Abstract
Rationale:
Hyponatremia following duloxetine treatment has been reported in patients with major depressive disorder, fibromyalgia, diabetic neuropathy, or sciatic pain. The manifestations of duloxetine-induced hyponatremia are varying in different individuals. The overall prognosis for this type of hyponatremia is favorable if properly managed.
Patient concerns and diagnoses:
Herein, we reported rapid-onset hyponatremia and delirium in an older patient after 2 doses of duloxetine, which was used to control his postherpetic neuralgia. Laboratory examinations revealed a rapid decline in serum sodium level and indicated the possibility of syndrome of inappropriate antidiuretic hormone (SIADH).
Interventions:
Discontinuation of duloxetine, restriction of water intake, and intravenous supplement of normal saline were adopted to manage the hyponatremia.
Outcomes:
Serum concentration of sodium gradually normalized following aforementioned strategies.
Lessons:
Special attention to the electrolyte abnormality is recommended in old patients undergoing duloxetine treatment.
Keywords: duloxetine, hyponatremia, postherpetic neuralgia
1. Introduction
Hyponatremia is a common electrolyte abnormality and has potentially life-threatening complications.[1] Hyponatremia caused by antidepressants treatment is also frequently observed in clinical practice.[2] Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs, e.g., venlafaxine) have been widely reported to induce hyponatremia in susceptive individuals.[2–4] However, inadequate attention has been paid to this adverse event caused by duloxetine in clinical practice.
To date, sporadic case studies have reported duloxetine-associated hyponatremia in patients with major depressive disorder, fibromyalgia, diabetic neuropathy, or sciatic pain,[5–18] but not in patients with postherpetic neuralgia. Postherpetic neuralgia is an intractable sequela of herpes zoster and greatly impacts the life quality.[19] Topical and systemic medications can be used to control this condition according to the severity of neuropathic pain.[20] Anticonvulsants, tricyclic antidepressants, and the opioid analgesics are the recommended systemic agents for patients with severe pain.[20] As a SNRI antidepressant, duloxetine has a satisfying effect in alleviating the accompanying somatic pain in depressed patients.[21] Moreover, duloxetine may also be effective in resolution of painful neuropathy and different types of chronic pain.[22] However, duloxetine is only approved to treat depression in China.
Herein, we present a case of rapid-onset hyponatremia in an old patient with postherpetic neuralgia, who was off-label treated by duloxetine. This patient rapidly developed weakness, lethargy, and delirium-like symptoms during hyponatremia and recovered after duloxetine discontinuation, water restriction, and intravenous supplement of normal saline. Moreover, this article briefly reviews the documented cases of duloxetine-associated hyponatremia and summarized the demographic and clinical characteristics of these patients.
2. Case presentation
A 78-year-old male patient was admitted to our hospital because of debilitating skin pain for 3 weeks. On admission, scattered rashes could be visually noted in the right side of the forehead, the upper eyelid, and the periorbital skin. He complained drooping eyelid, restricted eye-movement and double vision for 2 weeks. Given the existence of right oculomotor paralysis, lumber puncture was timely performed after excluding contraindications and obtaining informed consent. Examination of the cerebrospinal fluid (CSF) indicated an elevated count of white blood cell (0.041, normal: 0–0.005) and increased protein (0.60, normal: 0.15–0.45). Laboratory investigations of routine blood test, liver function, renal function, electrolyte concentration, thyroid function, cortical hormone, tumor biomarkers, and autoimmune antibodies were all within the normal limits. His past medical history included hypertension and chronic obstructive pulmonary disease (COPD). He was taking amlodipine tablets and tiotropium bromide power for inhalation to control these diseases.
Accordingly, herpes zoster with accompanying oculomotor paralysis was diagnosed. Intravenous acyclovir and dexamethasone was administrated. To cope with his skin pain, gabapentin was gradually titrated to 300 mg 3 times per day. An ophthalmologic consultation indicated keratitis and ganciclovir eye gel was prescribed. Nearly 2 weeks following this treatment strategy, lumber puncture was performed again and reexamination of the CSF returned to normal. Although this patient felt his right eye movement became flexible, skin pain around the lesion did not significantly alleviate. To relieve his pain, duloxetine in a daily dose of 60 mg was added. The other medications were kept the same as before. However, after 2 doses of duloxetine, this patient began to feel fatigued and appeared to be poorly orientated and lethargic. When falling asleep, he would wave his arms and randomly grope. When woken up, he explained these behaviors as catching chickens or carrying a bucket. Immediate blood electrolyte was performed and indicated hyponatremia (125, normal: 132–145 mmol/L) and hypochloridemia (89, normal: 90–108 mmol/L). Serum osmolality was 254 mOsm/L and urine osmolality was 430 mOsm/L. No indications of new-onset infection were discovered. Reexamination of renal function was also normal. Cranial magnetic resonance imaging revealed no significant findings. According to the laboratory results, SIADH was considered. His delirium-like symptoms were considered to be secondary to hyponatremia. Because hyponatremia emerged rapidly following duloxetine treatment, duloxetine was thought to be the culprit and subsequently discontinued. Meanwhile, daily water restriction and intravenous supplement of normal saline was initiated. Within 1 week after duloxetine withdrawal, his serum sodium concentration returned to normal level (the dynamic change of serum sodium concentration was shown in Figure 1). Symptoms of lethargy and weakness also improved. No recurrence of hyponatremia was detected in follow-up visits.
Figure 1.
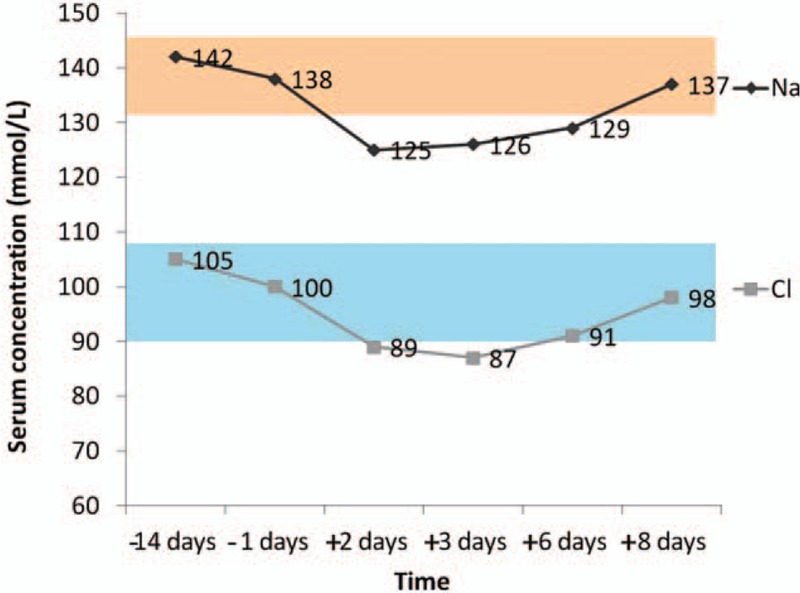
Dynamic monitoring of serum concentration of sodium and chloride in the patient. “−” refers to “before the onset of hyponatremia”, “+” refers to “after the onset of hyponatremia”, the pink area represents the reference range of serum sodium concentration, and the blue area represents the reference range of serum chloride concentration.
This case study obtained approval from the Institute Ethical Committee of the First Affiliated Hospital, Zhejiang University School of Medicine. An informed consent for publication of the case details was provided by our patient and his guardians.
3. Discussion
In this case study, we first present an old male patient with postherpetic neuralgia, who developed hyponatremia following duloxetine treatment. Before taking duloxetine, the baseline serum level of sodium was normal, but declined rapidly after ingesting only 2 doses of duloxetine. His condition improved within 1 week after duloxetine discontinuation, water restriction, and supplement of normal saline. According to the Naranjo scale for evaluating the probability of adverse drug effects, the relationship of duloxetine and hyponatremia in our patient was “probable.”[23]
According to the previous reports, SIADH was the most mentioned explanation accounting for duloxetine-induced hyponatremia. The exact molecular mechanism of SIADH caused by antidepressants remains unclear. As a dual-action antidepressant, duloxetine enables to increase the concentrations of serotonin and norepinephrine, and further possibly stimulate the secretion of antidiuretic hormone.[24] Several factors, such as older age, female gender, concomitant use of (thiazide) diuretics, a history of hyponatremia, low weight (<60 kg), psychosis, have been identified to increase the risk of hyponatremia induced by antidepressants.[3,4,25] In addition, COPD was also possibly one of the respiratory causes for SIADH.[17] Therefore, the older age (78-year-old), low weight (48 kg), and history of COPD could be the extra risk factors for our patient.
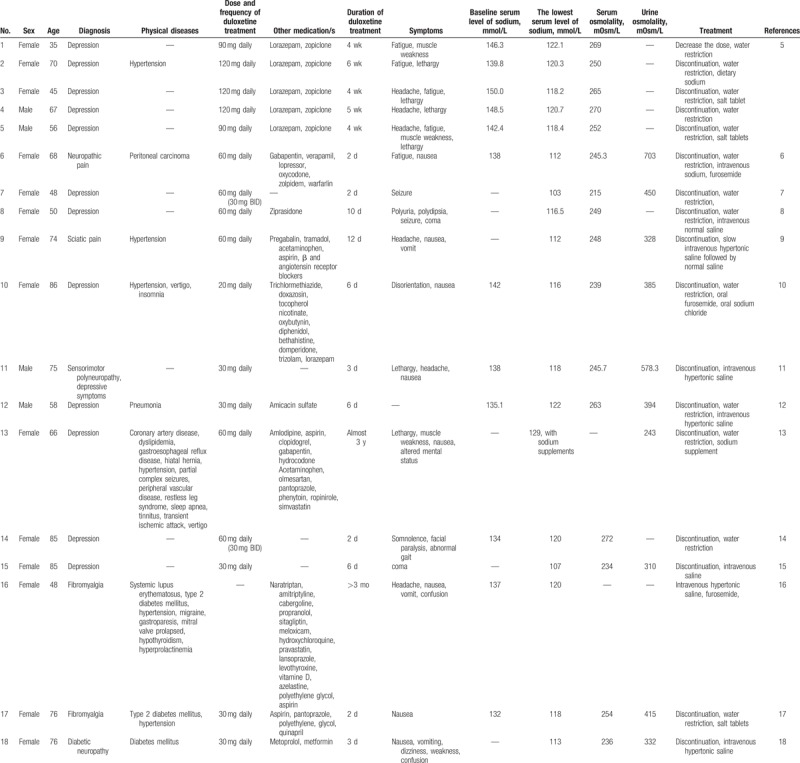
To better understand the features of duloxetine-related hyponatremia, we further reviewed the published relevant case reports and summarized the demographic and clinical characteristic of these individuals. As demonstrated in Table 1, only 26.3% (5/19, including our case, similarly hereinafter) of all patients was male, and 36.8% (7/19) was <65 years old. Most patients with duloxetine treatment are depressed and a few of them have neuropathic pain or fibromyalgia. Comorbid physical conditions included diabetic mellitus, hypertension, cardiovascular/cerebrovascular diseases, pneumonia, neurologic diseases, and even cancers. Most concomitant drugs were taken for these chronic diseases, and only 1 patient took diuretics (trichlormethiazide). The doses of duloxetine were different, and could be as low as 20 mg/daily and as high as 120 mg/daily. Hyponatremia could rapidly emerge after 2 days of duloxetine treatment, or delayed for several weeks or even months. Symptoms of duloxetine-induced hyponatremia were varying, including fatigue, weakness, lethargy, headache, nausea, dizziness, altered mental status and seizure as well. Some of these symptoms were mild and atypical, thus would be confused with the primary diseases and even be neglected. The average falling range of serum sodium concentration was 20.8 mmol/L in patients with duloxetine-induced hyponatremia. The overall prognosis was favorable in all patients after duloxetine withdrawal, water restriction, intravenous or oral supplement of sodium, or using diuretics (furosemide). It could be helpful for clinicians to better recognize and treat hyponatremia caused by duloxetine when getting hold of the aforementioned information.
Table 1.
Demographic and clinical profiles of patients with duloxetine-associated hyponatremia.
To conclude, we depict a case of rapid-onset hyponatremia following duloxetine treatment in an old male patient with post-herpetic neuralgia. Our work indicates the importance of continuous monitoring serum electrolyte when prescribing duloxetine, especially in patients with predisposing factors.
Acknowledgments
The authors thank the patient and her guardian for their understanding.
Author contributions
Funding acquisition: Shaojia Lu, Manli Huang, Shaohua Hu, Yi Xu.
Writing – original draft: Dandan Wang.
Writing – review and editing: Jianbo Lai, Shaojia Lu.
Footnotes
Abbreviations: COPD = chronic obstructive pulmonary disease, CSF = cerebrospinal fluid, SIADH = syndrome of inappropriate antidiuretic hormone, SNRIs = serotonin-norepinephrine reuptake inhibitors, SSRIs = selective serotonin reuptake inhibitors.
DW and JL equally contributed to the work.
This study was supported by grants from the National Natural Science Foundation of China (81601182), National Key Research and Development Program (2016YFC1307100, 2016YFC1307102), and the Key Research Project of Zhejiang Province (2015C03040).
The authors have no conflicts of interest to disclose.
References
- [1].Buffington MA, Abreo K. Hyponatremia: a review. J Intensive Care Med 2016;31:223–36. [DOI] [PubMed] [Google Scholar]
- [2].Gandhi S, Shariff SZ, Al-Jaishi A, et al. Second-generation antidepressants and hyponatremia risk: a population-based cohort study of older adults. Am J Kidney Dis 2017;69:87–96. [DOI] [PubMed] [Google Scholar]
- [3].Giorlando F, Teister J, Dodd S, et al. Hyponatremia: an audit of aged psychiatry patients taking SSRIs and SNRIs. Curr Drug Saf 2013;8:175–80. [DOI] [PubMed] [Google Scholar]
- [4].De Picker L, Van Den Eede F, Dumont G, et al. Antidepressants and the risk of hyponatremia: a class-by-class review of literature. Psychosomatics 2014;55:536–47. [DOI] [PubMed] [Google Scholar]
- [5].Krüger S, Lindstaedt M. Duloxetine and hyponatremia: a report of 5 cases. J Clin Psychopharmacol 2007;27:101–4. [DOI] [PubMed] [Google Scholar]
- [6].Safdieh JE, Rudominer R. A case of hyponatremia induced by duloxetine. J Clin Psychopharmacol 2006;26:675–6. [DOI] [PubMed] [Google Scholar]
- [7].Maramattom BV. Duloxetine-induced syndrome of inappropriate antidiuretic hormone secretion and seizures. Neurology 2006;66:773–4. [DOI] [PubMed] [Google Scholar]
- [8].Li RM, Wang C, Liu ZW, et al. A case of severe hyponatremia induced by duloxetine and ziprasidone. Chin Med J (Engl) 2012;125:3750–1. [PubMed] [Google Scholar]
- [9].Anwari JS, Hazazi AA. Another cause of headache after epidural injection. Neurosciences (Riyadh) 2015;20:167–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Mori M, Koide T, Imanishi Y, et al. Duloxetine-induced hyponatremia in an elderly patient treated with thiazide diuretics. Indian J Pharmacol 2014;46:657–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Demirci S, Demirci K, Altuntaş A, et al. Rapid-onset hyponatremia induced by duloxetine in an elderly patient. New Yeni Symposium 2015;53:20–2. [Google Scholar]
- [12].Choi JS, Lee HW, Lee JY, et al. Rapid-onset hyponatremia induced by duloxetine in a middle-aged male with depression and somatic symptoms. Psychiatry Investig 2012;9:83–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Stovall R, Brahm NC, Crosby KM. Recurrent episodes of serotonin-reuptake inhibitor-mediated hyponatremia in an elderly patient. Consult Pharm 2009;24:765–8. [DOI] [PubMed] [Google Scholar]
- [14].Dirks AC, van Hyfte DM. Recurrent hyponatremia after substitution of citalopram with duloxetine. J Clin Psychopharmacol 2007;27:313. [DOI] [PubMed] [Google Scholar]
- [15].Müssig K, Mörike K, Häring HU. Severe and symptomatic hyponatremia following duloxetine treatment. J Psychopharmacol 2009;23:338–9. [DOI] [PubMed] [Google Scholar]
- [16].Balaram M, Ford V, Townsend R. Symptomatic hyponatremia during glomerular filtration rate testing. NDT Plus 2010;3:539–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Amoako AO, Brown C, Riley T. Syndrome of inappropriate antidiuretic hormone secretion: a story of duloxetine-induced hyponatraemia. BMJ Case Rep 2015;2015. pii: bcr2014208037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Beydilli I, Akguc L, Korkmaz I, et al. Low dose duloxetine induced hyponatremia in an elderly patient: a case report. Bull Clin Psychopharmacol 2012;22:283–5. [Google Scholar]
- [19].Johnson RW, Rice AS. Postherpetic neuralgia. N Engl J Med 2014;371:1526–33. [DOI] [PubMed] [Google Scholar]
- [20].Gan EY, Tian EA, Tey HL. Management of herpes zoster and post-herpetic neuralgia. Am J Clin Dermatol 2013;14:77–85. [DOI] [PubMed] [Google Scholar]
- [21].Raskin J, Wiltse CG, Siegal A, et al. Efficacy of duloxetine on cognition, depression, and pain in elderly patients with major depressive disorder: an 8-week, double-blind, placebo-controlled trial. Am J Psychiatry 2007;164:900–9. [DOI] [PubMed] [Google Scholar]
- [22].Lunn MP, Hughes RA, Wiffen PJ. Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia. Cochrane Database Syst Rev 2014;CD007115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 1981;30:239–45. [DOI] [PubMed] [Google Scholar]
- [24].Arinzon ZH, Lehman YA, Fidelman ZG, et al. Delayed recurrent SIADH associated with SSRIs. Ann Pharmacother 2002;36:1175–7. [DOI] [PubMed] [Google Scholar]
- [25].Mannesse CK, Jansen PA, Van Marum RJ, et al. Characteristics, prevalence, risk factors, and underlying mechanism of hyponatremia in elderly patients treated with antidepressants: a cross-sectional study. Maturitas 2013;76:357–63. [DOI] [PubMed] [Google Scholar]


