Abstract
Latina breast cancer patients in the USA report significantly worse cancer-related symptom burden and health-related quality of life than non-Hispanic whites. However, health literacy (e.g. knowledge about cancer, coping skills and communication) has been found to improve quality of life. In this paper, we present a case study of the methodology used to design Mi Guía (My Guide), a mobile application that aims to improve symptom burden and health-related quality of life among Hispanic women who have completed active treatment for breast cancer by increasing their health literacy. We developed a community-supported approach to building the application, which involved: (1) eliciting feedback from community leaders such as support group organizers and facilitators who are bilingual in Spanish and English, prioritize patients’ preferences and best interests and have a unique knowledge of the women and their needs;(2) conducting a formal evaluation of design principles based on previous interaction design research and user responses;(3) incorporating feedback from potential future users. In this paper, we discuss our methodology, and the challenges and benefits of this approach. We believe that future studies that aim to develop mobile technologies for underserved populations may benefit from a community-supported approach to design.
Keywords: eHealth, mHealth, mobile app, community design, breast cancer, Hispanic
Introduction
Latinas experience lower breast cancer survival rates and later stages of breast cancer diagnosis compared to non-Hispanic whites (American Cancer Society 2014). Latinas also report significantly worse cancer-related symptom burden and health-related quality of life (HRQOL) than non-Hispanic whites during treatment and survivorship (Yanez, Thompson, and Stanton 2011; Luckett et al. 2011; Fu et al. 2009; Molina et al. 2013). Barriers to accessing and effectively engaging in health care, limited cancer information and beliefs about cancer are some factors that may contribute to these disparities (Kagawa-Singer et al. 2010; American Cancer Society 2014; Yanez, Thompson, and Stanton 2011). In addition, Latina women diagnosed with cancer may have difficulty gaining access to supportive and psychosocial services that can assist with symptom burden and HRQOL and face obstacles such as cost, lack of insurance coverage and time constraints (Byers et al. 2008; Kagawa-Singer et al. 2010). Despite this, very few randomized controlled trials have specifically targeted HRQOL among Hispanic women who have recently completed treatment for breast cancer. This is potentially a critical period to provide skills and tools to assist with the transition to survivorship (Fu et al. 2009).
The wide adoption of smartphone use among Hispanics in the USA provides a unique opportunity to implement psychosocial interventions that, through increasing health literacy, allow Hispanics to overcome some access to care barriers as well as time and logistical constraints of these populations (Lopez, Gonzalez-Barrera, and Patten 2013). Previous research has shown that delivering cancer-related knowledge, stress management, coping skills and communication, in a culturally appropriate intervention, can improve outcomes in the post-treatment survivorship phase (Penedo et al. 2007; Yanez, Thompson, and Stanton 2011; Yanez, Stanton, and Maly 2012). However, designing a mobile application for this population requires several important considerations. First, the content has to be provided in the appropriate language of the target population (Spanish and English) and despite the complexity of the material, the content has to be easy to browse and using a language that is clear and easy to follow. Second, although the design of most mobile application is developed based on the feedback of the users, the design process with Hispanic participants may be challenging. It is possible that Latinas may exhibit poor communication skills due to language barriers, and previous research suggests that they may have a bias towards responding affirmatively and in the least contentious way possible (Benson et al. 2016). Therefore, when designing a mobile solution, it may be appropriate to take into account feedback from stakeholders that live in their communities and whom patients trust.
The purpose of this paper is to describe the community-supported design approach we utilized to develop Mi Guía (My Guide), a mobile application that aims to improve symptom burden and HRQOL among Hispanic women completing active treatment for breast cancer through increasing health literacy. This community-supported approach involves: (1) obtaining ideas and feedback from community leaders such as support group organizers and facilitators, patients and medical professionals; (2) using students of human-computer interaction to evaluate the extent to which the application conforms to design principles based on previous interaction design research; (3) validating our design with actual Latina breast cancer survivors. The design of My Guide strives to ensure an application that supports interaction design principles, while being culturally appropriate and helpful for Latina breast cancer survivors.
Designing mHealth applications for Hispanic patients
Computer-based health applications (eHealth) include a wide range of solutions, from standalone systems, web interfaces and mobile applications. This latter subset of applications is called mHealth. Mobile devices provide an ideal method for improving access to health information for low-income or rural families (Martin 2012). In addition, mobile devices are widespread among diverse populations within the USA, including Hispanics, which make them ideal tools for health care (2012).
Over the past decade, there has been a proliferation of mHealth applications that deliver evidence-based treatments for health management (Eysenbach and CONSORT-EHEALTH Group 2011; Leykin et al. 2012; Yanez et al. 2015). There is a need for patient support systems in mobile phones, particularly for cancer patients (Mirkovic, Kaufman, and Ruland 2014; Pandey et al. 2013). Given the ubiquity of mobile devices, researchers have suggested that delivering interventions via mobile applications has several benefits, such as cost saving and increasing in health literacy (Almarri and Bhatti 2015). mHealth platforms may be particularly relevant for Hispanic patients. In comparison to non-Hispanic whites, 11% more Hispanics look up health-related information using their mobile devices. Furthermore, 4% more women than men use their mobile devices to look up medical information (Fox and Duggan 2012).
Community-supported design
Since mHealth applications are growing in popularity, usability is becoming a significant concern when designing a mobile app, particularly when designing an mHealth application (Zapata et al. 2015). Mohr et al. (2014) approach the design phase of eHealth and mHealth applications paying special attention to the content (‘what’), the purpose (‘why’) and the interactions (‘how’), but allow the immediate stakeholders to provide feedback for the design. However, in the development of computer-based applications, user-centred design is fundamental (Norman and Draper 1986). Involving users throughout the entire design process ensures a more usable system once deployed. User-centred design has been adopted by many mHealth and eHealth development processes (Jibb et al. 2014; Cafazzo et al. 2012; McCurdie et al. 2012). Thus, during the design phase of eHealth applications, designers obtain feedback from a target population (e.g. Atkinson et al. 2009) or directly from patient focus groups (e.g. Steele Gray et al. 2014). Then, they validate their applications by testing them with the target population. Some use mixed methods that involve interviewing some other stakeholders, like medical staff, in their capacity as users of the application (Gilbertson-White et al. 2016) or as a secondary source of information for the initial design phase (Van Velsen, Wentzel, and Van Gemert-Pijnen 2013). Finally, many developers base the content of their applications on previous literature and other secondary sources and conduct iterative user testing to improve their initial interface design (Fu et al. 2016).
De Vito Dabbs et al. (2009) discuss three user-centred design principles used to develop an mHealth tracking application: (1) Focus on the User and Tasks; (2) Measure Usability Empirically; (3) Design and Test Usability Iteratively. In the last phase of their research, a field study was conducted to determine if patients had an issue using the system independently. They were able to determine which features were used more often than other features and whether or not the application successfully prompted patients to report the study’s main outcomes to their doctor.
Co-Design is another approach that has been adopted for health care applications. This process is analogous to participatory design (Kensing and Blomberg 1998), where end-users, as well as other stakeholders, are not only testers of technology, but participate actively in the design process, blurring the lines between designers and users (Sanders and Stappers 2008; Reay et al. 2017). Users now express themselves and participate directly and proactively in the design process (Frascara 2002). However, a participatory design approach implicitly assumes that the design propositions of every party are easy to interpret.
When designing applications for Hispanic patients, one must consider a few unique characteristics of these users. First, limited English proficiency can be an important obstacle for patients’ understanding of physicians’ instructions or reading materials about their condition (Wilson et al. 2005). In addition, Bender et al. (2001) warn about the importance of designing research instruments that reflect the perceptions of the research subjects rather than simply those of the investigators. For example, research shows that minority patients are less expressive and assertive with their doctors (Schouten and Meeuwesen 2006) and that this behaviour may stem from social desirability beliefs.
In particular, Hispanics exhibit these social desirability biases talking to clinicians or responding surveys (Hopwood et al. 2009). This extends to interactions with researchers as well. Hispanics exhibit a bias to ‘yea-saying’ (answering questions in the affirmative) greater than the general US population (Aday, Chiu, and Andersen 1980; Benson et al. 2016). Hispanic women may have trouble with survey questionnaires, commonly used to assess user experience. In an effort to be courteous, they may opt for the least contentious responses (Saint-Germain, Bassford, and Montano 1993). This phenomenon is also prevalent in interviews.
To overcome some of the limitations of designing for this population, our methodology merged aspects of participatory design and user-centred design, and added a strong community emphasis to create a community-supported approach to design, whereby community leaders play a vital role in the design process. These leaders are part of the user’s community and are trusted by the users. For these leaders, language is not a barrier and they know the unbiased patient’s opinions. In addition, it is important that they have the patient’s best interest at heart, but have no motivation to exhibit social desirability on their behalf.
In our community-supported approach, we carried out iterative usability tests with fewer participants, but the iterations also involved interviews with community leaders who have gained the confidence of the participants. We asked them to give feedback from two perspectives: the participants’ and their own. The first perspective supplemented the feedback from the participants, and the second one provided valuable feedback on content and organization, as they are capable of prioritizing the content the participants need to know and care about.
The following section details our approach to design, which emphasized community and user input throughout the process.
Community-supported design process
The design of Mi Guía strived to ensure an application that respects interaction design principles, is culturally appropriate, and useful for Latina cancer survivors in terms of improving HRQOL. Accomplishing these overarching goals involved a process that iteratively refined a mock-up prototype, developed using NinjaMock (https://ninjamock.com/), by (1) obtaining ideas and feedback from community leaders such as support group organizers and facilitators as well as medical professionals; (2) performing heuristic evaluations of design principles based on previous interaction design research; (3) obtaining feedback, suggestions and validations of the prototype’s interactions with actual Latina breast cancer survivors within our target group.
It is important to note that the interactions with these stakeholders were not sequential, but the result of an iterative process that involved multiple sessions with the three groups of stakeholders.
Community-supported team: medical professionals and community leaders
Community leaders that support breast cancer patients and survivors have a unique knowledge of issues that affect breast cancer survivors. Throughout the design of Mi Guía, we consulted with two community leaders from not-for-profit organizations that provide support for breast cancer patients/survivors in our geographic area. One community leader was the programme manager for Latino community-based initiatives of a large urban cancer support centre, and the other was the founder of a smaller organization specially focused on breast cancer support for Latina patients. Both community leaders were bilingual Hispanics and one was a breast cancer survivor. Both leaders conduct support groups in their respective organizations. In addition, we included feedback of an oncologist and a patient navigator from a large medical school in Chicago. The roles of these community leaders and medical professionals put them in a unique position of intimate knowledge of the patient’s beliefs. We also included feedback from medical social scientists from two high research universities in Chicago. We held several meetings with all these medical professionals and community leaders where we brainstormed and discussed feedback from users. In addition, we held separate meetings with community leaders as well as meetings with medical social scientists throughout the design of My Guide. The feedback from these community leaders and cancer professionals was not only specific to design issues, but also covered content and delivery so that the application would resonate with the patients. These community leaders were able to articulate criticism and suggestions to a larger degree than the actual patients who participated in the design process.
Results from medical professionals’ and community leaders’ feedback
We started our design with our main section about breast cancer (‘Breast Cancer Education’). However, after our meetings with community leaders, medical social scientists and patient navigators, and understanding the difficulties that our target population experiences in searching information (Bickmore et al. 2016), we designed sections where patients could look up information of interest quickly. Specifically, participants were able to search for: (1) symptoms they may be experiencing by tapping in the affected area of the body (‘My Symptoms’); (2) information related to medications; (3) a list of resources such as support groups. In addition, the prototype contained an interactive section (Journal), where users could record their symptoms on a daily basis (see Figure 1). The application also had an icon to contact the experimenters.
Figure 1.
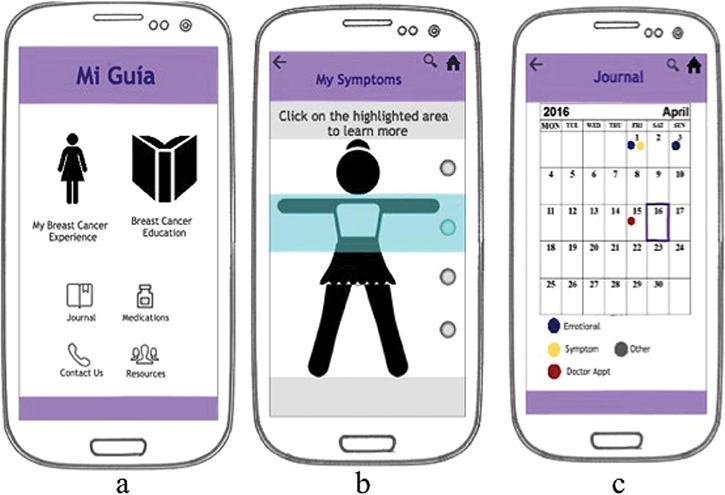
One of the early iteration of the Mi Guía prototype presented to community leaders and medical professionals. (a) The main screen, (b) the ‘My Symptoms’ subsection of ‘My Breast Cancer Experience’, (c) The Journal.
Based on feedback from our community leaders, several modifications were adopted:
(1) Our initial ‘My Symptoms’ section allowed tapping in any part of the body. However, our community leaders felt that patients may not feel comfortable clicking on private body parts when wanting to learn more about symptoms such as vaginal dryness or hardness of the skin in the chest. Moreover, community leaders expressed concern that end users may be uncomfortable clicking on the name of the body part. Therefore, our final version of the body included in the ‘My Symptoms’ section involved radio buttons on the side that users can tap to select a general region of the body. Tapping on these buttons navigates to a list of potential symptoms in and around the selected area. Furthermore, we learned that the patients may not be comfortable looking at those areas in pictures and therefore the body we designed was always fully clothed. An abstract body was suggested at first (see Figure 1(b)); however, a more realistic looking woman was suggested in future iterations (see Figure 2(a)).
(2) Our community leaders felt that the body of the more realistic looking woman used in the symptom checker was not representative of the norm in our target population. Community leaders recommended that the body be more normative (more athletic, older and less even breasts) as a figure that is not normative of our users may be intimidating and non-identifying for our target population (see Figure 2(b)).
(3) Our community leaders suggested that we include the technical medical terminology followed by the word that the patients use to refer to it in parentheses. For example, our participants rarely used the name of one of the common breast cancer medications (Tamoxifen). Instead, they simply referred to it as ‘the pill’. Another example is chemotherapy. Although there is a precise Spanish translation, patients often just refer to this as ‘chemo’. Thus, we included these more colloquial terms in parentheses.
(4) Other feedback referred to wording and slight reorganization of content. The ‘My Breast Cancer Experience’ section was sub-divided into three sections: (1) Symptoms related to emotional stability (‘My Emotions’); (2) Symptoms related to corporal discomfort (‘My Symptoms’) and (3) Symptoms related to relationships (‘My Family & Friends’). Lastly, an interactive component was added: A ‘Myth or Fact’ game to test the knowledge of the patients.
Figure 2.

Woman cartoon featured in ‘My Symptoms’ prototype. (a) Initial version; (b) version after feedback.
Heuristic evaluation of design principles
We evaluated numerous iterations of the application for adherence to design principles throughout the development of Mi Guía. In addition, before obtaining feedback from users, we conducted a more formal evaluation of Mi Guía based on widely accepted design principles. We trained 28 undergraduate students taking a human-computer interaction course at a Midwestern university to evaluate applications using the Nielsen’s 10-point usability heuristics (Nielsen 1994). Although the heuristics are geared towards computer-based applications, in practice, most of these are applicable to mobile application design. The heuristics include items such as: consistency, conventions, and the ability to prevent and recover from errors.
Students were divided into nine groups. Each group was assigned four questions they needed to answer, such as ‘What are the stages of breast cancer?’ or ‘Is cancer contagious?’ The questions covered all areas of the application (see Appendix). Each question was answered by all students as they interacted with the system.
Furthermore, we asked the students to monitor and record the number of clicks it took them to find the answer, specifying the paths they tried. We computed the average number of steps it took to accomplish each task in order to determine which questions were easier and harder to answer. We also looked at improvements between the first task and the last task performed by a single group by assessing the number of clicks.
Results from heuristic evaluation
The hardest task for students was finding causes of lymphedema, which took 7.1 clicks. The easiest task was to locate the patient’s next doctor’s appointment (1.5 clicks). Most other tasks took somewhere between 3–4 clicks, except ‘Myth or Fact’ - a section we had included to be a fun trivia-like quiz - which turned out to be unclear as to the information contained in it. As expected, however, by the fourth task, the students were able to find their destination much more quickly. Some of the most significant violations to design principles found were: (1) lack of help (two mentions), (2) the journal section violated several consistency practices (six mentions) and (3) the Myth or Fact section did not serve a clear purpose (four mentions). In addition, the breakdown and wording of the main icons of the application and its sections were mentioned. However, the average severity of issues in the Nielsen heuristics scale was 2.2, which correspond to minor usability problems (those that are not a priority to fix).
The application was modified significantly after the Heuristic Evaluation session. Some revisions based on their feedback included a help menu and moving all the sub-sections of ‘My Breast Cancer Experience’ (‘My Emotions’, ‘My Symptoms’ and ‘My Family & Friends’) to the main screen (Figure 3). This, together with feedback from other groups of stakeholders at later iterations also resulted in the ‘Myth or Fact’ section being removed from the resulting application as it was not a place where users went to seek information.
Figure 3.
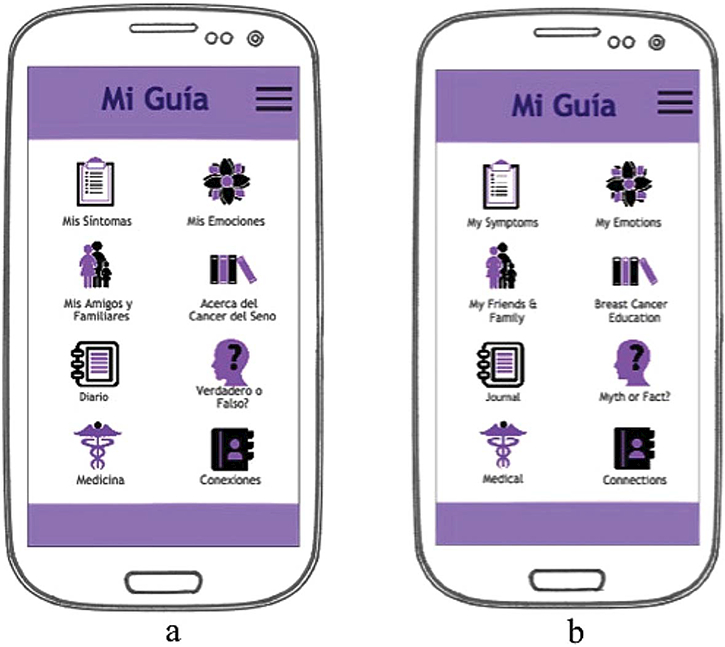
Prototype version shown in usability tests with Latina breast cancer survivors: (a) Spanish version; (b) English version.
Latina breast cancer survivors’ feedback
After conducting the evaluation of design principles, we iteratively evaluated our prototype with nine Latina breast cancer survivors. The survivors were recruited through a cancer centre. The main eligibility criteria were: (1) identify as a Latina adult female; (2) had a diagnosis of breast cancer (stages I–IIIA) and (3) have completed active treatment at least six months before the interview.
The usability test occurred in four stages. First, the researcher explained the basic organization of the application to the participants. Second, participants were presented with 4–6 scenarios taken from the heuristic evaluation common to breast cancer survivors (e.g. ‘My underarm is swollen, what could this be, and how can I manage it?’) that covered the utilization of all sections of our prototype application (see Appendix). Because thinking aloud is a method that provides cognitive insights and elicits feedback the user may not otherwise give (Jaspers 2009), participants were told to think aloud, voicing their decisions and deliberations, as they interacted with the application to find the answers to these questions. Meanwhile, the researchers recorded the steps that participants took to find the answers, noting errors, corrections and suggestions. These individual sessions were audio recorded. Third, after they completed the scenarios presented, researchers asked participants to fill out a modified System Usability Scale (Brooke 1996) questionnaire. The survey was augmented with measures of attributes specific to mobile applications as detailed in the People At the Centre of Mobile Application Development (PACMAD) (Harrison, Flood, and Duce 2013) evaluation model. In particular, the survey captures self-reports of: satisfaction, memorability (degree to which the content is easy to remember), error rate (the degree to which tasks are completed correctly or the degree to which it is easy to go back and correct the error), learnability (the degree to which the system is easy to learn), effectiveness (the degree to which users can complete the task in a given context), efficiency (the degree to which users are able to efficiently complete a task accurately) and cognitive load (how well can users complete tasks in different settings). The questionnaire contained 23 items. These statements were translated into Spanish and read to the participants. The participants had to assess the degree to which they agreed with each statement using a Likert scale: 1 – not at all, 5 – completely. We found the explanations and oral responses to be necessary due to lower literacy rates of some of our users. Because social desirability introduced a risk for bias, if the participants only reported positive impressions of the application, the researchers read a script that encouraged criticism as being more useful than praise, and also took notes of some of their answers that clearly contrasted the participant’s experience in the previous task. For example, we took note if they said that the application was easy to use, but we saw them struggle with certain sections. Lastly, the researchers and patients would have a conversation about design proposals, feedback and general experience while using the prototype.
Results from usability testing
Of the nine users, one of the participants had a college degree, one had some college, three had a high school degree, one had some high school and three had less than or up to eighth grade. Of the five participants who disclosed their age, the average age was 59.2 years (the minimum was 40 and maximum 77). All but one reported using a smartphone several times a day. In addition, we administered a questionnaire to assess their knowledge about breast cancer prior to interacting with the prototype. Eight participants responded to the questionnaire and, as expected, their health literacy about breast cancer was low, with an average score of 9.3 (SD = 2.4) out of 16 points (58%).
While interviewing the users, we realized that these users have their own stories and expressed a desire to exchange stories and share experiences. Therefore, we decided to add quotes from these interviews directly into our application with permission, as well as stories gathered from other breast cancer support websites.
Other design feedback from user testing include:
(1) Text sections and lists had too much content on it. While the material attempted to target a 6th grade reading level, the amount of content was a bit overwhelming for our participants. We therefore found that users were skimming the material without actually reading it. This leads to shorter lists with simpler, but still accurate language.
(2) Many users commented on the purple colour and asked why it was not pink given that pink is the colour for breast cancer awareness for the breast cancer colour. This resulted in changing the colour scheme of the application to a pink theme.
(3) Users had a lot of positive feedback about the app. The average response on the usability questionnaire was 4.23 out of a maximum of 5 (SD = 0.9). This average considers the reversed scores for some questions where higher scores denoted less favourable outcomes. Despite these high scores, we found surprising discrepancies. For example, although most women were in complete agreement with the statement: ‘I found the application easy to use’ (M = 4.25, SD = 0.9), we did not find a corresponding disagreement with statements like ‘I needed to learn a lot of things before I could get going with this system’ (M = 2, SD = 2.0) or ‘I think that I would need the support of a technical person to be able to use this system’ (M = 3.0, SD = 1.82) Based on this statement and our observations of patients’ interactions with the application, we simplified lists to provide a quicker search of content, as we detected that was a frequent impediment to using the application efficiently.
(4) Many breast cancer survivors thought it would be a good idea to have audio-visual material to help with reading difficulties (e.g. low literacy) and to enable women to listen to the application while walking, etc. Therefore, the research team audio-recorded all of the written content in the application and embedded ‘play’ buttons throughout the application so that participants could listen to the application content. In addition, the oncologist that participated in the design team recorded videos that were embedded in to the application content. These videos focused on topics of relevance to breast cancer survivors (e.g. managing breast cancer treatment side effects, transitioning from treatment to survivorship).
(5) We obtained significant feedback on the wording throughout the application. For example, one woman said that the word ‘operation’ should be used instead of ‘surgery’, another suggested that we stress that not every woman experiences the same - or any - of the side effects of hormonal therapy, and another suggested the application use a formal version of ‘you’ in Spanish (‘Usted’) consistently.
Resulting application
After several iterations with breast cancer survivors, community leaders, medical professionals and human-computer interaction professionals and students, we decided on the finalized look and feel of the application. In the end, it was determined that the application be developed as a web-based mobile application. This was in part driven by cost and to accommodate users with either Android or iOS devices more easily. In addition, section names were modified slightly to reflect actions. Time constraints, feedback from the heuristic evaluations and a final iteration with researchers and community leaders led to deleting the myth or fact section as well as the journal function and improving the section on community support. In addition, the wording and lists were simplified and subdivided into smaller lists. Lastly, every section with content was supplemented with a ‘Play’ button in order for the text to be read aloud. Furthermore, many sections now have videos to supplement the material (see Figure 4 for the webbased mobile application).
Figure 4.
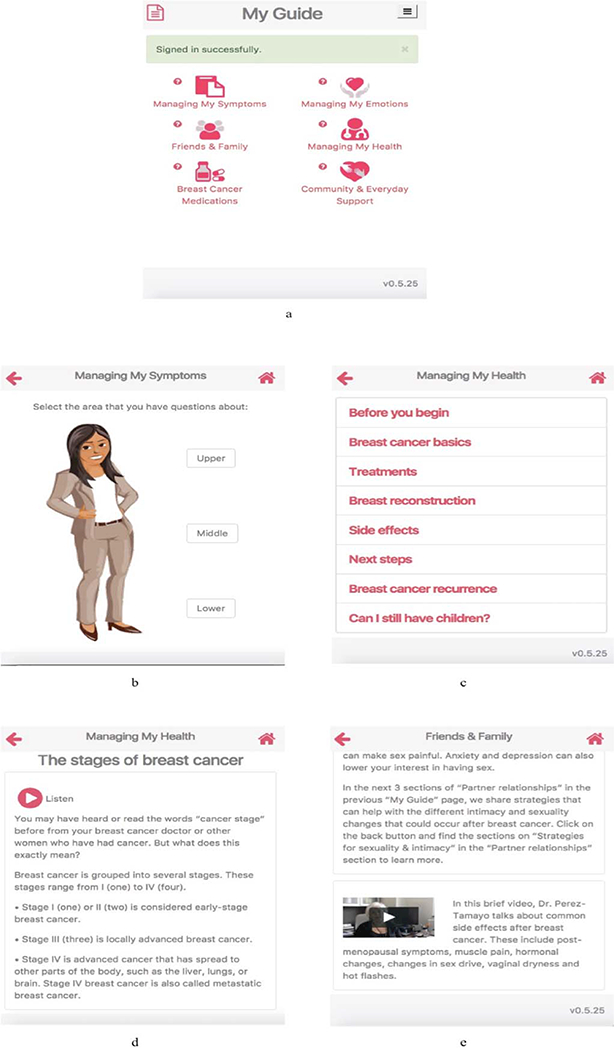
Features implemented in the final iteration of Mi Guía, web-based mobile application, based on the feedback of community leaders, researchers and medical professionals. (a) Main Screen of Mi Guia; (b) simpler interaction with a more relatable cartoon; (c) shorter and simpler lists; (d) all content supports audio and (e) some content has embedded video.
Discussion on community-supported design and feasibility
In order to design Mi Guía, an mHealth application for Hispanic breast cancer survivors, we use a community-supported design approach, where we relied on community leaders, such as doctors and support group leaders, for prototype feedback in addition to users. Our community-supported approach merged participatory design (Kensing and Blomberg 1998) and user-centred design (Norman and Draper 1986) and added a strong community emphasis, where community leaders play a crucial role in the design process.
Using feedback from community leaders, breast cancer survivors and a more formal heuristic evaluation, we were able to modify the content of Mi Guía to include appropriate language, colour and images, as well as stories, videos and audio. Furthermore, we reduced the amount of content in each section significantly.
Similar to Benson et al. (2016), we encountered anecdotal evidence of a response bias in our target population and participants tended to respond favourably. Therefore, we need to use caution when conducting user testing. For example, several users completely agreed with the statement ‘the application was easy to use’; however, at various points during some of the information finding tasks we noticed participants had difficulty completing them. In addition to careful observation during user testing, including community leaders who are able to be honest is a fundamental component in the design. For example, thanks to the contributions of community leaders, we were able to arrive at a satisfactory design of the cartoon figure in the ‘Managing My Symptoms’ section.
One of the main challenges of this approach is to reconcile feedback between stakeholders that may be contradictory. Researchers, community leaders, medical professionals and one patient (who is also a community leader) met several times as a large group to decide on contentious feedback. This approach can be expensive in terms of time, but we believe our community-supported approach resulted in an application that end users will benefit from.
Conclusion
In order to reduce disparities for Hispanic women with breast cancer who have limited cancer information, we designed Mi Guía (My Guide), a mobile webbased application that aims to improve symptom burden and HRQOL among Hispanic women with breast cancer. We use a community-supported design approach, where in addition to users, we obtained feedback from community leaders, such as support group organizers and facilitators as well as medical practitioners. This feedback helped us create an application which not only provides breast cancer information, but also provides an engaging way to interact with it, including audio, video and a symptom body checker. Finally, we believe this application is promising in great part due to the community-supported approach to its design.
Acknowledgments
Support for this project was provided by National Cancer Institute of the National Institutes of Health under Award Number NIH 1U54CA202995–01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. In addition, we would like to thank CBITs for their help developing the mobile application and tracking logs, and students Alexie Porres, Karla Salas, Karina Reyes and Namrata Shivapraksha.
Funding
National Cancer Institute of the National Institutes of Health [grant number NIH 1U54CA202995–01].
Notes on contributors
Francisco Iacobelli is an assistant professor in the Department of Computer Science at Northeastern Illinois University. His research interests are broadly at the intersection of artificial intelligence, information finding and education, in particular of disadvantaged populations. Dr Iacobelli received his PhD degree from Northwestern University.
Rachel F. Adler is an assistant professor in the Department of Computer Science at Northeastern Illinois University. She received her PhD degree in computer science from the Graduate Center of the City University of New York. Her research interests are in the areas of humancomputer interaction, multitasking and social media.
Diana Buitrago is a research coordinator in the Department of Medical Social Sciences at the Northwestern University Feinberg School of Medicine. Ms Buitrago collaborates in the design, implementation and analysis of projects related to behavioural medicine with an aim to understand health disparities. Ms Buitrago received a BA degree from Bradley University and expects to receive her MPH degree from Northwestern University in 2019.
Joanna Buscemi is an assistant professor in the Department of Psychology of DePaul University’s College of Science and Health. Until August 2016, she was a research scientist at the University of Illinois at Chicago. Her research aims to prevent chronic diseases linked to healthrisk behaviours via evidence-based behavioural interventions. Her recent work has focused on preventing cancer through community-based weight gain prevention interventions among minority children and families.
Marya Corden has ample experience managing research on behavioural medicine, as well as technology interventions for patients. She worked as a product manager at Northwestern University serving as lead liaison between technical and non-technical teams, by translating and facilitating communication. Marya obtained her MPH degree from John Hopkins University’s School of Public Health and her undergraduate from the University of Michigan.
Alejandra Perez-Tamayo is a board certified surgeon and Associate Professor of Clinical Surgery at the University of Illinois Hospital & Health Sciences System. Dr Perez-Tamayo’s interests include breast surgery as well as general surgery procedures: laparoscopy, open laparotomy, gastrointestinal/colorectal surgery and hernia repairs.
Frank J. Pinedo is the Director of Survivorship and of the Cancer Survivorship Institute of the Robert H. Lurie Comprehensive Cancer Center (LCC). He also serves as Program Leader of the Cancer Control and Survivorship Research Program at the LCC and directs the Biopsychosocial Mechanisms and Health Outcomes (BMHO) Program. He has over 160 publications, and his work has been recognized through several awards. He is current President of the International Society of Behavioral Medicine.
Melinda Rodriguez recently graduated with a BSc degree in computer science at Northeastern Illinois University. She works as a solutions analyst for Slalom Consulting. Melinda has 15 years of experience in management and customer care.
Betina Yanez is an assistant professor in the Department of Medical Social Sciences and a member of the Robert H. Lurie Comprehensive Cancer Center at the Northwestern University Feinberg School of Medicine. She received her PhD degree in Clinical Psychology from the University of California, Los Angeles. Dr Yanez’s focus is in the area of cancer control and survivorship. Her work bridges behavioural medicine, health equity and precision medicine to research improvements in the patient-centred and clinical outcomes of individuals diagnosed with cancer.
Appendix
Questions that participants had to answer using the prototype of the application:
(1) My underarms are swollen, why can that be? How do I prevent it?
(2) I am feeling sad sometimes, sometimes I cry, and sometimes I am cranky. Why is this?
(3) Tamoxifen is a common medication for breast cancer survivors. Do all patients experience the same side effects? What are they?
(4) When’s my next doctor’s appointment?
(5) What are the stages of breast cancer?
(6) Is cancer contagious?
(7) Besides this app where else can I get support?
(8) My chest is hard today. How can I record this information?
(9) Is it true that cancer is a death sentence?
(10) My chest is hard? Why is that?
(11) How long ago did you last feel depressed?
(12) What are the long term side effects of a mastectomy?
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Aday LA, Chiu GY, and Andersen R. 1980. “Methodological Issues in Health Care Surveys of the Spanish Heritage Population.” American Journal of Public Health 70 (4): 367–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almarri Ayesha, and Bhatti Tariq. 2015. “Consumers Attitude towards the Use of Mobile Health Apps: An Empirical Review.” In The Second International Conference on Electrical and Electronics Engineering, Clean Energy and Green Computing (EEECEGC2015), 56–63. Konya, Turkey: Society of Digital Information and Wireless Communication at Melvana Universitesi. [Google Scholar]
- American Cancer Society. 2014. “Cancer Facts & Figures for Hispanics/Latinos 2012–2014.” Accessed March 14 2018. http://www.cancer.org/acs/groups/content/@epidemiologysur veilance/documents/document/acspc-034778.pdf.
- Atkinson Nancy L., Saperstein Sandra L., Desmond Sharon M., Gold Robert S., Billing Amy S., and Tian Jing. 2009. “Rural eHealth Nutrition Education for Limited-Income Families: An Iterative and User-Centered Design Approach.” Journal of Medical Internet Research 11 (2): e21. doi:10.2196/jmir.1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender Deborah E., Harbour Catherine, Thorp John, and Morris Peter. 2001. “Tell Me What You Mean by ‘Sí’: Perceptions of Quality of Prenatal Care Among Immigrant Latina Women.” Qualitative Health Research 11 (6): 780–794. doi:10.1177/104973230101100607. [DOI] [PubMed] [Google Scholar]
- Benson Jemma, Garrison Emma, Dropkin Jonathan, and Jenkins Paul L.. 2016. “Methodological Concerns Related to Response Bias in Migrant and Seasonal Farmworkers.” American Journal of Industrial Medicine 59 (12): 1112–1119. doi:10.1002/ajim.22646. [DOI] [PubMed] [Google Scholar]
- Bickmore Timothy W., Utami Dina, Matsuyama Robin, and Paasche-Orlow Michael K.. 2016. “Improving Access to Online Health Information with Conversational Agents: A Randomized Controlled Experiment.” Journal of Medical Internet Research 18 (1): e1. doi:10.2196/jmir.5239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooke John. 1996. “SUS – a Quick and Dirty Usability Scale.” Usability Evaluation in Industry 189 (194): 4–7. doi:10.1002/hbm.20701. [Google Scholar]
- Byers TE, Wolf HJ, Bauer KR, Bolick-Aldrich S, Chen VW, Finch JL, Fulton JP, et al. 2008. “The Impact of Socioeconomic Status on Survival after Cancer in the United States : Findings from the National Program of Cancer Registries Patterns of Care Study.” Cancer 113 (3): 582–591. doi:10.1002/cncr.23567. [DOI] [PubMed] [Google Scholar]
- Cafazzo Joseph A., Casselman Mark, Hamming Nathaniel, Katzman Debra K., and Palmert Mark R.. 2012. “Design of an mHealth App for the Self-Management of Adolescent Type 1 Diabetes: A Pilot Study.” Journal of Medical Internet Research 14 (3) e70: doi:10.2196/jmir.2058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Vito Dabbs Annette, Myers Brad A., Mc Curry Kenneth R., Dunbar-Jacob Jacqueline, Hawkins Robert P., Begey Alex, and Dew Mary Amanda. 2009. “User-Centered Design and Interactive Health Technologies for Patients.” Computers, Informatics, Nursing : CIN 27 (3): 175–183. doi:10.1097/NCN.0b013e31819f7c7c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach Gunther, and CONSORT-EHEALTH Group. 2011. “CONSORT-EHEALTH: Improving and Standardizing Evaluation Reports of Web-Based and Mobile Health Interventions.” Journal of Medical Internet Research 13 (4): e126. doi:10.2196/jmir.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox Susannah, and Duggan Maeve. 2012. Mobile Health 2012. Washington, DC: Pew Internet. [Google Scholar]
- Frascara Jorge. 2002. “Summary for Policymakers.” In Climate Change 2013 - The Physical Science Basis, edited by Intergovernmental Panel on Climate Change, 1–30. Cambridge: Cambridge University Press; https://doi.org/10.1017/CBO9781107415324.004. [Google Scholar]
- Fu Mei R., Axelrod Deborah, Guth Amber A., Rampertaap Kavita, El-Shammaa Nardin, Hiotis Karen, Scagliola Joan, Yu Gary, and Wang Yao. 2016. “mHealth Self-Care Interventions: Managing Symptoms Following Breast Cancer Treatment.” mHealth 2 (July). 28–28. doi:10.21037/mhealth.2016.07.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu Olivia S., Crew Katherine D., Jacobson Judith S., Greenlee Heather, Yu Gary, Campbell Julie, Ortiz Yvette, and Hershman Dawn L.. 2009. “Ethnicity and Persistent Symptom Burden in Breast Cancer Survivors.” Journal of Cancer Survivorship : Research and Practice 3 (4): 241 – 250. doi:10.1007/s11764-009-0100-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbertson-White Stephanie, Yeung Chi, Mercer Keri Nace, Bartoczszyk Dorota, and Papke Todd. 2016. “Developing an eHealth Intervention for Cancer Symptom Management for Rural Residents.” Journal of Clinical Oncology 34 (26_suppl): 207 https://doi.org/10.1200/ jco.2016.34.26_suppl.207. [Google Scholar]
- Harrison Rachel, Flood Derek, and Duce David. 2013. “Usability of Mobile Applications: Literature Review and Rationale for a New Usability Model.” Journal of Interaction Science 1 (1): 1–16. doi:10.1186/2194-0827-1-1. [Google Scholar]
- Hopwood Christopher J., Flato Claudia G., Ambwani Suman, Garland Beth H., and Morey Leslie C.. 2009. “A Comparison of Latino and Anglo Socially Desirable Responding.” Journal of Clinical Psychology 65 (7): 769–780. doi:10.1002/jclp.20584. [DOI] [PubMed] [Google Scholar]
- Jaspers Monique W. M. 2009. “A Comparison of Usability Methods for Testing Interactive Health Technologies: Methodological Aspects and Empirical Evidence.” International Journal of Medical Informatics 78 (5): 340–353. doi:10.1016/j.ijmedinf.2008.10.002. [DOI] [PubMed] [Google Scholar]
- Jibb Lindsay A., Stevens Bonnie J., Nathan Paul C., Seto Emily, Cafazzo Joseph A., and Stinson Jennifer N.. 2014. “A Smartphone-Based Pain Management App for Adolescents with Cancer: Establishing System Requirements and a Pain Care Algorithm Based on Literature Review, Interviews, and Consensus.” JMIR Research Protocols 3 (1): e15 https://doi.org/10.2196/resprot.3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kagawa-Singer M, Dadia A. Valdez, Yu MC, and Surbone A. 2010. “Cancer, Culture, and Health Disparities: Time to Chart a New Course?” CA: A Cancer Journal for Clinicians 60 (1): 12–39. doi:10.3322/caac.20051. [DOI] [PubMed] [Google Scholar]
- Kensing Finn, and Blomberg Jeanette. 1998. “Participatory Design: Issues and Concerns.” Computer Supported Cooperative Work (CSCW) 7 (3–4): 167–185. doi:10.1023/A:1008689307411. [Google Scholar]
- Leykin Yan, Thekdi Seema M., Shumay Dianne M., Muñoz Ricardo F., Michelle Riba, and Dunn Laura B.. 2012. “Internet Interventions for Improving Psychological Well-Being in Psycho Oncology: Review and Recommendations.” Psycho-Oncology 21 (9): 1016–1025. https://doi. org/10.1002/pon.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez Mark Hugo, Gonzalez-Barrera Ana, and Patten Eileen. 2013. “Closing the Digital Divide: Latinos and Technology Adoption.” Pew Hispanic Center. Accessed December 12 2017. http://www.pewhispanic.org/2013/03/07/closing-the-digital-divide-latinos-and-technology-adoption/. [Google Scholar]
- Luckett Tim, Goldstein David, Butow Phyllis N., Gebski Val, Aldridge Lynley J., McGrane Joshua, Ng Weng, and King Madeleine T.. 2011. “Psychological Morbidity and Quality of Life of Ethnic Minority Patients with Cancer: A Systematic Review and Meta-Analysis.” The Lancet Oncology 12 (13): 1240–1248. doi:10.1016/S1470-2045(11)70212-1. [DOI] [PubMed] [Google Scholar]
- Martin Thomas. 2012. “Assessing mHealth: Opportunities and Barriers to Patient Engagement.” Journal of Health Care for the Poor and Underserved 23 (3): 935–941. doi:10.1353/hpu.2012.0087. [DOI] [PubMed] [Google Scholar]
- McCurdie Tara, Taneva Svetlena, Casselman Mark, Yeung Melanie, McDaniel Cassie, Ho Wayne, and Cafazzo Joseph. 2012. “mHealth Consumer Apps: The Case for User-Centered Design.” Biomedical Instrumentation & Technology/Association for the Advancement of Medical Instrumentation 46 (Suppl): 49–56. doi:10.2345/0899-8205-46.s2.49. [DOI] [PubMed] [Google Scholar]
- Mirkovic Jelena, Kaufman David R., and Ruland Cornelia M.. 2014. “Supporting Cancer Patients in Illness Management: Usability Evaluation of a Mobile App.” Journal of Medical Internet Research 16 (8): e33 https://doi.org/10.2196/mhealth.3359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr David C., Schueller Stephen M., Montague Enid, Burns Michelle Nicole, and Rashidi Parisa. 2014. “The Behavioral Intervention Technology Model: An Integrated Conceptual and Technological Framework for eHealth and mHealth Interventions.” Journal of Medical Internet Research 16 (6): e146. doi:10.2196/jmir.3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina Yamile, Thompson Beti, Espinoza Noah, and Ceballos Rachel. 2013. “Breast Cancer Interventions Serving US-Based Latinas: Current Approaches and Directions.” Women’s Health 9 (4): 335–350. doi:10.2217/whe.13.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen Jakob. 1994. “Heuristic Evaluation” In Usability Inspection Methods, edited by Nielsen Jakob and Mack Robert L., 1st ed, 25–62. New York: Wiley. [Google Scholar]
- Norman Donald A., and Draper Stephen W.. 1986. User Centered System Design New Perspectives on Human-Computer Interaction. Hillsdale, NJ: Lawrence Erlbaum. [Google Scholar]
- Pandey Ambarish, Hasan Sayeedul, Dubey Divyanshu, and Sarangi Sasmit. 2013. “Smartphone Apps as a Source of Cancer Information: Changing Trends in Health Information-Seeking Behavior.” Journal of Cancer Education 28 (1): 138–142. doi:10.1007/s13187-012-0446-9. [DOI] [PubMed] [Google Scholar]
- Penedo Frank J., Traeger Lara, Dahn Jason, Molton Ivan, Gonzalez Jeffrey S., Schneiderman Neil, and Antoni Michael H.. 2007. “Cognitive Behavioral Stress Management Intervention Improves Quality of Life in Spanish Monolingual Hispanic Men Treated for Localized Prostate Cancer: Results of a Randomized Controlled Trial.” International Journal of Behavioral Medicine 14 (3): 164–172. doi:10.1007/BF03000188. [DOI] [PubMed] [Google Scholar]
- Reay Stephen D., Collier Guy, Douglas Reid, Hayes Nick, Nakarada-Kordic Ivana, Nair Anil, and Kennedy-Good Justin. 2017. “Prototyping Collaborative Relationships between Design and Healthcare Experts: Mapping the Patient Journey.” Design for Health 1 (1): 65–79. doi:10.1080/24735132.2017.1294845. [Google Scholar]
- Saint-Germain Michelle A., Bassford Tamsen L., and Montano Gail. 1993. “Surveys and Focus Groups in Health Research with Older Hispanic Women.” Qualitative Health Research 3 (3): 341–367. doi:10.1177/104973239300300306. [Google Scholar]
- Sanders Elizabeth B.-N., and Stappers Pieter Jan. 2008. “Co-Creation and the New Landscapes of Design.” CoDesign 4 (1): 5–18. doi:10.1080/15710880701875068. [Google Scholar]
- Schouten Barbara C., and Meeuwesen Ludwien. 2006. “Cultural Differences in Medical Communication: A Review of the Literature.” Patient Education and Counseling 64 (1–3): 21–34. doi:10.1016/j.pec.2005.11.014. [DOI] [PubMed] [Google Scholar]
- Steele Gray, Daniel Miller Carolyn, Kuluski Kerry, and Cott Cheryl. 2014. “Tying eHealth Tools to Patient Needs: Exploring the Use of eHealth for Community-Dwelling Patients with Complex Chronic Disease and Disability.” JMIR Research Protocols 3 (4): e67. doi:10.2196/resprot.3500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Velsen Lex, Jobke Wentzel, and Julia EWC Van Gemert-Pijnen. 2013. “Designing eHealth That Matters via a Multidisciplinary Requirements Development Approach.” JMIR Research Protocols 2 (1): e21 https://doi.org/10.2196/resprot.2547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson Elisabeth, Chen Alice Hm, Grumbach Kevin, Wang Frances, and Fernandez Alicia. 2005. “Effects of Limited English Proficiency and Physician Language on Health Care Comprehension.” Journal of General Internal Medicine 20 (9): 800–806. doi:10.1111/j.1525-1497.2005.0174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanez Betina, McGinty Heather L., Mohr David C., Begale Mark J., Dahn Jason R., Flury Sarah C., Perry Kent T., and Penedo Frank J.. 2015. “Feasibility, Acceptability, and Preliminary Efficacy of a Technology-Assisted Psychosocial Intervention for Racially Diverse Men with Advanced Prostate Cancer.” Cancer 121 (24): 4407–4415. doi:10.1002/cncr.29658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanez Betina, Stanton Annette L., and Maly Rose C.. 2012. “Breast Cancer Treatment Decision Making among Latinas and Non-Latina Whites: A Communication Model Predicting Decisional Outcomes and Quality of Life.” Health Psychology : Official Journal of the Division of Health Psychology, American Psychological Association 31 (5): 552–561. doi:10.1037/a0028629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanez B, Thompson EH, and Stanton AL. 2011. “Quality of Life Among Latina Breast Cancer Patients: A Systematic Review of the Literature.” Journal of Cancer Survivorship 5 (2): 191–207. doi:10.1007/s11764-011-0171-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zapata Belén Cruz, Fernández-Alemán José Luis, Ali Idri, and Toval Ambrosio. 2015. “Empirical Studies on Usability of mHealth Apps: A Systematic Literature Review.” Journal of Medical Systems 39 (2): 1–19. doi:10.1007/s10916-014-0182-2. [DOI] [PubMed] [Google Scholar]


