Abstract
Cell cycle control genes are frequently mutated in cancer cells, which usually display higher rates of proliferation than normal cells. Dysregulated mitosis leads to genomic instability, which contributes to tumor progression and aggressiveness. Many drugs that disrupt mitosis have been studied because they induce cell cycle arrest and tumor cell death. These antitumor compounds are referred to as antimitotics. Vinca alkaloids and taxanes are natural products that target microtubules and inhibit mitosis, and their derivatives are among the most commonly used drugs in cancer therapy worldwide. However, severe adverse effects such as neuropathies are frequently observed during treatment with microtubule-targeting agents. Many efforts have been directed at developing improved antimitotics with increased specificity and decreased likelihood of inducing side effects. These new drugs generally target specific components of mitotic regulation that are mainly or exclusively expressed during cell division, such as kinases, motor proteins and multiprotein complexes. Such small molecules are now in preclinical studies and clinical trials, and many are products or derivatives from natural sources. In this review, we focused on the most promising targets for the development of antimitotics and discussed the advantages and disadvantages of these targets. We also highlighted the novel natural antimitotic agents under investigation by our research group, including combretastatins, withanolides and pterocarpans, which show the potential to circumvent the main issues in antimitotic therapy.
Keywords: Antimitotic Agents, Microtubules, Spindle Apparatus, Mitosis, Cancer
INTRODUCTION
Cancer pathogenesis is a complex process in which normal cycling cells acquire basic neoplastic characteristics typically common to all tumor types. Cells from normal tissues exhibit growth entirely controlled by the cell division machinery, which is orchestrated by the production, release, recognition and inhibition of growth-promoting signals to foster tissue homeostasis. Tumor cells escape from this growth orchestration through various pathways, usually those linked to self-sufficient growth. Therefore, an essential feature of cancer cells is the ability to maintain chronically disrupted homeostatic proliferation 1. Mitosis is the fundamental proliferation process of division in human somatic cells; dysregulated mitosis leads to genomic instability characterized by DNA mutations and chromosomal aberrations. These genetic changes result in proliferative advantages for neoplastic cells and increase the susceptibility of these cells to the accumulation of additional genetic mutations, which in turn contribute to tumor progression and an exacerbated aggressive phenotype 2.
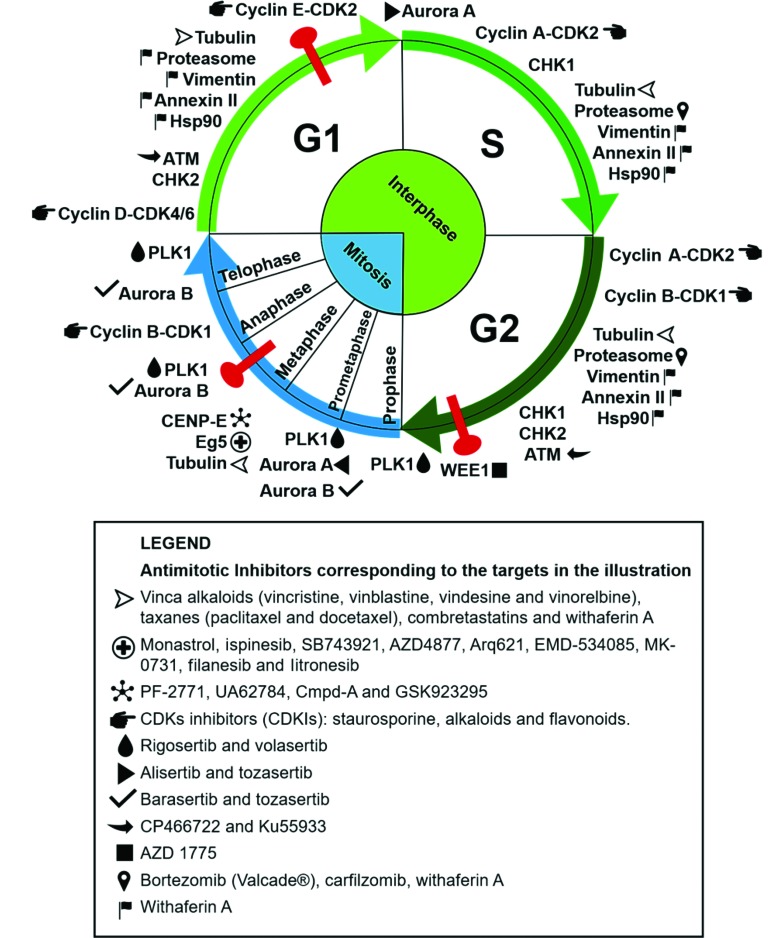
Some compounds used in cancer chemotherapy target protein components of the mitotic regulatory machinery, acting as cell division blockers and, consequently, cell death inducers 3. Many proteins involved in this process play an essential role in mitosis, making them interesting targets for the development of antimitotic anticancer drugs. The clinical success of compounds that disrupt microtubule dynamics, such as vinca alkaloids and taxanes, stimulated the development of new drugs with specific mitotic targets 4. Substantial research aimed at the development of new antimitotic compounds with different targets and increasingly selective antitumor activity has ensued. Herein, we discuss traditional and novel antimitotics with antitumor potential and the respective cellular targets of these agents, as summarized in Figure 1.
Figure 1.
Antimitotic targets and their respective inhibitors as cited in the text. The targets are placed in the illustration according to the cell cycle phase in which they perform their main functions. The corresponding inhibitors are listed in the legend. The phases of mitosis are depicted in blue, the phases of interphase are in green, and cell cycle checkpoints are in red. The compounds (+)2,3,9-trimethoxypterocarpan and withaphysalin F are not included, because their targets are unknown.
Antimitotic agents and their main targets
Mitosis is a crucial phase of the cell cycle when the chromosomes must be aligned on the metaphase plate and segregated correctly to generate two identical daughter cells. The search for new clinically effective antitumor compounds has yielded many drugs directed at targets expressed during mitosis. Such compounds, called antimitotics, target proteins involved in this complex process and are mitotic arrest agents 5.
Microtubules and microtubule-associated proteins
Microtubules are composed of α- and β-tubulin heterodimers that rapidly polymerize and depolymerize. Many microtubule-associated proteins (MAPs) fine-tune the organization of microtubules and promote or suppress microtubule dynamics 6. Microtubules play important roles in a wide range of cellular functions, such as the assembly of the mitotic spindle; the movement of organelles, vesicles and proteins; and the associated cell signaling, as well as in the development and maintenance of cellular shape 7. Chromosome segregation is first enabled by the connection between mitotic spindle microtubules and the kinetochore, a macromolecular complex positioned at the chromosomal centromere, which is assembled at the beginning of mitosis 4. Coupling between microtubules and the kinetochore is essential for correct spindle formation and subsequent chromosome alignment and segregation 6. Unsurprisingly, the first antimitotic drugs developed interfere with microtubule dynamics, through either the inhibition or stabilization of microtubule polymerization.
Tubulin-targeting antimitotics bind tubulin at different sites and may exert different effects. Vinca alkaloids (vincristine, vinblastine, vindesine, vinorelbine and vinflunine) are natural products capable of binding and destabilizing the polymeric structure of microtubules, thus causing microtubule disassembly. Colchicine also acts via this mechanism but at another interaction site. Taxanes (paclitaxel and docetaxel) and epothilones are examples of microtubule-stabilizing agents that prevent depolymerization 8. Tubulin-binding agents traditionally used in the clinic kill dividing tumor and healthy cells and affect microtubule dynamics in nonproliferating cells, resulting in various side effects, such as myelosuppression and neuropathies 9. Nevertheless, tubulin-binding agents are widely employed in the treatment of several solid tumors and oncohematological malignancies 8.
After the first tubulin-binding agents showed antitumor effects, many other tubulin-targeting antimitotic drugs were developed, along with related inhibitors directed at other targets such as kinases and mitotic protein complexes, aimed at inhibiting cell proliferation 5. Among the MAPs, the kinesin spindle protein (KSP) Eg5 is a kinesin responsible for the separation of centrosomes and for the bipolar configuration of the mitotic spindle. Inhibition of Eg5 causes monopolar spindle formation and cell cycle arrest, an effect demonstrated by monastrol, a small-molecule Eg5 inhibitor 10,11. Other Eg5 inhibitors, such as ispinesib (Cytokinetics), SB743921 (Cytokinetics), AZD4877 (AstraZeneca), Arq621 (ArQule), EMD-534085 (Merck-K GaA), MK-0731 (Merck & Co.), filanesib (Array Biopharma) and litronesib (Kyowa Hakko Kirin/Eli Lilly), have reached clinical trials 12. Centromeric protein E (CENP-E) is another MAP inhibited by antitumor agents. CENP-E is essential for the alignment of chromosomes during metaphase and passage to anaphase 3. Examples of CENP-E inhibitors are PF-2771 13, UA62784 14 and Cmpd-A 15, but only GSK923295 has reached clinical trials 16. Abnormalities in the function and expression of kinesins are important for the development and progression of many human cancers, suggesting that this class of proteins is an interesting target for new anticancer therapy strategies 17,18. Since some kinesins are expressed only during mitosis, their inhibition may reduce side effects related to antineoplastic agents targeting interphase proteins, such as traditional tubulintargeting antimitotics 9.
Cell cycle regulatory kinases
Mitosis is a strictly controlled set of events driven by many regulatory proteins that ensure cellular modifications suitable for the correct replication and distribution of genomic DNA between daughter cells. Among the proteins targeted by new antitumor agent prototypes are cell cycle regulators such as checkpoint kinases (CHKs) and cyclin-dependent kinases (CDKs), as well as regulators of the mitotic process, including Aurora kinases (AURKs) and polo-like kinases (PLKs) 19.
CDKs and CHKs control cell cycle progression. CHKs are responsible for maintaining cell genomic integrity since they are activated in response to DNA damage detected by molecular checking mechanisms in a temporally and spatially controlled manner. Activation of CHK1 and CHK2 results in cell cycle arrest, so that DNA is repaired or, if repair is not possible, apoptosis can be triggered. The defects in checkpoint signaling in many types of cancer are important drivers for the development of new drugs targeting CHKs 20. In addition, CDKs are kinases that control crucial steps in the cell cycle and are regulated by binding proteins called cyclins. Gene products that promote cell cycle progression are often mutated and constitutively active in tumor cells, increasing the interest in the development of selective inhibitors of CDKs and mitotic kinases 21. CDK inhibitors (CDKIs) include staurosporine, alkaloids and flavonoids, many of which have undergone clinical studies 22,23.
PLK1 is the most studied member of the PLK family, with important roles in some cell cycle steps, such as the activation of the CDK1-cyclin B complex, the onset of chromosomal segregation and cytokinesis 25. The expression of PLK1 is often elevated in tumors, which is correlated with a poor prognosis; thus, PLK1 is a target for anticancer therapy 26. Indeed, the development of PLK inhibitors is currently focused on PLK1 and has resulted in two promising inhibitors in clinical trials, namely, rigosertib and volasertib 27,28.
The Aurora family consists of serine-threonine kinases with a pivotal role in the control of the cell cycle and mitosis. Aurora A is located in the centrosome and acts in the progression from the G1 phase to the S phase of the cell cycle and in the initial stages of mitosis, enabling centrosome separation and mitotic spindle assembly. Aurora B is found in the mitotic spindle and controls chromosome condensation, in addition to acting at the end of mitosis to regulate cytokinesis 29. Both Auroras have an oncogenic role in human tumors 30-33. Among the effects associated with tumorigenesis, Aurora A overexpression leads to chromosomal instability characterized by aneuploidy and the premature segregation of sister chromatids 34. Inhibition of Aurora kinases is a strategy in cancer treatment, especially in combined therapeutic approaches. Most Aurora inhibitors, such as alisertib, tozasertib and barasertib, compete with ATP for binding to the catalytic site 35-37.
Nonmitotic targets affecting the cell proliferation rate
Functional interphase proteins are targets that disrupt the cell cycle and prevent mitosis via DNA repair modulation, protein turnover and checkpoint signaling. Targeting these nonmitotic proteins may hinder cell division. For example, the ataxia-telangiectasia mutated (ATM) kinase induces a cell signaling cascade in response to DNA double-strand breaks. When activated, ATM phosphorylates substrates that promote DNA repair and, consequently, cell cycle progression 38. Somatic mutations in the ATM gene are found in several cancers, especially in hematological malignancies, and are often associated with chemotherapy resistance and unfavorable prognoses 39,40. Due to the substantial influence of the ATM kinase on cell cycle progression, the development of ATM-specific inhibitors is a good strategy in the search for new anticancer therapies 41. For example, the ATM inhibitors CP466722 and Ku55933 were identified through a cell-based high-throughput screening assay 38.
WEE1 protein is a major tyrosine kinase involved in the progression of the cell cycle beyond the checkpoint between the G2 phase and mitosis (M phase), preventing entry into the mitotic cell division process in response to persistent DNA damage. High expression of this protein is often found in cancers (colorectal cancers, breast cancers, leukemias and other cancers) and correlates with tumor progression and negative prognoses, despite the cell cycle-arresting activity of WEE1 before mitosis onset 42-44. This apparent contradiction is not yet fully understood, and the current hypothesis is that WEE1 inhibition would promote the entry of cells with excessive DNA damage into mitosis, which would induce cell death during the ensuing M phase. WEE1 kinase inhibitors, e.g., AZD1775, have been studied in clinical trials, but their use is limited because of their nonselective action 45-47.
The 26S proteasome is an important multimeric complex responsible for the degradation of misfolded or overexpressed proteins 48. Neoplastic cells exhibit high dependence on the 26S proteasome because of the need to eliminate defective proteins, which are detrimental to cell cycle advancement, resulting from the genetic instability in the tumor and the high cell proliferation rate. The accumulation of ubiquitinated and misfolded proteins may induce apoptosis. Therefore, the 26S proteasome is a validated therapeutic target in oncology, with FDA-approved inhibitors such as bortezomib (Velcade®) and carfilzomib currently in clinical use 49 for the treatment of multiple myeloma, in which malignant cells have an abundance of proteasomes 49,50.
In addition to the proteins cited above, many others may be validated as targets for cancer therapy. A better understanding of mitotic mediators and their role in tumorigenesis may advance the fight against highly proliferative tumor cells.
Challenges in the search for new mitotic targets for anticancer therapy
Many efforts have been made in the search for and development of new antitumor compounds; however, cancer remains a difficult-to-treat disease 51. The available antimitotic therapies are somewhat successful but rarely eradicate tumors completely and generally promote tumor resistance and systemic toxicity 52. The selectivity of antimitotics for tumors has long been believed to be based on the high proliferation rate of cancer cells in contrast to the supposed quiescence or low division rate of most cells in normal tissues. Normal and tumor cells progress through the cell cycle in similar ways, but the higher proliferation rates of cancer cells cause mitotic targets to be more frequently expressed in tumors than in normal tissues, thus making neoplastic cells more sensitive to antimitotic action 52. However, Komlodi-Pasztor and colleagues emphasized that tumor proliferation rates may not be as high as expected, and thus the frequency of mitotic target expression may not be as different as expected between tumor and nontumor cell populations. This characteristic could be a reason for the lack of specificity of antimitotic agents such as mitosis-specific kinase inhibitors 53.
In addition to selectivity issues, antimitotic drugs acting only on M phase-exclusive targets allow interphase cancer cells to be refractory to treatment. In his review, Mitchison 54 compared data from the literature and showed that 2-5% of cells in primary tumors are in the S phase, while 40% of cells in in vitro tumor cell cultures are in the S phase. In addition, the doubling times of tumor cells in patients are very long, approximately fifty times greater than those in cell lines or animal models. Furthermore, the cell proliferation ratio varies greatly according to different cancer types, individual patient characteristics, and the primary tumor origin and location. Therefore, the number of neoplastic cells in interphase is probably high enough to make a tumor resistant to chemotherapeutics that act specifically on exclusive mitotic targets. This fact may explain the preclinical failure of many antimitotic compounds 52,55.
Antimitotics are considered mitosis blockers and, consequently, cell death inducers. The main issue in antimitotic therapy is that not all cells blocked in M phase will die, with many becoming aneuploid. This alteration is a direct consequence of chromosomal instability, that is, susceptibility to the gain and/or loss of chromosomes, which generates an unstable karyotype. This instability promotes the acquisition of malignant tumor characteristics as a proliferative advantage due to the increased mutation rate in oncogenes and tumor suppressor genes 55. The gain of malignant features by tumors hinders the prediction of patient response to therapy and facilitates the emergence of chemotherapy-resistant tumor cells. Treatment resistance is a major problem that hinders complete cure and limits the success of anticancer drug therapy. For example, the differential expression of β-tubulin isoforms has been shown to result in resistance to anti-tubulin chemotherapeutics such as paclitaxel, along with increasing tumor aggressiveness 56,57. Another emerging form of taxane resistance is the increased expression of multidrug resitance (MDR) proteins – efflux pumps that remove cancer drugs from the tumor cell cytoplasm – such as the ATP Binding Cassette Subfamily B Member 1 (ABCB1 protein), P-glycoprotein and the Multidrug resistance-associated protein 1 (MRP1) 58,59.
The side effects of antimitotics are also related to the ubiquitous function of targets such as microtubules, which act in mitosis, interphase and quiescence. Drugs that disrupt microtubule function are associated with side effects such as neurotoxicity, which may lead to irreversible neuropathies. The current generation of antimitotic therapies in clinical trials did not meet the expectations of reduced side effects, even with diminished neurotoxicity 60. In fact, new side effects were found in patients treated with antimitotics and included hematological changes such as neutropenia 61-63. Next, we review the novel classes of antimitotics under preclinical investigation by our research group, which have the potential to overcome or minimize the limitations of current anticancer antimitotics. These molecules are synthetic analogs of well-known microtubule-targeting agents (combretastatins) and natural products with multiple or unknown targets (withanolides and pterocarpans).
Combretastatins
The combretastatins are a potent class of natural products first isolated by Pettit and collaborators from the bark of the African bush willow, Combretum caffrum 64,65. These molecules are phenolic stilbenes that bind to the colchicine binding site on tubulin and lead to microtubule disruption and mitotic arrest by preventing spindle formation 66. Among the combretastatins, combretastatin A-4 (CA-4) is a lead compound that binds to the colchicine site and exerts antiproliferative activity by inhibiting tubulin polymerization. Despite its structural simplicity and potent activity, this natural product has problems related to its low solubility in natural biological systems and the lability of the cis-stilbene moiety. However, CA-4 is one of the most actively researched lead molecules in anticancer drug development programs worldwide, and extensive studies have been conducted to develop new CA-4 analogs to overcome the issues inherent to CA-4 and improve its pharmacotherapeutic profile 67.
Most of the recent structural modifications introduced in CA-4 have been based on changes in the cis olefinic bond, including the restriction of the cis configuration by a heterocyclic moiety and the replacement of this configuration by a stable linker. These modifications can maintain the original aromatic rings or can be associated with simultaneous alterations in either ring A or ring B 68. Among the new linkers explored to replace the cis olefinic bond of the CA-4 structure, N-acylhydrazone (NAH) is worth mentioning. From the synthetic and medicinal chemistry perspectives, NAH is considered a versatile subunit, and it has been described as a privileged structure 69. This review highlights some NAH derivatives that perturb microtubule/tubulin dynamics and have been synthesized by our research group using LASSBio® compounds from the Federal University of Rio de Janeiro.
Amaral et al. 70 identified a new series of CA-4 analogs designed in light of previous structure–activity relationship studies on CA-4 derivatives 71. Several compounds exhibit moderate to high antiproliferative activity in tumor cells, with IC50 values ranging between 18 and 4 nmol.L-1. Among these compounds, LASSBio-1586, patent number WO2013142935A1, has emerged as a lead antitumor candidate; LASSBio-1586 is structurally simple, able to inhibit microtubule polymerization, exhibits a broad in vitro and in vivo antiproliferative profile and has a better cytotoxic selectivity index than the natural prototype CA-4 70. In addition, the antiproliferative activity was evaluated in human lymphocytes to determine the selectivity indexes of the LASSBio derivatives, which were better than that of CA-4 72. More recently, our group described the synthesis of nine new isosteres of LASSBio-1586, aimed at improving the cytotoxicity and selectivity of LASSBio-1586 73. Among these derivatives, LASSBio-1920 was selected as the most potent, with IC50 values of 0.3, 9.0 and 5.0 nmol.L-1 in the HL-60, OVCAR-8 and HCT-8 tumor cell lines, respectively (Table 1). LASSBio-1920 also exhibited a notable cytotoxic selectivity index in comparison with that of CA-4 and LASSBio-1586 (Table 2, Figure 2), and its ability to modulate microtubule polymerization was confirmed. Docking studies indicated that LASSBio-1920 can interact with the same amino acid residues involved in the interaction of DAMA-colchicine as a cocrystal with β-tubulin.
Table 1. Cytotoxic activity (mean IC50±SEM) of LASSBio-1586 analogs and the CA-4 and LASSBio-1586 standards in tumor cell lines and peripheral blood mononuclear cells (PBMCs) after 72h of treatment (IC50 values are in µmol.L-1). SEM, standard error of the mean; IC50, the concentration of a compound needed to reduce cell growth by 50% in vitro.
| Compound | HL60 (mean IC50±SEM) | OVCAR-8 (mean IC50±SEM) | HCT-8 (mean IC50±SEM) | PBMCs (mean IC50±SEM) |
|---|---|---|---|---|
| LASSBio-1837 | 0.047±1.0×10-3 | 0.099±0.010 | 0.27±0.020 | 0.24±0.045 |
| LASSBio-1839 | 0.34±0.028 | 1.26±0.24 | 1.08±0.25 | 0.51±0.020 |
| LASSBio-1840 | 0.10±0.031 | 0.39±0.031 | 0.34±0.068 | 0.43±8.1×10-4 |
| LASSBio-1917 | 0.074±0.018 | 0.55±0.37 | 0.48±0.032 | 0.71±4.0×10-3 |
| LASSBio-1918 | 0.75±0.085 | 4.26±0.20 | 4.18±0.17 | 2.14±0.61 |
| LASSBio-1919 | 0.081±0.029 | 0.31±0.19 | 0.33±0.019 | 0.33±0.086 |
| LASSBio-1920 | 3.0×10-4±4.0×10-5 | 9.0×10-3±6.0×10-3 | 5.0×10-3±3.0×10-3 | 0.10±0.011 |
| CA-4 | 2.2×10-3±3.0×10-4 | 5.0×10-4±1.0×10-4 | 5.0×10-3±1.0×10-3 | 3.2×10-3 |
| LASSBio-1586 | 0.29±1.2×10-3 | 0.29±0.040 | 0.45±0.081 | 1.34±0.065 |
Table 2. Cytotoxic selectivity index (SI), which represents the IC50 for PBMCs/cancer cell lines after 72h of treatment. PBMCs, peripheral blood mononuclear cells; SEM, standard error of the mean; IC50, the concentration of a compound needed to reduce cell growth by 50% in vitro.
| Compound | SI PBMC/HL-60 | SI PBMC/OVCAR-8 | SI PBMC/HCT-8 |
|---|---|---|---|
| LASSBio-1920 | 333.30 | 11.11 | 20.0 |
| LASSBio-1586 | 4.60 | 4.60 | 3.0 |
| CA-4 | 1.45 | 6.40 | 0.60 |
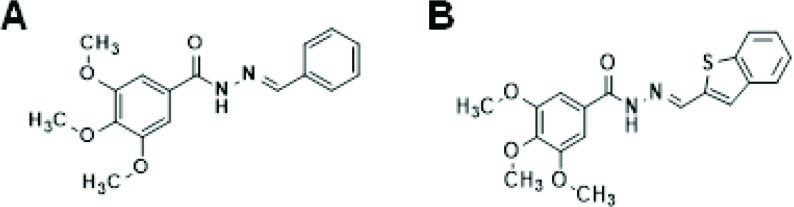
Figure 2.
Combretastatin A-4 analogs. (A) LASSBio-1586. (B) LASSBio-1920.
Our data from structure–activity relationship studies on combretastatins reveal that the presence of the methoxy (OCH3) group linked at position 5 of the aromatic subunit (ring A) is crucial for cytotoxic activity, while the OCH3 group at position 4 is not. Concerning the aromatic rings linked to the imine subunit (ring B) of the isostere, our data suggest a direct relationship between the increase in lipophilicity and the enhancement of cytotoxic activity, in agreement with previous results of Amaral et al. 70. These findings can be explained on the basis of the improved hydrophobic interaction with β-tubulin 70. The more lipophilic the group bound to ring B is, the stronger the interaction with β-tubulin. However, the addition of lipophilic/hydrophobic groups to the combretastatin core should be carefully considered, since this structural modification may impair aqueous solubility and pharmacokinetic properties.
On the basis of the articles discussed here, we observed that microtubules and their associated proteins are feasible targets in drug discovery programs, particularly for the treatment of cancer. Numerous potent CA-4 derivatives have been developed in recent years, although very few have been accepted for clinical studies. Therefore, further structure-based drug discovery and optimization steps focusing on the CA-4 molecule and its analogs should be supported and encouraged to overcome the limitations of CA-4.
Withanolides
Withanolides are lactones based on the cholesterol-derived ergostane molecule, with oxygen atoms enzymatically added to carbons of the steroidal core and its side chains, thus producing complex and unusual structures. These compounds are secondary metabolites found in plants of the family Solanaceae 74 and exhibit multiple biological activities, such as antitumor 75, cytotoxic 76, antistress 77, antifeedant 78, immunosuppressive 79 and antimicrobial 80 activities.
One of the most heavily investigated withanolides is withaferin A, which was originally isolated from the medicinal plant Withania somnifera (L.) Dunal, also called Ashwagandha or Indian ginseng. This molecule exhibits growth-inhibitory activity in many tumor cell lines through multiple mechanisms, including an antimitotic mode of action. Like taxanes and vinca alkaloids, withaferin A binds to β-tubulin, disorganizes the mitotic spindle and causes cell cycle arrest at the G2/M phase transition in breast cancer cells 81. This compound also impairs spindle assembly checkpoint function 82 and alters the expression levels of mitosis-related proteins, such as WEE1, phospho-histone H3, cyclin-dependent kinase inhibitor 1 (p21 protein), Aurora B 83 and the anaphase-promoting complex (APC) substrate securin 84. Withaferin A also targets a variety of nonmitotic proteins, such as vimentin 85, annexin II 86, heat shock protein 90 87 and the proteasome 88. Although these proteins function mainly during interphase, affecting them may prevent mitosis and inhibit cell cycle progression. The exact mechanism of action of withaferin A is not fully understood and may encompass different cell functions during different cell cycle phases.
Another group of withanolides called the withaphysalins was isolated from the plant Acnistus arborescens. Members of this group have chemical structures closely related to those of withaferin A and have also been studied by our research team 89-91. Rocha et al. showed that withaphysalin F and withaferin A may have mechanisms in common because the antiproliferative activity of withaphysalin F and its effect of arresting cells at the G2/M phase transition were also due to interference with microtubule polymerization 91.
Pterocarpans
Pterocarpans are compounds extracted from the plant families Fabaceae, Leguminosae, Papilionaceae and Bituminaria and comprise the second largest group of isoflavonoids. Pterocarpans are phytoalexins produced by plants to defend against adversities such as resource shortages, pathogens and UV radiation 92. In ethnopharmacology, these compounds are extensively used to treat different ailments. These compounds have interesting biological activities, such as snake antivenom 93, anti-HIV 94, anti-Trypanosoma spp., anti-Leishmania spp. 95, antifungal, antibiotic 96, and topoisomerase I-inhibiting activities 97. Pterocarpans have a benzofuran–benzopyran tetracyclic ring system, which contains two chiral centers derived from the flavonoid skeleton at the 6a and 11a positions 96,98.
Hundreds of different pterocarpans have been discovered through different extraction methods, and the pharmacological activity of these pterocarpans has been tested. Since the basic structure of these compounds is chiral, methods to synthesize pterocarpans have been suggested, for example, sodium borohydride reduction of 2'-hydroxy isoflavones, Heck arylation of 2H-chromenes, Claisen rearrangement of aryl allyl ethers, aldol condensation between phenylacetates and benzaldehydes, 5-endo-trig radical cyclization, alkene metathesis and many others 98. (+)2,3,9-Trimethoxypterocarpan was isolated from Platymiscium floribundum in Brazil, and the convergent syntheses of its racemic and enantiomerically pure forms was developed by Dr. M. Banwell at the Australian National University (ANU). The synthetic route was patented in 2012 [WO2013000054 (A1)]. The molecule synthesized by Professor Banwell showed the same 1H NMR spectrum as the natural product 99.
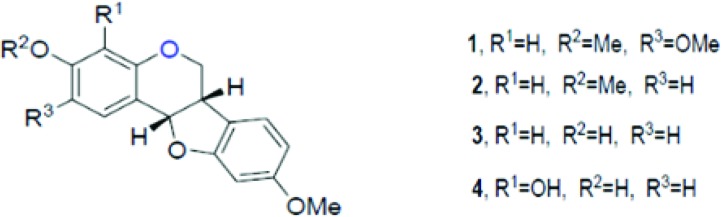
The compound (+)2,3,9-trimethoxypterocarpan has been investigated by our research group (Figure 3) as a potential anticancer compound 99. This molecule showed cytotoxicity against four leukemia cell lines (HL-60, Molt-4, Jurkat, and K562), and the proliferation of K562 cells was blocked after a 48-hour incubation period (at an IC50 of 0.8 µg.mL-1) 99,100. Flow cytometric analysis of HL-60 cells treated for 3 hours with (+)2,3,9-trimethoxypterocarpan showed the inhibition of DNA synthesis using a bromodeoxyuridine (BrdU) uptake assay. The pterocarpan inhibited BrdU incorporation by 37, 38 and 56% during the S phase at concentrations of 3.97, 7.95 and 15.9 μmol.L-1, respectively. After a 24-hour treatment with the same concentrations, propidium iodide-stained HL-60 cells showed no significant membrane damage but DNA fragmentation was seen in almost 50% of cells permeabilized with Triton X-100. Most HL-60 cells were arrested at the G2/M phase transition with tetraploid DNA content after treatment with 15.9 μmol.L-1 (+)2,3,9-trimethoxypterocarpan. In the indirect determination of mitochondrial depolarization via rhodamine 123, 38.6% of the HL-60 cell population exhibited depolarized mitochondria at the lowest treatment concentration. The results of the BrdU, membrane integrity and DNA content experiments suggested that (+)2,3,9-trimethoxypterocarpan is a cytostatic agent, while the results of the DNA fragmentation and mitochondrial depolarization experiments suggested that this pterocarpan induces apoptosis in HL-60 cells 101.
Figure 3.
Structure of pterocarpans isolated from Platymiscium floribundum by Falcão et al. 95.
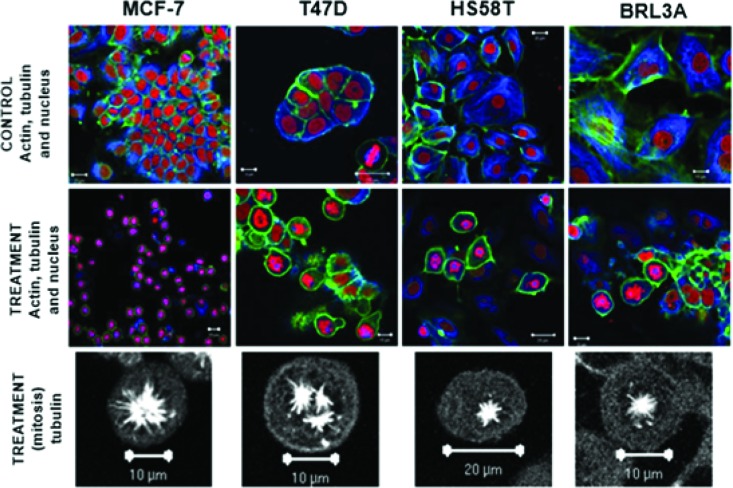
The cytostatic activity of (+)2,3,9-trimethoxypterocarpan in leukemia cells was corroborated by immunocytochemical experiments in the human breast adenocarcinoma cell lines MCF-7, T47D and HS58T. After treatment with 7.95 μmol.L-1 (+)2,3,9-trimethoxypterocarpan, the breast cancer cells remained arrested in mitosis with intact actin and microtubule networks. The same result was observed in nontumor BRL3A (murine liver) cells. However, the arrangement of microtubules was modified in most dividing cells, which exhibited monopolar mitotic spindles. Tripolar spindles were also observed, mainly in T47D cells (Figure 4). Such aberrant configurations prevented the alignment of chromosomes on the metaphase plate, blocking cell cycle progression and, consequently, cell division. Interestingly, none of the treated interphase cells exhibited microtubules with morphological alterations, suggesting that the effect of (+)2,3,9-trimethoxypterocarpan is restricted to mitosis. Lamin B labeling showed nuclear envelope disruption and confirmed cell cycle arrest at prometaphase 102. The monastral spindles observed in treated breast cancer cells resembled the phenotype induced by monastrol treatment 103,104. Monastrol impairs the acquisition of bipolarity in dividing cells without affecting centriole duplication 105, apparently due to its activity against the Eg5 kinesin 106.
Figure 4.
Formation of atypical mitotic spindles in 2,3,9-trimethoxypterocarpan-treated cells. Actin (green), tubulin (blue) and nuclei (red) are labeled in breast carcinoma and nontumor (BRL3A) cells treated or not treated with the compound. Note the normal arrangement of tubulin and actin fibers in the control cells; the formation of monopolar spindles in MCF-7, HS58T and BRL3A cells; and the formation of tripolar spindles in T47D cells. Figure from Militão et al. 97.
CONCLUSION
Antimitotic chemotherapeutics such as Taxol (paclitaxel), a microtubule-stabilizing agent that causes mitotic arrest, are currently successfully employed in cancer treatment 107. Regardless of the relative success of antimitotics, however, the death rate from cancer remains unacceptably high worldwide, and many efforts on different fronts have been made to improve cancer therapy 108. The reduction of drug resistance and side effects associated with antimitotics, such as neurotoxicity and bone marrow suppression, is a necessary improvement 60-63. In this review, we presented new antimitotic classes investigated by our research group that address the main issues of current chemotherapeutics.
The combretastatin derivatives are analogs of CA-4, an inhibitor of tubulin polymerization and microtubule formation 68. Because the functions of tubulin and microtubules are not limited to mitosis, CA-4 may affect quiescent or interphase cells, likely causing side effects in normal tissues 109. Thus, our structure–activity relationship studies identified structural characteristics of improved CA-4 analogs. We showed that the stability issues related to the cis stilbene nature of the combretastatin core were overcome by the replacement of the cis olefin double bond with an NAH framework, whose variation may result in inactive compounds. We discovered that compounds with the aromatic rings (A and B) in a trans configuration maintain tubulin-binding activity. Last, we showed a direct relationship between the increase in hydrophobicity and the cytotoxic effect of CA-4 analogs. Therefore, we described combretastatin analogs with increased cytotoxicity and selectivity toward tumor cells that can be lead molecules for new antimitotic agents inducing fewer side effects.
We also reviewed antimitotics derived from the natural products withanolides and pterocarpans. Indeed, natural sources are major sources of lead molecules and new drugs 110 such as CA-4 and Taxol. Although the mechanism of action of withanolides (withaphysalin F and withaferin A) is not fully understood, the targets of these agents may be proteins functioning in interphase, such as β-tubulin, vimentin, annexin II, heat shock protein 90 and proteasome subunits 81,85-88. Although these proteins are not mitosis-specific, their modulation may disrupt the cell cycle. Thus, withanolides may have greater-than-expected activity against targets of cancer cells in interphase 53,54, which could decrease the development of resistance to chemotherapy.
Finally, (+)2,3,9-trimethoxypterocarpan is an antimitotic agent that induces cell cycle arrest at the G2/M phase transition in leukemic cells and causes the aberrant organization of mitotic spindle microtubules in breast cancer cells. Although treatment of cells in M phase was found to result in monopolar and tripolar mitotic spindles, cells treated in interphase exhibited no microtubule modifications 102. These characteristics resemble the phenotype of cells treated with monastrol, a specific inhibitor of the kinesin motor protein Eg5, which is expressed only during mitosis 10,11. Such lines of evidence suggest that the target of (+)2,3,9-trimethoxypterocarpan is a mitosis-specific protein, and therefore, the action of this compound may be restricted to cells in mitosis. Therefore, this compound could potentially spare normal quiescent and interphase cells during clinical treatment, preventing neurotoxicity, for example.
All compounds reviewed demonstrate the potential to address important issues regarding current antimitotic-based cancer therapy. Therefore, in vivo antitumor assays will be performed to confirm these antimitotics as valuable lead molecules for the development of new anticancer drugs. However, specificity and toxicity issues concerning such molecules may arise but can be solved by combining antimitotics with other antineoplastic agents and/or monoclonal antibodies designed to bind to surface tumor antigens. This strategy can be implemented through direct covalent conjugation or drug encapsulation in nanoparticles functionalized with antibodies. Antibody-drug conjugates are a new trend in anticancer research 111; this approach also spurs the search for new and improved antimitotics.
AUTHOR CONTRIBUTIONS
Paier CR conceptualized the study and edited and supervised the manuscript writing. Maranhão SS wrote the “Introduction”, “Antimitotic agents and their main targets” and “Challenges in the search for new mitotic targets for anticancer therapy” sections. Carneiro TR and Lima LM wrote the “Combretastatins” section. Rocha DD wrote the “Withanolides” section. Santos RS and Farias KM wrote the “Pterocarpans” section. Moraes-Filho MO and Pessoa Claudia revised the manuscript.
ACKNOWLEDGMENTS
We are grateful to the Brazilian Coordination of Improvement of Higher Education Personnel (CAPES) and the Brazilian National Council for Scientific and Technological Development (CNPq) for the financial support for works cited in sections 4, 5 and 6. Dr. A. Leyva (USA) provided English language editing of the manuscript.
Footnotes
No potential conflict of interest was reported.
Commemorative Edition: 10 years of ICESP
REFERENCES
- 1.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144((5)):646–74. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 2.Malumbres M, Barbacid M. Cell cycle, CDKs and cancer: a changing paradigm. Nat Rev Cancer. 2009;9((3)):153–66. doi: 10.1038/nrc2602. [DOI] [PubMed] [Google Scholar]
- 3.Marzo I, Naval J. Antimitotic drugs in cancer chemotherapy: promises and pitfalls. Biochem Pharmacol. 2013;86((6)):703–10. doi: 10.1016/j.bcp.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 4.Sudakin V, Yen TJ. Targeting mitosis for anti-cancer therapy. BioDrugs. 2007;21((4)):225–33. doi: 10.2165/00063030-200721040-00003. [DOI] [PubMed] [Google Scholar]
- 5.Penna LS, Henriques JAP, Bonatto D. Anti-mitotic agents: are they emerging molecules for cancer treatment? Pharmacol Ther. 2017;173:67–82. doi: 10.1016/j.pharmthera.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 6.Muroyama A, Lechler T. Microtubule organization, dynamics and functions in differentiated cells. Development. 2017;144((17)):3012–21. doi: 10.1242/dev.153171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harrison MR, Holen KD, Liu G. Beyond taxanes: a review of novel agents that target mitotic tubulin and microtubules, kinases, and kinesins. Clin Adv Hematol Oncol. 2009;7((1)):54–64. [PMC free article] [PubMed] [Google Scholar]
- 8.Campos SM, Dizon DS. Antimitotic inhibitors. Hematol Oncol Clin North Am. 2012;26((3)):607–28. doi: 10.1016/j.hoc.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 9.Gascoigne KE, Taylor SS. How do anti-mitotic drugs kill cancer cells? J Cell Sci. 2009;122((Pt 15):2579–85. doi: 10.1242/jcs.039719. [DOI] [PubMed] [Google Scholar]
- 10.Mayer TU, Kapoor TM, Haggarty SJ, King RW, Schreiber SL, Mitchison TJ. Small molecule inhibitor of mitotic spindle bipolarity identified in a phenotype-based screen. Science. 1999;286((5441)):971–4. doi: 10.1126/science.286.5441.971. [DOI] [PubMed] [Google Scholar]
- 11.Jackson JR, Patrick DR, Dar MM, Huang PS. Targeted anti-mitotic therapies: can we improve on tubulin agents? Nat Rev Cancer. 2007;7((2)):107–17. doi: 10.1038/nrc2049. [DOI] [PubMed] [Google Scholar]
- 12.Myers SM, Collins I. Recent findings and future directions for interpolar mitotic kinesin inhibitors in cancer therapy. Future Med Chem. 2016;8((4)):463–89. doi: 10.4155/fmc.16.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kung PP, Martinez R, Zhu Z, Zager M, Blasina A, Rymer I, et al. Chemogenetic evaluation of the mitotic kinesin CENP-E reveals a critical role in triple-negative breast cancer. Mol Cancer Ther. 2014;13((8)):2104–15. doi: 10.1158/1535-7163.MCT-14-0083-T. [DOI] [PubMed] [Google Scholar]
- 14.Henderson MC, Shaw YJ, Wang H, Han H, Hurley LH, Flynn G, et al. UA62784, a novel inhibitor of centromere protein E kinesin-like protein. Mol Cancer Ther. 2009;8((1)):36–44. doi: 10.1158/1535-7163.MCT-08-0789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ohashi A, Ohori M, Iwai K, Nambu T, Miyamoto M, Kawamoto T, et al. A Novel Time-Dependent CENP-E Inhibitor with Potent Antitumor Activity. PLoS One. 2015;10((12)):e0144675. doi: 10.1371/journal.pone.0144675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chung V, Heath EI, Schelman WR, Johnson BM, Kirby LC, Lynch KM, et al. First-time-in-human study of GSK923295, a novel antimitotic inhibitor of centromere-associated protein E (CENP-E), in patients with refractory cancer. Cancer Chemother Pharmacol. 2012;69((3)):733–41. doi: 10.1007/s00280-011-1756-z. [DOI] [PubMed] [Google Scholar]
- 17.Hegde PS, Cogswell J, Carrick K, Jackson J, Wood KW, Eng WK, et al. Differential gene expression analysis of kinesin spindle protein in human solid tumors. Proc Am Soc Clin Oncol. 2003;22:535. [Google Scholar]
- 18.Maliga Z, Junqueira M, Toyoda Y, Ettinger A, Mora-Bermúdez F, Klemm RW, et al. A genomic toolkit to investigate kinesin and myosin motor function in cells. Nat Cell Biol. 2013;15((3)):325–34. doi: 10.1038/ncb2689. [DOI] [PubMed] [Google Scholar]
- 19.Pitts TM, Davis SL, Eckhardt SG, Bradshaw-Pierce EL. Targeting nuclear kinases in cancer: development of cell cycle kinase inhibitors. Pharmacol Ther. 2014;142((2)):258–69. doi: 10.1016/j.pharmthera.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 20.Bartek J, Lukas J. Chk1 and Chk2 kinases in checkpoint control and cancer. Cancer Cell. 2003;3((5)):421–9. doi: 10.1016/S1535-6108(03)00110-7. [DOI] [PubMed] [Google Scholar]
- 21.Ortega S, Malumbres M, Barbacid M. Cyclin D-dependent kinases, INK4 inhibitors and cancer. Biochim Biophys Acta. 2002;1602((1)):73–87. doi: 10.1016/S0304-419X(02)00037-9. [DOI] [PubMed] [Google Scholar]
- 22.Cirillo D, Pentimalli F, Giordano A. Peptides or small molecules? Different approaches to develop more effective CDK inhibitors. Curr Med Chem. 2011;18((19)):2854–66. doi: 10.2174/092986711796150496. [DOI] [PubMed] [Google Scholar]
- 23.Canavese M, Santo L, Raje N. Cyclin dependent kinases in cancer: potential for therapeutic intervention. Cancer Biol Ther. 2012;13((7)):451–7. doi: 10.4161/cbt.19589. [DOI] [PubMed] [Google Scholar]
- 24.Roshak AK, Capper EA, Imburgia C, Fornwald J, Scott G, Marshall LA. The human polo-like kinase, PLK, regulates cdc2/cyclin B through phosphorylation and activation of the cdc25C phosphatase. Cell Signal. 2000;12((6)):405–11. doi: 10.1016/S0898-6568(00)00080-2. [DOI] [PubMed] [Google Scholar]
- 25.Tut TG, Lim SH, Dissanayake IU, Descallar J, Chua W, Ng W, et al. Upregulated Polo-like Kinase 1 expression correlates with inferior survival outcomes in rectal cancer. PLoS One. 2015;10((6)):e0129313. doi: 10.1371/journal.pone.0129313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kanaji S, Saito H, Tsujitani S, Matsumoto S, Tatebe S, Kondo A, et al. Expression of polo-like kinase 1 (PLK1) protein predicts the survival of patients with gastric carcinoma. Oncology. 2006;70((2)):126–33. doi: 10.1159/000093003. [DOI] [PubMed] [Google Scholar]
- 27.Gumireddy K, Reddy MV, Cosenza SC, Boominathan R, Baker SJ, Papathi N, et al. ON01910, a non-ATP-competitive small molecule inhibitor of Plk1, is a potent anticancer agent. Cancer Cell. 2005;7((3)):275–86. doi: 10.1016/j.ccr.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 28.Rudolph D, Steegmaier M, Hoffmann M, Grauert M, Baum A, Quant J, et al. BI 6727, a Polo-like kinase inhibitor with improved pharmacokinetic profile and broad antitumor activity. Clin Cancer Res. 2009;15((9)):3094–102. doi: 10.1158/1078-0432.CCR-08-2445. [DOI] [PubMed] [Google Scholar]
- 29.Tang A, Gao K, Chu L, Zhang R, Yang J, Zheng J. Aurora kinases: novel therapy targets in cancers. Oncotarget. 2017;8((14)):23937–54. doi: 10.18632/oncotarget.14893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cirak Y, Furuncuoglu Y, Yapicier O, Aksu A, Cubukcu E. Aurora A overexpression in breast cancer patients induces taxane resistance and results in worse prognosis. J BUON. 2015;20((6)):1414–9. [PubMed] [Google Scholar]
- 31.Davidson B, Nymoen DA, Elgaaen BV, Staff AC, Tropé CG, Kærn J, et al. BUB1 mRNA is significantly co-expressed with AURKA and AURKB mRNA in advanced-stage ovarian serous carcinoma. Virchows Arch. 2014;464((6)):701–7. doi: 10.1007/s00428-014-1577-7. [DOI] [PubMed] [Google Scholar]
- 32.Jeng YM, Peng SY, Lin CY, Hsu HC. Overexpression and amplification of Aurora-A in hepatocellular carcinoma. Clin Cancer Res. 2004;10((6)):2065–71. doi: 10.1158/1078-0432.CCR-1057-03. [DOI] [PubMed] [Google Scholar]
- 33.Heredia FF, de Sousa JC, Ribeiro HL, Junior, Carvalho AF, Magalhães SM, Pinheiro RF. Proteins related to the spindle and checkpoint mitotic emphasize the different pathogenesis of hypoplastic MDS. Leuk Res. 2014;38((2)):218–24. doi: 10.1016/j.leukres.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 34.Lapenna S, Giordano A. Cell cycle kinases as therapeutic targets for cancer. Nat Rev Drug Discov. 2009;8((7)):547–66. doi: 10.1038/nrd2907. [DOI] [PubMed] [Google Scholar]
- 35.Matulonis UA, Sharma S, Ghamande S, Gordon MS, Del Prete SA, Ray-Coquard I, et al. Phase II study of MLN8237 (alisertib), an investigational Aurora A kinase inhibitor, in patients with platinum-resistant or -refractory epithelial ovarian, fallopian tube, or primary peritoneal carcinoma. Gynecol Oncol. 2012;127((1)):63–9. doi: 10.1016/j.ygyno.2012.06.040. [DOI] [PubMed] [Google Scholar]
- 36.Yang J, Ikezoe T, Nishioka C, Tasaka T, Taniguchi A, Kuwayama Y, et al. AZD1152, a novel and selective aurora B kinase inhibitor, induces growth arrest, apoptosis, and sensitization for tubulin depolymerizing agent or topoisomerase II inhibitor in human acute leukemia cells in vitro and in vivo. Blood. 2007;110((6)):2034–40. doi: 10.1182/blood-2007-02-073700. [DOI] [PubMed] [Google Scholar]
- 37.Giles FJ, Cortes J, Jones D, Bergstrom D, Kantarjian H, Freedman SJ. MK-0457, a novel kinase inhibitor, is active in patients with chronic myeloid leukemia or acute lymphocytic leukemia with the T315I BCR-ABL mutation. Blood. 2007;109((2)):500–2. doi: 10.1182/blood-2006-05-025049. [DOI] [PubMed] [Google Scholar]
- 38.Guo K, Shelat AA, Guy RK, Kastan MB. Development of a cell-based, high-throughput screening assay for ATM kinase inhibitors. J Biomol Screen. 2014;19((4)):538–46. doi: 10.1177/1087057113520325. [DOI] [PubMed] [Google Scholar]
- 39.Lin K, Adamson J, Johnson GG, Carter A, Oates M, Wade R, et al. Functional analysis of the ATM-p53-p21 pathway in the LRF CLL4 trial: blockade at the level of p21 is associated with short response duration. Clin Cancer Res. 2012;18((15)):4191–200. doi: 10.1158/1078-0432.CCR-11-2936. [DOI] [PubMed] [Google Scholar]
- 40.Forbes SA, Beare D, Gunasekaran P, Leung K, Bindal N, Boutselakis H, et al. COSMIC: exploring the world’s knowledge of somatic mutations in human cancer. Nucleic Acids Res. 2015;43((Database issue)):D805–11. doi: 10.1093/nar/gku1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Choi M, Kipps T, Kurzrock R. ATM Mutations in Cancer: therapeutic Implications. Mol Cancer Ther. 2016;15((8)):1781–91. doi: 10.1158/1535-7163.MCT-15-0945. [DOI] [PubMed] [Google Scholar]
- 42.Magnussen GI, Hellesylt E, Nesland JM, Trope CG, Flørenes VA, Holm R. High expression of wee1 is associated with malignancy in vulvar squamous cell carcinoma patients. BMC Cancer. 2013;13((1)):288. doi: 10.1186/1471-2407-13-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Porter CC, Kim J, Fosmire S, Gearheart CM, van Linden A, Baturin D, et al. Integrated genomic analyses identify WEE1 as a critical mediator of cell fate and a novel therapeutic target in acute myeloid leukemia. Leukemia. 2012;26((6)):1266–76. doi: 10.1038/leu.2011.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Slipicevic A, Holth A, Hellesylt E, Tropé CG, Davidson B, Flørenes VA. Wee1 is a novel independent prognostic marker of poor survival in post-chemotherapy ovarian carcinoma effusions. Gynecol Oncol. 2014;135((1)):118–24. doi: 10.1016/j.ygyno.2014.07.102. [DOI] [PubMed] [Google Scholar]
- 45.Wang Y, Li J, Booher RN, Kraker A, Lawrence T, Leopold WR, et al. Radiosensitization of p53 mutant cells by PD0166285, a novel G(2) checkpoint abrogator. Cancer Res. 2001;61((22)):8211–7. [PubMed] [Google Scholar]
- 46.Palmer BD, Thompson AM, Booth RJ, Dobrusin EM, Kraker AJ, Lee HH, et al. 4-Phenylpyrrolo[3,4-c]carbazole-1,3(2H,6H)-dione inhibitors of the checkpoint kinase Wee1. Structure-activity relationships for chromophore modification and phenyl ring substitution. J Med Chem. 2006;49((16)):4896–911. doi: 10.1021/jm0512591. [DOI] [PubMed] [Google Scholar]
- 47.Matheson CJ, Backos DS, Reigan P. Targeting WEE1 Kinase in Cancer. Trends Pharmacol Sci. 2016;37((10)):872–81. doi: 10.1016/j.tips.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 48.Grigoreva TA, Tribulovich VG, Garabadzhiu AV, Melino G, Barlev NA. The 26S proteasome is a multifaceted target for anti-cancer therapies. Oncotarget. 2015;6((28)):24733–49. doi: 10.18632/oncotarget.4619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moreau P. The emerging role of carfilzomib combination therapy in the management of multiple myeloma. Expert Rev Hematol. 2014;7((2)):265–90. doi: 10.1586/17474086.2014.873699. [DOI] [PubMed] [Google Scholar]
- 50.Teicher BA, Tomaszewski JE, Tomaszewski JE. Proteasome inhibitors. Biochem Pharmacol. 2015;96((1)):1–9. doi: 10.1016/j.bcp.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 51.Selvam C, Jordan BC, Prakash S, Mutisya D, Thilagavathi R. Pterocarpan scaffold: A natural lead molecule with diverse pharmacological properties. Eur J Med Chem. 2017;128:219–36. doi: 10.1016/j.ejmech.2017.01.023. [DOI] [PubMed] [Google Scholar]
- 52.Chan KS, Koh CG, Li HY. Mitosis-targeted anti-cancer therapies: where they stand. Cell Death Dis. 2012;3((10)):e411. doi: 10.1038/cddis.2012.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Komlodi-Pasztor E, Sackett DL, Fojo AT. Inhibitors targeting mitosis: tales of how great drugs against a promising target were brought down by a flawed rationale. Clin Cancer Res. 2012;18((1)):51–63. doi: 10.1158/1078-0432.CCR-11-0999. [DOI] [PubMed] [Google Scholar]
- 54.Mitchison TJ. The proliferation rate paradox in antimitotic chemotherapy. Mol Biol Cell. 2012;23((1)):1–6. doi: 10.1091/mbc.e10-04-0335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Manchado E, Guillamot M, Malumbres M. Killing cells by targeting mitosis. Cell Death Differ. 2012;19((3)):369–77. doi: 10.1038/cdd.2011.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Freedman H, Huzil JT, Luchko T, Ludueãa RF, Tuszynski JA. Identification and characterization of an intermediate taxol binding site within microtubule nanopores and a mechanism for tubulin isotype binding selectivity. J Chem Inf Model. 2009;49((2)):424–36. doi: 10.1021/ci8003336. [DOI] [PubMed] [Google Scholar]
- 57.Ferrandina G, Zannoni GF, Martinelli E, Paglia A, Gallotta V, Mozzetti S, et al. Class III β-tubulin overexpression is a marker of poor clinical outcome in advanced ovarian cancer patients. Clin Cancer Res. 2006;12((9)):2774–9. doi: 10.1158/1078-0432.CCR-05-2715. [DOI] [PubMed] [Google Scholar]
- 58.Leonard GD, Fojo T, Bates SE. The role of ABC transporters in clinical practice. Oncologist. 2003;8((5)):411–24. doi: 10.1634/theoncologist.8-5-411. [DOI] [PubMed] [Google Scholar]
- 59.Fojo AT, Menefee M. Microtubule targeting agents: basic mechanisms of multidrug resistance (MDR) Semin Oncol. 2005;32((6 Suppl 7)):S3–8. doi: 10.1053/j.seminoncol.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 60.Doménech E, Malumbres M. Mitosis-targeting therapies: a troubleshooting guide. Curr Opin Pharmacol. 2013;13((4)):519–28. doi: 10.1016/j.coph.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 61.Schöffski P, Awada A, Dumez H, Gil T, Bartholomeus S, Wolter P, et al. A phase I, dose-escalation study of the novel Polo-like kinase inhibitor volasertib (BI 6727) in patients with advanced solid tumours. Eur J Cancer. 2012;48((2)):179–86. doi: 10.1016/j.ejca.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 62.Arkenau HT, Plummer R, Molife LR, Olmos D, Yap TA, Squires M, et al. A phase I dose escalation study of AT9283, a small molecule inhibitor of aurora kinases, in patients with advanced solid malignancies. Ann Oncol. 2012;23((5)):1307–13. doi: 10.1093/annonc/mdr451. [DOI] [PubMed] [Google Scholar]
- 63.Jones R, Vuky J, Elliott T, Mead G, Arranz JA, Chester J, et al. Phase II study to assess the efficacy, safety and tolerability of the mitotic spindle kinesin inhibitor AZD4877 in patients with recurrent advanced urothelial cancer. Invest New Drugs. 2013;31((4)):1001–7. doi: 10.1007/s10637-013-9926-y. [DOI] [PubMed] [Google Scholar]
- 64.Fürst R, Zupkó I, Berényi A, Ecker GF, Rinner U. Synthesis and antitumor-evaluation of cyclopropyl-containing combretastatin analogs. Bioorg Med Chem Lett. 2009;19((24)):6948–51. doi: 10.1016/j.bmcl.2009.10.064. [DOI] [PubMed] [Google Scholar]
- 65.Shan Y, Zhang J, Liu Z, Wang M, Dong Y. Developments of combretastatin A-4 derivatives as anticancer agents. Curr Med Chem. 2011;18((4)):523–38. doi: 10.2174/092986711794480221. [DOI] [PubMed] [Google Scholar]
- 66.Seddigi ZS, Malik MS, Saraswati AP, Ahmed SA, Babalghith AO, Lamfon HA, et al. Recent advances in combretastatin based derivatives and prodrugs as antimitotic agents. MedChemComm. 2017;8((8)):1592–603. doi: 10.1039/C7MD00227K. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yang T, Wang Y, Li Z, Dai W, Yin J, Liang L, et al. Targeted delivery of a combination therapy consisting of combretastatin A4 and low-dose doxorubicin against tumor neovasculature. Nanomedicine (Lond) 2012;8((1)):81–92. doi: 10.1016/j.nano.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 68.Combes S, Barbier P, Douillard S, McLeer-Florin A, Bourgarel-Rey V, Pierson JT, et al. Synthesis and biological evaluation of 4-arylcoumarin analogues of combretastatins. Part 2. J Med Chem. 2011;54((9)):3153–62. doi: 10.1021/jm901826e. [DOI] [PubMed] [Google Scholar]
- 69.Duarte CD, Barreiro EJ, Fraga CA. Privileged structures: a useful concept for the rational design of new lead drug candidates. Mini Rev Med Chem. 2007;7((11)):1108–19. doi: 10.2174/138955707782331722. [DOI] [PubMed] [Google Scholar]
- 70.do Amaral DN, Cavalcanti BC, Bezerra DP, Ferreira PM, Castro RP, Sabino JR, et al. Docking, synthesis and antiproliferative activity of N-acylhydrazone derivatives designed as combretastatin A4 analogues. PLoS One. 2014;9((3)):e85380. doi: 10.1371/journal.pone.0085380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hu L, Li ZR, Li Y, Qu J, Ling YH, Jiang JD, et al. Synthesis and structure-activity relationships of carbazole sulfonamides as a novel class of antimitotic agents against solid tumors. J Med Chem. 2006;49((21)):6273–82. doi: 10.1021/jm060546h. [DOI] [PubMed] [Google Scholar]
- 72.Cavalcanti BC, Barros FW, Cabral IO, Ferreira JR, Magalhães HI, Júnior HV, et al. Preclinical genotoxicology of nor-β-lapachone in human cultured lymphocytes and Chinese hamster lung fibroblasts. Chem Res Toxicol. 2011;24((9)):1560–74. doi: 10.1021/tx200180y. [DOI] [PubMed] [Google Scholar]
- 73.Carneiro TR, Amaral DN, Fokoue HH, Sant’Anna CM, Porras ML, Oliveira AC. Synthesis, pharmacological evaluation and docking study of a new modulator of microtubule polymerization. Lett Drug Design Disc. 2018;15((7)):778–86. doi: 10.2174/1570180814666171012162557. [DOI] [Google Scholar]
- 74.Glotter E. Withanolides and related ergostane-type steroids. Nat Prod Rep. 1991;8((4)):415–40. doi: 10.1039/np9910800415. [DOI] [PubMed] [Google Scholar]
- 75.Zhu F, Dai C, Fu Y, Loo JF, Xia D, Gao SP, et al. Physalin A exerts anti-tumor activity in non-small cell lung cancer cell lines by suppressing JAK/STAT3 signaling. Oncotarget. 2016;7((8)):9462–76. doi: 10.18632/oncotarget.7051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rocha DD, Militão GC, Veras ML, Pessoa OD, Silveira ER, Alves AP, et al. Selective cytotoxicity of withaphysalins in myeloid leukemia cell lines versus peripheral blood mononuclear cells. Life Sci. 2006;79((18)):1692–701. doi: 10.1016/j.lfs.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 77.Kour K, Pandey A, Suri KA, Satti NK, Gupta KK, Bani S. Restoration of stress-induced altered T cell function and corresponding cytokines patterns by Withanolide A. Int Immunopharmacol. 2009;9((10)):1137–44. doi: 10.1016/j.intimp.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 78.Mareggiani G, Picollo MI, Zerba E, Burton G, Tettamanzi MC, Benedetti-Doctorovich MO, et al. Antifeedant activity of withanolides from Salpichroa origanifolia on Musca domestica. J Nat Prod. 2000;63((8)):1113–6. doi: 10.1021/np0001068. [DOI] [PubMed] [Google Scholar]
- 79.Soares MB, Brustolim D, Santos LA, Bellintani MC, Paiva FP, Ribeiro YM, et al. Physalins B, F and G, seco-steroids purified from Physalis angulata L., inhibit lymphocyte function and allogeneic transplant rejection. Int Immunopharmacol. 2006;6((3)):408–14. doi: 10.1016/j.intimp.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 80.Shanazbanu S, Shashidara S, Babu VL, Dhanapal R. Isolation of withaferin A from Withania somnifera Dun leaves and its antibacterial activity. Asian J Chem. 2006;18((2)):1243–7. [Google Scholar]
- 81.Antony ML, Lee J, Hahm ER, Kim SH, Marcus AI, Kumari V, et al. Growth arrest by the antitumor steroidal lactone withaferin A in human breast cancer cells is associated with down-regulation and covalent binding at cysteine 303 of β-tubulin. J Biol Chem. 2014;289((3)):1852–65. doi: 10.1074/jbc.M113.496844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Das T, Roy KS, Chakrabarti T, Mukhopadhyay S, Roychoudhury S. Withaferin A modulates the Spindle assembly checkpoint by degradation of Mad2-Cdc20 complex in colorectal cancer cell lines. Biochem Pharmacol. 2014;91((1)):31–9. doi: 10.1016/j.bcp.2014.06.022. [DOI] [PubMed] [Google Scholar]
- 83.Roy RV, Suman S, Das TP, Luevano JE, Damodaran C. Withaferin-A induces mitotic catastrophe and growth arrest in prostate cancer cells. J Nat Prod. 2013;76((10)):1909–15. doi: 10.1021/np400441f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Stan SD, Zeng Y, Singh SV. Ayurvedic medicine constituent withaferin a causes G2 and M phase cell cycle arrest in human breast cancer cells. Nutr Cancer. 2008;60((Suppl 1)):51–60. doi: 10.1080/01635580802381477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bargagna-Mohan P, Hamza A, Kim YE, Khuan Abby Ho Y, Mor-Vaknin N, Wendschlag N, et al. The tumor inhibitor and antiangiogenic agent withaferin A targets the intermediate filament protein vimentin. Chem Biol. 2007;14((6)):623–34. doi: 10.1016/j.chembiol.2007.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Falsey RR, Marron MT, Gunaherath GM, Shirahatti N, Mahadevan D, Gunatilaka AA, et al. Actin microfilament aggregation induced by withaferin A is mediated by annexin II. Nat Chem Biol. 2006;2((1)):33–8. doi: 10.1038/nchembio755. [DOI] [PubMed] [Google Scholar]
- 87.Yu Y, Hamza A, Zhang T, Gu M, Zou P, Newman B, et al. Withaferin A targets heat shock protein 90 in pancreatic cancer cells. Biochem Pharmacol. 2010;79((4)):542–51. doi: 10.1016/j.bcp.2009.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yang H, Shi G, Dou QP. The tumor proteasome is a primary target for the natural anticancer compound Withaferin A isolated from “Indian winter cherry”. Mol Pharmacol. 2007;71((2)):426–37. doi: 10.1124/mol.106.030015. [DOI] [PubMed] [Google Scholar]
- 89.Veras ML, Bezerra MZ, Braz-Filho R, Pessoa OD, Montenegro RC, do O Pessoa C, et al. Cytotoxic epimeric withaphysalins from leaves of Acnistus arborescens. Planta Med. 2004;70((6)):551–5. doi: 10.1055/s-2004-827156. [DOI] [PubMed] [Google Scholar]
- 90.Veras ML, Bezerra MZ, Lemos TL, Uchoa DE, Braz-Filho R, Chai HB, et al. Cytotoxic withaphysalins from the leaves of Acnistus arborescens. J Nat Prod. 2004;67((4)):710–3. doi: 10.1021/np0340347. [DOI] [PubMed] [Google Scholar]
- 91.Rocha DD, Balgi A, Maia AI, Pessoa OD, Silveira ER, Costa-Lotufo LV, et al. Cell cycle arrest through inhibition of tubulin polymerization by withaphysalin F, a bioactive compound isolated from Acnistus arborescens. Invest New Drugs. 2012;30((3)):959–66. doi: 10.1007/s10637-011-9649-x. [DOI] [PubMed] [Google Scholar]
- 92.Aoki T, Akashi T, Ayabe S. Flavonoids of leguminous plants: structure, biological activity, and biosynthesis. J Plant Res. 2000;113((4)):475–88. doi: 10.1007/PL00013958. [DOI] [Google Scholar]
- 93.Nakagawa M, Nakanishi K, Darko LL, Vick JA. Structures of cabenegrins AI and A-II, potent anti-snake venoms. Tetrahedron Lett. 1982;23((38)):3855–8. doi: 10.1016/S0040-4039(00)87726-6. [DOI] [Google Scholar]
- 94.Engler TA, Lynch KO, Reddy JP, Gregory GS. Synthetic pterocarpans with anti-HIV activity. Bioorg Med Chem Lett. 1993;3((6)):1229–32. doi: 10.1016/S0960-894X(00)80321-2. [DOI] [Google Scholar]
- 95.Salem MM, Werbovetz KA. Isoflavonoids and other compounds from Psorothamnus arborescens with antiprotozoal activities. J Nat Prod. 2006;69((1)):43–9. doi: 10.1021/np0502600. [DOI] [PubMed] [Google Scholar]
- 96.Jiménez-González L, Álvarez-Corral M, Muãoz-Dorado M, Rodríguez-García I. Pterocarpans: interesting natural products with antifungal activity and other biological properties. Phytochem Rev. 2008;7((1)):125–54. [Google Scholar]
- 97.Tesauro C, Fiorani P, D’Annessa I, Chillemi G, Turchi G, Desideri A, Erybraedin C. A natural compound from the plant Bituminaria bituminosa, inhibits both the cleavage and religation activities of human topoisomerase I. Biochem J. 2010;425((3)):531–9. doi: 10.1042/BJ20091127. [DOI] [PubMed] [Google Scholar]
- 98.Goel A, Kumar A, Raghuvanshi A. Synthesis, stereochemistry, structural classification, and chemical reactivity of natural pterocarpans. Chem Rev. 2013;113((3)):1614–40. doi: 10.1021/cr300219y. [DOI] [PubMed] [Google Scholar]
- 99.Falcão MJ, Pouliquem YB, Lima MA, Gramosa NV, Costa-Lotufo LV, Militão GC, et al. Cytotoxic flavonoids from Platymiscium floribundum. J Nat Prod. 2005;68((3)):423–6. doi: 10.1021/np049854d. [DOI] [PubMed] [Google Scholar]
- 100.Militão GC, Bezerra DP, Pessoa C, de Moraes MO, da Ponte FA, Lima MA, et al. Comparative cytotoxicity of 2, 3, 9-trimethoxypterocarpan in leukemia cell lines (HL-60, Jurkat, Molt-4, and K562) and human peripheral blood mononuclear cells. J Nat Med. 2007;61((2)):196–9. doi: 10.1007/s11418-006-0118-3. [DOI] [Google Scholar]
- 101.Militão GC, Dantas IN, Pessoa C, Falcão MJ, Silveira ER, Lima MA, et al. Induction of apoptosis by pterocarpans from Platymiscium floribundum in HL-60 human leukemia cells. Life Sci. 2006;78((20)):2409–17. doi: 10.1016/j.lfs.2005.09.044. [DOI] [PubMed] [Google Scholar]
- 102.Militão GC, Prado MP, Pessoa C, de Moraes MO, Silveira ER, Lima MA, et al. Pterocarpans induce tumor cell death through persistent mitotic arrest during prometaphase. Biochimie. 2014;104:147–55. doi: 10.1016/j.biochi.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 103.Klein E, DeBonis S, Thiede B, Skoufias DA, Kozielski F, Lebeau L. New chemical tools for investigating human mitotic kinesin Eg5. Bioorg Med Chem. 2007;15((19)):6474–88. doi: 10.1016/j.bmc.2007.06.016. [DOI] [PubMed] [Google Scholar]
- 104.Müller C, Gross D, Sarli V, Gartner M, Giannis A, Bernhardt G, et al. Inhibitors of kinesin Eg5: antiproliferative activity of monastrol analogues against human glioblastoma cells. Cancer Chemother Pharmacol. 2007;59((2)):157–64. doi: 10.1007/s00280-006-0254-1. [DOI] [PubMed] [Google Scholar]
- 105.Kapoor TM, Mayer TU, Coughlin ML, Mitchison TJ. Probing spindle assembly mechanisms with monastrol, a small molecule inhibitor of the mitotic kinesin, Eg5. J Cell Biol. 2000;150((5)):975–88. doi: 10.1083/jcb.150.5.975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gartner M, Sunder-Plassmann N, Seiler J, Utz M, Vernos I, Surrey T, et al. Development and biological evaluation of potent and specific inhibitors of mitotic Kinesin Eg5. ChemBioChem. 2005;6((7)):1173–7. doi: 10.1002/cbic.200500005. [DOI] [PubMed] [Google Scholar]
- 107.Weaver BA. How Taxol/paclitaxel kills cancer cells. Mol Biol Cell. 2014;25((18)):2677–81. doi: 10.1091/mbc.e14-04-0916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136((5)):E359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 109.Shi YW, Yuan W, Wang X, Gong J, Zhu SX, Chai LL, et al. Combretastatin A-4 efficiently inhibits angiogenesis and induces neuronal apoptosis in zebrafish. Sci Rep. 2016;6((1)):30189. doi: 10.1038/srep30189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Newman DJ, Cragg GM. Natural Products as Sources of New Drugs from 1981 to 2014. J Nat Prod. 2016;79((3)):629–61. doi: 10.1021/acs.jnatprod.5b01055. [DOI] [PubMed] [Google Scholar]
- 111.Dan N, Setua S, Kashyap VK, Khan S, Jaggi M, Yallapu MM, et al. Antibody-Drug Conjugates for Cancer Therapy: Chemistry to Clinical Implications. Pharmaceuticals (Basel) 2018;11((2)):E32. doi: 10.3390/ph11020032. pii: [DOI] [PMC free article] [PubMed] [Google Scholar]