Abstract
Computer-assisted telephone interviews were conducted after childbirth with 2,709 female residents of Iowa to examine experience of intimate partner violence (IPV) across pre-pregnancy, pregnancy, and postpartum. IPV was most prevalent during the postpartum period, followed by pre-pregnancy, and pregnancy. Violence in one period increased the likelihood of violence in subsequent periods. Latent Transition Analysis revealed three classes of women: those who experienced No IPV, Predominantly Sexual IPV, or Physical IPV Only. Change in IPV type across time was associated with whether women had intended, and whether their partners wanted, the pregnancy and with marital status. Findings suggest a continuity of violence for childbearing women who experience IPV prior to conception and have numerous implications for clinicians, researchers, and policymakers.
Keywords: Intimate partner violence, pregnancy, postpartum, latent transition analysis, maternal health, perinatal risk
Intimate partner violence (IPV) is a particularly serious problem when experienced by pregnant women. IPV is associated with severe adverse maternal and neonatal health outcomes (Donovan, Spracklen, Schweizer, Ryckman, & Saftlas, 2016; Silverman, Gupta, Decker, Kapur, & Ray, 2007). Prior research on IPV within the context of pregnancy has focused primarily on determining the prevalence of IPV (e.g., Gazmararian et al., 1996; Gilbert, Johnson, Morrow, Gaffield, & Ahluwalia, 1997) and has largely ignored the question of whether and how the type of abuse changes across pre-pregnancy, pregnancy, and the postpartum period. Knowing the correlates and patterns of IPV prior to, during, and after pregnancy may help researchers and health care practitioners to understand situational factors that contribute to IPV and help identify women at risk for IPV, although the success of violence screening programs has been limited (O’Doherty et al., 2014) and there has been no consensus regarding the most effective screening tool for IPV (Chisholm, Bullock, & Ferguson, 2017).
Examining patterns, correlates, and risk factors for IPV is challenging due to the heterogeneity of IPV experiences among women. A majority of studies have conceptualized IPV as a unitary construct and combined different IPV types to define general presence or absence of IPV (Sachs, Koziol-McLain, Glass, Webster, & Campbell, 2002). These studies have employed a variable-centered approach and corresponding data analytic techniques to identify risk factors for IPV in the general population. However, evidence suggests that different types of IPV might be associated with different outcomes and thus necessitate approaches and corresponding data analytic techniques that recognize the heterogeneity of IPV experiences (Sutherland, Sullivan, & Bybee, 2002). Such approaches may help to identify distinct subtypes or patterns of IPV and their effects on outcomes, and may aid the design and implementation of interventions that will be most effective for certain groups of women (Bogat, Levendosky, & von Eye, 2005). The present study is the first to employ latent transition analysis (LTA) to model change in the types and pattern of IPV occurrence across pre-pregnancy, pregnancy, and the postpartum period in conjunction with individual characteristics (e.g., marital status) and other contextual factors (e.g., whether self and partner intended the pregnancy).
Changes in IPV Across Pre-Pregnancy, Pregnancy, and Postpartum
The most commonly reported prevalence estimates for abuse during the year prior to pregnancy range from 3% to 30% (e.g., Cokkinides, Coker, Sanderson, Addy, & Bethea, 1999; Van Parys, Deschepper, Michielsen, Temmerman, & Verstraelen, 2014), whereas estimates for the postpartum period, defined as 3 to 12 months after birth, range from 3% to 24% (Groves et al., 2015; Hedin, 2000). History of violence, low socioeconomic status, unintended pregnancy, and being single are among the most commonly reported risk factors for IPV around the time of pregnancy (Fisher et al., 2005; Hedin & Janson, 2000; James, Brody, & Hamilton, 2013).
A majority of studies have been focused on physical and/or sexual abuse, as psychological abuse remains difficult to delineate and measure (Van Parys et al., 2014). With respect to comparisons of the pre-pregnancy and prenatal periods, existing data are mixed; some studies suggest that the frequency of abuse may increase during pregnancy relative to pre-pregnancy due to the unwanted nature of a pregnancy and/or to paternal uncertainty (e.g., Burch & Gallup, 2004), whereas others show a decrease in abuse during pregnancy (e.g., Martin, Mackie, Kupper, Buescher, & Moracco, 2001; Saltzman, Johnson, Gilbert, & Goodwin, 2003).
Studies on the prevalence of postpartum abuse by an intimate partner are also limited in number and vary substantially in their samples, methods employed, and definition of the postpartum period. For instance, in a cross-sectional study of a statewide sample from the North Carolina Pregnancy Risk Assessment Monitoring System (PRAMS), the prevalence of abuse before and during pregnancy was 6.9% and 6.1%, respectively, whereas the prevalence of postpartum abuse was 3.2% (Martin et al., 2001). On the other hand, in a national sample of Canadian women, the prevalence of abuse before pregnancy was 6%, during pregnancy was 1.4%, and during the postpartum was 1% (Daoud et al., 2012).
The months following childbirth are particularly stressful due to the challenges of taking care of a newborn (Graham, Lobel, & DeLuca, 2002), especially for those with limited resources, and therefore may be a particularly high-risk period for IPV (Charles & Perreira, 2007; Shoffner, 2008). There is some evidence that previous abuse (before and/or during pregnancy) predicts postpartum abuse. In a nationally representative cohort of pregnant women in 20 U.S. cities, prenatal abuse was the strongest predictor of abuse 1-year postpartum (Charles & Perreira, 2007). Similarly, in a study of Swedish women attending prenatal clinics, 90% of women who were abused during their pregnancy also reported having experienced abuse during the 3-month period following childbirth (Hedin, 2000), which suggests a continuity of IPV from pregnancy to the postpartum period.
Due to the lack of longitudinal, population-based studies of the frequency and type of abuse before, during, and after an index pregnancy, current knowledge is too limited to indicate whether the frequency and intensity of IPV increases, decreases, or remains constant from the period preceding pregnancy to the prenatal period, or whether the type of abuse changes across the pre-pregnancy, pregnancy, and postpartum periods.
Prenatal care is one of the rare windows of opportunity for identifying women abused during pregnancy. For many women with limited resources, prenatal care appointments are the only contact point with health care providers (Devries et al., 2010). Therefore, knowing the prevalence, correlates, and patterns of IPV prior to, during, and after pregnancy is the first step in helping to inform violence screening programs in health care clinics. Knowing correlates and risk factors for IPV around the time of pregnancy may not provide specific information about how to intervene in prenatal violence, but it may help researchers and health care practitioners to identify vulnerable groups and to understand when to target them for IPV prevention.
A Variable-Centered or a Person-Centered Approach to IPV?
The CDC defines the term intimate partner violence as physical, sexual, or psychological harm or threats by a current or former partner or spouse, and asserts that IPV should be considered as a continuum (Saltzman, Fanslow, McMahon, & Shelley, 2002). This definition implies that IPV may take various forms and may be experienced in different ways by each woman. Defining IPV on a continuum also necessitates examining the stability and change in occurrences of different types of IPV across time. Temporal stability of IPV has been shown across a wide range of samples (e.g., O’Leary et al., 1989; O’Leary & Slep, 2003); however, evidence for temporal stability of IPV across pre-pregnancy, pregnancy, and postpartum periods within a relationship has been inconclusive. As a result, our knowledge about whether IPV prior to pregnancy tends to cease during pregnancy or whether previously non-existent violence is initiated during pregnancy/postpartum is very limited.
Prior studies in which IPV was defined as a unitary construct have predominantly used a variable-centered approach, focused on predictors of IPV, and applied corresponding data analytic techniques, such as ANOVA and regression, which assume that inter-individual differences are negligible (Ansara & Hindin, 2010; Bogat et al., 2005). A unitary construct of IPV may increase the predictive power in detecting health effects of IPV due to the increased construct validity achieved by including different types of IPV experiences in a single operational definition of IPV. Furthermore, employing a variable-centered approach and data analytic techniques, such as ANOVA and regression, allows researchers to identify relations between IPV and associated risk factors in the general population. For instance, variable-centered studies have shown increased risks for IPV among single, unemployed, younger, and poorer women, and among women with an unintended pregnancy (e.g., Bourassa & Bérubé, 2007; Cokkinides & Coker, 1998; Finnbogadóttir, Dykes, & Wann-Hansson, 2016; Gazmararian et al., 1996). However, the heterogeneity of IPV experiences within a population is difficult to elucidate using this approach (Bogat et al., 2005). In contrast, a person-centered approach, which focuses on the uniqueness of IPV experiences, and use of corresponding data analytic techniques, such as latent class analysis and traditional cluster analysis, can illuminate individual differences in IPV experience within a population. The central aim of these analyses is to group individuals into classes based on distinctive patterns of shared characteristics. Thus, person-centered approaches may be particularly helpful for identifying distinct subtypes or patterns of IPV and their potential effects on health outcomes. The heterogeneity of IPV experiences underscores the necessity of targeted interventions. Person-centered approaches may help designers and implementers of intervention programs to identify which groups of women will be most amenable to which type of interventions (Bogat et al., 2005).
The Present Study
We employed a person-centered approach and corresponding data analytic techniques to model changes in the pattern of IPV type across the pre-pregnancy, pregnancy, and postpartum periods using latent transition analysis (LTA). We aimed to answer the following questions:
Are there distinct subgroups of women within the sample who experience particular patterns in the type of IPV, such as only physical IPV, only sexual IPV, or both? Can a model of IPV classes be identified among participants?
Is there any change in these particular patterns of IPV across the pre-pregnancy, pregnancy, and postpartum periods? For instance, if a woman experiences physical IPV prior to pregnancy, what is the probability that she will continue to experience physical IPV or no violence or experience sexual IPV during pregnancy and/or the postpartum periods?
How does the probability of latent status membership differ by some individual and contextual variables -- documented as risk factors for IPV by prior research -- including whether the pregnancy is unwanted by a partner, whether the pregnancy is unintended by a woman, and her marital status?
Identifying distinct patterns in the type of IPV among women of reproductive age and understanding how these patterns change across pre-pregnancy, pregnancy, and postpartum periods may provide more person-focused guidelines to researchers and clinicians that would help their research and screening efforts that target IPV.
Method
Participants
The sample consisted of 2,709 female residents of three Iowa counties (Polk, Scott, and Black Hawk) who gave birth to a singleton live baby. Participants were identified from birth certificate files. Because Iowa law mandates reporting of domestic abuse of a minor woman by a parent, legal guardian, or caretaker to legal authorities, we were unable to ensure complete confidentiality to those women. Therefore, the sample was restricted to women of legal age. Women were eligible if they were at least 18 years old at the time of childbirth and spoke English. Of the 7,202 potential respondents identified from birth records, 4,250 (59%) women were reached by telephone. Of these, 12.9% (N = 548) were ineligible based on study inclusion criteria. Over 77% (N = 2,866) of the 3,702 eligible women agreed to participate, and of these, 94.5% (N = 2,709) completed the computer-assisted telephone interview.
The sample was predominantly White (88.4%) and married (86.9 %) with an average age of 28.32 years (SD = 5.45). A majority of women reported having more than a high school education (80.2%) and moderate-to-high income (67%) (see Table 1). Approximately 58% of the women reported that their pregnancies were intended, and 8.3% of these women were in infertility treatment before they became pregnant.
Table 1.
Participant Characteristics (N= 2,709)
| Variable | Mean ± SD or % (N) |
|---|---|
| Age at delivery | 28.32 ± 5.45 |
| Parity | 0.86 ± 1.01 |
| Gravidity | 2.39 ± 1.46 |
| Ethnicity | |
| White | 88.4 % (2394) |
| Black | 5.1 % (139) |
| Asian or Pacific Islander | 3.4 % (93) |
| Mixed race | 3.1 % (83) |
| Education | |
| ≤ High school | 19.8 % (536) |
| Some college, associate degree or vocational school | 32.5 % (880) |
| College graduate (BA) | 33.1 % (898) |
| Graduate or professional school | 14.6 % (395) |
| Marital status | |
| Married or cohabitating as if married | 86.9 % (2355) |
| Single | 10.3 % (279) |
| Missing | 2.8 % (75) |
| Annual income* | Median: $ 60,000 |
| Poor | 17.4 % (471) |
| Near poor to low income | 15.6 % (423) |
| Moderate income | 31.7 % (859) |
| High income | 35.3 % (956) |
| Employment status during pregnancy | |
| Employed | 79 % (2134) |
| Unemployed | 21 % (575) |
| Pregnancy intendedness of participants | |
| Intended | 57.7 % (1564) |
| Unintended | 42.3 % (1145) |
An income-poverty ratio (IPR) was calculated by dividing participants’ annual household income by the number of people living with them. Based on the guidelines determined by the U.S. Department of Health & Human Services (2016), the following cut-off scores were used to determine income groups: Poor if IPR <1.0; near poor to low income if IPR > 1.0 and < 2.0; moderate income if IPR > 2.0 and < 4.0; high income if IPR > 4.
Procedure
Names and addresses of potential participants were obtained from the birth certificate files. Letters of invitation were then sent to each potential participant. The study was described as a 1-hour telephone interview that would cover how couples overcome disagreements in their intimate relationships. Compensation of $30 was offered for participation to be paid upon completion of the interview. A toll-free number for the project was provided in the letter so that women who wanted to participate, but preferred not to be contacted at home, and/or women whose phone numbers had changed, could call to arrange an interview or ask questions about the study. The telephone interview method was specifically chosen for its potential to elicit higher and more accurate responses related to IPV than face-to-face interviews would due to increased anonymity and confidentiality. All interviews were conducted by trained, experienced female interviewers. After completion of the interviews, participants were offered information about local and statewide IPV resources that provide counseling and shelter. This information was given over the telephone (to address safety concerns) unless participants asked that it be mailed to them. Ethical approval was obtained from the University of Iowa, Institutional Review Board.
Measures
Physical abuse.
A modified version of the three-item Abuse Assessment Screen (AAS; McFarlane & Parker, 1994) was used to assess presence or absence of physical abuse during three periods: 6 months preceding the pregnancy, the pregnancy period, and the postpartum period (Mean interval from delivery to interview = 43 wks; IQR = 20.9–68.9; Median = 49 wks). Presence or absence of physical abuse was coded dichotomously (yes/no). The modified AAS was used in the present study for several reasons. First, it is a brief measure that is highly correlated with more elaborate instruments (McFarlane, Parker, Soeken, & Bullock, 1992). Second, it enables participants to report abuse perpetrated by people other than their partners, as it asks about physical and sexual abuse perpetrated by “someone.” Given that evidence suggests that half of assault victims are injured by their partners, and the other half are injured by people other than their partners, such as family members, neighbors, and acquaintances, the focus of the AAS on “someone” as perpetrator is important and critical to differentiate partner violence from other types of violence (Grisso et al., 1999). Third, the AAS does not require participants to report violent behavior only within the context of disagreements as do some other measures.
Sexual Abuse.
Participants were asked 1) whether “they had sex because they were scared not to” and 2) whether “they were physically forced or threats were used to make them have sex or engage in a sex act when they did not want to” either before, during, and/or after pregnancy. A “yes” response to either of these questions for a given period was coded as positive for the presence of sexual abuse.
Pregnancy intendedness.
Pregnancy intendedness was assessed by asking respondents (1) whether they had wanted to be pregnant at that time or sooner, or later, or did not want to be pregnant then or at any time in the future and (2) whether they had felt excited about having the baby once they found out that they were pregnant (PRAMS, 2004). Those who had wanted to be pregnant later or did not want pregnancy then or at any time in the future, and those who did not report having been excited about having the baby, were coded as women with an unintended pregnancy. Each respondent was also asked whether her partner did not want her to be pregnant at any time during the 12 months before childbirth (coded yes/no).
Marital status.
Participants were asked to report their marital status at the time of the interview. Women who reported not being married were coded as single, and those who reported being married or in a relationship (i.e., cohabitating as if married) were coded as married.
Data Analytic Plan
Analyses were performed using SAS 9.2. Experience of IPV was coded for pre-pregnancy, pregnancy, and the postpartum period. Categories of no reported violence, physical violence only, sexual violence only, and both physical and sexual violence were created for each time period. Change in IPV type across the three time periods was examined by latent transition analysis (LTA). LTA is an extension of latent class analysis that examines movement from one latent subgroup to another over time and allows researchers to estimate how membership in a given subgroup changes across time. LTA uses a person-centered multivariate approach, which enables detection of unobserved heterogeneity in a given population, identification of meaningful subgroups based on similarity of responses to measured variables, and examination of change in these subgroups across time (Lanza & Collins, 2008; Nylund, Asparouhov, & Muthén, 2007). LTA was specifically chosen for its ability to represent multidimensional variables, that is, variables that cannot be represented by a single quantitative dimension and to model change over time. The basic LTA model includes three sets of parameters: latent status membership probabilities at Time 1, transition probabilities between latent statuses over time, and item-response probabilities conditional on latent status membership and time. A grouping variable may be included in an LTA model to allow parameters to be tested for measurement invariance and to be estimated conditional on group membership (Chung, Park, & Lanza, 2005).
In the present study, first, a model of IPV classes was established. Second, its measurement invariance was tested across groups of various individual and contextual variables using multi-group LTA. When measurement invariance was not achieved for a given group comparison, based on examination of parameter estimates, a modified model was specified for the groups compared and tested for measurement invariance. When measurement invariance was established, group differences were examined in the prevalence and transition of IPV classes across pre-pregnancy, pregnancy, and the postpartum period using multi-group LTA.
Results
Approximately 5.4% of women in the sample reported having experienced IPV at any time prior to, during, and/or after their pregnancy. IPV was most prevalent during the postpartum period (1%), followed by pre-pregnancy (0.9%), and pregnancy (0.7%). Experience of IPV both prior to and during pregnancy (1.2%), and both during and after pregnancy (1.2%), were also reported by a portion of women. Physical IPV was more prevalent during the postpartum period than during the other time periods; sexual IPV was most common prior to pregnancy (see Table 2).
Table 2.
Occurrence and Type of IPV Before, During, and After Pregnancy
| Occurrence and Type of IPV | Prior to Pregnancy | During Pregnancy | During Postpartum |
|---|---|---|---|
| N (%) | N (%) | N (%) | |
| No physical or sexual IPV | 2,626 (97.2) | 2,635 (97.4) | 2,631 (97.3) |
| Physical IPV only | 51 (1.9) | 46 (1.7) | 56 (2.1) |
| Sexual IPV only | 17 (0.6) | 13 (0.5) | 11 (0.4) |
| Both physical and sexual IPV | 8 (0.3) | 12 (0.4) | 7 (0.3) |
Question 1: Can a model of IPV classes be identified among women?
Four categorical variables were used as indicators of IPV type and occurrence across pre-pregnancy, pregnancy, and the postpartum period: No IPV, physical IPV only, sexual IPV only, and both physical and sexual IPV. First, several LTA models with 2, 3, 4, and 5 latent classes were tested to identify the best fitting, most parsimonious model. Fit of these models was compared using several statistics and criteria: the denoted goodness-of-fit statistic (G2; Goodman, 1970), Akaike’s information criterion (AIC; Akaike, 1974), and the Bayesian information criterion (BIC; Schwarz, 1978). The G2 statistic indicates correspondence between the observed and predicted response patterns; values lower than the degrees of freedom indicate good model fit. AIC and BIC are both penalized-likelihood criteria; that is, they assess model fit penalized for the number of parameters estimated. Therefore, lower values for these indices suggest good model fit. Table 3 shows fit indices for the 2-class, 3-class, 4-class, and 5-class models. Based on examination of these fit indices, the 3-class model was chosen and used in subsequent analyses due to its parsimony and lower G2, AIC, and BIC values. Examination of item-response probabilities suggested that the 3-class model can be labeled as No IPV, Predominantly Sexual IPV, and Physical IPV Only. Accordingly, the No IPV class was defined by absence of any reported physical or sexual violence. The Predominantly Sexual IPV class was characterized by a greater probability of experience of sexual violence (58%) and a lower probability of experience of both physical and sexual IPV (38%). Finally, all individuals in the Physical IPV Only class reported experiences of physical violence only.
Table 3.
Comparisons of Latent Class Models for Full Sample
| Model | Description | G2 | Degrees of freedom | AIC | BIC |
|---|---|---|---|---|---|
| 2 | Two-class | 217.26 | 500 | 239.26 | 304.21 |
| 3* | Three-class | 114.86 | 488 | 160.86 | 296.66 |
| 4 | Four-class | 112.76 | 472 | 190.76 | 421.03 |
| 5 | Five-class | 112.74 | 452 | 230.74 | 579.09 |
The latent class model accepted is shown in boldface.
Question 2: Is there any change in occurrence of types of IPV across the pre-pregnancy, pregnancy, and postpartum time periods?
The most common latent status at each of the three time periods was the No IPV class (97%), followed by Physical IPV Only (approximately 2%) and the Predominantly Sexual IPV (approximately 1%) classes. Figure 1 shows the stability of latent statuses, and Figure 2 illustrates change in the latent statuses across time. The probability of being in the same latent status in pregnancy as in pre-pregnancy was 98.6% for the No IPV class, 73% for the Predominantly Sexual IPV class, and 27.3% for the Physical IPV Only class. Whereas the probability of remaining in the same category in the postpartum period as during pregnancy was also high for the No IPV class (98.4%), the same probability was lower both for the Predominantly Sexual IPV (54%) and Physical IPV Only classes (39%).
Figure 1.
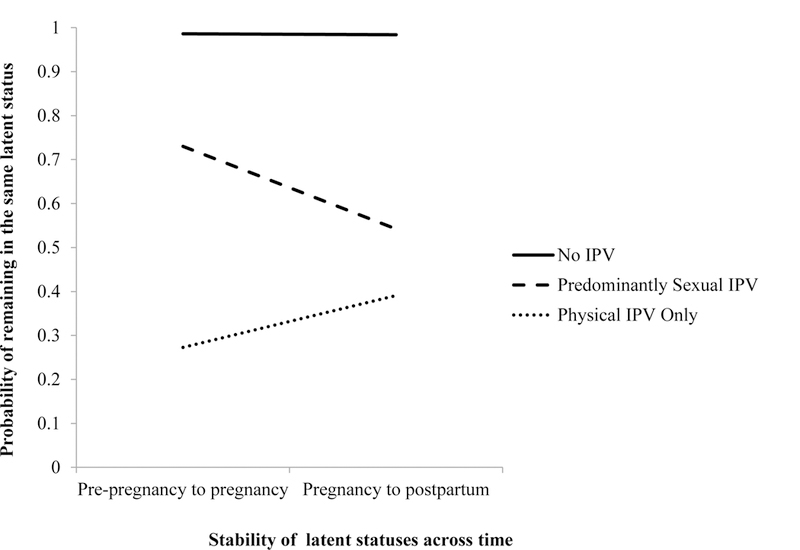
Stability of each latent status across time. Individuals in the No IPV class remained stable. Individuals in the Predominantly Sexual IPV class were most likely to change their status from pregnancy to the postpartum period, whereas those in the Physical IPV Only class were most likely to change their status from pre-pregnancy to pregnancy.
Figure 2.
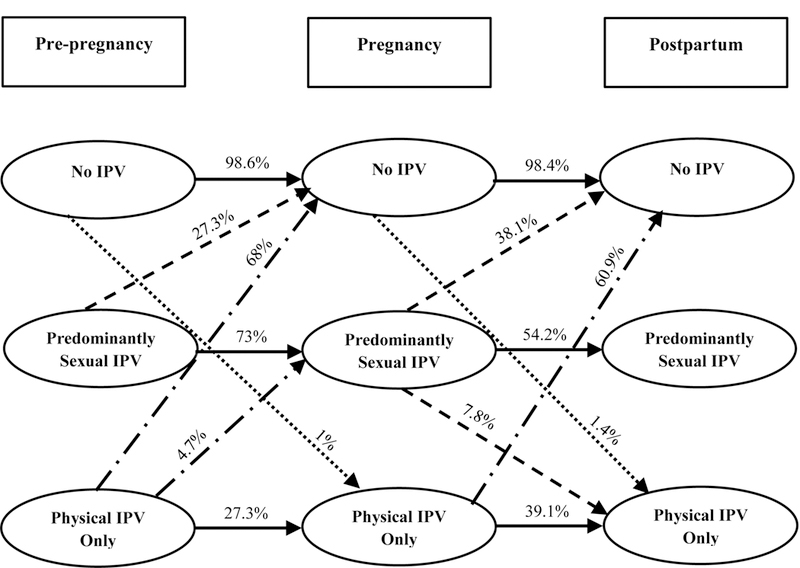
Probability of change in each latent status across pre-pregnancy, pregnancy, and postpartum. Solid lines (—) represent stability within each latent status, while the other lines represent the possibility of change for each latent status: Round dots (·······) represent the probability of change for No IPV status, dash lines (– – –) for Predominantly Sexual IPV status, and dot dash lines (— · — ) for Physical IPV Only status.
Members of the No IPV class during pre-pregnancy were more likely to have Physical IPV Only rather than Predominantly Sexual IPV status during pregnancy, but the probability of this transition was very low (1%). On the other hand, individuals in the Predominantly Sexual IPV class prior to pregnancy tended to move to the No IPV class during pregnancy. Finally, members of the Physical IPV Only class before pregnancy were more likely to be in the No IPV class (68%) during pregnancy. Approximately 5% of the members of the Physical IPV Only class were likely to move to the Predominantly Sexual IPV class when they became pregnant.
During the transition from pregnancy to the postpartum period, almost all members of the No IPV class (98.4%) maintained their status, whereas more than half of the Physical IPV Only class (60.9%) and 38.1% of the Predominantly Sexual IPV class tended to change to No IPV status. Approximately 8% of women in the Predominantly Sexual IPV class moved to the Physical IPV Only category at the postpartum period. Accordingly, members of the No IPV class tended to remain in the same status across the pre-pregnancy, pregnancy, and postpartum periods. Members of the Predominantly Sexual IPV class were more likely to move into the No Violence class during pregnancy, but some were at risk of Physical IPV (7.7%) during the postpartum period. On the other hand, the Physical IPV Only class tended to change to the No IPV class during the postpartum period, but had a relatively low risk (4.7%) of moving into the Predominantly Sexual IPV class during the transition from pre-pregnancy to pregnancy.
Question 3: How does the probability of latent status membership differ by some individual and contextual variables including whether the pregnancy was unwanted by a partner, intended by a woman, and her marital status?
The proportion of women whose partners did not want their pregnancy was higher in the Physical IPV Only class than in the Predominantly Sexual IPV class prior to (8% vs. 1%), during (8% vs. 3%), and after pregnancy (9% vs. 1%). Compared to women with partners who wanted their pregnancy, women whose partner did not want the pregnancy were more likely to move from No IPV status to Physical IPV Only status during pregnancy (4.4% vs. 1%) and from Predominantly Sexual IPV status to Physical IPV Only status during the postpartum period (86.2% vs. 42.2%). In addition, women in the Physical IPV Only class whose partner wanted the pregnancy were more likely to be in the No IPV status during the postpartum period than were those whose partner did not want the pregnancy (48.9% vs. 41.6%).
A 2-class latent model -- instead of the 3-class latent model -- was found to be invariant across women with an intended and unintended pregnancy and included the following classes: No IPV and Predominantly Physical IPV (G2 (12) =7 6.61, p <.001). Women with an unintended pregnancy were slightly less likely to belong to No IPV status at all time periods than were those with an intended pregnancy (95.4% vs. 98.6% for pre-pregnancy, 95.4% vs. 98.8% for pregnancy, and 95.6% vs. 98.5% for postpartum). Moreover, those with an unintended pregnancy were slightly more likely to be in the Predominantly Physical IPV class than were those with an intended pregnancy both from pre-pregnancy to pregnancy and from pregnancy to postpartum (4% vs. 1%). The proportions of individuals in each category across time remained stable.
Among women with an unintended pregnancy, the probability of staying in No IPV status from pre-pregnancy to pregnancy was slightly lower than for women with an intended pregnancy (97% vs. 99%). However, women who had an unintended pregnancy had a slightly higher probability of staying in the Predominantly Physical IPV class during pregnancy than did those who had an intended pregnancy (41% vs. 43%). Women with an unintended pregnancy in the No IPV class were slightly more likely to move to Predominantly Physical IPV status from pre-pregnancy to pregnancy than were those with an intended pregnancy (0.6% vs. 0.3%). Having an intended pregnancy was associated with a slightly higher probability of moving from Predominantly Physical IPV to No IPV status during pregnancy than was the case for women with an unintended pregnancy (59.1% vs. 56.8%), whereas unintended pregnancy was associated with a lower probability of transitioning to the No IPV class during the postpartum period than was intended pregnancy (44.4 % vs. 56.9 %).
Similarly, a 2-class latent model -- instead of the 3-class latent model -- was invariant across single and married women: No IPV and Predominantly Physical IPV. The proportion of married women in the No IPV class was greater than that of single women at all periods (approximately 99% vs. 88% for each period), whereas single women were more prevalent in the Predominantly Physical IPV class at each time period (approximately 12% vs. 1%). Single women in the No IPV class were slightly less likely to stay in the same status when they became pregnant than were married women (90.7% vs. 99.5%), and, if single women were in the Predominantly Physical IPV status prior to pregnancy, they were less likely to transition to the No IPV class than were married women (51.8% vs. 66.7%). Being single was associated with greater risk of moving from No IPV status to Predominantly Physical IPV status during the postpartum period than was the case for being married (5.4% vs. less than 1%). In addition, the probability of moving from Predominantly Physical IPV to No IPV status was also higher for single women than for married women (59.5% vs. 50%) during the postpartum period.
Discussion
In the present study we examined stability and change in occurrence of various types of IPV across pre-pregnancy, pregnancy, and the postpartum period, and identified three distinct groups of women: those who experienced No IPV, those who experienced Predominantly Sexual IPV, and those who experienced Physical IPV Only. The presence of violence in one time period increased the likelihood of violence in subsequent periods for all women. Physical violence prior to conception was more likely to continue during pregnancy among women with an unintended pregnancy than among those with an intended pregnancy. Women whose partners did not want the pregnancy were at a greater risk for initiation of physical violence during pregnancy than were women whose partners wanted the pregnancy. Compared to married women, single women also experienced distinct risks, such as being more likely to experience predominantly physical abuse at each time period.
Participants in our study reported more abusive experiences prior to and after pregnancy than during pregnancy. Physical abuse was most prevalent during the postpartum period, whereas sexual abuse was most prevalent prior to pregnancy. These findings initially suggested the possibility that pregnancy may be a protective factor against IPV for some women, which was further explored in the LTA analyses. LTA analysis identified three distinct groups of women defined by experiences of No IPV, Predominantly Sexual IPV, and Physical IPV Only. As expected, a majority of women in the study experienced no IPV across the pre-pregnancy, pregnancy, and the postpartum period. Women were more likely to experience Physical IPV than Predominantly Sexual IPV across the three time periods. The most vulnerable women were in the Predominantly Sexual IPV class, as the experiences of these women were defined by sexual abuse, which sometimes co-occurred with physical abuse. The Predominantly Sexual IPV class was more likely to remain the same during pregnancy than during the postpartum period, whereas the Physical IPV Only class was more likely to remain the same during the postpartum period as it was during pre-pregnancy. Women in the Predominantly Sexual IPV and the Physical IPV Only classes whose status changed were more likely to move to No IPV status across the pre-pregnancy, pregnancy, and postpartum periods. However, those in Physical IPV Only status prior to pregnancy were at risk for experiencing Predominantly Sexual IPV during pregnancy. Moreover, women in the Predominantly Sexual IPV class during pregnancy were at risk to be in the Physical IPV Only class during the postpartum period.
We found that violence experienced in one period tended to be present in the subsequent period, which suggests a continuity of violence from pre-conception through pregnancy and postpartum (Amaro, Fried, Cabral, & Zuckerman, 1990; Helton, McFarlane, & Anderson, 1987; Stewart & Cecutti, 1993). However, pregnancy may be protective for some women, particularly for those whose partners wanted the pregnancy, as evidenced by the change in their status from experiencing predominantly sexual IPV and physical IPV prior to pregnancy to no IPV during pregnancy. These findings corroborate prior research that showed a decrease in abuse during pregnancy (e.g., Daoud et al., 2012; Martin et al., 2001; Saltzman et al., 2003), although not all studies have shown this decrease (e.g., Amaro et al., 1990).
One notable finding of the present study is that a small subgroup of women who experienced violence at all three time periods tended to experience a change in the type of violence during the transition from pre-pregnancy to the postpartum period. Approximately 5% of women who experienced Physical IPV Only prior to pregnancy experienced Predominantly Sexual IPV during pregnancy. Moreover, 8% of women who experienced Predominantly Sexual IPV during pregnancy experienced Physical IPV Only during the postpartum period. The continuity of IPV and the change in the types of IPV experienced by some women after childbirth suggest that the postpartum period, which is particularly stressful (Graham et al., 2002), especially for those with limited resources, may be a particularly high-risk time period for IPV (Charles & Perreira, 2007; Shoffner, 2008). Our findings suggest that the types of IPV do change for some women across the pre-pregnancy, pregnancy, and postpartum periods. The observed changes in occurrences of the types of IPV might be due to changes in the psychological and emotional states and the behaviors of women and their partners in the presence of a baby. Future investigations are needed to identify predictors of these transitions between types of IPV across time.
Study Strengths and Limitations
The present study makes a unique contribution to the IPV literature because we examined stability and change in occurrence of different types of IPV across pre-pregnancy, pregnancy, and the postpartum period in the presence of individual and contextual risk factors. Our study has several strengths. First, we used a person-centered approach and corresponding methodology to examine the heterogeneity of IPV experiences around the time of pregnancy. Second, we recruited a large sample with a high participation rate, which increased statistical power to detect small effects. Third, instead of collecting data about a single time period, which was common in prior research, we asked respondents to report on IPV that occurred prior to, during, and after pregnancy.
Despite these study strengths, some caveats limit conclusions from this research. Only physical and sexual IPV were examined, and the findings are based on the small number of women who reported physical and/or sexual abuse. In addition, findings may be vulnerable to recall bias, as the IPV assessment for each time period was retrospective. However, recall bias may be an even greater limitation of previous studies that relied mostly on a single time point for retrospective assessment of 12 months prior to pregnancy (Jasinski, 2004; Silverman, Decker, Reed, & Raj, 2006a; Silverman, Decker, Reed, & Raj, 2006b). We attempted to minimize recall bias by conducting interviews following childbirth and asking participants to report on IPV occurrences during the 6 months prior to pregnancy, during pregnancy, and during the period following childbirth. However, the reported prevalence of IPV may have been unreliable because of potentially poorer recall for the earliest time periods, coping methods that involve repression of distressing past events, or the enhanced salience of more recent abuse. Type of abuse might also affect the extent to which it is remembered.
Generalizability of study findings is also limited because the data collection method restricted recruitment to women with telephones and those who gave birth to a singleton live baby (Keeter, 1995; Lavrakas, 1993). Furthermore, the sample was predominantly White and highly educated with moderate-to-high income. Finally, study findings are based on probabilities; therefore, no causal relationships can be inferred regarding the stability and change of IPV types across pre-pregnancy, pregnancy, and postpartum periods, and causality cannot be definitively established. Nonetheless, the results provide a strong foundation for further research to bolster confidence in the validity of conclusions about changes in IPV around the time of pregnancy.
Clinical and Policy Implications
Examination of group differences in the stability and change of IPV types across time provided some contextual information about the observed patterns. Among women who did not experience any violence prior to pregnancy, the probability of initiation of physical violence was higher during pregnancy for those whose partner did not want the pregnancy. Women who experienced predominantly sexual violence prior to pregnancy were also at greater risk for physical abuse during pregnancy if their partner did not want the pregnancy. Among women who were physically abused prior to pregnancy, those whose partner wanted the pregnancy were less likely to experience any violence during pregnancy than were those whose partner did not want the pregnancy. Similarly, women with an unintended pregnancy were more likely to experience violence during pregnancy. Compared to women with an intended pregnancy, those with an unintended pregnancy who experienced predominantly sexual abuse prior to pregnancy were more likely to endure the same experience during pregnancy. Unintended pregnancy may itself be the result of sexual abuse or of women’s reduced ability to control their reproductive health in the presence of a controlling partner, which underscores the importance of routine screening in prenatal care (Heise, 1996; Miller et al., 2010; Williams, Larsen, & McCloskey, 2008). Temporal associations between unintended pregnancy and violence warrant further investigation to address such possibilities.
As reported by other researchers (e.g., Cokkinides & Coker, 1998; Gazmararian et al., 1996), single women were more likely to experience predominantly physical abuse than were married women at each time period. Compared to married women, single women who did not experience violence during pregnancy were also at a greater risk of experiencing physical violence during the postpartum period.
IPV around the time of pregnancy is a complex problem that requires sophisticated theoretical approaches and corresponding data analytic techniques to understand its etiology and resolution. Pregnancy, which is a particularly vulnerable period for women, but one in which most women have contact with health care providers, may be a fitting and opportune context in which to investigate and identify distinct patterns of violence as well as their stability across time. We hope that these results can be used to improve the effectiveness of screening, prevention, and intervention programs for childbearing women. Given the extensive physical, emotional, social, economic, and other consequences of IPV, the stakes for women, their children, and our society at large are quite high.
Acknowledgments
The study was supported by NIH Grant RO1-HD39753. The authors are grateful to the many women who took part in this study.
Footnotes
Conflicts of Interest: The authrs have no conflicts to declare.
References
- Akaike H (1974). A new look at the statistical model identification. IEEE Transactions on Automatic Control 19, 716–723. [Google Scholar]
- Amaro H, Fried LE, Cabral H, & Zuckerman B (1990). Violence during pregnancy and substance use. American Journal of Public Health, 80, 575–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansara DL, & Hindin MJ (2010). Exploring gender differences in the patterns of intimate partner violence in Canada: A latent class approach. Journal of Epidemiology and Community Health, 64, 849–854. [DOI] [PubMed] [Google Scholar]
- Bogat GA, Levendosky AA, & von Eye A (2005). The future of research on intimate partner violence: Person-oriented and variable-oriented perspectives. American Journal of Community Psychology, 36(1–2), 49–70. [DOI] [PubMed] [Google Scholar]
- Bourassa D, & Bérubé J (2007). The prevalence of intimate partner violence among women and teenagers seeking abortion compared with those continuing pregnancy. Journal of Obstetrics and Gynaecology Canada, 29, 415–23. [DOI] [PubMed] [Google Scholar]
- Burch RL, & Gallup GG (2004). Pregnancy as a stimulus for domestic violence. Journal of Family Violence, 19, 243–247. [Google Scholar]
- Charles P, & Perreira KM (2007). Intimate partner violence during pregnancy and 1-year post-partum. Journal of Family Violence, 22, 609–619. [Google Scholar]
- Chisholm CA, Bullock L, & Ferguson JE (2017). Intimate partner violence and pregnancy: Screening and intervention. American Journal of Obstetrics & Gynecology, 217, 145 –149. [DOI] [PubMed] [Google Scholar]
- Chung H, Park Y, & Lanza ST (2005). Latent transition analysis with covariates: Pubertal timing and substance use behaviours in adolescent females. Statistics in Medicine, 24, 2895–2910. [DOI] [PubMed] [Google Scholar]
- Cokkinides VE, & Coker AL (1998). Experiencing physical violence during pregnancy: Prevalence and correlates. Family and Community Health, 20(4), 19–37. [Google Scholar]
- Cokkinides VE, Coker AL, Sanderson M, Addy C, & Bethea L (1999). Physical violence during pregnancy: Maternal complications and birth outcomes. Obstetrics and Gynecology, 93, 661–666. [DOI] [PubMed] [Google Scholar]
- Daoud N, Urquia ML, O’Campo P, Heaman M, Janssen PA, Smylie J, & Thiessen K (2012). Prevalence of abuse and violence before, during, and after pregnancy in a national sample of Canadian women. American Journal of Public Health, 102, 1893–1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devries KM, Kishor S, Johnson H, Stöckl H, Bacchus LJ, Garcia-Moreno C, & Watts C (2010). Intimate partner violence during pregnancy: Analysis of prevalence data from 19 countries. Reproductive Health Matters, 18, 158–170. [DOI] [PubMed] [Google Scholar]
- Donovan BM, Spracklen CN, Schweizer ML, Ryckman KK, Saftlas AF (2016). Intimate partner violence during pregnancy and the risk for adverse infant outcomes: A systematic review and meta-analysis. British Journal of Obstetrics & Gynaecology, 123, 1289–1299. [DOI] [PubMed] [Google Scholar]
- Finnbogadóttir H, Dykes A-K, & Wann-Hansson C (2016). Prevalence and incidence of domestic violence during pregnancy and associated risk factors: A longitudinal cohort study in the south of Sweden. BMC Pregnancy and Childbirth, 16, 228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher WA, Singh SS, Shuper PA, Carey M, Otchet F, MacLean-Brine D, Dal Bello D, & Gunter J (2005). Characteristics of women undergoing repeat induced abortion. Canadian Medical Association Journal, 172, 637–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazmararian JA, Lazorick S, Spitz AM, Ballard TJ, Saltzman LE, & Marks JS (1996). Prevalence of violence against women. Journal of American Medical Association, 275, 1915–1920. [PubMed] [Google Scholar]
- Gilbert BJC, Johnson CH, Morrow B, Gaffield ME, & Ahluwalia I (1997).Prevalence of selected maternal and infant characteristics, Pregnancy Risk Assessment Monitoring Surveillance System (PRAMS). Morbidity and Mortality Weekly Report, 48, 1–37. [PubMed] [Google Scholar]
- Goodman L (1970). The multivariate analysis of qualitative data: Interactions amongmultiple classifications. Journal of the American Statistical Association, 65, 226–256. [Google Scholar]
- Graham JE, Lobel M, & DeLuca RS (2002). Anger after childbirth: An overlooked reaction to childbirth and postpartum stressors. Psychology of Women’s Quarterly, 26, 222–233. [Google Scholar]
- Grisso JA, Schwarz DF, Hirschinger N, Sammel M, Brensinger C, Santanna J Teeple L (1999). Violent injuries among women in an urban area. New England Journal of Medicine, 341, 1899–1905. [DOI] [PubMed] [Google Scholar]
- Groves AK, Moodley D, McNaughton-Reyes L, Martin SL, Foshee V, & Maman S(2015). Prevalence and rates of intimate partner violence among South African women during pregnancy and the postpartum period. Maternal and Child Health Journal, 19, 487–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedin LW (2000). Postpartum, also a risk period for domestic violence. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 89(1), 41–45. [DOI] [PubMed] [Google Scholar]
- Hedin LW, & Janson PO (2000). Domestic violence during pregnancy: The prevalence of physical injuries, substance use, abortions, and miscarriages. Acta Obstetricia et Gynecologica Scandinavica,79, 625–630. [DOI] [PubMed] [Google Scholar]
- Heise LL (1996). Health workers: Potential allies in the battle against woman abuse in developing countries. Journal of the American Medical Women’s Association, 51(3), 120–122. [PubMed] [Google Scholar]
- Helton AS, McFarlane J, & Anderson ET (1987). Battered and pregnant: A prevalence study. American Journal of Public Health, 77, 1337–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James L, Brody D, & Hamilton Z (2013). Risk factors for domestic violence during pregnancy: A meta-analytic review. Violence and Victims, 28, 359–380. [DOI] [PubMed] [Google Scholar]
- Jasinski JL (2004). Pregnancy and domestic violence: A review of the literature. Trauma, Violence, & Abuse, 5, 47–64. [DOI] [PubMed] [Google Scholar]
- Keeter S (1995). Estimating non-coverage bias from a phone survey. Public Opinion Quarterly, 59, 196–217. [Google Scholar]
- Lanza ST, & Collins LM (2008). A new SAS procedure for latent transition analysis: Transitions in dating and sexual risk behavior. Developmental Psychology, 44, 446–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavrakas PJ (1993). Telephone survey methods: Sampling, selection, and supervision (2nd ed.). Newbury Park, CA: Sage. [Google Scholar]
- Martin SL, Mackie L, Kupper LL, Buescher PA, & Moracco KE (2001). Physical abuse of women before, during, and after pregnancy. Journal of American Medical Association, 285, 1581–1584. [DOI] [PubMed] [Google Scholar]
- McFarlane J, Parker B, Soeken K, & Bullock L (1992). Assessing for abuse during pregnancy: Severity and frequency of injuries and associated entry into prenatal care. Journal of American Medical Association, 267, 3176–3178. [DOI] [PubMed] [Google Scholar]
- McFarlane J, & Parker B (1994). Preventing abuse during pregnancy: An assessment and intervention protocol. American Journal of Maternal and Child Nursing, 19, 321–324. [PubMed] [Google Scholar]
- Miller E, Decker MR, McCauley HL, Tancredi DJ, Levenson RR, Waldman J,Schoenwald P, & Silverman JG (2010). Pregnancy coercion, intimate partner violence, and unintended pregnancy. Contraception, 81, 316–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén B (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling, 14, 535–569. [Google Scholar]
- O’Doherty LJ, Taft A, Hegarty K, Ramsay J, Davidson LL, & Feder G (2014). Screening women for intimate partner violence in healthcare settings: Abridged Cochrane systematic review and meta-analysis. British Medical Journal, 348, g2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Leary KD, Barling J, Arias I, Rosenbaum A, Malone J, & Tyree A (1989). Prevalence and stability of marital aggression between spouses: A longitudinal analysis. Journal of Consulting and Clinical Psychology, 57, 263–268. [DOI] [PubMed] [Google Scholar]
- O’Leary KD, & Slep AS (2003). A dyadic longitudinal model of adolescent dating aggression. Journal of Child and Adolescent Psychology, 32, 314–327. [DOI] [PubMed] [Google Scholar]
- PRAMS. (2004). Retrieved on 17 April 2016, from https://www.cdc.gov/prams/pdf/questionnaire/phase5_corequestions.pdf.
- Sachs C, Koziol-McLain J, Glass N, Webster D, & Campbell J (2002). A population-based survey assessing support for mandatory domestic violence reporting by health care personnel. Women & Health, 35(2/3), 121–133. [DOI] [PubMed] [Google Scholar]
- Saltzman LE, Fanslow JL, McMahon PM, & Shelley GA (2002). Intimate partner violence surveillance: Uniform definitions and recommended data elements, version 1.0 Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. [Google Scholar]
- Saltzman LE, Johnson CH, Gilbert BC, & Goodwin MM (2003). Physical abuse around the time of pregnancy: An examination of prevalence and risk factors in 16 states. Maternal and Child Health Journal, 7(1), 31–43. [DOI] [PubMed] [Google Scholar]
- Schwarz GE (1978). Estimating the dimension of a model. Annals of Statistics 6, 461–464. [Google Scholar]
- Shoeffner DH (2008). We don’t like to think about it: Intimate partner violence during pregnancy and postpartum. Journal of Perinatal & Neonatal Nursing, 22(1), 39–48. [DOI] [PubMed] [Google Scholar]
- Silverman JG, Decker MR, Reed E, & Raj A (2006a). Intimate partner violence victimization prior to and during pregnancy among women residing in 26 US states:Associations with maternal and neonatal health. American Journal of Obstetrics and Gynecology, 195, 140–148. [DOI] [PubMed] [Google Scholar]
- Silverman JG, Decker MR, Reed E, & Raj A (2006b). Intimate partner violence around the time of pregnancy: Association with breastfeeding behavior. Journal of Women’s Health, 15, 934–940. [DOI] [PubMed] [Google Scholar]
- Silverman JG, Gupta J, Decker MR, Kapur N, & Raj A (2007). Intimate partner violence and unwanted pregnancy, miscarriage, induced abortion, and stillbirth among a national sample of Bangladeshi women. British Journal of Obstetrics & Gynaecology, 114, 1246–1252. [DOI] [PubMed] [Google Scholar]
- Stewart DE, & Cecutti A (1993). Physical abuse in pregnancy. Canadian Medical Association Journal, 149, 1257–1263. [PMC free article] [PubMed] [Google Scholar]
- Sutherland CA, Sullivan CM, & Bybee DI (2001). Effects of intimate partner violence versus poverty on women’s health. Violence Against Women, 7, 1122–1143. [Google Scholar]
- U.S. Department of Health & Human Services. (2016). Office of the Assistant Secretary for Planning and Evaluation. U.S. Federal Poverty Guidelines Retrieved on 17 April 2016, from https://aspe.hhs.gov/poverty-guidelines.
- Van Parys A, Deschepper E, Michielsen K, Temmerman M, & Verstraelen H (2014). Prevalence and evolution of intimate partner violence before and during pregnancy: A cross-sectional study. BMC Pregnancy and Childbirth, 14, 294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams CM, Larsen U, & McCloskey LA (2008). Intimate partner violence and women’s contraceptive use. Violence Against Women, 14, 1382–1396. [DOI] [PubMed] [Google Scholar]


