone contacts, 303 085 resulted in face-to-face GP consultations. Of 234 patients who made 298 complaints, 185 (79%) related to GP care. The remainder related to nurse triage, other staff, and management issues. A total of 109 (46%) related to children aged ≤18 years, and 134 (58%) of complainants were female. There were 0.61 complaints per 1000 GP consultations. Most complaints (n = 126, 42%) were in relation to clinical care problems, largely diagnosis and prescribing. Common themes included unmet management expectations and clinical examination dissatisfaction. Inter-rater reliability was 90% (κ statistic 0.84, 95% confidence interval = 0.80 to 0.88). Following internal investigation, 158 (85%) of GP-related complaints were managed effectively by the out-of-hours service.
Conclusion
The majority of complaints related to clinical care problems and were successfully managed locally. Expectation management may be an important way to mitigate the risk of complaints.
Keywords: cohort studies, general practice, out-of-hours medical care, patient complaints, retrospective studies
INTRODUCTION
Patient complaints can provide valuable insights into the quality and safety of clinical care, acting as independent assessors of the healthcare service, and often reflect the expectations of society as a whole.1–4 Their role is different from that of peer assessment, and fulfils another purpose in promoting patient safety. When a patient makes a formal complaint, a threshold of dissatisfaction has been reached, and such complaints have been shown to highlight deficiencies in the quality and safety of health care.5 To maximise learning, it is critical to have an evidence-based and robust system of reviewing and using such complaints, and to implement change where needed.2
GPs providing out-of-hours care are at risk of facing patient complaints. An Australian study that analysed 18 907 formal complaints against doctors (2000–2011) reported that 47% related to GPs.5 In a 1-year retrospective case review (n = 526 complaints against GPs) by the Medical Protection Society (MPS), a total of 86 (16%) related to care provided in the out-of-hours setting.6 A Dutch study of 250 randomly selected disciplinary complaints against family physicians (2008–2010) reported that 45 (18%) originated in out-of-hours care.7
In terms of complaint content, a systematic review which included 59 primary studies reported that approximately one-third of complaints relate to the safety and quality of clinical care, one-third to the management of the healthcare organisation, and one-third to healthcare staff and patient communication.1 This review highlighted limitations in current approaches to analysing healthcare complaints, including the standardisation of the application of existing tools.1
Interestingly, only four studies included in this systematic review were conducted either principally or partially in primary care, highlighting the need for further research in this setting. Owen et al retrospectively analysed 1000 UK complaints regarding GP principals (1982–1989) randomly selected from the MPS database.8 Failure to perform a home visit was the main reason for complaints in this study.8 A German study that examined 13 505 formal national healthcare commission complaints (2004–2007), reported that unjust policies (23.8%), refusal or restriction of drugs (23.8%), and refusal or restriction of non-drug treatments (23.9%) were the main categories of complaints.9 An Australian study that analysed 18 907 formal complaints against doctors (2000–2011), of which 47% related to GPs, reported that the main categories of complaint were in relation to clinical care (61%), communication (23%), and other issues (for example, fees, access to care, or confidentiality).5 Another Australian study that focused solely on complaints concerning informed consent reported that, of 218 formal complaints, 11 (5%) were made in relation to GPs.10 The aim of the present study was to characterise patient complaints in an out-of-hours general practice setting over a 5-year period.
How this fits in
Research focusing on patient complaints in out-of-hours general practice is limited. This study found that the overall prevalence of patient complaints was 0.61 per 1000 consultations. The most common reason for complaints related to clinical care (diagnosis and prescribing) problems, in particular unmet patient expectations regarding management, and dissatisfaction with clinical examination. The majority (85%) of GP complaints were successfully resolved locally.
METHOD
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines were used in the conduct and reporting of this study.11
Study design, population, and setting
This retrospective cohort study examined all patient complaints recorded by Northdoc in Dublin, Ireland, over a 5-year period (1 January 2011 to 31 December 2016). Northdoc provides GPs for D-Doc, the out-of-hours GP service for all patients registered with a participating GP in North Dublin, Ireland, presenting with urgent medical problems. The Health Services Executive (HSE), the body responsible for public healthcare provision, provides the infrastructure for the service, including employment of triage nurses and administrative staff. The service operates from 18.00 to 08.00 Monday to Friday, and additionally provides a 24-hour service on Saturday, Sunday, and all public holidays. The service consists of nurse-led telephone triage and GP consultations in five treatment centres across North Dublin, and via home visits where necessary. A robust complaints process is in place, with complaints managed centrally and investigated internally by a designated complaints manager who is a GP and holds responsibility for maintaining records.
Complaint definition and coding of complaints
For the purposes of this study, a patient complaint was defined as ‘a verbal or written complaint made to and addressed by the Northdoc out-of-hours GP service complaints manager’. Anonymised designated complaints files containing written records of each complaint and any additional relevant correspondence were reviewed independently in duplicate by two experienced academic GPs, independent of Northdoc, with disagreements resolved by a third reviewer. In addition, anonymised patient consultation records relevant to the patient complaint were reviewed. A standardised template was used to extract relevant data.
A recent systematic review that included 59 studies reporting healthcare complaint coding tools revealed significant limitations with the way healthcare complaints are analysed.1 These issues include absence of an established taxonomy for categorising healthcare complaints, minimal standardisation of the procedures involved (for example, coding guidelines and training), absence of testing for reliability, and no assessment of complaint severity.
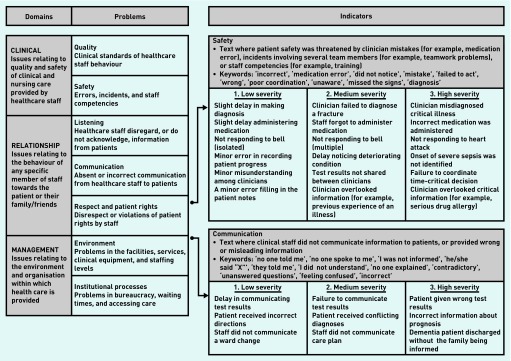
To address these limitations, the Healthcare Complaints Analysis Tool (HCAT) was developed in 2015 by aggregating the coding taxonomies from studies included in the systematic review, revealing 729 uniquely worded codes that were then refined and conceptualised into seven categories and three broad domains.1,12 The three domains are clinical, management, and relationship problems, and subcategories are outlined in Appendix 1. The HCAT has been tested for both reliability and accuracy in assessing healthcare complaints relating to UK inpatient care.13 A detailed handbook for applying the tool has been developed, in addition to online training materials.12
Applying the HCAT
According to the HCAT, there are four phases to coding a healthcare complaint. Phase A involves identifying the presence of a problem category (and subcategory if required) using the coding taxonomy provided, and assessing the severity using examples provided in the HCAT to guide the process (Appendix 2). Phase B involves specifying the stage of care in which the problem arose. Phase C involves rating the level of harm experienced by the patient as a result of the reported problem. Phase D involves providing descriptive information about the complaint.12 Patient level of harm is rated according to the UK National Reporting and Learning System and was coded from 1–5, as outlined in Appendix 3.14 Assessment is focused on the harm caused by the problems raised in the detail of the complaint and is rated independently of the severity of the complaint. For example, a high-severity complaint, such as a serious prescribing error, may not have resulted in any patient harm.
Piloting of the HCAT and modifications
As the HCAT was developed for use in inpatient settings, it required some modifications to the problem subcategories and severity indicators (Phase A) and stage of care (Phase B) for application to GP complaints. The HCAT was piloted on a sample of 20 general practice out-of-hours patient complaints by two academic GPs, who first completed online training regarding the application of the tool.
Following piloting, an additional sub-categorisation of ‘fees’ was included in the ‘management problems’ section. In contrast to the UK, where the HCAT was developed, Ireland has a mixed private–public healthcare system. Approximately 47% of the population receive free medical care through the General Medical Services (GMS) scheme and Doctor Visit Only (DVO) schemes.15 These schemes are means tested, but in 2015 free GP care (including out-of-hours) was introduced for all children aged ≤6 years. Second, further examples of severity indicators relevant for GP complaints were included, summarised in Appendix 2. Third, further options were included for the stage of care where the problem arose, as follows:
clinical examination;
diagnosis;
prescribing;
referral; and
other.
Illustrative examples of applying the HCAT to letters of complaint are available from the authors on request.
In addition to the HCAT coding, the outcome of the complaint following investigation was recorded as follows:
successfully defended to the mutual agreement of both parties;
defended but closed without agreement between parties;
complaint upheld and formal apology; or
complaint not GP related so referred to an alternative agency.
Statistical analysis
Descriptive statistics for the study participants are presented, in addition to the prevalence and incidence of patient complaints.
RESULTS
Descriptive statistics
There were a total of 445 598 telephone contacts to the out-of-hours nurse-led triage service from 2012–2016, of which 303 085 resulted in face-to-face GP consultations. A total of 234 patients made 298 complaints; 185 (79%) related to GP care. The remaining complaints related to nurse triage, other administrative staff, and other management issues (Table 1). Of the 234 patients who made complaints, 109 (46%) related to children aged ≤18 years, with the majority of these relating to children aged ≤5 years (Table 1). A total of 134 (58%) complaints related to female patients, and 98 (42%) were in receipt of free medical care (GMS card).
Table 1.
Descriptive statistics of study population 2012–2016 (n = 234)
| n (%) | |
|---|---|
| Age, yearsa | |
| ≤5 | 85 (36) |
| 6–17 | 23 (10) |
| ≥18–64 | 103 (44) |
| ≥65 | 22 (9) |
| Sexb | |
| Male | 98 (42) |
| Female | 134 (58) |
| General Medical Services (GMS) cardc | |
| Yes | 98 (42) |
| No | 127 (55) |
| Complainant | |
| Parent/guardian | 109 (46) |
| Patient | 88 (38) |
| Son/daughter | 11 (5) |
| Spouse/partner | 10 (4) |
| Other family member | 9 (4) |
| Healthcare professional | 5 (2) |
| Other | 2 (1) |
| Staff member complaint relates to | |
| GP | 185 (79) |
| Triage nurse | 8 (3) |
| Administrative staff | 6 (3) |
| Multiple healthcare professionals | 3 (1) |
| Other | 32 (14) |
Age was missing for one person.
Sex was missing for two people.
GMS card details missing for nine people.
The overall prevalence of patient complaints against GPs over the 5-year period was 0.61 per 1000 GP consultations. The annual rate of patient complaints per 1000 GP consultations remained relatively stable over time, with 0.81 in 2012, 0.56 in 2013, 0.69 in 2014, 0.56 in 2015, and 0.45 in 2016. Following the completion of an internal investigation by the complaints manager, 30 complaints (16%) against GPs were upheld and resulted in a formal apology to the complainant. This represents an annual rate of 0.18 per 1000 GP consultations. The remaining GP-related complaints were successfully defended to the satisfaction of both parties (n = 128, 69%), or were closed without agreement (n = 27, 15%).
Of the 30 upheld complaints, 13 related to a clinical problem, five to a management problem, and eight to a relationship problem. Four complaints were coded across multiple categories. Of the clinical problems, eight related to prescribing and four to diagnosis.
Categorisation of patient complaints
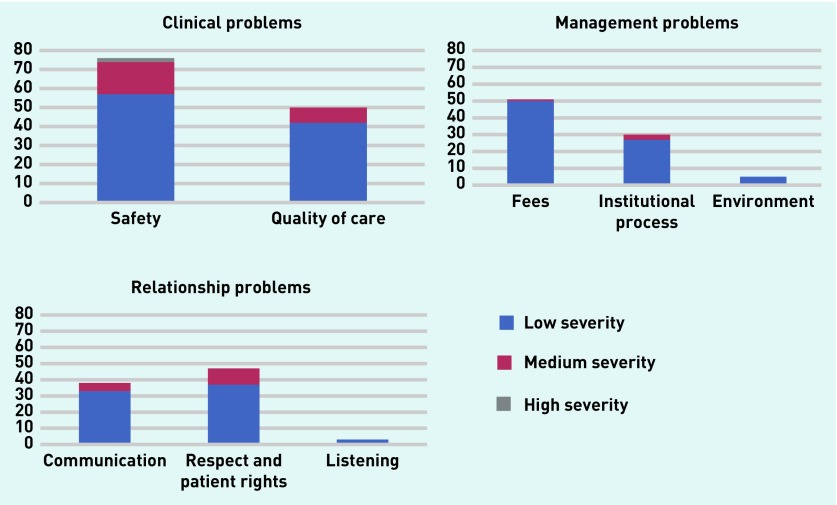
A total of 298 complaints relating to care received by 234 patients were made (Figure 2). Inter-rater reliability was 90%, with a κ statistic of 0.84 (95% confidence interval [CI] = 0.80 to 0.88). The majority of complaints (n = 126, 42%) related to clinical care. These complaints were further subcategorised according to clinical safety complaints (n = 76) and quality of care complaints (n = 50), and largely related to issues with diagnosis, prescribing, and referral (Table 2). Common themes included dissatisfaction with clinical examination and unmet expectations regarding management (for example, parental dissatisfaction that oral antibiotics were not prescribed to a child diagnosed with a viral infection).
Figure 2.
Complaints according to complaint category, subcategory, and severity (n = 298 complaints relating to n = 234 patients).
Table 2.
Clinical problem category complaints: stage of care and level of patient harm (n = 126)
| n (%) | |
|---|---|
| Stage of care | |
| Clinical examination | 20 (16) |
| Diagnosis | 45 (36) |
| Prescription | 46 (37) |
| Referral | 9 (7) |
| Other | 6 (4) |
| Level of patient harm | |
| No/minimal | 102 (81) |
| Minor | 19 (15) |
| Moderate | 4 (4) |
| Major | 1 (1) |
| Catastrophic | 0 (0) |
Of 45 complaints regarding diagnosis, five objective misdiagnoses were identified, which resulted in either moderate (n = 4) or major (n = 1) patient harm (Table 2). No misdiagnosis resulted in catastrophic harm. The majority of patient complaints regarding diagnosis related to the development of a recognised complication of their index visit condition, or a deterioration in a correctly diagnosed condition, subsequently misconstrued as a misdiagnosis. Similarly, of 46 complaints related to prescriptions, seven objective prescription errors were identified (for example, wrong dose of medication, prescription of a medication to a patient with known medication allergy, or incorrect treatment protocol used), which resulted in negligible or minor patient harm. The majority of prescription-related complaints resulted from unmet patient expectations regarding management (for example, oral antibiotics not prescribed when not clinically indicated), the type of medication prescribed (for example, oral formulation prescribed rather than intramuscular administration), the dose prescribed, or the duration of the prescription. In some cases, these complaints arose as a result of comments made to the patient by other healthcare professionals, such as other doctors or pharmacists (n = 14).
A total of 86 complaints (29%) related to relationship problems between the healthcare provider and patient. These were further subcategorised as issues regarding respect and patient rights (n = 47), communication issues (n = 36), and listening problems (n = 3). Common themes included perceived rudeness, abrupt manner, inadequate explanation of diagnosis or management plan, or dissatisfaction with the approach of the GP to the consultation. Finally, 86 complaints (29%) related to management problems subcategorised as issues regarding fees (n = 51), institutional processes (n = 30), and the environment (n = 5). Common fee complaint themes included dissatisfaction with payment for review consultations, refund requests if the patient subsequently attended their own GP or self-presented to the emergency department in the course of the same illness, and refund requests if patient expectations of the consultation were not met (for example, prescription of medication or referral). Other themes related to waiting time to see the GP, suitability of infrastructure (for example, building or consultation rooms), and triage processes (for example, triaged to treatment centre rather than a home visit, or triaged as routine rather than urgent home visit).
DISCUSSION
Summary
This study found that approximately one out of every 2000 GP consultations in this out-of-hours setting resulted in a patient complaint. This rate is similar to a previous Irish study examining out-of-hours GP complaints (2010–2013) in a different geographical location, where the reported complaint rate ranged from 0.49 to 0.77 per 1000 GP consultations.16 In the current study, complainants were most frequently parents on behalf of their child.
Approximately 40% of complaints related to clinical problems, with the remainder concerned with management issues and relationship problems between the patient and healthcare provider. Clinical problems were related to diagnosis, prescribing, and management. For diagnosis, the majority of complaints were due to the development of a known complication or subsequent deterioration in a correctly diagnosed index condition. There were five objective misdiagnoses that resulted in moderate (n = 4) or major (n = 1) patient harm. No misdiagnosis resulted in catastrophic harm. The majority of prescription complaints related to unmet management expectations. There were seven objective prescription errors identified, which included prescription of a medication to a patient with a known allergy, incorrect medication dose prescribed, and incorrect treatment protocol utilised. No prescription error resulted in moderate or severe patient harm.
The remainder of complaints related to management problems (29%) and relationship problems (29%). Management problems concerned issues with fees, institutional processes, and the environment. Fee complaints largely related to requests for refunds and dissatisfaction with paying for multiple out-of-hours consultations. Relationship problems were largely about breakdown in communication where the complainant perceived the healthcare provider to be rude, abrupt, or lacking empathy. Other relationship issues related to inadequate explanation of the management plan.
The majority (85%) of patient complaints against GPs were managed effectively by the out-of-hours service This highlights the value of local complaints resolution structures in general practice settings.
This study offers valuable insights into the epidemiology and content of patient complaints in out-of-hours general practice. The majority of complaints related to clinical care problems and were successfully managed locally. Expectation management may be one way of mitigating the risk of complaints.
Strengths and limitations
This study includes 5 years of data from a large out-of-hours care provider with a robust complaints system in place. All complaints were independently reviewed in duplicate by two experienced academic GPs using a validated coding system, amended for use in general practice. The number of participants with missing data was very low (Table 1). A limitation of the study was that the authors did not examine healthcare provider factors (for example, age, sex, years of clinical experience, or history of previous complaints) associated with complaints. Additionally, the case mix in the out-of-hours setting is different from routine general practice, as this service is designed to assess and manage urgent rather than routine problems. Therefore, the types of complaints encountered in out-of-hours care may not reflect routine general practice complaints. In addition, this study was conducted in an out-of-hours GP provider with an established complaints service, which may have influenced resolution rates.
Comparison with existing literature
International literature focusing on out-of-hours general practice complaints is very limited.17,18 A recent Dutch study examined the concept of patient safety culture across 16 out-of-hours GP cooperatives and two call centres in the Netherlands.19 Of 784 responders (of which 470 were GPs, and 189 were triage nurses), healthcare providers were most positive about teamwork, climate, and job satisfaction, and less about communication, openness, and safety climate. In the UK, the National Statistics Office produces an annual overview of written complaints against primary care healthcare professionals (including GPs, pharmacists, clinical therapists, and dentists). During 2016–2017, 65 637 complaints against GPs were resolved: 24 243 (37%) were upheld, 8809 (13%) were partially upheld, and 32 315 (50%) were not upheld.20 In the current study, 16% of all complaints were upheld, representing a smaller proportion of total complaints compared with routine UK general practice. However, out-of-hours Irish general practice is a different setting, with a different case mix from routine UK general practice. There is currently very limited literature on which to base comparisons. For GP practices, most complaints related to issues regarding communication (16.9%), clinical treatment (13.7%), and staff attitude, behaviour, and values (12.6%).20 Most complaints in the current study related to clinical problems (42%), with the remainder relating to management and relationship problems.
It is important to consider the reliability of current complaints coding systems and, more broadly speaking, how useful patient complaints are in identifying patient safety incidents. A systematic review published in 2014 identified several different taxonomies developed for the purpose of coding patient complaints, but methodologies varied considerably.1 A retrospective Dutch study of 1145 medical records concerning patient contacts with four out-of-hours GP cooperatives identified 27 patient safety incidents, an incident rate of 2.4% (95% CI = 1.5% to 3.2%).21 The most frequent incident type was treatment related (56%), with the majority not resulting in patient harm (70%).21 Another Dutch inpatient study (n = 5375, 14 hospitals) examined how reliable patient complaints, malpractice claims, and healthcare professional incident reports were in identifying patient safety incidents.22 Of a total of 498 adverse events detected, only 18 (3.6%) were identified by patient complaints and claims and/or healthcare professional incident reports.22 This highlights that, although patient complaints are an important part of examining overall patient safety and patient experience, they are not a substitute for having robust systems in place to regularly audit care. Therefore it is important to have multiple approaches in place to identify patient safety incidents, as all modalities have their limitations.
Implications for research and practice
In the current study, unmet patient expectations were a driver for many complaints, including parental expectation of antibiotic treatment for their child that was not deemed clinically indicated by the GP. There are many contributing factors to parental expectation of antibiotic treatment, including prior experience with receiving oral antibiotics and knowledge regarding the appropriate use of antibiotics.23,24 A large-scale Irish survey (n = 7487 participants aged ≥15 years) published in 2017 reported that 49% of responders believed that antibiotics were effective against viruses.25 It is important for GPs to actively address patient expectations during the consultation, while accepting that providing evidence-based care is not without risk of complaints. A recent Cochrane systematic review examining clinician interventions to influence antibiotic prescribing behaviour for acute respiratory infections in primary care reported that point-of-care testing (for example, for C-reactive protein) and shared decision making were effective in reducing antimicrobial prescribing.26 Another systematic review that focused on interventions to reduce antibiotic prescriptions for childhood upper respiratory tract infections reported that educational interventions targeting both parents and clinicians were most effective.27
A systematic review examining the epidemiology of malpractice claims in primary care internationally reported that the commonest medical misadventure resulting in claims was failure to or delay in diagnosis, which represented 26–63% of all claims across included studies.28 However, the majority of claims were successfully defended.28 In the current study, the number of objective misdiagnoses and prescription errors were very small. Interestingly, the development of a recognised complication of a correctly diagnosed condition, or a deterioration in a condition, were often misconstrued by complainants as diagnostic errors. It is important for GPs to communicate potential complications and prognosis, where feasible. However, as it is impossible to predict all clinical outcomes, safety netting is essential.29
In the UK, an external review of out-of-hours GP providers reported that some providers did not inform patients how they could make complaints about the service.30 From a clinical governance perspective, having robust complaints procedures in place is essential.
Acknowledgments
The authors wish to thank the Northdoc Board and staff for facilitating this study, in particular Dr Desmond MacDonell, Liam Quinn, and Alicja Konkol.
Appendix 1.
Healthcare Complaints Analysis Tool (modified): categorisation of complaints
| Complaint category and subcategories | Examples of complaint type |
|---|---|
| Clinical problems | |
| Quality of care (clinical standards of health care and behaviour) |
|
| Safety (errors and clinician competency) |
|
| Management problems | |
| Environment (facilities, clinical equipment, staffing levels) |
|
| Institutional process (waiting times, accessing care) |
|
| Fees |
|
| Relationship problems | |
| Listening |
|
| Communication |
|
| Respect and patient rights |
|
Appendix 2. The Healthcare Complaints Analysis Tool (HCAT). Reproduced with permission of the authors.13
Appendix 3. Coding of patient harm: UK National Reporting and Learning System
| Code | Description |
|---|---|
| 1) Negligible/minimal | No or minimal intervention required to ameliorate harm |
| 2) Minor | Minor intervention required to ameliorate harm — for example, needed to see GP |
| 3) Moderate | Significant intervention required to ameliorate harm — for example, needed to be admitted to hospital |
| 4) Major | Results in long-term incapacity |
| 5) Catastrophic | Death, permanent injury |
Funding
This research is funded by the Health Research Board of Ireland under grant reference number HRC-2014-1.
Ethical approval
Ethical approval was granted by the Irish College of General Practitioners (ICGP) Research Ethics Committee.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Reader TW, Gillespie A, Roberts J. Patient complaints in healthcare systems: a systematic review and coding taxonomy. BMJ Qual Saf. 2014;23(8):678–689. doi: 10.1136/bmjqs-2013-002437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verstappen W, Gaal S, Esmail A, Wensing M. Patient safety improvement programmes for primary care. Review of a Delphi procedure and pilot studies by the LINNEAUS collaboration on patient safety in primary care. Eur J Gen Pract. 2015;21(Suppl):50–55. doi: 10.3109/13814788.2015.1043725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Studdert DM, Bismark MM, Mello MM, et al. Prevalence and characteristics of physicians prone to malpractice claims. New Engl J Med. 2016;374(4):354–362. doi: 10.1056/NEJMsa1506137. [DOI] [PubMed] [Google Scholar]
- 4.Spittal MJ, Bismark MM, Studdert DM. The PRONE score: an algorithm for predicting doctors’ risks of formal patient complaints using routinely collected administrative data. BMJ Qual Saf. 2015;24(6):360–368. doi: 10.1136/bmjqs-2014-003834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bismark MM, Spittal MJ, Gurrin LC, et al. Identification of doctors at risk of recurrent complaints: a national study of healthcare complaints in Australia. BMJ Qual Saf. 2013;22(7):532–540. doi: 10.1136/bmjqs-2012-001691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Price J. Out of hours but not without risks. Medical Protection Society; 2013. Practice Matters. https://www.medicalprotection.org/ireland/practice-matters/issue-2---september-2013/out-of-hours-but-not-without-risks (accessed 29 Oct 2018) [Google Scholar]
- 7.Gaal S, Hartman C, Giesen P, et al. Complaints against family physicians submitted to disciplinary tribunals in the Netherlands: lessons for patient safety. Ann Fam Med. 2011;9(6):522–527. doi: 10.1370/afm.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Owen C. Formal complaints against general practitioners: a study of 1000 cases. Br J Gen Pract. 1991;41(344):113–115. [PMC free article] [PubMed] [Google Scholar]
- 9.Schnitzer S, Kuhlmey A, Adolph H, et al. Complaints as indicators of health care shortcomings: which groups of patients are affected? Int J Qual Health Care. 2012;24(5):476–482. doi: 10.1093/intqhc/mzs036. [DOI] [PubMed] [Google Scholar]
- 10.Gogos AJ, Clark RB, Bismark MM, et al. When informed consent goes poorly: a descriptive study of medical negligence claims and patient complaints. Med J Aust. 2011;195(6):340–344. doi: 10.5694/mja11.10379. [DOI] [PubMed] [Google Scholar]
- 11.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 12.Gillespie A, Reader T. Healthcare complaints analysis tool. 2015 doi: 10.1136/bmjqs-2015-004596. Version 3. http://qualitysafety.bmj.com/content/qhc/suppl/2016/01/05/bmjqs-2015-004596.DC1/bmjqs-2015-004596supp_new.pdf (accessed 11 Oct 2018) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gillespie A, Reader TW. The Healthcare Complaints Analysis Tool: development and reliability testing of a method for service monitoring and organisational learning. BMJ Qual Saf. 2016;25(12):937–946. doi: 10.1136/bmjqs-2015-004596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Patient Safety Agency. A risk matrix for risk managers. 2008. https://www.scribd.com/doc/307287247/Risk-Matrix-for-Risk-Managers (accessed 11 Oct 2018)
- 15.Health Service Executive. Primary Care Reimbursement Service: statistical analysis of claims and payments 2015. 2015. https://www.hse.ie/eng/staff/pcrs/pcrs-publications/pcrs-statistical-analysis-of-claims-and-payments-2015.pdf (accessed 11 Oct 2018)
- 16.Barragry RA, Varadkar LE, Hanlon DK, et al. An analytic observational study on complaints management in the general practice out-of-hours care setting: who complains, why, and what can we do about it? BMC Fam Pract. 2016;17:87. doi: 10.1186/s12875-016-0484-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smits M, Rutten M, Keizer E, et al. The development and performance of after-hours primary care in the Netherlands: a narrative review. Ann Int Med. 2017;166(10):737–742. doi: 10.7326/M16-2776. [DOI] [PubMed] [Google Scholar]
- 18.Colliers A, Bartholomeeusen S, Remmen R, et al. Improving Care And Research Electronic Data Trust Antwerp (iCAREdata): a research database of linked data on out-of-hours primary care. BMC Res Notes. 2016;9(1):259. doi: 10.1186/s13104-016-2055-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smits M, Keizer E, Giesen P, et al. Patient safety culture in out-of-hours primary care services in the Netherlands: a cross-sectional survey. Scand J Prim Health Care. 2018;36(1):28–35. doi: 10.1080/02813432.2018.1426150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.NHS Digital Data on written complaints in the NHS 2016–17. 2017. http://www.digital.nhs.uk/catalogue/PUB30080 (accessed 11 Oct 2018)
- 21.Smits M, Huibers L, Kerssemeijer B, et al. Patient safety in out-of-hours primary care: a review of patient records. BMC Health Services Res. 2010;10:335. doi: 10.1186/1472-6963-10-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Christiaans-Dingelhoff I, Smits M, Zwaan L, et al. To what extent are adverse events found in patient records reported by patients and healthcare professionals via complaints, claims and incident reports? BMC Health Services Res. 2011;11:49. doi: 10.1186/1472-6963-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shlomo V, Adi R, Eliezer K. The knowledge and expectations of parents about the role of antibiotic treatment in upper respiratory tract infection — a survey among parents attending the primary physician with their sick child. BMC Fam Pract. 2003;4:20. doi: 10.1186/1471-2296-4-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vaz LE, Kleinman KP, Lakoma MD, et al. Prevalence of parental misconceptions about antibiotic use. Pediatrics. 2015;136(2):221–231. doi: 10.1542/peds.2015-0883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ipsos MRBI. Healthy Ireland 2017: summary of findings. 2017. http://hdl.handle.net/10147/622624 (accessed 11 Oct 2018)
- 26.Tonkin-Crine SKG, Tan PS, van Hecke O, et al. Clinician-targeted interventions to influence antibiotic prescribing behaviour for acute respiratory infections in primary care: an overview of systematic reviews. Cochrane Database Syst Rev. 2017;(9):CD012252. doi: 10.1002/14651858.CD012252.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hu Y, Walley J, Chou R, et al. Interventions to reduce childhood antibiotic prescribing for upper respiratory infections: systematic review and meta-analysis. J Epidemiol Community Health. 2016;70:1162–1170. doi: 10.1136/jech-2015-206543. [DOI] [PubMed] [Google Scholar]
- 28.Wallace E, Lowry J, Smith SM, Fahey T. The epidemiology of malpractice claims in primary care: a systematic review. BMJ Open. 2013;3(6):e002929. doi: 10.1136/bmjopen-2013-002929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alam R, Cheraghi-Sohi S, Panagioti M, et al. Managing diagnostic uncertainty in primary care: a systematic critical review. BMC Fam Pract. 2017;18(1):79. doi: 10.1186/s12875-017-0650-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Care Quality Commission. Our new approach to the inspection of NHS GP out-of-hours services: findings from the first comprehensive inspections. 2014. http://www.cqc.org.uk/sites/default/files/20140924_gp_out_of_hours_final.pdf (accessed 11 Oct 2018)