A 40-year-old African American female (AAF) with history of systemic lupus erythematosus on hydroxychloroquine 200 mg twice daily (BID) for 10 years reported blurry vision for several months. Visual acuity was 20/30 in each eye. Color fundus photos [Fig. 1a and 1b] depict advanced bull's eye maculopathy with marked retinal pigment epithelium and photoreceptor loss highlighted by autofluorescence imaging [Fig. 1c and d]. Spectral domain optical coherence tomography (SD-OCT) imaging [Fig. 1e and f] demonstrates atrophic maculopathy bilaterally with significant outer retinal segment loss. Although retinal toxicity from hydroxychloroquine is rare, vision loss due to maculopathy is often irreversible and can be progressive. Despite the patient's daily dose of the recommended <5 mg/kg, her use of the medication for 10 years, coupled with a cumulative dose of 1460 g, increased her risk for hydroxychloroquine-related toxicity. Recommendation for immediate cessation of the hydroxychloroquine was communicated to the patient's rheumatologist. American Academy of Ophthalmology recommends baseline and annual screening after 5 years, minimally with OCT and automated visual field testing. Maximum daily hydroxychloroquine dose of 5mg/kg should be based on real body weight rather than ideal body weight.
Figure 1.
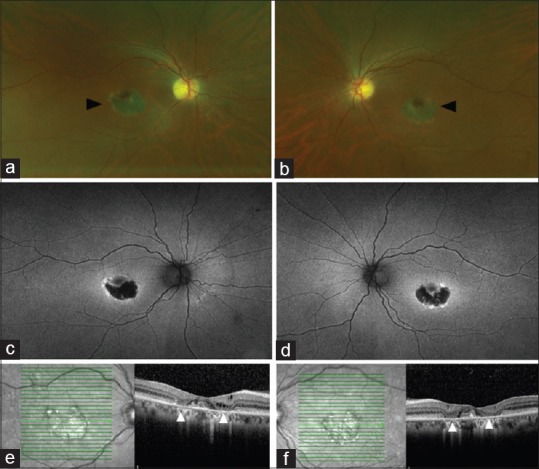
Bilateral eye findings in 40 year old woman with systemic lupus erythematosus on hydroxychloroquine for 10 years. Fundus photos (a and b) depict advanced bull's eye maculopathy in both eyes (arrow). Significantly decreased autofluorescence centrally with surrounding hyperfluorescence highlights marked retinal pigment epithelium and photoreceptor loss (c and d). Spectral domain optical coherence tomography imaging (e and f) demonstrates significant parafoveal outer retinal segment loss (arrow) and consequent “flying saucer sign” (between arrows).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.


