Abstract
Object: Leptomeningeal Carcinomatosis (LCM) represents a state of systemic malignant disease with poor prognosis. The purpose of this study is to compare overall survival (OS) between intraventricular chemotherapy through Ommaya reservoir (OR) and chemotherapy through lumbar puncture (LP) in LCM.
Patients and Methods: Forty adult patients with LCM were included. All patients underwent lumbar puncture and Magnetic resonance imaging (MRI). Thirty patients received chemotherapy through LP and 10 undergone colocation of Ommaya reservoir for intraventricular chemotherapy.
Results: The most common symptom was headache (Present in 50%). The cranial nerves most affected were VI and VII. Leptomeningeal enhancement was the most frequent finding in MRI. The OS in the LP group was 4 months and Ommaya group was 9.2 months (p = 0.0006; CI:1.8-3), with statistical differences in favor to Intraventricular treatment. Proportional hazard regression showed that receiving chemotherapy through Ommaya reservoir was a protective factor (Hazard ratio = 0.258, Standard Error = 0.112, p = 0.002 and 95% CI 0.110-0.606). Using KPS as a factor did not affect the hazard ratio of Ommaya reservoir itself.
Conclusions: OS was significantly higher in patients with Ommaya reservoir in spite of Karnofsky Performance Status (KPS) previous to chemotherapy. Therefore, intraventricular chemotherapy should be preferred over lumbar puncture chemotherapy administration if there are resources available.
Keywords: leptomeningeal carcinomatosis, overall survival, chemotherapy, ommaya reservoir, lumbar puncture, karnofsky performance status, intraventricular
Introduction
LCM is a rare complication of advanced cancer, which consists in infiltration of the meninges and Cerebrospinal fluid (CFS) space by malignant cells (1). Any cancer can metastasize to meninges but is mainly detected in association with breast cancer, lung cancer, melanoma, and in fewer occasions with other types of cancer (Gastrointestinal, prostate, lymphoma, leukemia, unknown primary cancer) (2). It has an incidence of ~5% of the patients with cancer but because of the asymptomatic patients or late-onset symptomatology, it may increase even to 20% as biopsies studies have demonstrated (3, 4). The median survival is around 4–6 weeks when untreated but it may improve as well as neurological status because of chemotherapy regimens (2, 4, 5). Karnofsky Performance Status (KPS) is the most reliable prognostic factor in patients with diagnosis of LCM (3, 4, 6). The gold standard remains the identification of malignant cells in CSF cytological study (7). The treatment goals are to improve the neurological status and to prolong survival. Different treatments are used (Radiotherapy and Neurosurgery) but the chemotherapy is essential in the management of LCM. Traditionally the method of election was the lumbar puncture (Intrathecal), but currently there are other options such as the Ommaya reservoir (Intraventricular) that might have better outcomes for patients (8). There is not a standard route of administration and both are recommended taking into consideration that chemotherapy needs good distribution and penetration; Intraventricular chemotherapy acts directly in CSF and probably it is superior to lumbar administration but there is not a trial that confirms this hypothesis completely. The present article is a retrospective study that compares the Intraventricular vs. the lumbar administration of chemotherapy in LCM.
Patients and methods
We conducted a retrospective study collecting and analyzing data from patients diagnosed with LCM between 1980 and 2016 at National Institute of Neurology and Neurosurgery. We obtained clinical, imaging, histological, and treatment outcome data from electronic database such as gender, age, Karnofsky Performance Status (KPS), overall survival in months (OS, established with date of decease), symptomatology, primary tumor, localization of lesion by neuroimaging, treatment received, date of histological diagnosis, lumbar puncture (Glucose, proteins, cells, malignant cells), HIV status, and type of treatment (Intraventricular and Intrathecal). Diagnosis was established by presence of malignant cells in CSF and by neuroimaging findings in patients with histological diagnosis of cancer. Statistical analysis was performed using Stata/MP 14.1. In an effort to identify potential bias we stablished mean and t-test for scalar variables. Survival was established by Kaplan-Meier method taking on account impact of primary tumor and KPS. We used log-rank test to establish the statistical significance of difference in overall survival.
Chemotherapy protocol
The chemotherapy regimen administered was Methotrexate 15 mg (MTX) monotherapy, and IT triple therapy (IT-triple; 15 mg MTX, 30 mg/m2 Cytarabine and 15 mg/m2 Hydrocortisone) or Cytarabine (Ara-C) alone 30 mg/m2. The regimen was administered up to twice a week, according to the condition of the patient, until negative cytology (Induction phase), followed by once weekly for 4 weeks (Consolidation phase) and the last maintenance phase was once a month until progression, maximal doses or death.
Results
We identified 40 patients; ten patients had undergone installation of an intraventricular Ommaya reservoir (Between 2000 and 2014) and received chemotherapy for LCM while 30 patients received intrathecal chemotherapy through lumbar puncture. We obtained the following data: 26 patients were male (65%) and 14 were female (35%) with a ratio of 1.8:1. The median age was 52 years range of 18–76 (Table 1).
Table 1.
Patients characteristics.
| All patients | Ommaya | LP | p | |
|---|---|---|---|---|
| Gender | n = 40 %(n) | 10 (25) | 30 (75) | 0.251 |
| Male | 26 (65) | 5 (50) | 21(70) | |
| Female | 14 (35) | 5 (50) | 9 (30) | |
| Age in years, median (range) | 52 (18-76) | 50 (18-64) | 54.5 (20-76) | 0.168 (Xi2) 0.033 (Fisher) |
| KPS, median (range) | 70 (40-100) | 70 (50-100) | 70 (40-100) | 0.580 |
| PRIMARY TUMOR | ||||
| •Breast | 10 (25) | 3 (30) | 7 (23.33) | |
| •Lung | 7 (17.5) | 0 (0) | 7 (23.33) | |
| •Leukemia | 7(17.5) | 2 (20) | 5 (16.67) | |
| •Melanoma | 5 (12.5) | 0 (0) | 5 (16.67) | |
| •Ovary | 4 (10) | 2 (20) | 2 (6.67) | |
| •Prostate | 3 (7.5) | 1 (10) | 2 (6.67) | |
| •Lymphoma | 2 (5) | 1 (10) | 1 (3.33) | |
| •Unknown | 2 (5) | 1 (10) | 1(3.33) | |
| TREATMENT REGIMEN | ||||
| •Ara-C | 7 (17.5) | 1 (10) | 6 (20) | 0.846 |
| •Mtx | 5 (12.5) | 1(10) | 4 (13.33) | |
| •Mtx/Ara | 28 (70) | 8 (80) | 20 (66.67) | |
| Overall survival (OS in months) | 0.4 – 10 | 3-10 | 0.4-7.1 | 0.0006 |
KPS, Karnofsky Performance Status; LP, Lumbar puncture; Ara-C, Citarabine; Mtx: Methotrexate.
The KPS range was 40–100, with median of 70. Neurological examination and clinical symptoms were as follows: Headache was the most common symptom, present in 20 patients (50%). The rest of signs and cranial nerves (CN) most affected as well as KPS previous treatment are resumed in Table 2.
Table 2.
Clinical symptoms and cranial nerves affected.
| Clinical features | No. patients | Percentage |
|---|---|---|
| Headache | 20 | 50 |
| Seizures (Tonic-clonic) | 5 | 12.5 |
| Nausea or vomit | 8 | 20 |
| Cognitive disorders | 6 | 15 |
| Altered state of consciousness | 5 | 12.5 |
| Motor | 12 | 30 |
| Sensitive | 6 | 15 |
| Cerebellum | 5 | 12.5 |
| Ataxia | 5 | 12.5 |
| Diplopia | 8 | 20 |
| Dysphagia | 2 | 5 |
| Dysarthria | 3 | 7.5 |
| Radicular pain | 3 | 7.5 |
| Cranial nerve affection | 18 | 45 |
| Cranial nerves affection | No. patients | Percentage |
| None | 20 | 50 |
| IX, X | 3 | 7.5 |
| VI | 4 | 10 |
| VI, III | 3 | 7.5 |
| VI, IX, X | 2 | 5 |
| VII | 5 | 12.5 |
| VIII | 3 | 7.5 |
| KPS previous treatment | LP (%) | Ommaya (%) |
| 40 | 1 (3.3) | 0 |
| 50 | 4 (13.3) | 3 (30) |
| 60 | 7 (23.3) | 2 (20) |
| 70 | 8 (26.6) | 2 (20) |
| 80 | 2 (6.6) | 0 |
| 90 | 4 (13.3) | 2 (20) |
| 100 | 4 (13.3) | 1 (10) |
| Total | 30 (100) | 10 (100) |
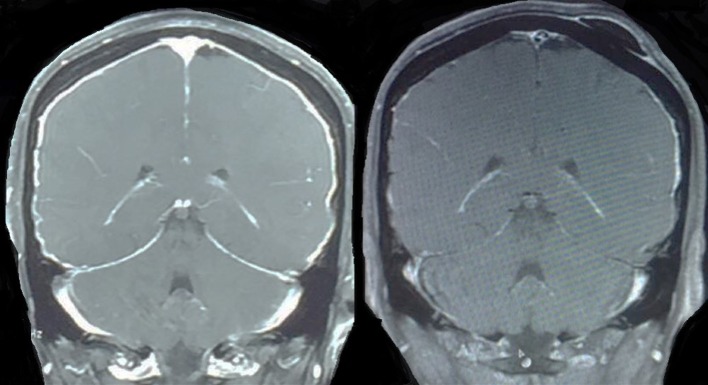
The most affected CN were VI and VII. Neuroimaging findings were: meningeal enhancement (especially in cerebellum 21/40 patients) and nodular lesions 15/40 patients (Figure 1), in the 30% of patients the Magnetic Resonance Imaging (MRI) was normal.
Figure 1.
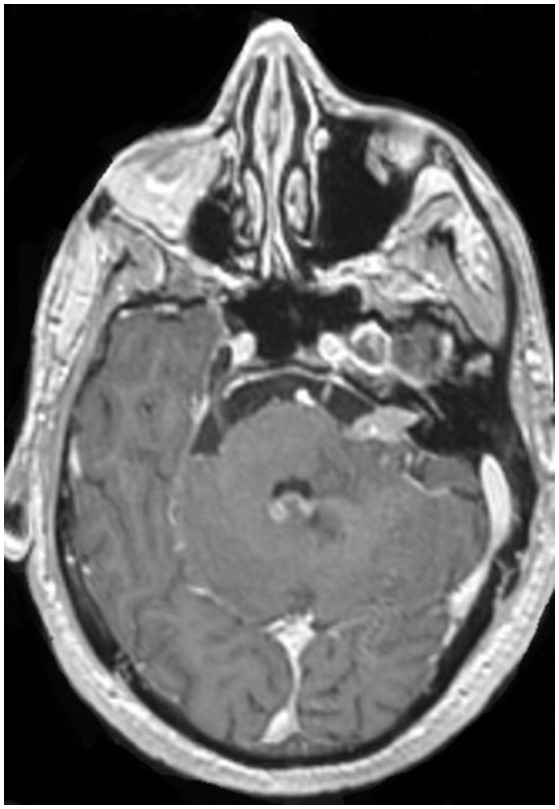
Axial MRI with nodular contrast enhancement in VII cranial nerve and enhancement in fourth ventricle, patient with diagnosis of lung cancer.
The most common site of primary tumor was breast with 10 patients (25%), followed by lung (7 patients, 17.5%) and Leukemia (7 patients, 17.5%), then melanoma with 5 patients (12.5%), ovary with 4 patients (10%), then prostate with 3 patients (7.5%) and at last but not least lymphoma and unknown with 2 patients (5%, respectively) (Figure 2).
Figure 2.
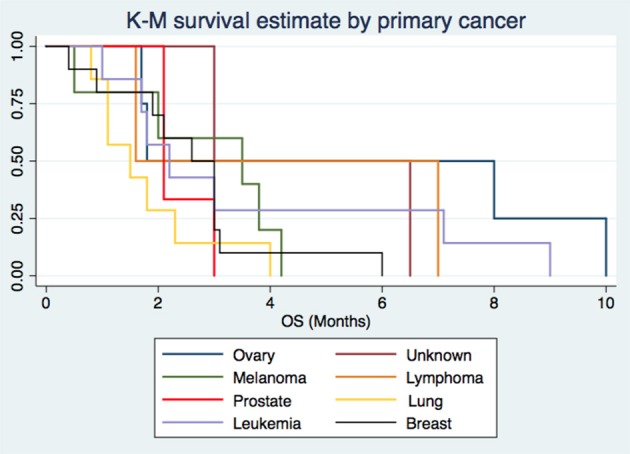
The origin of Leptomeningeal Carcinomatosis by primary cancer.
The classic pattern of LCM is Hypoglycorrhachia, hyperproteinorrhachia, and malignant cells present. We analyzed the percentage of patients that presented this classic pattern and those who present different pattern. Referent to proteins in CSF, all patients presented values >45 (Range of 53–245), mean of 101.8. Glucose outcomes were divided in: Normal (8 patients, 20%), hypoglycorrhachia (30 patients, 75%) and hyperglycorrhachia (2 patients, 5%). Cellularity was present in all patients, with a range of 5–985, mean of 55.3. Classic pattern was present in 30 patients of the sample (75%).
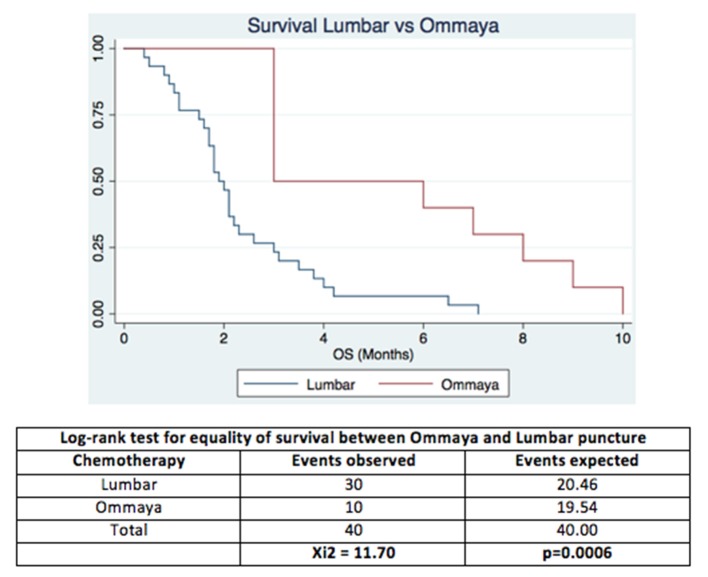
The Overall survival in the group with chemotherapy by LP was 4 months and Ommaya group was 9.2 months (p = 0.0006; CI:1.8-3), significantly higher in patients who received chemotherapy through Ommaya reservoir (see Figure 3).
Figure 3.
The Overall Survival by Lumbar chemotherapy vs. Intraventricular with Ommaya reservoir in patients with Leptomeningeal Carcinomatosis.
Cox model for proportional-hazard regression showed that receiving chemotherapy through Ommaya reservoir was a protective factor (Hazard ratio = 0.258, Standard Error = 0.112, p = 0.002 and 95% CI 0.110-0.606). Using KPS as a factor did not affect the hazard ratio of Ommaya reservoir itself.
Overall survival by primary cancer had a median of 1.5 months for lung cancer, 2.1 months for prostate, 2.2 months for leukemia, 2.8 months for breast cancer, 3 months for melanoma, 4.3 months for lymphoma, 4.7 months for unknown primary, and 4.9 months for ovary cancer. Cox regression method showed breast and lung cancer as risk factors for poor prognosis with statistical significance (p = 0.069 and p = 0.012, respectively) (see Figure 4).
Figure 4.
45 yr old female patient with diagnosis of breast cancer and leptomeningeal disease with complete radiological response after treatment with Mtx/Ara-C by Ommaya reservoir.
Regarding complications, two patients were reported with neuroinfectious disease with isolation and identification of Klebsiella pneumoniae in both cases. According to CTR (Common Toxicity Criteria) chemotherapy related complications noted were: Two patients with toxicity grade 2 in platelets count, two patients with toxicity grade 2 in WBC count, and one patient with toxicity grade 4 in platelet count.
We analyzed the prognostic factors (age, KPS, Chemotherapy and Intraventricular chemotherapy) without statistical differences (see Table 3).
Table 3.
Favorable prognostic factor in Leptomeningeal carcinomatosis by Cox regression method.
| Cox regression | ||||||
|---|---|---|---|---|---|---|
| No. subjects = 40 | No. observations = 40 | |||||
| No. failures = 40 | ||||||
| Variable | Hazard ratio | Standard error | z | p | 95% Conf. Interval | |
| KPS | 1.013 | 0.121 | 1.10 | 0.270 | 0.989 | 1.037 |
| Ommaya | 0.259 | 0.112 | −3.11 | 0.002 | 0.111 | 0.607 |
| Triple chemotherapy | 1.230 | 0.134 | 1.32 | 0.906 | 0.896 | 1.506 |
Discussion
LCM is a rare complication of advanced cancer, which consists in infiltration of the meninges and CFS space by malignant cells and with the presence of new treatments that increase survival it is likely that its frequency increases. We have reported and analyzed the outcomes obtained with chemotherapy through lumbar puncture vs. Ommaya reservoir in patients with diagnosis of LCM. There are numerous topics to underline. Some of our results were consistent with those reported on previous clinical trials.
As we mentioned before, headache was the most common symptom, present in 20 patients (50%), which is concordant with studies that described clinical features in LCM (9, 10). Cranial nerves are usually affected in patients with LCM, our patients presented mainly affection of VI and VII nerves alone or in combination with other cranial nerves (35% in total). Some reviews have noted that indeed, VI is the cranial nerve most affected (8, 11).
Previous studies showed abnormalities in CSF in more than 90% of the cases (11–13). It is necessary to have in mind that the most frequent pattern profile in lumbar puncture in patients with LCM began to be well identified since the 50's, nowadays CSF analysis has great importance in the approach of LCM (14–16). All of our patients presented abnormalities in CSF and 75% of them presented the classic pattern that we had discussed.
LCM involves the entire axis of CNS, therefore MRI takes great relevance. Contrast enhancement is necessary when obtaining a neuroaxis image. The principal site of lesion in our study was by far cerebellum, but it is clear that sites affected were variable and did not follow a pattern. However, bulky lesions are not always observable and diffuse pattern can be present as well as multiple lesions (17–19).
There are only three drugs available to administer intra-CSF: Methotrexate (MTX), Cytarabine (Ara-C) and less often Thiotepa. Effectiveness of these drugs is demonstrated in LCM, nevertheless is limited in some solid tumors associated to LCM (Melanoma and lung cancer). There was not significant difference between the three distinct types of chemotherapy employed in our study (Methotrexate, Liposomal Cytarabine and MTX/Ara-C). Until now, effectivity of these drugs remains similar (3, 20). In addition, combination vs. single agent therapy neither has shown overwhelming superiority so it remains controversial, but it can be associated to less tolerance (14, 21). OS was significantly higher in the Ommaya reservoir group. The patient with the highest OS was a young woman with low KPS, nevertheless the log-rank showed no significance to this point. Concerning to Intraventricular chemotherapy administration, there is adequate drug distribution within the leptomeningeal space. Even when CSF flow is unimpeded, the normal CSF circulation carries fluid preferentially to the ventricles (22, 23). As a result, the delivery of drug administered into the lumbar Intrathecal space is unlikely to achieve clinically relevant drug concentrations within the cerebral ventricles, where malignant cells are known to reside (24–27).This may explain the observation that there is better response in patients who receive Intraventricular chemotherapy, in contrast to Intrathecal chemotherapy.
On the other hand, a recent clinical phase II trial (28), demonstrates that disturbances in the CSF flow makes chemotherapy ineffective as it may hinder the drug distribution and increase intracranial pressure. Same authors have pointed that ventroculolumbar chemotherapy showed improvement of increased intracranial pressure, altered mental status and cauda echina symptoms. It must be noted that this trial only includes Methotrexate in evaluation, however is a reliable study about perfusion rate, adverse effects and toxicity.
About primary tumors, results were similar to the rest of literature. Confirming that breast cancer, lung cancer and melanoma are the solid tumors with major association to LCM (16).
OS was affected by primary cancer as other studies have demonstrated (3, 29, 30).
Data regarding complications related to placement of Ommaya reservoir was limited to those noted on database.
Conclusions
In our study, OS was determined by the factors previously mentioned, which is consistent with reports on similar trials. LCM represents an advanced stage of cancer and therefore it is a pathology of poor prognosis. Analysis of CSF and MRI to identify sites of lesions are fundamental to achieve diagnosis and to establish management. Recent research indicates that the future in the treatment of LCM is in the study of molecular targeted therapies such as epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK) (31).
Another diagnostic studies like rare cell capture technology should be taken into consideration to the approach of LCM on the future. As well as the detection of CSF malignant cells through CellSearch (32, 33).
Chemotherapy is the cornerstone of the treatment and Intraventricular administration through Ommaya reservoir or other dispositive, have shown similar outcomes and also have demonstrated to be the best option when available.
We should mention that our results stablish intraventricular chemotherapy as a better option of treatment in this group of patients, nevertheless, due to the retrospective design and extended time of study, result should be taken cautiously. Further studies must include bigger sample size with data about complications related to the procedures such as increased intracranial pressure and ventriculitis.
A prospective randomized study would be ideal to set conclusions but we consider it particularly difficult to select a homogeneous sample in patients with leptomeningeal disease.
Is important always having in mind that the objective of chemotherapy is to improve neurological status and quality of life more than prolonging survival. Next trials should be focused on improving diagnostic and therapeutic options that may reduce costs, avoid delayed processing, exempt patients from invasive procedures and allow a more precise diagnosis and prognosis.
Ethics statement
Ethical review process was not required due to the retrospective design of study and anonymized data of patients included, in accordance with the local legislation and institutional requirements.
Author contributions
MM and AGo: design of study, data collection, manuscript writing, analysis of results, discussion. BC, JS, VG, ML, EC, JA, SM, IR, and AGu: manuscript writing, analysis of results.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Eberth CJ. Zur Entwicklung des Epitheliomas (Cholesteatomas) dur Pia under der Lungs. Virchow's Arch. (1870) 49:51–63. 10.1007/BF02214196 [DOI] [Google Scholar]
- 2.Wasserstrom WR, Glass JP, Posner JB. Diagnosis and treatment of leptomeningeal metastases from solid tumors: experience with 90 patients. Cancer (1982) 49:759–72. [DOI] [PubMed] [Google Scholar]
- 3.Grossman SA, Krabak MJ. Leptomeningeal carcinomatosis. Cancer Treat Rev. (1999) 25:103–19. 10.1053/ctrv.1999.0119 [DOI] [PubMed] [Google Scholar]
- 4.Le Rhun E, Taillibert S, Chamberlain MC. Carcinomatous meningitis: leptomeningeal metastases in solid tumors. Surg Neurol Int. (2013) 4:S265–88. 10.4103/2152-7806.111304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leal T, Chang JE, Mehta M, Robins HI. Leptomeningeal metastasis: challenges in diagnosis and treatment. Curr Cancer Ther Rev. (2011) 7:319–27. 10.2174/157339411797642597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jaeckle KA. Neoplastic meningitis from systemic malignancies: diagnosis, prognosis and treatment. Semin Oncol. (2006) 33:312–23. 10.1053/j.seminoncol.2006.04.016 [DOI] [PubMed] [Google Scholar]
- 7.Clarke JL, Perez HR, Jacks LM, Panageas KS, Deangelis LM. Leptomeningeal metastases in the MRI era. Neurology (2010) 74:1449–54. 10.1212/WNL.0b013e3181dc1a69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gwak HS, Joo J, Kim S, Yoo H, Shin SH, Han JY, et al. Analysis of treatment outcomes of intraventricular chemotherapy in 105 patients for leptomeningeal carcinomatosis from non–small-cell lung cancer. J Thorac Oncol. (2013) 8:599–605. 10.1097/JTO.0b013e318287c943 [DOI] [PubMed] [Google Scholar]
- 9.Lara-Medina F, Crismatt A, Villareal-Garza C, Alvarado-Miranda A, Flores-Hernández L, González-Pinedo M, et al. Clinical features and prognostic factors in patients with carcinomatous meningitis secondary to breast cancer. Breast J. (2012) 18:233–41. 10.1111/j.1524-4741.2012.01228.x [DOI] [PubMed] [Google Scholar]
- 10.Palma JA, Fernandez-Torron R, Esteve-Belloch P, Fontes-Villalba A, Hernandez A, Fernandez-Hidalgo O, et al. Leptomeningeal carcinomatosis: prognostic value of clinical, cerebrospinal fluid, and neuroimaging features. Clin Neurol Neurosurg. (2013) 115:19–25. 10.1016/j.clineuro.2012.03.048 [DOI] [PubMed] [Google Scholar]
- 11.Chamberlain MC. Leptomeningeal Metastasis. Curr Opin Oncol. (2010) 22:627–35. 10.1097/CCO.0b013e32833de986 [DOI] [PubMed] [Google Scholar]
- 12.Kim YS, Resnick JS. Hypoglycorrhachia with meningeal carcinomatosis: report of two cases. Ann Intern Med. (1965) 63:115–21. 10.7326/0003-4819-63-1-115 [DOI] [PubMed] [Google Scholar]
- 13.Glantz MJ, Hall WA, Cole BF, Chozick BS, Shannon CM, Wahlberg L, et al. Diagnosis, management, and survival of patients with leptomeningeal cancer based on cerebrospinal fluid-flow status. Cancer (1995) 75:2919–31. [DOI] [PubMed] [Google Scholar]
- 14.Kim DY, Lee KW, Yun T, Park SR, Jung JY, Kim DW, et al. Comparison of intrathecal chemotherapy for leptomeningeal carcinomatosis of a solid tumor: methotrexate alone versus methotrexate in combination with cytosine arabinoside and hydrocortisone. Jpn J Clin Oncol. (2003) 33:608–12. 10.1093/jjco/hyg118 [DOI] [PubMed] [Google Scholar]
- 15.Little JR, Dale AJ, Okazaki H. Meningeal Carcinomatosis. Arch Neurol. (1974) 30:138–43. 10.1001/archneur.1974.00490320026003 [DOI] [PubMed] [Google Scholar]
- 16.Shim Y, Gwak HS, Kim S, Joo J, Shin SH, Yoo H. Retrospective analysis of cerebrospinal fluid profiles in 228 patients with leptomeningeal carcinomatosis: differences according to the sampling site, symptoms, and systemic factors. J Korean Neurosurg Soc. (2016) 59:570–6. 10.3340/jkns.2016.59.6.570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chamberlain MC. Comprehensive neuraxis imaging in leptomeningeal metastasis: a retrospective case series. CNS Oncol. (2013) 2:121–8. 10.2217/cns.12.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dietemann JL, Correia Bernardo R, Bogorin A, Abu Eid M, Koob M, Nogueria T, et al. Normal and abnormal meningeal enhancement: MRI features. J Radiol. (2005) 86:1659–83. 10.1016/S0221-0363(05)81507-0 [DOI] [PubMed] [Google Scholar]
- 19.Singh SK, Leeds NE, Ginsberg LE. MR imaging of leptomeningeal metastases: comparison of three sequences. Am J Neuroradiol. (2002) 23:817–21. [PMC free article] [PubMed] [Google Scholar]
- 20.Glantz MJ, Van Horn A, Fisher R, Chamberlain MC. Route of intracerebrospinal fluid chemotherapy administration and efficacy of therapy in neoplastic meningitis. Cancer (2010) 116:1947–52. 10.1002/cncr.24921 [DOI] [PubMed] [Google Scholar]
- 21.Hitchins RN, Bell DR, Woods RL, Levi JA. A prospective randomized trial of single-agent versus combination chemotherapy in meningeal carcinomatosis. J Clin Oncol. (1987) 5:1655–2. 10.1200/JCO.1987.5.10.1655 [DOI] [PubMed] [Google Scholar]
- 22.Chamberlain MC, Kormanik PA. Prognostic significance of 111indium-DTPA CSF flow studies in leptomeningeal metastases. Neurology (1996) 46:1674–77. 10.1212/WNL.46.6.1674 [DOI] [PubMed] [Google Scholar]
- 23.Glantz MJ, Jaeckle KA, Chamberlain MC, Phuphanich S, Recht L, Swinnen LJ, et al. A randomized controlled trial comparing intrathecal sustained-release cytarabine (DepoCyt) to intrathecal methotrexate in patients with neoplastic meningitis from solid tumors. Clin Cancer Res. (1999) 5:3394–402. [PubMed] [Google Scholar]
- 24.Bleyer WA, Drake JC, Chapner BA. Neurotoxicity and elevated cerebrospinal-fluid methotrexate concentration in meningeal leukemia. N Engl J Med. (1973) 289:770–3. 10.1056/NEJM197310112891503 [DOI] [PubMed] [Google Scholar]
- 25.Bleyer WA. Clinical pharmacology of intrathecal methotrexate: I. Pharmacokinetics in nontoxic patients after lumbar injection. Cancer Treat Rep. (1977) 61:703–8. [PubMed] [Google Scholar]
- 26.Bleyer WA. Clinical pharmacology of intrathecal methotrexate: II. An improved dosage regimen derived from age-related pharmacokinetics. Cancer Treat Rep. (1977) 61:1419–75. [PubMed] [Google Scholar]
- 27.Mason WP, Yeh SD, DeAngelis LM. 111Indium-diethylenetriamine pentaacetic acid cerebrospinal fluid flow studies predict distribution of intrathecally administered chemotherapy and outcome in patients with leptomeningeal metastases. Neurology (1998) 50:438–44. 10.1212/WNL.50.2.438 [DOI] [PubMed] [Google Scholar]
- 28.Gwak HS, Joo J, Shin SH, Yoo H, Han JY, Kim HT, et al. Ventriculolumbar perfusion chemotherapy with Methotrexate for treating Leptomeningeal carcinomatosis – A phase II study. Oncologist (2014) 19:1044–5. 10.1634/theoncologist.2014-0199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bruna J, González L, Miró J, Velasco R, Gil M, Tortosa A. Leptomeningeal carcinomatosis: prognostic implications of clinical and cerebrospinal fluid features. Cancer (2009) 115:369–81. 10.1002/cncr.24041 [DOI] [PubMed] [Google Scholar]
- 30.Taillibert S, Laigle-Donadey F, Chodkiewicz C, Sanson M, Hoang-Xuan K, Delattre JY. Leptomeningeal metastases from solid malignancy: a review. J. Neurooncol. (2005) 75:85–99. 10.1007/s11060-004-8101-x [DOI] [PubMed] [Google Scholar]
- 31.Lee DW, Lee KH, Kim JW, Keam B. Molecular targeted therapies for the treatment of leptomeningeal carcinomatosis: current evidence and future directions. Int J Mol Sci. (2016) 17(Suppl. 7):E1074. 10.3390/ijms17071074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Le Rhun E, Tu Q, De Carvalho Bittencourt M, Farre I, Mortier L, Cai H, et al. Detection and quantification of CSF malignant cells by the CellSearch technology in patients with melanoma leptomeningeal metastasis. Med Oncol. (2013) 30(Suppl. 2):538. 10.1007/s12032-013-0538-3 [DOI] [PubMed] [Google Scholar]
- 33.Nayak L, Fleisher M, Gonzalez-Espinoza R, Lin O, Panageas K, Reinr A, et al. Rare cell capture technology for the diagnosis of leptomeningeal metastasis in solid tumors. Neurology (2013) 80:1598–605. 10.1212/WNL.0b013e31828f183f [DOI] [PMC free article] [PubMed] [Google Scholar]