Abstract
Irrigation water is a major source of fresh produce contamination with undesired microorganisms including antibiotic-resistant bacteria (ARB), and contaminated fresh produce can transfer ARB to the consumer especially when consumed raw. Nevertheless, no legal guidelines exist so far regulating quality of irrigation water with respect to ARB. We therefore examined irrigation water from major vegetable growing areas for occurrence of antibiotic-resistant indicator bacteria Escherichia coli and Enterococcus spp., including extended-spectrum β-lactamase (ESBL)-producing E. coli and vancomycin-resistant Enterococcus spp. Occurrence of ARB strains was compared to total numbers of the respective species. We categorized water samples according to total numbers and found that categories with higher total E. coli or Enterococcus spp. numbers generally had an increased proportion of respective ARB-positive samples. We further detected high prevalence of ESBL-producing E. coli with eight positive samples of thirty-six (22%), while two presumptive vancomycin-resistant Enterococcus spp. were vancomycin-susceptible in confirmatory tests. In disk diffusion assays all ESBL-producing E. coli were multidrug-resistant (n = 21) and whole-genome sequencing of selected strains revealed a multitude of transmissible resistance genes (ARG), with blaCTX-M-1 (4 of 11) and blaCTX-M-15 (3 of 11) as the most frequent ESBL genes. Overall, the increased occurrence of indicator ARB with increased total indicator bacteria suggests that the latter might be a suitable estimate for presence of respective ARB strains. Finally, the high prevalence of ESBL-producing E. coli with transmissible ARG emphasizes the need to establish legal critical values and monitoring guidelines for ARB in irrigation water.
Introduction
Antibiotic resistance worldwide costs thousands of lives every month and has been listed by the World Health Organization (WHO) among today’s biggest threats for global health, food safety, and development, since it threatens our ability to treat common infectious diseases [1, 2]. The antibiotic resistome has been defined as the sum of all genes directly or indirectly contributing to antibiotic resistance both in the clinics and the environment, straightening out the fact that antibiotic resistance is far from being confined to hospitals [3]. On the contrary, antibiotic resistance is an ancient phenomenon which has been shown to evolve in the absence of human activity [4]. Nevertheless, it is acknowledged that antibiotic resistance in the environment is on the rise due to selective pressure exerted through anthropogenic factors [5].
Of all environmental compartments, the aquatic ecosystems have been entitled as the main reservoir of antibiotic-resistant bacteria (ARB) [6]. The presence of numerous ARB and their resistance determinants in various surface waters has been well documented and has been linked frequently to nearby wastewater treatment plants (WWTP) [6–12]. Wastewater treatment plants have been described to enrich rather than reduce ARB and their resistance determinants before discharge into nearby rivers or lakes [7, 13]. A likely explanation for this enrichment is that WWTP combine several factors favoring exchange of antibiotic resistance genes (ARG) among bacteria and selection of resistant strains, namely high bacterial and nutrient density in the presence of residual antibiotics [14]. In a recent study, Farkas and coworkers found that multidrug-resistant (MDR) bacteria, i.e. bacteria with resistance to at least three antibiotic classes, were more prevalent in surface waters than in wastewater [15], again suggesting enrichment of these contaminants through WWTP before release into nearby surface waters.
Human exposure to these contaminants can occur through various routes. Apart from being used for recreational purposes, surface waters such as rivers or lakes are often used for irrigation of fresh produce [16]. In agricultural regions in which water is scarce, the use of reclaimed wastewaters for irrigation of fresh produce has become common practice [17–19]. Irrigation water is one of the major sources of fresh produce contamination with bacteria [20]. Especially irrigation through overhead sprinklers, a common irrigation technique in fresh produce cultivation, will maximize the probability of contamination of edible plant parts, i.e. the leaves [21]. Through its frequent raw consumption, fresh produce represents an ideal direct vector of microorganisms to the consumer. In the past decade it has been recognized that consumption of fresh produce exposes the consumer not only to potential foodborne pathogens, but also to ARB [22–25].
The diversity of ARB present on fresh produce is considerable [26]. However, only if these resistances are transmissible will they be of clinical relevance, as opposed to intrinsic resistance which cannot be easily spread within the bacterial community [27]. The latter is of low concern unless it is harbored by a pathogen, and expert rules defining the levels of antimicrobial resistance (that is, multidrug-resistant, extensively drug-resistant, and pandrug-resistant) ignore known intrinsic resistances [28].
Among the ARB harboring transmissible antibiotic resistances of utmost clinical relevance are extended-spectrum β-lactamase (ESBL)-producing Enterobacteriaceae including Escherichia coli and vancomycin-resistant Enterococcus spp. (VRE), which have both been listed among the top twelve serious drug-resistant threats by the Centers for Disease Control and Prevention (CDC) [29] and have been listed recently in the WHO priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics [30]. ESBL-producing Enterobacteriaceae are increasingly detected outside the hospital setting in the environment. More specifically, ESBL-producing strains have been isolated from different surface waters lately [31–34]. An extensive review by Guenther and colleagues on ESBL-producing E. coli in wildlife pointed out that first isolation of such strains in wild animals dates back to the year 2006 only, whereas other antibiotic-resistant E. coli had been isolated long before that, for the first time in the early 1980s and thereafter repeatedly all over the world [35]. This observation suggests a relatively recent spread of ESBL-producing E. coli into the environment. Of note, ESBL-producing Enterobacteriaceae have also been isolated from fresh produce [25]. As to the spread of VRE into the environment outside hospital settings, sporadic detection of VRE and ARG associated with vancomycin-resistance in various surface waters has been described [36–40], but there is no such report so far for Switzerland. Finally, apart from ARB the presence of a plethora of ARG and antibiotic residues has been described for different surface waters and groundwater and has been attributed to the widespread and excessive usage of antibiotics worldwide [7, 13, 41, 42].
The growing request for fresh and healthy food products in conjunction with the demand for sustainable water usage will result in increased future exploitation of surface waters, reclaimed, or even untreated wastewater for irrigation of fresh produce [43]. Although guidelines including critical values for indicator bacteria exist for use of surface water in fresh produce production in many countries, up to now compulsory guidelines addressing ARB in irrigation water are absent. The use of a few indicator organisms and where possible the relative quantification of selected resistance genes would largely facilitate the task of monitoring irrigation water quality with respect to ARB. E. coli and Enterococcus spp. are both classical indicators of fecal contamination routinely used in assessing microbiological quality of water as well as foods [44–46]. Both species have also been used as indicators for monitoring antibiotic resistance in food products [47], and they are both key players in the spread of antibiotic resistance [48–51], including strains of utmost clinical relevance [29]. As to relevant resistance determinants, as mentioned earlier ARG are of concern when they can spread within bacterial communities through horizontal gene transfer (HGT), e.g. via transmissible plasmids [52]. When observing phenotypic resistance in bacterial isolates, it is therefore important to determine the underlying resistance determinant in order to elucidate whether the observed resistance is of clinical relevance. The present study aimed at quantifying indicator generic bacteria E. coli and Enterococcus spp. in irrigation water from different vegetable growing areas and characterizing antibiotic-resistant strains thereof including their underlying resistance determinants, with a focus on ESBL-producing E. coli and VRE.
Materials and methods
If not specified otherwise, material was purchased from Sigma-Aldrich (St. Louis, USA). No specific permission for sampling at the locations mentioned was required. Samples were taken within the Swiss Antibiotic Resistance Strategy (StAR) and the National Research Programme in collaboration with the Association of Vegetable Growers. We confirm that the field studies did not involve endangered or protected species.
Water sampling and bacterial culture preparation
Water applied for irrigation of fresh produce from three major Swiss vegetable growing areas was sampled in July 2016. Sampled locations included Ammerswil, Baden-Rütihof, Birmenstorf, Brittnau, Buttwil, Hüttikon, Kirchleerau, Laufenburg, Muhen, Riehen, Seengen, Suhr, Therwil, Unterentfelden, Villigen, Wohlen, Wohlenschwil, Kerzers, Ins and Brüttelen. Samples originated from either groundwater or various types of surface water (rivers, water canals, creeks, ponds, spring water, and open and closed rain water tanks). The average distance from each sample collection was 42 km and the sampling sites were not related, that is, not connected by rain force with the exception of samples No. 3 and 4. All samples (1 l each, n = 36) were collected in sterile water sampling bottles (VWR, Radnor, USA), transported at approximately 8°C, and processed within 10 h.
To determine aerobic mesophilic counts, ten-fold dilution series and 100 μl of undiluted water sample were plated on PCA in duplicate. For enumeration of generic E. coli and Enterococcus spp., 100 ml were concentrated on nitrocellulose filters (0.22 μm pore size, EMD Millipore, Billerica, USA) in duplicate and transferred to either CHROMagar or mEA. After enumeration of generic E. coli and Enterococcus spp., filters from CHROMagar or mEA were placed on tryptic soy agar (TSA, 4 h, 37°C) and then transferred for enrichment into 10 ml EE broth or BPW, respectively (24 h, 37°C). Target ARB were then cultured by streaking 10 μl of enrichment broth onto the respective antibiotic-containing selective media.
Bacterial culture conditions
The following media were used for bacterial cultivation: plate count agar (PCA) for determination of aerobic mesophilic count (AMC); CHROMagar E. coli (CHROMagar, Paris, France) and ready-to-use Brilliance ESBL plates (Oxoid Ltd., Hampshire, UK) for E. coli; m-Enterococcus agar (mEA) and ready-to-use Brilliance VRE plates (Oxoid Ltd.) for isolation of Enterococcus spp.
While AMC and generic E. coli and Enterococcus spp. were determined by direct incubation on PCA, CHROMagar, or mEA, respectively, antibiotic-resistant E. coli and Enterococcus spp. were cultured after enrichment. EE broth Mossel (Beckton Dickinson, Franklin Lakes, USA) was used for enrichment of E. coli, and buffered peptone water (BPW, 10.0 g of peptone, 5.0 g of NaCl, 3.5 g of anhydrous Na2HPO4, and 1.5 g of KH2PO4 per 1 l of water, pH 7.0) for enrichment of Enterococcus spp. After enrichment, ARB were cultured on the respective antibiotic-containing media: Additionally to commercial ESBL and VRE plates, CHROMagar and mEA plates supplemented with antibiotics were used. CHROMagar was supplemented with either ampicillin (AM, 100 mg/l), kanamycin (K, 16 mg/l), ciprofloxacin (CIP, 1 mg/l), or ceftazidime (CAZ, 8 mg/l), while mEA was supplemented with either erythromycin (ERY, 4 mg/l) or ciprofloxacin (1 mg/l). PCA plates were incubated at 30°C for 72 h; CHROMagar plates at 37°C for 24 h; mEA, VRE, and ESBL plates at 37°C for 48 h. Enrichment broths were incubated at 37°C for 24 h. All media were incubated under aerobic conditions.
MALDI biotyping
Representative colonies were identified by MALDI biotyping by direct smearing as described previously [53] with a microflex LT MALDI-TOF mass spectrometer (Bruker Daltonics, Bremen, Germany) and the associated MALDI biotyper RTC Software (Version 3.1). All colonies displaying the typical blue coloration from filters incubated on CHROMagar were confirmed to be E. coli. Colonies identified from filters incubated on mEA were almost exclusively Enterococcus spp. (115 of 117, 98%), as was expected from previous findings [54]. Therefore, all colonies enumerated on mEA were designated as Enterococcus spp.
Antibiotic susceptibility tests
E. coli and Enterococcus spp. isolated on either ESBL or VRE plates were screened for antibiotic resistances by disk diffusion assays. E. coli and Enterococcus spp. were tested against 32 or 11 clinically relevant antibiotics, respectively. After subculturing each strains on Columbia agar with 5% sheep blood (BioMérieux, Marcy l’Etoile, France) at 37°C and 7.5% CO2, disk diffusion assays were performed according to the European Committee of Antimicrobial Susceptibility Testing (EUCAST) guidelines from 2012 [55]. Briefly, bacterial suspensions of a turbidity equal to 0.5 McFarland was produced in 0.9% saline and were streaked on Mueller Hinton E (MHE) agar (Beckton Dickinson). Antibiotic disks were applied (i2a, Montpellier, France) and the plates were incubated at 35°C for 18 h ± 2 h or 24 h (E. coli or Enterococcus spp., respectively). Finally, inhibition zone measurement was performed using a Sirscan instrument (i2a) [56] followed by manual on-screen correction when needed. To determine antibiotic susceptibility, epidemiological cutoff (ECOFF) values were used according to EFSA recommendations for epidemiological screenings [57]. When ECOFF values were absent, clinical breakpoints were used (cefpodoxime and fosfomycin for E. coli), and when no value was defined in EUCAST guidelines, Clinical and Laboratory Standards Institute (CLSI) breakpoints were applied (colistin, minocycline, kanamycin, sulfonamide, tetracycline, temocillin, and cefalotin for E. coli; gentamicin high concentration, erythromycin, tetracycline, and chloramphenicol for Enterococcus spp.). Species with intrinsic resistances as defined by EUCAST expert rules were considered resistant (that is, erythromycin-resistance in Enterococcus faecalis) [58].
Presumptive ESBL-producing strains were confirmed by inoculating MHE agar as well as MHE agar containing cloxacillin (Axon Lab AG, Baden, Switzerland) and applying six antibiotic disks (cefoxitin with or without cloxacillin, cefotaxime with or without clavulanic acid, and ceftazidime with or without clavulanic acid) [59]. Plates were then incubated at 35°C for 18 h ± 2 h and inhibition zones were evaluated. Confirmation of presumptive VRE strains was performed using E-TEST Antimicrobial Resistance Detection strips (BioMérieux) on MHE agar inoculated with the test strain from a normalized bacterial suspension (0.5 McFarland). After incubation at 35°C for 24 h, the inhibitory concentration was read out.
Phylogenetic groups
E. coli phylogenetic groups (PG) were determined as described by Clermont and colleagues [60] by quadruplex PCR amplification. PCR was performed with custom-synthesized primers (Microsynth, Balgach, Switzerland) and a DreamTaq hot start PCR master mix (Thermo Fisher Scientific, Waltham, USA). Upon band visualization on a TBE gel (2% agarose, 35 min, 100 V), strains displaying ambiguous patterns were subjected to confirmatory C- or E-PCR.
DNA extraction, sequencing, and bioinformatics
Genomic DNA was extracted from eleven selected ESBL strains from different irrigation water samples covering the observed variety of phylogenetic group and antibiotic resistance with the commercial kit GenElute Bacterial Genomic DNA (Sigma-Aldrich). DNA was custom-sequenced using paired-end Illumina (HiSeq4000, 2 × 150 bp, 483 bp average insert size) at GATC Biotech (Konstanz, Germany). Data was processed using CLC Genomics Workbench Version 10.0 (Qiagen, Venlo, Netherlands) and resulting contigs were screened for genes of interest using online tools from the Center for Genomic Epidemiology (CGE): MLST 1.8, SerotypeFinder 1.1, VirulenceFinder 1.5, and ResFinder 3.0 [61–64].
To enrich plasmid DNA, extracts were produced using commercial PureYield Plasmid Maxiprep System (Promega, Fitchburg, USA). DNA was sequenced using a Pacific Biosciences RSII instrument at the Functional Genomics Center Zurich (8-kb insert library, P6/C4 chemistry). Four to five plasmid extracts were pooled per library. After size selection at 5 kb using a BluePippin (Sage Science, Beverly, USA) 360 min movies were recorded from each cell. Raw reads were assembled using Canu (version 1.5) [65]. Hybrid assemblies were produced (1) as polished Canu contigs (pilon, version 1.22) scaffolded with paired-end Illumina reads (SGA scaffolder, version v0.10.15) [66, 67] or (2) as assembled Illumina contigs scaffolded with Canu contigs and unassembled PacBio subreads (SPAdes, version 3.10.1) [68] to draw more robust conclusions from the two complementary approaches. Resulting scaffolds were screened for genes of interest as mentioned above. Additionally, the online tool Multiple Antibiotic Resistance Annotator (MARA) was used to identify mobile genetic elements in the genetic environment of the detected ARG [69].
Statistical analysis
Fisher’s exact test was applied to determine statistical significance of the observed increased frequency of ARB-positive irrigation water samples with increasing generic E. coli or Enterococcus spp. counts (P < 0.05).
Results
Aerobic mesophilic count and generic E. coli and Enterococcus spp
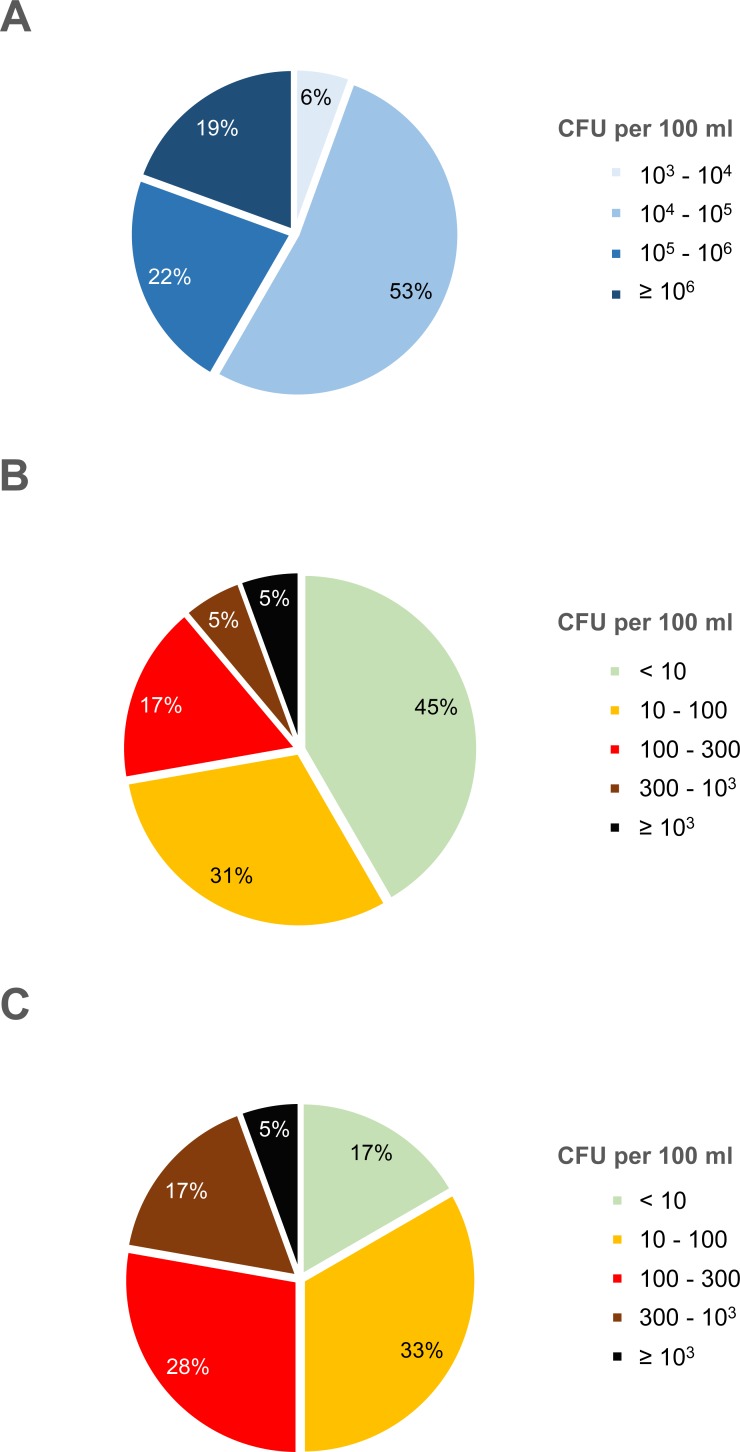
Aerobic mesophilic bacterial counts (AMC) ranged from 1.0 × 103 to 3.9 × 106 CFU per 100 ml, with about half of the samples (19 of 36) lying between 104 and 105 CFU per 100 ml (Fig 1A). No correlation was observed between AMC and either E. coli or Enterococcus spp. counts, i.e. increased AMC did not correlate with increased E. coli or Enterococcus spp. counts (S1 Fig). E. coli ranged from undetectable (< 1 CFU per 200 ml) to 1.0 × 103 CFU per 100 ml (Fig 1B). Almost half of the samples (16 of 36) had very low to undetectable E. coli counts (< 10 CFU per 100 ml). Two samples reached 1.0 × 103 CFU per 100 ml. Enterococcus spp. ranged from below the limit of detection (< 1 CFU per 200 ml) to 1.2 × 103 CFU per 100 ml (Fig 1C). Enterococcus spp. counts ranged from undetectable to at least 1.0 × 103 CFU per 100 ml as was observed for E. coli, however, more samples fell into the intermediate categories. About one in five water samples (22%) contained Enterococcus spp. above 300 CFU per 100 ml.
Fig 1. Aerobic mesophilic counts and generic E. coli and Enterococcus spp. counts in irrigation water.
Colony forming units (CFU) per 100 ml of water are indicated. (A) Aerobic mesophilic counts. (B) E. coli. (C) Enterococcus spp. For generic E. coli and Enterococcus spp., the first category (≤ 9 CFU per 100 ml) comprises samples from below the detection limit (1 CFU per 200 ml) up to 9 CFU per 100 ml. The percentage of water samples (total n = 36) falling into each category is displayed.
Antibiotic-resistant E. coli and Enterococcus spp
Antibiotic-resistant E. coli and Enterococcus spp. were isolated on either CHROMagar or mEA, respectively, containing selected antibiotics. In six samples, no ARB E. coli or Enterococcus spp. could be isolated on any of the tested antibiotics (samples 6, 7, 13, 19, 20, and 25; Table 1). In three of these samples no generic E. coli but generic Enterococcus spp. were detected (samples 19, 20, and 25; grey and white in Table 1, respectively), and in one sample neither generic E. coli nor generic Enterococcus spp. were detected (sample 13, grey in Table 1).
Table 1. Antibiotic-resistant E. coli and Enterococcus spp. isolated from irrigation water of different Swiss vegetable growing areas.
| no. | origin | AM | K | CIP | CAZ | ESBL | ERY | CIP | VRE | sequencing |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | canal A | |||||||||
| 2 | canal B | √ | H2, H6, H17 | |||||||
| 3 | canal C | √ | H10, H25 | |||||||
| 4 | river A | √ | H22 | |||||||
| 5 | pond | |||||||||
| 6 | rainwater tank (o) | |||||||||
| 7 | rainwater tank (c) | |||||||||
| 8 | rainwater tank (c) | |||||||||
| 9 | pond | |||||||||
| 10 | pond | |||||||||
| 11 | pond | |||||||||
| 12 | pond | |||||||||
| 13 | groundwater | |||||||||
| 14 | groundwater | |||||||||
| 15 | pond | |||||||||
| 16 | rainwater tank (o) | |||||||||
| 17 | rainwater tank (o) | |||||||||
| 18 | pond | × | ||||||||
| 19 | rainwater tank (c) | |||||||||
| 20 | rainwater tank (c) | |||||||||
| 21 | rainwater tank (c) | |||||||||
| 22 | spring water | √ | H30 | |||||||
| 23 | pond | × | ||||||||
| 24 | rainwater tank (o) | √ | H44 | |||||||
| 25 | groundwater | |||||||||
| 26 | pond | |||||||||
| 27 | rainwater tank (c) | |||||||||
| 28 | rainwater tank (c) | |||||||||
| 29 | pond | |||||||||
| 30 | pond | |||||||||
| 31 | rainwater tank (c) | √ | H38 | |||||||
| 32 | river B | √ | H40 | |||||||
| 33 | pond | |||||||||
| 34 | creek | |||||||||
| 35 | creek | |||||||||
| 36 | canal D | √ | H45 |
Grey: no generic E. coli or Enterococcus spp. detected on CHROMagar or mEA without antibiotics; white: only generic E. coli or Enterococcus spp. detected; blue: E. coli detected on CHROMagar containing the respective antibiotic or ESBL agar; pink: Enterococcus spp. detected on mEA containing the respective antibiotic or VRE agar. AM: ampicillin; K: kanamycin; CIP: ciprofloxacin; CAZ: ceftazidime; ESBL: commercial ESBL agar; ERY: erythromycin; VRE: commercial VRE agar; (c), closed; (o), open. √: ESBL-producing E. coli confirmed; ×: vancomycin-resistant E. faecalis not confirmed. Sequencing: sequenced ESBL-producing E. coli (whole-cell and plasmid extracts).
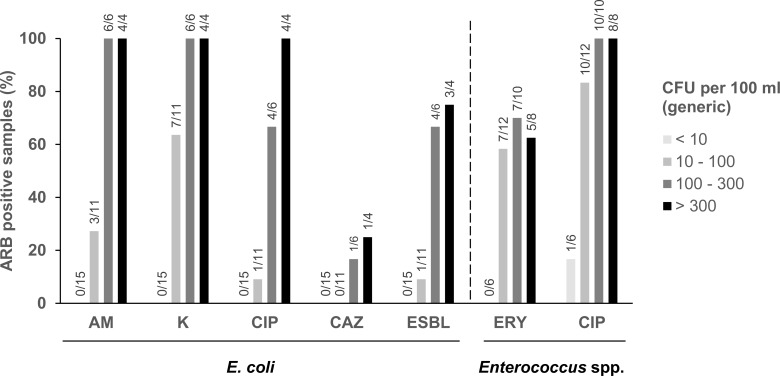
E. coli were most frequently isolated on kanamycin, followed by ampicillin, ciprofloxacin, and ceftazidime. Finally, presumptive ESBL-producing E. coli were cultured from eight of 36 water samples (22%), and all could be confirmed to be ESBL-producing E. coli in subsequent testing. The proportion of water samples containing E. coli growing on antibiotic-containing plates in dependence of generic E. coli content is shown in Fig 2. For all antibiotic plates, increased generic E. coli counts correlated with increased proportion of ARB E. coli positive samples. For instance, while no ESBL-producing E. coli were detected in samples with the lowest generic E. coli counts (< 10 CFU per 100 ml), proportion of ESBL-positive samples increased as generic E. coli counts increased (Fig 2). This increase was statistically significant with the only exception of CAZ-resistant E. coli (P < 0.0001 for AM-, K-, and CIP-resistant E. coli; P < 0.001 for ESBL-producing E. coli and CIP-resistant Enterococcus spp.; P < 0.05 for ERY-resistant Enterococcus spp.).
Fig 2. Generic E. coli or Enterococcus spp. counts and frequency of ARB-positive irrigation water samples.
With increasing generic E. coli or Enterococcus spp. counts, water samples containing different ARB of the respective species were more frequent. AM, ampicillin; K, kanamycin; CIP, ciprofloxacin; CAZ, ceftazidime; ERY, erythromycin. Numbers on top of bars indicate number of positive to total water samples.
Enterococcus spp. were isolated on ciprofloxacin from 29 of the 36 samples (Table 1) and from about half the samples (19 of 36) on erythromycin. Two samples contained presumptive VRE E. faecalis. In a confirmatory E-TEST, however, they proved vancomycin-susceptible with minimal inhibitory concentrations of 1 mg or 4 mg per l (resistance cutoff: > 4 mg/l). As for E. coli, the proportion of water samples positive for Enterococcus spp. isolated on broad-spectrum antibiotic ciprofloxacin increased with increasing generic Enterococcus spp. counts (Fig 2): While only one of six samples with less than 10 CFU per 100 ml generic Enterococcus spp. was positive for such strains, more than three quarter of the samples with 10 to 100 CFU per 100 ml and all water samples with more than 100 CFU per 100 ml were positive (Fig 2). The proportion of samples positive for erythromycin-resistant Enterococcus spp. similarly increased with higher generic Enterococcus spp. counts (only exception: > 300 CFU per 100 ml generic Enterococcus spp.; Fig 2).
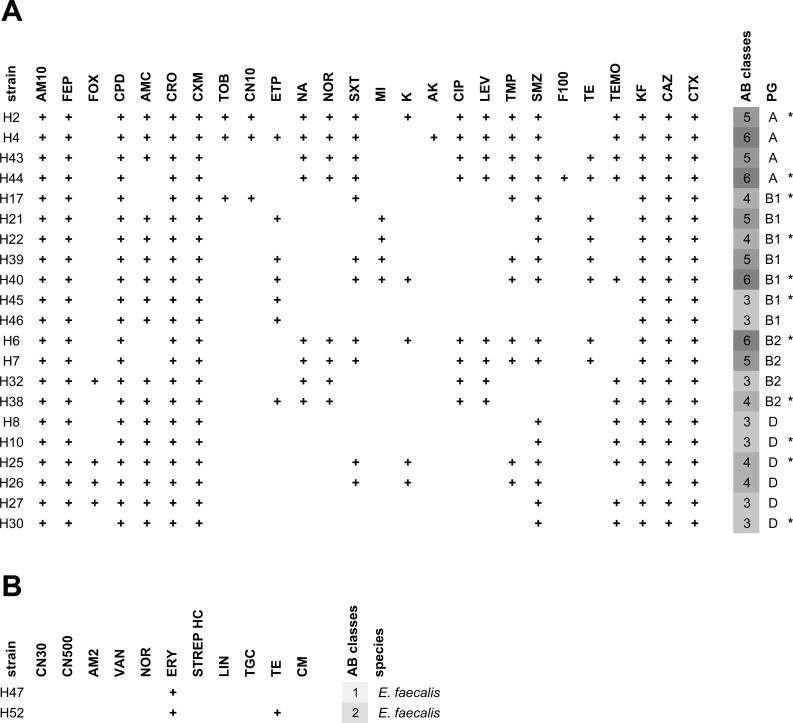
Antibiograms of ESBL-producing E. coli and presumptive VRE
For ESBL-producing E. coli and presumptive VRE, antibiotic resistance to clinically relevant antibiotics was determined in disk diffusion assays. All tested E. coli were resistant to ampicillin and the cephalosporins cefalothin (1st generation), cefuroxime (2nd generation), cefpodoxime, ceftriaxone, ceftazidime, and cefotaxime (3rd generation), and cefepime (4th generation) (Fig 3A). Further frequent resistances (more than half of the isolates) were detected to amoxicillin-clavulanic acid, sulfamethoxazole, and temocillin. Resistance to the carbapenem antibiotic ertapenem was detected in 7 of the 21 isolates. No resistance was observed in any of the tested strains to meropenem, imipenem, piperacillin-tazobactam, colistin, tigecycline, and fosfomycin. All isolates were MDR (resistant to at least three classes) and 9 of the 21 isolates were resistant to at least five antibiotic classes (Fig 3A). The two presumptive VRE strains identified by MALDI biotyping as E. faecalis carried intrinsic erythromycin-resistance and one was tetracycline-resistant (Fig 3B). In subsequent E-TEST none of the two strains proved vancomycin-resistant.
Fig 3. Antibiograms of ESBL-producing E. coli and presumptive VRE E. faecalis from irrigation water.
E. coli and E. faecalis were tested against 32 or 11 clinically relevant antibiotics, respectively. Isolates were grouped by phylogenetic group. (A) Resistance profiles of ESBL-producing E. coli. AM10: ampicillin 10 μg; FEP: cefepime; FOX: cefoxitin; CPD: cefpodoxime; AMC: amoxicillin-clavulanic acid; CRO: ceftriaxone; CXM: cefuroxime; TOB: tobramycin; CN10: gentamicin 10 μg; ETP: ertapenem; NA: nalidixic acid; NOR: norfloxacin; SXT: trimethoprim-sulfamethoxazole; MI: minocycline; K: kanamycin; AK: amikacin; CIP: ciprofloxacin; LEV: levofloxacin; TMP: trimethoprim; SMZ: sulfonamide; F100: nitrofurantoin; TE: tetracycline; TEMO: temocillin; KF: cefalotin; CAZ: ceftazidime; CTX: cefotaxime; PG: phylogenetic group; AB classes: number of antibiotic classes. No resistance was observed to meropenem, piperacillin-tazobactam, colistin, tigecycline, fosfomycin, and imipenem. Asterisks (*) mark isolates used for subsequent plasmid extraction and sequencing. (B) Resistance profiles of presumptive VRE E. faecalis. CN30: gentamicin 30 μg; CN500: gentamicin 500 μg; AM2: ampicillin 2 μg; VAN: vancomycin; NOR: norfloxacin; ERY: erythromycin; STREP HC: streptomycin high concentration; LIN: linezolid; TGC: tigecycline; TE: tetracycline; CM: chloramphenicol.
ESBL-producing E. coli
Typing and virulence factors
Eleven ESBL-producing E. coli strains covering all ESBL positive irrigation water samples were sequenced. Assembled contigs and scaffolds were used for strain typing with online tools. Phylogenetic groups A, B1, B2, and D were detected, with group B1 being the most prevalent one (4 of 11 strains, Table 2). Multilocus sequence typing revealed that two ESBL-producing strains isolated from different water samples (H10 and H30 from water canal B and spring water, respectively) belonged to ST-68 and had all investigated characteristics in common including serotype, virulence factors, and antibiotic resistance profile and determinants. The remaining ESBL-producing strains belonged to different sequence types including one allele combination with not assigned a known sequence type (strain H45, Table 2). Serotypes could be determined for all except three strains, in which no O-antigen was detected. The three O-serogroups, which could not be determined based on sequencing data were analyzed by agglutination at the German Federal Institute for Risk Assessment (BfR, Berlin, Germany).
Table 2. Virulence factors detected in ESBL-producing E. coli from irritation water by whole-cell and plasmid DNA sequencing.
| ID | origin (PG, ST) | previous isolation* | serotype | virulence factors |
|---|---|---|---|---|
| H2 | canal B (A, ST-361) [77] |
human, livestock, cheese, water, sewage | O9:H30 | gad, capU |
| H6 | canal B (B2, ST-1193) [78] |
human, dog, livestock, water, sewage | O75:H5 | gad, iha, sat, vat, senB‡, celb |
| H17 | canal B (B1, ST-1079) [79] |
human, livestock, wild animals, lettuce, water, sewage | O6:H49 | gad, lpfA |
| H10 | canal C (D, ST-68) [80] |
human, dog, cat, livestock, wild animals | O99:H6 | gad, iss, lpfA, eilA |
| H25 | canal C (D, ST-38) [81, 82] |
human, dog, livestock, wild animals, cheese, barley, water, sewage | O153:H30 | gad, iss, iha, eilA, sat, capU, aap, aar, aatA, aggA-D, aggR, ORF3, ORF4 |
| H45 | canal D (B1, n.d.†) |
– | O8:H2 | gad, iss, lpfA, |
| H30 | spring water (D, ST-68) [80] |
human, dog, cat, livestock, wild animals | O99:H6 | gad, iss, lpfA, eilA |
| H22 | river A (B1, ST-641) [83] |
human, livestock, wild animals, celery, water, sewage | O159:H21 | gad, iss, lpfA, |
| H40 | river B (B1, ST-58) [83] |
human, dog, livestock, wild animals, dairy, spinach, feed, water, sewage, soil | ONT:H37 | iss, lpfA, cba, cma |
| H38 | rainwater tank (c) (B2, ST-131) [77] |
human, cat, dog, livestock, wild animals, dairy, water, sewage | O25:H4 | gad, iss, iha, sat |
| H44 | rainwater tank (o) (A, ST-4981) [84] |
human, livestock, flies | O89:H9 | gad, iss |
PG, phylogenetic group according to Clermont et al. [60]; ST, sequence type; (c), closed; (o), open; ONT, O not typable; bold O, determined by agglutination; aap, dispersin; aatA, dispersin transporter protein; aar, aggR-activated regulator; aggA, AAF/I major fimbrial subunit; aggB, AAF/I minor adhesion; aggC/D, usher/chaperone (AAF/I assembly unit); aggR, araC transcriptional activator; capU, hexosyltransferase homolog; cba, colicin B; cma, colicin M; celb, endonuclease colicin E2; eilA, Salmonella HilA homolog; gad, glutamate decarboxylase; iha, adherence protein; iss, increased serum survival; lpfA, long polar fimbriae; ORF3, isoprenoid biosynthesis; ORF4, putative isopentenyl-diphosphate delta-isomerase; sat, secreted autotransporter toxin; senB, plasmid-encoded enterotoxin; vat, vacuolating autotransporter toxin. All virulence factors covered the full length of the detected virulence gene. Bold virulence factors indicate 100% identity between query sequence and virulence gene sequence while slim virulence factors mark imperfect matches (> 98.5% identity).
† adk-6, fumC-4, gyrB-14, icd-642, mdh-9, purA-7, recA-7
‡ plasmid-encoded
* based on sequence type (http://enterobase.warwick.ac.uk/)
A multitude of virulence factors was detected, varying between strains in number and combination. Glutamate decarboxylase (gad) was present in all but one strain (10 of 11), followed by increased serum survival (iss) and long polar fimbriae (lpfA) detected in 8 and 6 of 11 strains, respectively (Table 2). The remaining virulence factors including the putative adherence protein iha were detected in one to three ESBL-producing strains. Strain H38 belonging to the globally spread MDR pandemic clone B2:ST-131 [70] contained apart from gad, iss, and iha the secreted autotransporter toxin sat. Strain H6 B2:ST-1193 harbored three toxin-encoding genes sat, the vacuolating autotransporter toxin vat, and plasmid-encoded enterotoxin senB. Finally, strain H25 D:ST-38 contained by far the most with 13 virulence factors, including sat as well as aggR, aggA-D, dispersin aap, dispersin transporter aatA, and aggR-activated regulator aar (Table 2).
Antibiotic resistance genes and mobile elements
Acquired antibiotic resistance genes and chromosomal point mutations conferring resistance were identified for all ESBL-producing E. coli. All detected resistance genes were located on one to two scaffolds per strain (Table 3). Almost all phenotypic resistances observed in disk diffusion assays could be attributed to the identified resistance determinants.
Table 3. Antibiotic resistance phenotype and genotype of ESBL-producing E. coli from irrigation water.
| ID |
origin (PG, ST) |
antibiotic resistance phenotype | acquired antibiotic resistance genes (grouped by contigs) |
plasmid replicon (% ID; HSP/query) |
point mutations |
|---|---|---|---|---|---|
| H2 | canal B (A, ST-361) |
AM, FEP, CPD, AMC, CRO, CXM, TOB, CN, NA, NOR, SXT, K, CIP, LEV, TMP, SMZ, TEMO, KF, CAZ, CTX |
I. strA, strB, blaTEM-1B, mph(A), sul2, dfrA14 II. aac(3)-IIa, blaCTX-M-15 |
I. IncY (100; 765/765) II. n.d. |
parC p.S80I gyrA p.S83L gyrA p.D87N |
| H6 | canal B (B2, ST-1193) |
AM, FEP, CPD, CRO, CXM, NA, NOR, SXT, K, CIP, LEV, TMP, SMZ, TE, KF, CAZ, CTX | I. strA, strB, aadA5, blaCTX-M-27, mph(A), sul1, sul2, tet(A), dfrA17 | I. IncFIA (99.74; 388/388) IncFIB (96.63; 682/682) | parE p.L416F parC p.S80I gyrA p.S83L gyrA p.D87N |
| H17 | canal B (B1, ST-1079) |
AM, FEP, CPD, CRO, CXM, TOB, CN, SXT, TMP, SMZ, KF, CAZ, CTX |
I. strB, sul2, dfrA14 II. aac(3)-IId, blaCTX-M-1 |
I. n.d. II. n.d. |
n.d. |
| H10 | canal C (D, ST-68) |
AM, FEP, CPD, AMC, CRO, CXM, SMZ, TEMO, KF, CAZ, CTX |
I. strA, strB, blaTEM-1B, sul2 II. blaCTX-M-32 |
I. IncFII (100; 261/261) II. n.d. |
n.d. |
| H25 | canal C (D, ST-38) |
AM, FEP, FOX, CPD, AMC, CRO, CXM, SXT, K, AK, TMP, SMZ, TEMO, KF, CAZ, CTX |
I. strA, strB, aphA1, blaTEM-1B, sul2 II. aadA1, blaCTX-M-14b, dfrA1 |
I. IncQ12 (100, 529/796) II. n.d. |
n.d. |
| H45 | canal D (B1, n.a.1) |
AM, FEP, CPD, AMC, CRO, CXM, ETP, KF, CAZ, CTX | I. blaCTX-M-1 | I. IncI1 (98.59; 142/142) | n.d. |
| H30 | spring water (D, ST-68) |
AM, FEP, CPD, AMC, CRO, CXM, SMZ, TEMO, KF, CAZ, CTX |
I. strA, strB, blaTEM-1B, sul2 II. blaCTX-M-32 |
I. IncFII (100; 261/261) II. n.d. |
n.d. |
| H22 | river A (B1, ST-641) |
AM, FEP, CPD, AMC, CRO, CXM, MI, SMZ, TE, KF, CAZ, CTX | I. blaCTX-M-1, sul2, tet(A) | I. IncI1 (98.59; 142/142) | n.d. |
| H40 | river B (B1, ST-58) |
AM, FEP, CPD, AMC, CRO, CXM, ETP, SXT, MI, K, TMP, SMZ, TE, TEMO, KF, CAZ, CTX |
I. strA, strB, aadA1, sul1, sul2, tet(A), dfrA1 II. blaCTX-M-1, sul2, tet(A) |
I. IncFIB (97.07; 682/682) IncFIC (95.59; 499/499) II. IncI1 (98.59; 142/142) |
n.d. |
| H38 | rainwater tank (c) (B2, ST-131) |
AM, FEP, CPD, AMC, CRO, CXM, ETP, NA, NOR, CIP, LEV, TEMO, KF, CAZ, CTX | I. blaCTX-M-15, mph(A) | I. IncFIB (98.39; 682/682) | parE p.I529L parC p.S80I parC p.E84V gyrA p.S83L gyrA p.D87N |
| H44 | rainwater tank (o) (A, ST-4981) |
AM, FEP, CPD, CRO, CXM, NA, NOR, SXT, CIP, LEV, TMP, SMZ, F100, TE, TEMO, KF, CAZ, CTX |
I. strA, strB, blaTEM-1B, qnrS1, sul2, tet(A), dfrA14 II. blaCTX-M-15 |
I. IncFIB (96.77; 682/682) II. n.d. |
parC p.S80I gyrA p.S83L gyrA p.D87N |
PG, phylogenetic group; ST, sequence type; % ID, percent identical bases between query and sample sequence; HSP/query, alignment length compared to query sequence length; (c), closed; (o), open; n.a., not applicable; n.d., not detected.
1 adk-6, fumC-4, gyrB-14, icd-642, mdh-9, purA-7, recA-7
2 truncated form of IncQ1
Resistance genes sul1 and/or sul2 were present in all sulfonamide-resistant strains, and trimethoprim-resistance genes dfrA1, dfrA14, and dfrA17 were identified in six strains, all of which showed phenotypic trimethoprim-resistance. When these genes (sul and dfrA) were present in the same strain, phenotypic resistance toward antibiotic combination trimethoprim-sulfamethoxazole (SXT, Table 3) was observed. The four tetracycline-resistant strains all carried ARG tet(A). Three strains carried mph(A) but did not show detectable erythromycin-resistance in disk diffusion assays.
With respect to aminoglycoside-resistance, the most frequently detected ARG strA and strB (also designated aph(3”)-Ib and aph(6)-Id, respectively) confer resistance to streptomycin, which was not tested in disk diffusion assays. Further, aadA1 and aadA5 known to confer streptomycin- and spectinomycin-resistance were detected in three strains (not tested). Strains H2 and H17 carried ARG of the aac(3)-II group conferring the observed gentamicin-, tobramycin-resistance, and/or kanamycin-resistance, while no ARG was found in strains H6 and H40 conferring kanamycin-resistance (Table 3). In strain H25, the observed kanamycin-resistance can be explained by the presence of aphA1 [71].
All ESBL-producing strains carried genes of the blaCTX-M-type. Most frequent were blaCTX-M-1 (4 of 11) and blaCTX-M-15 (3 of 11) followed by blaCTX-M-32, blaCTX-M-14b, and blaCTX-M-27 (Table 3). Additionally, five strains harbored blaTEM-1B, which was never located on the same scaffold as the blaCTX-M gene. Apart from resistance to extended-spectrum cephalosporins, ertapenem-resistance was observed in three isolates. Of note, resistance was determined based on the ECOFF value. In addition to resistance towards a broad spectrum of beta-lactams, strains H2, H6, H38, and H44 were resistant to the (fluoro)quinolones nalidixic acid, norfloxacin, ciprofloxacin, and levofloxacin and all carried chromosomal point mutations known to confer resistance. Strain H44 additionally carried the plasmid-mediated quinolone resistance gene qnrS1 (Table 3).
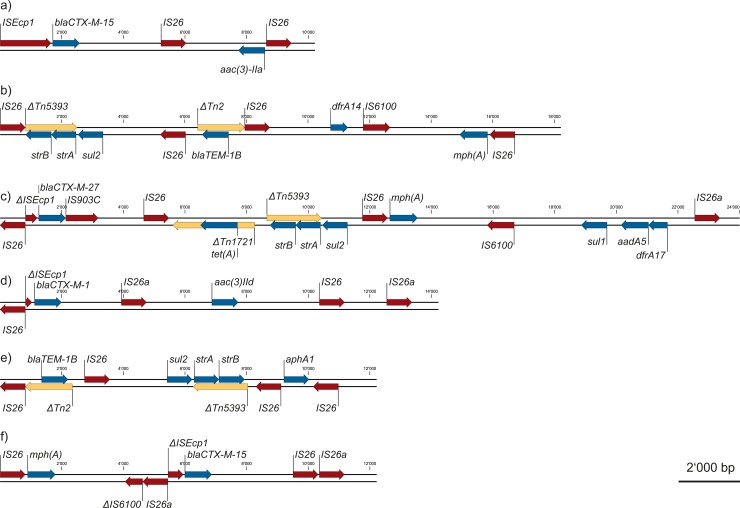
Apart from ARG, plasmid replicons were identified for all except one ESBL strain, suggesting mobility of the associated ARG (Table 3). Most prominent were replicons of the IncF-family, followed by IncI1, IncY, and one truncated version of IncQ1. Screening of the ARG genomic regions for other mobile elements revealed a multitude of insertion sequences and transposons, of which a representative selection is shown in Fig 4. Of special interest is the repeatedly identified insertion sequence IS26 which is frequently involved in remodeling MDR resistance plasmids [72]. ARG bracketed by IS26 or its three-nucleotide variant IS26a included aphA1, aac(3)-IIa, aac(3)-IId, strA, strB, mph(A), blaTEM-1B, blaCTX-M-1, blaCTX-M-15, blaCTX-M-27, dfrA14, tet(A), sul1, and sul2 (Fig 4). blaCTX-M genes were additionally often associated with full-length ISEcp1 (representative example in Fig 4), indicating their potential to be mobilized although no plasmid replicon was assigned to almost half of them (Table 3). Finally, blaTEM-1B was always embedded in a partial or complete Tn2, strA and strB in a partial Tn5393 (examples in Fig 4).
Fig 4. Representative ARG regions displaying ARG and associated insertion sequences.
ESBL strains H2 scaffold II (a) and I (b), H6 scaffold I (c), H17 scaffold II (d), H25 scaffold I (e), and H38 scaffold I (f). IS, insertion sequence; ΔIS, partial insertion sequence; Tn, transposon; ΔTn, partial transposon. Red: insertion sequences; blue: ARG; yellow: transposons.
Discussion
Fecal indicators E. coli and Enterococcus spp. have been well established for routine monitoring of water quality, and this principle has been extended to foods [44]. More recently, both E. coli and Enterococcus spp. have been proposed for monitoring antibiotic resistance [47]. Therefore, considering these bacteria for monitoring water quality with respect to ARB to estimate its suitability for irrigation is close at hand. Guidelines for safe use of waste- and greywater in agriculture exist [73, 74], however, they don’t include ARB, and studies investigating suitability of water for irrigation usually focus on pathogenic bacteria. Ideally, monitoring generic E. coli and Enterococcus spp. would yield a good prediction for presence of clinically relevant ARB and associated resistance genes. In this study, generic E. coli and Enterococcus spp. counts in irrigation water from different vegetable growing areas showed large variations. However, subsequent isolation of ARB strains on different antibiotics delineated a clear trend towards higher percentage of ARB-positive samples with increasing number of corresponding generic bacteria. Of special interest is the increasing number of ESBL-producing E. coli-positive water samples with increasing generic E. coli content. Whether such a correlation holds true for clinically relevant ARB of other species and related ARG remains to be studied. In any case, the presence of ESBL-producing E. coli in 22% of the investigated irrigation water samples is of great concern and emphasizes the need for monitoring irrigation water quality with respect to ARB. The cutoff for surface irrigation water presently advised by SwissGAP of 103 generic E. coli per 100 ml of water [75] is not sufficiently stringent to exclude ESBL-producing E. coli-positive samples, as only 2 of the 8 positive samples in this study reached this threshold.
ESBL-producing E. coli
Phylogeny and virulence factors
ESBL-producing E. coli from the different water samples were investigated in detail. Different phylogenetic groups have been assigned group-specific associations. While phylogenetic groups A and B1 encompass many commensal E. coli, groups B2 and D often contain extraintestinal pathogenic E. coli [76]. Indeed, ESBL strains of groups A and B1 harbored two to four virulence factors, while strains of groups B2 and D had four to thirteen virulence factors, including toxin-encoding genes sat, vat, and senB (Table 2). The sequence type/phylogenetic group combinations identified in this study have all been described before, except for strains H44 (A:ST-4981) and H45 (B1, unknown sequence type). Notably, all identified sequence types including ST-4981 have been described in association with ESBL-producing E. coli [77–84]. All these sequence types have been isolated previously from many different sources, always including humans and livestock and often water (Table 2). Based on these prior reports, humans, livestock, and wild animals (usually including birds) are all probable sources of water contamination with the detected ESBL-producing E. coli. Notably, two E. coli D:ST-68 were isolated once from spring water and once from a water canal, which have been previously isolated from humans, companion animals, livestock, and wild animals, but no isolation from water has been explicitly reported so far (Table 2).
Apart from many commensal strains, E. coli can harbor a wide variety of virulence genes and are divided into at least six main categories [85]. Pathogenic strains can be assigned a pathotype in dependence of the virulence genes they harbor. Increased serum survival (iss) gene, which has long been known for its role in virulence of extraintestinal pathogenic E. coli (ExPEC) [86] was detected in eight of eleven strains (Table 2). ExPEC are strains which can cause infection in organs other than the intestine, most commonly the urinary tract [85]. Other virulence factors frequently produced by uropathogenic E. coli are the type V secreted toxins vacuolating autotransporter toxin (Vat) and secreted autotransporter toxin (Sat) [87]. Encoding genes were present in three ESBL-producing E. coli in combination or alone including pandemic strain B2:ST-131 (Table 2). One strain (H6, B2:ST-1193) carried a plasmid-encoded secreted enterotoxin (senB) gene which has been described to play a role in development of severe diarrhea by enteroinvasive E. coli (EIEC) [88]. Apart from secreted toxins, adhesion factors play an important role for infection, both intra- and extra-intestinally. Such factors are long polar fimbrae (lpfA) as well as Iha, a putative adherence factor found in both ExPEC and diarrheagenic E. coli [89]. Encoding genes were detected in six and three strains, respectively. Finally, ESBL-producing strain H25 D:ST-38 outnumbered all other isolated ESBL-producing strains with thirteen virulence factors. Sequence type 38 has been associated with enteroaggregative E. coli (EAEC) [81]. Indeed, strain H25 harbored known EAEC virulence genes such as dispersin aap [90] or aggA and aggR [91]. The latter two genes have been suggested to suffice alone or in combination for identification of pathogenic EAEC strains. The presence of a pathogenic EAEC strain resistant to extended-spectrum beta-lactams in irrigation water used for fresh produce emphasizes the need for monitoring and regulating irrigation water quality.
Resistance phenotype and genetic background
ESBL-producing Enterobacteriaceae such as E. coli as well as vancomycin-resistant Enterococcus spp. (VRE) are among the clinically most relevant ARB. Being both typical inhabitants of the intestine and occasionally notorious MDR pathogens, they have the potential of establishing in the human gut where they can spread ARG or cause disease. In fact, 5.8% of the Swiss healthy population have been estimated to carry ESBL-producing E. coli [92]. We detected such strains in 22% of water samples all used for fresh produce irrigation, while no VRE were isolated. Presence of ESBL-producing Enterobacteriaceae in surface waters has been described previously [31]. The proportion, however, of ESBL-positive water used in vegetable growing areas for irrigation was unknown and seems considerable. On the other hand, VRE have been detected in wastewaters including un-chlorinated effluent but not water used for irrigation, although increased future use of reclaimed waters for irrigation has been predicted [93]. Genetic analysis of eleven ESBL-producing E. coli showed that apart from a variety of virulence factors, they harbored a high diversity of ARG, always including one gene of the blaCTX-M-type. Concurrent resistance towards fluoroquinolones and various other antibiotic classes considerably narrows down available treatment options. Including the fact that most detected ARG were situated on a plasmid backbone and/or associated with mobile genetic elements, such bacteria in water must be eliminated before applying it for irrigation. From the detected resistance plasmids, IncFII and IncI1 are considered epidemic having the highest occurrence among typed plasmids [94]. The IncF family in particular–the most frequent replicon family in this study–is detected in a variety of Enterobacteriaceae within which they can spread. The frequently detected IS26 (full-length, on 12 of 18 scaffolds) has recently been designated as major player in MDR plasmid remodeling [72] and ISEcp1 has been associated with genetic mobilization of blaCTX-M [95].
Antibiotic resistance profiling using disk diffusion assays is routinely performed in clinics for resistance monitoring and determination of appropriate treatment strategies. With the racing development of next generation sequencing technologies, plug-and-play tools for in silico detection of ARG based on sequence data have been developed, envisioning clinical decision-making based on molecular data rather than phenotypic tests. Our data showed almost perfect concordance between phenotypic and genotypic resistance profiles. Nevertheless, a few phenotypic resistances could not be explained based on the detected genetic determinants. Also, certain treatment options might be missed as the example of mph(A) shows, where despite presence of the ARG no phenotypic resistance was observed. Thus, the molecular approach appears to result in a very accurate albeit imperfect prediction of phenotypic resistance.
Conclusions
We could show high occurrence of ESBL-producing E. coli in irrigation water, with one positive sample in five. We further showed that these strains harbor a diversity of mobile ARG and a variety of virulence factor genes, including toxin genes. To determine the amount of such bacteria in irrigation water, a quantitative rather than enrichment-based approach is needed. However, whatever their abundance in the water, their spread via irrigation onto foods which are consumed raw poses a potential health risk which must be avoided. Therefore, monitoring and regulating irrigation water quality as well as developing affordable sanitation technologies is crucial, especially as the use of surface water and reclaimed wastewaters tends to become more and more common agricultural practice.
Supporting information
Colony forming units (CFU) per 100 ml of water are indicated. Dotted line marks the limit of detection. No significant correlation was observed (ns, not significant).
(TIF)
Fasta files containing scaffolds generated from ESBL-producing E. coli sequencing data using SPAdes algorithm.
(ZIP)
Fasta files containing scaffolds generated from ESBL-producing E. coli sequencing data using SGA scaffolder.
(ZIP)
Fasta files containing scaffolds generated from ESBL-producing E. coli sequencing data and selected for uploaded to online tool MARA.
(ZIP)
Acknowledgments
We are grateful to Hannah Bruderer for conducting part of the samplings and microbiological analysis, Monika Volkan and Anita Kläui for experimental assistance, Roger Marti for providing protocols and scientific assistance, and Martina Marchesi (Institute of Medical Microbiology, University of Zurich) for assistance in phenotypic resistance testing and critically reading the manuscript. We are thankful to Andrea Patrignani for support in PacBio sequencing. We acknowledge Elisabeth Hauser (German Federal Institute for Risk Assessment) for serotyping of strains.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was funded by the Agroscope Research Programme "Reduction and Dynamics of Antibiotic-resistant and Persistent Microorganisms along Food Chains (REDYMO)", the National Research Programme "Antimicrobial Resistance" (NRP 72) of the Swiss National Science Foundation and the COST Action CA16110 "Control of Human Pathogenic Micro-organisms in Plant Production Systems HUPLANTcontrol)". The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Holmstrup P, Klausen B. The growing problem of antimicrobial resistance. Oral Dis. 2018;24(3):291–5. 10.1111/odi.12610 [DOI] [PubMed] [Google Scholar]
- 2.who.int [Internet]. World Health Organization (WHO): Antibiotic resistance—fact sheet; c2017 [cited 2017 Nov]. Available from: http://www.who.int/mediacentre/factsheets/antibiotic-resistance/en/.
- 3.Perry JA, Wright GD. The antibiotic resistance “mobilome”: searching for the link between environment and clinic. Front Microbiol. 2013;4:138 10.3389/fmicb.2013.00138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perry JA, Waglechner N, Wright GD. The prehistory of antibiotic resistance. Cold Spring Harb Perspect Med. 2016;6(6):a025197 10.1101/cshperspect.a025197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finley RL, Collignon P, Larsson DGJ, McEwen SA, Li X-Z, Gaze WH, et al. The scourge of antibiotic resistance: the important role of the environment. Clin Infect Dis. 2013;57(5):704–10. 10.1093/cid/cit355 [DOI] [PubMed] [Google Scholar]
- 6.Bergeron S, Brown R, Homer J, Rehage S, Boopathy R. Presence of antibiotic resistance genes in different salinity gradients of freshwater to saltwater marshes in southeast Louisiana, USA. Int Biodeterior Biodegradation. 2016;113:80–7. [Google Scholar]
- 7.Czekalski N, Berthold T, Caucci S, Egli A, Bürgmann H. Increased levels of multiresistant bacteria and resistance genes after wastewater treatment and their dissemination into lake Geneva, Switzerland. Front Microbiol. 2012;3:106 10.3389/fmicb.2012.00106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adefisoye MA, Okoh AI. Identification and antimicrobial resistance prevalence of pathogenic Escherichia coli strains from treated wastewater effluents in Eastern Cape, South Africa. Microbiologyopen. 2016;5(1):143–51. 10.1002/mbo3.319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amos GCA, Hawkey PM, Gaze WH, Wellington EM. Waste water effluent contributes to the dissemination of CTX-M-15 in the natural environment. J Antimicrob Chemother. 2014;69(7):1785–91. 10.1093/jac/dku079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McKeon DM, Calabrese JP, Bissonnette GK. Antibiotic resistant Gram-negative bacteria in rural groundwater supplies. Water Res. 1995;29(8):1902–8. [Google Scholar]
- 11.Messi P, Guerrieri E, Bondi M. Antibiotic resistance and antibacterial activity in heterotrophic bacteria of mineral water origin. Sci Total Environ. 2005;346(1):213–9. [DOI] [PubMed] [Google Scholar]
- 12.Zhang X-X, Zhang T, Fang HH. Antibiotic resistance genes in water environment. Appl Microbiol Biotechnol. 2009;82(3):397–414. 10.1007/s00253-008-1829-z [DOI] [PubMed] [Google Scholar]
- 13.Bai X, Ma X, Xu F, Li J, Zhang H, Xiao X. The drinking water treatment process as a potential source of affecting the bacterial antibiotic resistance. Sci Total Environ. 2015;533:24–31. 10.1016/j.scitotenv.2015.06.082 [DOI] [PubMed] [Google Scholar]
- 14.Rizzo L, Manaia C, Merlin C, Schwartz T, Dagot C, Ploy M, et al. Urban wastewater treatment plants as hotspots for antibiotic resistant bacteria and genes spread into the environment: a review. Sci Total Environ. 2013;447:345–60. 10.1016/j.scitotenv.2013.01.032 [DOI] [PubMed] [Google Scholar]
- 15.Farkas A, Bocoş B, Butiuc-Keul A. Antibiotic resistance and intI1 carriage in waterborne Enterobacteriaceae. Water Air Soil Pollut. 2016;227(7):1–11. [Google Scholar]
- 16.Uyttendaele M, Jaykus LA, Amoah P, Chiodini A, Cunliffe D, Jacxsens L, et al. Microbial hazards in irrigation water: Standards, norms, and testing to manage use of water in fresh produce primary production. Compr Rev Food Sci Food Saf. 2015;14(4):336–56. [Google Scholar]
- 17.Christou A, Agüera A, Bayona JM, Cytryn E, Fotopoulos V, Lambropoulou D, et al. The potential implications of reclaimed wastewater reuse for irrigation on the agricultural environment: The knowns and unknowns of the fate of antibiotics and antibiotic resistant bacteria and resistance genes—A review. Water Res. 2017;123:448–67. 10.1016/j.watres.2017.07.004 [DOI] [PubMed] [Google Scholar]
- 18.Fahrenfeld N, Ma Y, O'Brien M, Pruden A. Reclaimed water as a reservoir of antibiotic resistance genes: distribution system and irrigation implications. Front Microbiol. 2013;4:130 10.3389/fmicb.2013.00130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gemmell ME, Schmidt S. Microbiological assessment of river water used for the irrigation of fresh produce in a sub-urban community in Sobantu, South Africa. Food Res Int. 2012;47(2):300–5. [Google Scholar]
- 20.Olaimat AN, Holley RA. Factors influencing the microbial safety of fresh produce: A review. Food Microbiol. 2012;32(1):1–19. 10.1016/j.fm.2012.04.016 [DOI] [PubMed] [Google Scholar]
- 21.Fonseca JM, Fallon SD, Sanchez CA, Nolte KD. Escherichia coli survival in lettuce fields following its introduction through different irrigation systems. J Appl Microbiol. 2011;110(4):893–902. 10.1111/j.1365-2672.2011.04942.x [DOI] [PubMed] [Google Scholar]
- 22.Araújo S, Silva IAT, Tacão M, Patinha C, Alves A, Henriques I. Characterization of antibiotic resistant and pathogenic Escherichia coli in irrigation water and vegetables in household farms. Int J Food Microbiol. 2017;257:192–200. 10.1016/j.ijfoodmicro.2017.06.020 [DOI] [PubMed] [Google Scholar]
- 23.Falomir MP, Gozalbo D, Rico H. Coliform bacteria in fresh vegetables: from cultivated land to consumers In: Méndez-Vilas A, editor. Current Research, Technology and Education Topics in Applied Microbiology and Microbial Biotechnology: FORMATEX; 2010. p. 1175–81. [Google Scholar]
- 24.Pesavento G, Calonico C, Ducci B, Magnanini A, Lo Nostro A. Prevalence and antibiotic resistance of Enterococcus spp. isolated from retail cheese, ready-to-eat salads, ham, and raw meat. Food Microbiol. 2014;41:1–7. 10.1016/j.fm.2014.01.008 [DOI] [PubMed] [Google Scholar]
- 25.Nüesch-Inderbinen M, Zurfluh K, Peterhans S, Hächler H, Stephan R. Assessment of the prevalence of extended-spectrum beta-lactamase-producing Enterobacteriaceae in ready-to-eat salads, fresh-cut fruit, and sprouts from the Swiss market. J Food Prot. 2015;78(6):1178–81. 10.4315/0362-028X.JFP-15-018 [DOI] [PubMed] [Google Scholar]
- 26.Hassan SA, Altalhi AD, Gherbawy YA, El-Deeb BA. Bacterial load of fresh vegetables and their resistance to the currently used antibiotics in Saudi Arabia. Foodborne Pathog Dis. 2011;8(9):1011–8. 10.1089/fpd.2010.0805 [DOI] [PubMed] [Google Scholar]
- 27.Tenover FC. Mechanisms of Antimicrobial Resistance in Bacteria. Am J Med. 2006;119(6 Suppl 1):S3–10. [DOI] [PubMed] [Google Scholar]
- 28.Magiorakos AP, Srinivasan A, Carey R, Carmeli Y, Falagas M, Giske C, et al. Multidrug‐resistant, extensively drug‐resistant and pandrug‐resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–81. 10.1111/j.1469-0691.2011.03570.x [DOI] [PubMed] [Google Scholar]
- 29.cdc.gov [Internet]. Centers for Disease Control and Prevention (CDC): Antibiotic / Antimicrobial Resistance—Biggest Threats; c2017 [cited 2017 Nov]. Available from: https://www.cdc.gov/drugresistance/biggest_threats.html.
- 30.Tacconelli E, Magrini N, Kahlmeter G, Singh N. Global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics. World Health Organization. 2017:1–7. [Google Scholar]
- 31.Zurfluh K, Hächler H, Nüesch-Inderbinen M, Stephan R. Characteristics of extended-spectrum beta-lactamase- and carbapenemase-producing Enterobacteriaceae isolates from rivers and lakes in Switzerland. Appl Environ Microbiol. 2013;79(9):3021–6. 10.1128/AEM.00054-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Blaak H, de Kruijf P, Hamidjaja RA, van Hoek AHAM, de Roda Husman AM, Schets FM. Prevalence and characteristics of ESBL-producing E. coli in Dutch recreational waters influenced by wastewater treatment plants. Vet Microbiol. 2014;171(3):448–59. [DOI] [PubMed] [Google Scholar]
- 33.Tissera S, Lee SM. Isolation of extended spectrum β-lactamase (ESBL) producing bacteria from urban surface waters in Malaysia. Malays J Med Sci. 2013;20(3):14–22. [PMC free article] [PubMed] [Google Scholar]
- 34.Korzeniewska E, Harnisz M. Extended-spectrum beta-lactamase (ESBL)-positive Enterobacteriaceae in municipal sewage and their emission to the environment. J Environ Manage. 2013;128(Suppl C):904–11. [DOI] [PubMed] [Google Scholar]
- 35.Guenther S, Ewers C, Wieler LH. Extended-spectrum beta-lactamases producing E. coli in wildlife, yet another form of environmental pollution? Front Microbiol. 2011;2:246 10.3389/fmicb.2011.00246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Young S, Nayak B, Sun S, Badgley BD, Rohr JR, Harwood VJ. Vancomycin-resistant enterococci and bacterial community structure following a sewage spill into an aquatic environment. Appl Environ Microbiol. 2016;82(18):5653–60. 10.1128/AEM.01927-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roberts M, Soge O, Giardino M, Mazengia E, Ma G, Meschke J. Vancomycin-resistant Enterococcus spp. in marine environments from the West Coast of the USA. J Appl Microbiol. 2009;107(1):300–7. 10.1111/j.1365-2672.2009.04207.x [DOI] [PubMed] [Google Scholar]
- 38.Nam S, Kim M-j, Park C, Park J-G, Maeng PJ, Lee G-C. Detection and genotyping of vancomycin-resistant Enterococcus spp. by multiplex polymerase chain reaction in Korean aquatic environmental samples. Int J Hyg Environ Health. 2013;216(4):421–7. 10.1016/j.ijheh.2012.12.004 [DOI] [PubMed] [Google Scholar]
- 39.Bessa LJ, Barbosa-Vasconcelos A, Mendes Â, Vaz-Pires P, Martins da Costa P. High prevalence of multidrug-resistant Escherichia coli and Enterococcus spp. in river water, upstream and downstream of a wastewater treatment plant. J Water Health. 2014;12(3):426–35. 10.2166/wh.2014.160 [DOI] [PubMed] [Google Scholar]
- 40.Santiago-Rodriguez TM, Rivera JI, Coradin M, Toranzos GA. Antibiotic-resistance and virulence genes in Enterococcus isolated from tropical recreational waters. J Water Health. 2013;11(3):387–96. 10.2166/wh.2013.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martinez JL. Environmental pollution by antibiotics and by antibiotic resistance determinants. Environ Pollut. 2009;157(11):2893–902. 10.1016/j.envpol.2009.05.051 [DOI] [PubMed] [Google Scholar]
- 42.Giger W, Alder AC, Golet EM, Kohler H-PE, McArdell CS, Molnar E, et al. Occurrence and fate of antibiotics as trace contaminants in wastewaters, sewage sludges, and surface waters. Chimia (Aarau). 2003;57(9):485–91. [Google Scholar]
- 43.Ensink JH, Mahmood T, Dalsgaard A. Wastewater‐irrigated vegetables: market handling versus irrigation water quality. Trop Med Int Health. 2007;12(S2):2–7. [DOI] [PubMed] [Google Scholar]
- 44.Jay JM, Loessner MJ, Golden DA. Indicators of food microbial quality and safety. Modern food microbiology 7th ed New York: Springer Science and Business Media; 2005. p. 473–95. [Google Scholar]
- 45.Pappas EA, Kanwar RS, Baker JL, Lorimor JC, Mickelson S. Fecal indicator bacteria in subsurface drain water following swine manure application. Trans ASABE. 2008;51(5):1567–73. [Google Scholar]
- 46.Anderson KL, Whitlock JE, Harwood VJ. Persistence and differential survival of fecal indicator bacteria in subtropical waters and sediments. Appl Environ Microbiol. 2005;71(6):3041–8. 10.1128/AEM.71.6.3041-3048.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.European Food Safety Authority (EFSA). Report from the Task Force on Zoonoses Data Collection including guidance for harmonized monitoring and reporting of antimicrobial resistance in commensal Escherichia coli and Enterococcus spp. from food animals. EFSA journal. 2008;141:1–44. [Google Scholar]
- 48.Szmolka A, Nagy B. Multidrug resistant commensal Escherichia coli in animals and its impact for public health. Front Microbiol. 2013;4:258 10.3389/fmicb.2013.00258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Leisibach S. Antibiotic resistance genes in food: molecular identification and transfer between microorganisms with emphasis on enterococci [dissertation]: Swiss Federal Institute of Technology Zurich (ETHZ); 2004.
- 50.Franz CMAP, Holzapfel WH, Stiles ME. Enterococci at the crossroads of food safety? Int J Food Microbiol. 1999;47(1–2):1–24. [DOI] [PubMed] [Google Scholar]
- 51.Palmer KL, Kos VN, Gilmore MS. Horizontal gene transfer and the genomics of enterococcal antibiotic resistance. Curr Opin Microbiol. 2010;13(5):632–9. 10.1016/j.mib.2010.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thomas CM, Nielsen KM. Mechanisms of, and barriers to, horizontal gene transfer between bacteria. Nat Rev Microbiol. 2005;3(9):711–21. 10.1038/nrmicro1234 [DOI] [PubMed] [Google Scholar]
- 53.Gekenidis MT, Studer P, Wüthrich S, Brunisholz R, Drissner D. Beyond the matrix-assisted laser desorption ionization (MALDI) biotyping workflow: in search of microorganism-specific tryptic peptides enabling discrimination of subspecies. Appl Environ Microbiol. 2014;80(14):4234–41. 10.1128/AEM.00740-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gekenidis MT, Gossin D, Schmelcher M, Schöner U, Remus‐Emsermann MN, Drissner D. Dynamics of culturable mesophilic bacterial communities of three fresh herbs and their production environment. J Appl Microbiol. 2017;123(4):916–32. 10.1111/jam.13532 [DOI] [PubMed] [Google Scholar]
- 55.European Committee on Antimicrobial Susceptibility Testing (EUCAST). Antimicrobial susceptibility testing EUCAST disk diffusion method. Version 2.0. 2012.
- 56.Hombach M, Zbinden R, Böttger EC. Standardisation of disk diffusion results for antibiotic susceptibility testing using the sirscan automated zone reader. BMC Microbiol. 2013;13(1):225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.European Food Safety Authority (EFSA). Technical specifications for the analysis and reporting of data on antimicrobial resistance (AMR) in the European Union Summary Report. EFSA journal. 2012;10(2):2587. [Google Scholar]
- 58.Leclercq R, Cantón R, Brown DF, Giske CG, Heisig P, MacGowan AP, et al. EUCAST expert rules in antimicrobial susceptibility testing. Clin Microbiol Infect. 2013;19(2):141–60. 10.1111/j.1469-0691.2011.03703.x [DOI] [PubMed] [Google Scholar]
- 59.European Committee on Antimicrobial Susceptibility Testing (EUCAST). EUCAST guidelines for detection of resistance mechanisms and specific resistances of clinical and/or epidemiological importance. Version 1.0. EUCAST, Basel, Switzerland. 2013.
- 60.Clermont O, Christenson JK, Denamur E, Gordon DM. The Clermont Escherichia coli phylo-typing method revisited: improvement of specificity and detection of new phylo-groups. Environ Microbiol Rep. 2013;5(1):58–65. 10.1111/1758-2229.12019 [DOI] [PubMed] [Google Scholar]
- 61.Larsen MV, Cosentino S, Rasmussen S, Friis C, Hasman H, Marvig RL, et al. Multilocus sequence typing of total genome sequenced bacteria. J Clin Microbiol. 2012;50:1355–61. 10.1128/JCM.06094-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Joensen KG, Tetzschner AM, Iguchi A, Aarestrup FM, Scheutz F. Rapid and easy in silico serotyping of Escherichia coli using whole genome sequencing (WGS) data. J Clin Microbiol. 2015;53(8):2410–26. 10.1128/JCM.00008-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Joensen KG, Scheutz F, Lund O, Hasman H, Kaas RS, Nielsen EM, et al. Real-time whole-genome sequencing for routine typing, surveillance, and outbreak detection of verotoxigenic Escherichia coli. J Clin Microbiol. 2014;52(5):1501–10. 10.1128/JCM.03617-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zankari E, Hasman H, Cosentino S, Vestergaard M, Rasmussen S, Lund O, et al. Identification of acquired antimicrobial resistance genes. J Antimicrob Chemother. 2012;67(11):2640–4. 10.1093/jac/dks261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Koren S, Walenz BP, Berlin K, Miller JR, Bergman NH, Phillippy AM. Canu: scalable and accurate long-read assembly via adaptive k-mer weighting and repeat separation. Genome Res. 2017;27(5):722–36. 10.1101/gr.215087.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Simpson JT, Durbin R. Efficient de novo assembly of large genomes using compressed data structures. Genome Res. 2012;22(3):549–56. 10.1101/gr.126953.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Walker BJ, Abeel T, Shea T, Priest M, Abouelliel A, Sakthikumar S, et al. Pilon: an integrated tool for comprehensive microbial variant detection and genome assembly improvement. PLoS One. 2014;9(11):e112963 10.1371/journal.pone.0112963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bankevich A, Nurk S, Antipov D, Gurevich AA, Dvorkin M, Kulikov AS, et al. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol. 2012;19(5):455–77. 10.1089/cmb.2012.0021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Partridge SR, Tsafnat G, Coiera E, Iredell JR. Gene cassettes and cassette arrays in mobile resistance integrons. FEMS Microbiol Rev. 2009;33(4):757–84. 10.1111/j.1574-6976.2009.00175.x [DOI] [PubMed] [Google Scholar]
- 70.Petty NK, Zakour NLB, Stanton-Cook M, Skippington E, Totsika M, Forde BM, et al. Global dissemination of a multidrug resistant Escherichia coli clone. PNAS. 2014;111(15):5694–9. 10.1073/pnas.1322678111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shaw K, Rather P, Hare R, Miller G. Molecular genetics of aminoglycoside resistance genes and familial relationships of the aminoglycoside-modifying enzymes. Microbiol Rev. 1993;57(1):138–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.He S, Hickman AB, Varani AM, Siguier P, Chandler M, Dekker JP, et al. Insertion sequence IS26 reorganizes plasmids in clinically isolated multidrug-resistant bacteria by replicative transposition. MBio. 2015;6(3):e00762–15. 10.1128/mBio.00762-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.World Health Organization (WHO). Guidelines for the safe use of wastewater, excreta and greywater. Volume II: Wastewater use in agriculture: Geneva: World Health Organization; 2006. [Google Scholar]
- 74.Maimon A, Tal A, Friedler E, Gross A. Safe on-site reuse of greywater for irrigation-a critical review of current guidelines. Environ Sci Technol. 2010;44(9):3213–20. 10.1021/es902646g [DOI] [PubMed] [Google Scholar]
- 75.agrosolution.ch [Internet]. SwissGAP: Risikoanalyse Bewässerungswasser (2017); c2018 [cited 2018 Feb]. Available from: https://agrosolution.ch/swissgap/.
- 76.Russo TA, Johnson JR. Proposal for a new inclusive designation for extraintestinal pathogenic isolates of Escherichia coli: ExPEC. J Infect Dis. 2000;181(5):1753–4. 10.1086/315418 [DOI] [PubMed] [Google Scholar]
- 77.Dahmen S, Haenni M, Châtre P, Madec J-Y. Characterization of blaCTX-M IncFII plasmids and clones of Escherichia coli from pets in France. J Antimicrob Chemother. 2013;68(12):2797–801. 10.1093/jac/dkt291 [DOI] [PubMed] [Google Scholar]
- 78.Xia S, Fan X, Huang Z, Xia L, Xiao M, Chen R, et al. Dominance of CTX-M-type extended-spectrum β-lactamase (ESBL)-producing Escherichia coli isolated from patients with community-onset and hospital-onset infection in China. PLoS One. 2014;9(7):e100707 10.1371/journal.pone.0100707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Apostolakos I, Franz E, van Hoek AH, Florijn A, Veenman C, Sloet-van Oldruitenborgh-Oosterbaan MM, et al. Occurrence and molecular characteristics of ESBL/AmpC-producing Escherichia coli in faecal samples from horses in an equine clinic. J Antimicrob Chemother. 2017;72(7):1915–21. 10.1093/jac/dkx072 [DOI] [PubMed] [Google Scholar]
- 80.Abdelaziz MO, Bonura C, Aleo A, Fasciana T, Calà C, Mammina C. Cephalosporin resistant Escherichia coli from cancer patients in Cairo, Egypt. Microbiol Immunol. 2013;57(5):391–5. 10.1111/1348-0421.12046 [DOI] [PubMed] [Google Scholar]
- 81.Chattaway MA, Jenkins C, Ciesielczuk H, Day M, DoNascimento V, Day M, et al. Evidence of evolving extraintestinal enteroaggregative Escherichia coli ST38 clone. Emerg Infect Dis. 2014;20(11):1935 10.3201/eid2011.131845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Poirel L, Bernabeu S, Fortineau N, Podglajen I, Lawrence C, Nordmann P. Emergence of OXA-48-producing Escherichia coli clone ST38 in France. Antimicrob Agents Chemother. 2011;55(10):4937–8. 10.1128/AAC.00413-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Schauss T, Glaeser SP, Gütschow A, Dott W, Kämpfer P. Improved detection of extended spectrum beta-lactamase (ESBL)-producing Escherichia coli in input and output samples of German biogas plants by a selective pre-enrichment procedure. PLoS One. 2015;10(3):e0119791 10.1371/journal.pone.0119791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lee W-C, Yeh K-S. Characteristics of extended-spectrum β-lactamase-producing Escherichia coli isolated from fecal samples of piglets with diarrhea in central and southern Taiwan in 2015. BMC Vet Res. 2017;13(1):66 10.1186/s12917-017-0986-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Scheutz F, Strockbine NA. Escherichia In: Whitman WB, editor. Bergey's manual of systematics of Archaea and Bacteria. Online: John Wiley and Sons; 2015. p. 1–49. [Google Scholar]
- 86.Johnson TJ, Wannemuehler YM, Nolan LK. Evolution of the iss gene in Escherichia coli. Appl Environ Microbiol. 2008;74(8):2360–9. 10.1128/AEM.02634-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wiles TJ, Kulesus RR, Mulvey MA. Origins and virulence mechanisms of uropathogenic Escherichia coli. Exp Mol Pathol. 2008;85(1):11–9. 10.1016/j.yexmp.2008.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kalu M, editor Enterotoxin-coding virulence gene senB and multidrug resistance genes in Escherichia coli. 2017 AAAS Annual Meeting (February 16–20, 2017); 2017: AAAS.
- 89.Léveillé S, Caza M, Johnson JR, Clabots C, Sabri M, Dozois CM. Iha from an Escherichia coli urinary tract infection outbreak clonal group A strain is expressed in vivo in the mouse urinary tract and functions as a catecholate siderophore receptor. Infect Immun. 2006;74(6):3427–36. 10.1128/IAI.00107-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sheikh J, Czeczulin JR, Harrington S, Hicks S, Henderson IR, Le Bouguénec C, et al. A novel dispersin protein in enteroaggregative Escherichia coli. J Clin Investig. 2002;110(9):1329 10.1172/JCI16172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jiang Z-D, Greenberg D, Nataro JP, Steffen R, DuPont HL. Rate of occurrence and pathogenic effect of enteroaggregative Escherichia coli virulence factors in international travelers. J Clin Microbiol. 2002;40(11):4185–90. 10.1128/JCM.40.11.4185-4190.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Geser N, Stephan R, Korczak BM, Beutin L, Hächler H. Molecular identification of blaESBL genes from Enterobacteriaceae isolated from healthy human carriers in Switzerland. Antimicrob Agents Chemother. 2011;56(3):1609–12. 10.1128/AAC.05539-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Goldstein RER, Micallef SA, Gibbs SG, George A, Claye E, Sapkota A, et al. Detection of vancomycin-resistant enterococci (VRE) at four US wastewater treatment plants that provide effluent for reuse. Sci Total Environ. 2014;466:404–11. 10.1016/j.scitotenv.2013.07.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Carattoli A. Resistance plasmid families in Enterobacteriaceae. Antimicrob Agents Chemother. 2009;53(6):2227–38. 10.1128/AAC.01707-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Cantón R, González-Alba JM, Galán JC. CTX-M Enzymes: Origin and Diffusion. Front Microbiol. 2012;3:110 10.3389/fmicb.2012.00110 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Colony forming units (CFU) per 100 ml of water are indicated. Dotted line marks the limit of detection. No significant correlation was observed (ns, not significant).
(TIF)
Fasta files containing scaffolds generated from ESBL-producing E. coli sequencing data using SPAdes algorithm.
(ZIP)
Fasta files containing scaffolds generated from ESBL-producing E. coli sequencing data using SGA scaffolder.
(ZIP)
Fasta files containing scaffolds generated from ESBL-producing E. coli sequencing data and selected for uploaded to online tool MARA.
(ZIP)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.