Abstract
The current study aimed to extend the results of White et al. (2015) by examining the moderating role of attention biases at age 5 on the relations between Behavioral Inhibition (BI) during toddlerhood and anxiety symptoms at age 10. Children’s BI at 2 and 3 years of age was measured using laboratory assessments, and attention bias towards threat was assessed using a dot-probe task at age 5. Latent Class Analysis (LCA) was used to identify the probability for children’s membership in an anxiety class, which reflected primary anxiety at age 10 that was not comorbid with symptoms of inattention. Maternal and self-report measures of children’s mental health, collected via questionnaires and semi-structured diagnostic interviews, were used as indicators for the LCA. The results revealed that threat-related attention biases moderated the relation between BI and anxiety, such that BI positively predicted the probability of being in the anxiety class only when children had an attention bias towards threat. BI was unrelated to anxiety when children had no attention bias or an attention bias away from threat. These results indicated that attention biases during preschool may differentiate between inhibited children who are at heightened risk for anxiety later in childhood from those who are not. The results are discussed in a framework detailing the role of attention biases in increasing the sensitivity for anxiety-related problems in children who display high levels of BI during early childhood.
Keywords: Attention Biases, Anxiety, Behavioral Inhibition, Temperament
Introduction
Behavioral inhibition (BI) is an early childhood temperamental trait characterized by high levels of vigilance, negative reactivity, and reticent behaviors in response to unfamiliar objects, people, or situations (Degnan & Fox, 2007). Most children with early childhood BI continue to display withdrawn behaviors across middle childhood and adolescence (Fox, Henderson, Marshall, Nicholas & Ghera, 2005; Rubin, Coplan, & Bowker, 2009). Further, adolescents with high and stable patterns of childhood BI exhibit more social avoidance, sensitivity towards social rejection, and stress-related anxiety than their non-inhibited counterparts (Fox & Pine, 2012). Hence, early childhood BI predicts risk for later anxiety, particularly social anxiety (Ballespi, Jane & Riba, 2012; Svihra & Katzman, 2004).
Nevertheless, not all inhibited children continue to develop anxiety later in life (Degnan & Fox, 2007). Indeed, some studies have found no direct link between early childhood BI and later anxiety problems (Gladstone, Parker, Mitchell, Wilhelm, & Malhi, 2005; Biederman et al., 2001), particularly when BI is not sustained across early childhood (Degnan et al., 2014). These results suggest that some inhibited children may have buffers that protect them from internalizing problems, including anxiety. Thus, there has been a growing interest in identifying moderating factors and mechanisms that may play a role in discontinuity of the relation between BI and later internalizing behavior problems (Degnan & Fox, 2007; Degnan, Almas, & Fox, 2010).
Several contextual (e.g., parenting; Lewis-Morraty et al., 2012) and individual factors (e.g., cognitive and attention mechanisms; Lamm et al., 2014; White, McDermott, Degan, Henderson & Fox, 2011) have been found to moderate the link between BI and later anxiety. For example, attention bias towards threat involves the preferential allocation of attention towards the threat. This cognitive mechanism may moderate the link between BI and anxiety (Bar-Haim, Lamy, Pergamin, Bakermans-Kranenburg, & van IJzendoorn, 2007; Lonigan, Vasey, Philips, & Hazen, 2004). Such biases manifest in individuals diagnosed with anxiety (Bar-Haim et al., 2007), and thus, may create vulnerability for the development of anxiety disorders (Lonigan et al., 2004).
Few developmental studies examine attention bias towards threat among anxious children from community samples (Lonigan & Vasey, 2008; Salum et al., 2013; Szpunar & Young, 2013). Even less research examines associations between attentional biases and anxiety symptoms during early childhood and among temperamentally inhibited children (Lonigan et al., 2004). Understanding the role that attentional biases play in the link between temperamental risk factors and anxiety among young children from non-clinical samples can inform treatment research and prevention programs (e.g., attention bias modification training; Lowther & Newman, 2014). One notable study among young children from community sample is Perez-Edgar et al. (2011); this work tested the associations of children’s behavioral inhibition across 2 and 3 years of age to 5-year attention biases and social withdrawn behaviors, and found that only inhibited children who had bias towards threatening facial expressions displayed socially withdrawn behaviors at age 5. To expand this work, White et al. (2015) tested the moderating roles of 5- and 7-year attention biases towards threat in relations between early BI and anxiety symptoms at 5 and 7 years of age, and found that early BI was positively related to children’s 7-year anxiety symptoms only for children who concurrently had attention bias towards threat (but not those who had attention bias away from the threat). However, White et al., (2015) did not find main or interaction effects involving 5-year attention biases. One potential reason for this lack of findings may be because anxiety disorders, particularly social anxiety, often emerge later in life during late childhood or early adolescence (Beesdo, Knappe, & Pine, 2009; McKay & Storch, 2011).
In the aforementioned studies, the results involved concurrent measures of attention bias and anxiety. More research needs to be conducted to examine long-term effects of early attention bias on later anxiety symptoms, particularly during transition to adolescence, which is characterized as a risk phases for developing anxiety disorders among temperamentally vulnerable children (Haller, Kadosh, Scerif, & Lau, 2015; Giedd, Keshavan, & Paus, 2009). Furthermore, previous studies used single measures to assess internalizing symptoms pertaining to anxiety, often parent or self-report questionnaires or clinical interviews. Current views of mental health research highlight the importance of examining psychopathology on several dimensions along a continuum (ranging from mild to extreme), and taking into account the possibility of comorbidity between dimensions as opposed to a qualitative split indexed by a mere presence or absence of clinical diagnosis (e.g. Frenkel et al., 2015; Adam, 2013; Cuthbert & Insel, 2010). This conceptualization of psychopathology emphasizes the importance of using multiple methods of assessment about the person’s behaviors (Achenbach, 2006; Horton, Laird, & Zahner, 1999).
Guided by this framework and to extend previous work by Perez-Edgar et al. (2011) and White et al. (2015), we used the same sample from these two reports to test the moderating role of attention bias towards threat in the relations between early childhood BI and children’s anxiety symptoms during transition into adolescence. The current study extended previous longitudinal work by White et al. (2015) to employ a person-oriented analytic approach (i.e., latent class analyses) rather than a variable-oriented approach and to identify a class of children who had high levels of anxiety that was not comorbid with other forms of psychopathology (see Frenkel et al., 2015). Consistent with previous studies, it was predicted that threat-related attention bias during early childhood would moderate the associations between early BI and anxiety during preadolescence.
Method
Participants
Participants were a subsample of 291 children (156 females), recruited from a large metropolitan area in the Mid-Atlantic region of the United States and selected to participate in a longitudinal study of temperament and social adaptation (see White et al., 2015). Infants who were full-term and did not have any developmental sickness/disorder were recruited and came to the laboratory at 4 months of age to participate in a series of tasks to assess their positive, negative, and motor reactivity (for a detailed description of the sample and early screening of infants for the large longitudinal study see Hane, Fox, Henderson, & Marshall, 2008). The ethnic distribution of the selected sample was as follows: 64.3% Caucasian, 14.1% African American, 3.4 % Hispanic, 2.1% Asian, with 14.7% of participants reported to be multiracial and 1.4% reported to have other ethnic backgrounds. The majority of mothers in the sample had college or graduate degree (84.4%) or graduated from high school (15.6%).
Of the 291 children from the original sample, 224 and 197 children came to the lab at 2 and 3 years of age, respectively, to participate in several laboratory tasks to measure their BI (Mage = 26.08 months, SD = 2.21; M = 36.82 months, SD = 1.56; at 2- and 3-year visit assessments, respectively). Children were brought back to the laboratory at 5 years of age (N = 207 Mage = 63.11 months, SD = 3.85) to complete the attention bias assessment. At 10 years of age, mental health was assessed using parents’ and children’s reports as well as clinical interviews administered during home visits (N = 189, Mage = 121.81 months, SD = 4.80).
BI composite score
Children’s BI was assessed using laboratory tasks during early toddler years. Specifically, children’s behaviors and reactions in response to unfamiliar social (i.e., interaction with an unfamiliar adult; stranger episode) and non-social (i.e., tunnel, robot) stimuli were coded from videotapes by two trained research assistants when children were 2 and 3 years of age. The stranger episode lasted three minutes and the robot and tunnel episodes lasted 2 minutes each. A more detailed description of the laboratory observation and episode is described in the Walker, Henderson, Degnan, Penela, & Fox (2014) study. The following behaviors were coded (in seconds) during each episode: latency to vocalize or the first sound that the child made, duration of proximity to mother, and latency to approach the stranger or touch the novel toy. The latency scores across episodes were standardized and averaged across three episodes to create the BI composite at each age (ns = 224 and 197; Range = −1.04–1.89 and −1.14–1.71, Ms = .00 and −.01, SDs = .50 and .59, for BI composites at 2 and 3 years of age, respectively). BI scores across the two assessments were then standardized and averaged to create a composite of BI across 2 and 3-years for all participants with data at either time point (n = 248; Range = −.96–1.25, M = −.01, SD = .46). The intra-class correlations (ICCs), computed for 20% of cases, ranged from .84 to .89 at the time of 2-year assessment and ranged from .97 to .99 at the 3-year assessment. Higher composite scores reflected higher levels of observed BI.
Attention bias towards threat
Children’s magnitude of bias towards threat was assessed using a dot-probe task at the 5-year assessment (see White et al., 2015). Attention bias to threat was not assessed at an earlier age in this sample given that children below the age of 5 typically show greater difficulties performing the task with reasonable accuracy (Perez-Edgar et al., 2011). Children were presented with a fixation cross that appeared in the middle of a computer’s screen for 1000ms followed by a pair of face photographs that stayed on the screen for 500ms. Pictures included 32 angry-neutral and 32 happy-neutral face pair with 16 neutral-neutral face pairs used as filler trials. The facial expression stimuli were taken from the NimStim face stimulus set (Tottenham et al., 2009). Following each face pair, a probe (i.e., an asterisk) appeared in the place of either the emotional (i.e., angry, happy) or the neutral face and remained on the screen for 2500ms. The only instruction that was given to children was to indicate the location of the probe by pressing a button. Faster reaction time for congruent trials, in which probe replaced the angry/positive facial expressions, than incongruent trials indicated attention bias towards threat/positive. Only children’s bias towards threat-related stimuli was used in further analyses. All of the analyses were carried out with positive attention bias as the moderator; however, no significant result was found involving positive attention bias.
The procedures that were employed for cleaning and processing reaction time (RT) and accuracy to remove anticipatory and aberrant responses were consistent with those used in previous studies (Perez-Edgar et al., 2011; White et al., 2015). Specifically, reaction times quicker than 200ms were excluded and RTs were then averaged across each trial condition (e.g., congruent angry, incongruent angry). Next, RTs that were larger or smaller than 2SDs of average RT (within each condition) were removed. Finally, children with accuracy rate less than 65% were identified as having poor task performance, and thus, were excluded (n = 26). The data related to accuracy scores for the remaining participants was normally distributed. The threat bias scores were then tested for outliers and two children were identified as having extreme bias scores (the Z-scores were ± 2.5 SD of the mean of bias score), and thus, were excluded from analyses (Tabachnik & Fidell, 2013). Positive scores indicated a bias towards threat, whereas negative scores indicated a bias away from threat. Bias scores that were zero (or near zero) reflected no bias. The descriptive statistics regarding final variables are reported in the bottom of Table 1.
Table 1.
Descriptive statistics for psychopathology measures and the dot-probe task
| N | Min - Max | M | SD | %N above borderline clinical cutoff | |
|---|---|---|---|---|---|
| CBCL | |||||
| Internalizing Problems | 182 | 33–90 | 50.93 | 10.08 | 23.63% |
| Externalizing Problems | 182 | 33–75 | 48.60 | 9.81 | 14.29% |
| Attention Problems | 182 | 50–93 | 55.01 | 7.69 | 15.38% |
| SCARED | |||||
| Anxiety (parent-report) | 147 | 0–53 | 12.84 | 10.54 | 12.24% |
| Anxiety (child-report) | 156 | 2–62 | 20.59 | 11.85 | 26.92% |
| KSAD | |||||
| Any current Anxiety Disorder | 124 | 0–1 | .11 | .31 | 0.81% |
| Any current Mood Disorder | 124 | 0–1 | .01 | .09 | 10.48% |
| Any current Behavior Disorder | 124 | 0–1 | .01 | .09 | 0.81% |
| Any current ADHD | 141 | 0–1 | .12 | .33 | 12.77 |
| DP Task | |||||
| Accuracy Rate | 181 | 65–100 | 89.80 | 8.19 | |
| ABT | 174 | −286.6–262.1 | −9.44 | 106.21 | |
| Bias Score > 0 | 89 | (−286.6)–(−1.24) | −89.22 | 74.72 | |
| Bias Score < 0 | 85 | .56–262.1 | 74.10 | 59.82 | |
Notes. KSAD = Kiddie-Schedule for Affective Disorders and Schizophrenia for School-Age Children; SCARED = Screen for Child Anxiety Related Disorder Questionnaire; CBCL = Child Behavior Checklist Questionnaire; DP = Dot-Probe; ABT = Attention Bias to Threat. Bias scores greater than zero reflects attention bias towards threat and bias scores less than zero reflects a bias to attend away from the threat. Only participants who had accuracy rate greater than 65% were included in the analysis.
Internalizing and Externalizing Behavior Problems
At 10 years of age, mothers reported on their children’s internalizing problems (i.e., anxious/depressed, withdrawn/depressed, somatic complaints), externalizing behavior problems (i.e., rule-breaking and aggressive behaviors), and attention problems using the Child Behavior Checklist (CBCL/6–18; Achenbach & Rescorla, 2001). All items were rated on a three-point scale (0 = not true to 2 = very true). For each participant, the raw scores on items related to externalizing and internalizing behavior problems and attention problems were summed and then were converted to T-scores based on the child’s age. In addition, using a 3-point Likert scale (0 = not true or hardly ever true to 2 = very true or often true), both mothers and children rated items of the Screen for Child Anxiety Related Disorder (SCARED; Birmaher et al., 1999). Lastly, using a semi-structured interview (Kiddie-Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime Version; K-SADS-PL; Kaufman et al. 1997), parents and children reported about children’s current mood, anxiety, behavior, and attention deficit hyperactivity disorders (ADHD). Specifically, the clinician judged the accuracy of each informant as the interview unfolded and then brought the parent and child together to dissolve discrepancies (Kappa = 1.0). The interviews were administered by an experienced clinician during the home-visit.
Attrition
Out of 291 participants that were recruited at the first data collection point for the original longitudinal study at 4 months, 224, 197, 207 and 189 children had data at 2, 3, 5, and 10 years of age, respectively. Missing data was mostly due to difficulty in scheduling participants and/or obtaining questionnaires. One child was excluded from the 5-year attention bias assessment due to poor motor ability/movement. Patterns of missing data did not violate the assumption that data were missing completely at random as indicated by Little’s MCAR test, χ2 (70) = 75.54, p = .30 (Little & Rubin, 1987). Children who attrited across 2 to 10 years of age were not different from those who stayed in the study in terms of 4-month temperament group, χ2 (2) = 1.973, p = .38, or gender, χ2 (1) = .03, p = .49. Children who were lost due to attrition from 2 to 10 years of age also were not different from those who participated at both time points on the BI measures at 2-year assessment, t(222) = .71, p = .52.
Data Analytic Strategy
The analyses involved BI across 2- and 3-years, which was used as the predictor, and 5-year assessment of attention biases towards threat as the moderator. With regards to the 10-year outcomes, Latent Class Analysis (LCA) was employed to create comprehensive psychopathology profiles or classes incorporating multiple measures collected from multiple informants (See Frenkel et al., 2015 for using a similar approach in quantifying mental health and psychopathology data). LCA seeks to identify membership in latent (i.e., unobserved) groups/classes comprised of individuals characterized by a specific profile with regard to a given set of observed variables. There are several advantages in using LCA over traditional algorithm-based clustering techniques (e.g., K-means clustering, cluster analysis using distance methods) including the use of a probabilistic statistical model to determine classes that reduces the uncertainty in class classification (Kent, Jensen, & Kongsted, 2014; Muthén, 2001; Vermunt, & Magidson, 2002). In particular, this probabilistic model-based approach allows for the use of appropriate fit statistics (maxim likelihood statistics) to assess the fit of model, and thus, reduces the uncertainty of classification (Vermunt, & Magidson, 2002).
The LCA included all participants with data on any of the psychopathology measures. Missing data patterns across measures in the LCA did not violate the assumption that they were missing completely at random as indicated by Little’s MCAR test, χ2 (15) = 21.31, p = .13 (Little & Rubin, 1987). Thus, data were analyzed in Mplus V.5 (Muthén & Muthén, 1998–2011) using all available data points. Full Information Maximum likelihood (FIML) estimation within a structural equation modeling (SEM) framework was used in order to calculate model parameters most likely to account for observed results. Assessment of best model fit was based on the interpretability of each model and 2 fit indices: Bayesian Information Criteria (BIC) and the Parametric Bootstrap Likelihood Ratio Test (BLRT; McLachlan & Peel, 2000). This ratio test provides a p-value comparing the increase in model fit between the k−1 and k class models. Once the number of classes was determined, based on Bayes’ theorem, continuous posterior probabilities of membership in the resulting psychopathology classes were computed for each participant.
The first step of analyses involved testing correlations among study variables, age and accuracy scores on task. The accuracy score on the task was used to be consistent with the White et al. (2015) study and because it indicated child’s performance on the task. Sex differences in terms of study variables were also examined. Next, three path models (separate models with the probability of being in each class as an outcome) were estimated using Mplus 7.31 (Muthen & Muthen, 1998–2015) and the FIML estimation. The fit of each path model was tested using the following fit indices: Chi-square test (non-significant values indicate good fit; Kline, 2010), Comparative Fit index (CFI; values greater than .95 indicate good fit; Kline, 2010), and Root Mean Square Error of Approximation (RMSEA; values less than .05 indicate good fit; Hu & Bentler, 1999). Lastly, significant interaction(s) were probed using procedures set forth by Aiken and West (1991) such that the models were re-estimated at +1/−1 SD below and above the mean of the attention bias variable representing attention bias towards and away from threat, respectively.
Results
Psychopathology Classes
The LCA included a total of 9 measures: 4 dummy-coded categorical measures indicating the presence or absence of any current Anxiety, Mood, Behavioral, and\or ADHD diagnoses based on the K-SADS semi-structured (K-SADS-PL; Kaufman et al. 1997), 3 continuous measures of CBCL Internalizing, Externalizing, and Attention-Related Problems (Achenbach, & Rescorla, 2001), and two continuous measures of anxiety, parent-report and child-report on SCARED; Birmaher et al., (1999). See Table 1 for descriptive statistics and N’s of all psychopathology measures. The LCA included 189 participants who provided psychopathology data on any of the measures. Two participants receiving a diagnosis of an Autism Spectrum Disorder in the community were excluded from analyses, after the clinical interview confirmed features of the diagnosis.
We estimated models with 1 to 5 classes. Interpretability was very low for the 5-class model and highest for the 4-class model, BLRT indicated that the 4-class model was significantly better than the 3-class model (p <0.0001). The BIC was 6497.13 for one class, 6368.12 for two classes, 6286.76 for three classes, 6255.03 for four classes and 6251.14 for five classes. Given the highest interpretability and all fit indices, the 4-class model was chosen as the best-fitting model. The best loglikelihood values were replicated in the final 4-class model following the recommendations provided by Asparouhov and Muthen (2012). In addition, the entropy for the final 4-class model was higher than .80 and the average latent class probabilities ranged from .83 to 1.000, suggesting that there was high accuracy in assigning individuals to classes and discrimination among classes (Clark & Muthen, 2010; Nagin, 2005). The final 4-class model yielded one healthy class (n = 112), one psychopathology class related primarily to anxiety (n = 48), and one psychopathology class related primarily to attention problems with comorbid secondary anxiety (n = 23). The fourth class was constituted of just 6 participants whom had extreme severe attention-related problems and ADHD diagnosis. The extreme severe ADHD class was preserved in both the 3-class and 4-class solutions, and was comprised of the same 6 participants across solutions. In addition to this extreme class, the three-class solution yielded one healthy class and one class of children with either anxiety and/or attention related problems. Thus, the difference between the three-class and four-class solutions was that the four class solution allowed for the more nuanced differentiation between children that appear to have primary anxiety without comorbid ADHD, versus children that display anxiety which was secondary and comorbid to primary ADHD.
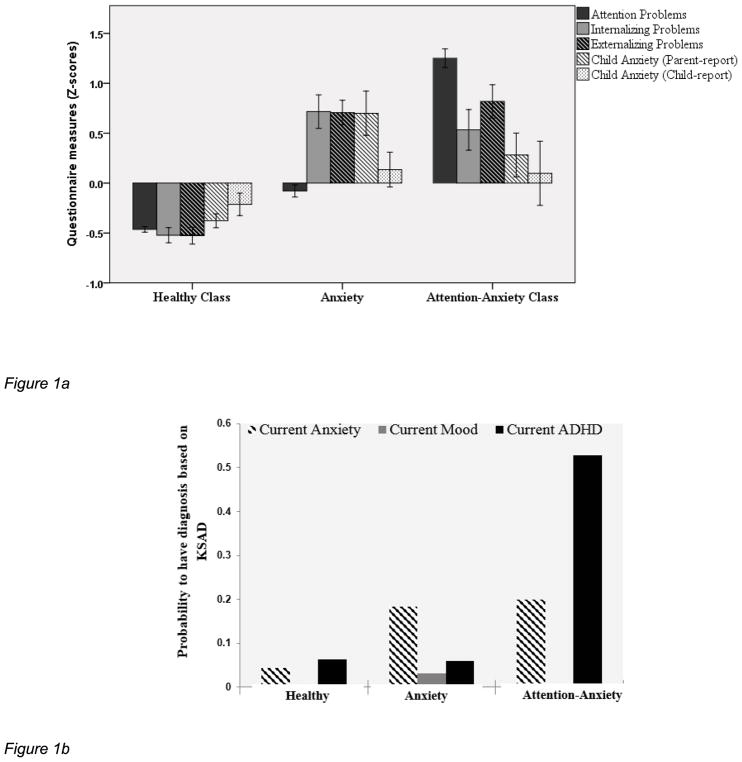
Participants’ continuous probability scores of class membership were calculated for each of the classes. Though taken to represent a valid extreme class of severe ADHD within the general population, we were cautious in employing membership in this class as an outcome variable in subsequent analyses due to the small class-size. Thus, participants’ continuous probability scores of class membership in the three main classes were used as the mental health outcome variables in all subsequent analyses. These probabilities were used as the mental health outcome variables in all subsequent analyses. For the sake of parsimony, these are referred to as the “Healthy”, “Anxiety” and “Attention-Anxiety” classes (n = 189, ranges = 0–1; Healthy class: M = .58; SD = .43; Anxiety class: M = .26, SD = .36; Attention-Anxiety class: M = .13, SD = .32). See Figure 1a and 1b for a depiction of the questionnaire measures and clinical interview psychiatric diagnosis by psychopathology classes, respectively.
Figure 1.
Figure 1a: Scores on questionnaire measures by psychopathology class
Figure 1b: Probability to have clinical diagnosis on Semi-structured clinical interview (KSADS) by psychopathology class
Preliminary Analyses
The correlations among study variables were computed. With the exception of correlations between psychopathology classes and children’s accuracy scores, no other significant correlations were found. Specifically, children’s high accuracy rate on the attention bias task was related to high probability of being in the anxiety class and low probability of being in the attention-anxiety class, rs(146, 146) = .18 and −.19 (ps < .05), respectively. In addition, the probabilities of being in psychopathology classes were negatively related to each other. BI and attention biases were not related to probability of being in psychopathology classes. Children’s age at the time of 10-year assessment also was not related to any of the variables of interest. Furthermore, sex differences were not found in terms of threat bias scores, BI, and membership in different classes. Based on the correlation analyses, children’s accuracy scores on the task (but not age and gender) were used as covariates in all subsequent analyses. Although direct relations between BI and probability of membership in the psychopathology classes were not present, we proceeded to test for relations between BI and psychopathology classes across varying levels of attention biases because the relation between two variables may change when moderator variables are included in the model (VanderWeele & Knol, 2014).
Relations of BI, Attention Bias and Psychopathology Outcomes
To examine the main and moderating roles of early BI and 5-year attention bias in relations to probability of being in each psychopathology class (i.e., anxiety, healthy, and attention-anxiety classes), three separate path models were estimated. In each model, the probability of being in each class was regressed onto the composite measure of BI, 5-year attention bias towards threat, and the interaction of BI by attention bias. Furthermore, to be consistent with previous study and because children’s accuracy scores were related to probabilities of being in anxiety and attention-anxiety classes, accuracy was used as covariate in all of analyses. BI and attention bias measures were mean-centered prior to analyses. All three models converged with no error and the resulting models fit the data well: X2s (1, 1, and 1) = .18, .16, and .16, ps = .67, .69, and .69 (for models with anxiety, healthy, and attention-anxiety classes, respectively), and CFIs = 1.00 and RMSEAs = .00 (for all three models). Results of the three models are presented in Table 2.
Table 2.
Models with BI, attention bias towards threat and probability of membership in anxious healthy, and attention/anxiety classes.
| Outcomes | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Anxious Class (R2 = .04) | Healthy Class (R2 = .04) | Attention-Anxiety Class (R2 = .04) | ||||
|
| ||||||
| Variables | B | SE B | B | SE B | B | SE B |
| BI | 0.05 | .06 | −.03 | .07 | .00 | .05 |
| 5-year attention bias towards threat | −.02 | .02 | .04 | .03 | −.02 | .02 |
| BI x 5-year attention bias | .12* | .05 | −.13* | .06 | −.01 | .04 |
| Accuracy scores | .01* | .00 | .00 | .00 | −.01* | .00 |
Notes.
p < .05,
p < .01.
Participants with poor performance scores (<65% accuracy rate) were excluded from analyses.
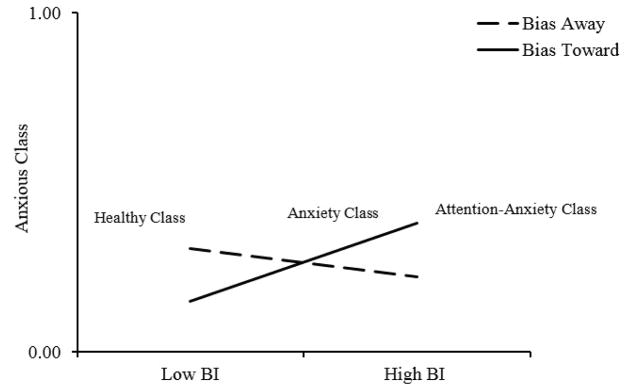
Children’s BI and threat attention bias towards threat were not directly related to any of the psychopathology classes. However, consistent with patterns for correlations, children’s low accuracy on the dot-probe task was related to low probability of being in the anxiety class and high probability of being in the attention-anxiety class. In addition, the interaction between BI and attention bias to membership in anxiety and healthy classes were significant. The two significant interactions were probed according to guidelines developed by Aiken and West (1991). The results showed that BI was positively related to probability of being in the anxiety class, only when children had a bias towards threat, b = .19, p = .03, but not when they had no bias or a bias away from the threat, b = −.10, p = .25 (see Figure 2). For the model with healthy class membership, BI was negatively related to membership in the healthy class when children had a bias towards the threat (b = −.19, p = .07), albeit marginally. BI was not related to membership in healthy class when children had no bias or a bias away from the threat, b = −.10, p = .26.
Figure 2.
Moderating role of attention bias towards threat in the longitudinal relation between early BI and membership in anxiety class at age 10.
Discussion
The current study extends previous work by White et al. (2015) using the same sample to identify children who had primary anxiety (not comorbid with other types of psychopathology) during preadolescence -- a developmental stage characterized by elevated rate of anxiety symptoms. In addition, the moderating role of attention bias towards threat in the longitudinal associations between toddlerhood BI and anxiety was examined. The results of LCA analysis using children’s clinical symptoms during preadolescence revealed four distinct groups of children characterized by having: primarily anxiety symptoms (anxiety group), symptoms of inattention comorbid with anxiety symptoms (attention-anxiety group), no clinical symptoms (healthy group), extreme and severe symptoms of inattention. Further analyses showed that children who displayed high levels of BI across toddler years were more likely to be in the group that was characterized by primary anxiety and less likely to be in the healthy group at age 10, particularly when they displayed attention bias towards threat.
These results expand the findings of previous studies that have found similar concurrent interaction effects among younger children (White et al., 2015, Perez-Edgar et al., 2011), by showing that attention bias towards threat may exacerbate long-term influences of early childhood BI on anxiety symptoms, particularly during transition to adolescence. It should be noted that in a previous study using the same data, 5-year attention bias towards threat did not moderate the associations between early BI and 7-year anxiety (White et al., 2015). Thus, attention biases may moderate the association between temperament and anxiety only when anxiety manifests at later stages in life (Beesdo et al., 2009; Giedd et al., 2009).
BI and attention bias to threat were not directly related to the membership in the class of children whom primarily displayed attention problems along with some comorbid anxiety. Further, the relations between BI and inclusion in this class were not dependent on whether children had attention bias away or towards threat-related information. It is possible that some of the symptoms related to attention problems may influence children’s performance on tasks that involve brief exposure of cues and stimuli such as the dot-probe task (O’Leary-Barrett et al., 2015). Indeed, in the current study, we found that children with high probability of membership in the attention class had poor performance on the dot-probe task. Other researchers also have reported increased variability in responses to cognitive tasks that require attention and executive functioning among children with symptoms of inattention (e.g., Castellanos et al., 2005; Schreiber, Possin, Girard, & Rey-Casserly, 2014). Thus, children with attention issues may perform more poorly on the dot-probe attention task, and thus, produce more noisy data that obscures associations with anxiety. Given the dearth of research directly examining the associations between BI and anxiety with and without comorbid symptomology, the association between these two and potentially differential mechanisms may be considered in future research. In addition, further research using experimental or quasi-experimental designs would be useful 1) to parse out differences between children with anxiety problems and those with attention-anxiety problems in terms of attention biases towards threat; and 2) to test the validity of dot-probe task across these two different groups.
Conversely, high probability of being in the anxiety class during pre-adolescence years was associated with children’s good performance, indicated by high accuracy rate, on the dot-probe task at 5 years of age. The research evidence on the associations between anxiety and cognitive control is complex. Whereas some researchers have reported cognitive control impairments among individuals with anxiety, others have found high levels of cognitive control in anxious individuals (Derakhshan & Eysneck, 2009; Eysneck, Derakhshan, Santos, & Calvo, 2007 for a review). Discrepancies among studies have been attributed to various factors, including whether the task requires use of stimulus-driven or goal-directed attentional system (top-down versus bottom-up information processing; Eysneck et al., 2007). For example, the results of several studies have shown that anxious individuals may show high levels of cognitive control and good performance for tasks (e.g., dot-probe task) that mostly influence stimulus-driven attentional system (e.g., McDermott et al., 2009; Moser, Moran, Schroder, Donnellan, & Yeung, 2013). Our results were consistent with this line of research showing that high levels of cognitive control and error monitoring, may increase children’s risk for developing anxiety disorder.
Although BI and attention bias towards threat have been identified as early risk markers for the emergence and development of anxiety (Chronis-Tuscano et al., 2009; Clauss & Blackford, 2012), we did not find direct associations between BI and attention biases to membership in anxiety or healthy classes. These results suggest that BI or attention biases towards threat by themselves may not affect anxiety but indeed the presence of both vulnerability factors may be responsible for the development of anxiety (Van Bockstaele et al., 2014). Alternatively, it is likely that the link between BI and anxiety may occur only among a subgroup of inhibited children or anxious children (Degnan & Fox, 2007). Specifically, previous research has shown that only a sub-group of inhibited children who continue to be socially reticent across childhood may be at-risk for developing anxiety problems (Chronis-Tuscano et al., 2009; Degnan et al., 2014; Degnan & Fox, 2007). In addition, the focus of most previous studies, in which the direct relation between BI and anxiety was reported, has been on children with social anxiety disorder (e.g., Chronis-Tuscano et al., 2009). Lastly, the direct relation between BI and anxiety that has been reported in previous studies, including the work conducted by White et al. (2015), may be due to the common-method variance. For example, the BI composite that was used in the White et al. (2015) study included mother reports of children’s BI to test the relation between BI and maternal reports of children’s anxiety symptoms. However, in the current study, the relation between observational measure of BI and anxiety symptoms, measured using multiple methods (e.g., maternal and children’s reports of anxiety), was tested.
An important strength of the current study was the use of the LCA and incorporating multiple assessment methods of both clinical and subclinical levels of functioning across various dimensions to create comprehensive psychopathology profiles. This approach limits the number of statistical tests, which correspondingly balances Type I and Type II errors (Spencer, 2011). Furthermore, this approach is aligned with current conceptualizations of psychopathology and consistent with the approach of psychiatric epidemiologists (Achenbach, 2006; Horton et al., 1999). Given that the assessment of psychopathology is often prone to (measurement) error, having multiple informants and methods as well as appropriate analytical approaches (i.e., LCA, cluster analysis) is useful in reliably assessing psychopathology and identifying possible comorbidity among various types (see Horton et al., 1999 for a review).
Utilization of aforementioned approaches was particularly important in the context of the current sample as two pathology classes emerged: one class included children who appeared to have anxiety symptoms which were secondary to attention problems, whereas the other class included children who displayed primary symptoms of anxiety without secondary comorbidity. The results of this study underscore the specificity of the link between BI and primary symptoms of anxiety. The findings suggest that the developmental pathway leading from BI to anxiety is specific to primary anxiety and not to anxiety that is secondary to comorbid symptomology. Anxiety that is secondary to comorbid symptomology appears to develop in a pathway that is unrelated to BI. Given the paucity of research directly examining the associations between BI and anxiety with and without comorbid symptomology, the association between these two and potential differential mechanisms may be considered in future research.
It is additionally noteworthy that there appear to be discrepancies between maternal and child report of anxiety in the present sample such that children did not report anxiety symptoms across all three classes (see Figure 1a). Informant discrepancies in the assessment of child psychopathology often exist and pose a serious challenge in the assessment of child mental health (See De Los Reyes & Kazdin, 2005 for a critical review). Previous studies with age groups similar to the present sample reveal only mild to moderate correlations between child and maternal reports of child anxiety (Burbosa, Tannock and Manassis, 2002; Manassiss, Tannock and Monga, 2009) and indicate that children often under-report their symptoms (Manassis, Mendlowitz & Menna, 1997). Nevertheless, current thinking on best practices in mental health assessment, assume that the value in multi-informant assessments lies in capturing the unique perspectives held by each informant (Hunsley, & Mash, 2007). In line with this view, class inclusion in the present study was based on measures of both child and maternal report. The employment of LCA allowed for the integration between parent and child report without biasing the report of either informant. Future research may benefit from the identification of informant characteristics that may influence discrepancies in the assessment of child psychopathology in general, and in the context of temperamental vulnerabilities in particular.
Although the early assessment of attention bias was an important strength of the study, the use of dot-probe tasks and reaction time to measure 5-year old’s attention biases may be considered a limitation of the study. Previous research has shown that the use of reaction time in the assessment of attention biases (used in tasks such as dot-probe, visual search) among young children may not to be appropriate due to children’s limited motor and cognitive abilities during early childhood (Brown et al., 2014). An alternative methodology would be the use of technologies such as eye-tracking, which has shown to be promising in measuring attention biases (Armstrong & Olatunji, 2012). Thus, future research that integrates traditional measures (e.g., dot-probe) along with eye-tracking to assess children’s attentional biases in testing relations among temperament, attention biases and anxiety is warranted. In addition, it should be noted that the proportion of variance that was explained by interaction effect, although significant, was small in the current study. Hence, future research examining such associations and potential moderating role of attentional biases must be conducted using large sample sizes to determine the significance of relations of BI and attention bias towards threat to development of anxiety symptoms. Further, in the current study we tested for the moderating role of positive biases in the link between BI and anxiety. However, given that no significant main or moderation effects were found, the results were not included in the current study. Given that previous studies (e.g., White et al. 2015) have found that positive biases play a role in the link between BI and anxiety problems, including positive biases in future research is highly encouraged.
Despite this limitation, the current study is among the few that have focused on examining attention biases during middle childhood as the moderator of BI related risk for anxiety during early adolescence years. There is some evidence to show that attention training programs are successful in reducing anxiety among at-risk children and adolescents (see Lowther & Newman, 2014 for a review; De Voogd, Wiers, Prins, & Salemink, 2014; Eldar et al., 2012). For example, Eldar et al. (2012) found that children, aged between 8 to 14 years old, had significant reduction in their severity and number of anxiety symptoms following the attention bias modification training. Thus, findings of the current study may have important implications for these attention training programs by informing them about who, when and under what conditions may be at risk for developing anxiety.
References
- Asparouhov T, Muthen B. Using Mplus TECH11 and TECH14 to test the number of latent classes. Mplus Web Notes: No.14. 2012 Retrieved from http://www.statmodel.com/examples/webnotes/webnote14.pdf.
- Achenbach TM. As other see us: Clinical and research implications of cross-informant correlations for psychopathology. Current Directions in Psychological Science. 2006;15:94–98. http://dx.doi.org/10.1111/j.0963-7214.2006.00414.x [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Adam D. Mental health: On the spectrum. Nature. 2013;496:416–418. doi: 10.1038/496416a. http://dx.doi.org/10.1038/496416a [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park: Sage; 1991. [Google Scholar]
- Armstrong T, Olatunji BO. Eye tracking of attention in the affective disorders: A meta-analytic review and synthesis. Clinical Psychology Review. 2012;32:704–723. doi: 10.1016/j.cpr.2012.09.004. http://dx.doi.org/10.1016/j.cpr.2012.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballespi S, Jane MC, Riba MD. Parent and teacher ratings of temperamental disposition to social anxiety: The BIS 3–6. Journal of Personality Assessment. 2012;94:164–164. doi: 10.1080/00223891.2011.645929. http://dx.doi.org/10.1080/00223891.2011.645929 [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg M, van IJzendoorn M. Threat-related attentional bias in anxious and non-anxious individuals: a meta-analytic study. Psychological Bulletin. 2007;133:1–24. doi: 10.1037/0033-2909.133.1.1. http://dx.doi.org/10.1037/0033-2909.133.1.1 [DOI] [PubMed] [Google Scholar]
- Beesdo K, Knappe S, Pine DS. Anxiety and Anxiety Disorders in Children and Adolescents: Developmental Issues and Implications for DSM-V. Psychiatric Clinics of North America. 2009;32:483–524. doi: 10.1016/j.psc.2009.06.002. http://dx.doi.org/10.1016/j.psc.2009.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. Journal of American Academy of Child and Adolescent Psychology. 1999;38:1230–1306. doi: 10.1097/00004583-199910000-00011. http://dx.doi.org/10.1097/00004583-199910000-00011 [DOI] [PubMed] [Google Scholar]
- Biederman J, Hirshfeld-Becker DR, Rosenbaum JF, Herot C, Friedman D, Snidman N, … Faraone SV. Further evidence of association between behavioral inhibition and social anxiety in children. American Journal of Psychiatry. 2001;158:1673–1679. doi: 10.1176/appi.ajp.158.10.1673. http://dx.doi.org/10.1176/appi.ajp.158.10.1673 [DOI] [PubMed] [Google Scholar]
- Brown HM, Eley TC, Broeren S, MacLeod C, Rinck M, Hadwin JA, Lester KJ. Psychometric properties of reaction time based experimental paradigms measuring anxiety-related information-processing biases in children. Journal of Anxiety Disorder. 2014;28:97–107. doi: 10.1016/j.janxdis.2013.11.004. http://dx.doi.org/10.1016/j.janxdis.2013.11.004 [DOI] [PubMed] [Google Scholar]
- Burbosa J, Tannock R, Manassis K. Measuring anxiety: Parent-child reporting differences in clinical samples. Depression and Anxiety. 2002;15:61–65. doi: 10.1002/da.10022. http://dx.doi.org/10.1002/da.10022 [DOI] [PubMed] [Google Scholar]
- Castenallo FX, Sonuga-Barke EJS, Scheres A, Martino AD, Hyde C, Walters JR. Varieties of Attention-Deficit/Hyperactivity disorder-related intra-individual variability. Biological Psychiatry. 2005;57:1416–1423. doi: 10.1016/j.biopsych.2004.12.005. http://dx.doi.org/10.1016/j.biopsych.2004.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Degnan KA, Pine DS, Pérez-Edgar K, Henderson HA, Diaz Y, … Fox NA. Stable early maternal report of behavioral inhibition predicts lifetime social anxiety disorder in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:928–35. doi: 10.1097/CHI.0b013e3181ae09df. http://dx.doi.org/10.1097/CHI.0b013e3181ae09df [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark S, Muthén B. Relating latent class analysis results to variables not included in the analysis. 2009 Retrieved from: https://www.statmodel.com/download/relatinglca.pdf.
- Clauss JA, Blackford JU. Behavioral inhibition and risk for developing social anxiety disorder: A meta-analytic study. Journal of American Academy of Child and Adolescent. 2012;51:1066–1075. doi: 10.1016/j.jaac.2012.08.002. http://dx.doi.org/10.1016/j.jaac.2012.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuthbert B, Insel T. The data of diagnosis: New approaches to psychiatric classification. Psychiatry. 2010;73:311–314. doi: 10.1521/psyc.2010.73.4.311. http://dx.doi.org/10.1521/psyc.2010.73.4.311 [DOI] [PubMed] [Google Scholar]
- Degnan KA, Almas A, Fox NA. Temperament and the Environment in the Etiology of Childhood Anxiety. Journal of Child Psychology and Psychiatry. 2010;51:497–517. doi: 10.1111/j.1469-7610.2010.02228.x. http://dx.doi.org/10.1111/j.1469-7610.2010.02228.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degnan KA, Almas AN, Henderson H, Hane A, Walker OL, Fox NA. Longitudinal trajectories of social reticence with unfamiliar peers across early childhood. Development and Psychology. 2014;150:2311–2323. doi: 10.1037/a0037751. http://dx.doi.org/10.1037/a0037751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degnan KA, Fox NA. Behavioral Inhibition and anxiety disorders. Development and Psychopathology. 2007;19:729–746. doi: 10.1017/S0954579407000363. http://dx.doi.org/10.1017/S0954579407000363 [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulliten. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. http://dx.doi.org/10.1037/0033-2909.131.4.483 [DOI] [PubMed] [Google Scholar]
- De Voogd EL, Wiers RW, Prins PJ, Salemink E. Visual search attentional bias modification reduced social phobia in adolescents. Journal of Behavior Therapy and Experimental Psychiatry. 2014;45:252–259. doi: 10.1016/j.jbtep.2013.11.006. http://dx.doi.org/10.1016/j.jbtep.2013.11.006 [DOI] [PubMed] [Google Scholar]
- Derakhshan N, Eysenck MW. Anxiety, processing efficiency, and cognitive performance: New developments from attentional control theory. European Psychologist. 2009;14:168–176. http://dx.doi.org/10.1027/1016-9040.14.2.168 [Google Scholar]
- Eldar S, Apter A, Lotan D, Perez-Edgar K, Naim R, Fox NA, Pine DS, Bar-Haim Y. Attention bias modification treatment for pediatric anxiety disorders: a randomized control trial. American Journal of Psychiatry. 2012;169:213–230. doi: 10.1176/appi.ajp.2011.11060886. http://dx.doi.org/10.1176/appi.ajp.2011.11060886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenck MW, Derakhshan N, Santos R, Calvo MG. Anxiety and cognitive performance: Attentional Control Theory. Emotion. 2007;7:336–353. doi: 10.1037/1528-3542.7.2.336. http://dx.doi.org/10.1037/1528-3542.7.2.336 [DOI] [PubMed] [Google Scholar]
- Fox NA, Henderson HA, Marshall PJ, Nichols KE, Ghera MM. Behavioral inhibition: linking biology and behavior within a developmental framework. Annual Review of Psychology. 2005;56:235–262. doi: 10.1146/annurev.psych.55.090902.141532. http://dx.doi.org/10.1146/annurev.psych.55.090902.141532 [DOI] [PubMed] [Google Scholar]
- Fox NA, Pine DS. Temperament and the emergence of anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51:125–128. doi: 10.1016/j.jaac.2011.10.006. http://dx.doi.org/10.1016/j.jaac.2011.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenkel TI, Fox NA, Pine DS, Walker OL, Degnan KA, Chronis-Tuscano A. Early childhood behavioral inhibition, adult psychopathology and the buffering effects of adolescent social networks: A twenty-year prospective study. Journal of Child Psychology and Psychiatry. 2015;56:1065–1073. doi: 10.1111/jcpp.12390. http://dx.doi.org/10.1111/jcpp.12390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of American Academy of Child and Adolescent. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. http://dx.doi.org/10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- Kent P, Jensen R, Kongsted A. A comparison of three clustering methods for finding subgroups in MRI, SMS, or clinical data: SPSS Two step Cluster analysis, Latent Gold and SNOB. BMC Medical Research Methodology. 2014;14:113. doi: 10.1186/1471-2288-14-113. http://dx.doi.org/10.1186/1471-2288-14-113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principals and practice of structural equation modeling. 3. New York: Guilford Press; 2010. [Google Scholar]
- Giedd JN, Keshavan M, Paus T. Why do many psychiatric disorder emerge during adolescence? Nature Reviews Neuroscience. 2009;9:947–957. doi: 10.1038/nrn2513. http://dx.doi.org/10.1038/nrn2513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gladstone GL, Parker GB, Mitchell PB, Wilhelm KA, Malhi GS. Relationship between self-reported childhood behavioral inhibition and lifetime anxiety disorders in a clinical sample. Depression and Anxiety. 2005;22:103–113. doi: 10.1002/da.20082. http://dx.doi.org/10.1002/da.20082 [DOI] [PubMed] [Google Scholar]
- Hane AA, Fox NA, Henderson HA, Marshall PJ. Behavioral reactivity and approach-withdrawal bias in infancy. Developmental Psychology. 2008;44:1491–1496. doi: 10.1037/a0012855. http://dx.doi.org/10.1037/a0012855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haller SPW, Kadosh KC, Scerif G, Lau JYF. Social anxiety disorder in adolescence: How developmental cognitive neuroscience findings may shape understanding and interventions for psychopathology. Developmental Cognitive Neuroscience. 2015;13:11–20. doi: 10.1016/j.dcn.2015.02.002. http://dx.doi.org/10.1016/j.dcn.2015.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horton NJ, Laird NM, Zahner GEP. Use of multiple informant data as a predictor in psychiatric epidemiology. International Journal of Methods in Psychiatric Research. 1999;8:6–18. http://dx.doi.org/10.1002/mpr.52 [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. http://dx.doi.org/10.1080/10705519909540118 [Google Scholar]
- Hunsley J, Mash EJ. Evidence-based assessment. Annual Review of Clinical Psychology. 2007;3:29–51. doi: 10.1146/annurev.clinpsy.3.022806.091419. http://dx.doi.org/10.1146/annurev.clinpsy.3.022806.091419 [DOI] [PubMed] [Google Scholar]
- Lamm C, Walker OL, Degnan KA, Henderson HA, Pine DS, McDermott JM, Fox NA. Cognitive control moderates early childhood temperament in predicting social behavior in 7-year-old children: an ERP study. Developmental Science. 2014;17:667–681. doi: 10.1111/desc.12158. http://dx.doi.org/10.1111/desc.12158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis-Morraty E, Degnan KA, Chronis-Tuscano A, Rubin KH, Chea CSL, Pine DS. Maternal over-control moderates the associations between early childhood behavioral inhibition and adolescent social anxiety. Journal Abnormal Child Psychology. 2012;40:1363–1373. doi: 10.1007/s10802-012-9663-2. http://dx.doi.org/10.1007/s10802-012-9663-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJ, Rubin DB. Statistical analysis with missing data. New York: Wiley; 1987. [Google Scholar]
- Lonigan CJ, Vasey MW, Philips BM, Hazen RA. Temperament, anxiety, and the processing of threat-relevant stimuli. Journal of Clinical Child and Adolescent Psychology. 2004;33:8–20. doi: 10.1207/S15374424JCCP3301_2. http://dx.doi.org/10.1207/S15374424JCCP3301_2 [DOI] [PubMed] [Google Scholar]
- Lonigan CJ, Vasey MW. Negative affectivity, effortful control, and attention to threat-relevant stimuli. Journal of Abnormal Child Psychology. 2008;37:387–399. doi: 10.1007/s10802-008-9284-y. http://dx.doi.org/10.1007/s10802-008-9284-y [DOI] [PubMed] [Google Scholar]
- Lowther H, Newman E. Attention bias modification (ABM) as a treatment for child and adolescent anxiety: A systematic Review. Journal of Affective Disorder. 2014;168:125–135. doi: 10.1016/j.jad.2014.06.051. http://dx.doi.org/10.1016/j.jad.2014.06.051 [DOI] [PubMed] [Google Scholar]
- Manassis K, Mendlowitz S, Menna R. Child and parent reports of childhood anxiety: differences in coping styles. Depression and Anxiety. 1997;6:62–69. http://dx.doi.org/10.1146/annurev.clinpsy.3.022806.091419 [PubMed] [Google Scholar]
- Manassis K, Tannock R, Monga S. Anxious by maternal – versus self-report: Are they the same children? Journal of the Canadian Acadamy of Child and Adolescence Psychiatry. 2009;18:103–109. http://dx.doi.org/10.1037/t03542-000 [PMC free article] [PubMed] [Google Scholar]
- McKay D, Storch E, editors. Handbook of anxiety disorders in children and adolescents. Boston, MA: Springer-Verlag; 2011. [Google Scholar]
- McDermot JM, Perez-Edgar K, Henderson HA, Chronis-Tuscano A, Pine DS, Fox NAA. History of childhood behavioral inhibition and enhanced response monitoring in adolescence are linked to clinical anxiety. Biological Psychiatry. 2009;65:445–448. doi: 10.1016/j.biopsych.2008.10.043. http://dx.doi.org/10.1016/j.biopsych.2008.10.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLachlan G, Peel D. Finite mixture models. New York: Wiley; 2000. http://dx.doi.org/10.1002/0471721182 [Google Scholar]
- Moser JS, Moran TP, Schroder HS, Donnellan MB, Yeung N. The case for compensatory processes in the relationship between anxiety and error monitoring: A reply to Proudfit, Inzlicht, & Mennin. Frontiers in Human Neuroscience. 2014;8:64. doi: 10.3389/fnhum.2014.00064. http://dx.doi.org/10.3389/fnhum.2013.00466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B. Latent variable mixture modeling. In: Marcoulides GA, Schumacker RE, editors. New Developments and Techniques in Structural Equation Modeling. Mawah, NJ: Lawrence Erlbaum Associates; 2001. pp. 1–33. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2011. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2015. [Google Scholar]
- Nagin DS. Group-based modeling of development. Cambridge, MA: Harvard University Press; 2005. http://dx.doi.org/10.4159/9780674041318 [Google Scholar]
- O’Leary-Barrett M, Pihl RO, Artiges E, Banaschewski T, Bokdge ALW, Büchel C … IMAGEN Consortium. Personality, Attentional Biases towards Emotional Faces and Symptoms of Mental Disorders in an Adolescent Sample. PLoS One. 2015;10:e0128271. doi: 10.1371/journal.pone.0128271. http://dx.doi.org/10.1371/journal.pone.0128271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Edgar K, Reeb-Sutherland BC, McDermott JM, White LK, Henderson HA, Degnan KA, … Fox NA. Attention biases to threat link behavioral inhibition to social withdrawal over time in very young children. Journal of Abnormal Child Psychology. 2011;39:885–95. doi: 10.1007/s10802-011-9495-5. http://dx.doi.org/10.1007/s10802-011-9495-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin K, Coplan RJ, Bowker JC. Social withdrawal in childhood. Annual Review of Psychology. 2009;60:141–171. doi: 10.1146/annurev.psych.60.110707.163642. http://dx.doi.org/10.1146/annurev.psych.60.110707.163642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salum GA, Mogg K, Bradley BP, Gadelha A, Pan P, Tananaha AC, … Pine DS. Threat bias in attention orienting: evidence of specificity in a large community-based study. Psychological Medicine. 2013;43:733–745. doi: 10.1017/S0033291712001651. http://dx.doi.org/10.1017/S0033291712001651 [DOI] [PubMed] [Google Scholar]
- Schreiber JE, Possin KL, Girard JM, Rey-Casserly C. Executive function in children with attention deficit/hyperactivity disorder: The NIH Examiner battery. Journal of International Neuropsychological Society. 2014;20:41–51. doi: 10.1017/S1355617713001100. http://dx.doi.org/10.1017/S1355617713001100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer BD. When Do Latent Class Models Overstate Accuracy for Diagnostic and Other Classifiers in the Absence of a Gold Standard? Biometrics. 2011;68:559–566. doi: 10.1111/j.1541-0420.2011.01694.x. [DOI] [PubMed] [Google Scholar]
- Svihra M, Katzman MA. Behavioral inhibition: A predictor of anxiety. Pediatric Child Health. 2004;9:547–550. doi: 10.1093/pch/9.8.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szpunar M, Young AR. Information processing biases in behaviorally inhibited children: Responses to threat and novelty. Child Health and Education. 2013;4:47–63. [Google Scholar]
- Tabachnik BG, Fidell LS. Using multivariate statistics. 6. Boston: Pearson; 2013. [Google Scholar]
- Tottenham N, Tanaka JW, Leon AC, McCarry T, Nurse M, Hare TA, … Nelson C. The NimStim set of facial expressions: Judgments from untrained research participants. Psychiatry Research. 2009;168:242–9. doi: 10.1016/j.psychres.2008.05.006. http://dx.doi.org/10.1016/j.psychres.2008.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadlinger HA, Isaacowitz DM. Fixing our focus: Training attention to regulate emotion. Personality and Social Psychology Review. 2011;15:75–102. doi: 10.1177/1088868310365565. http://dx.doi.org/10.1177/1088868310365565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker OL, Henderson HA, Degnan KA, Penela EC, Fox NA. Associations between behavioral inhibition and children’s social problem-solving behavior during social exclusion. Social Development. 2014;23:487–501. doi: 10.1111/sode.12053. http://dx.doi.org/10.1111/sode.12053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White LK, Henderson HA, Pérez-Edgar K, Walker OL, Degnan KA, Shechner T, … Fox NA. Developmental relations between behavioral inhibition, anxiety, and attention biases to threat and positive information. Child Development. 2015;80:49–69. doi: 10.1111/cdev.12696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White LK, McDermott JM, Degnan KA, Henderson HA, Fox NA. Behavioral inhibition and anxiety: The moderating roles of inhibitory control and attention shifting. Journal of Abnormal Child Psychology. 2011;39:735–747. doi: 10.1007/s10802-011-9490-x. http://dx.doi.org/10.1007/s10802-011-9490-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Bockstaele B, Verschuere B, Tibboel H, De Houwer J, Crombez G, Koster EHW. A review of current evidence for the causal impact of attentional bias on fear and anxiety. Psychological Bulliten. 2014;140:682–721. doi: 10.1037/a0034834. http://dx.doi.org/10.1037/a0034834 [DOI] [PubMed] [Google Scholar]
- VanderWeele TJ, Knol MJ. A tutorial on interaction. Epidemiologic Methods. 2014;3:33–72. http://dx.doi.org/10.1515/em-2013-0005 [Google Scholar]
- Vermunt JK, Magidson J. Latent class cluster analysis. In: Hagenaars J, McCutcheon A, editors. Applied latent class analysis. Cambridge: Cambridge University Press; 2002. pp. 89–106.http://dx.doi.org/10.1017/CBO9780511499531.004 [Google Scholar]