Highlights
-
•
The most frequent and severe complication after laparoscopic sleeve gastrectomy is gastric leak.
-
•
The endoscopic placement of a double-pigtail drain across the leak has been proven to be effective and minimally invasive.
-
•
Drain’s migration into the abdominal cavity is not common and its intrasplenic displacement is even more rare.
-
•
Pigtail drain migration involving the spleen may expose the patient to the risk of parenchymal abscess or haemorrhage.
Keywords: Case report, Gastric leak, Pigtail, Internal drainage, Intrasplenic migration
Abstract
Introduction
The most frequent and severe complication after laparoscopic sleeve gastrectomy is gastric leak. Nowadays, there is no specific standard recommendation for its management, but the endoscopic placement of a double-pigtail drain across the leak has been proven to be effective and minimally invasive. Stent displacement into the abdominal cavity is not common and intrasplenic migration is even more rare.
Case presentation
We report a case of a 49-year-old woman with intrasplenic displacement of an endoscopic double-pigtail stent as a treatment for laparoscopic sleeve gastrectomy leak.
Discussion
Pigtail drain migration involving the spleen is rare but may potentially expose the patient to the risk of parenchymal abscess or haemorrhage. Often the clinic does not indicate early this complication.
Conclusion
We underline the need for a close radiologic follow-up, regardless of clinical conditions, in all patients treated with double-pigtail drain and its early removal in case of migration.
1. Introduction
The most frequent and severe complication after laparoscopic sleeve gastrectomy (LSG) is gastric leak (1–20%), that can lead to abdominal sepsis or chronic gastric fistula [1]. Nowadays, there is no specific standard recommendation for its management, but the current algorithm includes drainage, antibiotics and nutritional support [2]. Among the endoscopic procedures, the placement of an internal double-pigtail drain across the leak has been proven to be effective and minimally invasive, but not free of complications [3,4]. Drain’s migration into the abdominal cavity is not common and its intrasplenic displacement is even more rare. Only two cases are described in literature [3,5]. We report a new case because this complication could be, very likely, deadly. The work reported is in line with the SCARE criteria [6].
2. Case presentation
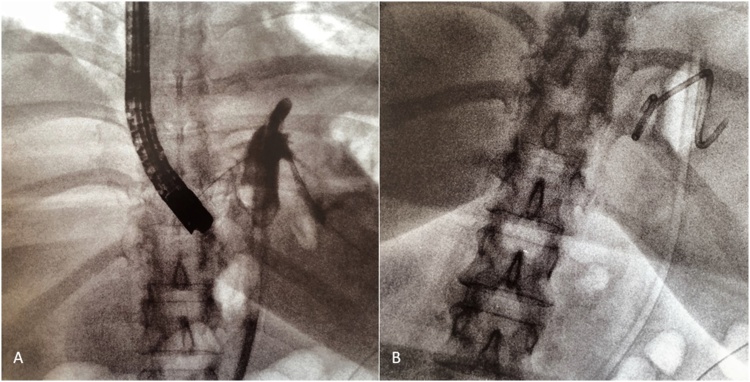
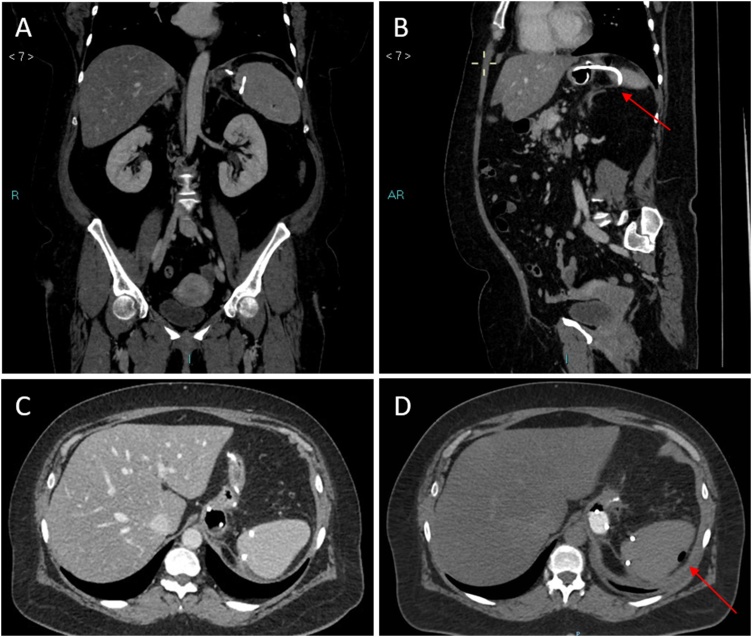
The patient was a 49-year-old woman with a body mass index (BMI) of 40.8 kg/m2 who underwent a laparoscopic sleeve gastric resection on May 2018 in our centre. She did not take drugs, and had no history of significant diseases. Six days after surgery, she presented with tachycardia, dyspnea and fever (38 °C). The abdomen was tender, without signs of peritonitis. Blood tests revealed an increased white blood cell count of 11.84 migl/mmc, a C-reactive protein level of 10.23 mg/dl and a procalcitonin level of 0.74 ng/ml. A TC scan of the abdomen was performed after oral administration of water-soluble contrast medium, and it was suggestive of a proximal staple-line leak with abdominal collection in left hypochondrium and left lumbar. A surgical laparoscopic management was decided: two abdominal drain tubes were placed, and a 8.5 Fr, 2-cm lenght double-pigtail stent was endoscopically delivered by our reference endoscopists through the fistula orifice into the collection (Fig. 1). A repeat scan after administration of oral water-soluble contrast performed 10 days after endoscopic procedure revealed the presence of pigtail drainage with an endo-luminal end and an extra-luminal end, with an associated blind-ending cavity of about 3 cm. About 20 days after pigtail placement, a control CT scan was performed, which showed the external tip of the tube in close proximity to the medial side of the spleen, with partial intra-splenic displacement, but without parenchymal or vascular damage. The presence of air in the subcapsular region confirmed intrasplenic displacement of the drain (Fig. 2). At that time, the patient was completely asymptomatic and underwent endoscopic pigtail removal, without any bleeding. The last CT scan confirmed no laceration of the splenic parenchyma and no vessel injury or extravasation of contrast medium. At a 3-month follow-up the patient presented no further complications.
Fig. 1.
(A, B) – 8.5 Fr, 2-cm lenght double-pigtail stent was endoscopically delivered through the fistula orifice into the abdominal collection.
Fig. 2.
(A– D) – Abdominal computed tomographic scan with intravenous contrast, showing partial intrasplenic displacement of the double-pigtail stent, more evident in oblique projection along the axis of the vessel (red arrow in B).
The presence of air in the subcapsular region confirmed intrasplenic displacement of the drain (red arrow in D).
3. Discussion
In our paper we reported a case of partial intrasplenic displacement of a double-pigtail stent following internal drainage for a post-LSG leak, that required endoscopic removal. Also the case reported by Donatelli et al. [3], in which double-pigtail stent migration was responsible for the laceration of the splenic parenchyma without vessels injury, required endoscopic removal. In the case reported by Genser et al. [5], the migration of the drain was complicated by a splenic abscess and portal, splenic, and hepatic venous gas. In our case, as occured in the case described by Donatelli et al. [3], the patient had no symptoms and the discovery of the displaced drainage was occasional. Considering therefore the lack of reliability of the clinic and the severity of the damage that could be caused by drainage displacement, we would be led to strongly recommend the execution of a close radiologic follow-up.
4. Conclusion
Pigtail drain migration involving the spleen is rare but may potentially expose the patient to the risk of parenchymal abscess or haemorrhage. To early detect this condition, we suggests the need for a close radiologic follow-up, regardless of clinical conditions, in all patients treated with double-pigtail drain, and its early removal in case of migration.
Conflicts of interest
No conflict of interest.
Sources of funding
NO source of funding.
Ethical approval
This study was approved by the Research Ethics Committee of the University of L’Aquila.
Consent
The authors obtained patient consent to use all the images presented.
Author contribution
Romano Lucia, Giuliani Antonio: Writing the paper.
Cianca Giovanni, Di Sibio Alessandra: Data collection and analysis.
Carlei Francesco, Amicucci Gianfranco, Schietroma Mario: Study concept.
Romano Lucia, Giuliani Antonio, Cianca Giovanni, Di Sibio Alessandra, Carlei Francesco, Amicucci Gianfranco, Schietroma Mario:Critical revision.
Registration of research studies
NA.
Guarantor
Prof. Mario Schietroma.
Provenance and peer review
Not commissioned externally peer reviewed.
Acknowledgments
All authors disclose the absence of any financial and personal relationships with other people or organizations that could inappropriately influence (bias) their work.
References
- 1.Tan J.T., Kariyawasam S., Wijeratne T. Diagnosis and management of gastric leaks after laparoscopic sleeve gastrectomy for morbid obesity. Obes. Surg. 2010;20(4):403–409. doi: 10.1007/s11695-009-0020-7. [DOI] [PubMed] [Google Scholar]
- 2.Donatelli G., Ferretti S., Vergeau B.M. Endoscopic internal drainage with enteral nutrition (EDEN) for treatment of leaks following sleeve gastrectomy. Obes. Surg. 2014;24:1400–1407. doi: 10.1007/s11695-014-1298-7. [DOI] [PubMed] [Google Scholar]
- 3.Donatelli G., Airinei G., Poupardin E. Double-pigtail stent migration invading the spleen: rare potentially fatal complication of endoscopic internal drainage for sleeve gastrectomy leak. Endoscopy. 2016;48(Suppl. 1):E74–5. doi: 10.1055/s-0042-102446. UCTN. [DOI] [PubMed] [Google Scholar]
- 4.Garofalo F., Noreau-Nguyen M., Denis R. Evolution of endoscopic treatment of sleeve gastrectomy leaks: from partially covered to long, fully covered stents. Surg. Obes. Relat. Dis. 2017;13(6):925–932. doi: 10.1016/j.soard.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 5.Genser L., Pattou F., Caiazzo R. Splenic abscess with portal venous gas caused by intrasplenic migration of an endoscopic double pigtail drain as a treatment of post–sleeve gastrectomy fistula. Surg. Obes. Relat. Dis. 2016;12(1):e1–3. doi: 10.1016/j.soard.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]