Supplemental Digital Content is available in the text
Keywords: cardiovascular disease risk factors, high protein diet, meta-analysis, type 2 diabetes
Abstract
Currently, the prevalence of type 2 diabetes is still increasing worldwide and has become a major public health burden.
This meta-analysis was performed to further assess high protein (HP) diet on body weight, glycemic control, and cardiovascular disease risk factors in type 2 diabetes.
A literature search was conducted in PubMed and Embase databases up to June 2018. The pooled standard mean difference (SMD) and the corresponding 95% confidence interval (CI) were calculated using RevMan 5.3 software.
In total, 18 randomized control trials involving 1099 adults with type 2 diabetes were included. Pooled results indicated that HP diet could not significantly affect blood pressure of patients with type 2 diabetes, compared with low protein (LP) diet. However, the overall analyses showed the significant effect of HP diet on triglycerides reduction (SMD = −0.20, 95% CI = −0.35 to −0.05, P = .01) in patients with type 2 diabetes, compared with LP diet. Subgroup analyses showed that the ratio of energy from fat and carbohydrate in diet could affect the effect of HP diet on weight and triglyceride.
HP diet could be indicated to obtain beneficial results in weight loss and lipid metabolism.
1. Introduction
Currently, the prevalence of type 2 diabetes is still increasing worldwide[1] and has become a major public health burden.[2] Type 2 diabetes is characterized by insulin resistance in most subjects and approximately 80% of patients with type 2 diabetes are overweight or obese. Obesity and insulin resistance are all associated with the risk factors of cardiovascular diseases.[3–5] Weight management is a major component of effective diabetes care, which can significantly improve the cardiovascular diseases markers (such as blood pressure, high-density lipoprotein cholesterol [HDL], and triglycerides [TG]) and glycemic control.[6,7] Thus, long-term weight management is essential for the patients with type 2 diabetes.
The dietary approach to weight loss and treating type 2 diabetes is commonly used in clinical practice. Many studies suggest nutrient composition (both in energy restriction and energy balance) of dietary strategies may be important and affect glucose and lipid profile in diabetes patients.[8–11] However, the optimal diet for people with diabetes is still unknown. High protein (HP) diet has been frequently used for weight loss in obese people. Currently, some studies have proved that a HP intake can enhance weight loss, glycemic control, and cardiovascular disease risk factors.[6,12,13] A previous meta-analysis has proved beneficial effects on weight loss, HbA1c, and blood pressure.[14] However, the controversies still exist among recent published studies.[12,15–17]
We speculated that the HP diet is benefit for the diabetes patients. Therefore, we performed this updated meta-analysis to further confirm the effect of HP diet on weight loss, glycemic control, and cardiovascular disease risk factors. In addition, the secondary purpose was to assess the effect of ratio of energy from carbohydrate and fat in diets on the results by subgroup analysis.
2. Materials and methods
2.1. Search strategy
A literature search was conducted in PubMed and Embase databases up to June 2018. The following key words were used: (“type 2 diabetes” or “diabetes”) and (“diet” or “diets” or “dietary” or “protein” or “high protein”) and “randomized.” In addition, we also manually scanned the reference lists of some relevant reviews to select additional studies.
2.2. Inclusion and exclusion criteria
All included studies should meet the following criteria: the study type was randomized control trial (RCT); participants were patients with diabetes; the HP and low protein (LP) diets were applied and compared; the intervention of HP diet was kept for ≥1 month (or 4 weeks); the weight loss, glycemic control, blood lipids change, or blood pressure change after diet intervention in each group was investigated.
The exclusion criteria were: comparison was not performed based on diet composition; the ratio of energy from protein in diet intervention was equal between groups; duplicated publications; no available data; and letters, comments, or reviews.
2.3. Data extraction and quality assessment
Two investigators independently reviewed the full texts of included studies and assessed their quality. Differences were resolved by discussion to ensure consistency. The following data should be recorded in a predesigned form: first author, year of publication, country, sample size, age, sex, the duration of intervention, diets component, and the outcomes.
In addition, the design, execution, and reporting of the included studies were assessed using the Cochrane risk of bias tool, which included the following items: random sequence generation and allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), and selective reporting (reporting bias).
2.4. Statistical analysis
All analyses were performed using RevMan 5.3 software. The chi-squared and I2 tests were used to assess the heterogeneity among studies. A P value < .1 or I2 > 50% indicated the existence of significant heterogeneity. An appropriate statistical model (random- or fixed-effects model) was used to calculate the pooled standard mean difference (SMD) as well as the corresponding 95% confidence interval (CI) based on the results of heterogeneity testing. In addition, the subgroup analyses were performed based on the diet composition. The sensitivity analysis was performed to evaluate the stability of the results by removing each individual study from the pooled analysis. The publication bias was assessed using the funnel plot.
3. Results
3.1. Characteristics of included studies
After the initial literature search, totally 1022 articles were found (450 from PubMed and 572 from Embase). After excluding duplicates, 318 potentially relevant articles remained. Among them, 230 irrelevant articles were removed by scanning the titles; 59 articles were excluded by reading abstracts based on the inclusion and exclusion criteria. Then 11 articles were excluded by reading the full texts. Finally, 18 studies[11–13,15–29] were included in this meta-analysis. In addition, no additional studies were selected by manual search (Fig. 1).
Figure 1.
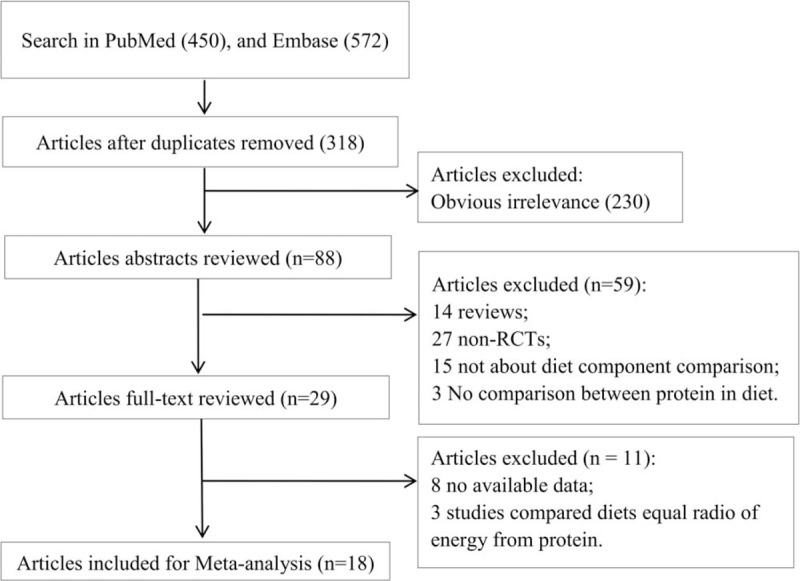
Literature search and study selection.
The characteristics of these included studies were shown in Table 1. A total of 1099 adults with diabetes were reanalyzed in this meta-analysis. The publication year was from 2002 to 2018. These studies were, respectively, conducted in Australia (n = 7), the United States (n = 6), New Zealand (n = 1), Greece (n = 1), Sweden (n = 1), and the United Kingdom (n = 2). The subjects were all patients with type 2 diabetes. The duration of diet intervention ranged from 4 weeks to 24 months. The baseline weight/body mass index (BMI) was similar between groups in each included study. In addition, risk of bias in most studies was low or unclear, but high risk of performance bias was shown in all the included studies due to no blinding of subject or implementer (see Supplementary Table 1 and Fig. 2). Detection or other bias risk may exist in some studies due to less rigorous study design or procedure.
Table 1.
Characteristics of included studies.
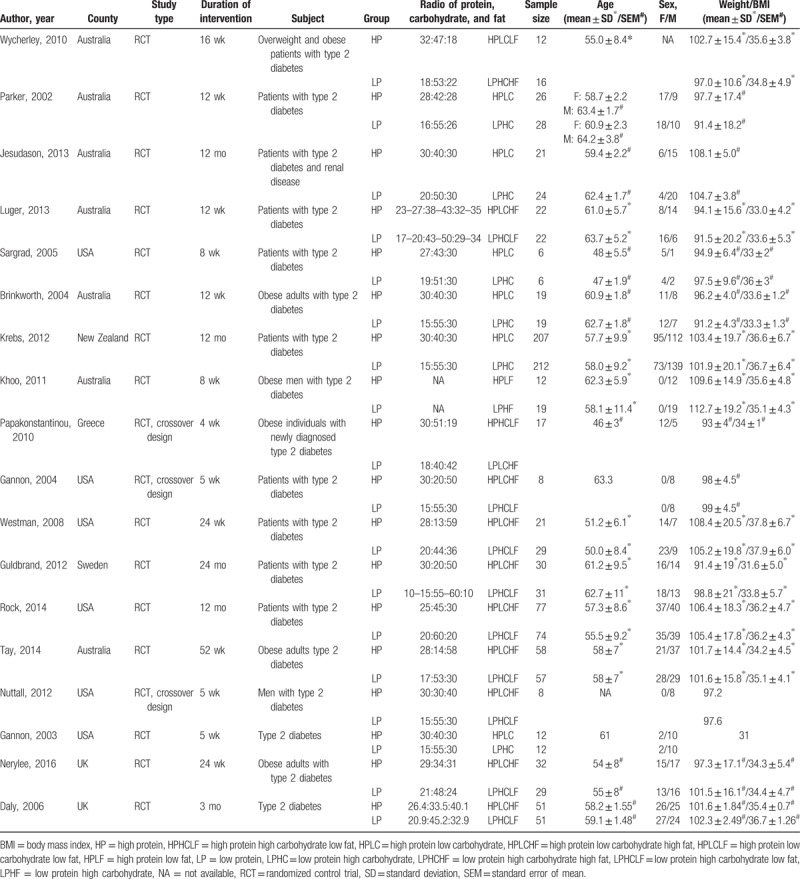
Figure 2.
Risk of bias graph and risk of bias summary.
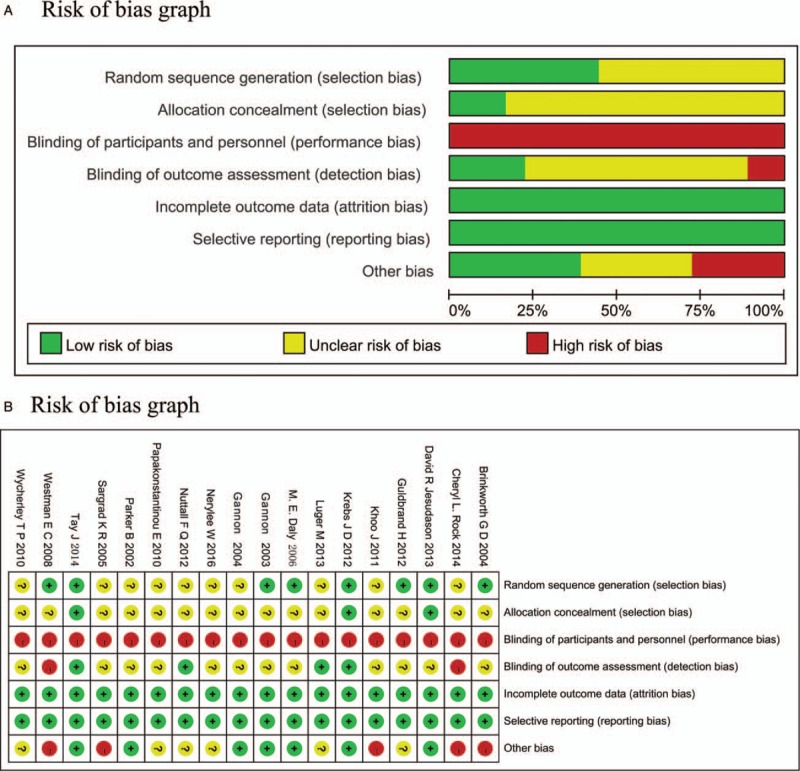
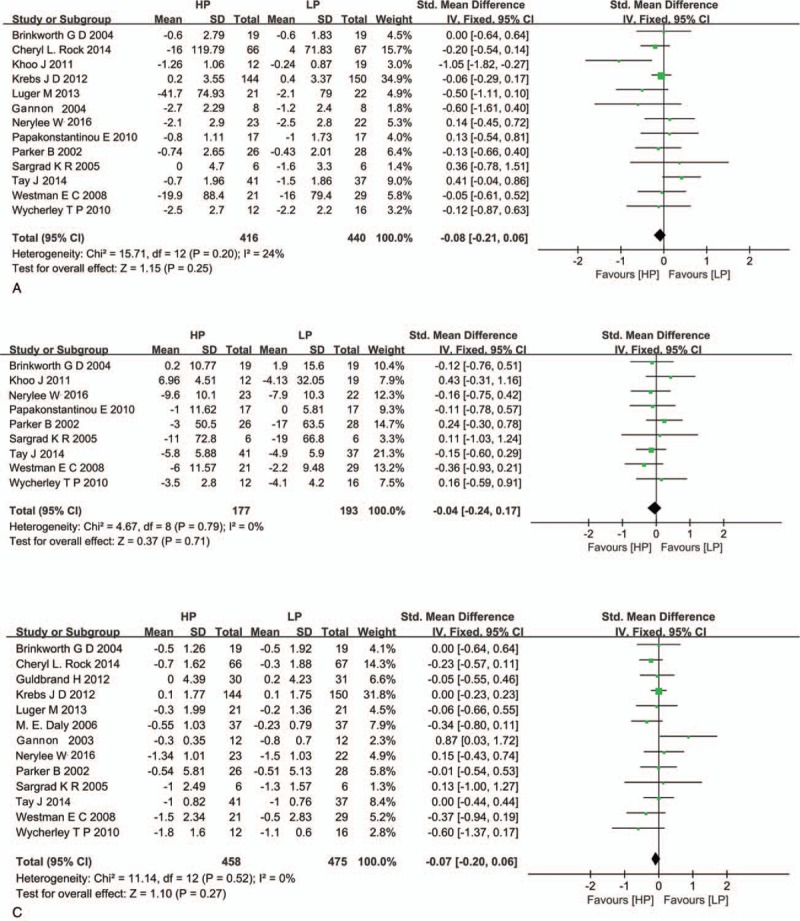
3.2. Effect of HP diet on weight loss
Most of these included studies investigated the effect of HP diet on weight loss. No significant heterogeneity was found among these studies (I2 = 0%, P > .10), so the pooled SMDs were calculated by fixed-effects model. Results showed that the HP diet did not significantly affect the body weight compared with LP diet (SMD = −0.09, 95% CI = −0.21 to 0.04, P = .17, Fig. 3A). Similarly, there was also no significant difference between HP and LP groups in BMI (SMD = −0.06, 95% CI = −0.24 to 0.12, P = .49, Fig. 3B), fat mass (SMD = −0.01, 95% CI = −0.18 to 0.15, P = .88, Fig. 3C), and fat-free mass (SMD = −0.04, 95% CI = −0.27 to 0.20, P = .76, Fig. 3D). These results indicated that the weight loss of patients with type 2 diabetes HP diet could not affected by the ratio of energy from protein in diet.
Figure 3.
Meta-analysis for effect of high protein diet on body weight (A), body mass index (B), fat mass (C), and fat-free mass (D).
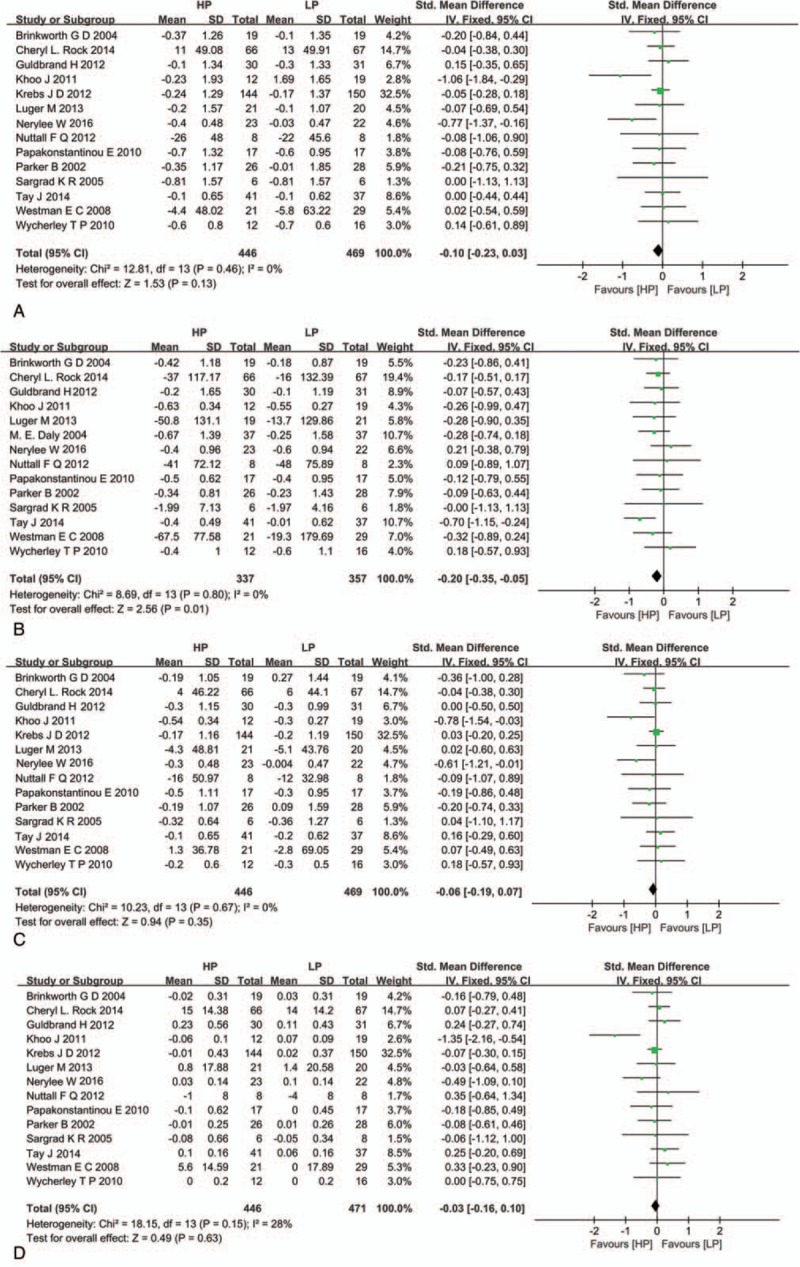
3.3. Effect of HP diet on glycemic control
Figure 4 shows the results of meta-analysis for effect of HP diet on glycemic control. No significant evidence of heterogeneity among studies was found in the analysis for fasting glucose, fasting insulin, and HbA1c (I2 < 50%, P > .10). Thus, the fixed-effects model was applied, respectively. The pooled estimate indicated that the change of fasting glucose (SMD = −0.08, 95% CI = −0.21 to 0.06, P = .25, Fig. 4A), fasting insulin (SMD = −0.04, 95% CI = −0.24 to 0.17, P = .71, Fig. 4B), and HbA1c (SMD = −0.07, 95% CI = −0.20 to 0.06, P = .27, Fig. 4C) after HP and LP diets were similar, suggesting that the ratio of energy from protein in diets did not affect the glycemic control in patients with type 2 diabetes.
Figure 4.
Meta-analysis for effect of high protein diet on fasting glucose (A), fasting insulin (B), and HbA1c (C).
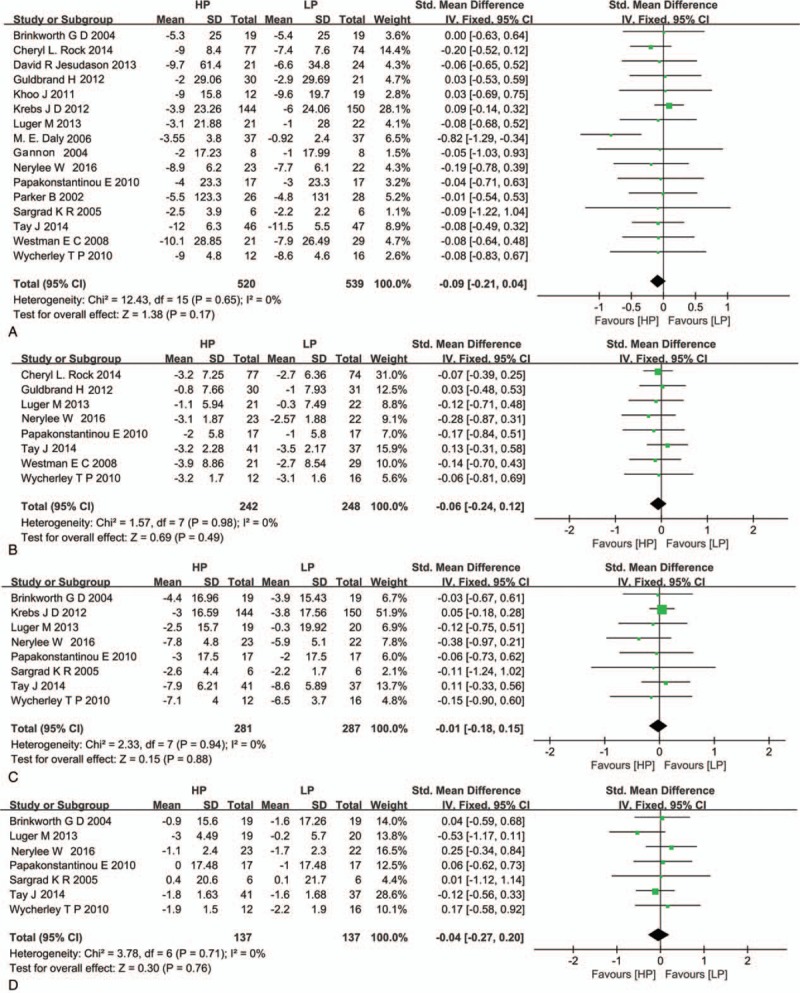
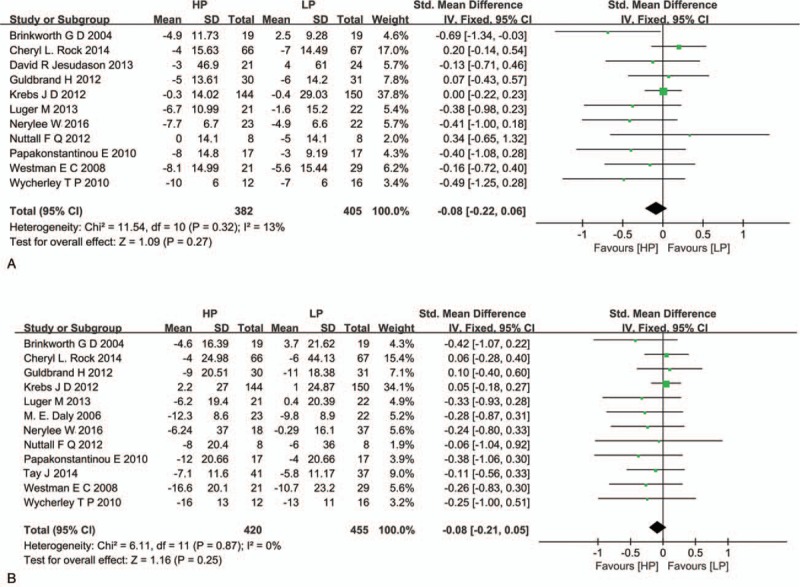
3.4. Effect of HP diet on lipid metabolism
The effects of HP diet on blood lipid levels were investigated by 14 included studies. There was no significant heterogeneity (I2 < 50%, P > .10) among these studies in the analysis for total cholesterol (TC), TG, low-density lipoprotein cholesterol (LDL), and HDL, and then the fixed-effects model was applied to pool the data. The results showed that the HP diet could significantly increase the reduction of TG (SMD = −0.20, 95% CI = −0.35 to −0.05, P = .01, Fig. 5B) but not significantly affect the TC (SMD = −0.10, 95% CI = −0.23 to 0.03, P = .13, Fig. 5A), LDL (SMD = −0.06, 95% CI = −0.19 to 0.07, P = .35, Fig. 5C), and HDL (SMD = −0.03, 95% CI = −0.16 to 0.10, P = .63, Fig. 5D) levels compared with the LP diet.
Figure 5.
Meta-analysis for effect of high protein diet on total cholesterol (A), triglycerides (B), low-density lipoprotein cholesterol (C), and high-density lipoprotein cholesterol (D).
3.5. Effect of HP diet on blood pressure
Figure 6 shows the pooled estimate for the effect of HP diet on blood pressure. No significant heterogeneity suggested the use of fixed-effects model in the meta-analysis (I2 < 50%, P > .10). The pooled estimate indicated that the change of diastolic (SMD = −0.08, 95% CI = −0.22 to 0.06, P = .27, Fig. 6A) and systolic (SMD = −0.08, 95% CI = −0.21 to −0.05, P = .25, Fig. 6B) blood pressures was not significantly affected by HP diet in HP group compared with that in LP group.
Figure 6.
Meta-analysis for effect of high protein diet on diastolic (A) and systolic (B) blood pressures.
3.6. Subgroup analysis
In total, 6 studies compared the HP low carbohydrate (HPLC) and LP high carbohydrate (LPHC) diets (which showed similar ratio of energy from fat) and 9 studies compared HPLC high fat (HPLCHF) and LPHC low fat (LPHCLF) diets. The results of subgroup analyses were shown in Table 2.
Table 2.
Results of subgroup analysis.
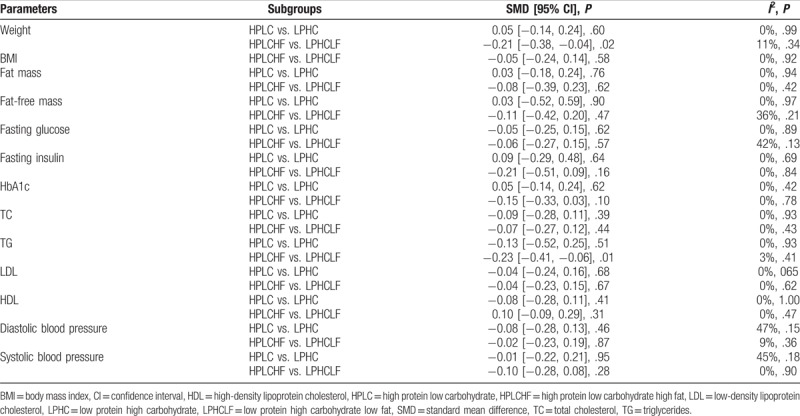
In subgroup analyses, the significant effect of HP diet on TG disappeared in subgroup analysis of HPLC versus LPHC diets (SMD = −0.13, 95% CI = −0.52 to 0.25, P = .51), which were inconsistent with the overall analyses. Meanwhile, the inconsistent results with the overall meta-analyses were also found in the subgroup analyses for weight. These results showed significant effect of HPLCHF diet on weight loss compared with LPHCLF diet (SMD = −0.21, 95% CI = −0.38 to −0.04, P = .02).
3.7. Sensitivity analysis and publication bias
Sensitivity analysis showed that after omitting the data of the studies of Krebs 2012 (SMD = −0.15, 95% CI = −0.30 to −0.01, P = .04), the result of analysis for weight was changed; after excluding the study of Tay 2014, the results of analyses for TG (SMD = −0.14, 955 CI = −0.30 to 0.02, P = .09) were affected.
In addition, the funnel plot (based on the data of weight) showed the study of Daly 2006 significantly deviate from the central axis (Fig. 7). However, sensitivity analysis showed no change of study result after excluding the study of Daly 2006.
Figure 7.
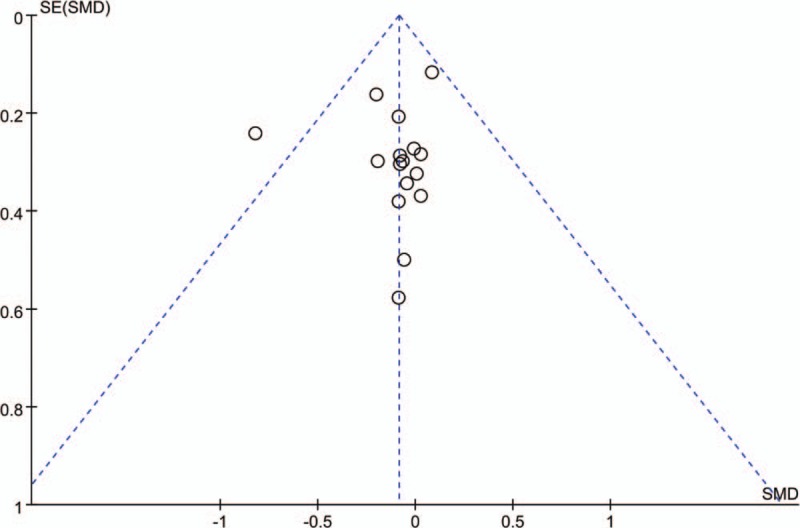
Funnel plot based on the analysis for body weight.
4. Discussion
In this meta-analysis, the results were inconsistent with that in the previous meta-analysis.[14] In the present meta-analysis, results showed that the HP diet could not significantly improve the weight loss, glycemic control of patients with type 2 diabetes but there may be significant effect of HP diet on lipid metabolism. The inconsistent results may be caused by the difference in included studies. The present studies included more studies and the sample size was larger than that in the previous study.[14] Moreover, beside body weight, BMI, fat mass, and fat-free mass were also assessed in this meta-analysis to provide more evidences for the effect of HP diet on weight loss; fasting insulin was also analyzed to show the effect of HP diet on glycemic control. In addition, sensitivity analyses and subgroup analyses all indicated consistent results with the overall analysis for the parameters of weight loss and glycemic control. Thus, this meta-analysis provided more evidences to prove no significant effect of HP diet on weight loss and glycemic control in patients with type 2 diabetes, compared with LP diet.
The results also showed that HP diet could significantly affect the TG level of patients with type 2 diabetes, when compared with the LP diets. Sensitivity analysis showed that, after excluding the study of Tay 2014 (HPLCHF vs. LPHCLF), the results changed. Meanwhile, subgroup analyses by HPLC versus LPHC (equal ratio of energy from fat) showed the inconsistent results with the overall analyses. These results indicated that the ratio of energy from fat or carbohydrate in diet may affect the effect of HP diet on TG level. As known for us, HF diets can induce the change of lipid metabolism.[30,31] Moreover, it was reported different carbohydrate and types of fat intake could result in different TG levels.[32,33] Thus, it is important to further explore the effect of ratio of energy from fat or carbohydrate in diet on the results and confirm the optimal nutrition component. Similarly, for weight, sensitivity analysis showed that, after excluding the study of Krebs 2012 (HPLC vs. LPHC), the significant effect of HP diet on weight loss presented. Subgroup analyses also showed that the effect of HP diet on weight may be affected by the ratio of energy from fat or carbohydrate in diet. The patients received HPLCHF diet is benefit for weight loss than LPHCLF. More studies should be performed to confirm the results of this study.
In addition, TG is one of the risk factors of cardiovascular diseases.[34,35] These results indicated HP diet is of benefit for the improvement of risk factors of cardiovascular diseases, and then decrease the risk of cardiovascular diseases in patients with type 2 diabetes. Thus, the HP diet may be benefit for reducing risk of cardiovascular diseases in patients with type 2 diabetes. The investigation on it will be performed in future studies.
There were some limitations in this meta-analysis. First, the treatment time of these studies was greatly different, from 4 weeks to 24 months, which could be another barrier for subgroup analysis. Second, there were many confounding factors (such as country, ethnicity, study design, duration of intervention), which may affect the results of this meta-analysis. Besides, nonsignificant different was found in weight loss, glycemic control, and blood pressure, which may be caused by the impact of some important variables that influence the metabolism sex, age, and duration of intervention. Thus, the results of this study should be further verified by more RCTs with larger sample size and longer follow up.
5. Conclusion
In conclusion, HP diet could be indicated to obtain beneficial results in weight loss and lipid metabolism. Based on the radio in all the included studies, the HP diet with about 30% protein is appropriate. The broader implications of HP diet on patients with type 2 diabetes should be further investigated.
Author contributions
Conceptualization: Wen-Ting Zhao, Ting-Ting Zhao.
Data curation: Wen-Ting Zhao.
Formal analysis: Wen-Ting Zhao.
Funding acquisition: Ting-Ting Zhao.
Investigation: Yu Luo.
Methodology: Yu Luo, Ying Zhang, Ting-Ting Zhao.
Project administration: Yu Luo, Ting-Ting Zhao.
Software: Wen-Ting Zhao, Yun Zhou.
Supplementary Material
Footnotes
Abbreviations: BMI = body mass index, CI = confidence interval, HDL = high-density lipoprotein cholesterol, HP = high protein, HPLC = high protein low carbohydrate, HPLCHF = high protein low carbohydrate high fat, LDL = low-density lipoprotein cholesterol, LP = low protein, LPHC = low protein high carbohydrate, LPHCLF = low protein high carbohydrate low fat, RCT = randomized control trial, SMD = standard mean difference, TC = total cholesterol, TG = triglycerides.
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Guariguata L, Whiting DR, Hambleton I, et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 2014;103:137–49. [DOI] [PubMed] [Google Scholar]
- [2].Hahr AJ, Molitch ME. Diabetes, cardiovascular risk and nephropathy. Cardiol Clin 2010;28:467–75. [DOI] [PubMed] [Google Scholar]
- [3].Casanueva FF, Moreno B, Rodriguez-Azeredo R, et al. Relationship of abdominal obesity with cardiovascular disease, diabetes and hyperlipidaemia in Spain. Clin Endocrinol (Oxf) 2010;73:35–40. [DOI] [PubMed] [Google Scholar]
- [4].Hinnouho GM, Czernichow S, Dugravot A, et al. Metabolically healthy obesity and the risk of cardiovascular disease and type 2 diabetes: the Whitehall II cohort study. Eur Heart J 2015;36:551–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Paneni F, Costantino S, Cosentino F. Insulin resistance, diabetes, and cardiovascular risk. Curr Atheroscler Rep 2014;16:419. [DOI] [PubMed] [Google Scholar]
- [6].Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 2011;34:1481–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Horton ES, Silberman C, Davis KL, et al. Weight loss, glycemic control, and changes in cardiovascular biomarkers in patients with type 2 diabetes receiving incretin therapies or insulin in a large cohort database. Diabetes Care 2010;33:1759–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Larsen RN, Mann NJ, Maclean E, et al. The effect of high-protein, low-carbohydrate diets in the treatment of type 2 diabetes: a 12 month randomised controlled trial. Diabetologia 2011;54:731–40. [DOI] [PubMed] [Google Scholar]
- [9].Castaneda-Gonzalez LM, Bacardi GM, Jimenez CA. Effects of low carbohydrate diets on weight and glycemic control among type 2 diabetes individuals: a systemic review of RCT greater than 12 weeks. Nutr Hosp 2011;26:1270–6. [DOI] [PubMed] [Google Scholar]
- [10].Wolfram T, Ismail-Beigi F. Efficacy of high-fiber diets in the management of type 2 diabetes mellitus. Endocr Pract 2011;17:132–42. [DOI] [PubMed] [Google Scholar]
- [11].Parker B, Noakes M, Luscombe N, et al. Effect of a high-protein, high-monounsaturated fat weight loss diet on glycemic control and lipid levels in type 2 diabetes. Diabetes Care 2002;25:425–30. [DOI] [PubMed] [Google Scholar]
- [12].Rock CL, Flatt SW, Pakiz B, et al. Weight loss, glycemic control, and cardiovascular disease risk factors in response to differential diet composition in a weight loss program in type 2 diabetes: a randomized controlled trial. Diabetes Care 2014;37:1573–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sargrad KR, Homko C, Mozzoli M, et al. Effect of high protein vs high carbohydrate intake on insulin sensitivity, body weight, hemoglobin A1c, and blood pressure in patients with type 2 diabetes mellitus. J Am Diet Assoc 2005;105:573–80. [DOI] [PubMed] [Google Scholar]
- [14].Dong JY, Zhang ZL, Wang PY, et al. Effects of high-protein diets on body weight, glycaemic control, blood lipids and blood pressure in type 2 diabetes: meta-analysis of randomised controlled trials. Br J Nutr 2013;110:781–9. [DOI] [PubMed] [Google Scholar]
- [15].Jesudason DR, Pedersen E, Clifton PM. Weight-loss diets in people with type 2 diabetes and renal disease: a randomized controlled trial of the effect of different dietary protein amounts. Am J Clin Nutr 2013;98:494–501. [DOI] [PubMed] [Google Scholar]
- [16].Luger M, Holstein B, Schindler K, et al. Feasibility and efficacy of an isocaloric high-protein vs. standard diet on insulin requirement, body weight and metabolic parameters in patients with type 2 diabetes on insulin therapy. Exp Clin Endocrinol Diabetes 2013;121:286–94. [DOI] [PubMed] [Google Scholar]
- [17].Tay J, Luscombe-Marsh ND, Thompson CH, et al. A very low-carbohydrate, low-saturated fat diet for type 2 diabetes management: a randomized trial. Diabetes Care 2014;37:2909–18. [DOI] [PubMed] [Google Scholar]
- [18].Wycherley TP, Noakes M, Clifton PM, et al. A high-protein diet with resistance exercise training improves weight loss and body composition in overweight and obese patients with type 2 diabetes. Diabetes Care 2010;33:969–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Brinkworth GD, Noakes M, Parker B, et al. Long-term effects of advice to consume a high-protein, low-fat diet, rather than a conventional weight-loss diet, in obese adults with type 2 diabetes: one-year follow-up of a randomised trial. Diabetologia 2004;47:1677–86. [DOI] [PubMed] [Google Scholar]
- [20].Krebs JD, Elley CR, Parry-Strong A, et al. The Diabetes Excess Weight Loss (DEWL) trial: a randomised controlled trial of high-protein versus high-carbohydrate diets over 2 years in type 2 diabetes. Diabetologia 2012;55:905–14. [DOI] [PubMed] [Google Scholar]
- [21].Papakonstantinou E, Triantafillidou D, Panagiotakos DB, et al. A high-protein low-fat diet is more effective in improving blood pressure and triglycerides in calorie-restricted obese individuals with newly diagnosed type 2 diabetes. Eur J Clin Nutr 2010;64:595–602. [DOI] [PubMed] [Google Scholar]
- [22].Gannon MC, Nuttall FQ. Effect of a high-protein, low-carbohydrate diet on blood glucose control in people with type 2 diabetes. Diabetes 2004;53:2375–82. [DOI] [PubMed] [Google Scholar]
- [23].Khoo J, Piantadosi C, Duncan R, et al. Comparing effects of a low-energy diet and a high-protein low-fat diet on sexual and endothelial function, urinary tract symptoms, and inflammation in obese diabetic men. J Sex Med 2011;8:2868–75. [DOI] [PubMed] [Google Scholar]
- [24].Westman EC, Yancy WJ, Mavropoulos JC, et al. The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutr Metab (Lond) 2008;5:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Guldbrand H, Dizdar B, Bunjaku B, et al. In type 2 diabetes, randomisation to advice to follow a low-carbohydrate diet transiently improves glycaemic control compared with advice to follow a low-fat diet producing a similar weight loss. Diabetologia 2012;55:2118–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Nuttall FQ, Gannon MC. Effect of a LoBAG30 diet on protein metabolism in men with type 2 diabetes. A randomized controlled trial. Nutr Metab (Lond) 2012;9:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Daly ME, Paisey R, Millward BA, et al. Short-term effects of severe dietary carbohydrate-restriction advice in type 2 diabetes—a randomized controlled trial. Diabetic Med 2006;23:15–20. [DOI] [PubMed] [Google Scholar]
- [28].Gannon MC, Nuttall FQ, Saeed A, et al. An increase in dietary protein improves the blood glucose response in persons with type 2 diabetes. Am J Clin Nutr 2003;78:734–41. [DOI] [PubMed] [Google Scholar]
- [29].Nerylee W, Kathryn D, Jonathan B, et al. Effects of low-fat diets differing in protein and carbohydrate content on cardiometabolic risk factors during weight loss and weight maintenance in obese adults with type 2 diabetes. Nutrients 2016;8:289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Gaidhu MP, Anthony NM, Patel P, et al. Dysregulation of lipolysis and lipid metabolism in visceral and subcutaneous adipocytes by high-fat diet: role of ATGL, HSL, and AMPK. Am J Physiol Cell Physiol 2010;298:C961–71. [DOI] [PubMed] [Google Scholar]
- [31].Jung CH, Cho I, Ahn J, et al. Quercetin reduces high-fat diet-induced fat accumulation in the liver by regulating lipid metabolism genes. Phytother Res 2013;27:139–43. [DOI] [PubMed] [Google Scholar]
- [32].Schwingshackl L, Hoffmann G. Comparison of effects of long-term low-fat vs high-fat diets on blood lipid levels in overweight or obese patients: a systematic review and meta-analysis. J Acad Nutr Diet 2013;113:1640–61. [DOI] [PubMed] [Google Scholar]
- [33].Knuiman JT, West CE, Katan MB, et al. Total cholesterol and high density lipoprotein cholesterol levels in populations differing in fat and carbohydrate intake. Arteriosclerosis 1987;7:612–9. [DOI] [PubMed] [Google Scholar]
- [34].Sarwar N, Danesh J, Eiriksdottir G, et al. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation 2007;115:450–8. [DOI] [PubMed] [Google Scholar]
- [35].Nakamura Y, Iso H, Kita Y, et al. Egg consumption, serum total cholesterol concentrations and coronary heart disease incidence: Japan Public Health Center-based prospective study. Br J Nutr 2006;96:921–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


