Abstract
Background
Nosocomial amplification resulted in nearly 200 cases of Middle East respiratory syndrome (MERS) during the 2015 South Korean MERS-coronavirus outbreak. It remains unclear whether certain types of cases were more likely to cause secondary infections than others, and if so, why.
Methods
Publicly available demographic and transmission network data for all cases were collected from the Ministry of Health and Welfare. Statistical analyses were conducted to determine the relationship between demographic characteristics and the likelihood of human-to-human transmission. Findings from the statistical analyses were used to inform a hypothesis-directed literature review, through which mechanistic explanations for nosocomial amplification were developed.
Results
Cases that failed to recover from MERS were more likely to cause secondary infections than those that did. Increased probability of direct, human-to-human transmission due to clinical manifestations associated with death, as well as indirect transmission via environmental contamination (e.g., fomites and indoor ventilation systems), may serve as mechanistic explanations for nosocomial amplification of MERS-coronavirus in South Korea.
Conclusions
In addition to closely monitoring contacts of MERS cases that fail to recover during future nosocomial outbreaks, potential fomites with which they may have had contact should be sanitized. Furthermore, indoor ventilation systems that minimize recirculation of pathogen-bearing droplets should be implemented whenever possible.
Keywords: MERS (Middle East respiratory syndrome), Nosocomial infections
Background
Middle East respiratory syndrome (MERS) was first discovered in 2012 and has since caused more than 1700 cases and 700 deaths worldwide.1,2 MERS is caused by MERS-coronavirus, which can be transmitted from camels to humans and from humans to other humans.3,4 The vast majority of cases to date have been reported out of Saudi Arabia, where MERS is endemic due to frequent interactions between humans and dromedary camels.2,5 That said, the World Health Organization (WHO) estimates that about 75% of cases in Saudi Arabia are due to human-to-human transmission, although the vast majority of cases cause no secondary infections.6–9
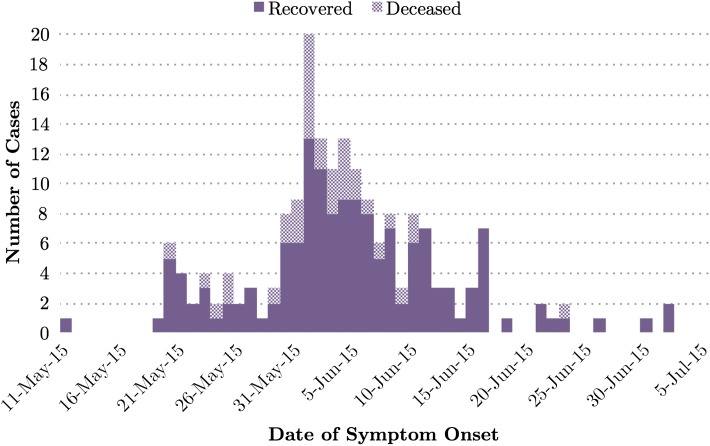
Worldwide MERS-coronavirus transmission appears to be amplified in nosocomial (healthcare) settings, resulting in greater numbers of infections than would be otherwise expected given only direct (i.e., human-to-human) household or community-wide transmission.7–11 This was exemplified during the 2015 MERS outbreak in South Korea, which was initiated by a local businessman returning home from a visit to the Middle East and resulted in nearly 200 nosocomial cases soon thereafter (Figure 1).12
Figure 1.
Epidemic curve of the 2015 South Korean MERS outbreak.
Throughout the entirety of the outbreak, the South Korean government provided a wealth of publicly available information on case demographics, including case contact details crucial for reconstructing networks of infectivity. However, it remains unclear whether or not certain types of cases were more likely to cause direct (i.e., human-to-human) secondary transmissions than others, and if so, why.
Here, we explore the following two questions:
Can a network of infectivity for the 2015 South Korean MERS outbreak be reconstructed, and if so, can we deduce which demographic characteristics were associated with direct disease transmission within the nosocomial setting?
Can knowledge gleaned from the network of infectivity and analyses of demographic characteristics lend insight into potential mechanisms for nosocomial amplification of MERS-coronavirus around the world?
Methods
Analysis 1
Publicly available case data were manually curated from text-based MERS reports via the South Korean Ministry of Health and Welfare (MOHW).13 Whenever possible, the MOHW-derived data set was cross-checked against relevant WHO Disease Outbreak News reports (DONs); in such instances, matching between data sources was conducted using age, sex and date of reporting.14 It is worth acknowledging that the use of publicly available data poses unique challenges; although such data enable timely execution of preliminary epidemiological research for novel and emerging pathogens such as MERS-coronavirus, case information is restricted to protect patient privacy. Because of this, follow-up analyses should be conducted pending availability of additional case data from the South Korean Ministry of Health and Welfare.
The following variables were available for 100% of the 186 South Korean MERS cases:
Case class (categorical: healthcare worker, patient, visitor).
Gender (binary).
Age (continuous, normally distributed, mean=55 years old).
Comorbidity status (e.g., pre-existing non-communicable disease; binary).
Case outcome (binary).
Case contact details necessary for deducing direct (i.e., human-to-human) cause of infection (i.e., identification number of causative infectious case) were available for 77% (n=144) of cases. Direct transmission of MERS-coronavirus was presumed if a given case—during his or her infectivity period—had close contact with an individual who went on to be diagnosed with MERS within 2 weeks after exposure. Close contact was defined as being within 6 feet of or in the same room (or care area) as a confirmed case for a prolonged period of time without wearing recommended personal protective equipment.15
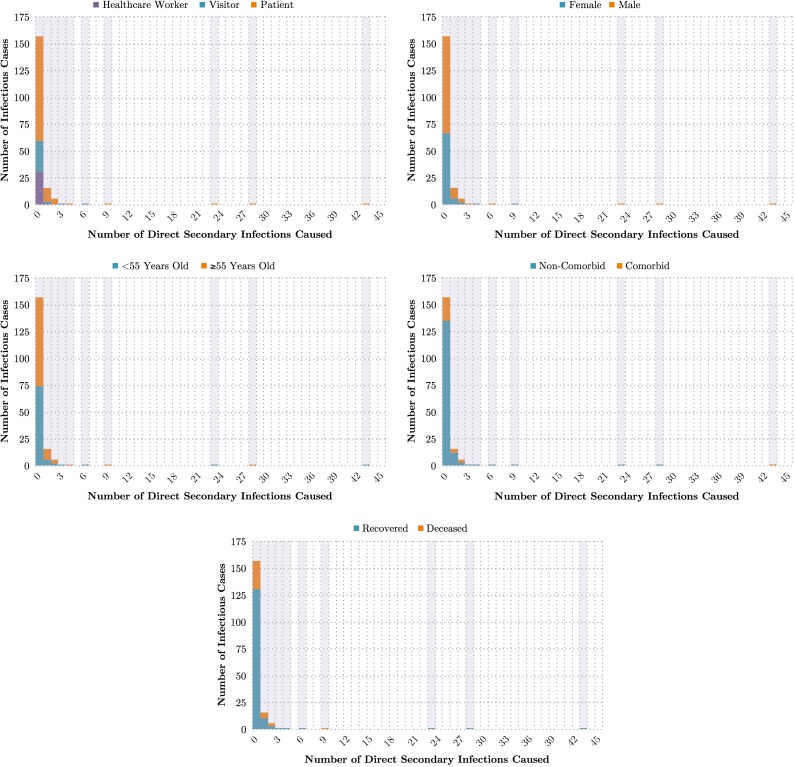
Thus, case contact details from 144 cases were used to approximate the number of direct secondary transmissions caused by each of the 186 cases (i.e., identification numbers) in the data set. These counts were then used to generate distributions of direct secondary transmissions caused per infectious case, organized by case class (healthcare worker, visitor or patient), gender (female or male), age (<55 years old or ≥55 years old), comorbidity status (non-comorbid or comorbid), and case outcome (recovered or deceased) (Figure 2).
Figure 2.
Distributions of direct secondary infections caused, by characteristic.
Given that univariate statistics do not consider potential confounders, multivariate logistic regression was also conducted against all 186 cases to further refine our understanding of the relationship between independent demographic characteristics and the likelihood of human-to-human transmission (Tables 1 and 2). Each of the 186 cases in the data set was categorized as either a ‘human-to-human transmission agent’ (n=29) or not (n=157). Human-to-human transmission agents were defined as cases that caused one or more direct secondary MERS-coronavirus infections. Binary dummy variables were created for case class, and the ‘healthcare worker’ class was treated as the reference category. Age was retained as a continuous variable and all other demographic characteristics (e.g., gender, comorbidity status, and case outcome) were retained as binary variables.
Table 1.
Characteristics associated with human-to-human transmission, univariate statistics
| Variable | Average number of direct secondary infections caused | % Human-to-human transmission agents | χ2 | p-value |
|---|---|---|---|---|
| Case class | 5.64 | 0.06 | ||
| Healthcare worker | 0.03 | 3% | ||
| Visitor | 0.32 | 12% | ||
| Patient | 1.09 | 20% | ||
| Gender | 0.67 | 0.41 | ||
| Female | 0.3 | 13% | ||
| Male | 1.11 | 17% | ||
| Age | 0.33 | 0.57 | ||
| <55 years old | 0.99 | 14% | ||
| ≥55 years old | 0.59 | 17% | ||
| Comorbidity status | 3.33 | 0.07 | ||
| Non-comorbid | 0.58 | 13% | ||
| Comorbid | 1.77 | 27% | ||
| Case outcome | 5.04 | 0.02 | ||
| Recovered | 0.82 | 13% | ||
| Deceased | 0.58 | 28% |
Table 2.
Characteristics associated with human-to-human transmission, multivariate statistics
| Variable | Adjusted odds ratio | 95% CI | p-value |
|---|---|---|---|
| Case class | |||
| Healthcare worker | Reference | ||
| Visitor | 4.71 | 0.47–46.80 | 0.19 |
| Patient | 8.35 | 0.95–73.01 | 0.06 |
| Gender | |||
| Female | Reference | ||
| Male | 1.08 | 0.45–2.58 | 0.87 |
| Age (continuous) | 0.98 | 0.94–1.01 | 0.13 |
| Comorbidity status | |||
| Non-comorbid | Reference | ||
| Comorbid | 1.42 | 0.50–4.04 | 0.51 |
| Case outcome | |||
| Recovered | Reference | ||
| Deceased | 2.96 | 1.03–8.48 | 0.04 |
Analysis 2
Results from Analysis 1 were used to inform a hypothesis-directed literature review, through which mechanistic explanations for the data-driven findings were developed. Search terms for the hypothesis-directed literature review can be found in Appendix I. The literature review was expanded beyond MERS-coronavirus to include the related, but less novel SARS-coronavirus.
Results
Analysis 1
On average, cases caused 0.77 direct secondary transmissions of MERS-coronavirus throughout the course of the outbreak. However, significant heterogeneity existed across various demographic characteristics (Table 1). The percentage of deceased cases that were human-to-human transmission agents (i.e., MERS cases that caused one or more direct secondary infections) was significantly greater than that of recovered cases (χ2=5.04, p=0.02) (Table 1). Univariate statistics for all other demographic characteristics were insignificant (p≥0.05) (Table 1). After controlling for all demographic characteristics, case outcome remained a statistically significant (p<0.05) predictor (Table 2). When compared with those who recovered, odds of being a human-to-human transmission agent were nearly three times higher for those who died from MERS (adjusted odds ratio: 2.96; 95% confidence interval [95% CI]: 1.03, 8.48) (Table 2).
All distributions generated from the South Korean MERS outbreak data were long-tailed; the vast majority (84%) (n=157) of infectious cases caused 0 direct secondary transmissions (Figure 2). Of all 186 cases, 23% (n=42) had unknown causes of infection.
Analysis 2
To develop mechanistic explanations for the findings from Analysis 1—namely, that case outcome was a statistically significant predictor for human-to-human transmission of MERS-coronavirus and that causative agents for 42 cases were unknown—a two-pronged, hypothesis-directed literature review was utilized.
Literature review I: clinical manifestations
A review of the relevant literature revealed that clinical manifestations—namely, deposition location of virus particles and viral load—might impact transmissibility of a variety of respiratory pathogens.16–19 Lower respiratory tract (LRT) infections often necessitate smaller particle size; thus, upon expulsion, the virus particles can stay suspended in the air for longer, where they may be redirected and dispersed by airflow.18–20 Similarly, high viral loads of respiratory pathogens has been shown to correlate with high rates of viral shedding into the surrounding environment.16,17,21 Variance in viral load has been noted among MERS cases, and both lower and upper respiratory tract MERS-coronavirus infections have been observed.22–26 Thus, to mechanistically explain the relationship between case outcome and human-to-human transmission, the following hypothesis was further explored using the search terms specified in Appendix I: ‘LRT infections and/or higher viral load are more common in individuals who suffer from severe disease and/or fail to recover from MERS (or SARS).’ Of the 12 635 total articles recommended by Google Scholar, 632 abstracts were considered. A total of 12 articles were relevant to the aforementioned hypothesis (Table 3). All 12 articles found either LRT infections or higher viral load to be more common among severe and fatal MERS and SARS cases (Table 3). None of the articles reviewed nullified the aforementioned hypothesis.
Table 3.
Clinical manifestations, summary of relevant articles
| Citation number | Causative agent | Number of cases studied | Relevant finding |
|---|---|---|---|
| 42 | SARS-coronavirus | 218 | Increased viral shedding in cases with severe disease |
| 43 | SARS-coronavirus | 323 | Higher viral load in cases that failed to recover |
| 44 | SARS-coronavirus | 415 | Increased viral shedding in cases with severe disease |
| 45 | SARS-coronavirus | 133 | Higher viral load in cases that failed to recover |
| 46 | SARS-coronavirus | 154 | Higher viral load in cases that failed to recover |
| 47 | SARS-coronavirus | 79 | Higher viral load among cases that failed to recover |
| 48 | MERS-coronavirus | 2 | Higher viral load in LRT in case that failed to recover |
| 49 | MERS-coronavirus | 26 | Increased viral shedding in cases with severe disease |
| 50 | MERS-coronavirus | 2 | Higher viral load in case that failed to recover |
| 51 | MERS-coronavirus | 37 | Higher viral load in LRT in cases that failed to recover |
| 52 | MERS-coronavirus | 102 | Higher viral load in cases that failed to recover |
| 53 | MERS-coronavirus | 14 | Higher viral load in LRT in cases that failed to recover |
Literature review II: indirect transmission via environmental contamination
Given that 23% of cases in the reconstructed infectivity network could not be directly attributed to a causative agent, it is possible that—in addition to human-to-human transmission of MERS-coronavirus—environmental contamination may have also played a role in nosocomial amplification during the 2015 South Korean MERS outbreak via indirect transmission. A review of the relevant literature revealed that pathogen density and indoor confinement of patients might result in contamination of surfaces, fomites and indoor ventilation systems by viral infections.27–30 Moreover, recent studies have shown—via imaging, fluid dynamics analysis and mathematical modeling—how respiratory emissions from patients can lead to both surface and long-term air contamination. In particular, this newer research—which focuses on examining the fundamental mechanics of disease transmission—demonstrates that respiratory droplet deposition and suspension in indoor spaces is dependent on coupling between host physiology and indoor environmental conditions.19,20,31 Therefore, to mechanistically explain the potential role of environmental contamination in nosocomial amplification of MERS-coronavirus transmission, the following hypothesis was further explored using the search terms specified in Appendix I: ‘Indirect transmission of MERS-coronavirus (or SARS-coronavirus) via fomites and/or indoor ventilation systems has been posited or deemed probable in nosocomial settings.’ Of the 4098 total articles recommended by Google Scholar, 489 abstracts were considered. In all, 14 articles were relevant to the aforementioned hypothesis (Table 4). All 14 articles posited or demonstrated either fomite or indoor ventilation system transmission of MERS- or SARS-coronavirus in nosocomial settings (Table 4). None of the articles reviewed nullified the aforementioned hypothesis.
Table 4.
Indirect transmission via environmental contamination, summary of relevant articles
| Article number | Causative agent | Environmental contamination studied | Relevant finding |
|---|---|---|---|
| 54 | SARS-coronavirus | Indoor ventilation system | Probable transmission |
| 55 | SARS-coronavirus | Fomite | Posited transmission |
| 56 | SARS-coronavirus | Fomite | Posited transmission |
| 57 | SARS-coronavirus | Both | Probable transmission |
| 58 | SARS-coronavirus | Both | Posited transmission |
| 59 | SARS-coronavirus | Indoor ventilation system | Probable transmission |
| 60 | SARS-coronavirus | Indoor ventilation system | Probable transmission |
| 61 | SARS-coronavirus | Indoor ventilation system | Probable transmission |
| 62 | MERS-coronavirus | Fomite | Posited transmission |
| 63 | MERS-coronavirus | Fomite | Posited transmission |
| 64 | MERS-coronavirus | Fomite | Probable transmission |
| 65 | MERS-coronavirus | Indoor ventilation system | Posited transmission |
| 66 | MERS-coronavirus | Fomite | Probable transmission |
| 67 | MERS-coronavirus | Fomite | Posited transmission |
Discussion
In this paper, a combination of data- and review-driven approaches was utilized to propose potential mechanisms for nosocomial amplification of MERS-coronavirus during the 2015 South Korean MERS outbreak.
For the data-driven components of this paper (Analysis 1), a potential network of infectivity was reconstructed using available case contact details from the 2015 South Korean MERS outbreak. Of infectious cases, 84% caused 0 direct secondary infections, resulting in a long-tailed distribution that is consistent with previous work regarding transmission heterogeneity of respiratory pathogens.32,33 The direct cause of infection (i.e., the identification number of each causative infectious case) was deducible for 77% of each cases, from which distributions of direct secondary infections caused per case (i.e., identification number) were approximated. The remaining 23% of cases were likely caused by undocumented contact between cases (i.e., direct transmission) or indirect transmission of MERS-coronavirus via environmental contamination.
Assuming that some of these cases were, in fact, due to undocumented direct transmission, results from both the univariate and multivariate statistical analyses were likely biased towards the null (Tables 1 and 2). However, this also suggests that the statistically significant dependent variable that did emerge (i.e., case outcome) is a robust predictor for human-to-human transmission—and thus, nosocomial amplification—within the context of the 2015 South Korean MERS outbreak.
Review of the relevant literature indicates that the mechanistic relationship between case outcome and human-to-human transmission of MERS-coronavirus may be due to the fact that LRT infections and higher viral load appear to be more common among severe and fatal coronavirus infections (Table 3). Furthermore, just as LRT infections and higher viral load among fatal cases may increase the probability of direct secondary infections, such clinical manifestations may also increase the probability of indirect transmission. Thus, under the assumption that the statistical results from Analysis 1 are applicable to other nosocomial outbreaks of MERS-coronavirus, contact tracing should be prioritized for cases that fail to recover (post-mortem), as well as for cases that have a high risk of mortality, such as the comorbid and the elderly.34,35
While human-to-human transmission contributed substantially to nosocomial amplification during the 2015 South Korean MERS outbreak, it is possible that environmental contamination—as noted above—played a role as well. The relevant literature suggests that fomite and indoor ventilation system transmission may be the mechanism through which environmental contamination potentially amplifies disease transmission in hospital settings (Table 4). Although fomite transmission of viral pathogens is notoriously challenging to eliminate (e.g., via sanitization), simulation studies involving computational fluid dynamics suggest that low-cost solutions for the mitigation of indoor ventilation system transmission may exist.36,37 Unfortunately, such simulations remain limited in terms of use for recommendations due to lack of calibration and excessive utilization of free parameters, as well as notable absences of physical modeling for critical small-scale processes, such as mixing and pathogen re-suspension among others. However, recent validation studies—which have directly measured the role of violent respiratory events (e.g., sneezing and coughing) on indoor environmental contamination—show a new path ahead where pathogen loads, transport and mixing from a range of patient types can be addressed.19,20,31 Moving forward, such studies will likely be integral to the development and effective deployment of more robust solutions for low cost redesign of indoor ventilation systems and patient-specific pathogen containment strategies, which should be implemented and evaluated in hospitals that are likely to treat MERS cases in the future.
Translatability of these findings to Saudi Arabia, where MERS-coronavirus is endemic and causes frequent nosocomial outbreaks, requires deeper consideration given the additional complexity posed by the prevalence of zoonotic transmissions from dromedary camels to humans, as well as the occurrence of household and community spread. It is possible that the characteristics associated with human-to-human transmission in hospital settings, though the former is much more common.7–11 As a result, the role of zoonotic cases and human-to-human transmission in nosocomial settings must be further explored. A rich data set recently obtained from the Saudi Arabian Ministry of Health—which includes information on demographic characteristics (e.g., case outcome, zoonotic and human contacts) and clinical manifestations (e.g., presence or absence of LRT infection, viral load) of cases that have sought care at government hospitals during nosocomial MERS outbreaks—may allow us to investigate the possible relationship between camel-acquired cases and direct secondary transmissions caused by said cases in the near future.
Although they are most certainly interconnected, direct transmission (i.e., human-to-human) and indirect transmission (i.e., via environmental contamination) of MERS-coronavirus were treated as decidedly distinct in this paper. Prior mathematical modeling studies in other disease contexts have shown that competition between the timescales of these two transmission routes is key to determining the dominant observed effect on and nature of the epidemic curve.38,39 Unfortunately, the number of indirect secondary transmissions caused per case was not discernible from the available data and could probably have only been determined via molecular epidemiology methods (e.g., viral phylogenetic analysis). If possible, such methods should be employed during future investigations of nosocomial MERS outbreaks in Saudi Arabia (and elsewhere, as applicable) to lend insight into the real-world interactions between direct and indirect transmission.
At present, it seems reasonable to posit that individuals who are more likely to cause direct secondary transmissions (i.e., human-to-human transmission agents) may also be more likely to cause indirect secondary transmissions (i.e., via environmental contamination) within nosocomial settings. However, high rates of human-to-human contact in healthcare settings suggest that direct transmissions are considerably more likely than indirect transmissions, which is further supported by the fact that direct causes of human-to-human infection were deducible for 77% of cases in our data set. Nevertheless, if human-to-human transmission agents are, indeed, more likely to experience LRT infections and higher viral loads in such settings, elongated mid-air suspension of virus particles and increased rates of viral shedding, may result in considerable environmental contamination of indoor ventilation systems and fomites.
Ideally, thorough sanitization of all fomites and ventilation system components should be implemented to mitigate environmental contamination. However, doing so may be cost-prohibitive in low-resource healthcare settings. With this in mind, our study suggests that—in addition to closely monitoring contacts of likely human-to-human transmission agents (i.e., MERS cases that fail to recover and cases at high risk of death) during future nosocomial outbreaks of MERS—potential fomites with which patients may have had contact should be sanitized preferentially. Furthermore, if solutions for the mitigation of indoor ventilation system transmission cannot be implemented hospital-wide, wards intended for biosecurity level 2 respiratory pathogens (i.e., MERS-coronavirus) should be given precedence.
Our study—and recommendations therein—are not without limitations, however. Due to our use of publicly available data, the dimensions of our data-driven analysis (Analysis 1) were determined by what the South Korean Ministry of Health and Welfare shared. As a result, direct causes of MERS-coronavirus infection (i.e., identification number of causative infectious case) were not deducible for 23% of cases, and additional variables that may have been of interest—such as length of hospital stay and viral phylogenetic data—were either incomplete or unavailable for analysis. Furthermore, because MERS-coronavirus and MERS remain scarce in the existing literature, the review-driven components of our study (Analysis 2) were broadened to include SARS-coronavirus and SARS, which—although virologically and clinically similar—are not without their differences.40,41 Thus, the mechanistic explanations proposed in Analysis 2 are tentative at best.
The proposed mechanisms—including clinical manifestations and indirect transmission via environmental contamination—by which case outcome acts as a predictor for human-to-human transmission and environmental contamination must be studied more extensively in order to establish causality. In particular, indirect transmission (i.e., via fomites and/or indoor ventilation systems) must be demonstrably correlated with both environmental contamination and nosocomial amplification. Similarly, clinical manifestations (i.e., LRT infection and/or high viral load) must be demonstrably correlated with both case outcome and direct or indirect transmission in future nosocomial outbreaks of MERS-coronavirus.
It is also worth considering that case outcome may be partially confounded with length of hospital stay. Cases that failed to recover from MERS may have spent longer periods of time within the hospital setting, giving them greater opportunity to cause both direct and indirect transmission—perhaps via the mechanisms proposed above. When length of hospital stay was included in our multivariate logistic regression model and run against cases for which these data were available (n=166), case outcome remained the strongest predictor for human-to-human transmission of MERS-coronavirus, followed by length of hospital stay (Appendix II). Notably, the inclusion of length of hospital stay in the model moderately dampens the statistical significance of case outcome as a predictor, indicating that a confounding relationship between the two variables may indeed exist. That said, given the considerable gaps in the length of hospital stay data (>10%), results from this secondary analysis should be treated as preliminary and will be further extended as additional data become available.
In addition to length of hospital stay, other potentially confounding variables exist as well. For example, MERS cases that failed to recover may have received more visitors on average due to the severity of their illness or been more likely to undergo aerosolizing procedures (e.g., bronchoscopy) in advanced stages of illness than those who recovered. Forthcoming work will explore these factors—namely, length of stay, visitor volume and virus dissemination (including aerosolizing procedures)—and their impact on nosocomial amplification of MERS-coronavirus in the future.
Acknowledgments
Authors’ contributions: MSM, JSB, SNF, RCL and LB conceived the design of this study. MSM and LB implemented the study. MSM, JSB, SNF, RCL and LB analyzed and interpreted the data. MSM, JSB, SNF, RCL and LB contributed to writing and revising the manuscript. MSM, JSB, SNF, RCL and LB read and approved the final version of this manuscript. MSM and LB are acting guarantors of this study.
Funding statement: This work was supported by the National Library of Medicine of the National Institutes of Health [R01LM010812]. The funder had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Competing interests: None declared.
Ethical approval: Not required.
Appendix I
Literature review I: clinical manifestations
‘MERS-coronavirus’ or ‘Middle East respiratory syndrome’ or ‘MERS-CoV’ and ‘lower respiratory’ (678 results; 5% considered).
‘MERS-coronavirus’ or ‘Middle East respiratory syndrome’ or ‘MERS-CoV’ and ‘viral load’ (506 total results; 5% considered).
‘MERS-coronavirus’ or ‘Middle East respiratory syndrome’ or ‘MERS-CoV’ and ‘viral shedding’ (195 total results; 5% considered).
‘SARS-coronavirus’ or ‘severe acute respiratory syndrome’ or ‘SARS-CoV’ and ‘lower respiratory’ (4830 total results; 5% considered).
‘SARS-coronavirus’ or ‘severe acute respiratory syndrome’ or ‘SARS-CoV’ and ‘viral load’ (5200 total results; 5% considered).
‘SARS-coronavirus’ or ‘severe acute respiratory syndrome’ or ‘SARS-CoV’ and ‘viral shedding’ (1220 total results; 5% considered).
Literature review II: indirect transmission via environmental contamination
‘MERS-coronavirus’ or ‘Middle East respiratory syndrome’ or ‘MERS-CoV’ and ‘indoor’ and ‘ventilation’ (53 total results; 100% considered).
‘MERS-coronavirus’ or ‘Middle East respiratory syndrome’ or ‘MERS-CoV’ and ‘indoor’ and ‘air’ (107 total results; 100% considered).
‘MERS-coronavirus’ or ‘Middle East respiratory syndrome’ or ‘MERS-CoV’ and ‘fomite’ (139 total results; 100% considered).
‘SARS-coronavirus’ or ‘severe acute respiratory syndrome’ or ‘SARS-CoV’ and ‘indoor’ and ‘ventilation’ (1230 total results; 5% considered).
‘SARS-coronavirus’ or ‘severe acute respiratory syndrome’ or ‘SARS-CoV’ and ‘indoor’ and ‘air’ (2220 total results; 5% considered).
‘SARS-coronavirus’ or ‘severe acute respiratory syndrome’ or ‘SARS-CoV’ and ‘fomite’ (349 total results; 5% considered).
Appendix II
Supplementary table
Table AII.1.
Characteristics associated with human-to-human transmission, multivariate statistics (including length of hospital stay data for n=166 cases)
| Variable | Adjusted odds ratio | 95% CI | p-value |
|---|---|---|---|
| Case class | |||
| Healthcare Worker | Reference | ||
| Visitor | 1.97 | 0.16–24.71 | 0.6 |
| Patient | 5.93 | 0.66–53.39 | 0.11 |
| Gender | |||
| Female | Reference | ||
| Male | 0.85 | 0.33–2.17 | 0.73 |
| Age (continuous) | 0.98 | 0.94–1.01 | 0.22 |
| Comorbidity status | |||
| Non-comorbid | Reference | ||
| Comorbid | 2.18 | 0.72–6.63 | 0.17 |
| Case outcome | |||
| Recovered | Reference | ||
| Deceased | 3.51 | 0.95–12.90 | 0.06* |
| Length of hospital stay (continuous) | 1.07 | 0.99–1.14 | 0.06* |
*Rounded from p=0.059 (case outcome) and p=0.063 (length of hospital stay), respectively.
References
- 1. ProMED Mail Novel coronavirus—Saudi Arabia: human isolate. http://www.promedmail.org (accessed 13 March, 2017).
- 2. World Health Organization Middle East respiratory syndrome coronavirus (MERS-CoV). http://www.who.int/emergencies/mers-cov/en/ (accessed 13 March, 2017).
- 3. Memish ZA, Cotton M, Meyer B et al. Human infection with MERS-coronavirus after exposure to infected camels, Saudi Arabia, 2013. Emerg Inf Dis 2014;20:1012–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Raj VS, Osterhaus AD, Fouchier RA et al. MERS: emergence of a novel human coronavirus. Curr Opin Virol 2014;5:58–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Saudi Ministry of Health MERS Statistics Arabic. http://www.moh.gov.sa/ccc/pressreleases/pages/default.aspx (accessed 13 March, 2017).
- 6. World Health Organization Middle East respiratory syndrome coronavirus (MERS-CoV)—update. http://www.who.int/csr/don/2014_06_26/en/ (accessed 13 March, 2017).
- 7. Chu KH, Tsang WK, Tang CS et al. Acute renal impairment in coronavirus-associated severe acute respiratory syndrome. Kidney Int 2005;67:698–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tsiodras S, Baka A, Mentis A et al. A case of imported Middle East respiratory syndrome coronavirus infection and public health response, Greece, April 2014. Euro Surveill 2014;19:pii. 20782. [DOI] [PubMed] [Google Scholar]
- 9. Penttinen PM, Kaasik-Aaslav K, Friaux A et al. Taking stock of the first 133 MERS-coronavirus cases globally—is the epidemic changing? Euro Surveill 2013;18:pii. 20596. [DOI] [PubMed] [Google Scholar]
- 10. Hijawi B, Abdallat M, Sayaydeh A et al. Novel coronavirus infections in Jordan, April 2012: epidemiological findings from a retrospective investigation. East Mediterr Health J 2013;19:S12–18. [PubMed] [Google Scholar]
- 11. Majumder MS, River C, Lofgren E et al. Estimation of MERS-coronavirus reproductive number and case fatality rate for the Spring 2014 Saudi Arabia outbreak: insights from publicly available data. PLoS Curr Out 2014;6:pii. ecurrents.outbreaks.98d2f8f3382d84f390736cd5f5fe133c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cowling BJ, Park M, Fang VJ et al. Preliminary epidemiological assessment of MERS-CoV outbreak in South Korea, May to June 2015. Euro Surveill 2015;20:pii. 21163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. South Korea Ministry of Health and Welfare. Press releases http://www.mohw.go.kr/eng/sg/ssg0111ls.jsp?PAR_MENU_ID=1001&MENU_ID=100111 (accessed 13 March, 2017).
- 14. World Health Organization Coronavirus infections: disease outbreak news. http://www.who.int/csr/don/archive/disease/coronavirus_infections/en/ (accessed 13 March, 2017).
- 15. Centers for Disease Control and Prevention Middle East Respiratory Syndrome (MERS). https://www.cdc.gov/coronavirus/mers/faq.html. (accessed 30 March, 2017).
- 16. Lee N, Chan PKS, Hui DSC et al. Viral loads and duration of viral shedding in adult patients hospitalized with influenza. J Infect Dis 2009;200:492–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Li CC, Wang L, You HL et al. Correlation of pandemic (H1N1) 2009 viral load with disease severity and prolonged viral shedding in children. Emerg Infect Dis 2010;16:1265–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Thomas RJ. Particle size and pathogenicity in the respiratory tract. Virulence 2013;4:847–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bourouiba L, Dehandschoewercker E, Bush JWM. Violent expiratory events: on coughing and sneezing. J Fluid Mech 2014;745:537–63. [Google Scholar]
- 20. Bourouiba L. A sneeze. N Engl J Med 2016;357:e15. [DOI] [PubMed] [Google Scholar]
- 21. Pitzer VE, Leung GM, Lipsitch M. Estimating variability in the transmission of severe acute respiratory syndrome to household contacts in Hong Kong, China. Am J Epidemiol 2007;166:355–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Drosten C, Seilmaier M, Croman VM et al. Clinical features and virological analysis of a case of Middle East respiratory syndrome coronavirus infection. Lancet Infect Dis 2013;13:745–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Memish ZA, Zmula AI, Assiri A. Middle East Respiratory Syndrome coronavirus infections in health care workers. N Engl J Med 2013;369:884–6. [DOI] [PubMed] [Google Scholar]
- 24. Omrani AS, Matin MA, Haddad Q et al. A family cluster of Middle East Respiratory Syndrome coronavirus infections related to a likely unrecognized asymptomatic or mild case. Int J Infect Dis 2013;17:e668–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Al-Gethamy M, Corman VM, Hussain R et al. A case of long-term excretion and subclinical infection with Middle East Respiratory Syndrome coronavirus in a healthcare worker. Clin Infect Dis 2015;60:973–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Memish ZA, Al-Tawfiq JA, Makhdoom HQ et al. Respiratory tract samples, viral load, and genome fraction yield in patients with Middle East Respiratory Syndrome. J Infect Dis 2014;210:1590–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moser MR, Bender TR, Margolis HS et al. An outbreak of influenza aboard a commercial airliner. Am J Epidemiol 1979;110:1–6. [DOI] [PubMed] [Google Scholar]
- 28. Bloch AB, Orenstein WA, Ewing WM et al. Measles outbreak in a pediatric practice: airborne transmission in an office setting. Pediatrics 1985;75:676–83. [PubMed] [Google Scholar]
- 29. Butz AM, Fosarelli P, Dick J et al. Prevalence of rotavirus on high-risk fomites in day-care facilities. Pediatrics 1993;92:202–5. [PubMed] [Google Scholar]
- 30. Boone SA, Gerba CP. Significance of fomites in the spread of respiratory and enteric viral disease. Appl Environ Microbiol 2007;73:1687–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Scharfman BE, Techet AH, Bush JWM et al. Visualization of sneeze ejecta: steps of fluid fragmentation leading to respiratory droplets. Exp Fluids 2016;57:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Teytelman A, Larson RC. Modeling influenza progression within a continuous-attribute heterogeneous population. Eur J Oper Res 2012;220:238–50. [Google Scholar]
- 33. Finkelstein SN, Larson RC, Nigmatulina K et al. Engineering effective responses to influenza outbreaks. Serv Sci 2015;7:119–31. [Google Scholar]
- 34. Majumder MS, Kluberg SA, Mekaru SR et al. Mortality risk factors for Middle East Respiratory Syndrome outbreak, South Korea, 2015. Emerg Infect Dis 2015;21:2088–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rivers CM, Majumder MS, Lofgren ET. Risks of death and severe disease in patients with Middle East Respiratory Syndrome coronavirus, 2012–2015. Am J Epidemiol 2016;184:460–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jiang Y, Zhao B, Li X et al. Investigating a safe ventilation rate for the prevention of indoor SARS transmission: an attempt based on a simulation approach. Build Simul 2009;2:281–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Yam R, Yuen PL, Yung R et al. Rethinking hospital general ward ventilation design using computational fluid dynamics. J Hosp Infect 2011;77:31–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bourouiba L, Gourley S, Liu R et al. Avian influenza spread and transmission dynamics In: D. Chen, B. Moulin, J. Wu (editors). Analyzing and Modeling Spatial and Temporal Dynamics of Infectious Diseases, 1st edn Hoboken, New Jersey: John Wiley & Sons, Inc.; 2014, pp. 137–63. [Google Scholar]
- 39. Bourouiba L, Teslya SL, Wu J. Highly pathogenic avian influenza outbreak mitigated by seasonal low pathogenic strains: Insights from dynamic modeling. J Theor Biol 2011;271:181–201. [DOI] [PubMed] [Google Scholar]
- 40. Momattin H, Mohammed K, Zumia A et al. Therapeutic options for Middle East Respiratory Syndrome coronavirus (MERS-CoV)—possible lessons from a systematic review of SARS-CoV therapy. Int J Infect Dis 2013;17:e792–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Al-Tawfiq JA, Zumla A, Memish ZA. Travel implications of emerging coronaviruses: SARS and MERS-CoV. Travel Med Infect Dis 2014;12:422–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tsang OT, Chau TN, Choi KW et al. Coronavirus-positive nasopharyngeal aspirate as predictor for severe acute respiratory syndrome mortality. Emerg Infect Dis 2003;9:1381–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Tsui PT, Kwok ML, Yuen H et al. Severe acute respiratory syndrome: clinical outcome and prognostic correlates. Emerg Infect Dis 2003;9:1064–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Chan PKS, To WK, Ng KC et al. Laboratory diagnosis of SARS. Emerg Infect Dis 2004;10:825–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Chu CM, Poon LL, Cheng VC et al. Initial viral load and outcomes of SARS. Canad Med Assoc J 2004;171:1349–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hung IFN, Cheng VCC, Wu AKL et al. Viral loads in clinical specimens and SARS manifestations. Emerg Infect Dis 2004;10:1550–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Chu CM, Cheng VC, Hung IF et al. Viral load distribution in SARS outbreak. Emerg Infect Dis 2005;11:1882–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Guery B, Poissy J, El-Mansouf L et al. Clinical features and viral diagnosis of two cases of infection with Middle East Respiratory Syndrome coronavirus: a report of nosocomial transmission. Lancet 2013;381:2265–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Memish ZA, Assiri AM, Al-Tawfiq JA. Middle East Respiratory Syndrome coronavirus (MERS-CoV) viral shedding in the respiratory tract: an observational analysis with infection control implications. Int J Infect Dis 2014;29:307–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Poissy J, Goffard A, Parmentier-Decrucq E et al. Kinetics and pattern of viral excretion in biological specimens of two MERS-CoV cases. J Clin Virol 2014;61:275–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Corman VM, Albarrak AM, Omran AS et al. Viral shedding and antibody response in 37 patients with MERS-Coronavirus infection. Clin Infect Dis 2016;62:477–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Feikin DR, Alraddadi B, Qutub M et al. Association of higher MERS-CoV virus load with severe disease and death, Saudi Arabia, 2014. Emerg Infect Dis 2015;21:2029–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Min CK, Cheon S, Ha NY et al. Comparative and kinetic analysis of viral shedding and immunological responses in MERS patients representing a broad spectrum of disease severity. Sci Rep 2016;6:pii. 25359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Jiang S, Huang L, Chen X et al. Ventilation of wards and nosocomial outbreak of severe acute respiratory syndrome among healthcare workers. Chin Med J (Engl) 2003;116:1293–7. [PubMed] [Google Scholar]
- 55. Lee N, Hui D, Wu A et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med 2003;348:1986–94. [DOI] [PubMed] [Google Scholar]
- 56. Dowell SF, Simmerman JM, Erdman DD et al. Severe acute respiratory syndrome coronavirus on hospital surfaces. Clin Infect Dis 2004;39:652–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lau JTF, Yang X, Leung PC et al. SARS in three categories of hospital workers, Hong Kong. Emerg Infect Dis 2004; 10(8): 1399–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Booth TF, Kournikakis B, Bastien N et al. Detection of airborne severe acute respiratory syndrome (SARS) coronavirus and environmental contamination in SARS outbreak units. J Infect Dis 2005;191:1472–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Li Y, Huang X, Yu IT et al. Role of air distribution in SARS transmission during the largest nosocomial outbreak in Hong Kong. Indoor Air 2005;15:83–95. [DOI] [PubMed] [Google Scholar]
- 60. Yu IT, Wong TW, Chiu YL et al. Temporal-spatial analysis of severe acute respiratory syndrome among hospital inpatients. Clin Infect Dis 2005;40:1237–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Chen C, Zhao B, Yang X et al. Role of two-way airflow owing to temperature difference in severe acute respiratory syndrome transmission: revisiting the largest nosocomial severe acute respiratory syndrome outbreak in Hong Kong. J R Soc Interface 2011;8:699–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Van Doremalen N, Bushmaker T, Munster VJ. Stability of Middle East Respiratory Syndrome coronavirus (MERS-CoV) under different environmental conditions. Euro Surveill 2013;18:pii. 20590. [DOI] [PubMed] [Google Scholar]
- 63. Bin SY, Heo JY, Song MS et al. Environmental contamination and viral shedding in MERS patients during MERS-CoV outbreak in South Korea. Clin Infect Dis 2016;62:755–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Fagbo SF, Skakni L, Chu DKW et al. Molecular epidemiology of hospital outbreak of Middle East Respiratory Syndrome, Riyadh, Saudi Arabia, 2014. Emerg Infect Dis 2015;21:1981–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Heo DA, Lee J, Huh EH et al. Problems of the Middle East Respiratory Syndrome outbreak from the perspective of environmental health: focusing on control of indoor air quality in hospitals. Korean J Environ Health Sci 2015;41:216–21. [Google Scholar]
- 66. Lee SS, Wong NS. Probable transmission chains of Middle East Respiratory Syndrome coronavirus and the multiple generations of secondary infection in South Korea. Int J Infect Dis 2015;38:65–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Song JY, Cheong HJ, Choi MJ, et al. Viral shedding and environmental cleaning in Middle East Respiratory Syndrome coronavirus infection. Infect Chemother 2015;47:252–5. [DOI] [PMC free article] [PubMed] [Google Scholar]