Abstract
Background. Stair climb power is an important clinical measure of lower-extremity power. The stair climb power test (SCPT) was validated by requiring individuals to climb a full flight of stairs. A 4-step SCPT (4SCPT) would be more clinically feasible and easier to perform, yet its reliability and validity are unknown.
Objective. To evaluate reliability, validity, and minimal detectable change of 4SCPT among community-dwelling older adults.
Design. This study is a cross-sectional analysis of baseline data from a clinical trial.
Methods. Fifty older adults ≥65 years of age, at risk for mobility decline, consented to participate in this ancillary study. Test-retest reliability was derived from 2 measurements within each participant measured by a single assessor. Pearson correlation analyses among leg power measures (4SCPT, SCPT, single leg press power at 40% and 70% of the 1-repetition maximum [SLP40, SLP70]) were performed. Separate multivariate linear regressions were conducted evaluating the associations between each leg power measure and 2 mobility outcomes, the Short Physical Performance Battery (SPPB) and habitual gait speed (HGS). Minimal detectable change was based on a 90% confidence interval (MDC90).
Results. The 4SCPT had excellent test-retest reliability (ICC(2,1) = 0.951), and strong correlation with SCPT, SLP40, and SLP70 (r = 0.85-0.96). The 4SCPT explained a greater amount of variance in the SPPB (R2 = 0.31) than other leg power measurements (R2 = 0.23-0.25). The 4SCPT (R2 = 0.41) and SCPT (R2 = 0.42) described equivalent amounts of variance in HGS, and greater than that with SLP40 (R2 = 0.28) and SLP70 (R2 = 0.30). The MDC90 for 4SCPT was 44.0 watts.
Limitations. This was a cross-sectional analysis within a small, nonrepresentative sample. Interrater reliability was not evaluated.
Conclusions. The 4SCPT shows scientific promise as a valid and reliable leg power measurement among community-dwelling older adults.
Leg muscular power is a neuromuscular attribute linked with balance, falls, and the maintenance of functional independence of community-dwelling older adults.1-3 For the purposes of research, leg muscle power is typically measured with specialized and expensive exercise testing equipment. A more clinically feasible and inexpensive test that has been advocated for use in ambulatory clinical settings and large-scale clinical trials is the stair climb power test (SCPT). This test has been utilized as an outcome in a variety of clinical trials addressing hip or knee osteoarthritis,4–6 stroke,7 and diabetes.8 Also, it has been used in trials aiming to improve muscle mass9,10 and physical function,11 and to prevent fall12 in healthy and mobility-limited elderly.
The SCPT is viewed as clinically feasible and low cost because the pieces of equipment required to conduct it are only a stopwatch, a scale to measure a participant's weight, and a flight of stairs. The SCPT test was originally validated using a full flight of 10–11 stairs,13 which may not always be available or feasible for use in ambulatory care settings treating vulnerable patients. However, many physical therapy clinics have training staircases with a small flight up to 4 steps, which is available commercially and easier to utilize within clinical settings with limited space or without simple access to a full flight of stairs. Two clinical trials have used the 4-step stair climb test as an outcome to examine the changes in leg power after exercise interventions.14,15 However, the psychometric properties of this simpler mode of stair climbing power testing have not yet been evaluated. Therefore, we sought to examine the test-retest reliability, validity, and minimal detectable change of leg power measured on a flight of 4 steps (4SCPT) among community-dwelling older adults at risk for mobility decline. We hypothesized that the 4SCPT would be reliable and valid when compared to the standard SCPT as well as other established measures of lower-extremity power and mobility.
Methods
Participants
We conducted an ancillary cross-sectional analysis of baseline data from a clinical trial (ClinicalTrial.gov Identifier: NCT02580409) of exercise among community-dwelling older adults. This ancillary study was initiated after inception of the larger clinical trial from which it was derived. Therefore, the final 50 participants recruited into the clinical trial participated in this ancillary study. This study was approved by the Institutional Review Board at Spaulding Rehabilitation Hospital. Participants were recruited from primary care practices with the following inclusion criteria: age ≥65 years, ability to speak and understand English, difficulty or task modification with walking ½ mile and/or climbing 1 flight of stairs, no planned major surgery, expectation of living in the area for ≥2 years, Short Physical Performance Battery (SPPB) score ≥4, and able to finish 400 m walk test within 15 min. Exclusion criteria included: significant visual impairment, uncontrolled hypertension, lower-extremity amputation, supplemental oxygen use, myocardial infarction, major surgery in the previous 6 months, Mini Mental State Exam (MMSE) score <18, Short Physical Performance Battery (SPPB) score <4, and not able to finish 400 m walk test within 15 min.
Procedure
The baseline evaluations were given on 2 separate days at participants’ convenience. The time lag between the 2 evaluation visits was an average of 10.9 ± 7.3 days (mean ± SD). On the first testing day after providing informed consent, participants underwent an MMSE, comprehensive history examination, SPPB, and 6-minute walk test to confirm the eligibility for participation. On the second testing day, each participant underwent 4 leg muscle power tests, including SCPT, 4SCPT, and single leg press power tests (at 2 intensities) consecutively. Rest periods were offered to participants between every test of the study assessments. All of the physical assessments were performed by a physical therapist (with more than 3 years of working experience with older individuals). Each SCPT and 4SCPT was performed 2 times for each participant, and the average of 2 repetitions was used for analysis. The first trial was followed immediately by the second trial. If participants used the handrail in the SCPT, they were asked to use the handrail in the 4SCPT.
Leg Power Measures
4SCPT
Participants were instructed to ascend a flight of 4 stairs as fast as they could, and were allowed to use the handrail if they thought it was necessary for the purpose of safety. They stood at the base of the stairs and started climbing when the tester said, “Ready, set, go.” Timing began after the tester said “go” and stopped when both feet of a participant reached the top step. Stair climb power was calculated with the following formula: power = ((body weight in kg) x (9.8 m/s2) x (stair height in meter))/(time in seconds), where the height of the full flight of stairs was 0.762 meter (30 inches).
SCPT
This test was conducted as previously described, which is identical to the 4SCPT except the flight height is different.11 There were 10 stairs for this test, with the total flight height being 1.985 meters.13
Single leg press test
A pneumatic leg press resistance machine (Keiser A420, Keiser Sports Health Equipment, Fresno, CA) was used to measure peak power performed at both 40% and 70% of the 1-repetition maximum. First, participants had their 1-repetition maximum (1RM) measured separately for each leg. This was obtained as previously described16 by gradually increasing the load, based on their perceived exertion level using the Borg Rating of Perceived Exertion Scale,17 until the maximum amount of force could be generated in 1 maximal contraction through the full range of motion. Once the 1RM was obtained, single leg press power was measured by completing 5 repetitions with each leg at both 40% 1RM and 70% 1RM. The peak power at 40%1RM (SLP40) or 70%1RM (SLP70) was recorded as the best of 5 repetitions with either leg at the corresponding resistance. For each trial, participants were told to exert force as fast as possible during the concentric phase and move slowly through the eccentric phase. The software integrated in the Keiser pneumatic resistance machine calculates work and power only based on the outgoing stroke (concentric phase) of each trial by sampling the system pressure (force) at the cylinder 400 times per second and recording the distance traveled by the piston. Therefore, the data was only collected during the concentric phase of the muscle action.18,19
Mobility Performance Measures
SPPB
The SPPB comprises 3 subcomponents: standing balance, habitual gait speed (HGS), and a 5-repetition chair stand test.20 The standing balance component includes scoring based upon the ability to perform 3 progressive standing positions (side-by-side standing, semi-tandem stand, and tandem stand). For gait speed, participants were asked to stand behind a line and then start to walk at their comfortable speed across a 4 m distance. Timing starts on the “begin” command and stops when 1 foot crosses the end of the 4 m course. Two trials were performed for each participant, with the fastest of the trials being scored based on time. The 5-time chair stand test requires participants to stand up straight and sit down as quickly as possible, without stopping in between. Participants keep their arms folded across the chest. Performance on each subcomponent is scored between 0–4 and added to yield a composite score ranging from 0–12, with higher scores indicating better performance. The SPPB is a reliable and valid measure of lower-extremity performance and predictive of disability, hospitalization, and death.21,22
HGS
The HGS was derived from the subcomponent of SPPB, in which participants were instructed to walk at their usual pace over a distance of 4 m, and was calculated as 4/(time in second). Gait speed is also predictive of disability and mortality.21,23
Statistical Analysis
Statistical Analysis Software version 9.4 (SAS Institute Inc., Cary, NC) was used for analysis. A total of 50 participants were included in the data analyses. The assumption of normality, by using the Shapiro–Wilk test and Kolmogorov–Smirnov test, was tested to evaluate for influential data points. The test-retest reliability of the 4SCPT was measured by using intraclass correlation coefficient (ICC). The first and second measures were used to calculate the ICC(2,1). The value of ICC can be interpreted as those above 0.75 indicating good reliability, those between 0.50 and 0.75 indicating moderate reliability, and those below 0.50 indicating poor reliability.24
Bivariate Pearson correlation analyses among leg power tests were conducted to evaluate: a) the concurrent validity (the degree that a measurement correlates a standard measurement) of 4SCPT, by comparing it to the reference standard test, SCPT; and b) the criterion validity (compares a test with other measures already held to be valid) of 4SCPT, by comparing it to SLP40 and SLP70 values. Meanwhile, linear regression analysis was used to evaluate the agreement between 4SCPT and SCPT, with 4SCPT as the predictor and SCPT as the outcome. Bland–Altman analysis was used to show the amount of difference between the 2 stair climb power measures. The Bland–Altman plot is a scatter plot of the variable's means on the horizontal axis and the variable's differences on the vertical axis. It also includes 95% confidence intervals of the mean difference.
The convergent validity (the degree that a measurement is consistent with other measurements) of 4SCPT was evaluated by examining the relationship between each stair climb power test and measures of performance-based mobility. Separate linear regression models were constructed to evaluate the contribution of each stair climb power measurement (4SCPT or SCPT) to either of the 2 mobility tests (SPPB and HGS), adjusting for age, gender, weight, and height. The significance level of the following analyses was set at .05. As part of post hoc analysis, we evaluated the correlation coefficients with the chair stand and balance components of the SPPB using Spearman correlation analyses in order to understand which components were most strongly associated with the 2 SCPT tests.
Finally, the minimal detectable change of 4SCPT was measured by using standard error of measurement (SEM). Minimal detectable change is an estimate of the smallest amount of change that can be detected by a measure that corresponds to a noticeable change in ability. It was calculated as MDC90 = SEM*1.645*√2,25 with 90% confidence intervals, where the SEM = SDbaseline* √(1-r) and r is the test-retest reliability.15
Results
Demographic Characteristics
Participants had a mean age of 77.2 years and were predominantly women (52%) and Caucasians (92%) (Table 1). Participants had a mean SPPB of 8.6, and a habitual gait speed of .86 m/s. Thirty-eight (76%) of the 50 participants used the handrail during stair climb tests (4SCPT, SCPT) because of self-perceived safety concerns.
Table 1.
Baseline Characteristics of 50 Community–Dwelling Older Individualsa
| Characteristic | Mean ± SD | Range |
|---|---|---|
| Age (y) | 77.2 ± 6.1 | 67–88 |
| Female (%) | 52 | |
| Race (%) | ||
| Caucasian | 92 | |
| African American | 6 | |
| Asian | 2 | |
| Using handrail (%) | 76 | |
| Height (cm) | 168.8 ± 10.7 | 147–202 |
| Weight (kg) | 79.2 ± 17.2 | 46–132 |
| SPPB (score) | 8.6 ± 1.8 | 4–12 |
| HGS (m/s) | 0.86 ± 0.2 | 0.56–1.32 |
| 4SCPT (watts) | 211.1 ± 85.5 | 57–470 |
| SCPT (watts) | 225.9 ± 96.7 | 56–555 |
| SLP40 (watts) | 377.5 ± 172.9 | 62–864 |
| SLP70 (watts) | 393.8 ± 179.4 | 100–837 |
a4SCPT = 4–step stair climb power test; SCPT = stair climb power test; SLP40 = single leg press power at 40%1RM; SLP70 = single leg press power at 70%1RM.
Test-Retest Reliability
The 4SCPT test-retest reliability revealed an ICC(2,1) = 0.951 with the 95% confidence interval ranging from 0.920 to 0.972 (P < .001).
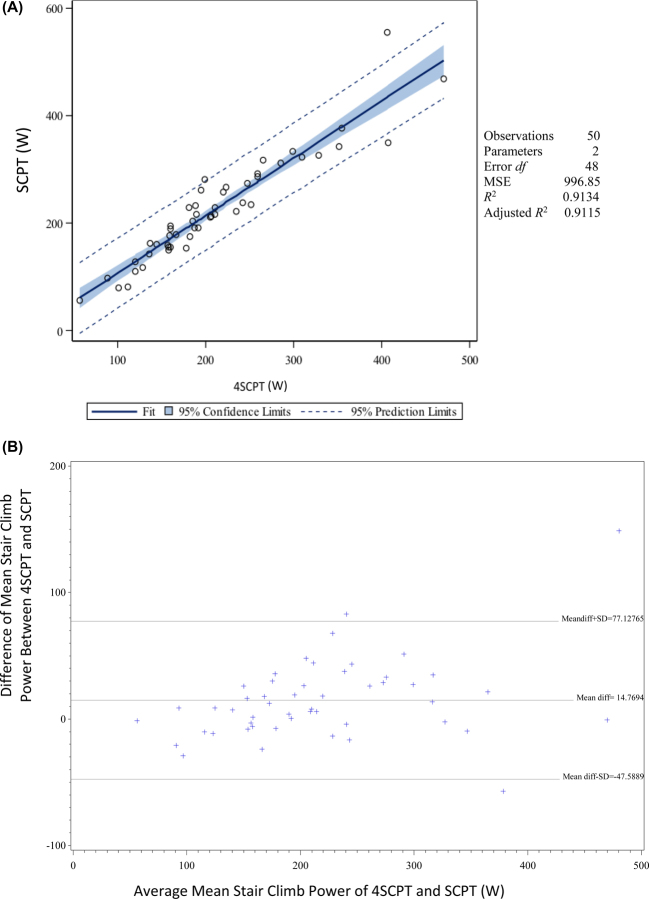
Concurrent Validity
The Pearson correlation coefficients between 4SCPT and SCPT are excellent, with r = 0.96 (P <. 001). Figure 1A shows the regression line between 4SCPT and SCPT, and Figure 1B shows the Bland–Altman plot. The average of the differences between 4SCPT and SCPT was 14.8 watts (95% CI, -47.6, 77.1, P <. 001). The regression model showed that 1 participant was considered as an outlier for the high value of SCPT (555 watts) according to a Cook's D value of 1.2, where R2 = 0.91, P < .001. The regression equation was SCPT = 0.2 + 1.06*4SCPT. When the analysis was repeated excluding this value, the findings were not materially different, except the mean difference between 4SCPT and SCPT was decreased to 12.0 watts (95% CI, -38.0, 62.1, P < .001). The regression analysis yielded an R2 at 0.92, SCPT = 12.0 + 4SCPT, P < .001.
Figure.
(A) Linear regression line of leg power from 4-step stair climb power (4SCPT) and 10-step stair climb power (SCPT); (B) Bland–Altman plots of the measured 4-step stair climb power and 10-step stair climb power. W = watts.
Criterion Validity
The correlations between 4SCPT and SLP40 or SLP70 were 0.85 (P < .001) and 0.86 (P < .001), respectively. And the correlations between SCPT and SLP40 or SLP70 were 0.85 (P < .001) and 0.87 (P < .001), respectively.
Convergent Validity
Table 2 reports separate multivariable linear regression models predicting both the SPPB and HGS. Within models adjusted for age, gender, weight, and height, the 4SCPT described (adjusted R2 = 0.31, 95%CI 0.12, 0.50, P < .001) greater variance with the outcome than did the other models using other leg power measures (adjusted R2 = 0.23-0.25, 95%CI 0.05, 0.43, P < .05). Within multivariable linear regression models predicting HGS, stair climb power measures explained similar levels of variance with the outcome (4SCPT: adjusted R2 = 0.41, 95%CI 0.23, 0.59; SCPT: adjusted R2 = 0.42, 95%CI 0.24, 0.60, P < .001) and greater levels of variance than with models using the single leg press measures (SLP40: adjusted R2 = 0.28, P = .01; SLP70: adjusted R2 = 0.31, P < .001). No change in regression coefficient was detected after excluding the outliner. Within our post hoc analysis, we found that the correlations between the balance components of the SPPB and 4SCPT or SCPT were 0.19 (P = .041) and.22 (P = .039), respectively. And the correlations between the 5-time chair stand time and 4SCPT or SCPT were -0.14 (P = .45) and -0.07 (P = .13), respectively.
Table 2.
Separate Linear Regression Models Between Leg Muscle Power and Mobility Measures Adjusting for Age, Gender, Weight, and Height in 50 Participantsa
| Performance test | Power measure (watts) | Parameter Estimate | Adjusted R-square (95% CI) | Model P |
|---|---|---|---|---|
| SPPB | 4SCPT | 0.015 | 0.31 (0.12-0.50) | .004 |
| SCPT | 0.01 | 0.23 (0.05-0.41) | .04 | |
| SLP40 | 0.007 | 0.25 (0.07-0.43) | .03 | |
| SLP70 | 0.007 | 0.25 (0.07-0.43) | .03 | |
| HGS | 4SCPT | 0.002 | 0.41 (0.23-0.59) | <.001 |
| SCPT | 0.002 | 0.42 (0.24-0.60) | <.001 | |
| SLP40 | 0.005 | 0.28 (0.09-0.47) | .01 | |
| SLP70 | 0.006 | 0.31 (0.11-0.49) | .006 |
a4SCPT = 4-step stair climb power test; SCPT = stair climb power test; SLP40, SLP70 = single leg press at 40% and 70% 1-repetition maximum; SPPB = short physical performance battery; HGS = habitual gait speed; CI = confidence interval.
Minimal Detectable Change
The calculated SEM for 4SCPT was 18.9 watts, and for SCPT was 19.6 watts. The calculated MDC90 for 4SCPT was 44.0 watts and for SCPT was 45.6 watts.
Discussion
The purpose of this study was to evaluate the psychometric properties of the 4SCPT, a simple and clinically feasible means of measuring lower limb muscle power. Within our sample of mobility-limited older adults, and in comparison to more standard measures of lower limb power, we were able to observe excellent reliability and strong validity of the 4SCPT. Similar values of the standard error of measurement and minimal detectable change were found to those observed with SCPT. Taken together, these observations strongly support the reliability and validity of using the 4SCPT as a clinical measure of lower limb power.
Our analyses of concurrent and criterion validity support the use of the 4SCPT among mobility-limited older adults. The 4SCPT was strongly correlated with SCPT, SLP40, and SLP70, identifying it as a valid test of leg muscle power, as SCPT and single leg press test have been validated to test leg muscle power in older populations.13 With regard to the convergent validity, we used well-established measures of mobility (ie, SPPB, HGS) that are predictive for the development of important adverse outcomes such as disability, institutionalization, and death. It is important to note that the model with the 4SCPT described more variance in the SPPB than did the SCPT (adjusted R2 = 0.31 vs adjusted R2 = 0.23). In other words, performance of the 4SCPT is more closely associated with components of the SPPB than is the SCPT. The relatively equivalent strength of association with HGS suggests that much of the difference between 4SCPT and SCPT with the SPPB may be due to stronger associations with the balance and/or chair stand components of the SPPB. To evaluate this, we performed a post hoc analysis and found a stronger and statically significant association between chair stand and 4SCPT (r = -0.14, P = .045) than that between chair stand and SCPT (r = -0.07, p = 0.13), but similar strength of correlation between balance component and the 2 stair climb tests (4SCPT: r = 0.19; SCPT: r = 0.22). Although the confidence intervals of the variances in SPPB explained by 4SCPT and SCPT overlap to some extent, the significant correlation between chair stand and 4SCPT may indicate a stronger correlation between SPPB and 4SCPT. This suggests that in comparison to the SCPT, the 4SCPT, with its shorter flight distance, may be more functionally compatible to the chair stand component of the SPPB. Chair stand performance is predictive of injurious falls.26 Taken together, these points suggest that the 4SCPT might be useful in the assessment of older adults at risk for fall-related injuries.
We found that the SEMs of the 2 stair climb power measures obtained in this study ranged from 18.9 to 19.6 watts, and the MDC90 ranged from 44.0 to 45.6 watts. This was lower than values previously reported by Beauchamp et al,27 with an SEM of 27.3 watts and an MDC90 at 63.4 watts for the SCPT. In the current study, the SDbaseline for the 4SCPT was 85.5 watts, which was similar to that reported by Beauchamps et al (86.1 watts). Since the SEM is partly dependent upon the test-retest reliability (SEM = SDbaseline* √(1-r), and r is the test-retest reliability), it may be that the greater test-retest reliability of the current cohort contributed to a lower SEM value, and therefore a lower MDC90 value. However, the heterogeneity of the sample should also be taken into consideration. Therefore, the MDC90 may need to be further validated within a larger and more representative cohort of older adults.
Timed stair climb tests have been widely utilized as an outcome to measure muscle power and mobility function29 across a wide range of ages and health conditions.4,7,12,30 The 4-step training staircase is common among outpatient rehabilitative care clinics, making the potential for lower-extremity leg power testing widely feasible in the care of older adults. A systematic review30 has suggested that a longer flight of stairs may place greater demand on cardiovascular capacity, thereby potentially limiting test performance by factors other than leg power.31 Also, from a practical standpoint, it may be easier for a busy therapist to conduct the 4SCPT, given the greater ease with guarding potential falls and shortened test duration. Commercially available 4-step training staircases currently cost <$1000 and take up approximately 1500 square feet, further underscoring the feasibility for busy clinics across a variety of care settings to provide this mode of testing.
This study has several potential limitations. Our study had a small sample size and the majority of the participants are Caucasians, so it may not generalize to other samples of older adults. Also, as a single tester made all the assessments, the interrater reliability of 4SCPT is unknown. It would be worthwhile confirming these relationships, within a study of larger and more functionally diverse sample that evaluated the 4SCPT ability to predict adverse outcomes relevant to rehabilitative care such as functional decline. Also, there are several strengths of this study. We conducted our study within a vulnerable population, older adults at risk for mobility decline. They manifested a mean SPPB score of 8.6, which is consistent with a moderate risk for adverse health outcomes.20 Based upon the severity of their mobility status, these are individuals for whom outpatient rehabilitative care would be clinically indicated. Also, we compared the test of interest, 4SCPT, with other measures of leg power and compared them with other important physical performance tasks.
Conclusion
The results of this study showed that the 4-step stair climb power test had excellent test-retest reliability (r = 0.95) and provided evidence of the responsiveness of stair climb power measures. The criterion of MDC90 (44 watts) could be used to determine a real change within similar populations. Our findings support the contention that the 4SCPT is a valid measure of leg muscle power, feasible for use in a variety of clinical settings.
Author Contributions and Acknowledgments
Concept/idea/research design: M. Ni, L.G. Brown, D. Lawler, J.F. Bean
Writing: M. Ni, J.F. Bean
Data collection: M. Ni, D. Lawler, J.F. Bean
Data analysis: M. Ni, J.F. Bean
Project management: L.G. Brown, D. Lawler, J.F. Bean
Fund procurement: J.F. Bean
Providing participants: J.F. Bean
Providing facilities/equipment: J.F. Bean
Providing institutional liaisons: J.F. Bean
Clerical/secretarial support: J.F. Bean
Consultation (including review of manuscript before submitting): J.F. Bean
The authors thank Dan Kiely for his contribution to the SAS coding.
Ethics Approval
This study was approved by the Institutional Review Board at Spaulding Rehabilitation Hospital.
Funding
This clinical trial (ClinicalTrial.gov Identifier: NCT02580409) was funded by a grant from the Rx Foundation.
Disclosures
The authors declare no potential conflicts of interest with respect to the research, authorship, or publication of this article.
Clinical Trial Registration
ClinicalTrial.gov Identifier: NCT02580409.
References
- 1. Bassey EJ, Fiatarone MA, O’Neill EF, Kelly M, Evans WJ, Lipsitz LA. Leg extensor power and functional performance in very old men and women. Clin Sci. 1992;82(Pt 3):321–327. [DOI] [PubMed] [Google Scholar]
- 2. Foldvari M, Clark M, Laviolette LC et al. . Association of muscle power with functional status in community-dwelling elderly women. J Gerontol A Biol Sci Med Sci. 2000;55(4):M192–199. [DOI] [PubMed] [Google Scholar]
- 3. Skelton DA, Greig CA, Davies JM, Young A. Strength, power and related functional ability of healthy people aged 65–89 years. Age Ageing. 1994;23(5):371–377. [DOI] [PubMed] [Google Scholar]
- 4. University of Iowa; The American Geriatrics Society Assessment of efficacy of low intensity resistance training in women at risk for symptomatic knee osteoarthritis. Available at: http://clinicaltrials.gov/show/NCT01440972. NLM Identifier: NCT01440972. Accessed September 20, 2016.
- 5. University of Iowa; National Institute on Aging (NIA) Mobility optimization through velocity exercise. Available at: http://clinicaltrials.gov/show/NCT00844558. NLM Identifier: NCT00844558. Accessed September 20, 2016.
- 6. Institute of Sports Medicine-Copenhagen & Musculoskeletal Rehabilitation Research Unit, Bispebjerg Hospital Exercise in patients with osteoarthritis of the hip. Available at: http://clinicaltrials.gov/show/NCT01387867. NLM Içdentifier: NCT01387867. Accessed September 20, 2016.
- 7. Ouellette MM, LeBrasseur NK, Bean JF et al. . High-intensity resistance training improves muscle strength, self-reported function, and disability in long-term stroke survivors. Stroke. 2004;35(6):1404–1409. [DOI] [PubMed] [Google Scholar]
- 8. Hospital de Clinicas de Porto Alegrel; Federal University of Rio Grande do Sul Diabetes resistance training adaptations in elderly. Available at: http://clinicaltrials.gov/show/NCT02548000. NLM Identifier: NCT02548000. Accessed September 20, 2016.
- 9. University of Toronto Functional changes and power training in older women. Available at: http://clinicaltrials.gov/show/NCT02530723. NLM Identifier: NCT02530723. Accessed September 20, 2016.
- 10. Regeneron Pharmaceuticals; Sanofi Study of the safety and efficacy of REGN1033 (SAR391786) in patients with sarcopenia. Available at: http://clinicaltrials.gov/show/NCT01963598. NLM Identifier: NCT01963598. Accessed September 20, 2016.
- 11. University of Southern Denmark; European Union; Odense University Hospital; University of Pittsburgh; National Institute on Aging (NIA); Maastricht University; University of Washington Functional impairments and exercise in older adults with low physical function. Available at: http://clinicaltrials.gov/show/NCT02051725. NLM Identifier: NCT02051725. Accessed September 20, 2016.
- 12. University of Potsdam; Swiss Council for Accident Prevention Effects of a fall preventive exercise program on intrinsic fall risk factors in healthy older adults. Available at: http://clinicaltrials.gov/show/NCT01906034. NLM Identifier: NCT01906034. Accessed September 20, 2016.
- 13. Bean JF, Kiely DK, LaRose S, Alian J, Frontera WR. Is stair climb power a clinically relevant measure of leg power impairments in at-risk older adults? Arch Phys Med Rehabil. 2007;88(5):604–609. [DOI] [PubMed] [Google Scholar]
- 14. Storer TW, Casaburi R, Sawelson S, Kopple JD. Endurance exercise training during haemodialysis improves strength, power, fatigability and physical performance in maintenance haemodialysis patients. Nephrol Dial Transplant. 2005;20(7):1429–1437. [DOI] [PubMed] [Google Scholar]
- 15. Galea MP, Levinger P, Lythgo N et al. . A targeted home-and center-based exercise program for people after total hip replacement: a randomized clinical trial. Arch Phys Med Rehabil. 2008;89(8):1442–1447. [DOI] [PubMed] [Google Scholar]
- 16. Callahan D, Phillips E, Carabello R, Frontera WR, Fielding RA. Assessment of lower extremity muscle power in functionally-limited elders. Aging Clin Exp Res. 2007;19(3):194–199. [DOI] [PubMed] [Google Scholar]
- 17. Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. [PubMed] [Google Scholar]
- 18. Foldvari M, Clark M, Laviolette LC et al. . Association of muscle power with functional status in community-dwelling elderly women. J Gerontol A Biol Sci Med Sci. 2000;55(4):M192–199. [DOI] [PubMed] [Google Scholar]
- 19. Bean JF, Kiely DK, Herman S et al. . The relationship between leg power and physical performance in mobility‐limited older people. J Am Geriatr Soc. 2002;50(3):461–467. [DOI] [PubMed] [Google Scholar]
- 20. Guralnik JM, Simonsick EM, Ferrucci L et al. . A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94. [DOI] [PubMed] [Google Scholar]
- 21. Guralnik JM, Ferrucci L, Pieper CF et al. . Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55(4):M221–231. [DOI] [PubMed] [Google Scholar]
- 22. Guralnik JM, Simonsick EM, Ferrucci L et al. . A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94. [DOI] [PubMed] [Google Scholar]
- 23. Fragala MS, Dam TT, Barber V et al. . Strength and function response to clinical interventions of older women categorized by weakness and low lean mass using classifications from the foundation for the national institute of health sarcopenia project. J Gerontol A Biol Sci Med Sci. 2015;70(2):202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 2nd ed Upper Saddle River, NJ: Prentice Hall Health; 2000:49–60, 557–586. [Google Scholar]
- 25. Haley SM, Fragala-Pinkham MA. Interpreting change scores of tests and measures used in physical therapy. Phys Ther. 2006;86(5):735–743. [PubMed] [Google Scholar]
- 26. Ward RE, Leveille SG, Beauchamp MK et al. . Functional performance as a predictor of injurious falls in older adults. J Am Geriatr Soc. 2015;63(2):315–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Beauchamp MK, Jette AM, Ward RE et al. . Predictive validity and responsiveness of patient-reported and performance-based measures of function in the Boston RISE study. J Gerontol A Biol Sci Med Sci. 2015;70(5):616–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Roig M, Eng JJ, MacIntyre DL, Road JD, Reid WD. Associations of the stair climb power test with muscle strength and functional performance in people with chronic obstructive pulmonary disease: A cross-sectional study. Phys Ther. 2010;90(12):1774–1782. [DOI] [PubMed] [Google Scholar]
- 29. World Health Organization International classification of functioning, disability and health (ICF). Available at: http://www.who.int/classifications/icf/en/. Updated July 22, 2016. Accessed September 20, 2016
- 30. Nightingale EJ, Pourkazemi F, Hiller CE. Systematic review of timed stair tests. J Rehabil Res Dev. 2014;51(3):335–350. [DOI] [PubMed] [Google Scholar]
- 31. Teh KC, Aziz AR. Heart rate, oxygen uptake, and energy cost of ascending and descending the stairs. Med Sci Sports Exerc. 2002;34(4):695–699. [DOI] [PubMed] [Google Scholar]