Abstract
Background
This is an update of the original Cochrane review first published in Issue 1, 2003, and previously updated in 2009, 2012 and 2014. Chronic pain, defined as pain that recurs or persists for more than three months, is common in childhood. Chronic pain can affect nearly every aspect of daily life and is associated with disability, anxiety, and depressive symptoms.
Objectives
The aim of this review was to update the published evidence on the efficacy of psychological treatments for chronic and recurrent pain in children and adolescents.
The primary objective of this updated review was to determine any effect of psychological therapy on the clinical outcomes of pain intensity and disability for chronic and recurrent pain in children and adolescents compared with active treatment, waiting‐list, or treatment‐as‐usual care.
The secondary objective was to examine the impact of psychological therapies on children's depressive symptoms and anxiety symptoms, and determine adverse events.
Search methods
Searches were undertaken of CENTRAL, MEDLINE, MEDLINE in Process, Embase, and PsycINFO databases. We searched for further RCTs in the references of all identified studies, meta‐analyses, and reviews, and trial registry databases. The most recent search was conducted in May 2018.
Selection criteria
RCTs with at least 10 participants in each arm post‐treatment comparing psychological therapies with active treatment, treatment‐as‐usual, or waiting‐list control for children or adolescents with recurrent or chronic pain were eligible for inclusion. We excluded trials conducted remotely via the Internet.
Data collection and analysis
We analysed included studies and we assessed quality of outcomes. We combined all treatments into one class named 'psychological treatments'. We separated the trials by the number of participants that were included in each arm; trials with > 20 participants per arm versus trials with < 20 participants per arm. We split pain conditions into headache and mixed chronic pain conditions. We assessed the impact of both conditions on four outcomes: pain, disability, depression, and anxiety. We extracted data at two time points; post‐treatment (immediately or the earliest data available following end of treatment) and at follow‐up (between three and 12 months post‐treatment).
Main results
We identified 10 new studies (an additional 869 participants) in the updated search. The review thus included a total of 47 studies, with 2884 children and adolescents completing treatment (mean age 12.65 years, SD 2.21 years). Twenty‐three studies addressed treatments for headache (including migraine); 10 for abdominal pain; two studies treated participants with either a primary diagnosis of abdominal pain or irritable bowel syndrome, two studies treated adolescents with fibromyalgia, two studies included adolescents with temporomandibular disorders, three were for the treatment of pain associated with sickle cell disease, and two studies treated adolescents with inflammatory bowel disease. Finally, three studies included adolescents with mixed pain conditions. Overall, we judged the included studies to be at unclear or high risk of bias.
Children with headache pain
We found that psychological therapies reduced pain frequency post‐treatment for children and adolescents with headaches (risk ratio (RR) 2.35, 95% confidence interval (CI) 1.67 to 3.30, P < 0.01, number needed to treat for an additional beneficial outcome (NNTB) = 2.86), but these effects were not maintained at follow‐up. We did not find a beneficial effect of psychological therapies on reducing disability in young people post‐treatment (SMD ‐0.26, 95% CI ‐0.56 to 0.03), but we did find a beneficial effect in a small number of studies at follow‐up (SMD ‐0.34, 95% CI ‐0.54 to ‐0.15). We found no beneficial effect of psychological interventions on depression or anxiety symptoms.
Children with mixed pain conditions
We found that psychological therapies reduced pain intensity post‐treatment for children and adolescents with mixed pain conditions (SMD ‐0.43, 95% CI ‐0.67 to ‐0.19, P < 0.01), but these effects were not maintained at follow‐up. We did find beneficial effects of psychological therapies on reducing disability for young people with mixed pain conditions post‐treatment (SMD ‐0.34, 95% CI ‐0.54 to ‐0.15) and at follow‐up (SMD ‐0.27, 95% CI ‐0.49 to ‐0.06). We found no beneficial effect of psychological interventions on depression symptoms. In contrast, we found a beneficial effect on anxiety at post‐treatment in children with mixed pain conditions (SMD ‐0.16, 95% CI ‐0.29 to ‐0.03), but this was not maintained at follow‐up.
Across all pain conditions, we found that adverse events were reported in seven trials, of which two studies reported adverse events that were study‐related.
Quality of evidence
We found the quality of evidence for all outcomes to be low or very low, mostly downgraded for unexplained heterogeneity, limitations in study design, imprecise and sparse data, or suspicion of publication bias. This means our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect, or we have very little confidence in the effect estimate; or the true effect is likely to be substantially different from the estimate of effect.
Authors' conclusions
Psychological treatments delivered predominantly face‐to‐face might be effective for reducing pain outcomes for children and adolescents with headache or other chronic pain conditions post‐treatment. However, there were no effects at follow‐up. Psychological therapies were also beneficial for reducing disability in children with mixed chronic pain conditions at post‐treatment and follow‐up, and for children with headache at follow‐up. We found no beneficial effect of therapies for improving depression or anxiety. The conclusions of this update replicate and add to those of a previous version of the review which found that psychological therapies were effective in reducing pain frequency/intensity for children with headache and mixed chronic pain conditions post‐treatment.
Plain language summary
Psychological therapies for the management of chronic and recurrent pain in children and adolescents
Bottom line
Psychological therapies reduce pain frequency immediately following treatment for children and adolescents with chronic headache and reduce pain intensity for children and adolescents with mixed chronic pain conditions. Psychological therapies also reduce disability for children and adolescents with mixed chronic pain conditions immediately following treatment and up to 12 months later, and for children with headache conditions up to 12 months later.
Background
Chronic pain or pain that lasts for longer than three months is common in young people. Psychological therapies (e.g. relaxation, hypnosis, coping skills training, biofeedback, and cognitive behavioural therapy) may help people manage pain and its disabling consequences. Therapies can be delivered face‐to‐face by a therapist, via the Internet, by telephone call, or by computer programme. This review focused on treatments that are delivered face‐to‐face by a therapist, which includes therapies delivered by telephone or via a book with exercise instructions. For children and adolescents, there is evidence that relaxation by itself and cognitive behavioural therapy (treatment that helps people test and revise their thoughts and actions) are effective in reducing the intensity of pain in chronic headache, recurrent abdominal pain, fibromyalgia, and sickle cell disease immediately after treatment.
Study Characteristics
This review included 47 studies with 2884 participants. The average age of the children and adolescents was 12.6 years. Most studies included young people with headache (23 studies) or stomach pain (10 studies), The remaining studies investigated children with irritable bowel syndrome, fibromyalgia, temporomandibular disorders, sickle cell disease, inflammatory bowel disease, or included samples with various chronic pain conditions.
Key results
Psychological therapies reduced pain frequency immediately following treatment for children and adolescents with chronic headache, and pain intensity and anxiety for children and adolescents with other chronic pain conditions. Psychological therapies also reduced disability for children and adolescents with non‐headache chronic pain conditions immediately following treatment and for children with headache and mixed chronic pain conditions up to 12 months later. We did not find any benefit of psychological treatments on reducing anxiety for children with headache or for depression in children with headache or mixed chronic pain conditions.
Quality of evidence
We judged all outcomes to be low or very low‐quality, meaning our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect or we have very little confidence in the effect estimate; or the true effect is likely to be substantially different from the estimate of effect.
Summary of findings
Summary of findings 1. Summary of findings.
| Psychological therapies compared with any control for children and adolescents with frequent headaches | ||||||
|
Patient or population: Children and adolescents with chronic pain Settings: Community and hospitals Intervention: Psychological therapies (cognitive behavioural therapy or behavioural therapy) Comparison: Any control (active, treatment‐as‐usual, wait‐list) | ||||||
| Outcomes | Probable outcome with control | Probable outcome with intervention | NNTB and/or relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments |
|
Pain: 50% reduction in headache frequency Post‐treatment Lower scores = fewer headaches |
10 per 1000 | 24 per 1000 |
NNTB = 2.86; RR 2.35 (1.67 to 3.30) |
644 participants (15 studies) | ⊕⊝⊝⊝ very lowb,c,h | |
|
Pain: 50% reduction in headache frequency Follow‐up (up to 12 months) Lower scores = fewer headaches |
10 per 1000 | 27 per 1000 |
NNTB = 3.16; RR 2.73 (0.98 to 7.63) |
223 participants (5 studies) |
⊕⊝⊝⊝ very lowb,c,e,f,g,h | |
|
Disability Post‐treatment Lower scores = lower reported disability |
The mean disability in the intervention groups was 0.26 lower (95% CI ‐0.56 to 0.03) | 446 participants (6 studies) |
⊕⊝⊝⊝ very lowd,f,g | |||
|
Disability Follow‐up Lower scores = lower reported disability |
The mean disability in the intervention groups was 0.37 lower (95% CI ‐0.65 to ‐0.10) | 209 participants (3 studies) |
⊕⊝⊝⊝ very lowf,g | |||
|
Anxiety Post‐treatment Lower scores = lower reported anxiety |
The mean anxiety in the intervention groups was 0.11 lower (95% CI ‐0.39 to 0.17) | 439 participants (7 studies) |
⊕⊝⊝⊝ very low a,d,f,h,i | |||
|
Anxiety Follow‐up Lower scores = lower reported anxiety |
The mean anxiety in the intervention groups was 0.12 lower (95% CI ‐0.46 to 0.21) | 271 participants (4 studies) |
⊕⊝⊝⊝ very lowa,f,g | |||
|
Depression Post‐treatment Lower scores = lower reported depression |
The mean depression in the intervention groups was 0.08 lower (95% CI ‐0.28 to 0.11) | 400 participants (6 studies) |
⊕⊝⊝⊝ very lowa,f,g | |||
| CI: Confidence interval; RR: Risk Ratio; NNTB; Number needed to treat to benefit. | ||||||
| GRADE Working Group grades of evidence High‐quality: we are very confident that the true effect lies close to that of the estimate of the effect; Moderate‐quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different; Low‐quality: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect; Very low‐quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
a50 to 75% risk of bias ratings were unclear/high.
b> 75% of risk of bias ratings were unclear or high.
cConfidence intervals were wide.
dHeterogeneity (I2) was 46 to 65%.
eHeterogeneity (I2) was 66 to 100%.
f75 to 100% of studies eligible to be included in the analysis were not included in the analysis.
gSmall number of participants contributing to the outcome.
hAsymmetrical funnel plots suggesting publication bias.
iThere was mostly unclear/high risk of bias in the selective reporting category.
Summary of findings 2. Summary of findings.
| Psychological therapies compared with any control for children and adolescents with chronic pain conditions (mixed) | |||||
|
Patient or population: Children and adolescents with chronic pain Settings: Community and hospitals Intervention: Psychological therapies (cognitive behavioural therapy or behavioural therapy) Comparison: Any control (active, treatment‐as‐usual, wait‐list) | |||||
| Outcomes | Probable outcome with control | Probable outcome with intervention | No of Participants (studies) | Quality of the evidence (GRADE) | Comments |
|
Pain Post‐treatment Lower scores = lower reported pain intensity |
The mean pain intensity in the intervention group was 0.43 lower (95% CI ‐0.67 to ‐0.19) | 1210 participants (16 studies) |
⊕⊝⊝⊝ very lowd,f | ||
|
Pain Follow‐up Lower scores = lower reported pain intensity |
The mean pain intensity in the intervention group was 0.08 lower (95% CI ‐0.30 to 0.13) | 763 participants (9 studies) |
⊕⊝⊝⊝ very lowb,c,e,f | ||
|
Disability Post‐treatment Lower scores = lower reported disability |
The mean disability in the intervention group was 0.34 lower (95% CI ‐0.54 to ‐0.15) | 1226 participants (14 studies) |
⊕⊕⊝⊝ lowc,f | ||
|
Disability Follow‐up Lower scores = lower reported disability |
The mean disability in the intervention group was 0.27 lower (95% CI ‐0.49 to ‐0.06) | 866 participants (9 studies) |
⊕⊕⊝⊝ lowc,e | ||
|
Anxiety Post‐treatment Lower scores = lower reported anxiety |
The mean anxiety in the intervention group was 0.16 lower (95% CI ‐0.29 to ‐0.03) | 883 participants (8 studies) |
⊕⊕⊝⊝ lowf | ||
|
Anxiety Follow‐up Lower scores = lower reported anxiety |
The mean anxiety in the intervention group was 0.01 lower (95% CI ‐0.20 to 0.18) | 805 participants (8 studies) |
⊕⊕⊝⊝ lowb,f | ||
|
Depression Post‐treatment Lower scores = lower reported depression |
The mean disability in the intervention group was 0.05 lower (95% CI ‐0.23 to 0.12) | 757 participants (8 studies) |
⊕⊝⊝⊝ verylowb,e,f | ||
| CI: Confidence interval. | |||||
| GRADE Working Group grades of evidence High‐quality: we are very confident that the true effect lies close to that of the estimate of the effect; Moderate‐quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different; Low‐quality: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect; Very low‐quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | |||||
a50 to 75% risk of bias ratings were unclear/high.
bConfidence intervals were wide.
cHeterogeneity (I2) was 46 to 65%.
dHeterogeneity (I2) was 66 to 100%.
e50 to 75% of studies eligible to be included in the analysis were not included in the analysis.
fAsymmetrical funnel plots suggesting publication bias.
Background
Description of the condition
This review is an update of a previously published review in the Cochrane Library on 'Psychological therapies for the management of chronic and recurrent pain in children and adolescents' (Eccleston 2003; Eccleston 2009; Eccleston 2012; Eccleston 2014). Chronic (pain lasting more than three months) and recurrent pain is a common problem in young people. Recent epidemiology suggests a prevalence of 15% to 30%, with 8% of children described as having severe and frequent pain (King 2011; Perquin 2000; Perquin 2001; Stanford 2008). The most common pain locations are the head, abdomen, and limbs (King 2011). Girls more commonly report all types of chronic and recurrent pain, and there is a peak in incidence at ages 14 to 15 years (Stanford 2008). Young people report pain to be distressing and interfering, and in some cases this can be severely debilitating, affecting all aspects of a child's life, and the lives of the parents and family members (Palermo 2005; Palermo 2014). The deleterious effects of chronic pain in childhood can also extend to adulthood (Horst 2014; Walker 2012).
Description of the intervention
Psychological treatments for children and adolescents with chronic pain conditions are specifically designed to alter psychological processes thought to underlie, or significantly contribute to, pain, distress, and disability. The design of psychological treatments is informed by specific theories of the causes of human behaviour, or has developed pragmatically through observation and study of response to intervention. Behavioural and cognitive treatments designed to ameliorate pain, distress, and disability were first introduced in adults over 40 years ago (Fordyce 1968; Keefe 2004), and were used to inform the development of psychological treatments for children and adolescents with chronic pain. In paediatric practice, the treatments have different therapeutic aims and components than those for adults. In general, psychological treatments for children and adolescents aim to control pain and modify situational, emotional, familial, and behavioural factors that play a role in the onset and maintenance of pain (Palermo 2012).
Treatments were originally delivered in a face‐to‐face format in which the patients and therapists worked together in person to implement therapeutic strategies. Methods of remote delivery of psychological treatments for children with chronic pain conditions have also been developed; these are the subject of a separate Cochrane review 'Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents' (Fisher 2015). A companion review of psychological treatments for the management of chronic pain in adults is also published (Williams 2012). Pharmacological interventions are also delivered to children and adolescents with chronic pain and a recent suite of Cochrane reviews have investigated the efficacy of opioids, paracetamol, antidepressants, anti‐epiletic drugs, and NSAIDs, but there is little evidence in young people (Cooper 2017a; Cooper 2017b; Cooper 2017c; Cooper 2017d; Eccleston 2017).
How the intervention might work
A variety of intervention strategies have been designed to reduce pain, increase comfort, and reduce associated disability and dysfunction in children with pain conditions. Behavioural strategies include relaxation training, biofeedback, and behavioural management programmes (e.g. teaching parents strategies to reinforce adaptive behaviours such as school attendance). Cognitive strategies include hypnosis, stress management, guided imagery, and cognitive coping skills (Palermo 2012). Cognitive‐behavioural therapy programmes incorporate elements of both behavioural and cognitive strategies. Parent interventions may include operant strategies, communication strategies, or problem‐solving skills (PST). PST is aimed at decreasing distress in parents of children with chronic pain by teaching problem‐solving skills, including steps to define a problem, generate possible solutions, implement a solution, and then evaluate (D'Zurilla 1999; D'Zurilla 2007). The efficacy of parent therapies are investigated in a sister review (Eccleston 2015) which is currently being updated.
Given that headache and abdominal pain are the most common types of recurrent pain in children, most of the treatment literature has focused on these two populations. By far the most commonly described treatment is relaxation training or biofeedback, or both, for headache (Law 2017), and recommendations have been made to offer psychological treatment as a matter of routine care for children with headaches (Ernst 2015; Palermo 2014). Older trials investigated efficacy of treatment predominantly for children with headache, comparing different elements of relaxation training and biofeedback and with different treatment doses, and treatment setting (clinic, school, and home; Griffiths 1996; Larsson 1987a). More recently, the quality of trials has improved to include larger sample sizes, multiple recruitment sites, and active control comparator conditions (e.g. Kashikar‐Zuck 2012; Levy 2016; Levy 2017; Palermo 2016; Powers 2013). Indeed, psychological therapies have now been developed and evaluated for children with a variety of chronic pain conditions including abdominal pain (Levy 2017), musculoskeletal pain (Kashikar‐Zuck 2012) and disease‐related pain (Barakat 2010; Levy 2016).
In clinical practice, psychological therapies for children with chronic pain are often delivered as one component of a multidisciplinary treatment programme (Palermo 2012). Such programmes aim to restore function and ameliorate pain through physical rehabilitation, psychological pain management strategies, and medical strategies (Palermo 2012). This treatment is typically offered in specialised outpatient clinics or more intensive day treatment or inpatient rehabilitation programs housed within tertiary medical centres (Hechler 2015).
Why it is important to do this review
Several reviews have documented the effectiveness of psychological therapies for children with headache, abdominal, and disease‐related pain (Fisher 2015; Huertas‐Ceballos 2008; Kibby 1998; Ng 2017; Walco 1999). Reviews have used data pooling techniques for studies of children with headache (Eccleston 2014; Fisher 2015; Ng 2017). In the previously published Cochrane review (Eccleston 2014), we found that psychological treatments were effective in reducing pain intensity in youth with headache and mixed chronic pain conditions. Fisher 2015 and Ng 2017 reported similar findings for children and adolescents with headache. Since the protocol of this review, there has been growing awareness of the limitations of smaller trials. Small studies are now a significant problem in pain research (Moore 2013) and are typically pilot studies or older trials. Therefore, in this update we have presented subgroup analyses to investigate smaller versus larger trials.
Objectives
The aim of this review was to update the published evidence on the efficacy of psychological treatments for chronic and recurrent pain in children and adolescents.
The primary objective of this updated review was to determine any effect of psychological therapy on the clinical outcomes of pain intensity and disability for chronic and recurrent pain in children and adolescents compared with active treatment, waiting‐list, or treatment‐as‐usual care.
The secondary objective was to examine the impact of psychological therapies on children's depressive symptoms and anxiety symptoms, and determine adverse events.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) comparing a credible psychological treatment, or a compound treatment with credible primary psychological content, to an active treatment, treatment‐as‐usual, or waiting‐list control. We judged content as credible if it was based on an extant psychological theory or framework. We excluded studies if the pain was associated with life‐limiting conditions (e.g. cancer) or if the therapy was delivered remotely using methods such as telephone or Internet.
We included studies if they:
were available as a full report of a RCT;
had a design that placed a psychological treatment as an active treatment of primary interest;
had a psychological treatment with definable psychotherapeutic content (although not necessarily delivered by someone with psychological qualifications);
were published (or electronically pre‐published) in a peer‐reviewed scientific journal;
had participants who reported chronic pain (i.e. pain that recurs or persists for at least three months duration);
had 10 or more participants in each treatment arm at the end‐of‐treatment assessment; and
included a psychological intervention that was delivered in person (face‐to‐face treatment), via telephone and at home via a written instruction booklet. We excluded studies delivered via technology (e.g. Internet, smartphone).
Types of participants
Children and adolescents (< 18 years) reporting chronic or recurrent pain in any body site, not associated with cancer. We separated conditions into headache conditions or mixed pain conditions. Mixed pain conditions (previously referred to as 'non‐headache conditions') refer to other types of chronic pain (e.g. recurrent abdominal pain, musculoskeletal pain, disease‐related pain).
Types of interventions
We included studies if at least one trial arm consisted of a psychological intervention (not delivered via technology), and a comparator arm consisted of active treatment, treatment‐as‐usual, or waiting‐list control. We excluded primary interventions that were delivered remotely via other methods (e.g. Internet, telephone).
Types of outcome measures
We assessed and recorded data from all measurement instruments reported in each study. We extracted data from the most appropriate measurement instruments for the outcomes below. We decided on the most appropriate measurement instruments as measures that were psychometrically established and frequently used across the studies.
Primary outcomes
Pain intensity
Pain‐related disability
Secondary outcomes
Depression
Anxiety
Adverse events
Search methods for identification of studies
Electronic searches
For this update, searching the following databases identified RCTs of any psychological therapy for paediatric chronic or recurrent pain:
CENTRAL (CRSO): searched 22/1/14 to 1/5/18
MEDLINE and MEDLINE in Process (OVID): searched January 2017 to 1/5/18
Embase (OVID): searched January 2014 to 2018 week 18
PsycINFO (OVID): searched January 2014 to May week 1 2018
Searching other resources
We searched clinicaltrials.gov for possible ongoing or completed trials in this area on 1 May 2018. We also examined reference lists and citation searches of included studies and relevant systematic reviews for other potential RCTs.
Data collection and analysis
Selection of studies
For this update, two authors sifted abstracts (EF, JD), and a third author (TP) arbitrated any disagreements. We selected studies for inclusion based on the following criteria: the study had to be a RCT in design and published in a peer‐reviewed journal, included children (< 18 years of age) who had chronic or recurrent pain (non‐cancer pain), included a psychological intervention as an active treatment, and had >10 participants in each arm at each extraction time point. Studies that had not been peer‐reviewed were excluded in order to keep the quality of included studies high. Consistent with our last update (Eccleston 2014), remotely‐delivered interventions were excluded from this review. We considered psychological interventions for inclusion if they had credible, recognisable psychological/psychotherapeutic content and were specifically designed to change the child's behaviour, cognition, or social‐environmental contingencies. All trials included in our previous systematic review and meta‐analysis were considered automatically eligible for inclusion (Eccleston 2014).
Data extraction and management
Data extracted included: details relating to the design of the study, the participants, primary diagnosis, characteristics of treatment (e.g. treatment setting, treatment delivered, and length of treatment), adverse events, outcome measurement tools used, and outcome data for computation of effect sizes. We contacted trial authors via email to obtain data necessary for effect size calculations if data were missing for primary outcomes of interest. We entered data suitable for pooling into RevMan 5.3 (RevMan 2014).
Assessment of risk of bias in included studies
We measured risk of bias using the recommended Cochrane 'Risk of bias' tool (Higgins 2011). We assessed five categories from this tool: random sequence generation (selection bias), allocation concealment (selection bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), and selective reporting (reporting bias). We excluded 'Blinding of participant or personnel' (performance bias) for the purposes of this review as we deemed it redundant because of the nature of delivering or receiving a psychological intervention. We made judgements on the 'risk of bias' categories using the following rules.
Selection bias (random sequence generation and allocation concealment)
We based judgements of random sequence generation on whether authors used a convincing method of randomisation. We judged studies that provided an adequate method of randomisation as at low risk of bias. We judged studies that did not provide a convincing method of randomisation as at unclear risk of bias. Studies that did not randomise participants were excluded from this review.
We based judgements of allocation concealment on whether there were convincing methods used for random allocation to take place. We did not deem studies as biased if participants were stratified by age or gender. We judged studies that provided a convincing method of allocation concealment (e.g. opaque envelopes) as at low risk of bias. We judged studies that did not report allocation concealment as at unclear risk of bias.
Detection bias (blinding of outcome assessment)
We based judgements of blinding of outcome assessment on whether the measures were taken by a third party who was blind to the treatment condition. We judged studies that reported an outcome assessor blinded to treatment as having a low risk of bias. We judged studies where a description was not provided, as at unclear risk of bias.
Attrition bias (incomplete outcome data)
We based judgements of incomplete outcome data on whether attrition was fully reported. Authors had to report attrition at each measurement time point (post‐treatment and follow‐up), and state whether there were any significant differences between completers and non‐completers. We judged studies as having low risk of bias if studies reported attrition and no differences between completers and non‐completers. We judged studies to be at unclear risk of bias if they reported attrition but did not report if there were differences between completers and non‐completers. Finally, we judged studies to be at high risk of bias if they did not report attrition.
Reporting bias (selecting reporting bias)
Finally, we based judgements of selective reporting bias on whether data could be fully extracted for analyses in this review. We judged studies that reported all outcomes in the manuscript as having low risk of bias. We marked this category as 'unclear bias' if authors provided data when requested. We allocated high risk of bias to studies that did not report all outcomes.
Measures of treatment effect
We combined all treatments labelled as psychological in the following meta‐analyses, and designated these as 'Treatment'. Similarly, we combined all control conditions and designated these as 'Control'. We combined the intervention or control arms if more than one intervention or control group was reported to create a single pairwise comparison in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). The studies were divided into two groups based on pain condition. We labelled the first group 'headache' and the second group 'mixed chronic pain conditions'. We also selected two assessment points: post‐treatment and follow‐up. Post‐treatment was the assessment point occurring soonest following treatment (often after a delay of several weeks to allow for recording of episodic pain), and follow‐up was the assessment point at least three months after the post‐treatment assessment point, but not more than 12 months. We selected the longer time point if there were two or more follow‐up assessments within this time frame. Therefore, we designed four separate comparisons comprising two forms of comparator (Treatment, Control) and two assessment time points (post‐treatment and follow‐up). They were labelled as follows.
Treatment versus control (headache) post‐treatment.
Treatment versus control (headache) follow‐up.
Treatment versus control (mixed chronic pain) post‐treatment.
Treatment versus control (mixed chronic pain) follow‐up.
For each comparison, we identified five outcomes labelled 'Pain', 'Disability', 'Depression', 'Anxiety', and 'Adverse events'. From each trial we selected the measure considered most appropriate for each outcome. We applied two rules to guide the choice of outcome measure. First, if an outcome measure was established and occurred frequently among studies it was selected over more novel instruments. Second, given a choice between single item and multi‐item self‐report tools, multi‐item tools were chosen on the basis of inferred increased reliability. Studies did not necessarily report data on all five outcomes. For headache treatments, we preferentially extracted the proportion of participants achieving a clinically significant (50%) reduction in headache frequency as the outcome for pain. We extracted the proportion of participants achieving a 50% reduction in pain intensity when headache frequency was not reported. Thus, for pain outcomes for headache treatments, we used relative ratios or risk ratios (RR) and we calculated numbers needed to treat for an additional beneficial outcome (NNTBs). All other extracted outcomes were continuous. Due to different populations and measures used, we analysed data using random effect models and standardised mean differences. We calculated effect sizes for the continuous outcomes which could be interpreted as follows; small = 0.2, medium = 0.5, large = 0.8 (Cohen 1992).
Due to the number of analyses in this review, we checked for model overfitting using Aikaike Information Criteria (AIC) comparing meta‐analysis and the additive combination of risk of bias and sample size in random‐effects meta‐regressions without an interaction term.
Unit of analysis issues
Randomisation occurred at the individual level. When studies included both children with headache and children with mixed pain conditions, we included the data in both analyses.
Dealing with missing data
We contacted study authors if there were missing data in the peer reviewed manuscript needed for data analysis.
Assessment of heterogeneity
We followed the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) to interpret heterogeneity in our meta‐analyses. We interpreted heterogeneity in analyses as follows: 0 to 40% as not important, 30 to 60% as moderate, 50 to 90% as substantial, and 75 to 100% as considerable heterogeneity.
Assessment of reporting biases
We checked for publication bias by using contour‐enhanced funnel plots, tests of funnel plot asymmetry, and meta‐regressions including total sample size as a moderator.
Quality of Evidence
Two review authors (EF, JD) rated the quality of the outcomes. We used the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) system to rank the quality of the evidence using the RevMan 'Summary of Findings' table, and the guidelines provided in Chapter 12.2 of the CochraneHandbook for Systematic Reviews of Interventions (Higgins 2011).
The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) to assess the quality of the body of evidence for each outcome. The GRADE system uses the following criteria for assigning grades of evidence:
High: we are very confident that the true effect lies close to that of the estimate of the effect;
Moderate: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different;
Low: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect;
Very low: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect.
The GRADE system uses the following criteria for assigning a quality level to a body of evidence (Chapter 12, Higgins 2011).
High: randomised trials; or double‐upgraded observational studies;
Moderate: downgraded randomised trials; or upgraded observational studies;
Low: double‐downgraded randomised trials; or observational studies;
Very low: triple‐downgraded randomised trials; or downgraded observational studies; or case series/case reports.
Factors that may decrease the quality level of a body of evidence are:
limitations in the design and implementation of available studies suggesting high likelihood of bias;
indirectness of evidence (indirect population, intervention, control, outcomes);
unexplained heterogeneity or inconsistency of results (including problems with subgroup analyses);
imprecision of results (wide confidence intervals);
high probability of publication bias.
Factors that may increase the quality level of a body of evidence are:
large magnitude of effect;
all plausible confounding would reduce a demonstrated effect or suggest a spurious effect when results show no effect;
dose‐response gradient.
We decreased the grade rating by one (‐ 1) or two (‐ 2) if we identified:
Serious (‐ 1) or very serious (‐ 2) limitations to study quality;
Important inconsistency (‐ 1);
Some (‐ 1) or major (‐ 2) uncertainty about directness;
Imprecise or sparse data (‐ 1);
High probability of reporting bias (‐ 1).
There are sometimes reasons to downgrade an outcome directly to 'very low‐quality', as recommended by GRADE guidelines (Guyatt 2013). Where relevant, we describe all our reasons for making this judgement.
'Summary of findings' table
We included two 'Summary of findings' tables to present the main findings in a transparent and simple tabular format. In particular, we included key information concerning the quality of evidence, the magnitude of effect of the interventions examined, and the sum of available data on the outcomes, pain intensity, and disability post‐treatment and at follow‐up. We also included anxiety and depression post‐treatment, and anxiety at follow‐up.
Subgroup analysis and investigation of heterogeneity
In this update, we included two sets of subgroup analyses for each analysis, where data were available. We chose 20 participants as a cutoff to be consistent with other reviews (e.g. Eccleston 2015 (currently being updated); Williams 2012) which have raised their minimum n from 10 to 20 participants per arm. As a group of authors, we still feel it is premature to raise the minimum n to 20 participants per arm and therefore, in this update, we conducted the following subgroup analyses:
trials including fewer than 20 participants in each arm (n < 20);
trials including more than 20 participants in each arm (n > 20).
Sensitivity analysis
For this update, we conducted sensitivity analyses on analyses that included more than 10 studies. We removed studies where we judged high or unclear risk of reporting biases to determine whether higher quality studies reported similar effects.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies.
Results of the search
Five separate searches were undertaken using databases from inception to May 2018. Details of the previous four searches can be found in Appendix 1. In the most recent search, we searched databases from January 2014 to May 2018 (see Figure 1). The current search yielded 3021 abstracts (2110 abstracts after duplication) and we included nine trials (Chen 2014; Daniel 2015; Greenley 2015; Hickman 2015; Levy 2016; Levy 2017; Palermo 2016; Wahlund 2003; Wahlund 2015). Due to the revised inclusion criteria to include trials delivered via the telephone, we also included one trial (Cottrell 2007) from Fisher 2015. Therefore, we included 10 new studies (n = 869 at post‐treatment), a total of 47 RCTs (49 papers) (Abram 2007; Alfven 2007; Barakat 2010; Barry 1997; Bussone 1998; Chen 2014; Cottrell 2007; Daniel 2015; Duarte 2006; Fichtel 2001; Gil 1997; Greenley 2015; Griffiths 1996; Grob 2013; Gulewitsch 2013; Hechler 2014; Hickman 2015; Humphreys 2000; Kashikar‐Zuck 2005; Kashikar‐Zuck 2012; Kroener‐Herwig 2002; Labbe 1984; Labbe 1995; Larsson 1987a; Larsson 1987b; Larsson 1990; Larsson 1996; Levy 2010; Levy 2016; Levy 2017; McGrath 1988; McGrath 1992; Osterhaus 1997; Palermo 2016; Passchier 1990; Powers 2013; Richter 1986; Robins 2005; Sanders 1994; Sartory 1998; Scharff 2002; Van der Veek 2013; Van Tilburg 2009; Vlieger 2007; Wahlund 2003; Wahlund 2015; Wicksell 2009).
1.
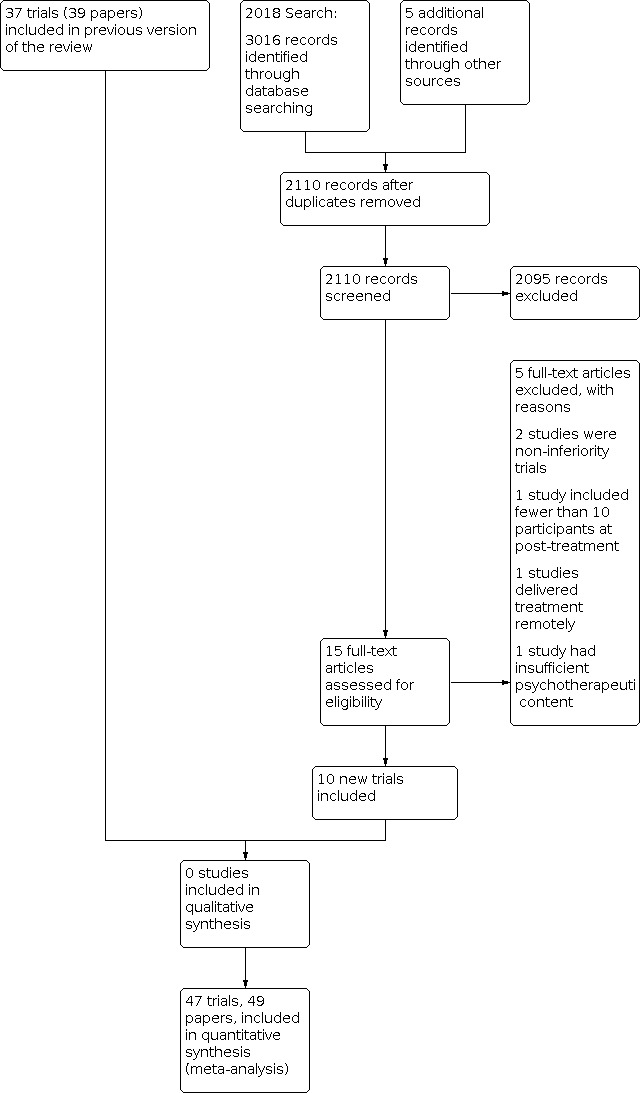
Study flow diagram.
Included studies
The total number of participants completing treatments from the 47 studies was 2884. Of the 47 studies, one had four treatment arms, 12 had three arms, and 30 had two arms. Twenty‐five studies included fewer than 20 participants per arm. We included these in separate subgroup analyses in this update (Barakat 2010; Barry 1997; Bussone 1998; Cottrell 2007; Duarte 2006; Fichtel 2001; Griffiths 1996; Grob 2013; Gulewitsch 2013; Hickman 2015; Humphreys 2000; Kashikar‐Zuck 2005; Kroener‐Herwig 2002; Labbe 1984; Labbe 1995; Larsson 1987a; Larsson 1987b; Larsson 1990; Larsson 1996; Osterhaus 1997; Richter 1986; Sartory 1998; Scharff 2002; Van Tilburg 2009; Wicksell 2009). Two studies delivered treatment to parents only (Levy 2017; Palermo 2016). Incidentally, both studies included more than 20 participants per arm. Across all studies, the mean number of participants per study at the end of treatment was 68 (standard deviation (SD) = 45.04). For studies including fewer and more than 20 participants per arm, the mean number of participants per study at the end of treatment was 36 (SD = 8.17) for studies including less than 20 participants per arm, and 91 (SD = 48.61) for studies including more than 20 participants per arm. Girls outnumbered boys in most studies (mean 66% girls). Child age was reported in 44 studies (Mean 12.65 years, SD 2.21 years).
Young people were recruited from a range of healthcare settings and other sources. Thirty trials recruited from hospital or clinic settings and 12 recruited participants from a mixture of of advertisements, schools, community, or hospital settings. Five trials did not report their recruitment source.
There were 23 trials of treatments for children with headache (including migraine). Of the remainder, 10 were for abdominal pain (Alfven 2007; Duarte 2006; Grob 2013; Humphreys 2000; Levy 2010; Levy 2017; Robins 2005; Sanders 1994; Van der Veek 2013; Van Tilburg 2009) and two studies treated participants with either a primary diagnosis of abdominal pain or irritable bowel syndrome (Gulewitsch 2013; Vlieger 2007). Two studies treated children with fibromyalgia (Kashikar‐Zuck 2005; Kashikar‐Zuck 2012), two studies included children with temporomandibular disorders (Wahlund 2003; Wahlund 2015), three were for the treatment of pain associated with sickle cell disease (Barakat 2010; Daniel 2015; Gil 1997), and two studies treated children and adolescents with inflammatory bowel disease (Greenley 2015; Levy 2016). Finally, three studies included mixed pain conditions including headache and mixed chronic pain conditions (Hechler 2014; Palermo 2016; Wicksell 2009) For these three studies, we included data in both analyses, as appropriate.
We classified treatment arms on the basis of their content and of the label given by the study authors. We classified interventions into four broad groups. The first is best described as behavioural, typically relaxation‐based, with or without biofeedback, and including autogenic or hypnotherapeutic content (Bussone 1998; Chen 2014; Fichtel 2001; Labbe 1984; Labbe 1995; Larsson 1987a; Larsson 1987b; Larsson 1990; Larsson 1996; McGrath 1988; McGrath 1992; Passchier 1990; Wahlund 2003; Wahlund 2015; Van Tilburg 2009; Vlieger 2007). The second is best described as cognitive behavioural therapy, including coping skills training (Abram 2007; Alfven 2007; Barakat 2010; Barry 1997; Duarte 2006; Gil 1997; Griffiths 1996; Grob 2013; Gulewitsch 2013; Hickman 2015; Humphreys 2000; Kashikar‐Zuck 2005; Kashikar‐Zuck 2012; Kroener‐Herwig 2002; Levy 2010; Levy 2017; McGrath 1992; Osterhaus 1997; Powers 2013; Richter 1986; Robins 2005; Sanders 1994; Sartory 1998; Scharff 2002; Van der Veek 2013; Wicksell 2009). Problem‐solving therapy was the third category, which involved problem‐solving strategies delivered to the family (Daniel 2015). We also included interventions delivered exclusively to parents, which is new to this update. Parent interventions included cognitive‐behavioural therapy (Levy 2016) and problem‐solving therapy (Palermo 2016), with a primary aim to improve parenting behaviour or parent mental health, or both, and a secondary aim to improve children's pain, disability, and/or emotional functioning. One trial (Hechler 2014) evaluated the efficacy of a three‐week intensive inpatient pain rehabilitation programme, which included psychological therapy.
We categorised different control conditions into either treatment‐as‐usual (n = 8), active (e.g. education, sham therapy; n = 27) or wait‐list (n = 12). We were able to extract post‐treatment data for outcomes included in this review from 31 studies post‐treatment, and for 16 studies at follow‐up. Thirty‐nine studies reported the treatment length; this was typically short (mean = 6 hours 36 minutes for headache studies, mean = 5 hours for mixed chronic pain studies (Table 3, note ‐ these averages excluded Hechler 2014 as they delivered an in‐patient programme which would have skewed the findings). Six studies did not report the duration of psychological treatment (Alfven 2007; Chen 2014; Humphreys 2000; Larsson 1990; Sartory 1998; Wahlund 2003).
1. Duration of treatment and setting by condition.
| Headache Studies | |||
| Author | Illness | Treatment duration (hours) | Setting |
| Abram 2007 | Headache | 1.5 | Clinic |
| Barry 1997 | Headache | 3 | Unknown |
| Bussone 1998 | Headache | 7 | Clinic |
| Chen 2014 | Headache | Unknown | Unknown |
| Cottrell 2007 | Headache | 4 hours plus tasks | Home |
| Fichtel 2001 | Headache | 6.75 | Clinic |
| Griffiths 1996 | Headache | 12 | Home/clinic |
| Hickman 2015 | Headache | 2.8 | Home/clinic |
| Hechler 2014* | Mixed | 136.5 (3‐week intensive therapy) | Clinic |
| Kroener‐Herwig 2002 | Headache | 12 | Clinic |
| Labbe 1984 | Headache | 6.7 | Clinic |
| Labbe 1995 | Headache | 7.5 | Clinic |
| Larsson 1987a | Headache | 6.75 | School |
| Larsson 1987b | Headache | 5 | School |
| Larsson 1990 | Headache | Unknown | Home |
| Larsson 1996 | Headache | 3.3 | Clinic |
| McGrath 1988 | Headache | 6 | Unknown |
| McGrath 1992 | Headache | 8 | Home/clinic |
| Osterhaus 1997 | Headache | 9.3 | Clinic |
| Passchier 1990 | Headache | 2.5 | School |
| Palermo 2016* | Mixed | 5 | Home/clinic |
| Powers 2013 | Headache | 13 | Clinic |
| Richter 1986 | Headache | 9 | Unknown |
| Sartory 1998 | Headache | Unknown | Clinic |
| Scharff 2002 | Headache | 4 | Clinic |
| Wicksell 2009* | Mixed | 10 | Clinic |
| Mixed Chronic Pain Studies | |||
| Author | Illness | Treatment duration hours) | Setting |
| Alfven 2007 | RAP | Unknown | Clinic |
| Barakat 2010 | SCD | 6 | Home |
| Daniel 2015 | SCD | 9.5 | Home/clinic |
| Duarte 2006 | RAP | 3.3 | Unknown |
| Gil 1997 | SCD | 0.75 | Clinic |
| Greenley 2015 | IBD | 4 | Home |
| Grob 2013 | RAP | 9 | Clinic |
| Gulewitsch 2013 | RAP/IBS | 2 | Clinic |
| Hechler 2014* | Mixed | 136.5 (3‐week intensive therapy) | Clinic |
| Humphreys 2000 | RAP | Unknown | Clinic |
| Kashikar‐Zuck 2005 | Fibromyalgia | 6 | Clinic |
| Kashikar‐Zuck 2012 | Fibromyalgia | 7.5 | Unknown |
| Levy 2010 | RAP | 4 | Home/clinic |
| Levy 2016 | IBD | 3.5 | Home/clinic |
| Levy 2017 | RAP | 3 | Home/clinic |
| Palermo 2016* | Mixed | 5 | Home/clinic |
| Robins 2005 | RAP | 3.5 | Clinic |
| Sanders 1994 | RAP | 6 | Clinic |
| Van der Veek 2013 | RAP | 4.5 | Clinic |
| Van Tilburg 2009 | RAP | 1.8 | Home |
| Vlieger 2007 | RAP/IBS | 5 | Clinic |
| Wahlund 2003 | TMD | Unknown | Unknown |
| Wahlund 2015 | TMD | 6 | Clinic |
| Wicksell 2009* | Mixed | 10 | Clinic |
*Headache and mixed chronic pain studies were entered twice. IBD: inflammatory bowel disease IBS: irritable bowel syndrome JIA: Juvenile idiopathic arthritis RAP: Recurrent abdominal pain SCD: Sickle cell disease TMD: temporomandibular disorders
The setting of treatment delivery varied between studies (Table 3). Twenty‐three studies delivered treatment in a clinic, eight were based either in a clinic or at home, and five delivered treatment to families at home, so exposure to treatment was uncontrolled. One study delivered treatment in an inpatient hospital setting. A further three were based in schools and seven studies were unclear as to the location of treatment delivery. Home maintenance or practice of treatment was a common and important feature of many studies, but overall treatment exposure including home practice was not reported.
Excluded studies
Nineteen studies were excluded, of which four were new to this update (Jastrowski Mano 2013; Korterink 2016; Rapoff 2014; Rutten 2017). We excluded Connelly 2006, Hicks 2006, Palermo 2009, Rapoff 2014, Stinson 2010, Trautmann 2010 as they were delivered remotely, so did not meet the new inclusion criteria. Eight studies were excluded as they had fewer than 10 participants in a treatment arm at the end of treatment (Fentress 1986; Jastrowski Mano 2013;Kroener‐Herwig 1998; Larsson 1986; Sanders 1989; Trautmann 2008; Weydert 2006; Youssef 2009), three studies were judged to have insufficient psychological content in the treatment (Koenig 2013; Korterink 2016; Olness 1987), one study reported only follow‐up data of more than one year (Vlieger 2012), and one trial was had a non‐inferiority design (Rutten 2017).
Risk of bias in included studies
We rated all included studies for risk of bias in five categories: random sequence generation (selection bias), allocation concealment (selection bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), and selective reporting (reporting bias) (Figure 2; Figure 3).
2.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
3.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Allocation
Random sequence generation
We found 16 trials used a convincing method of randomisation which we judged as having low risk of bias and we found a further 31 trials were judged at unclear risk of bias on random sequence generation, as they did not provide an adequate description of the method of randomisation. We scored none as having high risk of bias as the inclusion criteria required that studies randomised participants.
Allocation concealment
We found 12 trials adequately concealed allocation of participants, 31 had unclear allocation concealment, and we judged four studies as having high risk of bias.
Blinding
We found 11 trials that described adequate blinding of outcome assessors and, therefore, we allocated these trials as having low risk of bias. We found the remaining trials did not report on blinding and so were judged as having unclear risk of bias.
Incomplete outcome data
We found 17 studies reported attrition fully, reporting that there was no significant difference between completers and non‐completers. We found 24 studies only partially reported attrition and so we judged them to be at unclear risk of bias and we judged six studies to have a high risk of bias as they did not report attrition.
Selective reporting
We found 25 studies reported data fully, which could be extracted and used in analyses; seven studies did not fully report data in the published trial, but provided data when contacted via email; we judged 15 studies to have high risk of bias for selective reporting as they did not provide full extractable data.
Effects of interventions
For this update, we conducted subgroup analyses of trials that included fewer than 20 participants per arm or more than 20 participants per arm. A scorecard outlining the treatment effects is included in Table 4.
2. Scorecard of findings.
| Psychological treatments for children and adolescents with headache pain | ||||
| Pain | Disability | Depression | Anxiety | |
| Post‐treatment | Effect (15) | No effect (6) | No effect (6) | No effect (7) |
| < 20/arm | Effect (13) | No effect (2) | No effect (3) | No effect (4) |
| > 20/arm | Effect (2) | Effect (4) | No effect (3) | No effect (3) |
| Follow‐up | No effect (5) | Effect (3) | No effect (3) | No effect (4) |
| < 20/arm | Effect (4) | Unknown* | Unknown* | No effect (2) |
| > 20/arm | Unknown* | Effect (2) | No effect (2) | No effect (2) |
| Psychological treatments for children and adolescents with mixed pain conditions | ||||
| Pain | Disability | Depression | Anxiety | |
| Post‐treatment | Effect (16) | Effect (14) | No effect (8) | Effect (8) |
| < 20/arm | Effect (7) | Effect (6) | No effect (2) | Unknown* |
| > 20/arm | No effect (9) | Effect (8) | No effect (6) | Effect (7) |
| Follow‐up | No effect (9) | Effect (9) | No effect (7) | No effect (8) |
| < 20/arm | Effect (2) | No effect (2) | Unknown* | Unknown* |
| > 20/arm | No effect (7) | Effect (7) | No effect (6) | No effect (7) |
Unknown (no data); Unknown* (only one study); Number in brackets denotes number of studies in analysis.
Treatment versus control (headache) post‐treatment
Headache frequency/intensity, post‐treatment
We included 15 studies with 644 participants in an analysis of the effects of treatment on headache frequency/intensity post‐treatment (Barry 1997; Fichtel 2001; Griffiths 1996; Kroener‐Herwig 2002; Labbe 1984; Labbe 1995; Larsson 1987a; Larsson 1987b; Larsson 1990; Larsson 1996; McGrath 1992; Osterhaus 1997; Powers 2013; Sartory 1998; Scharff 2002). Overall, the analysis suggested a risk ratio (RR) of 2.35 (95% confidence interval (CI) 1.67 to 3.30; P < 0.01) for a beneficial reduction in headache frequency (number needed to treat for an additional beneficial outcome (NNTB) = 2.86) (Analysis 1.1; Figure 4). However, the GRADE quality rating for this outcome was very low, meaning we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. We downgraded this outcome due to limitations in design, imprecision of results, and asymmetrical funnel plot.
1.1. Analysis.

Comparison 1: Treatment versus control (headache) post‐treatment, Outcome 1: Pain
4.

Forest plot of comparison: 1 Treatment versus control (headache) post‐treatment, outcome: 1.1 Pain.
Subgroup analysis:
We found 13 studies (n = 437) that included fewer than 20 participants per arm for a beneficial reduction in headache frequency post‐treatment (RR 2.86; 95% CI 1.73 to 4.72, P < 0.01; NNTB = 2.59). Two studies (McGrath 1992; Powers 2013; n = 207), including more than 20 participants per arm, also had a beneficial effect on reducing headache frequency (RR 1.88, 95% CI 1.36 to 2.58, P < 0.01; NNTB = 3.58).
Disability, post‐treatment
We included six studies with 446 participants in the analysis of the effects of treatment on disability (Chen 2014; Hechler 2014; Hickman 2015; Palermo 2016; Powers 2013; Wicksell 2009). Overall, we did not find a beneficial effect of psychological therapies on reducing disability in children with headache (Standardised mean difference (SMD) ‐0.26, 95% CI ‐0.56 to 0.03, P = 0.08; Analysis 1.2). The GRADE quality rating for this outcome was very low, downgraded due to limitations in the design, unexplained heterogeneity, and for sparse data.
1.2. Analysis.

Comparison 1: Treatment versus control (headache) post‐treatment, Outcome 2: Disability
Subgroup analysis:
First, in two studies (Hickman 2015; Wicksell 2009, n = 61) that included fewer than 20 participants per arm, we did not find a beneficial effect of psychological treatment (SMD 0.04, 95% CI ‐0.47 to 0.54, P = 0.88). Second, for studies that included more than 20 participants per arm (Chen 2014; Hechler 2014; Palermo 2016; Powers 2013, n = 385), we found a medium beneficial effect of treatment on reducing disability (SMD ‐0.35, 95% CI ‐0.69 to 0.00, P = 0.05).
Depression, post‐treatment
We entered six studies with 400 participants in an analysis of the effects of treatment on depression (Griffiths 1996; Hechler 2014; Hickman 2015; Palermo 2016; Powers 2013; Wicksell 2009). We found psychological therapies did not show a beneficial effect for reducing depression for children with headache (SMD ‐0.08, 95% CI ‐0.28 to 0.11, P = 0.41; Analysis 1.3). We judged this outcome as having a very low‐quality rating, meaning we have very little confidence in the effect estimate. We downgraded the outcome due to limitations of study design, high probability of publication bias, and sparse data.
1.3. Analysis.

Comparison 1: Treatment versus control (headache) post‐treatment, Outcome 3: Depression
Subgroup analyses:
We found three trials that included fewer than 20 participants per arm (Griffiths 1996; Hickman 2015; Wicksell 2009, n = 103) but did not find a beneficial effect of therapy on depression (SMD ‐0.16, 95% CI ‐0.68 to 0.35, P = 0.53). In three studies that included more than 20 participants per arm (Hechler 2014; Palermo 2016; Powers 2013, n = 297), we found no beneficial effect of treatment on depression (SMD ‐0.06, 95% CI ‐0.29 to 0.17; P = 0.60).
Anixety, post‐treatment
We entered data from seven studies with 439 participants into an analysis of the effects of treatment on anxiety at post‐treatment (Bussone 1998; Griffiths 1996; Hechler 2014; Hickman 2015; Palermo 2016; Powers 2013; Wicksell 2009). We found no beneficial effect for psychological therapies (SMD ‐0.11, 95% CI ‐0.39 to 0.17, P = 0.43; Analysis 1.4). We have low confidence in this estimate of effect, meaning our confidence in the effect estimate was limited; the true effect may be substantially different from the estimate of the effect. We judged the quality of evidence to be very low due to limitations in study design, unexplained heterogeneity, high probability of publication bias, and asymmetrical funnel plot.
1.4. Analysis.

Comparison 1: Treatment versus control (headache) post‐treatment, Outcome 4: Anxiety
Subgroup analyses:
We found four studies that included fewer than 20 participants per arm (Bussone 1998; Griffiths 1996; Hickman 2015; Wicksell 2009, n = 136), but we found no beneficial effect of psychological treatments on reducing anxiety (SMD 0.01, 95% CI ‐0.54 to 0.57, P = 0.97). In three studies that included more than 20 participants (Hechler 2014; Palermo 2016; Powers 2013; n = 303), we also found no beneficial effect of treatment on reducing anxiety (SMD ‐0.19, 95% CI ‐0.49 to 0.11; P = 0.21)
Adverse events
Out of the 23 headache studies, Larsson 1990, Palermo 2016, Powers 2013, and Wicksell 2009 reported adverse events. Larsson 1990 reported four adverse events in relation to medications that were part of the trial. All participants dropped out. Palermo 2016 reported that there were no study‐related adverse events. Powers 2013 categorised adverse events into different grades dependent on severity. There were 199 adverse events in total, although the authors did not state how many were due to the psychological intervention. However, this trial delivered amitriptyline to participants. There was no difference in the severity of events between the cognitive behaviour therapy (CBT) and headache education group. Wicksell 2009 reported that two participants dropped out due to adverse events associated with amitriptyline.
Treatment versus control (headache) follow‐up
Headache frequency, follow‐up
We entered data from five studies of 223 participants into analysis of the effects of treatment on headache frequency at follow‐up (Labbe 1984; Larsson 1987a; Larsson 1987b; Larsson 1996; Powers 2013). This analysis produced a RR of 2.73 (95% CI 0.98 to 7.63; P = 0.06; Analysis 2.1), for a clinically beneficial change in pain (NNTB = 3.16). Using the GRADE criteria, pain at follow‐up was based on studies having very low‐quality, meaning we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. We downgraded the outcome due to limitations in the design, unexplained heterogeneity, imprecision of results and sparse data, high probability of publication bias, and asymmetrical funnel plot.
2.1. Analysis.

Comparison 2: Treatment versus control (headache) follow‐up, Outcome 1: Pain
Subgroup analyses:
Out of the five trials included in the analysis, four included fewer than 20 participants per arm (Labbe 1984; Larsson 1987a; Larsson 1987b; Larsson 1996; n = 99), and we found a beneficial effect of psychological treatments at reducing headache frequency (RR = 3.49, 95% CI 1.31 to 9.26; P = 0.01; NNTB = 1.77). Only one study (Powers 2013) could be included in the second subgroup analysis, therefore we did not report the findings.
Disability, follow‐up
We included data from three studies with 209 participants in the analysis to determine the effects of treatment on disability at follow‐up (Palermo 2016; Powers 2013; Wicksell 2009). Psychological therapies appeared to indicate a medium beneficial effect for reducing disability at follow‐up (SMD ‐0.37, 95% CI ‐0.65 to ‐0.10, P < 0.01; Analysis 2.2). We judged the quality of evidence for this outcome as very low, which we downgraded, due to high probability of publication bias and sparse data.
2.2. Analysis.

Comparison 2: Treatment versus control (headache) follow‐up, Outcome 2: Disability
Subgroup analyses:
Due to the small number of studies included in this analysis, we could not conduct a subgroup analysis for studies including fewer than 20 participants per arm. For studies including more than 20 participants per arm, we included two studies (Palermo 2016; Powers 2013; n = 185). We found a medium effect on disability at follow‐up (SMD ‐0.36, 95% CI ‐0.65 to ‐0.07; P = 0.02).
Depression, follow‐up
We found three studies that assessed depression at follow‐up (Palermo 2016; Powers 2013; Wicksell 2009, n = 228). We did not find a beneficial effect of psychological treatments for reducing depression at follow‐up (SMD ‐0.05, 95% CI ‐0.62 to 0.52, P = 0.86; Analysis 2.3). We judged the quality of evidence as very low, downgraded due to unexplained heterogeneity and imprecision of the result.
2.3. Analysis.

Comparison 2: Treatment versus control (headache) follow‐up, Outcome 3: Depression
Subgroup analyses:
Similar to disability, due to the small number of studies included in this analysis, we could not conduct a subgroup analysis for studies including fewer than 20 participants per arm. We did not find a significant effect for depression at follow‐up in two studies (Palermo 2016; Powers 2013; n = 204; SMD 0.11, 95% CI ‐0.61 to 0.83; P = 0.76).
Anxiety, follow‐up
We found four studies with 271 participants that assessed anxiety at follow‐up (Bussone 1998; Palermo 2016; Powers 2013; Wicksell 2009). We found no beneficial effect of psychological interventions in reducing anxiety at follow‐up (SMD ‐0.12, 95% CI ‐0.46 to 0.21; P = 0.47; Analysis 2.4). We judged the quality of evidence for this outcome as very low, which we downgraded due to limitations in study design and sparse data. Therefore, we were very uncertain of this estimate of effect.
2.4. Analysis.

Comparison 2: Treatment versus control (headache) follow‐up, Outcome 4: Anxiety
Subgroup analyses:
We were able to conduct a subgroup analysis on studies including fewer than 20 participants per arm (Bussone 1998; Wicksell 2009, n = 67) and did not find a beneficial effect of treatment on anxiety (SMD ‐0.28, 95% CI ‐1.00 to 0.45; P = 0.45). For studies including more than 20 participants per arm, we also did not find a beneficial effect of psychological therapies on anxiety at follow‐up (Palermo 2016; Powers 2013; n = 204; SMD ‐0.04, 95% CI ‐0.48 to 0.41; P = 0.88).
Treatment versus control (mixed chronic pain) post‐treatment
Pain intensity
To assess the effects of psychological therapies on pain intensity post‐treatment, we included 16 studies of 1210 participants (Barakat 2010; Grob 2013; Gulewitsch 2013; Hechler 2014; Humphreys 2000; Kashikar‐Zuck 2005; Kashikar‐Zuck 2012; Levy 2010; Levy 2017; Palermo 2016; Robins 2005; Van der Veek 2013; Van Tilburg 2009; Vlieger 2007; Wahlund 2015; Wicksell 2009) in an analysis. When analysing all studies combined, we found a moderate beneficial effect of psychological treatments on reducing pain intensity (SMD ‐0.43, 95% CI ‐0.67 to ‐0.19, P < 0.01; Analysis 3.1; Figure 5). According to the GRADE criteria for assessing quality of outcomes, pain post‐treatment was based on studies of very low‐quality, meaning we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. We downgraded the outcome twice due to unexplained heterogeneity and asymmetrical funnel plot.
3.1. Analysis.

Comparison 3: Treatment versus control (mixed pain) post‐treatment, Outcome 1: Pain
5.

Forest plot of comparison: 3 Treatment versus control (mixed chronic pain conditions) post‐treatment, outcome: 3.1 Pain.
Subgroup analyses:
We found seven studies including 250 participants (Barakat 2010; Grob 2013; Gulewitsch 2013; Humphreys 2000; Kashikar‐Zuck 2005; Van Tilburg 2009; Wicksell 2009) that included fewer than 20 participants per arm. We found a large beneficial effect of psychological therapies on reducing pain intensity (SMD ‐0.83, 95% CI ‐1.19 to ‐0.46, P < 0.01). In contrast, we found a small but non‐beneficial effect for studies including more than 20 participants per arm on reducing pain intensity (9 studies, 960 participants; SMD ‐0.20, 95% CI ‐0.45 to 0.05; P = 0.11).
Disability
We found 14 studies, 1226 participants, that investigated the effects of psychological interventions on disability post‐treatment (Grob 2013; Gulewitsch 2013; Hechler 2014; Humphreys 2000; Kashikar‐Zuck 2005; Kashikar‐Zuck 2012; Levy 2010; Levy 2016; Levy 2017; Palermo 2016; Robins 2005; Van der Veek 2013; Van Tilburg 2009; Wicksell 2009). We found a small beneficial effect of psychological therapies on reducing disability for children with chronic pain (SMD ‐0.34, 95% CI ‐0.54 to ‐0.15, P < 0.01; Analysis 3.2). We judged the quality of the evidence to be low, meaning our confidence in the effect estimate was limited; the true effect may be substantially different from the estimate of the effect. The outcome was downgraded once due to unexplained heterogeneity and asymmetrical funnel plot.
3.2. Analysis.

Comparison 3: Treatment versus control (mixed pain) post‐treatment, Outcome 2: Disability
Subgroup analyses:
We found six studies including 213 participants that included fewer than 20 participants per arm. We found a large beneficial effect in this subgroup analysis for reducing disability post‐treatment (SMD ‐0.72, 95% CI ‐1.17 to ‐0.26, P = 0.01). For the eight studies that included more than 20 participants per arm (n = 1013), we found a small beneficial effect of psychological therapies for reducing disability (SMD ‐0.20, 95% CI ‐0.37 to ‐0.04; P = 0.02).
Depression
Overall, we found eight studies with 757 participants that evaluated the effects of psychological treatment on depression (Hechler 2014; Kashikar‐Zuck 2005; Kashikar‐Zuck 2012; Levy 2010; Levy 2016; Palermo 2016; Van der Veek 2013; Wicksell 2009). The analysis revealed no beneficial effect of psychological therapies on depression (SMD ‐0.05, 95% CI ‐0.23 to 0.12, P = 0.54; Analysis 3.3). We judged the quality of evidence to be very low. We downgraded the outcome twice due to high probability of publication bias and asymmetrical funnel plot.
3.3. Analysis.

Comparison 3: Treatment versus control (mixed pain) post‐treatment, Outcome 3: Depression
Subgroup analyses:
We found two studies (n = 59) that included fewer than 20 participants per arm. There was no beneficial effect of psychological treatment on depression across these two studies (SMD ‐0.27, 95% CI ‐0.95 to 0.41, P = 0.44). Similarly, we found no beneficial effect of six studies with more than 20 participants per arm that included 698 participants post‐treatment, for reducing depression symptoms (SMD ‐0.03, 95% CI ‐0.21 to 0.15; P = 0.74).
Anxiety
We found eight studies including 957 participants that assessed the effect of psychological therapies on the outcome of anxiety post‐treatment (Hechler 2014; Kashikar‐Zuck 2012; Levy 2010; Levy 2016; Levy 2017; Palermo 2016; Van der Veek 2013; Wicksell 2009). The results revealed a beneficial effect of psychological therapies on anxiety in children with chronic pain, (SMD ‐0.16, 95% CI ‐0.29 to ‐0.03, P = 0.02; Analysis 3.4). Similar to depression, we judged the evidence for this estimate of effect as low; we downgraded the outcome twice due to high probability of publication bias.
3.4. Analysis.

Comparison 3: Treatment versus control (mixed pain) post‐treatment, Outcome 4: Anxiety
Subgroup analyses:
Only one study assessed anxiety post‐treatment and included fewer than 20 participants per arm, therefore we did not report the finding here. We found seven studies including 851 participants with more than 20 participants per arm. These studies indicated a small beneficial effect of psychological therapies for reducing anxiety at post‐treatment (SMD ‐0.17, 95% CI ‐0.30 to ‐0.04; P = 0.01).
Adverse events
Of the 24 mixed pain studies, six reported adverse events. Gulewitsch 2013, Kashikar‐Zuck 2012, Levy 2017, Palermo 2016, and Van der Veek 2013 reported no adverse events that were study‐related. Wicksell 2009reported that two participants withdrew due to adverse effects of amitriptyline, which was part of the study conditions.
Treatment versus control (mixed chronic pain) follow‐up
Pain intensity
We found nine studies of 833 participants that investigated the effect of psychological treatments on pain at follow‐up (Barakat 2010; Grob 2013; Hechler 2014; Kashikar‐Zuck 2012; Levy 2010; Levy 2017; Palermo 2016; Van der Veek 2013; Wicksell 2009). Overall, we did not find a beneficial effect on reducing pain intensity at follow‐up (SMD ‐0.08, 95% CI ‐0.30 to 0.13, P = 0.45; Analysis 4.1). The quality was very low for this outcome, meaning we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. We downgraded the outcome once due to unexplained heterogeneity, once due to high probability of publication bias and asymmetrical funnel plot.
4.1. Analysis.

Comparison 4: Treatment versus control (mixed pain) follow‐up, Outcome 1: Pain
Subgroup analyses:
We found two studies with 53 participants that included fewer than 20 participants per arm. We found a beneficial effect of psychological therapies on reducing pain intensity at follow‐up (SMD ‐0.94, 95% CI ‐1.75 to ‐0.13, P = 0.02). Seven studies with 780 participants included more than 20 participants per arm but in contrast to the prior subgroup analysis, we did not find a beneficial effect for reducing pain intensity (SMD ‐0.00, 95% CI ‐0.15 to 0.14; P = 0.99).
Disability
Overall, we found nine studies that included 935 participants that assessed the effect of psychological interventions on disability at follow‐up (Grob 2013; Hechler 2014; Kashikar‐Zuck 2012; Levy 2010; Levy 2016; Levy 2017; Palermo 2016; Van der Veek 2013Wicksell 2009). We found a beneficial effect of psychological treatments on reducing disability at follow‐up (SMD ‐0.27, 95% CI ‐0.49 to ‐0.06, P = 0.01; Analysis 4.2). We judged the quality of evidence to be low due to unexplained heterogeneity and once due to high probability of publication bias.
4.2. Analysis.

Comparison 4: Treatment versus control (mixed pain) follow‐up, Outcome 2: Disability
Subgroup analyses:
We were able to conduct three subgroup analyses. For trials including fewer than 20 participants per arm, we found two studies including 53 participants. We did not find a beneficial effect of psychological treatments on disability at follow‐up (SMD ‐1.17, 95% CI ‐2.60 to 0.26, P = 0.11). In seven trials including 882 participants, we found a small beneficial effect of psychological treatments for reducing disability (SMD ‐0.20, 95% CI ‐0.34 to ‐0.07; P < 0.01).
Depression
We found seven studies including 667 participants reporting on the effects of treatment on depression at follow‐up (Hechler 2014; Kashikar‐Zuck 2012; Levy 2010; Levy 2016; Palermo 2016; Van der Veek 2013; Wicksell 2009). We did not find a beneficial effect of psychological therapies on depression at follow‐up (SMD 0.09, 95% CI ‐0.10 to 0.28, P = 0.35; Analysis 4.3). We judged the quality of evidence to be very low due to unexplained heterogeneity, high probability of publication bias, and asymmetrical funnel plot.
4.3. Analysis.

Comparison 4: Treatment versus control (mixed pain) follow‐up, Outcome 3: Depression
Subgroup analyses:
We were only able to conduct a subgroup analysis of trials that included more than 20 participants per arm. In six studies including 643 participants, we did not find a beneficial effect of treatment for reducing depression at follow‐up (SMD 0.12, 95% CI ‐0.06 to 0.30; P = 0.20).
Anxiety
Eight studies including 975 participants assessed anxiety at follow‐up (Hechler 2014; Kashikar‐Zuck 2012; Levy 2010; Levy 2016; Levy 2017; Palermo 2016; Van der Veek 2013; Wicksell 2009). We did not find a beneficial effect of psychological therapies on anxiety outcomes at follow‐up (SMD 0.01, 95% CI ‐0.20 to 0.18, P = 0.92; Analysis 4.4). Similar to anxiety post‐treatment, we have low confidence in the estimate of effect, downgraded twice due to high probability of publication bias.
4.4. Analysis.

Comparison 4: Treatment versus control (mixed pain) follow‐up, Outcome 4: Anxiety
Subgroup analyses:
We were able to conduct a subgroup analysis on studies including more than 20 participants per arm. In seven studies (n = 843) we found that psychological therapies did not have a beneficial effect on anxiety outcomes at follow‐up (SMD ‐0.01, 95% CI ‐0.22 to 0.19; P = 0.89).
Heterogeneity
We conducted 16 analyses and found that six analyses indicated low heterogeneity, six analyses indicated moderate heterogeneity, and three analyses had considerable heterogeneity.
Reporting biases
We checked for publication bias using contour‐enhanced funnel plots, tests of funnel plot asymmetry and meta‐regressions including total sample size as a moderator. We conducted the analysis for all analyses conducted in the review, and we found evidence of significant funnel plot asymmetry for the following analyses:
Children and adolescents with headache:
Headache frequency at post‐treatment;
Headache frequency at follow‐up;
Anxiety post‐treatment for children.
Children and adolescents with mixed pain conditions:
Pain intensity at post‐treatment;
Pain intensity at follow‐up;
Disability at post‐treatment;
Depression at post‐treatment;
Depression at follow‐up.
Funnel plot asymmetry is not synonymous with publication bias but leads us to suspect its presence which may lead to over‐estimates of effectiveness, particularly where regression tests of asymmetry are statistically significant. However, there was no evidence of statistically significant linear relationships between effect size and sample size for these analyses, with the exception of pain intensity in children with mixed pain conditions at post‐treatment.
Quality of evidence
The quality of evidence was assessed separately for headache and mixed pain condition studies using the GRADE criteria. For headache conditions, we judged all outcomes as being based on studies of low or very low‐quality meaning we were very uncertain of the estimates and that future research is very likely to have an important impact on the estimate of effect (Summary of findings table 1). We judged the outcomes of pain post‐treatment and at follow‐up, disability at follow‐up and anxiety at follow‐up as being based on studies of very low‐quality. We judged disability, anxiety, and depression post‐treatment as being based on studies of low‐quality. For mixed pain conditions, we judged all outcomes as low‐quality or very low‐quality (Summary of findings table 2).
Sensitivity analyses
We conducted sensitivity analyses on three analyses that included more than 10 studies: pain outcomes in children with headache pain and mixed chronic pain, and disability in children with mixed chronic pain. All analyses were conducted at post‐treatment (Table 5). We did not find any differences in the beneficial effects of treatment. For children with headache, the sensitivity analysis indicated a beneficial effect (RR 2.79, 95% CI 2.01 to 3.89; participants = 325; studies = 15; I2 = 56%), although heterogeneity remained high. Similar findings were found for children with mixed pain conditions for pain post‐treatment (SMD ‐0.57, 95% CI ‐0.90 to ‐0.24, I2 = 74%, 11 studies, 671 participants, P < 0.001) and disability post‐treatment (SMD ‐0.37, 95% CI ‐0.64 to ‐0.11, I2 = 60%, 9 studies, 687 participants, P < 0.001). Please see Appendix 2 for results regarding model over‐fitting for the sensitivity analyses.
3. Results of sensitivity analyses.
| Outcome | Sensitivity analysis |
| Pain, children with headache, post‐treatment | RR 2.79, 95% CI 2.01 to 3.89; participants = 325; studies = 15; I2 = 56% |
| N < 20 | RR 2.79, 95% CI 2.01 to 3.89; participants = 325; studies = 15; I2 = 56% |
| N > 20 | No studies could be included in the analysis |
| Pain, children with mixed pain conditions, post‐treatment | SMD ‐0.57, 95% CI ‐0.90 to ‐0.24; participants = 671; studies = 16; I2 = 74% |
| N < 20 | SMD ‐0.84, 95% CI ‐1.27 to ‐0.41; participants = 221; studies = 7; I2 = 54% |
| N > 20 | SMD ‐0.31, 95% CI ‐0.73 to 0.12; participants = 450; studies = 9; I2 = 79% |
| Disability, children with mixed pain conditions, post‐treatment | SMD ‐0.37, 95% CI ‐0.64 to ‐0.11; participants = 687; studies = 14; I2 = 60% |
| N < 20 | SMD ‐0.67, 95% CI ‐1.21 to ‐0.13; participants = 184; studies = 6; I2 = 64% |
| N > 20 | SMD ‐0.21, 95% CI ‐0.41 to ‐0.00; participants = 503; studies = 8; I2 = 25% |
CI: confidence intervals SMD: standardised mean difference
Discussion
Summary of main results
We assessed the evidence for psychological therapies on pain, disability, anxiety, and depression in children and adolescents with chronic pain. We found 10 new trials and included an additional 869 participants in this update, resulting in 47 randomised controlled trials (end of treatment, N = 2884). In each update, the author team discussed the validity of the inclusion and exclusion criteria. We were aware that small studies are a significant problem in pain research (Moore 2013) and sought, wherever possible, to increase the accuracy of our review by controlling for the imprecision inherent in small n studies. In this case, the trade‐off between accuracy and comprehensiveness was considered and we decided to retain the previous criteria (included studies should have a minimum of 10 participants per arm). For transparency, however, we decided to present subgroup analyses. We undertook subgroup analyses of those studies with fewer than 20 participants per arm, and those with more, allowing for an indirect comparison between analyses based on sample size. Typically, the studies with fewer participants were older or pilot studies. The majority of studies evaluated one or two treatment conditions in comparison to a waiting‐list or to a treatment‐as‐usual control group. For the first time in the history of this review, we included a treatment that we categorised as problem‐solving, adding to the previously included behavioural and cognitive‐behavioural treatments delivered to children with chronic pain. The average length of treatment in studies of headache conditions and mixed chronic pain studies was very similar, between five and seven hours. Follow‐up data were increasingly being reported in more recent studies and we included these, when available.
The inclusion of new studies in this updated meta‐analysis has extended the evidence base. Of the 16 possible analyses, psychological therapies were beneficial for six outcomes. For children with headache, we found psychological treatments were beneficial at reducing headache pain frequency/intensity post‐treatment, but the effect was not maintained at follow‐up. We found a NNTB of 2.86 for psychological therapies post‐treatment, and 3.16 at follow‐up for more than 50% reduction in pain frequency/intensity in children with headaches. In the sub‐group analyses of more than and less than 20 participants per arm, we also found that psychological therapies demonstrated beneficial effects on reducing pain intensity. We found a beneficial effect on reducing disability at follow‐up, but findings at post‐treatment showed an overall null effect of psychological therapies on reducing disability. However, in the subgroup analysis including more than 20 participants per arm, we found a beneficial effect on disability whereas there was no effect in studies including fewer than 20 participants per arm. For the outcomes of depressive and anxious symptoms, we did not detect an effect at either post‐treatment or follow‐up.
There were similar findings for analyses investigating children with mixed pain conditions. First, we found that psychological therapies were beneficial at reducing pain intensity, disability, and anxiety post‐treatment, but only the benefits for disability were maintained at follow‐up. Interestingly, larger studies (> 20 per arm) did not show a beneficial effect for pain reduction at post‐treatment whereas smaller studies in this analysis (< 20 per arm) indicated a large beneficial effect. In the subgroup analysis investigating disability post‐treatment, we found improvements in disability, regardless of the size of the study. At follow‐up, we found an overall beneficial effect for disability, but when investigating the subgroups, we found only larger studies (n > 20 participants per arm) were significant. Similar to headache conditions, no effect was found for depressive symptoms.
Overall completeness and applicability of evidence
More recent trials typically used cognitive behavioural therapy rather than behavioural therapy, likely reflecting changes in practice by psychologists entering the field of paediatric pain management. For the first time in the history of this review, we included a trial that used problem‐solving therapy for parents of children with chronic pain. This is consistent with recent calls to develop and evaluate other types of therapies for children with chronic pain conditions and their families (Eccleston 2015; Law 2014).
In regard to pain conditions, this review included 23 trials of children and adolescents with headache pain, 10 abdominal pain studies, two abdominal pain and irritable bowel syndrome studies, two fibromyalgia studies, two temporomandibular disorder studies, three sickle cell disease studies, two studies with inflammatory bowel disease, and three mixed pain studies (including headache and mixed chronic pain conditions). There was limited evidence to draw conclusions about the effects of psychological treatment on disability in headache conditions. Although we found psychological therapies to be beneficial for disability outcomes, only six studies could be included in this analysis post‐treatment, and three at follow‐up. In addition, we were only able to include a small number of studies in the follow‐up analyses for the outcomes of depression and anxiety, meaning we were unable to draw any conclusions regarding whether psychological interventions resulted in long‐term changes in anxiety and depressive symptoms for children with headaches.
In 2008, consensus guidelines were published which outlined core outcome domains and measures for clinical trials of psychological interventions for children and adolescents with chronic pain (McGrath 2008). Adherence to these guidelines has increased over time. In the previous update, we encouraged trial authors to include anxiety and depression symptom measures as outcomes, in addition to pain and disability outcomes. Most of the trials included in this update did include such measures.
One limitation of this review is that we did not conduct a sub‐group analysis comparing results from trials that used an active control condition versus a wait‐list control condition. This has been explored in our companion review of psychological treatments for adults with pain, and findings suggested that larger effects were found when a waiting‐list or treatment‐as‐usual control was used (Williams 2012). Thus, findings from this update may have overestimated the treatment effects, since some of the trials included in our meta‐analyses used less rigorous control conditions. However, we did conduct subgroup analyses on smaller versus larger trials based on the number of participants.
Quality of the evidence
We judged the quality of the evidence to be low or very low for all outcomes. The primary reason for low and very low judgements for studies treating children with headache was due to high risk of bias, high levels of heterogeneity, suspicion of publication bias, and most studies did not assess depression and anxiety outcomes. With regards to low and very low judgements for mixed pain conditions, we found high levels of heterogeneity in the analyses and a large proportion of studies did not report on the outcomes. Therefore, this evidence is likely to change when more data are available and interpretations should be made cautiously.
There was widespread evidence of funnel plot asymmetry leading us to suspect publication bias in many of our findings. This means that it is likely there are unpublished studies investigating psychological therapies for children with chronic pain conditions. This has resulted in reductions in the strength of evidence for many outcomes but the impact of the potential bias is unknown. For the pain intensity for children with mixed pain, there was strong evidence of small study effects, suggesting that the effect size was an overestimate of effectiveness. Coupled with the high level of unexplained and clinically significant inconsistency, this resulted in low strength of the evidence for this combination of population, intervention, and outcome.
Potential biases in the review process
We have conducted searches of four large databases, we checked the reference lists and conducted citation searches of included studies, and searched trial registries for studies. Therefore, we think it is unlikely that we have missed any published, randomised controlled trials eligible for this review. An author of this review conducted one trial included in this update. Review authors not involved in the trial or the publication of the trial extracted data and conducted 'risk of bias' assessments for this trial.
Agreements and disagreements with other studies or reviews
The findings from this review largely supports findings from previous updates of this review (Eccleston 2003; Eccleston 2009; Eccleston 2012; Eccleston 2014). It also supports the findings of the sister review that investigated remotely delivered trials to children with chronic pain (Fisher 2015). Further, a separate systematic review, that included all trials that delivered psychological therapies to children with chronic pain, also supports the majority of the findings here (Fisher 2014). However, in the current review we found beneficial effects at follow‐up on disability for children with mixed pain conditions, whereas Fisher 2014 did not find beneficial effects at follow‐up. There are also reviews of individual pain conditions in the field. A systematic review investigating children with migraine found beneficial effects of migraine post‐treatment and at follow‐up (Ng 2017). A review investigating rheumatic diseases did not have enough data to combine in a meta‐analysis and found conflicting evidence (Cohen 2017). Similarly, a review investigating sickle cell disease (Anie 2015) identified five studies but a meta‐analysis could not be conducted. Results from individual studies indicated that cognitive behavioural therapy was not beneficial at reducing pain outcomes in this population. No studies reported on mood, and disability was not assessed in children with sickle cell disease (Anie 2015). Finally, a review investigating recurrent abdominal pain did not find a significant reduction in pain intensity at short‐term follow‐up for children and adolescents receiving CBT, but significant beneficial effects were identified for children with recurrent abdominal pain receiving hypnotherapy (Abbott 2017). Despite some disagreement with findings in this review, Abbott 2017 included fewer studies, due to only including children with abdominal pain. Therefore, this may indicate that psychological therapies may have different effects for different populations. Further, in agreement with this review, Abbott 2017 found no beneficial effect for improving anxiety and depressive symptoms.
Authors' conclusions
Implications for practice.
For children and adolescents with chronic pain
Most therapies that have been delivered to children and adolescents with chronic pain, their parents, or both, are cognitive behavioural therapy or behavioural therapy. We found that these psychological therapies are effective for reducing pain for children with headaches, and reducing pain intensity and disability in children with mixed chronic pain conditions. However, most effects were not maintained at follow‐up, with the exception of disability for children with mixed chronic pain conditions. The treatments had no positive effect on anxiety or depression immediately after treatment or at follow‐up. Quality issues in these trials reduced our confidence in the effect estimates, meaning that new studies could substantially alter the findings.
For clinicians
Taken together, these findings suggested that behavioural and cognitive‐behavioural treatment should be considered as part of standard care for children and adolescents with chronic pain conditions to improve pain and reduce disability. We did not find any beneficial effects for the outcomes of depression at any time point, and only for anxiety in mixed pain conditions post‐treatment. This lack of effect may be due to the fact that anxiety and depression are typically not a specific intervention target of cognitive and behavioural pain management interventions, and enrolled youth had varying levels of anxiety and depression (including many youth with nonclinical levels of anxiety and depression). We also found two trials (n = 277 participants across both trials) that delivered therapy to parents of children with chronic pain, but these should be interpreted with caution. Further data are needed to understand possible downstream effects for children.
For policy makers
The quality of evidence for psychological therapies to reduce pain, disability, anxiety, and depression was mostly low or very low, meaning our confidence in the effect estimate is limited, open to change with future study, and, therefore, should be interpreted with caution. A sister review (Eccleston 2015) included an analysis investigating parent interventions for children with chronic pain and found beneficial effects on parent mental health and behaviour as well as child outcomes. However, the downstream effects for children with chronic pain in trials that only included parents are unknown. More studies will determine this, but this type of treatment could be beneficial for both parent and child.
Implications for research.
General
Since the original version of this review, there has been an improvement in the evidence base by the addition of new studies, including additional studies of youth with a variety of chronic pain conditions and the development of treatments that target parents as well as children. We also conducted new subanalyses to evaluate outcomes in larger versus smaller trials. The author team will continue to consider the following changes in the next version of the review.
Splitting the title into two: one for headache only and one for mixed pain conditions.
Exploring the possibility of subgroup analyses to try to identify variance attributable to nonspecific factors which can affect treatment outcome, such as type of therapy.
Exploring the possibility of subgroup analyses by pain condition (e.g. recurrent abdominal pain versus musculoskeletal pain versus headache).
Exploring the possibility of subgroup analyses to try to identify whether effects differ by type of comparator (e.g. wait‐list versus active comparators).
Design
Methodologically, there were challenges in this review with trial designs. The majority of included studies were relatively small randomised controlled trials, recruiting fewer than 100 participants. Most trials have evaluated the efficacy of treatment for children with headache, while few trials have been conducted in young people with other chronic pain conditions (e.g. complex regional pain syndrome, sickle cell disease, arthritis). Indeed, it was unclear whether children had different treatment needs, depending on the characteristics of their pain problem, or if a one‐size‐fits‐all approach is appropriate. Treatments tailored to children and adolescents to treat distress before working to reduce pain and disability might find larger effect sizes. Finally, we still do not know the active ingredient of psychological therapies. More detailed description of treatments and inclusion of process measures would help to identify active components of therapies, and allow the development of more targeted interventions for this population. In this update, one trial used problem‐solving therapy delivered to parents of children with chronic pain (Palermo 2016). Divergence from traditional cognitive behavioural therapy and from models where the child is the treatment target may be beneficial, and we encourage further exploration of these alternatives in future trials.
Measurement
Although guidelines for measurement in clinical trials for young people with chronic pain have been published (McGrath 2008), consensus between researchers and clinicians is still needed with regards to gold standard measures of disability, depression, and anxiety. This would reduce the heterogeneity of analyses. Sensitivity to change should be a core psychometric property for measures used in randomised controlled trials (Fisher 2017). Further, clinically meaningful change should be established for outcomes used in trials to help interpret whether therapies are achieving meaningful change for participants. Researchers and clinicians have previously agreed on headache outcomes for young people. There is consensus amongst headache researchers and clinicians that 50% reduction in headache frequency is clinically meaningful and should be used as a primary outcome in headache trials. However, such consensus has not been reached for other pain characteristics and for other pain conditions. Finally, adverse events should be reported in every trial. Although more trials reported adverse events in this update, this was not universal. Development of a common measure of adverse events might encourage more widespread use and reporting of this outcome.
What's new
| Date | Event | Description |
|---|---|---|
| 13 October 2020 | Review declared as stable | See Published notes. |
History
Protocol first published: Issue 1, 2003 Review first published: Issue 1, 2003
| Date | Event | Description |
|---|---|---|
| 30 September 2019 | Amended | Clarification added to Declarations of interest. |
| 1 October 2018 | Amended | Date Next Stage Expected updated. |
| 23 May 2018 | New search has been performed | This review has been updated to include the results of a new search on 1 May 2018. |
| 23 May 2018 | New citation required but conclusions have not changed | 10 new studies (869 additional participants). Findings not substantially different from previous review. GRADE ratings were similar. |
| 9 February 2016 | Review declared as stable | See Published notes. |
| 14 May 2014 | Amended | Minor change to the GRADE assessment wording. |
| 30 April 2014 | New citation required but conclusions have not changed | A new search was run in January 2014. |
| 14 March 2014 | New search has been performed | Five new studies were added. Two trials containing additional information for previously included studies were included. Five studies that were previously included were excluded as they delivered treatment remotely. These will be included in the new Cochrane review ('Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents'). 'Mood' outcome was split into two discrete domains; anxiety and depression. |
| 21 August 2013 | Amended | 'Summary of findings' tables have been updated. |
| 24 October 2012 | New citation required and conclusions have changed | The previous review reported that psychological treatments were effective for headache and non‐headache groups at post‐treatment and effects were maintained at follow‐up. Updated studies have altered the previous results. The current update found that pain improved at post‐treatment for headache and non‐headache groups, and for headache groups at follow‐up. An additional significant finding for disability at post‐treatment for the non‐headache group was found. Conclusions have been updated accordingly. |
| 24 October 2012 | New search has been performed | New authors have been added to this review. A new search was run in March 2012. Eight new studies were added (Barakat 2010; Kashikar‐Zuck 2012; Levy 2010; Palermo 2009; Stinson 2010; Trautmann 2010; van Tilburg 2009a; Wicksell 2009), and four new studies were excluded (Trautmann 2008; Vlieger 2012; Weydert 2006; Youssef 2009). |
| 16 May 2008 | Amended | Converted to new review format. |
Notes
At October 2020, we are not aware of any new potentially relevant studies likely to change the conclusions. Therefore, this review has now been stabilised following discussion with the authors and editors. The review will be reassessed for updating in two years. If appropriate, we will update the review before this date if new evidence likely to change the conclusions is published, or if standards change substantially which necessitate major revisions.
Acknowledgements
We would like to thank Stephen Morley (deceased), Amy Lewandowski, and Amanda Williams for their contributions to the original review and previous updates.
We would like to thank Kiki Mastroyannopoulou and Louise Yorke for their contributions to the original version of this review. Thank you also to Hannah Somhegyi for help with coding and data management during previous versions of this review. Thanks to Jane Hayes and Jo Abbott for running the updated searches. Finally, thanks also go to the PaPaS review group team and to the peer referees for their helpful comments.
Cochrane Review Group funding acknowledgement: this project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Cochrane Pain, Palliative and Supportive Care Review Group (PaPaS). The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS, or the Department of Health.
Appendices
Appendix 1. Previous search results
Four separate searches were undertaken. The first search was undertaken from inception of the abstracting services to the end of 1999 (Eccleston 2003). This yielded 3715 abstracts, of which 123 were read in full, identifying 18 RCTs.
The second search, which updated the original review, was undertaken focusing on the 10 years since the previous search, overlapping by one year (from 1999 to 2008) and was later published (Eccleston 2009). This yielded 1319 abstracts, of which 45 papers were read in full, identifying a further 16 RCTs, giving a total set of 34. However, five studies were later excluded because they did not meet the minimum criteria of 10 participants in each arm, therefore, leaving 29 studies.
The third search, which searched databases from 2008 to March 2012, yielded 851 abstracts, of which 25 papers were read in full, and eight further RCTs were included in the review (Eccleston 2012).
The fourth search, which searched databases from March 2012 to January 2014, yielded 443 abstracts, of which 19 were read in full, and seven papers were included (Grob 2013; Gulewitsch 2013; Hechler 2014; Kashikar‐Zuck 2012; Levy 2010; Powers 2013; Van der Veek 2013). Kashikar‐Zuck 2012 and Levy 2010 provided additional data for studies previously included in this review. Five studies that were previously included, were excluded from this review since treatment was delivered remotely (Connelly 2006; Hicks 2006; Palermo 2009; Stinson 2010; Trautmann 2010). Therefore, a total of 37 RCTs were included (39 papers; Eccleston 2014).
Appendix 2. Model over‐fitting
We used AIC to mitigate the risk of overfitting due to repeated sensitivity analyses. The AIC scores indicate that all meta‐analyses are more parsimonious than meta‐regressions/subgroup analyses except pain intensity in children with mixed pain conditions at post‐treatment. Here, sample size explained enough variation to be worth including in the model based on change in AIC score. The model had very high inconsistency, partly explained by publication bias, but there was further heterogeneity not explained by our subgroup and sensitivity analyses. This reduced our confidence in the estimate of effect which is reflected in the GRADE assessment and 'summary of findings' tables.
Appendix 3. 2017 Search strategies
CENTRAL (CRSO)
#1 MeSH descriptor: [Child] explode all trees #2 MeSH descriptor: [Infant] explode all trees #3 MeSH descriptor: [Adolescent] explode all trees #4 (child* or adolescent* or infant*or juvenil* or pediatric* or paediatric* or "young person*" or "young people" or youth* or "young adult*"):it,ab,kw (Word variations have been searched) #5 #1 or #2 or #3 or #4 #6 MeSH descriptor: [Psychology] explode all trees #7 MeSH descriptor: [Psychotherapy] explode all trees #8 MeSH descriptor: [Behavior Therapy] explode all trees #9 (psycholog* or (behavio?r and therapy) or hypnos* or relaxation* or ((family or color or colour or music or play) next therap*) or imagery or cogniti* or psychotherap*):it,ab,kw (Word variations have been searched) #10 #6 or #7 or #8 or #9 #11 (pain* or headache* or "head ache*" or head‐ache* or migraine* or cephalalgi* or "stomach ache*" or "tummy ache*" or "abdominal ache*" or "belly ache*" or earache* or ear‐ache* or toothache* or tooth‐ache* or odontalgi* or dysmenorrh* or neuralgi*):it,ab,kw (Word variations have been searched) #12 MeSH descriptor: [Pain] explode all trees #13 MeSH descriptor: [Headache Disorders] explode all trees #14 #11 or #12 or #13 #15 #5 and #10 and #14
MEDLINE via Ovid search strategy
1. exp child/
2. Infant/
3. Adolescent/
4. (child$ or adolescent$ or infant$ or juvenil$ or pediatric$ or paediatric$ or "young person$" or "young people" or youth$ or "young adult$").ab,it,kf.
5. 1 or 2 or 3 or 4
6. exp Psychology/
7. exp Psychotherapy/
8. exp Behavior Therapy/
9. (psycholog$ or (behavio?r and therapy) or hypnos$ or relaxation$ or ((family or color or colour or music or play) adj therap$) or imagery or cogniti$ or psychotherap$).ab,it,kf.
10. 6 or 7 or 8 or 9
11. (pain$ or headache$ or "head ache$" or head‐ache$ or migraine$ or cephalalgi$ or "stomach ache$" or "tummy ache$" or "abdominal ache$" or "belly ache$" or earache$ or ear‐ache$ or toothache$ or tooth‐ache$ or odontalgi$ or dysmenorrh$ or neuralgi$).ab,it,kf.
12. exp Pain/
13. exp Headache Disorders/
14. 11 or 12 or 13
15. 5 and 10 and 14
16 randomized controlled trial.pt.
17 controlled clinical trial.pt.
18 randomized.ab.
19 placebo.ab.
20 drug therapy.fs.
21 randomly.ab.
22 trial.ab.
23 or/16‐22
24 exp animals/ not humans.sh.
25 23 not 24
26 25 and 15
Embase via Ovid search strategy
1. Child/
2. Infant/
3. Adolescent/
4. (child$ or adolescent$ or infant$ or juvenil$ or pediatric$ or paediatric$ or "young person$" or "young people" or youth$ or "young adult$").ab,it.
5. 1 or 2 or 3 or 4
6. exp PSYCHOLOGY/
7. exp PSYCHOTHERAPY/
8. behavior therapy/
9. (psycholog$ or (behavio?r and therapy) or hypnos$ or relaxation$ or ((family or color or colour or music or play) adj therap$) or imagery or cogniti$ or psychotherap$).ab,it.
10. 6 or 7 or 8 or 9
11. (pain$ or headache$ or "head ache$" or head‐ache$ or migraine$ or cephalalgi$ or "stomach ache$" or "tummy ache$" or "abdominal ache$" or "belly ache$" or earache$ or ear‐ache$ or toothache$ or tooth‐ache$ or odontalgi$ or dysmenorrh$ or neuralgi$).ab,it.
12. exp Pain/
13. exp "Headache and Facial Pain"/
14. 11 or 12 or 13
15. 5 and 10 and 14
16 random$.tw.
17 factorial$.tw.
18 crossover$.tw.
19 cross over$.tw.
20 cross‐over$.tw.
21 placebo$.tw.
22 (doubl$ adj blind$).tw.
23 (singl$ adj blind$).tw.
24 assign$.tw.
25 allocat$.tw.
26 volunteer$.tw.
27 Crossover Procedure/
28 double‐blind procedure.tw.
29 Randomized Controlled Trial/
30 Single Blind Procedure/
31 or/16‐30
32 (animal/ or nonhuman/) not human/
33 31 not 32
34 15 and 33
PsycINFO via OVID
1. (child$ or adolescent$ or infant$ or juvenil$ or pediatric$ or paediatric$ or "young person$" or "young people" or youth$ or "young adult$").ab,it.
2. exp PSYCHOLOGY/
3. exp PSYCHOTHERAPY/
4. behavior therapy/
5. (psycholog$ or (behavio?r and therapy) or hypnos$ or relaxation$ or ((family or color or colour or music or play) adj therap$) or imagery or cogniti$ or psychotherap$).ab,it.
6. 2 or 3 or 4 or 5
7. (pain$ or headache$ or "head ache$" or head‐ache$ or migraine$ or cephalalgi$ or "stomach ache$" or "tummy ache$" or "abdominal ache$" or "belly ache$" or earache$ or ear‐ache$ or toothache$ or tooth‐ache$ or odontalgi$ or dysmenorrh$ or neuralgi$).ab,it.
8. exp Pain/
9. Headache/
10. Migraine Headache/
11. Muscle Contraction Headache/
12. 7 or 8 or 9 or 10 or 11
13. 1 and 6 and 12
14 clinical trials/
15 (randomis* or randomiz*).tw.
16 (random$ adj3 (allocat$ or assign$)).tw.
17 ((clinic$ or control$) adj trial$).tw.
18 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw.
19 (crossover$ or "cross over$").tw.
20 random sampling/
21 Experiment Controls/
22 Placebo/
23 placebo$.tw.
24 exp program evaluation/
25 treatment effectiveness evaluation/
26 ((effectiveness or evaluat$) adj3 (stud$ or research$)).tw.
27 or/14‐26
28 13 and 27
Data and analyses
Comparison 1. Treatment versus control (headache) post‐treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Pain | 15 | 644 | Risk Ratio (M‐H, Random, 95% CI) | 2.35 [1.67, 3.30] |
| 1.1.1 N < 20 | 13 | 437 | Risk Ratio (M‐H, Random, 95% CI) | 2.86 [1.73, 4.72] |
| 1.1.2 N > 20 | 2 | 207 | Risk Ratio (M‐H, Random, 95% CI) | 1.88 [1.36, 2.58] |
| 1.2 Disability | 6 | 446 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.56, 0.03] |
| 1.2.1 N < 20 | 2 | 61 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.47, 0.54] |
| 1.2.2 N > 20 | 4 | 385 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.69, ‐0.00] |
| 1.3 Depression | 6 | 400 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.28, 0.11] |
| 1.3.1 N < 20 | 3 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.68, 0.35] |
| 1.3.2 N > 20 | 3 | 297 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.29, 0.17] |
| 1.4 Anxiety | 7 | 439 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.39, 0.17] |
| 1.4.1 N < 20 | 4 | 136 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.54, 0.57] |
| 1.4.2 N > 20 | 3 | 303 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.49, 0.11] |
Comparison 2. Treatment versus control (headache) follow‐up.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Pain | 5 | 223 | Risk Ratio (M‐H, Random, 95% CI) | 2.73 [0.98, 7.63] |
| 2.1.1 N < 20 | 4 | 99 | Risk Ratio (M‐H, Random, 95% CI) | 3.49 [1.31, 9.26] |
| 2.1.2 N > 20 | 1 | 124 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [1.03, 1.52] |
| 2.2 Disability | 3 | 209 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.65, ‐0.10] |
| 2.2.1 N < 20 | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐1.27, 0.36] |
| 2.2.2 N > 20 | 2 | 185 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.65, ‐0.07] |
| 2.3 Depression | 3 | 228 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.62, 0.52] |
| 2.3.1 N < 20 | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.54 [‐1.36, 0.28] |
| 2.3.2 N > 20 | 2 | 204 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.61, 0.83] |
| 2.4 Anxiety | 4 | 271 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.46, 0.21] |
| 2.4.1 N < 20 | 2 | 67 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐1.00, 0.45] |
| 2.4.2 N > 20 | 2 | 204 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.48, 0.41] |
Comparison 3. Treatment versus control (mixed pain) post‐treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Pain | 16 | 1210 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.67, ‐0.19] |
| 3.1.1 N < 20 | 7 | 250 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.83 [‐1.19, ‐0.46] |
| 3.1.2 N > 20 | 9 | 960 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.45, 0.05] |
| 3.2 Disability | 14 | 1226 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.54, ‐0.15] |
| 3.2.1 N < 20 | 6 | 213 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.72 [‐1.17, ‐0.26] |
| 3.2.2 N > 20 | 8 | 1013 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.37, ‐0.04] |
| 3.3 Depression | 8 | 757 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.23, 0.12] |
| 3.3.1 N < 20 | 2 | 59 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.95, 0.41] |
| 3.3.2 N > 20 | 6 | 698 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.21, 0.15] |
| 3.4 Anxiety | 8 | 957 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.29, ‐0.03] |
| 3.4.1 N < 20 | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.57, 0.82] |
| 3.4.2 N > 20 | 7 | 925 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.30, ‐0.04] |
Comparison 4. Treatment versus control (mixed pain) follow‐up.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Pain | 9 | 833 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.30, 0.13] |
| 4.1.1 N < 20 | 2 | 53 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.94 [‐1.75, ‐0.13] |
| 4.1.2 N > 20 | 7 | 780 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.00 [‐0.15, 0.14] |
| 4.2 Disability | 9 | 935 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.49, ‐0.06] |
| 4.2.1 N < 20 | 2 | 53 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.17 [‐2.60, 0.26] |
| 4.2.2 N > 20 | 7 | 882 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.34, ‐0.07] |
| 4.3 Depression | 7 | 667 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.10, 0.28] |
| 4.3.1 N < 20 | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.35, 0.29] |
| 4.3.2 N > 20 | 6 | 643 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.06, 0.30] |
| 4.4 Anxiety | 8 | 875 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.20, 0.18] |
| 4.4.1 N < 20 | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.60, 0.79] |
| 4.4.2 N > 20 | 7 | 843 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.22, 0.19] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abram 2007.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment (3‐month follow‐up), 6 months | |
| Participants | End of treatment: n = 50 Start of treatment: n = 81 Sex: 45 F, 36 M Mean age = 12.7 years (range 10 to 18) Source = hospital and clinic Diagnosis = headache Mean years of pain = not given |
|
| Interventions | "Headache Clinical Model: behavioural intervention" "Headache Traditional Model: consultation with neurologist" |
|
| Outcomes | Primary pain outcome: none Primary disability outcome: Ped‐MIDAS Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: "This study was funded by the Nemours Clinical Management Program, Orlando, FL." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "If the family was interested in the study, they were randomised (using a random number table) to either a TCM appointment or a HCM appointment." Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described, however no significant differences between completers and non‐completers were reported |
| Selective reporting (reporting bias) | High risk | Data were incompletely reported |
Alfven 2007.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment and 1‐year follow‐up | |
| Participants | End of treatment: n = 48 Start of treatment: n = 48 Sex: 35 F, 12 M Mean age = 9.5 years (range 6 to 18) Source = hospital Diagnosis = recurrent abdominal pain Mean years of pain = 2.3 |
|
| Interventions | "Psychological treatment and physiotherapy" "Physiotherapy alone" |
|
| Outcomes | Primary pain outcome: pain score Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: "No conflict of interest...exists." Funding: "No...funding exists." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The children recruited during 1996–1999 were randomised" Comment: probably done, method not described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | High risk | Data were incompletely reported |
Barakat 2010.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment and 12 months | |
| Participants | End of treatment: n = 42; follow‐up 1 year: n = 34 Start of treatment: n = 42 Sex: 12 F, 15 M Mean age = 14.17 years (1.75) Source = sickle cell centre Diagnosis = sickle cell disease Mean years of pain = lifetime |
|
| Interventions | "Pain Management Intervention" "Disease Education Intervention" | |
| Outcomes | Primary pain outcome: pain diary Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: "This research was funded by National Heart, Lung, and Blood Institute (U54 30117 to J.R.)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A 2‐group, randomised treatment design was used." Comment: probably done, method not described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described; no significant differences between completers and non‐completers were reported |
| Selective reporting (reporting bias) | Low risk | Data were fully reported |
Barry 1997.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment, 3 months | |
| Participants | End of treatment: n = 29 Start of treatment: n = 36 Sex: 19 F, 10 M Mean age = 9.4 years Source = volunteers via school and primary healthcare settings; referrals invited from primary and secondary care Diagnosis = headache Mean years of pain not given |
|
| Interventions | "Cognitive behaviour therapy" "waiting‐list control" | |
| Outcomes | Primary pain outcome: headache intensity Primary disability outcome: school absence Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not described Funding: not described |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Each parent‐child pair was initially matched with another pair based on the child's age, sex and headache pain as indicated by the parents' ratings of average duration, frequency, and intensity of headaches. Subsequently, one of each of the matched parent‐child pairs was randomly assigned to either the treatment condition or the waiting‐list control condition." Comment: probably done, method not described |
| Allocation concealment (selection bias) | High risk | "Each parent‐child pair was initially matched with another pair based on the child's age, sex and headache pain as indicated by the parents' ratings of average duration, frequency, and intensity of headaches. Subsequently, one of each of the matched parent‐child pairs was randomly assigned to either the treatment condition or the waiting‐list control condition." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described; no significant differences between completers and non‐completers were reported |
| Selective reporting (reporting bias) | Unclear risk | Data were completely reported on request |
Bussone 1998.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment, 6 months, 12 months | |
| Participants | End of treatment: n = 35 Start of treatment: n = 35 Sex: 17 F, 18 M Mean age = 11.4 years (range 11 to 15) Source = specialised headache clinic Diagnosis = headache Mean years of pain (mean) = 2.6 |
|
| Interventions | "Biofeedback (assisted relaxation)" "Relaxation" |
|
| Outcomes | Primary pain outcome: Pain Index Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: State Trait Anxiety Index
|
|
| Notes | COI: not reported Funding: "Preparation of this research was supported in part by a research grant from the National Institute of Nuerological Disorders and Stroke, NS‐29855." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomly assigned to one of two experimental conditions" Comment: probably done, method not described |
| Allocation concealment (selection bias) | High risk | "... with the constraint that subjects be over‐sampled in BFB‐REL treatment (2:1 ratio) in order to make actual treatment available to as many children as possible." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts reported in study |
| Selective reporting (reporting bias) | High risk | Data incompletely reported |
Chen 2014.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment and post‐treatment. | |
| Participants | End of treatment: n = unknown Start of treatment: n = 90 Sex: 52 F, 38 M Mean age = 11.6 years (SD = 2.0; range 8 to 12) Source = unknown Diagnosis = migraine Mean years of pain (range) = 1 to 4 years |
|
| Interventions | "Standard treatment (0.2 mg/kg of oral flunarizine) + Behavior therapy" "Standard treatment" (0.2 mg/kg of oral flunarizine)" |
|
| Outcomes | Primary pain outcome: Headache frequency Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: none stated Funding: none stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "We adapt prospective randomized controlled study method, where the 90 patients (children) were randomized to control group and treatment group." Comment: unclear randomization procedure |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition in the study was not described |
| Selective reporting (reporting bias) | High risk | Not all data was included in the paper |
Cottrell 2007.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment, and 8 months | |
| Participants | End of treatment: n = 30, follow‐up n = 28 Start of treatment: n = 34 Sex: 15 F, 15 M Mean age: 14.1 years (SD 1.91) Source: referral by neurologist and community advertisement Diagnosis: headache Duration (mean): unknown | |
| Interventions | "STOP Migraines treatment" ‐ behavioural treatment delivered via telephone Triptan treatment | |
| Outcomes | Primary pain outcome: none Primary disability outcome: hours disabled by headache Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | Funding source: National Institutes of Health (NINDS #N32374) Declarations of interest: Dr. O'Donnell was an employee of OrthoNeuro Inc. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Thus, 34 adolescents were randomized to treatment (16 TT and 18 TAT)." Comment: probably done; description of randomisation not provided |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition completely reported; significant differences between completers and non‐completers were not reported |
| Selective reporting (reporting bias) | High risk | Outcomes incompletely reported |
Daniel 2015.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed pretreatment and post‐treatment (6 months) | |
| Participants | End of treatment: n = 62 Start of treatment: n = 83 Sex of children: 42 M, 41 F Mean age of children = 8.48 years (± 2.11) Source = two comprehensive sickle cell clinics in children’s hospitals Diagnosis = sickle cell disease Mean years of illness = lifetime |
|
| Interventions | "Families Taking Control" (PSST) "Delayed Intervention Control" |
|
| Outcomes | Primary pain outcome: none Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: "Conflicts of interest: None declared." Funding: "NHLBI (U54 HL070585) to M.S. (PI), BTRP to LPB (PI); and NCMHD (1RC1MD004418) to L.P.B. (PI)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomization (stratified by gender in blocks of 10) was concealed from the family and the study team until after completing the baseline assessment when an envelope with randomization status was opened and the family was informed of next steps." Comment: insufficient information about the sequence generation process to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | "Randomization (stratified by gender in blocks of 10) was concealed from the family and the study team until after completing the baseline assessment when an envelope with randomization status was opened and the family was informed of next steps." Comment: insufficient information about allocation concealment provided to permit judgement; it was unclear if envelopes were sequentially numbered, opaque, and sealed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement; no statement about whether or not blinding of outcome assessment occurred |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was reported, no significant differences between completers and non‐completers were reported |
| Selective reporting (reporting bias) | Low risk | Data were fully reported |
Duarte 2006.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment | |
| Participants | End of treatment: n = 32 Start of treatment: n = 32 Sex: 22 F, 10 M Mean age = 9.1 years (SD 2.1) Source = paediatric gastroenterology service Diagnosis = recurrent abdominal pain Mean years of pain = 2.1 |
|
| Interventions | "Cognitive behavioural family intervention" "Standard paediatric care, 4 sessions" |
|
| Outcomes | Primary pain outcome: pain intensity VAS Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly allocated to 2 groups." Comment: probably done, method not described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts were reported in the study |
| Selective reporting (reporting bias) | High risk | Data were incompletely reported |
Fichtel 2001.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment, 8 to 12 months | |
| Participants | End of treatment: n = 36 Start of treatment: n = 36 Sex: 25 F, 11 M Mean age = 15.4 years (range 13 to 18) Source = school Diagnosis = headache Mean years of pain = not given |
|
| Interventions | "Relaxation" "waiting‐list control" |
|
| Outcomes | Primary pain outcome: total headache score Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The subjects were randomly assigned to the relaxation treatment or waiting‐list groups" Comment: probably done, no method was described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts were reported in the study |
| Selective reporting (reporting bias) | Low risk | Data were fully reported |
Gil 1997.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment | |
| Participants | End of treatment: n = 49 Start of treatment: n = 49 Sex: 23 F, 26 M Mean age = 11.9 years Source = university medical centre, sickle cell centre Diagnosis = sickle cell anaemia (SS), sickle cell disease (SC), sickle beta thalassaemia Mean years of pain = not given |
|
| Interventions | "Cognitive coping skills" "Standard care control" |
|
| Outcomes | Primary pain outcome: none Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: "This work was supported by Grant RO1 HL46953‐06, by Project VI.B.2 in the Duke University‐University of North Carolina Sickle Cell Center Grant in P60HL2839‐13, and by the University of North Carolina at Chapel Hill GCRC Grant RR00046." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Participants were then randomly assigned to one of two conditions." Comment: probably done, method not described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts reported in study |
| Selective reporting (reporting bias) | High risk | Data not fully reported |
Greenley 2015.
| Study characteristics | ||
| Methods | RCT. 3 Arms. Assessed pretreatment, after initial treatment (12 weeks), after additional treatment (20 weeks) | |
| Participants | End of treatment (12 weeks): n = 65; end of treatment (20 weeks): n = 65 Start of treatment: n = 76 Sex of children: 46 M, 30 F Sex of parents: not reported Mean age of children = 14.54 ± 1.84 years Mean age of parents = not reported Source = Paediatric IBD Center Diagnosis = inflammatory bowel disease Mean years of illness = not reported | |
| Interventions | "PSST IBD" "Wait‐list control" | |
| Outcomes | Primary pain outcome: none Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | Funding: "Supported by the Crohn’s and Colitis Foundation of America (Senior Research Award #2838; PI: Greenley)." COI: "The authors have no conflicts of interest to disclose." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The randomization sequence was generated by a biostatistician using Windows version 6.0 of randomization program 'Rand.exe.'" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | "The random allocation sequence was stored electronically in a password‐protected file accessible only to the research assistant in charge of informing participants of randomization outcomes. Research assistants enrolling participants and those conducting assessment visits were blind to participant intervention condition." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "All assessments were conducted in participants' homes...Research assistants...conducting assessment visits were blind to participant intervention condition." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was reported but differences between completers and non‐completers are not reported |
| Selective reporting (reporting bias) | Unclear risk | All data reported |
Griffiths 1996.
| Study characteristics | ||
| Methods | RCT. 3 arms. Assessed at pretreatment, post‐treatment and 9 weeks post‐treatment | |
| Participants | End of treatment: n = 42; follow‐up: n = 42 Start of treatment: n = 51 Sex: 21 F, 21 M Mean age = 11.3 years Source = not known Diagnosis = migraine Mean years of pain = not given: minimum 6 months |
|
| Interventions | "Cognitive behavioural therapy (clinic‐based)" (n = 15) "Cognitive behavioural therapy (home‐based)" (n = 15) "Self monitoring" (n = 12) | |
| Outcomes | Primary pain outcome: headache index Primary disability outcome: none Primary depression outcome: Child Depression Scale Primary anxiety outcome: Child Manifest Anxiety Scale (CMAS)
|
|
| Notes | COI: not reported Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "It was decided to assign children to groups by true randomisation rather than on the basis of headache diagnosis" Comment: probably done, no method was described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition was not described |
| Selective reporting (reporting bias) | Low risk | Data were fully reported |
Grob 2013.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed pretreatment, post‐treatment and at 3 months | |
| Participants | End of treatment: n = 28; follow‐up: n = 28 Start of treatment: n = 29 Sex: 25 F, 4 M Mean age = 9.6 years (SD = 1.47) Source = schools Diagnosis = chronic abdominal pain Mean years of pain = 2.8 years (SD = 1.71) |
|
| Interventions | "Stop the pain with Happy Pingu" CBT "Wait‐list control" |
|
| Outcomes | Primary pain outcome: pain intensity Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: "There are no conflicts of interest." Funding: "This work was supported by a grant to M. G. of Potsdam Graduate School." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Computer‐aided randomization was performed by a person who was not involved in the study" Comment: probably done, no method was described |
| Allocation concealment (selection bias) | Low risk | "Computer‐aided randomization was performed by a person who was not involved in the study" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described; differences between completers and non‐completers were not described |
| Selective reporting (reporting bias) | Low risk | Data were fully reported |
Gulewitsch 2013.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed pretreatment, post‐treatment (3 months) | |
| Participants | End of treatment: n = 37 Start of treatment: n = 38 Sex: 24 F, 14 M Mean age = 9.4 years (SD = 1.72) Source = adverts in local newspapers and paediatricians' offices Diagnosis = functional abdominal pain or irritable bowel syndrome Mean years of pain = 34.84 months (SD = 40.7) |
|
| Interventions | "Hypnotherapeutic therapy" (hypnotherapeutic and behavioural methods) "Wait‐list control group" |
|
| Outcomes | Primary pain outcome: mean pain intensity Primary disability outcome: Paediatric Pain Disability Index Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: "The authors declare that they have no conflict of interest." Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Families were randomly assigned following simple randomization procedures (computerized random number generator)" Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described; differences between completers and non‐completers were not described |
| Selective reporting (reporting bias) | Low risk | Data fully reported |
Hechler 2014.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed pretreatment, post‐treatment, 6 months, and 12 months | |
| Participants | End of treatment: n = 108 Start of treatment: n = 120 Sex: 87 F, 27 M Mean age = 14 years (SD 2.85) Source = clinic Diagnosis = chronic pain (mixed conditions) Mean years of pain = median of 18 months (intervention group) and 13.5 months (control group) |
|
| Interventions | "Intensive interdisciplinary pain treatment" "Wait‐list control" |
|
| Outcomes | Primary pain outcome: mean pain intensity Primary disability outcome: Paediatric Pain Disability Index Primary depression outcome: Depression Inventory for Children and Adolescents (DIKJ) Primary anxiety outcome: Pain‐Related Cognitions Questionnaire for Children (catastrophising subscale)
|
|
| Notes | COI: "The authors declare no conflict of interest." Funding: "The present study was supported in part by the Robert Bosch Foundation GmbH (Grant 11.5.1344.0010.0). The Robert Bosch Foundation was not involved in (1) the study design; (2) collection, analysis, and interpretation of data; (3) the writing of the report; and (4) the decision to submit the paper for publication." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomisation was conducted with a 1:1 approach and in blocks of 4 and blocks or 6 for both groups and was stratified for gender" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | "The individual who carried out the randomization procedure was blinded to the treatment condition" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described; differences between completers and non‐completers were not described |
| Selective reporting (reporting bias) | Unclear risk | Data fully reported on request |
Hickman 2015.
| Study characteristics | ||
| Methods | RCT. Two arms. Assessed pretreatment and post‐treatment. | |
| Participants | End of treatment: n = 32 Start of treatment: n = 36 Sex: 87 F, 27 M Mean age = 14 years (SD 2.85) Source = clinic Diagnosis = chronic pain (mixed conditions) Mean years of pain = unknown |
|
| Interventions | "COPE‐HEP; Creating Opportunities for Personal Empowerment ‐ Headache Education Program" "Treatment‐as‐usual" |
|
| Outcomes | Primary pain outcome: none Primary disability outcome: Ped‐MIDAS Primary depression outcome: Beck Youth Inventory II, Depressive symptoms Primary anxiety outcome: Beck Youth Inventory II, Anxiety symptoms
|
|
| Notes | COI: The authors report no financial incentives that may create a conflict of interest." Funding: "This research was supported by a grant from the National Institute of Nursing Research/National Institutes of Health (1F31NR012112‐01A1)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Adolescents were randomized to the COPE‐HEP intervention or a comparison headache education group." Comment: no method described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was reported but differences between completers and non‐completers were not described |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
Humphreys 2000.
| Study characteristics | ||
| Methods | RCT. 4 arms. Assessed at pretreatment, post‐treatment | |
| Participants | End of treatment: n = 61 Start of treatment: n = 64 Sex: 38 F, 26 M Mean age = 9.8 years (SD 2.5) Source = advertisement and physician referral Diagnosis = recurrent abdominal pain Mean years of pain = none given |
|
| Interventions | "CBT + biofeedback + parental support + fibre" "CBT + biofeedback + fibre" "Biofeedback + fibre" "Fibre" |
|
| Outcomes | Primary pain outcome: pain diary Primary disability outcome: school attendance Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: none stated.Funding: none stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomly assigned to one of the four groups" Comment: probably done, method not described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition not described; significant differences between completers and non‐completers not reported |
| Selective reporting (reporting bias) | Low risk | Data fully reported |
Kashikar‐Zuck 2005.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment (week 8), 6 weeks | |
| Participants | End of treatment: n = 27 Start of treatment: n = 30 Sex: 30 F, 0 M Median age = 15.8 years (SD 1.3) Source = paediatric rheumatology clinic of a children's hospital Diagnosis = juvenile primary fibromyalgia (JPFM criteria; Yunus) Mean years of pain = 19 for > 2 years, 11 for 6 months to 2 years |
|
| Interventions | "Coping skills training" "Self‐monitoring" |
|
| Outcomes | Primary pain outcome: average pain VAS Primary disability outcome: Functional Disability Inventory Primary depression outcome: Children's Depression Inventory Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: "Supported by grants from the Cincinnati Children’s Hospital Research Foundation and National Institutes of Health Grant 1P60AR47784‐01." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A computer generated pseudo‐random number list was used. A simple randomisation technique was used with a 1:1 allocation ratio for 30 subjects as a single block." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | "A computer generated pseudo‐random number list was used. A simple randomisation technique was used with a 1:1 allocation ratio for 30 subjects as a single block." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "A research assistant who was blind to the study objectives and to the subjects' treatment assignment administered the self‐report measures. The rheumatologist or occupational therapist who conducted the tender point assessments was blind to the subjects' treatment assignment." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition is described, however significant differences between completers and non‐completers were not reported |
| Selective reporting (reporting bias) | Low risk | Data were fully reported on request for additional data |
Kashikar‐Zuck 2012.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed pretreatment, post‐treatment, 6‐month follow‐up | |
| Participants | End of treatment: n = 106; follow‐up 6 months n = 100 Start of treatment: n = 114 Sex: 105 F, 9 M Mean age = 15.0 years (1.8) Source = paediatric rheumatology centres in Midwestern USA Diagnosis = fibromyalgia syndrome Mean years of pain = 2 years, 10 months (2 years, 6 months) |
|
| Interventions | "Cognitive behavioural therapy" "Fibromyalgia education" | |
| Outcomes | Primary pain outcome: pain severity VAS (averaged over 7 days) Primary disability outcome: Functional Disability Scale Primary depression outcome: Children's Depression Inventory Primary anxiety outcome: Pain Coping Questionnaire
|
|
| Notes | COI: "Dr. Passo has received consulting fees, speaking fees, and/or honoraria from Pfizer (less than $10,000)." Funding: "Supported by the NIH (National Institute of Arthritis and Musculoskeletal and Skin Diseases grant R01‐AR‐050028 to Dr. Kashikar‐Zuck)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Eligible patients were randomly assigned to 1 of the 2 treatment arms based upon a computer‐generated randomisation list. Randomisation was stratified by site." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | "When a patient was enrolled, the study therapist contacted the biostatistician to obtain the subject identification number and treatment allocation." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The principal investigator, study physicians, study coordinator, and assessment staff were all blinded to the patients' treatment condition throughout the trial. Patients were asked not to divulge what treatment they were receiving to the study physician." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was described; no significant differences between completers and non‐completers were reported |
| Selective reporting (reporting bias) | Low risk | Data were fully reported |
Kroener‐Herwig 2002.
| Study characteristics | ||
| Methods | RCT. 3 arms. Assessed at pretreatment, post‐treatment, 6 months | |
| Participants | End of treatment: n = 75 Start of treatment: n = 78 Sex: 35 F, 40 M Mean age = 12.1 years (SD 1.3) Source = newspaper advertisement ‐ 2 or more headaches per month reported by parents Diagnosis = paediatric headache: migraine (30%), tension‐type (40%), combined (30%) Mean years of pain = 4.0 (SD 2.6) |
|
| Interventions | "Cognitive behavioural training group" (n = 29) "Self‐help" (n = 27) "Waiting‐list control" (n = 19) |
|
| Outcomes | Primary pain outcome: pain intensity Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: "The study was supported by a grant from the Technician’s Health Care Insurance of Germany (Technikerkrankenkasse)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Assignment to the treatment groups was random." Comment: probably done, method not described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described, however significant differences between completers and non‐completers were not reported |
| Selective reporting (reporting bias) | Low risk | Data were fully reported |
Labbe 1984.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment (1 month after end of treatment), 6 months | |
| Participants | End of treatment: n = 28 Start of treatment: n = 28 Sex: 14 F, 14 M Mean age = 10.8 years Source = community paediatrician referral, newspaper advertisement Diagnosis = migraine headache Mean years of pain = 4.3 |
|
| Interventions | "Autogenic feedback training" "waiting‐list control" | |
| Outcomes | Primary pain outcome: headache diary Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The children who attended the first session were matched on age, sex, and baseline headache index and then randomly assigned to either a treatment group or waiting‐list control group." Comment: probably done, method not described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts reported in study |
| Selective reporting (reporting bias) | Low risk | Data were reported fully |
Labbe 1995.
| Study characteristics | ||
| Methods | RCT. 3 arms. Assessed at pretreatment, post‐treatment, 6 months | |
| Participants | End of treatment: n = 30 Start of treatment: n = 46 Sex: 17 F, 13 M Mean age = 12.0 years Source = not given Diagnosis = vascular or migraine headache Mean years of pain = not given |
|
| Interventions | "Skin temperature biofeedback and autogenic relaxation" "Autogenic relaxation" "Waiting‐list control" | |
| Outcomes | Primary pain outcome: headache diary Primary disability outcome: none Primary depression outcome: Childhood Depression Inventory Primary anxiety outcome: How‐I‐Feel questionnaire
|
|
| Notes | COI: not reported Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Children were matched by age, sex, and baseline headache activity and then randomly assigned to one of three groups." Comment: probably done, no method described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Data on the dropouts were compared to those children participating in the treatment sessions. No differences were found in sex, age or headache history." Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Data were fully reported |
Larsson 1987a.
| Study characteristics | ||
| Methods | RCT. 3 arms. Assessed at pretreatment, post‐treatment, 5 months | |
| Participants | End of treatment: n = 41 Start of treatment: n = 46 Sex: 40 F, 6 M Mean age = not given: range 16 to 18 years Source = not given Diagnosis = headache (migraine, tension, or both) Mean years of pain = mostly 1 to 5 years |
|
| Interventions | "Therapist assisted relaxation" (n = 14) "Self‐help relaxation" (n = 16) "Self monitoring group" (n = 11) |
|
| Outcomes | Primary pain outcome: headache sum Primary disability outcome: school absence Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "In the randomisation procedure" Comment: probably done, no method described |
| Allocation concealment (selection bias) | High risk | "In the randomisation procedure the following restrictions were applied: (a) class mates were assigned to the same treatment group in order to lessen the risk of treatment contamination, (b) subjects were evenly distributed across groups within separate schools." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described, however significant differences between completers and non‐completers were not reported |
| Selective reporting (reporting bias) | High risk | Data were not fully reported |
Larsson 1987b.
| Study characteristics | ||
| Methods | RCT. 3 arms. Assessed at pretreatment, post‐treatment, 5 months | |
| Participants | End of treatment: n = 36; follow‐up: n = 34 Start of treatment: n = 36 Sex: 32 F, 2 M Mean age = 17 years Source = not given Diagnosis = headache Mean years of pain = mostly 1 to 5 years |
|
| Interventions | "Self‐help relaxation" (n = 12) "Problem discussion group" (n = 10) "Self monitoring (control)" (n = 12) | |
| Outcomes | Primary pain outcome: headache sum Primary disability outcome: school absence Primary depression outcome: Depression Scale for Female Adolescents Primary anxiety outcome: Swedish translation of Children's Manifest Anxiety Scale
|
|
| Notes | COI: not reported Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Finally, 36 students were randomly assigned to the three experimental conditions." Comment: probably done, no method described |
| Allocation concealment (selection bias) | High risk | "The allocation of subjects was conducted with two restrictions on the procedure: (a) Classmates were assigned to the same treatment condition (to lessen the risk of treatment contamination), and (b) students with a high frequency of headaches were identified and evenly distributed across groups." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition was not described |
| Selective reporting (reporting bias) | High risk | Data were not fully reported |
Larsson 1990.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment | |
| Participants | End of treatment: n = 43 Start of treatment: n = 49 Sex: 44 F, 5 M Mean age = 17 years Source = school Diagnosis = headache Mean years of pain = median 2 to 5 years | |
| Interventions | “Self help relaxation” “Waiting‐list control” | |
| Outcomes | Primary pain outcome: headache activity Primary disability outcome: none given Primary depression outcome: Beck Depression Inventory Primary anxiety outcome: Modified Child Manifest Anxiety Scale
|
|
| Notes | COI: none stated. Funding: none stated. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “...the outlines of the study including the use of randomisation and a placebo treatment period.” Comment: probably done, method not described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | “A graduate student in psychology administered the assessment instruments and the treatment material used in the study.” Comment: unsure |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described, however significant differences between completers and non‐completers were not reported |
| Selective reporting (reporting bias) | Low risk | Data were fully reported |
Larsson 1996.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment, 6 months | |
| Participants | End of treatment: n = 26 Start of treatment: n = 26 Sex: 25 F, 1 M Mean age = not given: range 10 to 15 years Source = school Diagnosis = headache Mean years of pain = 2.1 |
|
| Interventions | "Relaxation treatment" "No treatment" | |
| Outcomes |
Primary pain outcome: headache intensity Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: "This study was supported by grants from the First May Flower Annual Campaign and from the Glaxo and Allenburys AB, Sweden." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Thus, 26 pupils were randomly allocated into a relaxation training group or to a no‐treatment control group". Comment: probably done, no method described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no dropouts reported in the study |
| Selective reporting (reporting bias) | Low risk | Data were fully reported |
Levy 2010.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment, 3‐month follow‐up, 6‐month follow‐up | |
| Participants | End of treatment: n = 168; follow‐up 3 months: n = 143; follow‐up 6 months: n = 154 Start of treatment: n = 200 Sex: 145 F, 55 M Mean (SD) age = 11.21 years (2.55) Source = paediatric gastroenterology clinics at Seattle Children's Hospital and the Atlantic Health System in Morristown, New Jersey. Seattle participants were also recruited through local area clinics and community‐posted flyers Diagnosis = functional abdominal pain Mean years of pain = 3+ episodes of abdominal pain during a 3‐month period |
|
| Interventions | "Cognitive‐behavioural treatment" "Educational intervention" | |
| Outcomes | Primary pain outcome: Faces Pain Scale‐Revised Primary disability outcome: Functional Disability Inventory Primary depression outcome: Children's Depression Inventory Primary anxiety outcome: Multidimensional Anxiety Scale for Children
|
|
| Notes | COI: "William E. Whitehead is a member of the Board of Directors of the Rome Foundation. Nader Youssef is currently the Director of Clinical Research at AstraZeneca LP. At the time the study was conducted, however, he was not affiliated with this company and contributed to the project by his appointment at Goryeb Children’s Hospital." Funding: "This study was supported by grant number 5R01HD036069 from the National Institutes of Health — National Institute of Child Health and Human Development." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomisation was then performed by a different researcher using a computerised random‐number generator, stratifying by age." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | "Randomisation was then performed by a different researcher using a computerised random‐number generator, stratifying by age." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Nurse assessors were blind to the treatment assignment of the children." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described; significant differences between completers and non‐completers are not reported |
| Selective reporting (reporting bias) | Unclear risk | Data were fully reported when requested |
Levy 2016.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment, 3 months, 6 months, and 12 months | |
| Participants | End of treatment: n = 158; follow‐up 3 months: n = 137; follow‐up 6 months: n = 144, follow‐up 12 months: n = 133 Start of treatment: n = 185 Sex: 87 F, 98 M Mean age = 13.5 years (SD = 2.7) Source = paediatric GI clinics Diagnosis = Crohn's disease or ulcerative colitis Mean years of pain = not reported |
|
| Interventions | "Social learning cognitive‐behavioral therapy" "Education support" |
|
| Outcomes | Primary pain outcome: none Primary disability outcome: Functional Disability Inventory Primary depression outcome: Children's Depression Inventory Primary anxiety outcome: Multidimensional Anxiety Scale for Children
|
|
| Notes | COI: "The authors have no conflict of interest to disclose." Funding: "Supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (award number R01HD050345 to R. L. Levy)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was then performed by a different researcher using a computerized random‐number generator, stratifying by age (7–11 or 12–18 years old) and then by physician‐reported disease severity (quiescent, mild, or moderate/severe based on either the Pediatric Ulcerative Colitis Activity Index (PUCAI) for patients with UC or the Pediatric Crohn’s Disease Activity Index (PCDAI) for Crohn’s patients) completed during enrolment." Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | No description Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "At all assessment points, parents completed questionnaires online or by mail (whichever modality they preferred). Children completed assessments through a scheduled telephone call with a highly trained research nurse who was blinded to the participant’s treatment assignment." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described; significant differences between completers and non‐completers were not reported |
| Selective reporting (reporting bias) | Low risk | Data were fully reported. |
Levy 2017.
| Study characteristics | ||
| Methods | RCT. 3 arms (only 2 arms included here, see Interventions below). Assessed at pretreatment, 1 week, 3 months, and 6 months after treatment. | |
| Participants | End of treatment: n = 166 children; 170 parents. 3 month follow‐up: n = 160 children; 164 parents. 6 months follow‐up: n = 159 children; 164 parents. Start of treatment: n = 216 Child Sex: 140 F, 76 M; Parent Sex: 205 F, 11 M Child mean age = 9.4 years (SD = 1.7); parent mean age = 39.8 years (7.7) Source = paediatric GI clinics Diagnosis = functional abdominal pain Mean years of pain = not reported |
|
| Interventions | "Social learning cognitive‐behavioral therapy (face‐to‐face)" "Social learning cognitive‐behavioral therapy‐Remote (delivered via the telephone)" ‐ this condition was excluded from this review. See Fisher 2015 for remotely‐delivered psychological interventions. "Education support" |
|
| Outcomes | Primary pain outcome: Abdominal Pain Index‐ Severity Primary disability outcome: Functional Disability Inventory (parent report) Primary depression outcome: None Primary anxiety outcome: Pain Response Inventory ‐ Catastrophizing subscale
|
|
| Notes | COI: "The authors have no conflicts of interest relevant to this article to disclose." Funding: "This study was supported by award R01HD36069‐0981 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R.L.L.)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization using a computer‐generated randomization sequence occurred after baseline assessments, stratified by child gender and baseline parent‐reported child pain severity scores on the Abdominal Pain Index (API) (scores at or above 1.75 [the median value from our previous study] vs below)" Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | "After enrolment and completion of baseline assessments, the study coordinator queried the randomization database for treatment assignment and then scheduled sessions with the
participant." Comment: unclear allocation concealment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Parents completed questionnaires online or by mail (90.5% online). Children completed assessments through a telephone call with a trained interviewer blinded to study hypotheses and treatment assignment." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data attrition fully reported. Differences between completers and non‐completers of the study |
| Selective reporting (reporting bias) | Low risk | All data was reported |
McGrath 1988.
| Study characteristics | ||
| Methods | RCT. 3 arms. Assessed at pretreatment, post‐treatment, 3 months, 12 months | |
| Participants | End of treatment: n = 99 Start of treatment: n = 136 Sex: 69 F, 30 M Mean age = 13.1 years (range 11 to 18) Source = hospital Diagnosis = headache Mean years of pain = not given: minimum 3 months |
|
| Interventions | "Relaxation training" "Attention control" "Own best efforts" | |
| Outcomes | Primary pain outcome: headache index Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: "Research supported by the Ontario Ministry of Health, Ontario Ministry of Community and Social Services and the Children's Hospital of Eastern Ontario. Dr. McGrath is supported by a Career Scientist Award of the Ontario Ministry of Health." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly assigned to one of three groups" Comment: probably done, no method described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was described, however significant differences between completers and non‐completers were not reported |
| Selective reporting (reporting bias) | Low risk | Data were completely reported |
McGrath 1992.
| Study characteristics | ||
| Methods | RCT. 3 arms. Assessed at pretreatment, post‐treatment, 3 months, and 1‐year follow‐up | |
| Participants | End of treatment: n = 74 Start of treatment: n = 87 Sex: 63 F, 24 M Mean age = not given: range 11 to 18 years Source = paediatricians and family physicians Diagnosis = migraine Mean years of pain not given: minimum 3 months |
|
| Interventions | "Therapist administered cognitive behavioural/stress coping/relaxation training" "Self‐administered cognitive behavioural/stress coping/relaxation training" "Information and support" |
|
| Outcomes | Primary pain outcome: headache diary Primary disability outcome: none Primary depression outcome: Poznanski Depression Scale Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: "This research was funded by the National Health and Welfare Research and DeveIopment Program of Canada. Dr. McGrath was supported by a Career Scientist Award of the Ontario Ministry of Health." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomised to 1 of the 8‐week treatments" Comment: probably done, no method described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described, however significant differences between completers and non‐completers were not reported |
| Selective reporting (reporting bias) | High risk | Data were incompletely reported |
Osterhaus 1997.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment and 1‐year follow‐up | |
| Participants | End of treatment: n = 39, 1‐year follow‐up: n = 21 Start of treatment: n = 39 Sex: 29 F, 10 M Mean age = 15.2 years (SD 3.3) Source = newspaper article Diagnosis = headache (migraine, tension‐type, mixed) Mean years of pain = 5.6 |
|
| Interventions | "Behavioural treatment package" "waiting‐list control" | |
| Outcomes | Primary pain outcome: headache index Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported. Funding: "This study was supported by Iht: Dutch Fund for Menial Hcalqh (NFGV)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The participants were randomly assigned to one of two groups" Comment: probably done, no method described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition was not described |
| Selective reporting (reporting bias) | Low risk | Data were fully reported |
Palermo 2016.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment and 3 month follow‐up | |
| Participants | End of treatment: n = 60, 3 month follow‐up: n = 59 Start of treatment: n = 61 Child sex: 49 F, 11 M Parent sex: 60 F, 1 M Child mean (SD) age = 14.07 years (1.80) Source = pain clinic Diagnosis = mixed chronic pain conditions Mean years of pain = unknown |
|
| Interventions | "Problem‐solving skills training" "Treatment‐as‐usual" |
|
| Outcomes | Primary pain outcome: Child pain intensity Primary disability outcome: Physical disability (BAPQ) Primary depression outcome: Depression (BAPQ) Primary anxiety outcome: General anxiety (BAPQ)
|
|
| Notes | COI: "The authors have no conflicts of interest to declare." Funding: "Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R21HD065180 (PI: T. M. P.)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A fixed allocation randomization scheme was used. The order of randomization to the 2 treatment conditions was generated separately for each site with an online program (randomizer.org). A blocked method design was used, with blocks of 4 for each identification number" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | "Only the research coordinator had the password to the randomization table. Group assignment was concealed by formatting the document to block out group assignment until the time of randomization." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "All study assessments were self‐report measures completed in participants’ homes through mailings; children and parents were instructed to complete the measures independently." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was fully reported and there were no differences between completers and non‐completers |
| Selective reporting (reporting bias) | Low risk | All data were fully reported |
Passchier 1990.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment | |
| Participants | End of treatment: n = 119 Start of treatment: n = 119 Sex: 65 F, 54 M Mean age = 13.7 years (SD 1.4) Source = school Diagnosis = headache (at least weekly) Mean years of pain = none given |
|
| Interventions | "Progressive relaxation training" "Placebo physical concentration training" | |
| Outcomes | Primary pain outcome: headache intensity Primary disability outcome: school problems Primary depression outcome: none Primary anxiety outcome: Fear of Failure
|
|
| Notes | COI: not reported Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The 19 classes of the participating teachers were allocated at random to a Progressive Relaxation Training or a Placebo Training group." Comment: probably done, no method described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts were reported |
| Selective reporting (reporting bias) | High risk | Data were incompletely reported |
Powers 2013.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed pretreatment, post‐treatment, and 12 months | |
| Participants | End of treatment: n = 124 Start of treatment: n = 135 Sex: 107 F, 28 M Mean age = 14.4 years (SD 2.0) Source = clinic Diagnosis = migraine Mean years of pain = none given |
|
| Interventions | "Cognitive behavioral therapy plus amitriptyline" "Headache education plus amitriptyline" |
|
| Outcomes | Primary pain outcome: headache frequency Primary disability outcome: Ped‐MIDAS Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: "The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported." Funding: "Funding was provided by grant R01NS05036 from the National Institute of Neurological Disorders and Stroke (Dr Powers), grant 8 UL1 TR000077 from the National Center for Research Resources and the National Center for Advancing Translational Sciences, and grant T32DK063929 from the National Institute of Diabetes and Digestive and Kidney Diseases for some of the postdoctoral fellows who contributed to the trial (Dr Powers, program director). Amitriptyline, which was provided without cost to participants, was purchased using National Institutes of Health grant funds and managed by the investigational pharmacy at Cincinnati Children’s Hospital Medical Center. If prevention drug was clinically prescribed during the 12‐month follow‐up period, families had financial responsibility for the medications as with typical clinical practice." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Block randomization (with varying block sizes of 4‐10) was used, and participants were stratified by age. Randomization was computer generated and supplied via secure e‐mail to the study therapist." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | "Randomization was computer generated and supplied via secure e‐mail to the study therapist." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Outcome assessments were conducted by blinded study personnel." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described, however significant differences between completers and non‐completers were not described |
| Selective reporting (reporting bias) | Unclear risk | Data fully reported on request |
Richter 1986.
| Study characteristics | ||
| Methods | RCT. 3 arms. Assessed at pretreatment, post‐treatment | |
| Participants | End of treatment: n = 43 Start of treatment: n = 51 Sex: 34 F, 17 M Mean age = 12.9 years Source = referred by physicians to children's hospital Diagnosis = migraine Mean years of pain = not given: mostly over 2 years |
|
| Interventions | "Relaxation training" "Cognitive coping" "Attention control" | |
| Outcomes | Primary pain outcome: headache diary Primary disability outcome: none Primary depression outcome: Child Depression Rating Scale Primary anxiety outcome: State Trait Anxiety Inventory
|
|
| Notes | COI: not reported Funding: "This research was supported by grants from the Ontario Ministry of Health and the Ontario Ministry of Community and Social Services." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "... and randomly assigned to treatment" Comment: probably done, no method described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Over the course of treatment there were 8 drop‐outs. A chi‐square analysis comparing attrition rates across interventions was not significant." Comment: attrition adequately reported and no significant differences between completers and non‐completers reported |
| Selective reporting (reporting bias) | High risk | Data were incompletely reported |
Robins 2005.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment (3 months after start), 6 to 12 months | |
| Participants | End of treatment: n = 69 Start of treatment: n = 86 Sex: 39 F, 30 M Mean age = 11.4 years (SD 2.4) Source = paediatric gastroenterology outpatient clinic of children's hospital Diagnosis = recurrent abdominal pain Mean years of pain = not stated |
|
| Interventions | "Short term cognitive behavioural family treatment plus standard medical care" "Standard medical care" |
|
| Outcomes | Primary pain outcome: Abdominal Pain Index Primary disability outcome: Functional Disability Inventory Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported. Funding: "This study was supported in part by a grant through the Nemours Research Programs, awarded to the first author." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The remaining sample of 86 were randomly assigned using a coin‐flip method." Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described, however significant differences between completers and non‐completers were not described |
| Selective reporting (reporting bias) | High risk | Data were incompletely reported |
Sanders 1994.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment, 6 months, 1 year | |
| Participants | End of treatment: n = 44 Start of treatment: n = 44 Sex: 28 F, 16 M Mean age = 9.2 years (SD 1.9) Source = not given Diagnosis = recurrent abdominal pain Mean years of pain = 3.7 |
|
| Interventions | "Cognitive behaviour therapy" "Standard paediatric care" | |
| Outcomes | Primary pain outcome: pain diary Primary disability outcome: interference with child activity Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: "This study was supported by Grant 53091 from the National Health and Medical Research Council of Australia to Matthew R. Sanders, Ross W. Shepherd, and Geoggery Cleghorn." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The study used a randomised group comparison design with two treatment conditions." Comment: method not described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition was not described and significant differences between completers and non‐completers were not reported |
| Selective reporting (reporting bias) | High risk | Data were incompletely reported |
Sartory 1998.
| Study characteristics | ||
| Methods | RCT. 3 arms. Assessed at pretreatment, post‐treatment (4 weeks after end of intervention), 8 months follow‐up | |
| Participants | End of treatment: n = 43 Start of treatment: n = 43 Sex: 17 F, 26 M Mean age = 11.3 years (SD 2.1) Source = outpatient clinic of paediatric hospital and advertising in press Diagnosis = migraine Mean years of pain = 4.6 |
|
| Interventions | "Cephalic vasomotor training + stress management" "Relaxation training + stress management" "Beta‐blocker (metoprolol)" |
|
| Outcomes | Primary pain outcome: headache index Primary disability outcome: none Primary depression outcome: mood faces scale Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: "This study was supported by the Bundesminister fuÈ r Forschung und Technologie (BMFT; Federal Minister for Research and Technology, Germany)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Children were allocated randomly to one of three treatment groups" Comment: probably done, no method described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described, however significant differences between completers and non‐completers were not described |
| Selective reporting (reporting bias) | Low risk | Data were fully reported |
Scharff 2002.
| Study characteristics | ||
| Methods | RCT. 3 arms. Assessed at pretreatment, post‐treatment, 3 months, 6 months, 12 months | |
| Participants | End of treatment: n = 34 Start of treatment: n = 36 Sex: 24 F, 12 M Mean age 12.8 years (SD 2.4) Source = children's hospital Diagnosis = migraine (all), tension‐type headache (minority) Mean years of pain = 2.4 (SD 2.1) |
|
| Interventions | "Handwarming biofeedback and stress management" "Handcooling attention control" "Waitlist control" |
|
| Outcomes | Primary pain outcome: headache index Primary disability outcome: none Primary depression outcome: Child Depression Inventory Primary anxiety outcome: State Trait Anxiety Inventory for Children
|
|
| Notes | COI: not reported Funding: "This research was supported by grants from the University of Pittsburgh Anethesiology and Critical Care Foundatation, the Raymond and Elizabeth Bloch Educational and Charitable Foundation, and the NIH/NICHD (HD38647)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "At the assessment visit children were randomised into three groups using a randomisation table" Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was described; there were no significant differences between completers and non‐completers |
| Selective reporting (reporting bias) | High risk | Data were incompletely reported |
Van der Veek 2013.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed pretreatment, post‐treatment, 6 months, and 12 months follow‐up | |
| Participants | End of treatment: n = 92; n = 88 at 12 months follow‐up Start of treatment: n = 104 Sex: 24 F, 12 M Mean age 11.9 years (SD 2.77) Source = children's hospital Diagnosis = abdominal pain Mean months of pain = 34.01 (SD 37.54) |
|
| Interventions | "Cognitive behavior therapy" "Intensive medical care" |
|
| Outcomes | Primary pain outcome: Abdominal Pain Index (child report) Primary disability outcome: Functional Disability Inventory (child report) Primary depression outcome: Revised Child Anxiety and Depression Scale ‐ Short Version (child report) Primary anxiety outcome: Revised Child Anxiety and Depression Scale ‐ Short Version (child report)
|
|
| Notes | COI: "The authors have indicated they have no potential conflicts of interest to disclose." Funding: "The current study was funded by the Dutch Digestive Foundation, grant SWO 05‐09." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The first author randomized the children using a computerized randomization program" Comment: probably done, method not described |
| Allocation concealment (selection bias) | Unclear risk | No description found in text Comment: probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Diary data were entered in SPSS by students who were blinded to treatment." Comment: probably not done but no description given for other measures |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described, however significant differences between completers and non‐completers were not described |
| Selective reporting (reporting bias) | Unclear risk | Data fully reported when requested |
Van Tilburg 2009.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment, 6 months | |
| Participants | End of treatment: n = 29; follow‐up: n = 24 Start of treatment: n = 34 Sex: 25 F, 9 M Mean age = 10.25 years (SD 2.6) Source = University of North Carolina and Duke University Medical Centres Diagnosis = functional abdominal pain Mean years of pain = unknown | |
| Interventions | “Guided imagery treatment” “Standard medical care” | |
| Outcomes | Primary pain outcome: Abdominal Pain Index Primary disability outcome: Functional Disability Inventory Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: the authors indicated they had no financial relationships relevant to this article to disclose Funding: this work was supported by National Institutes of Health grants R24 DK067674 and RR00046 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Thirty‐four children were assigned randomly to receive 2 months of standard medical care with or without home‐based, guided imagery treatment.” Comment: probably done, method not described |
| Allocation concealment (selection bias) | Low risk | “Children picked a closed envelope that determined whether they would receive standard medical care with or without guided imagery treatment.” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described, however significant differences between completers and non‐completers were not reported |
| Selective reporting (reporting bias) | Unclear risk | Data provided on request. |
Vlieger 2007.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment, 6 months, 1 year | |
| Participants | End of treatment: n = 51 Start of treatment: n = 52 Sex: 39 F, 13 M Mean age = 13.3 years (SD 2.7) Source = paediatric gastroenterology department in hospital Diagnosis = functional abdominal pain (n = 31) and irritable bowel syndrome (IBS) (n = 22) Mean years of pain = 3.4 |
|
| Interventions | "Gut‐directed hypnotherapy" "Standard medical care plus supportive therapy" |
|
| Outcomes | Primary pain outcome: weekly pain intensity Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported. Funding: "There was no external funding source." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomly allocated using a computerised random‐number generator for concealment to either HT or standard medical care." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | "Patients were randomly allocated using a computerised random‐number generator for concealment to either HT or standard medical care." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Pain diaries were analysed by S. W. (medical student), who was blinded to the treatment arm." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described, however significant differences between completers and non‐completers were not reported |
| Selective reporting (reporting bias) | Low risk | Data were fully reported |
Wahlund 2003.
| Study characteristics | ||
| Methods | RCT. 3 arms. Assessed at pretreatment, post‐treatment, and 6 months | |
| Participants | End of treatment: n = 110 Start of treatment: n = 122 (BI + RT = 41; BI + OA = 42; BI = 39) Sex: 93 F, 29 M Mean age = 15.3 years (SD 2.0) Source = TMD clinic in Linköping, Sweden Diagnosis = temporomandibular disorders Mean years of pain = unknown |
|
| Interventions | "Brief Information + Relaxation training (BI + RT)"* "Brief Information + Occlusal appliance (BI + OA)" "Brief Information"* *For the purposes of this review, we excluded only BI + RT (treatment) and BI (control) |
|
| Outcomes | Primary pain outcome: pain intensity Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: not reported Funding: "The study was supported by the Public Dental Service of Östergötland (Östergötland's Country Council), Sweden." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The patients were randomly assigned to one of the following 3 treatment groups...." Comment: randomisation procedure unclear |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "At each evaluation, all subjects filled out a self‐administered questionnaire and were clinically examined by a 'blinded' calibrated clinician." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition reported, and there were no differences between completers and non‐completers |
| Selective reporting (reporting bias) | Low risk | All measures were reported |
Wahlund 2015.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment and three months. Non‐responders were then assigned to the other condition and assessed at 6 months. We extracted data only from the three‐month time point | |
| Participants | End of treatment: n = 57 Start of treatment: n = 64 Sex: 61 F, 3 M Mean age = 16.4 years (SD 1.87) Source = two specialist temporomandibular clinics in Sweden Diagnosis = temporomandibular pain at least once a week for more than three months Mean years of pain = 23.9 months (SD 19.05) |
|
| Interventions | "Occlusal appliance therapy" "Relaxation treatment" |
|
| Outcomes | Primary pain outcome: pain intensity Primary disability outcome: none Primary depression outcome: none Primary anxiety outcome: none
|
|
| Notes | COI: "The authors report no conflicts of interest related to this study." Funding: "This study was supported by the Swedish Dental Society; the Public Dental Service of (Östergötland County Council), Sweden; and the Public Dental Service of Kalmar (Kalmar County Council), Sweden. The authors report no conflicts of interest related to this study." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Using a random number table, a secretary not otherwise involved in the study generated the allocation sequence to assign patients to a treatment, either occlusal appliance therapy or relaxation treatment." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | "Using a random number table, a secretary not otherwise involved in the study generated the allocation sequence to assign patients to a treatment, either occlusal appliance therapy or relaxation treatment. The secretary put these assignments in sealed opaque envelopes." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description found in text Comment: probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described, however significant differences between completers and non‐completers were not reported |
| Selective reporting (reporting bias) | Low risk | Data fully reported |
Wicksell 2009.
| Study characteristics | ||
| Methods | RCT. 2 arms. Assessed at pretreatment, post‐treatment, 3.5 months, 6.8 months | |
| Participants | End of treatment: n = 29; follow‐up 3.5 months: n = 24; follow‐up 6.8 months: n = 24 Start of treatment: n = 32 Sex: 25 F, 7 M Mean age = 14.8 years (SD 2.4) Source = Astrid Lindgren Children's Hospital, Karolinska University Hospital Diagnosis = mixed pain (headache, back/neck, widespread musculoskeletal, complex regional pain syndrome, visceral, lower extremities, postherpetic type cheek pain) Mean years of pain = 2.7 |
|
| Interventions | "Exposure and acceptance" "Multidisciplinary treatment and amitriptyline" |
|
| Outcomes | Primary pain outcome: pain intensity Primary disability outcome: Functional Disability Inventory Primary depression outcome: Center for Epidemiological Studies Depression Scale for Children Primary anxiety outcome: Pain Coping Scale (catastrophising subscale)
|
|
| Notes | COI: "There are no financial or other relationships that might lead to a conflict of interest." Funding: "This study was in part financed by the Swedish Research Council and by fundings from the Karolinska Institute." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A total of 32 participants were included in the study and randomised to one of the two treatment conditions. A simple randomisation technique was used." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | "A sealed envelope (prepared by a secretary blind to the objective of the study) containing a code for 'exposure and acceptance' or 'MDT' was opened, assigning the participant to one of the treatment conditions." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "All assessments were conducted by a nurse who was not involved in delivering the treatment protocol." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was described, however significant differences between completers and non‐completers were not reported |
| Selective reporting (reporting bias) | Low risk | Data were fully reported |
AP: abdominal pain BAPQ: BFB‐REL: BI: CBCL: CBT: cognitive behavioural therapy CDI: CDS: CHS: CMAS: COI: COPE‐HEP: DIKJ: F: female FDI‐C: Functional Disability Inventory ‐ Children HCM: HT: hypnotherapy IBD: inflammatory bowel disease (IBD) IMPACT: JPFM: juvenile primary fibromyalgia KIDSCREEN: KINDL‐R M: male MDT: MEMS: NRS: numeric rating scale OA: PCQ: Ped‐MIDAS: Pediatric Migraine Disability Assessment PEDSQL: Paediatric Scale Quality of Life Inventory POR: PSSI: RCT: randomised controlled trial RT: SC: SCD: sickle cell disease SD: standard deviation SS: STAI: STAIC: TAT: TCM: TMD: TT: VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Connelly 2006 | Intervention delivered remotely |
| Fentress 1986 | Inadequate sample size (n < 10 in 1 arm of study design) |
| Gulewitsch 2017 | Non‐inferiority trial |
| Hicks 2006 | Intervention delivered remotely |
| Jastrowski Mano 2013 | Inadequate sample size (n < 10 in 1 arm of study design) |
| Koenig 2013 | Insufficient psychological treatment |
| Korterink 2016 | Insufficient psychological treatment |
| Kroener‐Herwig 1998 | Inadequate sample size (n < 10 in 1 arm of study design) |
| Larsson 1986 | Inadequate sample size (n < 10 in 1 arm of study design) |
| Olness 1987 | Insufficient psychological treatment |
| Palermo 2009 | Intervention delivered remotely |
| Rapoff 2014 | Intervention delivered remotely |
| Rutten 2017 | Non‐inferiority trial |
| Sanders 1989 | Inadequate sample size (n < 10 in 1 arm of study design) |
| Stinson 2010 | Intervention delivered remotely |
| Trautmann 2008 | Inadequate sample size (n < 10 in 1 arm of study design) |
| Trautmann 2010 | Intervention delivered remotely |
| Vlieger 2012 | Follow‐up period more than 1 year |
| Weydert 2006 | Inadequate sample size (n < 10 in 1 arm of study design) |
| Youssef 2009 | Inadequate sample size (n < 10 in 1 arm of study design) |
Differences between protocol and review
In Eccleston 2009, odds ratios and risk ratios were reported for dichotomous outcomes. In this review we only reported risk ratio.
In Eccleston 2014, therapy that was delivered remotely (e.g. via Internet, telephone) was removed as an outcome and the 'mood' outcome was separated into two discrete outcomes: depression and anxiety.
In the latest update, we updated the references in the background section and included a section on problem‐solving therapy, as this was a new therapy delivered to parents of children with chronic pain.
In the latest update, we clarified the inclusion criteria of participants included in the studies. We also expanded our definition of 'face‐to‐face' interventions to include therapies delivered by phone or written instruction book. The authors felt that these types of therapies were more similar to interventions included in this review, and that the Fisher 2015 review on remotely delivered interventions should be exclusively for those delivered via technology.
In the latest update, we included trials that delivered therapy to parents of children with chronic pain.
In the latest update, we ran subgroup analyses of smaller (i.e. n < 20 participants per arm) versus larger (i.e. n > 20 participants per arm).
In the latest update, we assessed and reported potential reporting biases.
In the latest update, we added the following sections 'Unit of analysis issues', 'Dealing with missing data', 'Assessment of reporting biases', 'Data synthesis', and 'Sensitivity analyses'.
In the latest update, we searched MEDLINE in Process in addition to other databases.
Contributions of authors
Emma Fisher oversaw the project, contributed to the design, analysis and authoring of the text, and is responsible for any future update of this review.
Christopher Eccleston, Emily Law, Joanne Dudeney, and Tonya Palermo all contributed to the design, analysis, and authoring of the text.
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Institutes of Health/National Institute of Neurological Disorders and Stroke, USA
Grant number K23NS089966 (PI: EL).
-
National Institutes of Health, USA
Grant number K24HD060068 (PI: TP)
Declarations of interest
EF: None known.
EL: None known; EL is a paediatric psychologist and provides clinical service to children and adolescents with chronic pain. EL is an author on one study included in this review (Palermo 2016) and was not involved in data extraction or assessments of this study. During the completion of this work, EL received salary support from the National Institutes of Health/National Institute of Neurological Disorders and Stroke (Grant number K23NS089966, PI: Law).
JD: None known.
TP: None known; TP is an author on one study included in this review (Palermo 2016) and was not involved in data extraction or assessments of this study. During the completion of this work, TP received salary support from the National Institutes of Health/National Institute of Child Health, behaviour and Development (K24HD060068, PI: Palermo).
CE: None known; CE is an author on one study included in this review (Palermo 2016) and was not involved in data extraction or assessments of this study. Since CE is an author as well as the PaPaS Co‐ordinating Editor at the time of writing, we acknowledge the input of Amanda C de C Williams who acted as Sign Off Editor for this review. CE had no input into the editorial decisions or processes for this review.
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Abram 2007 {published data only}
- Abram HS, Buckloh LM, Schilling LS, Armatti Wiltrout S, Ramirez-Garnica G, Turk WR. A randomized, controlled trial of a neurological and psychoeducational group appointment model for pediatric headaches. Children's Healthcare 2007;36:249-65. [Google Scholar]
Alfven 2007 {published data only}
- Alfven G, Lindstrom A. A new method for the treatment of recurrent abdominal pain of prolonged negative stress origin. Acta Paediatrica 2007;96:76-81. [DOI] [PubMed] [Google Scholar]
Barakat 2010 {published data only}
- Barakat LP, Schwartz LA, Salamon KS, Radcliffe J. A family-based randomized controlled trial of pain intervention for adolescents with sickle cell disease. Journal of Pediatric Hematology/Oncology 2010;32(7):540-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barry 1997 {published data only}
- Barry J, Von Baeyer CL. Brief cognitive-behavioral group treatment for children's headache. Clinical Journal of Pain 1997;13:215-20. [DOI] [PubMed] [Google Scholar]
Bussone 1998 {published data only}
- Bussone G, Grazzi L, D'Amico D, Leone M, Andrasik F. Biofeedback-assisted relaxation training for young adolescents with tension-type headache: a controlled study. Cephalalgia 1988;18:463-7. [DOI] [PubMed] [Google Scholar]
Chen 2014 {published data only}
- Chen YZ, Li N, Zhou KY. Preventive effect of behavioral therapy plus flunarizine in children with migraine. Chinese Journal of Contemporary Pediatrics 2014;16(11):1105-8. [PubMed] [Google Scholar]
Cottrell 2007 {published data only}
- Cottrell C, Drew J, Gibson J, Holroyd, K, O'Donnell F. Feasibility assessment of telephone-administered behavioral treatment for adolescent migraine. Headache 2007;47:1293-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
Daniel 2015 {published data only}
- Daniel LC, Li Y, Smith K, Tarazi R, Robinson R, Patterson CA, et al. Lessons learned from a randomized controlled trial of a family-based intervention to promote school functioning for school-age children with sickle cell disease. Journal of Pediatric Psychology 2015;40(10):1085-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Duarte 2006 {published data only}
- Duarte MA, Penna FJ, Andrade EM, Cancela CSP, Neto JCA, Barbosa TF. Treatment of nonorganic recurrent abdominal pain: cognitive-behavioral family intervention. Journal of Pediatric Gastroenterology and Nutrition 2006;43:59-64. [DOI] [PubMed] [Google Scholar]
Fichtel 2001 {published data only}
- Fichtel A, Larsson B. Does relaxation treatment have differential effects on migraine and tension-type headache in adolescents. Headache 2001;41:290-6. [DOI] [PubMed] [Google Scholar]
Gil 1997 {published data only}
- Gil KM, Wilson JJ, Edens JL, Workman E, Ready J, Sedway J, et al. Cognitive coping skills training in children with sickle cell disease pain. International Journal of Behavioural Medicine 1997;4:364-77. [DOI] [PubMed] [Google Scholar]
Greenley 2015 {published data only}
- Greenley RA, Gumidyala AP, Nguyen E, Plevinsky JM, Poulopoulos N, Thomason MM, et al. Can you teach a teen new tricks? Problem solving skills training improves oral medication adherence in pediatric patients with inflammatory bowel disease participating in a randomized trial. Inflammatory Bowel Disease 2015;21:2649-57. [DOI] [PubMed] [Google Scholar]
Griffiths 1996 {published data only}
- Griffiths JD, Martin PR. Clinical versus home-based treatment formats for children with chronic headache. British Journal of Health Psychology 1996;1:151-66. [Google Scholar]
Grob 2013 {published data only}
- Grob M, Warschburger P. Evaluation of a cognitive-behavioral pain management program for children with chronic abdominal pain: a randomized controlled study. International Journal of Behavioral Medicine 2013;20:434-43. [DOI: 10.1007/s12529-012-9228-3] [DOI] [PubMed] [Google Scholar]
Gulewitsch 2013 {published data only}
- Gulewitsch MD, Muller J, Hautzinger M, Schlarb AA. Brief hypnotherapeutic-behavioral intervention for functional abdominal pain and irritable bowel syndrome in childhood: a randomized controlled trial. European Journal of Pediatrics 2013;172:1043-51. [DOI] [PubMed] [Google Scholar]
Hechler 2014 {published data only}
- Hechler T, Ruhe A, Schmidt P, Hirsch J, Wager J, Dobe M, et al. Inpatient-based intensive interdisciplinary pain treatment for highly impaired children with severe chronic pain: randomized controlled trial of efficacy and economic effects. Pain 2014;155:118-28. [DOI] [PubMed] [Google Scholar]
Hickman 2015 {published data only}
- Hickman C, Jacobson D, Melnyk B. Randomized controlled trial of the acceptability, feasibility, and preliminary effects of a cognitive behavioral skills building intervention in adolescents with chronic daily headaches: a pilot study. Journal of Pediatric Health Care 2015;29(1):5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Humphreys 2000 {published data only}
- Humphreys PA, Gevirtz RN. Treatment of recurrent abdominal pain: components analysis of four treatment protocols. Journal of Pediatric Gastroenterology and Nutrition 2000;31:47-51. [DOI] [PubMed] [Google Scholar]
Kashikar‐Zuck 2005 {published data only}
- Kashikar-Zuck S, Swain NF, Jones BA, Graham TB. Efficacy of cognitive-behavioral intervention for juvenile primary fibromyalgia syndrome. Journal of Rheumatology 2005;32:1594-602. [PubMed] [Google Scholar]
Kashikar‐Zuck 2012 {published data only}
- Kashikar-Zuck S, Sil S, Lynch-Jordan AM, Ting TV, Peugh J, Schikler KN, et al. Changes in pain coping, catastrophizing, and coping efficacy after cognitive-behavioral therapy in children and adolescents with juvenile fibromyalgia. Journal of Pain 2013;14(5):492-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashikar-Zuck S, Ting TV, Arnold LM, Bean J, Powers SW, Graham B, et al. Cognitive behavioral therapy for the treatment of juvenile fibromyalgia. Arthritis & Rheumatism 2012;64(1):297-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kroener‐Herwig 2002 {published data only}
- Kroener-Herwig B, Denecke H. Cognitive-behavioral therapy of pediatric headache: are there differences in efficacy between a therapist-administered group training and a self-help format? Journal of Psychosomatic Research 2002;53:1107-14. [DOI] [PubMed] [Google Scholar]
Labbe 1984 {published data only}
- Labbe EE, Williamson DA. Treatment of childhood migraine using autogenic feedback training. Journal of Consulting and Clinical Psychology 1984;52(6):968-76. [DOI] [PubMed] [Google Scholar]
Labbe 1995 {published data only}
- Labbe EE. Treatment of childhood migraine with autogenic training and skin temperature biofeedback: a component analysis. Headache 1995;35:10-3. [DOI] [PubMed] [Google Scholar]
Larsson 1987a {published data only}
- Larsson B, Daleflod B, Hakansson L, Melin L. Therapist-assisted versus self-help relaxation treatment of chronic headaches in adolescents: a school-based intervention. Journal of Child Psychology 1987;28(1):127-36. [DOI] [PubMed] [Google Scholar]
Larsson 1987b {published data only}
- Larsson B, Melin L, Lamminen M, Ullstedt F. A school-based treatment of chronic headaches in adolescents. Journal of Pediatric Psychology 1987;12(4):553-66. [DOI] [PubMed] [Google Scholar]
Larsson 1990 {published data only}
- Larsson B, Melin L, Doberl A. Recurrent tension headache in adolescents treated with self-help relaxation training and a muscle relaxant drug. Headache 1990;30:665-71. [DOI] [PubMed] [Google Scholar]
Larsson 1996 {published data only}
- Larsson B, Carlsson J. A school-based, nurse-administered relaxation training for children with chronic tension-type headache. Journal of Pediatric Psychology 1996;21(5):603-14. [DOI] [PubMed] [Google Scholar]
Levy 2010 {published data only}
- Levy RL, Langer SL, Walker LS, Romano JM, Christie DL, Youssef N, et al. Cognitive-behavioral therapy for children with functional abdominal pain and their parents decreases pain and other symptoms. American Journal of Gastroenterology 2010;105(4):946-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy RL, Langer SL, Walker LS, Romano JM, Christie DL, Youssef N, et al. Twelve-month follow-up of cognitive behavioral therapy for children with functional abdominal pain. JAMA Pediatrics 2013;167(2):178-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levy 2016 {published data only}
- Levy RL, Van Tilburg MAL, Langer SL, Romano JM, Walker LS, Mancl LA, et al. Effects of a cognitive behavioral therapy intervention trial to improve disease outcomes in children with inflammatory bowel disease. Inflammatory Bowel Diseases 2016;22(9):2134-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levy 2017 {published data only}
- Levy RL, Langer SL, Van Tilburg MAL, Romano JM, Murphy TB, Walker LS, et al. Brief telephone-delivered cognitive behavioral therapy targeted to parents of children with functional abdominal pain: a randomized controlled trial. Pain 2017;158:618-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
McGrath 1988 {published data only}
- McGrath PJ, Humphreys P, Goodman JT, Keene D, Firestone P, Jacob P, et al. Relaxation prophylaxis for childhood migraine: a randomized placebo-controlled trial. Developmental Medicine and Child Neurology 1988;30:626-31. [DOI] [PubMed] [Google Scholar]
McGrath 1992 {published data only}
- McGrath PJ, Humphreys P, Keene D, Goodman JT, Lascelles MA, Cunningham SJ, et al. The efficacy and efficiency of a self-administered treatment for adolescent migraine. Pain 1992;49:321-4. [DOI] [PubMed] [Google Scholar]
Osterhaus 1997 {published data only}
- Osterhaus SOL, Lange A, Linssen WHJP, Passchier J. A behavioral treatment of young migrainous and nonmigrainous headache patients: prediction of treatment success. International Journal of Behavioral Medicine 1997;4(4):378-96. [DOI] [PubMed] [Google Scholar]
Palermo 2016 {published data only}
- Palermo TM, Law EF, Bromberg M, Fales J, Ecceston C, Wilson AC. Problem-solving skills training for parents of children with chronic pain: a pilot randomized controlled trial. Pain 2016;157:1213-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Passchier 1990 {published data only}
- Passchier J, Van Den Bree MBM, Emmen HH, Osterhaus SOL, Orlebeke JF, Verhage F. Relaxation training in school classes does not reduce headache complaints. Headache 1990;30:660-4. [DOI] [PubMed] [Google Scholar]
Powers 2013 {published data only}
- Powers SW, Kashikar-Zuck SM, Allen JR, LeCates SL, Slater SK, Zafar M, et al. Cognitive behavioral therapy plus amitriptyline for chronic migraine in children and adolescents. A randomized clinical trial. JAMA 2013;310(24):2622-30. [DOI: 10.1001/jama.2013.282533] [DOI] [PMC free article] [PubMed] [Google Scholar]
Richter 1986 {published data only}
- Richter IL, McGrath PJ, Humphreys PJ, Goodman JT, Firestone P, Keene D. Cognitive and relaxation treatment of paediatric migraine. Pain 1986;25:195-203. [DOI] [PubMed] [Google Scholar]
Robins 2005 {published data only}
- Robins PM, Smith SM, Glutting JJ, Bishop CT. A randomized controlled trial of a cognitive-behavioral family intervention for pediatric recurrent abdominal pain. Journal of Pediatric Psychology 2005;30:397-408. [DOI] [PubMed] [Google Scholar]
Sanders 1994 {published data only}
- Sanders MR, Shepherd RW, Cleghorn G, Woolford H. The treatment of recurrent abdominal pain in children: a controlled comparison of cognitive-behavioral family intervention and standard pediatric care. Journal of Consulting and Clinical Psychology 1994;62(2):306-14. [DOI] [PubMed] [Google Scholar]
Sartory 1998 {published data only}
- Sartory G, Muller B, Metsch J, Pothmann R. A comparison of psychological and pharmacological treatment of pediatric migraine. Behaviour Research and Therapy 1998;36:1155-70. [DOI] [PubMed] [Google Scholar]
Scharff 2002 {published data only}
- Scharff L, Marcus DA, Masek BJ. A controlled study of minimal-contact thermal biofeedback treatment in children with migraine. Journal of Pediatric Psychology 2002;27:109-19. [DOI] [PubMed] [Google Scholar]
Van der Veek 2013 {published data only}
- Van der Veek SMC, Derkx BHF, Benninga MA, Boer F, De Haan E. Cognitive behavior therapy for pediatric functional abdominal pain: a randomized controlled trial. Pediatrics 2013;132(5):e1163-72. [DOI: 10.1542/peds.2013-0242] [DOI] [PubMed] [Google Scholar]
Van Tilburg 2009 {published data only}
- Van Tilburg MAL, Chitkara DK, Palsson OS, Turner M, Blois-Martin N. Audio-recorded guided imagery treatment reduces functional abdominal pain in children: a pilot study. Pediatrics 2009;124(5):e890-7. [DOI] [PubMed] [Google Scholar]
Vlieger 2007 {published data only}
- Vlieger AM, Menko-Frankenhuis C, Wolfkamp SC, Tromp E, Benninga MA. Hypnotherapy for children with functional abdominal pain or irritable bowel syndrome: a randomized controlled trial. Gastroenterology 2007;133:1430-6. [DOI] [PubMed] [Google Scholar]
Wahlund 2003 {published data only}
- Wahlund K, List, T, Larsson B. Treatment of temporomandibular disorders among adolescents: a comparison between occlusal appliance, relaxation training, and brief information. Acta Odontologica Scandinavica 2003;34(4):203-11. [DOI] [PubMed] [Google Scholar]
Wahlund 2015 {published data only}
- Wahlund K, Nilsson I, Larsson B. Treating temporomandibular disorders in adolescents: a randomized, controlled, sequential comparison of relaxation training and occlusal appliance therapy. Journal of Oral & Facial Pain and Headache 2015;29:41-50. [DOI] [PubMed] [Google Scholar]
Wicksell 2009 {published data only}
- Wicksell RK, Melin L, Lekander M, Olsson GL. Evaluating the effectiveness of exposure and acceptance strategies to improve functioning and quality of life in longstanding pediatric pain - a randomized controlled trial. Pain 2009;141:248-57. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Connelly 2006 {published data only}
- Connelly M, Rapoff MA, Thompson N, Connelly W. Headstrong: a pilot study of a CD-ROM intervention for recurrent pediatric headache. Journal of Pediatric Psychology 2006;31:737-47. [DOI] [PubMed] [Google Scholar]
Fentress 1986 {published data only}
- Fentress DW, Masek BJ, Mehegan JE, Benson H. Biofeedback and relaxation-response training in the treatment of pediatric migraine. Developmental Medicine and Child Neurology 1986;28:139-46. [DOI] [PubMed] [Google Scholar]
Gulewitsch 2017 {published data only}
- Gulewitsch MD, Schlarb AA. Comparison of gut-directed hypnotherapy and unspecific hypnotherapy as self-help format in children and adolescents with functional abdominal pain or irritable bowel syndrome: a randomized pilot study. European Journal of Gastroenterology & Hepatology 2017;29:1351-60. [DOI] [PubMed] [Google Scholar]
Hicks 2006 {published data only}
- Hicks CL, Von Baeyer CL, McGrath PJ. Online psychological treatment for pediatric recurrent pain: a randomized evaluation. Journal of Pediatric Psychology 2006;31:724-36. [DOI] [PubMed] [Google Scholar]
Jastrowski Mano 2013 {published data only}
- Jastro-Mano KE, Salamon KS, Hainsworth KR, Anderson-Khan KJ, Ladwig RJ, Davies WH, et al. A randomized, controlled pilot study of mindfulness-based stress reduction for pediatric chronic pain. Alternative Therapies in Health and Medicine 2013;19(6):8-14. [PubMed] [Google Scholar]
Koenig 2013 {published data only}
- Koenig J, Oelkers-Ax R, Kaess M, Parzer P, Lenzen C, Hillecke TK, et al. Specific music therapy techniques in the treatment of primary headache disorders in adolescents: a randomized attention-placebo-controlled trial. Journal of Pain 2013;14(10):1196-207. [DOI] [PubMed] [Google Scholar]
Korterink 2016 {published data only}
- Koterink JJ, Ockeloen LE, Hilbink M, Benninga MA, Deckers-Krocken JM. Yoga therapy for abdominal pain-related functional gastrointestinal disorders in children: a randomized controlled trial. Journal of Pediatric Gastroenterology and Nutrition 2016;63(5):481-7. [DOI] [PubMed] [Google Scholar]
Kroener‐Herwig 1998 {published data only}
- Kroner-Herwig B, Mohn U, Pothmann R. Comparison of biofeedback and relaxation in the treatment of pediatric headache and the influence of parent involvement on outcome. Applied Psychophysiology and Biofeedback 1998;23:143-57. [DOI] [PubMed] [Google Scholar]
Larsson 1986 {published data only}
- Larsson B, Melin L. Chronic headaches in adolescents: treatment in a school setting with relaxation training as compared with information-contact and self-registration. Pain 1986;25:325-36. [DOI] [PubMed] [Google Scholar]
Olness 1987 {published data only}
- Olness K, MacDonald JT, Uden DL. Comparison of self-hypnosis and propranolol in the treatment of juvenile classic migraine. Pediatrics 1987;79(4):593-7. [PubMed] [Google Scholar]
Palermo 2009 {published data only}
- Palermo TM, Wilson AC, Peters M, Lewandowski A, Somhegyi H. Randomized controlled trial of an internet delivered family cognitive behavioral therapy intervention for children and adolescents with chronic pain. Pain 2009;146(1-2):205-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rapoff 2014 {published data only}
- Rapoff MA, Connelly M, Bickel JL, Powers SW, Hershey AD, Allen JR, et al. Headstrong intervention for pediatric migraine headache: a randomized clinical trial. Journal of Headache and Pain 2014;15(1):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rutten 2017 {published data only}
- Rutten J, Vlieger AM, Frankenhuis C, George EK, Groeneweg M, Norbrius OF, et al. Home-based hypnotherapy self-exercises vs individual hypnotherapy with a therapist for treatment of pediatric irritable bowel syndrome, functional abdominal pain, or functional abdominal pain syndrome: a randomized clinical trial. JAMA 2017;171(5):470-7. [DOI] [PubMed] [Google Scholar]
Sanders 1989 {published data only}
- Sanders MR, Rebgetz M, Morrison M, Bor W, Gordon A, Dadds M, et al. Cognitive-behavioral treatment of recurrent nonspecific abdominal pain in children: an analysis of generalization, maintenance, and side effects. Journal of Consulting and Clinical Psychology 1989;57(2):294-300. [DOI] [PubMed] [Google Scholar]
Stinson 2010 {published data only}
- Stinson JN, McGrath PJ, Hodnett ED, Feldman BM, Duffy CM, Huber AM, et al. An internet-based self-management program with telephone support for adolescents with arthritis: a pilot randomized controlled trial. Journal of Rheumatology 2010;37(9):1944-52. [DOI] [PubMed] [Google Scholar]
Trautmann 2008 {published data only}
- Trautmann E, Kroner-Herwig B. Internet-based self-help training for children and adolescents with recurrent headache: a pilot study. Behavioural and Cognitive Psychotherapy 2008;36:241-5. [Google Scholar]
Trautmann 2010 {published data only}
- Trautmann E, Kroner-Herwig B. A randomized controlled trial of internet-based self-help training for recurrent headache in childhood and adolescence. Behaviour Research and Therapy 2010;48:28-37. [DOI] [PubMed] [Google Scholar]
Vlieger 2012 {published data only}
- Vlieger AM, Rutten JMTM, Govers AMAO, Frankenhuis C, Benninga MA. Long-term follow-up of gut-directed hypnotherapy vs. standard care in children with functional abdominal pain or irritable bowel syndrome. American Journal of Gastroenterology 2012;107:627-31. [DOI] [PubMed] [Google Scholar]
Weydert 2006 {published data only}
- Weydert JA, Shapiro DE, Acra SA, Monheim CJ, Chambers AS, Ball TM. Evaluation of guided imagery as treatment for recurrent abdominal pain in children: a randomized controlled trial. BMC Pediatrics 2006;6(29):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Youssef 2009 {published data only}
- Youssef NN, Van Tilburg MA, Matta EN, Langseder A, Whitehead WE. Feasibility and efficacy of pilot study investigating a school nurse administered guided imagery program for childhood functional abdominal pain. Gastroenterology 2009;136(5):156-7. [Google Scholar]
Additional references
Abbott 2017
- Abbott RA, Martin AE, Newlove-Delgado TV, Bethel A, Thompson-Coon J, Whear R, et al. Psychosocial interventions for recurrent abdominal pain in childhood. Cochrane Database of Systematic Reviews 2017, Issue 1. Art. No: CD010971. [DOI: 10.1002/14651858.CD010971.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Anie 2015
- Anie KA, Green J. Psychological therapies for sickle cell disease and pain. Cochrane Database of Systematic Reviews 2015, Issue 5. Art. No: CD001916. [DOI: 10.1002/14651858.CD001916.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen 1992
- Cohen J. A power primer. Psychological Bulletin 1992;112(1):155-9. [DOI] [PubMed] [Google Scholar]
Cohen 2017
- Cohen EM, Morley-Fletcher A, Mehta DH, Lee YC. A systematic review of psychosocial therapies for children with rheumatic diseases. Pediatric Rheumatology 2017;15(6):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cooper 2017a
- Cooper TE, Fisher E, Gray AL, Krane E, Sethna N, Van Tilburg MAL, et al. Opioids for chronic non-cancer pain in children and adolescents. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No: CD012538. [DOI: 10.1002/14651858.CD012538.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cooper 2017b
- Cooper TE, Fisher E, Anderson B, Wilkinson NMR, Williams DG, Eccleston C. Paracetamol (acetaminophen) for chronic non-cancer pain in children and adolescents. Cochrane Database of Systematic Reviews 2017, Issue 8. Art. No: CD012539. [DOI: 10.1002/14651858.CD012539.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cooper 2017c
- Cooper TE, Heathcote LC, Clinch J, Gold JI, Howard R, Lord SM, et al. Antidepressants for chronic non-cancer pain in children and adolescents. Cochrane Database of Systematic Reviews 2017, Issue 8. Art. No: CD012535. [DOI: 10.1002/14651858.CD012535.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cooper 2017d
- Cooper TE, Wiffen PJ, Heathcote LC, Clinch J, Howard R, Krane E, et al. Antiepileptic drugs for chronic non-cancer pain in children and adolescents. Cochrane Database of Systematic Reviews 2017, Issue 8. Art. No: CD012536. [DOI: 10.1002/14651858.CD012536.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
D'Zurilla 1999
- D’Zurilla TJ, Nezu AM. Problem Solving Therapy: A Social Competence Approach to Clinical Intervention. 2nd edition. New York: Springer Publishing, 1999. [Google Scholar]
D'Zurilla 2007
- D’Zurilla TJ, Nezu AM. Problem Solving Therapy: A Positive Approach to Clinical Intervention. 3rd edition. New York: Springer Publishing Company, LLC, 2007. [Google Scholar]
Eccleston 2015
- Eccleston C, Fisher E, Law EF, Bartlett J, Palermo TM. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database of Systematic Reviews 2015, Issue 4. Art. No: CD009660. [DOI: 10.1002/14651858.CD009660.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Eccleston 2017
- Eccleston C, Cooper TE, Fisher E, Anderson B, Wilkinson NMR. Non-steroidal anti-inflammatory drugs (NSAIDs) for chronic non-cancer pain in children and adolescents. Cochrane Database of Systematic Reviews 2017, Issue 8. Art. No: CD012537. [DOI: 10.1002/14651858.CD012537.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ernst 2015
- Ernst MM, O'Brien H, Powers SW. Cognitive-behavioral therapy: how medical providers can increase patient and family openness and access to evidence-based multimodal therapy for pediatric migraine. Headache 2015;55(1-):1382-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fisher 2014
- Fisher E, Heathcote L, Palermo TM, Williams DCA, Lau J, Eccleston C. Systematic review and meta-analysis of psychological therapies for children with chronic pain. Journal of Pediatric Psychology 2014;39(8):763-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fisher 2015
- Fisher E, Law E, Palermo TM, Eccleston C. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database of Systematic Reviews 2015, Issue 3. Art. No: CD011118. [DOI: 10.1002/14651858.CD011118.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fisher 2017
- Fisher E, Heathcote LC, Eccleston C, Simons LE, Palermo TM. Assessment of pain anxiety, pain catastrophizing, and fear of pain in children and adolescents with chronic pain: a systematic review and meta-analysis. Journal of Pediatric Psychology 2018;43(3):314-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fordyce 1968
- Fordyce WE, Fowler RS Jr, Lehmann JF, DeLateur BJ. Some implications of learning on problems of chronic pain. Journal of Chronic Disease 1968;21:179-90. [DOI] [PubMed] [Google Scholar]
Guyatt 2013
- Guyatt G, Oxman AD, Sultan S, Brozek J, Glasziou P, Alonso-Coello P, et al. GRADE guidelines: 11. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. Journal of Clinical Epidemiology 2013;66:151-7. [DOI] [PubMed] [Google Scholar]
Hechler 2015
- Hechler T, Kanstrup M, Lewandowski Holley A, Simons LE, Wicksell R, Hirschfeld G, et al. Systematic review on intensive interdisciplinary pain treatment of children with chronic pain. Pediatrics 2015;136(1):115-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Horst 2014
- Horst S, Shelby G, Anderson J, Acra S, Polk DB, Saville BR, et al. Predicting persistence of functional abdominal pain from childhood into young adulthood. Clinical Gastroenterology and Hepatology 2014;12(12):2026-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Huertas‐Ceballos 2008
- Huertas-Ceballos A, Logan S, Bennett C, Macarthur C. Psychosocial interventions for recurrent abdominal pain (RAP) and irritable bowel syndrome (IBS) in childhood. Cochrane Database of Systematic Reviews 2008, Issue 1. Art. No: CD003014. [DOI: 10.1002/14651858.CD003014.pub2] [DOI] [PubMed] [Google Scholar]
Keefe 2004
- Keefe FJ, Rumble ME, Scipio CD, Giordano LA, Perri LM. Psychological aspects of persistent pain: current state of the science. Journal of Pain 2004;5:195-211. [DOI] [PubMed] [Google Scholar]
Kibby 1998
- Kibby MY, Tyc VL, Mulhern RK. Effectiveness of psychological intervention for children and adolescents with chronic medical illness: a meta-analysis. Clinical Psychology Reviews 1998;18:103-17. [DOI] [PubMed] [Google Scholar]
King 2011
- King S, Chamber CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, et al. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain 2011;152:2729–38. [DOI] [PubMed] [Google Scholar]
Law 2014
- Law EF, Fisher E, Fales J, Noel M, Eccleston C. Systematic review and meta-analysis of parent and family-based interventions for children and adolescents with chronic medical conditions. Journal of Pediatric Psychology 2014;39(8):866-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Law 2017
- Law EF, Fisher E, Beals-Erickson S, Fisher E, Lang E, Palermo TM. Components of effective cognitive-behavioral therapy for pediatric headache: a mixed methods approach. Clinical Practice in Pediatric Psychology 2017;5(4):376-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
McGrath 2008
- McGrath PJ, Walco G, Turk DC, Dworkin RH, Brown MT, Davidson K, et al. Core outcome domains and measures for pediatric acute and chronic/recurrent pain clinical trials: PedIMMPACT recommendations. Journal of Pain 2008;9:771-83. [DOI] [PubMed] [Google Scholar]
Moore 2013
- Moore RA, Derry S, Wiffen PJ. Challenges in design and interpretation of chronic pain trials. British Journal of Anaesthesia 2013;111(1):38-45. [DOI] [PubMed] [Google Scholar]
Ng 2017
- Ng QX, Venkatanarayanan N, Kumar L. A systematic review and meta-analysis of the efficacy of cognitive behavioral therapy for the management of pediatric migraine. Headache: The Journal of Head and Face Pain 2017;57:349-62. [DOI] [PubMed] [Google Scholar]
Palermo 2005
- Palermo TM, Chambers CT. Parent and family factors in pediatric chronic pain and disability: an integrative approach. Pain 2005;119:1-4. [DOI] [PubMed] [Google Scholar]
Palermo 2012
- Palermo TM. Cognitive-Behavioral Therapy for Chronic Pain in Children and Adolescents. New York: Oxford University Press, 2012. [Google Scholar]
Palermo 2014
- Palermo TM, Valrie CR, Karlson CW. Family and parent influences on pediatric chronic pain: a developmental perspective. American Psychologist 2014;69(2):142-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Perquin 2000
- Perquin CW, Hazebroek-Kampscheur AAJM, Hunfeld JAM, Bohnene AM, Van Suijlekom-Smit LWA, Passchier J, et al. Pain in children and adolescents: a common experience. Pain 2000;87:51-8. [DOI] [PubMed] [Google Scholar]
Perquin 2001
- Perquin CW, Hazebroek-Kampscheur AAJM, Hunfeld JAM, Van Suijlekom-Smit LWA, Passchier J, Van der Wouden JC. Chronic pain among children and adolescents: physician consultation and medication use. Clinical Journal of Pain 2001;16:229-35. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Stanford 2008
- Stanford EA, Chambers CT, Biesanz JC, Chen E. The frequency, trajectories and predictors of adolescent recurrent pain: a population-based approach. Pain 2008;138:11-21. [DOI] [PubMed] [Google Scholar]
Walco 1999
- Walco GA, Sterling CM, Conte PM, Engel RG. Empirically supported treatments in pediatric psychology: disease related pain. Journal of Pediatric Psychology 1999;24:155-67. [DOI] [PubMed] [Google Scholar]
Walker 2012
- Walker LS, Sherman AL, Bruehl S, Garber J, Smith CA. Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric co morbidities in adolescence and adulthood.. Pain 2012;153(9):1798-806. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 2012
- Williams ACDC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database of Systematic Reviews 2012, Issue 11. Art. No: CD007407. [DOI: 10.1002/14651858.CD007407] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Eccleston 2003
- Eccleston C, Yorke L, Morley S, Williams ACDC, Mastroyannopoulou A. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database of Systematic Reviews 2003, Issue 1. Art. No: CD003968. [DOI: 10.1002/14651858.CD003968] [DOI] [PubMed] [Google Scholar]
Eccleston 2009
- Eccleston C, Palermo TM, Williams ACDC, Lewandowski A, Morley S. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No: CD003968. [DOI: 10.1002/14651858.CD003968.pub2] [DOI] [PubMed] [Google Scholar]
Eccleston 2012
- Eccleston C, Palermo TM, Williams ACDC, Lewandowski A, Morley S, Fisher E, et al. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database of Systematic Reviews 2012, Issue 12. Art. No: CD003968. [DOI: 10.1002/14651858.CD003968.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Eccleston 2014
- Eccleston C, Palermo TM, Williams ACDC, Lewandowski Holley A, Morley S, Fisher E, et al. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database of Systematic Reviews 2014, Issue 5. Art. No: CD003968. [DOI: 10.1002/14651858.CD003968.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]


