Abstract
Common approaches to the psychological treatment of distressing voice hearing experiences, such as cognitive behavioural therapy, aim to promote more adaptive cognitive, emotional and behavioural responses to these experiences. Digital technologies such as smartphones show promise for supporting and enhancing these treatments by linking immediate therapeutic settings to the context of daily life. Two promising technologies include ecological momentary assessment and intervention (EMA/I), which may offer a means of advanced assessment and support in daily life, and inform the tailoring of interventions to suit individual needs. In this study, a highly novel intervention approach was developed involving four face-to-face sessions with a psychologist blended with EMA/I between sessions in order to improve coping with distressing voice hearing experiences. The authors describe the background and development of this approach along-side a single case illustration, which supported feasibility and acceptability. This study details how digital technologies such as EMA/I may be used in future as clinical tools to enhance standard psychological treatments and clinical care of people with persisting and distressing experiences.
Abbreviations: EMA, ecological momentary assessment; EMI, ecological momentary intervention; CBT, cognitive behavioural therapy; CSE, coping strategy enhancement; apps, application; SEPS, Subjective Experiences of Psychosis Scale; PSYRATS-AH, Auditory Hallucinations subscale of the Psychotic Symptom Rating Scales; DASS-21, Depression Anxiety Stress Scale; RCIs, reliable change indices
Keywords: Hearing voices, Auditory hallucinations, Digital technology, Smartphone, Blended therapy, Psychological treatment
Highlights
-
•
Self-monitoring of voice hearing experiences using smartphones has potential for improving awareness and understanding of voices
-
•
Summaries of individual momentary assessment data has potential to be used as a clinical tool for informing functional analysis of voices
-
•
Using smartphones to prompt the use of self-management strategies for voices can reinforce their use and improve coping in daily life
-
•
It is possible to blend smartphone technology with standard face-to-face therapy for hearing voices, however a larger trial is needed
1. Introduction
Hearing voices, or auditory verbal hallucinations, are common in psychiatric disorders such as schizophrenia, and more broadly in the general population (Sommer et al., 2012; Waters and Fernyhough, 2016). Although some people who hear persisting voices do not require specific support, many experience significant distress or interference with functioning (Johns et al., 2014; de Leede-Smith and Barkus, 2013). To minimise this impact, psychological therapies have been applied to promote more effective adaptation (Thomas et al., 2014).
A core component of cognitive behavioural therapies (CBT) for voices is improving effective self-regulation of this experience, used both as a specific therapy (Tarrier et al., 1993a; Tarrier et al., 1990) and within wider CBT protocols (Tarrier et al., 1998; Wykes et al., 2005; Wykes et al., 1999). Early research has suggested that people develop identifiable coping responses to voices, yet more effective coping strategies may be underutilised (Falloon and Talbot, 1981; Farhall et al., 2007; Tarrier, 1987). Tarrier et al. (1990) formalised a therapeutic approach called coping strategy enhancement (CSE), involving functional analysis of antecedents and responses to symptoms to inform implementation of effective coping more consistently. Initial trials of CSE showed broad support for reducing overall symptom severity, and to some degree voices (Tarrier et al., 1993a, Tarrier et al., 1993b). More recently, the approach has been confirmed as feasible as a four-session model specifically targeting voices (Hayward et al., 2018; Paulik et al., 2018).
In developing such approaches further, a key emerging area of therapy development for psychosis has been to utilise digital technologies, including mobile devices and smartphone applications (apps) (Ben-Zeev et al., 2012; Lal and Adair, 2014). Smartphones show particular promise given their transportability and immediate accessibility, and ownership is now widespread in psychosis populations (Firth et al., 2015; Gay et al., 2016; Thomas et al., 2017). Smartphone apps can provide access to therapeutic tools during daily life, whether used independently of, or in conjunction with, traditional mental health care services (Donker et al., 2013; Gravenhorst et al., 2015). Such user‑lead treatment may be empowering for people with psychosis and could overcome barriers such as memory and motivational deficits commonly encountered in psychological treatment (Johansen et al., 2011; Lysaker et al., 2013).
A recent pilot randomised controlled trial (RCT) conducted by Bucci et al. (2018) examined the effects of a CBT-based smartphone app for early psychosis, with findings indicating the app was highly acceptable, feasible and engaging to use, and showed promise for improving outcomes related to psychotic symptoms and mood. Schlosser et al. (2018) also found positive effects of a smartphone app aiming to improve motivation and quality of life in young people diagnosed with schizophrenia. Compared to a control condition, users of the app improved in their levels of motivation, as well as secondary measures of depression, defeatist beliefs, and self-efficacy, but not for psychotic symptom severity, quality of life, or functioning. Similar positive findings have been indicated for adults with persisting psychosis, with a number of studies supporting the feasibility of smartphone-based interventions in this population along-side high satisfaction rates (for review, see Firth and Torous, 2015).
Similar technologies have also been applied to symptoms of psychosis, including a trial currently underway by Garety et al. (2017) of a smartphone app targeting thinking processes associated with paranoia. Another app was developed by Jongeneel et al. (2018) which prompts users to engage with language tasks designed to disrupt the processes associated with voice hearing experiences. As these interventions are delivered in real-time, they have great potential to intervene as symptoms occur and offer immediate support for the individual (Myin-Germeys et al., 2016). Supporting further development of digital interventions, research has shown that attitudes towards the use of digital technologies for mental health amongst people with psychotic conditions are largely positive, although concerns such as privacy and data security exist (Bucci et al., 2018; Gay et al., 2016).
Two promising approaches that make use of smartphone technology are termed ecological momentary assessment (EMA, also referred to as experience sampling methodology; Shiffman et al., 2008) and ecological momentary intervention (EMI; Heron and Smyth, 2010). EMA is a data collection method involving repeated sampling of momentary experiences within a person's natural environment over several days, commonly using specialised smartphone apps (Shiffman et al., 2008). The method has unique monitoring and assessment capabilities given that information is collected in real time, overcoming recall bias, and the temporal interaction between variables can be examined (Moskowitz and Young, 2006; Shiffman et al., 2008; Stone et al., 2007). EMA has traditionally been used as a research tool, however more recently there has been interest in its use for clinical purposes, such as illness monitoring and improving the quality of assessment (Ebner-Priemer and Trull, 2009; Roberts et al., 2018; Torous et al., 2017; Trull and Ebner-Priemer, 2009; Van Os et al., 2013, van Os et al., 2017). EMI extends EMA to the therapeutic domain by providing momentary reminders or prompts via mobile devices to promote illness self-management during the person's daily life (Heron and Smyth, 2010; Myin-Germeys et al., 2016). These approaches are commonly used together, such as different EMI prompts being presented depending on responses to EMA questions indicating the presence or absence of symptoms (e.g. Ben-Zeev et al., 2014a).
A recent systematic review by Bell et al. (2017) found a range of emerging applications of EMA and EMI (EMA/I) approaches to the psychological treatment of psychotic disorders. These include remote monitoring of illness states to minimise relapse and hospitalisation (e.g. Španiel et al., 2012), and promotion of illness self-management through momentary reminders or instructions for a variety of clinical targets, including managing symptoms and psychosocial impairments (e.g. Ben-Zeev et al., 2014a, Ben-Zeev et al., 2014b; Granholm et al., 2011). Findings supported the feasibility and acceptability of these approaches, and showed promise for reducing symptoms and improving functioning. Since this review, further EMI studies have been conducted in the context of psychosis treatment, highlighting the growth in this area (e.g., Bucci et al., 2018; Schlosser et al., 2018; Garety et al., 2017; Jongeneel et al., 2018).
Utilising digital technologies such as EMA/I and other internet-based interventions in conjunction with standard treatments has been referred to as blended therapy (Erbe et al., 2017). Only a small number of studies have examined the effect of these types of interventions. Very few have been conducted in the context of psychosis treatment and these have been limited to the use of digital components within therapy sessions (e.g. Thomas et al., 2016; Craig et al., 2018). Findings from these studies have been positive, suggesting people with psychosis are open to the idea of using digital tools within therapy settings, and these can be used to enhance therapeutic components. A larger number of studies have been conducted outside of psychosis. A systematic review by Erbe et al. (2017) synthesised the findings of 44 studies of blended therapy in depression, anxiety and substance abuse. Across the studies, there was evidence that these interventions can result in similar outcomes to traditional therapies, using fewer resources, and may enhance the effects of standard therapy by supporting the delivery and uptake of intervention components. The use of blended therapies in psychosis warrants further research given the limited effectiveness of current interventions (Bighelli et al., 2018), which may be overcome using technologies aimed at supporting therapeutic components to maximise their effects. This might include promoting the use of specific intervention strategies discussed in session in daily life using EMI and enhancing the quality of assessment using EMA.
Smartphone-based EMA/I technology could offer a means of supporting brief coping interventions for distressing voice hearing experiences. Whilst a small number of studies have examined standalone smartphone apps for psychosis (Firth and Torous, 2015), none have focused on the integration of these technologies within standard therapies. In psychotic disorders, EMA has traditionally been used in research examining putative mechanisms underlying symptoms (Oorschot et al., 2009). Nonetheless, because data is collected repeatedly over time, processes which evolve momentarily can be captured and analysed to elucidate the temporal interplay between variables in real time on an individual basis (Oorschot et al., 2012; Os et al., 2017). Applying this therapeutically, EMA may be well suited to developing a behavioural functional analysis, i.e. formulating how symptoms can be modulated through identifying antecedents (occurring prior to symptoms) and responses (occurring following symptoms) (Sturmey, 2011). This is complementary to the CSE approach developed by Tarrier et al. (1990) that has considered antecedents and responses to voices via interviewing as a first stage of the intervention. This highlights the potential of EMA to support idiographic approaches to mental health treatment, which involve the identification of person-specific variables and their dynamic relation in order to inform more individually tailored interventions (Fisher, 2015; Haynes et al., 2009; Os et al., 2017). This use of EMA as an idiographic formulation tool for psychosis has never been examined, despite recognition for this potential (Ebner-Priemer and Trull, 2009; Roberts et al., 2018; Torous et al., 2017; Thomas et al., in press; Trull and Ebner-Priemer, 2009; Van Os et al., 2013, van Os et al., 2017). Additionally, the process of regular self-monitoring in daily life via diary methods is a common component of traditional CBT which can lead to improved understanding of one's own experiences (Cohen et al., 2013; Os et al., 2017). Furthermore, EMI could be used to remind people of coping strategies during daily life, facilitating implementation, and potentially reinforcing their use. The personalisation of EMI-based prompts in daily life to support generalisation of specific intervention strategies determined during psychological sessions has not yet been the focus of research in psychosis.
In this paper, we describe the development of a brief coping-focused intervention for distressing voices that blends face-to-face sessions based on CSE with smartphone EMA/I administered during participants' daily life. We illustrate the application of the intervention and demonstrate that the approach can be delivered feasibly and acceptably using a single case illustration.
2. Intervention development
Informed by the coping strategy enhancement (CSE) framework of Tarrier et al. (1990), we developed a model of smartphone-supported intervention that used EMA to inform functional analysis of voice fluctuations and EMI to support implementation of coping responses in daily life.
2.1. Selection of smartphone application
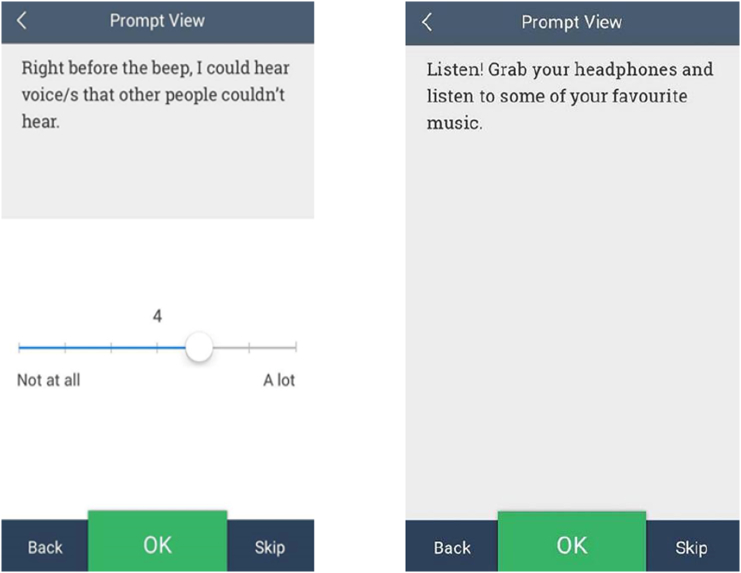
In reviewing the various EMA/I packages available, we selected an app called RealLife™ Exp (LifeData, 2015), which included a cost for programming license but was available for users to download for free on Android and iPhone. This app connects with a web-based platform that allows researchers to program simple and secure EMA/I surveys and schedules that can be individualised for each participant, and download data remotely. Images of the app are displayed below in Fig. 1.
Fig. 1.
Images of the smartphone app (example EMA item on left, example EMI reminder on right).
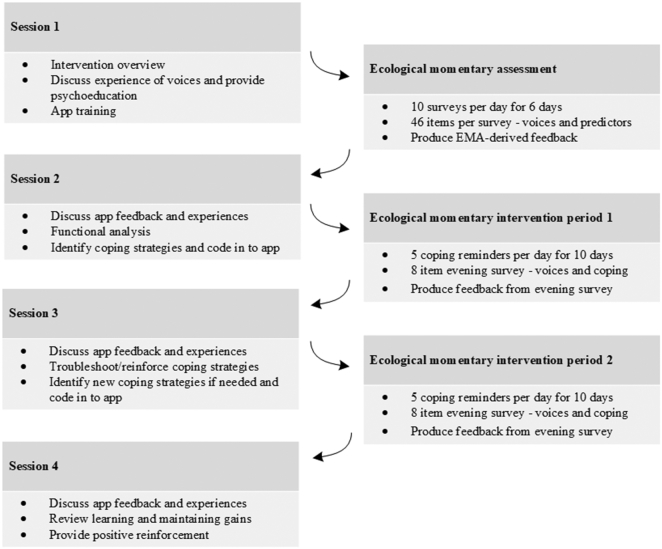
2.2. Intervention procedure
Aligning with the original CSE model (Tarrier et al., 1990), the four-session intervention can be conceptually divided in to two separate stages with an overall aim of improving coping with distressing voices. A breakdown of the intervention components is shown in Fig. 2 and is described below.
Fig. 2.
Intervention procedure.
2.2.1. Stage 1: functional analysis and ecological momentary assessment
The first stage occurred over session one and two, and involved information gathering to inform functional analysis of voice antecedents and responses. Whilst in classic CSE this has been done via interview, we utilised additional EMA self-monitoring to gather data in real time using 10 identical surveys per day over a 6-day period between session one and two (see later section for details of the survey items and schedule). Following the first session involving orientation to the intervention procedure, psychoeducation, and smartphone app training, the participant completed the EMA monitoring period, with the data then downloaded and analysed by a member of the research team. A feedback summary sheet of the data analysis was then provided to the participant in the second session, following the EMA monitoring period.
Within-person analysis of EMA data was conducted using Stata Statistical Software (StataCorp, 2013). The analysis protocol involved the calculation of; (i) the number of surveys completed during the monitoring period (out of 60); (ii) average momentary voice intensity and distress scores over the monitoring period; (iii) mean momentary voice intensity across different situations/contexts. We additionally used a time-lagged regression approach to identify (iv) which, if any, of the measured ‘antecedents’ (e.g. anxiety, low mood, etc.) were associated with subsequent changes in voice intensity. In these analyses, the outcome variable was voice intensity at moment t (i.e. the current survey), whilst proposed antecedents at moment t-1 (i.e. the previous survey) were entered as predictor variables. A similar approach was taken to identify (v) which, if any, of the measured responses to voices (e.g. relaxation, substance use, etc.), were associated with subsequent changes in voice intensity. Here, reported use of responses since the last measurement occasion were entered as dichotomous predictors (response reported = 1; response not reported = 0) of current momentary voice intensity. Following consultation with experts in the field (Wichers, personal communication), associations with a standardised beta co-efficient of greater than 0.3 were considered large enough to justify provision of feedback. Finally, (vi) the frequency and mean self-reported helpfulness of each response to voices was calculated.
It was anticipated that it might not always be possible to produce feedback, due to either low rates of survey completion, low frequency of voice reports, or lack of variation in voice intensity. The participant was made aware of this prior to the EMA period. The aim of the EMA self-monitoring phase was not just to gather data, but to engage the participant in building awareness of factors influencing their voices, which has been proposed as an important therapeutic mechanism (Cohen et al., 2013; Os et al., 2017).
During the second session, EMA-derived feedback was discussed along-side patterns noticed by the participant during the EMA monitoring period, with the aim of building a functional analysis of voice activity. This feedback included a lay-summary of: i) the number of surveys completed; ii) average voice intensity and distress scores; iii) mean voice intensity across different contexts; iv) triggers and responses associated with increased or decreased voice intensity; and v) a list of the specific responses to voices reported, and their average reported helpfulness. The presentation of the feedback was simple to ensure ease of understanding (e.g. “Your voice hearing experiences tended to be more intense when you were feeling anxious”). The feedback was framed as a guide due to potential limitations in capturing sufficient voice hearing occasions to detect predictors and to avoid inferring causation from correlation data.
2.2.2. Stage 2: identification and implementation of coping strategies and ecological momentary intervention
The second stage of the intervention involved building on the functional analysis by collaboratively identifying coping strategies which may theoretically disrupt maintenance cycles associated with the voices. Towards the end of session two, the therapist (IHB) helped the participant to identify up to four coping strategies, which were then worded as short sentences created by the participant and coded in to the app. To encourage and reinforce the use of these strategies, following session two, the participant then received five EMI reminders of these personalised coping strategies per day for a 10-day period, at random intervals between waking hours. They were also able to view the coping reminders on-demand by pressing a button within the app.
In addition to receiving EMI reminders of personalised coping strategies following session two, the participant also completed an additional brief survey each evening via the smartphone app. This survey assessed their daily use of the app and coping strategies, and their average voice intensity, impact and distress over the course of that day. During session three, a summary of responses to these questions was provided, which was used as a basis for discussing the helpfulness of the coping strategies since the last session. This session also involved reinforcing progress to maintain motivation and enhance self-efficacy, and addressing potential challenges in using the coping strategies. The participant was then able to choose new coping strategy reminders for the app or keep the same ones from the previous session, before completing an identical EMI period following session three. The fourth, final, session involved discussing the coping strategies used since the last session (again facilitated by personalised feedback based on evening survey data), reviewing progress, and how to maintain gains following the intervention.
2.3. Ecological momentary assessment items and procedure
The EMA sampling schedule was chosen due to it being a standard duration adopted in EMA research, providing a feasible model for implementation (e.g. Delespaul, 1995; Delespaul and van Os, 2002; Myin-Germeys et al., 2001). The selection and wording of EMA items involved several iterative stages. An initial systematic review was conducted to identify previous studies using EMA to examine momentary predictors of positive psychotic symptoms. This review identified 23 research studies, from which key variables and their corresponding EMA items were extracted. From here, additional items were added where no previous EMA items existed for these constructs in the literature. These items reflected common antecedents and responses to voices, as reported in non-EMA literature (e.g. environmental noise; Margo et al., 1981). This included a list of the most common coping responses derived from non-EMA literature on this topic (e.g. Farhall et al., 2007). A full list of potential EMA items was then reviewed by the authors, who have clinical and research expertise in psychosis and/or EMA. These items were also presented to a panel of people with lived experience of hearing voices (n = 4), who provided feedback regarding item wording. Based on this, we developed a set of 46 EMA items measuring momentary constructs related to voice antecedents (e.g. Right before the beep, I felt anxious), voice intensity and impact (e.g. Right before the beep, I could hear voice/s that other people couldn't hear), and common responses to voices (e.g. “…talking to the voice/s”. A full list of EMA items is provided in Supplementary 1.
3. Case study illustration
The following case describes the procedure and experiences of a participant who completed the intervention during the initial piloting stage and is presented here to illustrate the potential integration of EMA/I software with a coping-focused intervention. This participant was recruited through a specialist voices clinic in Melbourne (Thomas et al., 2011) and provided informed consent for report of his experiences in this publication.
Although the following case illustration was intended to be primarily descriptive, the participant was also asked to complete measures before and after the intervention, including a 1–10 visual analogue scale: How confident are you in your ability to cope with your voices day to day? (1, not at all confident to 10, very confident), and the following outcome scales: the negative impact subscale of the Subjective Experiences of Psychosis Scale (SEPS; Haddock et al., 2011), a measure of the negative emotional and functional impact of psychotic experiences, which the participant rated for voices; the Auditory Hallucinations subscale of the Psychotic Symptom Rating Scales (PSYRATS-AH; Haddock et al., 1999), measuring overall severity of voices; and the 21 item Depression Anxiety Stress Scale (DASS-21; Lovibond and Lovibond, 1995), measuring negative emotional symptoms. Significance of individual changes was calculated using the formula of Jacobson and Truax (1991) and published data on internal consistency to derive a threshold for reliable change. Reliable change indices (RCIs) were calculated from internal consistency and standard deviation data for people taking part in a trial of a coping focused intervention for voices (PSYRATS-AH, Sdiff = 4.37 and DASS-21, Sdiff = 9.97; Hayward et al., 2018) and people with clinically significant auditory hallucinations in a local trial of a psychosocial intervention (SEPS - negative impact, Sdiff = 6.93; Thomas et al., 2016).
3.1. Case illustration: Harry
Harry was a 38-year-old single male diagnosed with schizophrenia who lived independently and worked part-time. Harry had completed up to secondary level education and had above average estimated intelligence as measured by the Wechsler Test of Adult Reading (WTAR; Wechsler, 2001). He was on both antipsychotic and mood stabilising medication. He heard multiple voices intermittently several times a day, which varied in nature, including both commenting and commanding voices, and were primarily negative and critical in content. Although these experiences no longer caused Harry significant distress, they still required active self-management which tended to be both time consuming and overwhelming. Harry reported an interest in using an app for self-monitoring his voices and reminders for activities which might help him learn new ways of managing them.
3.1.1. Procedure and intervention
Harry completed the first session with no difficulties and learnt how to use the smartphone app quickly and easily. Similarly, he completed the EMA monitoring period with no issues, although the data from the app did not consistently upload automatically on a few occasions, requiring manual upload. Harry found this process slightly confusing.
Harry completed 68% of the daytime EMA surveys, reporting voices on 51% of occasions, and all six EMA evening surveys. Analysis of EMA responses highlighted that voice intensity was on average higher when in the company of several people and tended to increase following occasions where he was feeling anxious. In contrast, Harry's voices tended to be less intense following occasions where he was focused on his environment, engaging in meaningful activities, spending time with a person he was comfortable with, and feeling happy and relaxed. This was reflected in the analysis of his responses to the voices, which showed that engaging in relaxing activities and letting the voices come and go rather than interacting with them was associated with lower levels of voice intensity.
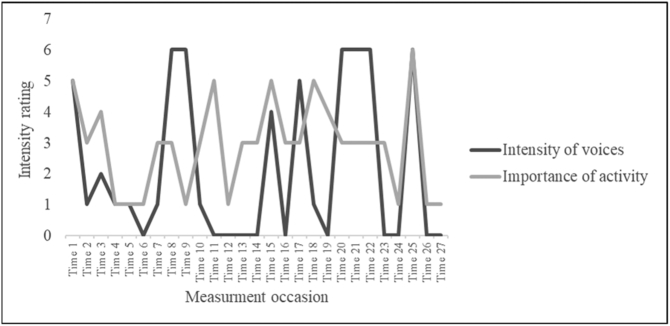
Harry was interested in this feedback and time was spent discussing potential interpretations. For example, an unexpected point of feedback indicated that Harry's voices tended to be more intense following times when he was doing something important to him. A depiction of this relationship is displayed in Fig. 3, showing comparative fluctuations in voice intensity at each timepoint across the six days, and the level of perceived importance of an activity at the prior timepoint. Although variability is clear from the figure, the data suggests that there is a positive relationship between these variables on many occasions. Harry interpreted this to be a consequence of work-related stress, which he recalled experiencing when endorsing high ratings on these items. This lead to a discussion surrounding the pressure and expectations Harry placed on himself at work, and the consequences of this generally making the voices more intense.
Fig. 3.
Intensity of voices at t = 0 and level of importance of an activity at t − 1, across the week (note that only time points in which both current and prior data was available is displayed).
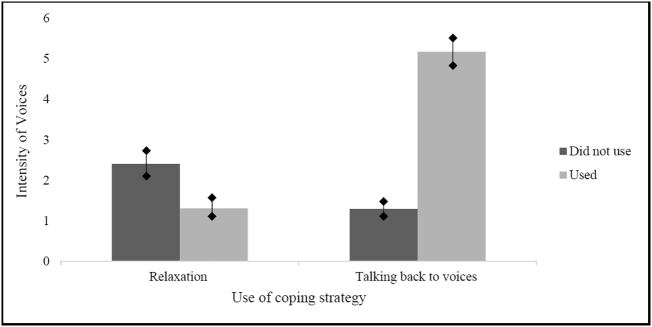
Notably, despite Harry's self-report that his most consistent coping response was talking with the voices, the EMA feedback found that relaxation and distraction activities (e.g. listening to music) and accepting the voices without responding were reported as being more helpful in the moment. Further, the analysis found that these coping responses predicted decreased levels of voice intensity, whereas engaging with the voices was associated with increased voice intensity. A depiction of this relationship is displayed in Fig. 4, showing the differences in mean voice intensity across all time points between times when the coping strategy of relaxation and talking back to the voices were, and were not, used between the current and prior time point.
Fig. 4.
Mean voice intensity between times when relaxation and talking back to the voices were, and were not, used as coping responses to the voices.
From this discussion, Harry chose three coping reminders to code in to the app, including “relax, remember to breath”, “pat the dog” and “put your headphones on”. These reminders were selected as Harry was motivated to focus on relaxation and being more ‘present’ in his environment as an alternative approach to coping with the voices.
Harry completed the EMI reminder period and reported no difficulties using the app. The feedback from the app highlighted that some coping strategies were rated as more helpful than others and this formed the basis of a discussion in session three. Harry stated that the reminders were particularly useful in the evenings when he found himself getting “caught-up” in talking with the voices, however were less helpful when the strategy was inapplicable given the context (e.g. could not listen to music when at work). Following session three, Harry chose to add two additional reminders “fire up the PlayStation” and “work on that project on the bench”. In the final session, Harry reflected on his progress and noted changes to his ability to cope with the voices since commencing the intervention.
3.1.2. Feedback at end of intervention
Over the course of the intervention, Harry reported improvements to his awareness of different and more effective coping responses for his voices. He described the coping reminders as the most important part of the intervention, finding them particularly helpful as a “circuit breaker” to prevent him getting “caught up” in his voices. He described the reminders and feedback as helpful to connect the content of therapy sessions with experiences in daily life, which he reported was often forgotten when sessions contained a lot of information. Harry reported that the consistency of the reminders helped to reinforce their use in his memory and force him to “check-in” and concentrate on the way he was responding. He also felt that the individualisation of the app was particularly important, which made it feel more personal. Harry reported that the schedule, timing and number of EMA/I items was acceptable and no negative experiences were reported, however he suggested that fewer EMA surveys per day over a longer time period may help reduce the burden of this monitoring period.
Clinical measures completed following the intervention showed Harry had increased the level of confidence in coping with the voices from 5/10 to 8/10. The final assessment coincided with some external stressors which he attributed to an increase in the severity of his voices, which was evident on the increased PSYRATS-AH overall voice severity score, though this was not clinically significant (pre: 17, post: 23). There was a reduction in the SEPS negative impact of the voices (pre: 95, post: 87), though this change was not clinically significant, and there was no change in DASS-21 negative emotional symptoms (pre: 66, post: 66).
4. Discussion
We set out to develop an intervention approach aimed at improving coping with distressing voices using brief face-to-face therapy blended with smartphone-based ecological momentary assessment and intervention (EMA/I). In the case presented, the participant showed good engagement and reported finding the intervention helpful. The intervention and procedures employed appeared feasible and acceptable, however some technological issues were encountered which highlight the importance of piloting new technology-based interventions (Berry et al., 2016). Overall, these findings show promise for the potential application of this approach for the psychological treatment of distressing voice hearing experiences.
Despite the relatively intense EMA monitoring schedule, the participant did not report any negative experiences and completed a sufficient number of surveys in order to produce the EMA-derived feedback (33%; Palmier-Claus et al., 2011). This is in line with prior research supporting the feasibility and acceptability of EMA in those with severe mental illness, including psychotic disorders (Granholm et al., 2008; Johnson et al., 2009). Both the EMA self-monitoring and EMA-derived feedback were seen as helpful for improving awareness, highlighting a willingness to engage with more intense monitoring for clinical purposes. The participant tended to notice new aspects of his voice hearing experiences which he was not previously aware of (e.g. questioning the helpfulness of certain responses, noting the relationship between voices and context). This is a commonly observed outcome of self-monitoring associated with increased self-regulation, perception of control, and behavioural change (Cohen et al., 2013; Humphreys et al., 2009). During this piloting, the participant provided feedback about the EMA items and schedule, suggesting some items could be removed, revised or added. For example, it was suggested to include a measure of paranoia as this tended to influence the intensity of his voices. In addition, the participant reported that the monitoring schedule was onerous at times, and suggested less frequent surveys over a longer period of time would be more ideal.
Together, these findings suggest that EMA self-monitoring and EMA-derived feedback can be used for assessing voice hearing experiences to inform the tailoring of clinical interventions and improve awareness, which warrants further exploration. This is important because this use of EMA has not yet been investigated in the context of a clinical intervention for psychotic conditions, despite growing interest (Ebner-Priemer and Trull, 2009; Roberts et al., 2018; Torous et al., 2017; Trull and Ebner-Priemer, 2009; Van Os et al., 2013, van Os et al., 2017). In particular, these findings support the potential use of EMA as a tool in the idiographic assessment and treatment approaches (Fisher, 2015; Haynes et al., 2009; Os et al., 2017). Only one other trial has investigated the use of EMA-derived feedback in therapy to the authors' knowledge, which was in an intervention involving monitoring and feedback of affect in people with depression, with positive outcomes (Kramer et al., 2014; Simons et al., 2015; Wichers et al., 2011). In the current study, embedded within the data was a rich tapestry of nuanced interactions between variables, which formed the basis of a productive discussion and gave rise to unique insights. Importantly, the EMA-derived feedback was reported to be consistent with the participants own experiences, suggesting the analysis identified meaningful and relevant patterns. In line with our aim, this feedback offered an in-depth point of reference for informing functional analysis of the participant's voices. However, given the limitations of using a select sample of data and the inherent inability to imply causation from correlation, it was important during this intervention to approach the discussion of feedback from an exploratory standpoint. This will be a relevant consideration for the future use of EMA in clinical contexts, as the popularity of this technology for assessing, monitoring and predicting illness states grows (Roberts et al., 2018).
Receiving personalised EMI reminders of coping strategies was reported by this participant to be the most useful aspect of the intervention. This is in line with prior trials examining the use of EMI for treating psychosis, which found positive feedback from participants regarding the usefulness of prompting self-management strategies for psychotic symptoms (Bell et al., 2017; Ben-Zeev et al., 2014a, Ben-Zeev et al., 2014b; Granholm et al., 2011). The participant in this study found the reminders were useful to overcome a tendency to get caught up in unhelpful ways of responding to the voices and as a reminder to use pre-determined coping strategies. Personalisation of the reminders was regarded as highly important as it created a more meaningful connection with the app, as was the ability to reflect and update these over the course of the intervention. Pre-post clinical measures demonstrated that although there was an increase in perceived ability to cope with the voices day-to-day, there was a non-significant increase in the overall severity of the participant's voices. However, this occurred along-side a decrease in the negative impact of the voices on multiple domains in his life. Although the participant attributed this worsening of his voices to external factors occurring during the intervention, the possibility that monitoring or other elements of the intervention may have contributed cannot be ruled out. The potential for symptomatic reactivity has been raised as a potential outcome of EMA monitoring (Kimhy et al., 2012; Shiffman et al., 2008), albeit empirical research has failed to find such a phenomenon (Johnson et al., 2009). Taken together, the observed clinical changes suggest that this intervention may have clinician benefits, particularly in reducing the negative impact of the voices on the person and increasing coping, however clearly further investigation is required.
Clearly, the current findings require investigation in a larger sample. In particular, it is important to recognise that the participant in this study was relatively high functioning, interested in digital technology, demonstrated above average intelligence, and had a good existing understanding of his own voice hearing experiences. Therefore, this use of EMA/I may not be as readily acceptable amongst the wider voice hearing population where these characteristics may not be as common (de Leede-Smith and Barkus, 2013).
In conclusion, the current case illustration demonstrated support for the clinical utility of the integration of smartphone EMA/I with traditional face-to-face therapy for improving coping with distressing voices. To more precisely evaluate the feasibility, acceptability and preliminary clinical effects of this approach, a pilot randomised controlled trial is currently being conducted (Bell et al., 2018).
The following is the supplementary data related to this article.
EMA Items and Schedule.
Declarations of interest
None.
Acknowledgments
Acknowledgements
The authors wish to thank the participants involved in this research, as well as colleagues and members of the lived experience panels who provided valuable feedback on the design of the intervention.
Financial support
This research was supported by the Australian Government Research Training Program Scholarship and the Barbara Dicker Brain Sciences Foundation Grant Scheme. The funding source had no other role in this project.
References
- Bell I.H., Lim M.H., Rossell S.L., Thomas N. Ecological momentary assessment and intervention in the treatment of psychotic disorders: a systematic review. Psychiatr. Serv. 2017;68(11):1172–1181. doi: 10.1176/appi.ps.201600523. [DOI] [PubMed] [Google Scholar]
- Bell I.H., Fielding-Smith S.F., Hayward M., Rossell S.L., Lim M.H., Farhall J., Thomas N. Smartphone-based ecological momentary assessment and intervention in a coping-focused intervention for hearing voices (SAVVy): study protocol for a pilot randomised controlled trial. Trials. 2018;19(1):262. doi: 10.1186/s13063-018-2607-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D., Drake R.E., Corrigan P.W., Rotondi A.J., Nilsen W., Depp C. Using contemporary technologies in the assessment and treatment of serious mental illness. Am. J. Psychiatr. Rehabil. 2012;15(4):357–376. [Google Scholar]
- Ben-Zeev D., Brenner C., Begale M., Duffecy J., Mohr D., Mueser K. Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophr. Bull. 2014;40(6):1244–1253. doi: 10.1093/schbul/sbu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D., Kaiser S.M., Krzos I. Remote “hovering” with individuals with psychotic disorders and substance sse: feasibility, engagement, and therapeutic alliance with a text-messaging mobile interventionist. J. Dual Diagn. 2014;10(4):197–203. doi: 10.1080/15504263.2014.962336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry N., Lobban F., Emsley R., Bucci S. Acceptability of interventions delivered online and through mobile phones for people who experience severe mental health problems: a systematic review. J. Med. Internet Res. 2016;18(5) doi: 10.2196/jmir.5250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bighelli I., Salanti G., Huhn M., Schneider-Thoma J., Krause M., Reitmeir C.…Furukawa T.A. Psychological interventions to reduce positive symptoms in schizophrenia: systematic review and network meta-analysis. World Psychiatry. 2018;17(3):316–329. doi: 10.1002/wps.20577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucci S., Barrowclough C., Ainsworth J., Machin M., Morris R., Berry K.…Haddock G. Actissist: proof-of-concept trial of a theory-driven digital intervention for psychosis. Schizophr. Bull. 2018;44(5):1070–1080. doi: 10.1093/schbul/sby032. sby032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J.S., Edmunds J.M., Brodman D.M., Benjamin C.L., Kendall P.C. Using self-monitoring: implementation of collaborative empiricism in cognitive-behavioral therapy. Cogn. Behav. Pract. 2013;20(4):419–428. [Google Scholar]
- Craig T.K., Rus-Calafell M., Ward T., Leff J.P., Huckvale M., Howarth E.…Garety P.A. AVATAR therapy for auditory verbal hallucinations in people with psychosis: a single-blind, randomised controlled trial. Lancet Psychiatry. 2018;5(1):31–40. doi: 10.1016/S2215-0366(17)30427-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Leede-Smith S., Barkus E. A comprehensive review of auditory verbal hallucinations: lifetime prevalence, correlates and mechanisms in healthy and clinical individuals. Front. Hum. Neurosci. 2013;7 doi: 10.3389/fnhum.2013.00367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delespaul P. IPSER Foundation; Maastricht, Netherlands: 1995. Assessing Schizophrenia in Daily Life—The Experience Sampling Method. [Google Scholar]
- Delespaul P., van Os J. Determinants of occurrence and recovery from hallucinations in daily life. Soc. Psychiatry Psychiatr. Epidemiol. 2002;37(3):97–104. doi: 10.1007/s001270200000. [DOI] [PubMed] [Google Scholar]
- Donker T., Petrie K., Proudfoot J., Clarke J., Birch M., Christensen H. Smartphones for smarter delivery of mental health programs: a systematic review. J. Med. Internet Res. 2013;15(11) doi: 10.2196/jmir.2791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebner-Priemer U.W., Trull T.J. Ambulatory assessment: an innovative and promising approach for clinical psychology. Eur. Psychol. 2009;14(2):109–119. [Google Scholar]
- Erbe D., Eichert H.C., Riper H., Ebert D.D. Blending face-to-face and internet-based interventions for the treatment of mental disorders in adults: systematic review. J. Med. Internet Res. 2017;19(9) doi: 10.2196/jmir.6588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falloon I.R., Talbot R.E. Persistent auditory hallucinations: coping mechanisms and implications for management. Psychol. Med. 1981;11(2):329–339. doi: 10.1017/s0033291700052144. [DOI] [PubMed] [Google Scholar]
- Farhall J., Greenwood K., Jackson H. Coping with hallucinated voices in schizophrenia: a review of self-initiated strategies and therapeutic interventions. Clin. Psychol. Rev. 2007;27(4):476–493. doi: 10.1016/j.cpr.2006.12.002. [DOI] [PubMed] [Google Scholar]
- Firth J., Torous J. Smartphone apps for schizophrenia: a systematic review. JMIR mHealth uHealth. 2015;3(4) doi: 10.2196/mhealth.4930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J., Cotter J., Torous J., Bucci S., Firth J.A., Yung A.R. Mobile phone ownership and endorsement of “mHealth” among people with psychosis: a meta-analysis of cross-sectional studies. Schizophr. Bull. 2015;42(2):448–455. doi: 10.1093/schbul/sbv132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher A.J. Toward a dynamic model of psychological assessment: implications for personalized care. J. Consult. Clin. Psychol. 2015;83(4):825. doi: 10.1037/ccp0000026. [DOI] [PubMed] [Google Scholar]
- Garety P.A., Ward T., Freeman D., Fowler D., Emsley R., Dunn G.…Greenwood K. SlowMo, a digital therapy targeting reasoning in paranoia, versus treatment as usual in the treatment of people who fear harm from others: study protocol for a randomised controlled trial. Trials. 2017;18(1):510. doi: 10.1186/s13063-017-2242-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gay K., Torous J., Joseph A., Pandya A., Duckworth K. Digital technology use among individuals with schizophrenia: results of an online survey. JMIR Mental Health. 2016;3(2) doi: 10.2196/mental.5379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granholm E., Loh C., Swendsen J. Feasibility and validity of computerized ecological momentary assessment in schizophrenia. Schizophr. Bull. 2008;34(3):507–514. doi: 10.1093/schbul/sbm113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granholm E., Ben-Zeev D., Link P., Bradshaw K., Holden J. Mobile Assessment and Treatment for Schizophrenia (MATS): a pilot trial of an interactive text-messaging intervention for medication adherence, socialization, and auditory hallucinations. Schizophr. Bull. 2011;38(3):414–425. doi: 10.1093/schbul/sbr155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravenhorst F., Muaremi A., Bardram J., Grünerbl A., Mayora O., Wurzer G.…Lukowicz P. Mobile phones as medical devices in mental disorder treatment: an overview. Pers. Ubiquit. Comput. 2015;19(2):335–353. [Google Scholar]
- Haddock G., McCarron J., Tarrier N., Faragher E. Scales to measure dimensions of hallucinations and delusions: the psychotic symptom rating scales (PSYRATS) Psychol. Med. 1999;29(04):879–889. doi: 10.1017/s0033291799008661. [DOI] [PubMed] [Google Scholar]
- Haddock G., Wood L., Watts R., Dunn G., Morrison A.P., Price J. The Subjective Experiences of Psychosis Scale (SEPS): psychometric evaluation of a scale to assess outcome in psychosis. Schizophr. Res. 2011;133(1):244–249. doi: 10.1016/j.schres.2011.09.023. [DOI] [PubMed] [Google Scholar]
- Haynes S.N., Mumma G.H., Pinson C. Idiographic assessment: conceptual and psychometric foundations of individualized behavioral assessment. Clin. Psychol. Rev. 2009;29(2):179–191. doi: 10.1016/j.cpr.2008.12.003. [DOI] [PubMed] [Google Scholar]
- Hayward M., Jones A., Berry C., Strauss C. Brief Coping Strategy Enhancement for distressing voices: an evaluation in routine clinical practice. Behav. Cogn. Psychother. 2018;46:226–237. doi: 10.1017/S1352465817000388. [DOI] [PubMed] [Google Scholar]
- Heron K., Smyth J. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. Br. J. Health Psychol. 2010;15(1):1–39. doi: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K.L., Marx B.P., Heidt J.M. Self-monitoring as a treatment vehicle. In: O'Donohue W.T., Fisher J.E., O'Donohue W., editors. Cognitive Behavior Therapy: Applying Empirically Supported Techniques in your Practice. John Wiley & Sons; Hoboken, NJ: 2009. pp. 478–485. [Google Scholar]
- Jacobson N.S., Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 1991;59(1):12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Johansen R., Hestad K., Iversen V.C., Agartz I., Sundet K., Andreassen O.A., Melle I. Cognitive and clinical factors are associated with service engagement in early-phase schizophrenia spectrum disorders. J. Nerv. Ment. Dis. 2011;199(3):176–182. doi: 10.1097/NMD.0b013e31820bc2f9. [DOI] [PubMed] [Google Scholar]
- Johns L.C., Kompus K., Connell M., Humpston C., Lincoln T.M., Longden E.…Cella M. Auditory verbal hallucinations in persons with and without a need for care. Schizophr. Bull. 2014;40(Suppl. 4):S255–S264. doi: 10.1093/schbul/sbu005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson E.I., Grondin O., Barrault M., Faytout M., Helbig S., Husky M.…Wittchen H.U. Computerized ambulatory monitoring in psychiatry: a multi-site collaborative study of acceptability, compliance, and reactivity. Int. J. Methods Psychiatr. Res. 2009;18(1):48–57. doi: 10.1002/mpr.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jongeneel A., Scheffers D., Tromp N., Nuij C., Delespaul P., Riper H.…van den Berg D. Reducing distress and improving social functioning in daily life in people with auditory verbal hallucinations: study protocol for the ‘Temstem’ randomised controlled trial. BMJ Open. 2018;8(3) doi: 10.1136/bmjopen-2017-020537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhy D., Myin-Germeys I., Palmier-Claus J., Swendsen J. Mobile assessment guide for research in schizophrenia and severe mental disorders. Schizophr. Bull. 2012;38(3):386–395. doi: 10.1093/schbul/sbr186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer I., Simons C.J., Hartmann J.A., Menne-Lothmann C., Viechtbauer W., Peeters F.…Delespaul P. A therapeutic application of the experience sampling method in the treatment of depression: a randomized controlled trial. World Psychiatry. 2014;13(1):68–77. doi: 10.1002/wps.20090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lal S., Adair C.E. E-mental health: a rapid review of the literature. Psychiatr. Serv. 2014;65(1):24–32. doi: 10.1176/appi.ps.201300009. [DOI] [PubMed] [Google Scholar]
- LifeData Corp RealLife Exp [Mobile application software] 2015. http://www.lifedatacorp.com/ Retrieved from.
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Lysaker P.H., Vohs J.L., Ballard R., Fogley R., Salvatore G., Popolo R., Dimaggio G. Metacognition, self-reflection and recovery in schizophrenia. Future Neurol. 2013;8(1):103–115. [Google Scholar]
- Margo A., Hemsley D.R., Slade P.D. The effects of varying auditory input on schizophrenic hallucinations. Br. J. Psychiatry. 1981;139(2):122–127. doi: 10.1192/bjp.139.2.122. [DOI] [PubMed] [Google Scholar]
- Moskowitz D.S., Young S.N. Ecological momentary assessment: what it is and why it is a method of the future in clinical psychopharmacology. J. Psychiatry Neurosci. 2006;31(1):13–20. [PMC free article] [PubMed] [Google Scholar]
- Myin-Germeys I., van Os J., Schwartz J., Stone A., Delespaul P. Emotional reactivity to daily life stress in psychosis. Arch. Gen. Psychiatry. 2001;58(12):1137–1144. doi: 10.1001/archpsyc.58.12.1137. [DOI] [PubMed] [Google Scholar]
- Myin-Germeys I., Klippel A., Steinhart H., Reininghaus U. Ecological momentary interventions in psychiatry. Curr. Opin. Psychiatry. 2016;29(4):258–263. doi: 10.1097/YCO.0000000000000255. [DOI] [PubMed] [Google Scholar]
- Oorschot M., Kwapil T., Delespaul P., Myin-Germeys I. Momentary assessment research in psychosis. Psychol. Assess. 2009;21(4):498–505. doi: 10.1037/a0017077. [DOI] [PubMed] [Google Scholar]
- Oorschot M., Lataster T., Thewissen V., Wichers M., Myin-Germeys I. Mobile assessment in schizophrenia: a data-driven momentary approach. Schizophr. Bull. 2012;38(3):405–413. doi: 10.1093/schbul/sbr166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Os J., Verhagen S., Marsman A., Peeters F., Bak M., Marcelis M.…Lataster T. The experience sampling method as an mHealth tool to support self-monitoring, self-insight, and personalized health care in clinical practice. Depress. Anxiety. 2017;34(6):481–493. doi: 10.1002/da.22647. [DOI] [PubMed] [Google Scholar]
- Palmier-Claus J., Myin-Germeys I., Barkus E., Bentley L., Udachina A., Delespaul P.…Dunn G. Experience sampling research in individuals with mental illness: reflections and guidance. Acta Psychiatr. Scand. 2011;123(1):12–20. doi: 10.1111/j.1600-0447.2010.01596.x. [DOI] [PubMed] [Google Scholar]
- Paulik G., Jones A.M., Hayward M. Brief coping strategy enhancement for distressing voices: predictors of engagement and outcome in routine clinical practice. Clin. Psychol. Psychother. 2018:1–7. doi: 10.1002/cpp.2299. [DOI] [PubMed] [Google Scholar]
- Roberts L.W., Chan S., Torous J. New tests, new tools: mobile and connected technologies in advancing psychiatric diagnosis. npj Digital Med. 2018;1(20176):1–4. doi: 10.1038/s41746-017-0006-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlosser D.A., Campellone T.R., Truong B., Etter K., Vergani S., Komaiko K., Vinogradov S. Efficacy of PRIME, a mobile app intervention designed to improve motivation in young people with schizophrenia. Schizophr. Bull. 2018;44(5):1010–1020. doi: 10.1093/schbul/sby078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S., Stone A., Hufford M. Ecological momentary assessment. Annu. Rev. Clin. Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Simons C., Hartmann J., Kramer I., Menne-Lothmann C., Höhn P., van Bemmel A.…Wichers M. Effects of momentary self-monitoring on empowerment in a randomized controlled trial in patients with depression. Eur. Psychiatry. 2015;30(8):900–906. doi: 10.1016/j.eurpsy.2015.09.004. [DOI] [PubMed] [Google Scholar]
- Sommer I.E., Koops S., Blom J.D. Comparison of auditory hallucinations across different disorders and syndromes. Neuropsychiatry. 2012;2(1):57–68. [Google Scholar]
- Španiel F., Hrdlicka J., Novak T., Kozeny J., Hoeschl C., Mohr P., Motlova L.B. Effectiveness of the information technology-aided program of relapse prevention in schizophrenia (ITAREPS): a randomized, controlled, double-blind study. J. Psychiatr. Pract. 2012;18(4):269–280. doi: 10.1097/01.pra.0000416017.45591.c1. [DOI] [PubMed] [Google Scholar]
- StataCorp . StataCorp LP; College Station, TX: 2013. Stata Statistical Software: Release 14. [Google Scholar]
- Stone A., Shiffman S., Atienza A., Nebeling L. Oxford University Press; 2007. The science of real-time data capture: Self-reports in health research. [Google Scholar]
- Sturmey P. Elsevier Academic Press; San Diego, CA, US: 2011. Functional Analysis in Clinical Treatment. [Google Scholar]
- Tarrier N. An investigation of residual psychotic symptoms in discharged schizophrenic patients. Br. J. Clin. Psychol. 1987;26(2):141–143. doi: 10.1111/j.2044-8260.1987.tb00740.x. [DOI] [PubMed] [Google Scholar]
- Tarrier N., Harwood S., Yusopoff L., Beckett R., Baker A. Coping strategy enhancement (CSE): a method of treating residual schizophrenic symptoms. Behav. Psychother. 1990;18(04):283–293. [Google Scholar]
- Tarrier N., Beckett R., Harwood S., Baker A., Yusupoff L., Ugarteburu I. A trial of two cognitive-behavioural methods of treating drug-resistant residual psychotic symptoms in schizophrenic patients: I. Outcome. Br. J. Psychiatry. 1993;162(4):524–532. doi: 10.1192/bjp.162.4.524. [DOI] [PubMed] [Google Scholar]
- Tarrier N., Sharpe L., Beckett R., Harwood S., Baker A., Yusopoff L. A trial of two cognitive behavioural methods of treating drug-resistant residual psychotic symptoms in schizophrenic patients. II. Treatment-specific changes in coping and problem-solving skills. Soc. Psychiatry Psychiatr. Epidemiol. 1993;28(1):5–10. doi: 10.1007/BF00797826. [DOI] [PubMed] [Google Scholar]
- Tarrier N., Yusupoff L., Kinney C., McCarthy E., Gledhill A., Haddock G., Morris J. Randomised controlled trial of intensive cognitive behaviour therapy for patients with chronic schizophrenia. Br. Med. J. 1998;317(7154):303–307. doi: 10.1136/bmj.317.7154.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas N., Rossell S., Farhall J., Shawyer F., Castle D. Cognitive behavioural therapy for auditory hallucinations: effectiveness and predictors of outcome in a specialist clinic. Behav. Cogn. Psychother. 2011;39(02):129–138. doi: 10.1017/S1352465810000548. [DOI] [PubMed] [Google Scholar]
- Thomas N., Hayward M., Peters E., van der Gaag M., Bentall R., Jenner J.…Varese F. Psychological therapies for auditory hallucinations (voices): current status and key directions for future research. Schizophr. Bull. 2014;40(Suppl. 4):S202–S212. doi: 10.1093/schbul/sbu037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas N., Farhall J., Foley F., Leitan N.D., Villagonzalo K.-A., Ladd E.…Smark T. Promoting personal recovery in people with persisting psychotic disorders: development and pilot study of a novel digital intervention. Front. Psych. 2016;7 doi: 10.3389/fpsyt.2016.00196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas N., Foley F., Lindblom K., Lee S. Are people with severe mental illness ready for online interventions? Access and use of the Internet in Australian mental health service users. Australas. Psychiatry. 2017 doi: 10.1177/1039856217689913. [DOI] [PubMed] [Google Scholar]
- Thomas N., Bless J., Alderson-Day B., Bell I.H., Cella M., Craig T.…Jardri R. Potential applications of digital resources in assessment, treatment and self-help for hallucinations. Schizophr. Bull. 2018 doi: 10.1093/schbul/sby103. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torous J., Onnela J., Keshavan M. New dimensions and new tools to realize the potential of RDoC: digital phenotyping via smartphones and connected devices. Transl. Psychiatry. 2017;7(3) doi: 10.1038/tp.2017.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull T., Ebner-Priemer U. Using experience sampling methods/ecological momentary assessment (ESM/EMA) in clinical assessment and clinical research: introduction to the special section. Psychol. Assess. 2009;21(4):457–462. doi: 10.1037/a0017653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Os J., Delespaul P., Wigman J., Myin-Germeys I., Wichers M. Psychiatry beyond labels: introducing contextual precision diagnosis across stages of psychopathology. Psychol. Med. 2013;43(7):1563–1567. doi: 10.1017/S0033291713000937. [DOI] [PubMed] [Google Scholar]
- van Os J., Verhagen S., Marsman A., Peeters F., Bak M., Marcelis M.…Lataster T. The experience sampling method as an mHealth tool to support self-monitoring, self-insight, and personalized health care in clinical practice. Depress. Anxiety. 2017;34(6):481–493. doi: 10.1002/da.22647. [DOI] [PubMed] [Google Scholar]
- Waters F., Fernyhough C. Hallucinations: a systematic review of points of similarity and difference across diagnostic classes. Schizophr. Bull. 2016;43(1):32–43. doi: 10.1093/schbul/sbw132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. The Psychological Corporation; San Antonio, TX: 2001. Wechsler Test of Adult Reading (WTAR) [Google Scholar]
- Wichers M., Hartmann J., Kramer I., Lothmann C., Peeters F., van Bemmel L.…Simons C. Translating assessments of the film of daily life into person-tailored feedback interventions in depression. Acta Psychiatr. Scand. 2011;123(5):402–403. doi: 10.1111/j.1600-0447.2011.01684.x. [DOI] [PubMed] [Google Scholar]
- Wykes T., Parr A.-M., Landau S. Group treatment of auditory hallucinations. Exploratory study of effectiveness. Br. J. Psychiatry. 1999;175(2):180–185. doi: 10.1192/bjp.175.2.180. [DOI] [PubMed] [Google Scholar]
- Wykes T., Hayward P., Thomas N., Green N., Surguladze S., Fannon D., Landau S. What are the effects of group cognitive behaviour therapy for voices? A randomised control trial. Schizophr. Res. 2005;77(2):201–210. doi: 10.1016/j.schres.2005.03.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
EMA Items and Schedule.