Abstract
With rapid urbanisation and improved living conditions as a result of rising incomes in Gulf Cooperation Council (GCC) countries, obesity has become a major and growing health problem for the region. The United Arab Emirates (UAE) has a resident population of 9.3 million (in 2016), many of whom (85.5%) lived in urban areas and led sedentary lifestyles. Based on the World Health Organisation (WHO) estimates for 2010, 25% of Emirati men and 40% of the women were obese. Obesity rates in this country has doubled from 16 to 34% compared to the year 2000, and severe obesity (BMI > 40 kg/m2) has risen dramatically from 2 to 11%. While a number of international guidelines for the management of obesity are already available in public domain, local guidelines for the UAE and the region, which are structured and individualized for the management of obesity, are sorely needed to help the family physician to provide affordable treatment for the patient at the point-of-care and to reduce the burden on the local healthcare system. A multi-disciplinary panel of international and regional experts who treat patients with overweight and obesity was convened with the aim of developing consensus recommendations for the UAE. The objective is to have a simple and easy-to-refer set of recommendations for busy clinicians as there were already many comprehensive international guidelines available. The panel reviewed and streamlined these recommendations in its entirety for relevance, coherence and usability in the local context. These recommendations for overweight and obesity management were circulated and endorsed by the local practising family medicine community, namely, the Emirates Medical Association and Family Medicine Society. We believe these recommendations would also be of interest to clinicians in other GCC countries. A summary and algorithm of these recommendations are provided.
Keywords: Obesity guidelines, Multi-disciplinary, Comprehensive lifestyle management, United Arab Emirates
Introduction
Obesity is defined as an abnormal or excessive fat accumulation caused by an imbalance between calories ingested versus calories expended [1, 2]. It is this excessive body fat which has accumulated that impairs bodily health and predisposes individuals to a range of chronic diseases such as heart disease, hypertension, stroke and diabetes which can lead to disability and death [3], or to debilitating conditions such as osteoarthritis, respiratory disorders and clinical depression which affect the quality of life (QoL) [4]. Obesity is also influenced by genetic, environmental and lifestyle factors [3]. Common measures of obesity include the BMI, waist circumference and waist-to-hip circumference ratio [3].
With rapid urbanisation and improved living conditions as a result of rising incomes in Gulf Co-Operation Council (GCC) countries, obesity has become a major and growing health problem for the region [5, 6, 7, 8]. The mean BMI for male and female patients visiting primary care physicians was found to be 28.2 and 28.7 kg/m2 and for WC 98.2 and 93.4 cm respectively [9]. The United Arab Emirates (UAE) has a resident population of 9.3 million (in 2016), many of whom (85.5%) lived in urban areas and led sedentary lifestyles [10]. Based on the World Health Organisation (WHO) estimates for 2010, 25% of Emirati men and 40% of the women were obese [5]. Obesity rates in this country has doubled from 16 to 34% compared to 2000, and severe obesity (BMI ≥ 40 kg/m2) has risen dramatically from 2 to 11% [11]. This trend of rising obesity rates is especially alarming among its school-going children: 11.5–41.2% of them were found to be overweight or obese depending on the age group. The highest rate was in the age group of 11–14 years [12].
With the prevalence of obesity, obesity-related complications are also on the rise in the UAE. There is a need for concerted effort to implement robust preventive measures to control and diffuse this problem. Obesity, when associated with diabetes, imposes a great economic burden, and the prevalence of this disease and its complications is increasing worldwide [13]. Obesity is also ranked second to depression in terms of its cost to employers [14].
Obesity is a chronic disease that needs life-long management. It requires coherent strategies to prevent the progression from normal weight to overweight to obesity and regaining weight after weight loss [1]. A number of international guidelines for the management of obesity are already available in public domain [15, 16, 17, 18, 19, 20]. However, local guidelines for the UAE and the region, which are structured and individualised for the management of obesity, are sorely needed to help the family physician to provide affordable treatment to the patient at the point-of-care and reduce the burden on the local healthcare system.
Objective
We set out to develop a set of recommendations for the management of patients with overweight and obesity that are relevant to the population of the UAE.
Methods
A multi-disciplinary panel of international and regional experts who treat patients with overweight and obesity was convened with the aim of developing consensus recommendations for the UAE. The panel considered a number of international guidelines on obesity as baseline references to identify the relevant recommendations. These were:
- American Association of Clinical Endocrinologists and American College of Endocrinology: Comprehensive Clinical Practice Guidelines for Medical Care of Patients with Obesity. 2016 [15];
- Academy of Nutrition and Dietetics: Interventions for the Treatment of Overweight and Obesity in Adults. 2016 [20];
- American College of Cardiology/American Heart Association/The Obesity Society (AHA/ACC/TOS): Guideline for the Management of Overweight and Obesity in Adults. 2014 [19].
Each member of the panel reviewed the references together with the research literature on obesity in the region. Based on their clinical experience, they proposed recommendations, which suited the local environment and aggregated them to form a set of practice recommendations. The panel held a second meeting to review and streamline these recommendations in its entirety for relevance, coherence and usability in the local context. The recommendations were circulated to the practicing family medicine community, namely the Emirates Medical Association and Family Medicine Society for their endorsement. The society has given their approval and support for our consensus recommendations for overweight and obesity management.
Classification and Diagnosis of Obesity
-
(1) The BMI should be used initially to confirm the presence of an excessive degree of adiposity, taking into consideration the ethnicity of the patient. Adults should be screened annually using the BMI measurement.
The BMI is a simple and widely used method for estimating body fat mass. In most populations, a cut-off point of ≥25 kg/m2 is used to initiate further evaluation of overweight or obesity [15, 21] (table 1 [15, 22]). The BMI cut-offs vary in individuals of different ethnicities [15], e.g., a BMI of ≥23 kg/m2 and ≥27.5 kg/m2 for overweight and obesity respectively should be used for screening for excess adiposity in South Asian, Southeast Asian and East Asian adults. With the highest net migration rates in the world, 88.4% of the population of the UAE were migrants, mostly from South Asia (58%), followed by other parts of Asia (17%) and the West (9%) [10].
The BMI is mostly a linear measure of the weight, which continues to grow till an individual is in his fifties, but his height remained relatively stable after his twenties [23]. Hence, clinical evaluation and judgement must be used when BMI is employed as an anthropometric indicator of excess adiposity [24]. Physicians should use the BMI alongside other indicators if the BMI and physical examination results require further evaluation. However, some indicators, e.g. bioelectric impedance, air/water displacement plethysmography or dual-energy X-ray absorptiometry, are limited, costly or not available in clinics; and their outcomes data are not validated for cut-off points [15].
(2) The waist circumference (WC) measurement is recommended as a simple and complementary measure of excess visceral fat, taking into consideration the ethnicity and sex of the patient. (table 1 [15, 22])
(3) For patients with obesity, additional assessment of co-morbidities related to obesity is recommended.
Table 1.
Recommendations for assessment of overweight and obesity
| Populations | Classification | BMI, kg/m2 | Co-morbidity risk | Waist circumference, cm |
|
|---|---|---|---|---|---|
| males < 94; | males ≥ 94; | ||||
| females < 80 | females ≥ 80 | ||||
| General population (Caucasian, Europid, Middle-Eastern, Sub-Saharan African) | underweight | <18.5 | low but with other problems | - | - |
| normal weight | 18.5–24.9 | average | - | - | |
| overweight | 25.0–29.9 | increased | increased | high | |
| obese class I | 30.0–34.9 | moderate | high | very high | |
| obese class II | 35.0–39.9 | severe | very high | very high | |
| obese class III | ≥40 | very severe | extremely high | extremely high | |
| Waist circumference, cm |
|||||
|---|---|---|---|---|---|
| males < 85; | males ≥ 85; | ||||
| females < 74 | females ≥ 74 | ||||
| East Asian, South Asian and Southeast Asian populations | normal weight | <23 | - | - | - |
| overweight | ≥23 | increased | increased | high | |
| obese | ≥27.5 | high | high | very high | |
Morbid obesity is associated with many diseases, and these affect essentially every organ system in the body (table 2[25, 26, 27, 28, 29]).
Table 2.
Practice recommendations for co-morbidities associated with obesity
| Body system | Disease/condition | Practice recommendations |
|---|---|---|
| Cardiovascular (CV) | Hypertension, atherosclerotic heart and peripheral vascular disease with myocardial infarction and cerebral vascular accidents, peripheral venous insufficiency, thrombophlebitis, pulmonary embolism | Patients with obesity are at higher risk of hypertension and cardiovascular disease. • Measure blood pressure for all patients with overweight or obesity. • Screen for active CV disease by taking careful history, physical examination and additional testing or expert referral. |
| Endocrine and reproductive | Polycystic ovarian syndrome (PCOS), increased risk of pregnancy and fetal abnormalities, male hypogonadism, cancers of the endometrium, breast, ovary, prostate and pancreas | Premenopausal women should be screened for PCOS by careful and detailed history, physical examination and laboratory testing. All men who have an increased waist circumference or obesity should be assessed for hypogonadism by history and physical examination and testing if indicated. |
| Gastrointestinal | Cholelithiasis, gastro-esophageal reflux disease (GERD), nonalcoholic fatty liver disease, hepatic cirrhosis, hepatic carcinoma, and colorectal carcinoma | Patients with obesity and a diagnosis of GERD should be examined by endoscopy if medical treatment fails to control symptoms. Obesity is associated with nonalcoholic fatty liver disease and nonalcoholic steatohepatitis [27]. Patients with overweight or obesity should be screened for fatty liver with: • Liver function testing. • Ultrasound or other imaging modality if transaminases are elevated. |
| Metabolic | Type 2 diabetes, impaired glucose tolerance, hyperlipidemia | Patients should be assessed for these co-morbidities through: • Measurements of waist circumference. • Fasting glucose, HbA1C, blood pressure and lipid panel. |
| Musculoskeletal | Back strain, disc disease, weight-bearing osteoarthritis of the hips, knees, ankles and feet | There is a strong association between obesity and osteoarthritis (OA) [26]. This should be assessed by: • Symptoms. • Physical examination for OA of the knee and other weight-bearing joints. |
| Psychological | Depression, eating disorders, body image disturbance. | Patients with overweight or obesity should be screened for depression. |
| Respiratory | Asthma, obstructive sleep apnea, obesity-hypoventilation syndrome | A strong association exists between asthma/reactive airway disease and obesity [25]. Assessment includes: • Medical history and physical examination • Spirometry and other pulmonary function tests should be considered for patients at high risk for asthma and reactive airway disease. • Polysomnography and other sleep studies, at home or in a sleep lab. |
| Urologic | Stress incontinence | Mainly seen in female patients with overweight or obesity [28]. Such patients should be screened by: • Symptomatology; or • Referral to a specialist. |
Treatment and Disease Management
-
(4) A multi-disciplinary team approach to the treatment of obesity is recommended [30].
The team members would have a number of expertise, i.e. dietitian, health educator, physical activity coach, exercise trainer, clinical psychologist, psychiatrist and physician. Effective obesity management needs the close partnership of a committed health team and the motivated patient. Obesity treatment has wider benefits for the patient beyond weight loss: it improves his/her QoL and general health and reduces the risk of obesity-related complications. Significant health benefits can be achieved even with a modest weight loss (5–10% of baseline weight), dietary modifications and increased physical activity [31].
-
(5) Obesity management should focus on body composition and not merely BMI targets.
Improving the body composition translates into better risk management, and controlling and treating co-morbidities can improve QoL and the well-being of the patient. Obesity management also reduces the need to treat co-morbidities through prescription drugs.
(6) A comprehensive lifestyle intervention, when delivered on-site with face-to-face contact on an average of one to two treatment sessions per month over a period of at least 6 months, produces greater weight loss relative to usual care [20].
Comprehensive Lifestyle Intervention
-
(7) Obesity management should address the following: self-monitoring of caloric intake and physical activity, goal setting, stimulus control, non-food rewards and relapse prevention.
The optimal management of overweight and obesity requires achieving a state of negative energy balance in the patient through a comprehensive lifestyle intervention programme, which combines three principal components: reduced-calorie diet, increased physical activity and behavioural therapy. Combining these three components in an intervention produces greater weight loss as compared to the singular use of these same components.
(8) A comprehensive lifestyle intervention through diet, exercise and behavioural modifications is recommended for individuals with BMI ≥ 25 kg/m2.
This intervention should consist of:
Diet Therapy
A review of dietary patterns showed that a diet consisting of sweets, fatty foods, meat, dairy products and canned foods is predominant in the Middle East and North African countries [32]. Where the patient is prepared to make changes to his/her daily dietary intake, a registered dietitian/nutritionist can prescribe an individualised diet, taking into consideration his/her degree of overweight/obesity, preferences and health condition.
(9) The individualised diet should be designed to induce an energy deficit of approximately 500–750 kcal/day from the current daily calorie intake. This can be achieved by prescribing 1,200–1,500 kcal/day for women and 1,500–1,800 kcal/day for men. Changes should be adapted depending on the presence of co-morbidities and ability of the patient to follow the diet.
A dietary prescription targeting either the larger nutrient (i.e. energy and macronutrient) or dietary pattern-based changes has been shown to be efficacious at producing clinically meaningful weight loss [20] (table 3[33]).
Table 3.
Diet plans for weight loss
| Diet plan | Nature of diet | Description |
|---|---|---|
| Energy-based | Low calorie diet (LCD) | A LCD is usually >800 kcal/day, and typically ranges from 1,200 to 1,600 kcal/day. For weight loss or weight maintenance, the RDN should recommend portion control, and meal replacement or structured meal plans as part of a comprehensive weight-management program. |
| Very low calorie diet (VLCD) | A VLCD provides less than or equal 800 kcal/day, a high degree of dietary structure and is commonly consumed as a liquid shake. VLCDs are considered to be appropriate only for patients with a BMI ≥30 kg/m2, and are increasingly used for patients with severe obesity prior to having bariatric surgery in order to reduce their overall surgical risks. | |
| Macronutrient-based | High protein diet | A high-protein diet is commonly defined as consuming at least 20% of the energy intake from proteins, with no standard defined amount for fats or carbohydrates. For weight loss, the high protein diet also includes an energy restriction requirement. |
| Low carbohydrate diet | A low-carbohydrate diet is commonly defined as consuming no more than 20 g of carbohydrates per day for up to 3 months and once a desired weight is achieved, carbohydrate intake can be increased to 50 g/day. Energy and other macronutrients are not restricted in low carbohydrate diets. A low-carbohydrate diet produces a greater reduction in triglycerides and a larger increase in high-density lipoprotein cholesterol than the low-fat LCD. | |
| Dietary pattern-based | Mediterranean diet | There is no standard definition for the Mediterranean diet but such diets are regarded as following traditional dietary pattern commonly found in the olive-growing areas of the Mediterranean. The traditional Mediterranean diet is focused on plant-based foods e.g. fruits, vegetables, grains, nuts and seeds, minimally processed foods and olive oil as the primary source of fat. Dairy products, fish and poultry are consumed in low to moderate amounts with a minimal amount of red meat [33]. A Mediterranean diet can be prescribed with or without an energy restriction. In addition, this diet may improve cardiovascular risk factors, such as blood pressure, blood glucose and lipids. |
Physical Activity
A medical evaluation of the physical fitness of the patient is important to ensure safety prior to a new exercise programme. It includes an assessment of current physical activity level, readiness, mobility and fitness and, if necessary, cardiac stress testing, pulmonary function test and musculoskeletal assessment. Tracking daily physical activity through an activity log, pedometer or training metrics is recommended as a tool to improve adherence to the physical activity plan. Greater time spent on sedentary behaviour (activities with very low level energy expenditure i.e. leisure, occupation, transportation and recreation) has been associated with increased risk of obesity despite having spent time performing moderate to vigorous physical activity [34]. Sedentary behaviour indirectly influences eating habits, and increased sedentary behaviour is reported to be one of the causes of the obesity epidemic in the UAE [35]. Conversely, an increase in physical activity may help reduce the calorie intake. Hence, a re-allocation of time spent on sedentary behaviour, particularly leisure screen time, such as watching television, computer and tablet use, to light physical activity can increase overall energy expenditure.
(10) Moderate-intensity activity for at least 150 min/week (or 30 min/day for most days of the week) is recommended. For weight maintenance, 200–300 min or more of physical activity per week is recommended, again, depending on its intensity, unless medically contraindicated.
Behavioural Therapy
-
(11) When addressing obesity issues in patients, it is important to have a thorough psychological assessment to identify factors that may hinder goals for weight loss.
Many patients have undergone such an assessment without any issues being highlighted; and they have achieved their weight loss goals with minimal, if any, psychological intervention. However, for others, such intervention may be needed as psychological factors may pose an actual risk to the weight loss plan.
The most common psychiatric disorders that may co-exist with obesity are: dysthymic disorder, major depressive disorder, generalized anxiety disorder and binge eating disorder [36, 37, 38]. Patients with a history of such disorders experience poor weight loss due to the nature of their psychiatric illness [39]. They are also susceptible to internalized weight bias and body shame [40, 41]. Women who are obese tend to report higher body image dissatisfaction than those with a healthy weight, which exacerbates the depressive symptoms and decreases self-esteem [42, 43]. Body shame can also affect the sexual function of these individuals even though the cause of the sexual dysfunction may be due to other issues such as depression [38]. Personality factors also contribute to mood symptoms and dysfunctional eating behaviours [44]. For example, neurotic personality traits are related to heightened concerns about body figure and contribute to inadequate coping habits. This results in binge eating driven by stress, and may increase depression and anxiety.
Patients with obesity often have psychiatric co-morbidities, e.g. substance-related disorders, physical abuse and suicidal ideations [45, 46, 47]. Substance-related disorders such as alcohol abuse pose a particular risk as they exacerbate the lack of coping skills [48] and control. It may impair judgement and result in a suicide attempt. A history of sexual abuse also affects weight loss [37] as patients use dysfunctional eating habits as a way of coping with the associated emotional distress. In addition, the extra body fat could act as a protective mechanism against further sexual abuse. Childhood experience of parental loss is also another factor that has been associated with metabolic syndrome [49].
-
(12) The use of psychological intervention, such as Cognitive Behaviour Therapy (CBT), can help to resolve many psychosocial issues related to obesity and motivate the patient to implement the necessary behavioural and dietary changes for weight loss.
The National Institute for Clinical Excellence has recommended CBT as the treatment of choice to reduce psychological symptoms that pose a risk to weight loss regimens [50]. CBT is also used to treat eating disorder symptoms in high-risk situations, such as in pre- and post-bariatric surgery. Table 4[51] shows some interventions derived from a CBT modality that may benefit individuals suffering from obesity with or without severe psychological symptoms. This is by no means an exhaustive list of what the treatment entails.
Psychologists using CBT for psychosocial issues have to tailor their treatment plans to include cultural aspects to ensure positive outcomes. The cultural norms underpinning CBT needs to be tailored to accommodate Middle Eastern cultural norms of eating, observing and acknowledging religious holidays during the treatment process [52]. In addition, methods of challenging cognitive distortions need to be culturally appropriate so as to not come off as offensive.
Table 4.
Interventions using Cognitive Behavior Therapy to treat patients with obesity
| Intervention | Lifestyle modification |
|---|---|
| Education | • Dysfunctional eating behaviour and associated cognition and emotions • Instructed to eat slowly • Best way to purchase food • Perform mastication exercises |
| Self-monitoring | • Keeping daily record of the food consumed • Keeping daily records of the physical exercise |
| Stimulus control | • Meal planning • Carry appropriate food in portable containers • Restrict places where eating is allowed • Not skipping meals |
| Stimulus control Positive reinforcement | • Setting small achievable goals • Rewarding behaviours with non-food related incentives when target is reached |
Pharmacotherapy
-
(13) Pharmacotherapy for the treatment of obesity may be considered in patients with a BMI ≥ 30 kg/m2 with no co-morbidities or BMI ≥ 27 kg/m2 with co-morbidities and used in addition to lifestyle intervention [53].
Weight loss medication should be prescribed in the long term as for treatment of any chronic condition as an adjunct to lifestyle modification. There is little evidence to demonstrate the health benefits of short-term treatment with pharmacotherapy [54]. However, if <5% weight loss is achieved after 12 weeks, medication should be withdrawn. For certain ethnicities, a lower BMI can be considered for pharmacotherapy. The available anti-obesity drugs are orlistat (Xenical®, Alli®) and liraglutide (3 mg, Saxenda®) (table 5).
Orlistat. Orlistat is a lipase inhibitor which inhibits the breakdown of triglycerides in the gut into free fatty acids and monoglycerides, thus reducing their absorption into the blood stream [53]. Clinical trials of this drug have shown a 4.0% weight loss at 1 year over placebo and 2.6% weight loss at 4 years as well as a reduced progression from impaired glucose tolerance to type 2 diabetes mellitus (T2DM) by 45% over 4 years [55].
Liraglutide. Liraglutide is an acylated human glucagon-like peptide-1 (GLP-1) analogue which stimulates insulin secretion [56]. It lowers body weight through loss of fat mass, with greater reductions in visceral fat compared to subcutaneous fat. It increases feelings of fullness and satiety, while lowering feelings of hunger and prospective food consumption, thereby reducing food intake.
The efficacy and safety of liraglutide in reducing weight has been evaluated in four randomized, double-blinded, placebo-controlled trials: SCALE 1 [57], SCALE 2 [58], SCALE 3 [59] and SCALE-Maintenance [60]. In SCALE-Obesity and pre-diabetes and SCALE-Diabetes, 67.5% and 50.4% respectively achieved ≥5% weight loss after 12 weeks (early responders). With continued treatment, 86.2% were expected to achieve a weight loss of ≥5% and 51%, ≥10% weight loss after 1 year of treatment. In SCALE-Sleep Apnoea, the improvement in apnoea/hypo-apnoea index in patients with obstructive sleep apnoea was greater for patients with liraglutide compared to placebo. In SCALE-Maintenance, more patients (81.4% vs. 48.9%) maintained their weight loss (prior to treatment) with liraglutide than with placebo [60]. Liraglutide also significantly improved glycaemic parameters across various sub-populations: normal-glycaemia, pre-diabetes and T2DM.
(14) The choice of weight loss medication should take into account contra-indications and safety profile, associated co-morbidities, efficacy, cost and availability. We have listed specific consideration for patients with certain co-morbidities and special circumstances (table 6 [61, 62, 63, 64, 65, 66, 67, 68]).
Table 5.
Anti-obesity drugs for weight loss
| Medication | Dosing | Side-effects and contraindications |
|---|---|---|
| Orlistat (Xenical®, Alli®-OTC) | • 120 mg TDS taken orally before meals (Xenical); or • 60 mg TDS (Alli) over the counter • Vitamin A, D, E and K, should to be taken 2 h after orlistat. |
• Mostly gastrointestinal e.g. steatorrhoea, faecal incontinence and urgency, oily/fatty stools, flatulence and abdominal pain, and headaches. Exacerbated by diets containing >30% in fat content. • Contraindicated in pregnancy and breastfeeding, cholestasis, oxalate nephrolithiasis and chronic mal-absorption syndrome. May cause mal-absorption of fat-soluble vitamins, cholelithiasis and rare severe liver injury. • Use caution when taken concurrently with warfarin (enhances effect), anti-epileptics and cyclosporine (decreases effect), levothyroxine (decreases effect and should be taken 4 h from orlistat). |
| Liraglutide (3 mg, Saxenda®, Novo Nordisk) | • Escalated on weekly basis: 0.6 mg/day, 1.2 mg/day, 1.8 mg/day, 2.4 mg/day and finally 3 mg/day | • Mostly nausea, vomiting, diarrhoea, constipation, hypoglycaemia, insomnia, dizziness, dysgeusia, dry mouth, dyspepsia, gastritis, gastro-oesophageal reflux, abdominal pain, abdominal distension, cholelithiasis, asthenia, fatigue, increased lipase and amylase |
Table 6.
Modifications to obesity management plan for patients with co-morbidities
| Co-morbidity | Recommended modifications |
||||||
|---|---|---|---|---|---|---|---|
| Cardiovascular disease (CV) and cardiac arrhythmia | The AACE 2016 guidelines [15] recommended that liraglutide be used with caution. If weight loss goals are met, continue with careful monitoring of heart rate/rhythm and blood pressure. We suggest considering liraglutide as first-line treatment based on the positive CV outcomes in patients with T2DM [68]. The AACE guidelines [15] also suggested using orlistat as first line for such patients. | ||||||
| Chronic kidney disease | In patients treated with GLP-1 receptor agonists including liraglutide, there have been instances of acute renal failure and worsening of chronic renal failure, which sometimes require haemodialysis. Some events were reported in patients without known underlying renal disease [61, 62]. Use liraglutide with caution in patients with or at very high risk of chronic kidney disease; and discontinued if patients develop volume depletion, e.g. due to nausea, vomiting or diarrhoea [63]. Weight-loss medication should not be used in end-stage renal failure, with the exception of orlistat. Orlistat and liraglutide can be used with appropriate caution in patients with mild (eGFR 50–79 ml/min) and moderate (eGFR 30–49 ml/min) renal impairment (see below). | ||||||
| Weight loss medication | eGFR >50ml/min | eGFR 30–49ml/min | eGFR <30ml/min | ||||
| Orlistat | ✓ | ✓ | ✓ | ||||
| Liraglutide | ✓ | ✓ | Use with caution | ||||
| ✓ Safe to use | |||||||
| Depression and anxiety | Patients started on weight loss medication should be monitored for symptoms of depression and suicidal ideation. Orlistat and liraglutide may be considered in patients with obesity and depression | ||||||
| Hypertension | For patients with existing hypertension, preferred medications are orlistat and liraglutide. | ||||||
| Hepatic impairment | Use weight loss medication with caution in patients with hepatic impairment and avoided in severe hepatic impairment (i.e. Child-Pugh score > 9). Patients losing weight are at risk of cholelithiasis [64, 65] and in cases with elevated liver enzymes, clinicians should always consider gallstones. | ||||||
| Weight loss medication | Mild | Moderate | Child-Pugh score > 9 | ||||
| Orlistat | ✓ | Use with caution | Contra-indicated | ||||
| Liraglutide | ✓ | Use with caution | Contra-indicated | ||||
| ✓ Safe to use | |||||||
| Nephrolithiasis | The first choice for patients with history of nephrolithiasis is liraglutide. Other medications should be used with caution. | ||||||
| Pancreatitis | Orlistat and liraglutide should not be prescribed in cases where there is a history of pancreatitis or current pancreatitis [66, 67]. | ||||||
| Seizure disorder | Liraglutide and orlistat are preferred for patients with a history or at risk of seizure/epilepsy. | ||||||
The use of pharmacotherapy for weight loss should also take into account:
- Pregnancy: Pharmacotherapy must not be used in pregnancy, and in breastfeeding women. Women of childbearing age, who are on pharmacotherapy, should be advised to use contraception.
- Post-bariatric surgery: Patient who have re-gained excess weight (>25% of weight loss), have not responded to intensive diet or exercise and cannot be considered for revisional surgery, may be considered for treatment with liraglutide post-surgery.
Bariatric Surgery
-
(15) Bariatric surgery should be considered for patients with a BMI ≥ 40 kg/m2 and no co-morbidities; or ≥ 35 kg/m2 with one or more co-morbidities and for whom the procedure would not be associated with excessive risk [69].
Patients with a BMI of 30–34.9 kg/m2 with T2DM can be considered for bariatric surgery, although the evidence is limited [70]. For certain ethnicities, e.g. patients of Asian origin, lower BMI cut-off criteria can be considered [71]. Patients should undergo a pre-operative assessment of obesity-related complications, and the choice of bariatric surgery should be discussed with the surgeon, including the advantages and disadvantages of each procedure. Patients should be followed-up life-long for nutritional surveillance.
-
(16) Assessments for psychological stability should be undertaken for patients undergoing bariatric surgery.
Assessing psychological stability of the patient to identify aspects that needed to be addressed and resolved in order for the surgery to be successful would also aid weight loss success post-surgery. For example, the American Society for Metabolic and Bariatric Surgery have made available an excellent psychological assessment template which takes into account the reasons for seeking surgery, expectation and understanding of surgery options, history of weight management, eating behaviour and diet history, risk-taking behaviour, physical activity, coping skills, cognitive functioning and psychopathology [72]. If issues are uncovered, they can be addressed and resolved through psychotherapy.
Long-Term Maintenance of Weight Loss
-
(17) Patients should maintain their weight loss and be encouraged to keep in contact with a nutritionist to ensure that their dietary plan remains suitable to their evolving needs.
Patients typically regain 35–40% of their lost weight in the year following the weight loss programme [73]. Maintaining long-term weight loss takes a different approach than losing the weight. Besides having information on nutritional needs, healthy and balanced nutrition and menu preparation, it is important to maintain a consistent eating pattern and, if a setback occurs with the diet (e.g. during vacation or on holidays), to get back on track as soon as possible.
-
(18) Physical activity is essential to achieving long-term weight loss, and as a rule patients should perform moderate intensity physical activity for at least 200–300 min/week and weigh themselves regularly (daily) [30].
Patients should have a plan of action especially when they see themselves regaining weight. They are encouraged to meet regularly with physical health advisers so that they can sustain their personalized fitness regimes.
-
(19) Patients should be trained in relaxation methods and meditation with positive thoughts to address emotional fluctuations rather than give in to compulsive eating behaviours.
For emotional eaters, counselling to help patients learn new ways to handle their emotions: e.g. rather than turning to food, instead go for an activity that they enjoy or connect with a friend. Stress confrontation is used to identify and recognise emotional triggers that may contribute to compulsive eating behaviours.
The use of weight loss medication is encouraged to promote long-term weight maintenance, ameliorate co-morbidities and increase adherence to behavioural changes. This can improve the physical function and allow for greater physical activity [15].
Conclusion
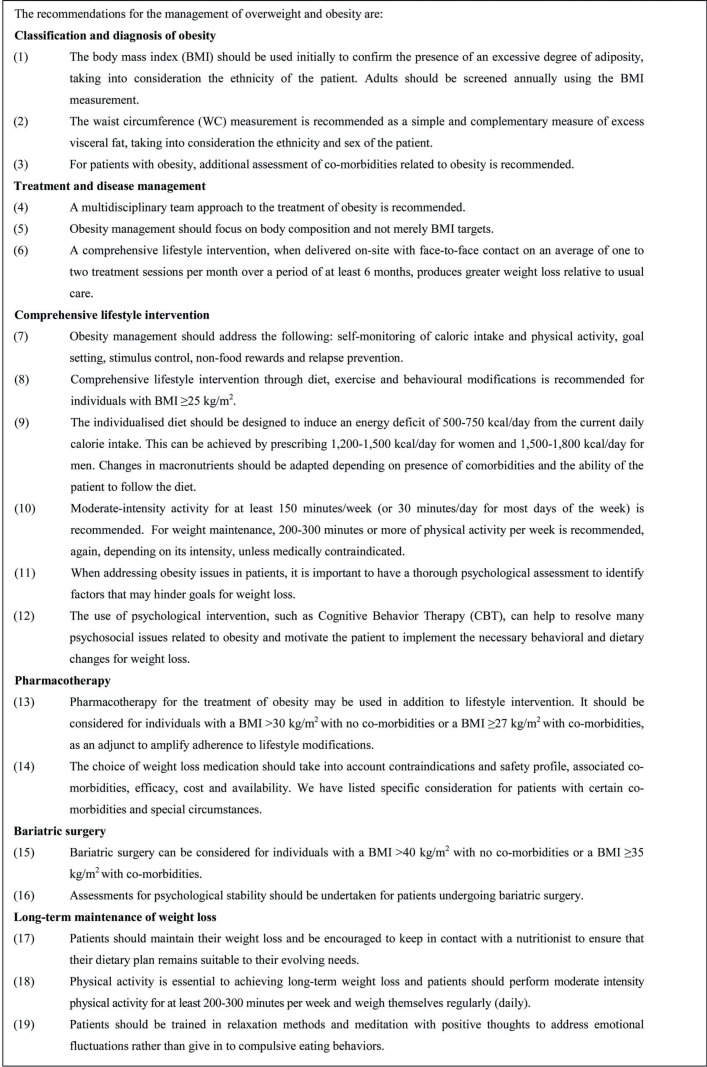
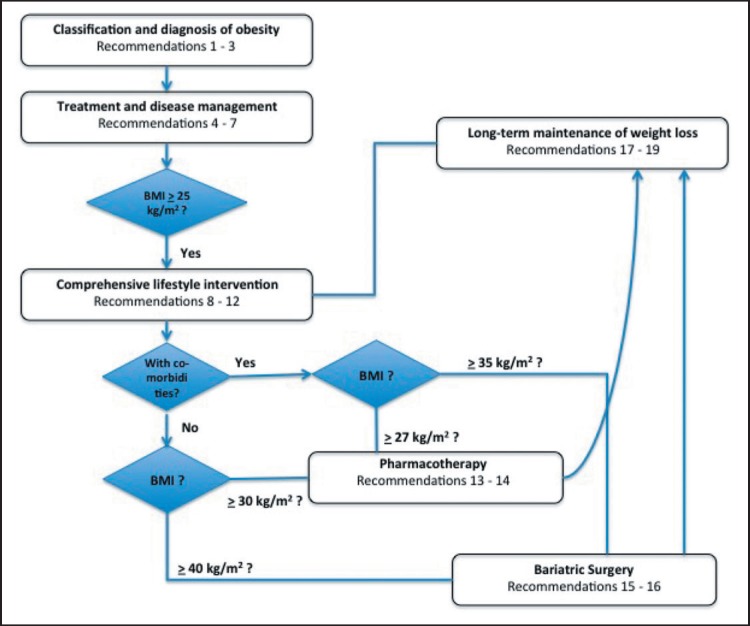
These consensus recommendations for managing overweight and obesity are developed in response to the high prevalence of obesity and lack of local clinical recommendations in the UAE. A summary of these recommendations is provided (fig. 1), and the accompanying algorithm is shown in figure 2. Overweight and obesity are chronic conditions that require comprehensive lifestyle modification [73], augmented by pharmacotherapy and/or surgery [60]. Besides reducing weight in subjects who are obese, it is also important to maintain the weight loss achieved. A multi-disciplinary approach is required to implement these strategies, control the associated co-morbidities and long-term patient follow-up to ensure success.
Fig. 1.
Summary of recommendations.
Fig. 2.
Algorithm for the management of overweight and obesity. For description of recommendations, please refer to figure 1 as numbered.
Author Contributions
All authors were involved in conceptualising the study design, drafting their respective sections, proposing the recommendations and revising it critically for important intellectual content, and all authors approved the final version submitted for publication. Drs. Fargaly and Abusnana co-chaired the panel meetings.
Disclosure Statement
Drs. Kaddaha, McGowan and Nawar are on the advisory board of Novo Nordisk.
Acknowledgements
We would like to thank the Emirates Medical Association and Family Medicine Society for reviewing and endorsing the recommendations in our manuscript. Their support and endorsement will greatly facilitate the implementation of these recommendations in clinical practice. Novo Nordisk provided support for the panel meetings. Technical editorial and manuscript drafting assistance was provided by Sen-Kwan Tay of Tech Observer Asia-Pacific Pte Ltd and supported by Novo Nordisk.
References
- 1.Nammi S, Koka S, Chinnala KM, Boini KM. Obesity: an overview on its current perspectives and treatment options. Nutr J. 2004;3:3. doi: 10.1186/1475-2891-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organisation Obesity and Overweight. 2018 www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (last accessed October 1, 2018) [Google Scholar]
- 3.Abdelaal M, le Roux CW, Docherty NG. Morbidity and mortality associated with obesity. Ann Transl Med. 2017;5:161. doi: 10.21037/atm.2017.03.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumanyika S, Jeffery RW, Morabia A, Ritenbaugh C, Antipatis VJ, Public Health Approaches to the Prevention of Obesity Working Group of the International Obesity Task F Obesity prevention: THE case for action. Int J Obes Relat Metab Disord. 2002;26:425–436. doi: 10.1038/sj.ijo.0801938. [DOI] [PubMed] [Google Scholar]
- 5.Badran M, Laher I. Obesity in Arabic-speaking countries. J Obes. 2011;2011:686430. doi: 10.1155/2011/686430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Nohair S. Obesity in gulf countries. Int J Health Sci (Qassim) 2014;8:79–83. doi: 10.12816/0006074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vats MG, Mahboub BH, Al Hariri H, Al Zaabi A, Vats D. Obesity and sleep-related breathing disorders in middle east and UAE. Can Respir J. 2016;2016:9673054. doi: 10.1155/2016/9673054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kilpi F, Webber L, Musaigner A, Aitsi-Selmi A, Marsh T, Rtveladze K, McPherson K, Brown M. Alarming predictions for obesity and non-communicable diseases in the middle east. Public Health Nutr. 2014;17:1078–1086. doi: 10.1017/S1368980013000840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balkau B, Deanfield JE, Despres JP, Bassand JP, Fox KA, Smith SC, Jr, Barter P, Tan CE, Van Gaal L, Wittchen HU, Massien C, Haffner SM. International day for the evaluation of abdominal obesity (idea): a study of waist circumference, cardiovascular disease, and diabetes mellitus in 168,000 primary care patients in 63 countries. Circulation. 2007;116:1942–1951. doi: 10.1161/CIRCULATIONAHA.106.676379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.UNdata a World of Information United Arab Emirates. 2015 http://data.un.org/en/iso/ae.html (last accessed October 1, 2018) [Google Scholar]
- 11.Ng SW, Zaghloul S, Ali H, Harrison G, Yeatts K, El Sadig M, Popkin BM. Nutrition transition in the United Arab Emirates. Eur J Clin Nutr. 2011;65:1328–1337. doi: 10.1038/ejcn.2011.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.AlBlooshi A, Shaban S, AlTunaiji M, Fares N, AlShehhi L, AlShehhi H, AlMazrouei A, Souid AK. Increasing obesity rates in school children in United Arab Emirates. Obesi Sci Pract. 2016;2:196–202. doi: 10.1002/osp4.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seidell JC. Obesity, insulin resistance and diabetes-a worldwide epidemic. Br J Nutr. 2000;83((suppl 1)):S5–8. doi: 10.1017/s000711450000088x. [DOI] [PubMed] [Google Scholar]
- 14.Loeppke R, Taitel M, Haufle V, Parry T, Kessler RC, Jinnett K. Health and productivity as a business strategy: a multiemployer study. JOccup Environ Med. 2009;51:411–428. doi: 10.1097/JOM.0b013e3181a39180. [DOI] [PubMed] [Google Scholar]
- 15.Garvey WT, Mechanick JI, Brett EM, Garber AJ, Hurley DL, Jastreboff AM, Nadolsky K, Pessah-Pollack R, Plodkowski R, Reviewers of the AACE/ACE Obesity Clinical Practice Guidelines American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016;22((suppl 3)):1–203. doi: 10.4158/EP161365.GL. [DOI] [PubMed] [Google Scholar]
- 16.Yumuk V, Tsigos C, Fried M, Schindler K, Busetto L, Micic D, Toplak H, Obesity Management Task Force of the European Association for the Study of Obesity European guidelines for obesity management in adults. Obes Facts. 2015;8:402–424. doi: 10.1159/000442721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stegenga H, Haines A, Jones K, Wilding J, Guideline Development Group Identification, assessment, and management of overweight and obesity: summary of updated NICE guidance. BMJ. 2014;349:g6608. doi: 10.1136/bmj.g6608. [DOI] [PubMed] [Google Scholar]
- 18.National Institute for Health and Care Excellence Obesity: Identification, Assessment and Management. London, National Institute for Health and Care Excellence. 2014 https://www.nice.org.uk/guidance/cg189 (last accessed October 1, 2018) [Google Scholar]
- 19.Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, Hu FB, Hubbard VS, Jakicic JM, Kushner RF, Loria CM, Millen BE, Nonas CA, Pi-Sunyer FX, Stevens J, Stevens VJ, Wadden TA, Wolfe BM, Yanovski SZ. American College of Cardiology/American Heart Association Task Force on Practice Guidelines Obesity Society: 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63:2985–3023. doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 20.Raynor HA, Champagne CM. Position of the Academy of Nutrition and Dietetics: interventions for the treatment of overweight and obesity in adults. J Acad Nutr Diet. 2016;116:129–147. doi: 10.1016/j.jand.2015.10.031. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization Obesity: Preventing and managing the global epidemic. Report of a WHO consultation. WHO Tech Rep Ser. 2000;894:i–xii. 1–253. [PubMed] [Google Scholar]
- 22.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC., Jr Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 23.Keys A, Fidanza F, Karvonen MJ, Kimura N, Taylor HL. Indices of relative weight and obesity. Int J Epidemiol. 2014;43:655–665. doi: 10.1093/ije/dyu058. [DOI] [PubMed] [Google Scholar]
- 24.Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris T, Heymsfield SB. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol. 1996;143:228–239. doi: 10.1093/oxfordjournals.aje.a008733. [DOI] [PubMed] [Google Scholar]
- 25.Poulain M, Doucet M, Major GC, Drapeau V, Series F, Boulet LP, Tremblay A, Maltais F. The effect of obesity on chronic respiratory diseases: Pathophysiology and therapeutic strategies. CMAJ. 2006;174:1293–1299. doi: 10.1503/cmaj.051299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duclos M. Osteoarthritis, obesity and type 2 diabetes: the weight of waist circumference. Ann Phys Rehab Med. 2016;59:157–160. doi: 10.1016/j.rehab.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 27.Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R, Natale S, Vanni E, Villanova N, Melchionda N, Rizzetto M. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37:917–923. doi: 10.1053/jhep.2003.50161. [DOI] [PubMed] [Google Scholar]
- 28.Subak LL, Richter HE, Hunskaar S. Obesity and urinary incontinence: epidemiology and clinical research update. J Urol. 2009;182((6 suppl)):S2–7. doi: 10.1016/j.juro.2009.08.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Buchwald H, Consensus Conference Panel Bariatric surgery for morbid obesity: HEALTH implications for patients, health professionals, and third-party payers. J Am Coll Surg. 2005;200:593–604. doi: 10.1016/j.jamcollsurg.2004.10.039. [DOI] [PubMed] [Google Scholar]
- 30.Montesi L, El Ghoch M, Brodosi L, Calugi S, Marchesini G, Dalle Grave R. Long-term weight loss maintenance for obesity: a multidisciplinary approach. Diabetes Metab Syndr Obes. 2016;9:37–46. doi: 10.2147/DMSO.S89836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Clinical guidelines on the identification and treatment of overweight and obesity in adults-the evidence report National institutes of health. Obe Res. 1998;6((suppl 2)):51s–209s. [PubMed] [Google Scholar]
- 32.Aljefree N, Ahmed F. Association between dietary pattern and risk of cardiovascular disease among adults in the Middle East and North Africa region: a systematic review. Food Nutr Res. 2015;59:27486. doi: 10.3402/fnr.v59.27486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davis C, Bryan J, Hodgson J, Murphy K. Definition of the Mediterranean diet; a literature review. Nutrients. 2015;7:9139–9153. doi: 10.3390/nu7115459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Owen N, Sugiyama T, Eakin EE, Gardiner PA, Tremblay MS, Sallis JF. Adults' sedentary behavior determinants and interventions. Am J Prev Med. 2011;41:189–196. doi: 10.1016/j.amepre.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 35.Yammine K. The prevalence of physical activity among the young population of UAE: a meta-analysis. Perspect Public Health. 2017;137:275–280. doi: 10.1177/1757913916675388. [DOI] [PubMed] [Google Scholar]
- 36.Abiles V, Rodriguez-Ruiz S, Abiles J, Obispo A, Gandara N, Luna V, Fernandez-Santaella MC. Effectiveness of cognitive-behavioral therapy in morbidity obese candidates for bariatric surgery with and without binge eating disorder. Nutr Hosp. 2013;28:1523–1529. doi: 10.3305/nh.2013.28.5.6699. [DOI] [PubMed] [Google Scholar]
- 37.Yen YC, Huang CK, Tai CM. Psychiatric aspects of bariatric surgery. Curr Opin Psychiatry. 2014;27:374–379. doi: 10.1097/YCO.0000000000000085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sarwer DB, Lavery M, Spitzer JC. A review of the relationships between extreme obesity, quality of life, and sexual function. Obes Surg. 2012;22:668–676. doi: 10.1007/s11695-012-0588-1. [DOI] [PubMed] [Google Scholar]
- 39.Malik S, Mitchell JE, Engel S, Crosby R, Wonderlich S. Psychopathology in bariatric surgery candidates: a review of studies using structured diagnostic interviews. Compr Psychiatry. 2014;55:248–259. doi: 10.1016/j.comppsych.2013.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burmeister JM, Hinman N, Koball A, Hoffmann DA, Carels RA. Food addiction in adults seeking weight loss treatment. Implications for psychosocial health and weight loss. Appetite. 2013;60:103–110. doi: 10.1016/j.appet.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 41.Carels RA, Burmeister JM, Koball AM, Oehlhof MW, Hinman N, LeRoy M, Bannon E, Ashrafioun L, Storfer-Isser A, Darby LA, Gumble A. A randomized trial comparing two approaches to weight loss: differences in weight loss maintenance. J Health Psychol. 2014;19:296–311. doi: 10.1177/1359105312470156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Matz PE, Foster GD, Faith MS, Wadden TA. Correlates of body image dissatisfaction among overweight women seeking weight loss. J Consult Clin Psychol. 2002;70:1040–1044. [PubMed] [Google Scholar]
- 43.Schwartz MB, Brownell KD. Obesity and body image. Body Image. 2004;1:43–56. doi: 10.1016/S1740-1445(03)00007-X. [DOI] [PubMed] [Google Scholar]
- 44.Claes L, Vandereycken W, Vandeputte A, Braet C. Personality subtypes in female pre-bariatric obese patients: do they differ in eating disorder symptoms, psychological complaints and coping behaviour? Eur Eat Disord Rev. 2013;21:72–77. doi: 10.1002/erv.2188. [DOI] [PubMed] [Google Scholar]
- 45.Gabert DL, Majumdar SR, Sharma AM, Rueda-Clausen CF, Klarenbach SW, Birch DW, Karmali S, McCargar L, Fassbender K, Padwal RS. Prevalence and predictors of self-reported sexual abuse in severely obese patients in a population-based bariatric program. J Obes. 2013;2013:374050. doi: 10.1155/2013/374050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mahony D. Assessing sexual abuse/attack histories with bariatric surgery patients. J Child Sex Abuse. 2010;19:469–484. doi: 10.1080/10538712.2010.496713. [DOI] [PubMed] [Google Scholar]
- 47.Windover AK, Merrell J, Ashton K, Heinberg LJ. Prevalence and psychosocial correlates of self-reported past suicide attempts among bariatric surgery candidates. Surg Obes Relat Dis. 2010;6:702–706. doi: 10.1016/j.soard.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 48.Heinberg LJ, Ashton K, Coughlin J. Alcohol and bariatric surgery: review and suggested recommendations for assessment and management. Surg Obes Relat Dis. 2012;8:357–363. doi: 10.1016/j.soard.2012.01.016. [DOI] [PubMed] [Google Scholar]
- 49.Alciati A, Gesuele F, Casazza G, Foschi D. The relationship between childhood parental loss and metabolic syndrome in obese subjects. Stress Health. 2013;29:5–13. doi: 10.1002/smi.1435. [DOI] [PubMed] [Google Scholar]
- 50.National Institute for Health and Care Excellence (NICE) Computerised cognitive behaviour therapy for depression and anxiety. London, National Institute for Health and Care Excellence. 2006 [Google Scholar]
- 51.Gade H, Hjelmesaeth J, Rosenvinge JH, Friborg O. Effectiveness of a cognitive behavioral therapy for dysfunctional eating among patients admitted for bariatric surgery: a randomized controlled trial. J Obes. 2014;2014:127936. doi: 10.1155/2014/127936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Abudabbeh N, Hays PA, Chapter 6. Cognitive-Behavior Therapy with people of Arab heritage . Culturally Responsive Cognitive-Behavioral Therapy: Assessment, Practice, and Supervision. In: Hays PA, Iwamasa GY, editors. Washington, DC, American Psychological Association. 2006. [Google Scholar]
- 53.Manning S, Pucci A, Finer N. Pharmacotherapy for obesity: novel agents and paradigms. Ther Adv Chronic Dis. 2014;5:135–148. doi: 10.1177/2040622314522848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yanovski SZ, Yanovski JA. Long-term drug treatment for obesity: a systematic and clinical review. JAMA. 2014;311:74–86. doi: 10.1001/jama.2013.281361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Torgerson JS, Hauptman J, Boldrin MN, Sjostrom L. XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care. 2004;27:155–161. doi: 10.2337/diacare.27.1.155. [DOI] [PubMed] [Google Scholar]
- 56.Mehta A, Marso SP, Neeland IJ. Liraglutide for weight management: a critical review of the evidence. Obes Sci Pract. 2017;3:3–14. doi: 10.1002/osp4.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pi-Sunyer X, Astrup A, Fujioka K, Greenway F, Halpern A, Krempf M, Lau DC, le Roux CW, Violante Ortiz R, Jensen CB, Wilding JP, SCALE Obesity and Prediabetes NN8022-1839 Study Group A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N Engl J Med. 2015;373:11–22. doi: 10.1056/NEJMoa1411892. [DOI] [PubMed] [Google Scholar]
- 58.Davies MJ, Bergenstal R, Bode B, Kushner RF, Lewin A, Skjoth TV, Andreasen AH, Jensen CB, DeFronzo RA. Efficacy of liraglutide for weight loss among patients with type 2 diabetes: the SCALE Diabetes randomized clinical trial. JAMA. 2015;314:687–699. doi: 10.1001/jama.2015.9676. [DOI] [PubMed] [Google Scholar]
- 59.Blackman A, Foster GD, Zammit G, Rosenberg R, Aronne L, Wadden T, Claudius B, Jensen CB, Mignot E. Effect of liraglutide 3.0 mg in individuals with obesity and moderate or severe obstructive sleep apnea: the SCALE Sleep Apnea randomized clinical trial. Int J Obes. 2016;40:1310–1319. doi: 10.1038/ijo.2016.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wadden TA, Hollander P, Klein S, Niswender K, Woo V, Hale PM, Aronne L. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet-induced weight loss: the SCALE Maintenance randomized study. Int J Obes. 2015;39:187. doi: 10.1038/ijo.2014.88. [DOI] [PubMed] [Google Scholar]
- 61.Davies M, Chatterjee S, Khunti K. The treatment of type 2 diabetes in the presence of renal impairment: what we should know about newer therapies. Clin Pharmacol. 2016;8:61–81. doi: 10.2147/CPAA.S82008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Thrasher J. Pharmacologic management of type 2 diabetes mellitus: AVAILABLE therapies. Am J Cardiol. 2017;120((1 suppl)):S4–s16. doi: 10.1016/j.amjcard.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 63.US Food and Drug Administration Drugs@FDA: FDA Approved Drug Products. Saxenda, U.S. Department of Health and Human Services. 2017 www.accessdata.fda.gov/scripts/cder/daf/ (last accessed October 1, 2018) [Google Scholar]
- 64.Weinsier RL, Ullmann DO. Gallstone formation and weight loss. Obes Res. 1993;1:51–56. doi: 10.1002/j.1550-8528.1993.tb00008.x. [DOI] [PubMed] [Google Scholar]
- 65.Festi D, Colecchia A, Larocca A, Villanova N, Mazzella G, Petroni ML, Romano F, Roda E. Review: Low caloric intake and gall-bladder motor function. Aliment Pharmacol Ther. 2000;14((suppl 2)):51–53. doi: 10.1046/j.1365-2036.2000.014s2051.x. [DOI] [PubMed] [Google Scholar]
- 66.Franks AS, Lee PH, George CM. Pancreatitis: a potential complication of liraglutide? Ann Pharmacother. 2012;46:1547–1553. doi: 10.1345/aph.1Q789. [DOI] [PubMed] [Google Scholar]
- 67.Kose M, Emet S, Akpinar TS, Ilhan M, Gok AF, Dadashov M, Tukek T. An unexpected result of obesity treatment: orlistat-related acute pancreatitis. Case Rep Gastroenterol. 2015;9:152–155. doi: 10.1159/000430433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, Nissen SE, Pocock S, Poulter NR, Ravn LS, Steinberg WM, Stockner M, Zinman B, Bergenstal RM, Buse JB. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375:311–322. doi: 10.1056/NEJMoa1603827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wolfe BM, Kvach E, Eckel RH. Treatment of obesity: weight loss and bariatric surgery. Circ Res. 2016;118:1844–1855. doi: 10.1161/CIRCRESAHA.116.307591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Baskota A, Li S, Dhakal N, Liu G, Tian H. Bariatric surgery for type 2 diabetes mellitus in patients with BMI <30 kg/m2: a systematic review and meta-analysis. PloS One. 2015;10:e0132335. doi: 10.1371/journal.pone.0132335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lee WJ, Aung L. Metabolic surgery for type 2 diabetes mellitus: Experience from Asia. Diabetes Metab J. 2016;40:433–443. doi: 10.4093/dmj.2016.40.6.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sogg S, Lauretti J, West-Smith L. Recommendations for the presurgical psychosocial evaluation of bariatric surgery patients. Surg Obesity Relat Dis. 2016;12:731–749. doi: 10.1016/j.soard.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 73.Wadden TA, Webb VL, Moran CH, Bailer BA. Lifestyle modification for obesity: new developments in diet, physical activity, and behavior therapy. Circulation. 2012;125:1157–1170. doi: 10.1161/CIRCULATIONAHA.111.039453. [DOI] [PMC free article] [PubMed] [Google Scholar]