Abstract
Basement membranes are thin connective tissue structures composed of organ-specific assemblages of collagens, laminins, proteoglycan like perlecan, nidogens and other components. Traditionally, basement membranes are thought of as structures which primarily function to anchor epithelial, endothelial or parenchymal cells to underlying connective tissues. While this role is important, other functions such as the modulation of growth factors and cytokines that regulate cell proliferation, migration, differentiation and fibrosis are equally important. An example of this is the critical role of both the epithelial basement membrane and Descemet’s basement membrane in the cornea in modulating myofibroblast development and fibrosis, as well as myofibroblast apoptosis and the resolution of fibrosis. This article compares the ultrastructure and functions of key basement membranes in several organs to illustrate the variability and importance of these structures in organs that commonly develop fibrosis.
Keywords: basement membrane, cornea, skin, lung, fibrosis
Introduction
Basement membranes (BM) are specialized extracellular matrix protein complexes found in every organ of the human body. They have specific structures that provide adhesion for epithelium, endothelium or parenchymal cells and separate them from connective tissues, nerves, and muscles. BMs delineate boundaries and compartmentalize tissues in organs while providing scaffolds that guide morphogenesis and tissue repair. BM-mediated cell signaling events and cellular behavior are altered by tissue specific BM composition and structure. BMs are best detected with transmission electron microscopy (TEM) or immunohistochemical staining. The four major components most BMs have in common are nidogens, perlecan, laminins and collagen type IV (Fig. 1). However, even though is great heterogeneity of the primary components, other components also are commonly present and provide specificity of function. Basement membrane components are key players in specialized extracellular matrices and changes in BM composition play significant roles in facilitating the development of various diseases in different organs (Kruegel and Miosge, 2010).
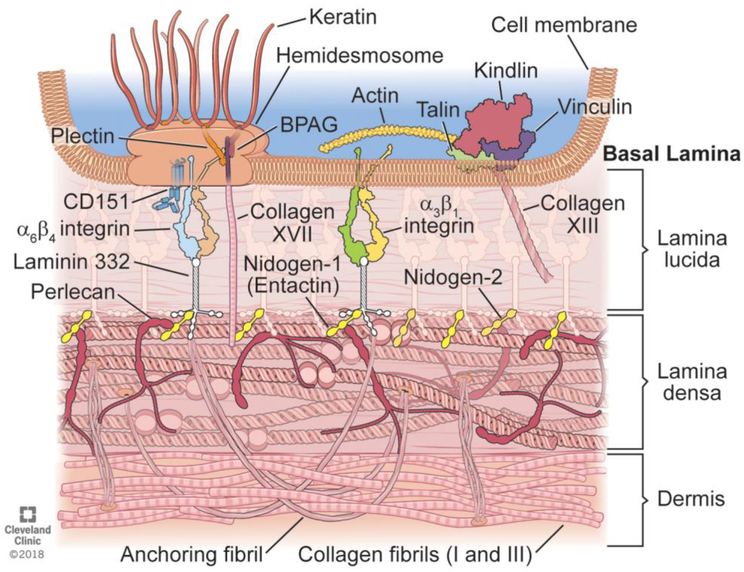
Fig. 1.
Schematic diagram of typical components found in basement membranes, using skin as an example. A basal keratinocyte adheres to the underlying basement membrane and dermis via the focal adhesions that transmit mechanical force and regulatory signals that consist of numerous interacting components such as the hemidesmosome with bullous pemphigoid antigen (BPAG), integrin a6b4, laminin 332, perlecan, anchoring fibrils, and dozens of other components that vary depending on the organ and the status (homeostasis, post-injury, etc.) of the tissues. Many of these components extend into, and are part of, the lamina lucida of the basement membrane. The underling lamina densa of the basement membrane is composed of collagen type IV, nidogens, perlecan, laminin 332, that directly interact with each other, and other components. Lamina lucida is not as wide naturally as it is drawn here for clarity reasons. Illustration by David Schumick, BS, CMI. Reprinted with the permission of the Cleveland Clinic Center for Medical Art & Photography © 2018. All Rights Reserved.
BM proteins were first discovered in mouse yolk sac tumors which produce typical extracellular matrix (ECM) proteins (Chung, et al., 1977, Kleinman and Martin, 2005, Orkin, et al., 1977). Further analysis showed that laminins (Chung, et al., 1979, Timpl, et al., 1979), nidogens (Carlin, et al., 1981, Timpl, 1989), perlecan (Carlin, et al., 1981) and collagen type IV (Kleinman, et al., 1982) are large multi-domain proteins that self-polymerize, bind to other proteins to augment function and promote stability of the tissue (Timpl and Brown, 1996).
Laminins are alpha1, beta1, gamma1 heterotrimeric glycoproteins with more than 15 trimer combinations identified that contribute to tissue specificity of BMs (Miner and Yurchenco, 2004). The laminin nomenclature has been simplified to refer to the alpha, beta, and gamma chains that comprise a specific laminin—such as laminin 332 (Aumailley, et al., 2005). Laminins initiate the BM self-polymerization process during development, repair and regeneration following injury, and other BM components bind to and assemble the mature BM (Miner and Yurchenco, 2004, Smyth, et al., 1999). Collagen type IV has six genetically different α-chains that assemble into three linear collagen type IV heterotrimers (Khoshnoodi, et al., 2008). The stability of the BM structure is attributable primarily to the network formed by laminins and collagen type IV along with other linker components (Halfter, et al., 2015, Timpl, 1989, Yurchenco, et al., 1986).
Nidogen I and nidogen II are sulfated monomeric glycoproteins (Ho, et al., 2008) with the molecular mass of ~ 150 kDa that specifically interact with other BM components such as laminins and collagens to organize and stabilize the BM. Perlecan, also known as basement membrane-specific heparan sulfate proteoglycan core protein (HSPG) or heparan sulfate proteoglycan 2 (HSPG2), is a large multi-domain heparan sulfate proteoglycan (HSPG) that also interacts with other BM components (Hassell, et al., 1980). Unlike laminin and collagen type IV, nidogen and perlecan form irregular polymers using their multiple binding sites. They bridge these scaffolds for laminin and collagen type IV, as well as for each other, and hence they are called as bridging molecules (Aumailley, et al., 1993, Ettner, et al., 1998, Fox, et al., 1991). Complete perlecan deficiency is lethal for mouse embryos at the mid-gestational stage (Arikawa-Hirasawa, et al., 1999, Costell, et al., 1999) and the deletion of both nidogens is prenatally lethal (Bader, et al., 2005). Although nidogen-1 and nidogen-2 are present in all tissues, nidogen-2 alone show more restricted expression patterns and tissue specificity(Kimura, et al., 1998). In vitro, both proteins interact with laminins and collagen type IV and play a critical role in assembly of the mature BM (Fox, et al., 1991, Salmivirta, et al., 2002). Perlecan establishes a high negative charge in the BM because of its three heparan sulfate side chains. Therefore, perlecan plays a major role in regulatory processes of BMs by providing a barrier for some regulatory molecules in addition to serving as an anchoring port and connecting bridges in BMs (Behrens, et al., 2012, Yurchenco, et al., 1986).
In general, BMs have at least one component from the four major proteins and the tissue specificity depends on the differential expression of the respective isoforms and inclusion of other tissue-specific BM components. Thus, the main structural elements, collagen type IV and laminin form a highly-organized network which is non-covalently interconnected by nidogen and perlecan (Paulsson, 1988, Timpl, 1989, Yurchenco, et al., 1986). Laminin gamma 3 chain binds specifically to nidogen (Gersdorff, et al., 2005). In vivo, laminin is necessary for the initial steps involved in the BM assembly (Miner and Yurchenco, 2004, Smyth, et al., 1999) but the stability of the entire BM is determined by the collagen type IV network (Poschl, et al., 2004) forming structured polymers (Fig. 1). Gene deletion analysis of the several mutant phenotypes demonstrate the numerous tissue-specific roles of the four major BM components (LeBleu, et al., 2007). Additional components such as fibrillin (Tiedemann, et al., 2005), collagen type V (Bonod-Bidaud, et al., 2012) and BM-associated collagen type XV and type XVIII may also be involved in these complexes depending on the specific tissue (Breitkreutz, et al., 2013, Miosge, et al., 2003). Agrin is a major proteoglycan component in some BMs, such as the glomerular basement membrane (Denzer, et al., 1995, Tsen, et al., 1995). Collagen type XVIII has also been found to be BM heparan sulfate proteoglycan that is important in retinal BM (Halfter, et al., 1998, Saarela, et al., 1998).
Epithelial, endothelial, and parenchymal cells adhere to the BM via a large family of transmembrane cell adhesion proteins called integrins, that are commonly tissue-specific in distribution, and are receptors that tie the matrix to the cell’s cytoskelatin (Boudreau and Jones, 1999). There are also other cell-associated receptors that bind BM besides integrins (Boudreau and Jones, 1999). The binding of cell surface receptors to BM proteins initiates’ intracellular signaling pathway that influence cellular functions such as migration, proliferation, differentiation and maintenance of the BM.
BMs have many biological functions ranging from tissue organization to functions as depositors for very active molecule such as growth or differentiation factors, including TGFβ and PDGF that can alter the cellularity and composition of underlying tissue such as the stroma in the cornea (Schubert and Kimura, 1991, Torricelli, et al., 2013b). The binding of such growth factors to BM is a very efficient way to regulate the signaling of these growth factors and differentiation factors that can, for example, trigger fibrotic wound healing changes in tissues underlying BMs. The following sections will highlight some of the organ-specific structures and functions of a few BMs.
BM in Cornea
In the cornea, the epithelial BM is present between the basal epithelial cells and the underlying stroma composed primarily of extracellular matrix and fibroblastic keratocytes (Fig. 2). The functions of the epithelial BM include anchoring of the epithelium to the stroma, bidirectional regulation of the passage, and therefore functions, of growth factors and cytokines that modulate functions such as cell proliferation, migration, and differentiation in the epithelium and stroma, as well as the production of chemokines, metalloproteinases and collagenases (Torricelli, et al., 2013b). The composition of corneal BM is different from other organ BMs due to their heterogeneity. Corneal epithelial BM components include laminins, collagen type IV and other collagens, heparan sulfate proteoglycans and nidogens (Tuori, et al., 1996). Descemet’s membrane is the basement membrane of the posterior cornea that lies between the corneal endothelium and posterior stroma. It has functions similar to the epithelial BM but contributes to the “leaky” barrier function of the endothelial-Descemet’s membrane complex important to corneal function (Murphy, et al., 1984). Descemet’s membrane, in contrast to the epithelial BM in the cornea, increases in thickness during both prenatal development (striated BM) and post-natal during the life of the animal by addition of non-striated, non-lamellar extracellular matrix (Murphy, Alvarado and Juster, 1984). The structure and function of Descemet’s layer is altered in corneal diseases such as Fuchs’ endothelial dystrophy and bullous keratopathy, (Johnson, et al., 1982, Zhang and Patel, 2015).
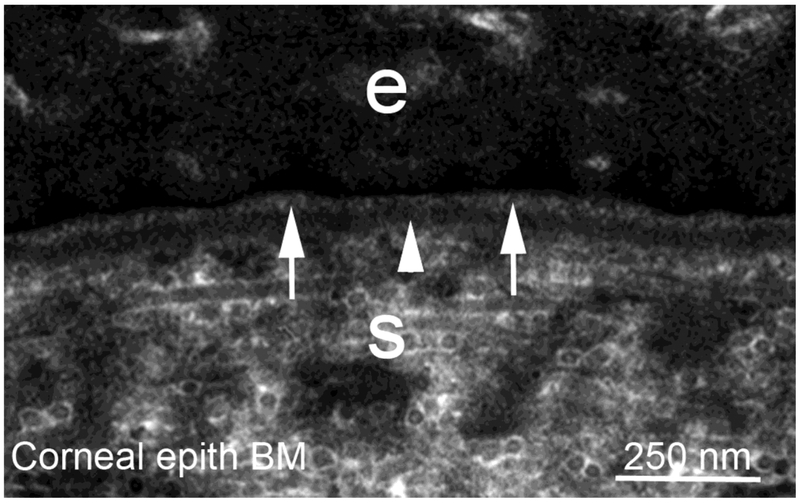
Fig. 2.
Transmission electron micrograph from central rabbit cornea of the epithelial basement membrane (EBM) at 36,000X magnification. In the cornea, the EBM functions to adhere basal epithelial cells (e) to the underlying stroma and to modulate growth factor-mediated communications between the epithelium and the keratocytes within the stroma (S). As artifacts of fixation, the lamina lucida (arrows) and lamina densa (arrowhead) can be seen. Although this morphology is an artifact of fixation, it signifies the presence of a mature skin BM. The regular packing of the collagen fibrils, visible as uniform diameter circles, in the stroma contributes to corneal transparency.
Initially, it was reported that laminin-111 and laminin-332 were the major laminins in the epithelial BM of the human cornea (Ljubimov, et al., 1995; Tuori, et al., 1996). Later, however, Filenius et al found that the BM of human cornea contain only laminin-332 and laminin-511 but not laminin-111. Laminin-332 is produced by the epithelial cells (Filenius, et al., 2001) and laminin-511 is produced by the keratocytes (Hassell, et al., 1992). Corneal epithelial cells adhere to the laminins in the epithelial BM through integrins. Human corneal epithelial cells have been shown to express integrins α6β4, α3β1 and α2β1 involved in these interactions (Tervo, et al., 1991, Virtanen, et al., 1992). Epithelial BM contains collagen type IV, as well as collagen type VII, collagen type XVII and collagen type XVIII (Michelacci, 2003). Several investigators identified collagen type IV in the epithelial BM, but some were not able to identify this molecule in the BM of the central cornea in some species (Cameron, et al., 1991). Collagen type IV is known to be present in the human corneal BM as early as eight weeks of gestation and throughout life (Ben-Zvi, et al., 1986) . After injury, collagen type IV is present in the re-synthesized BM and it is involved in the binding the basal surface of the epithelial cells to the BM. In vitro, collagen type IV has been shown to promote migration and adhesion of corneal epithelial cells (Cameron, Skubitz and Furcht, 1991). Thus, collagen type IV is one of the native components in BM involved in the development, maintenance and wound healing process in the cornea. Collagen type XVII and α6β4 integrin are present in the hemi-desmosomes, the stud-like structures present in basal corneal epithelial cells that adhere the epithelium to the underlying stroma via anchoring fibrils (Gipson, et al., 1988). In vitro, it has been shown that collagen type XVII interacts with the β3 chain of the laminin-332, to support cell binding (Torricelli, et al., 2013a).
Collagen type XVIII is the only known BM component with heparan sulfate glycosaminoglycan side chains (Dong, et al., 2003). In cornea, collagen type XVIII is localized in the epithelial BM and Descemet membrane (Lin, et al., 2001). Knockout of collagen type XVIII doesn’t result in a known corneal phenotype but is known to cause other eye abnormalities (Fukai, et al., 2002, Maatta, et al., 2007), including pigment granule release, massive disorganization of retinal pigment epithelium, and photoreceptor and iris abnormalities (Marneros, et al., 2004, Marneros and Olsen, 2003). In humans with Knobloch syndrome, a rare disorder with retinal degeneration and high myopia, have mutations in the gene encoding the α1 chain or deficiency of collagen type XVIII (Menzel, et al., 2004, Nystrom, et al., 2017, Suzuki, et al., 2002).
Perlecan is a key component of the corneal epithelial BM which interacts with other basement membrane components to establish the epithelial barrier function and epithelial morphology. A thinner corneal epithelium and microphthalmos were observed in perlecan deficient mice (Inomata, et al., 2012). Pseudomonas aeruginosa is a bacterium that can produce corneal ulcers and perlecan is known to serve as a binding site for these bacteria. Chen and Hazlett (Chen and Hazlett, 2001) showed that anti-perlecan antibody can decrease binding of Pseudomonas aeruginosa to corneal epithelial cells in the human cornea. After epithelial scrape injury in humans that damages the corneal epithelial basement membrane, stromal keratocytes were shown to produce high levels of perlecan and nidogen-2 and, therefore, contribute to epithelial BM regeneration (Torricelli, et al., 2015).
Nidogens are present in the epithelial BM, stroma and Descemet’s membrane of the cornea. Nidogen-1 and nidogen-2 bind to various BM-associated proteins and they are known to be a connecting element between laminin and the collagen network in BM (Kabosova, et al., 2007). Keratocytes and myofibroblasts have been shown to produce nidogen-1 and −2 in vitro (Santhanam, et al., 2015). In nidogen-1 knockout mice, minimal pathological changes were observed in the anterior segment of the eye, including the epithelial BM (May, 2012). These changes were not seen in the nidogen-2 knockout mice (May, 2012).
In addition to epithelial BM, cornea possesses another basement membrane called Descemet’s membrane (DM) that lies between the corneal endothelium and posterior stroma (Fig. 3) that participates in the “leaky barrier function” of the corneal endothelium (Zhang and Patel, 2015; Kapoor, et al., 1986). For example, the endothelial-DM complex allows critical nutrients to pass into the stroma but restricts the passage of transforming growth factor beta from the aqueous humor into the stroma in the absence of endothelial-DM injury (Marino, et al., 2017a). The thickness of DM increases with age, with it having approximately 3μm of thickness in children and 10um in adults (Chi, et al., 1958, Johnson, Bourne and Campbell, 1982). DM is composed of two layers: an anterior banded layer which is composed of collagen lamellae and proteoglycans and a posterior non-banded layer which is continually synthesized and thickens over decades (Kefalides, et al., 1976). Freeze–fracture, deep-etch replica method has clearly showed that the lattice of the DM is constructed of mainly four components (Sawada, 1982): (1) round densities forming the nodes of the lattice, (2) rod-like structures connecting the nodes, (3) fine filaments two-dimensionally distributed in the interstices and (4) amorphous materials. Biochemical studies of DM revealed similarities with other BM in major molecular components, including collagen type IV, fibronectin, laminins and heparan sulphate proteoglycan (Carlson, et al., 1981, Kefalides and Denduchis, 1969) and nidogens (Medeiros, et al., 2018). In contrast to other BMs, collagen type VIII is a major constituent in DM, which forms ladder like structure visible with electron microscopy (Labermeier and Kenney, 1983). The finding that corneal endothelial cells in vitro synthesized collagen type VIII supports the presence of type VIII collagen in DM (Benya and Padilla, 1986, Sage, et al., 1981). Collagen type VIII is a hetero-trimer composed of two distinct alpha chains, α1 and α2, each with molecular weight of about 60,000 daltons (Benya and Padilla, 1986, Shuttleworth, 1997). The hexagonal lattice structure creates a matrix that can resist compression and maintains the open porous structure that allows nutrients to pass in to stroma (Shuttleworth, 1997), an important function of the Descemet’s membrane-endothelial complex. Fuchs’ endothelial corneal dystrophy (FECD) has typical pathological changes that include progressive loss of endothelial cells, thickening of the DM, and deposition of anomalous extracellular matrix in the form of guttae (Chi, Teng and Katzin, 1958). FECD is likely a group of genetic disorders affecting the corneal endothelium and DM.
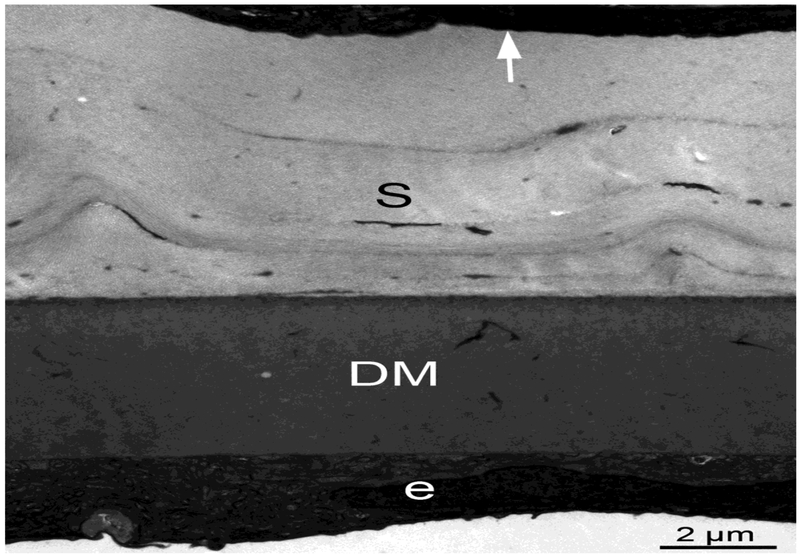
Fig. 3.
Rabbit cornea Descemet’s basement membrane at 12,600X magnification. Notice the impressive thickness (greater than 6 μm) of Descemet’s basement membrane (DM) in a rabbit only 14 weeks old. Descemet’s basement membrane continues to increase in thickness throughout life. Descemet’s basement membrane provides adhesion for the monolayered corneal endothelial cells (e) that modulate corneal hydration critical to corneal transparency, allows passage of nutrients from the aqueous humor into the stroma, and modulates the passage of TGFβ from the aqueous humor into the corneal stroma that would drive keratocyte differentiation into myofibroblasts and trigger fibrosis. S is the stroma that makes up greater than 90% of the corneal thickness. A stromal fibroblastic cell referred to as a “keratocyte” is indicated by the arrow.
BM in Skin
Skin consists of two compartments, epidermis and dermis (Fig. 4). Epidermis serves as first line of defense between the external environment and the animal’s internal organs, and it is connected to the dermis compartment by the BM (Breitkreutz, et al., 2013). Apart from structural properties, the BM controls keratinocyte adhesion, traffic of cells, and diffusion of molecules such as growth factors and cytokines, including keratinocyte growth factor and platelet-derived growth factor, that regulate both keratinocyte and dermal fibroblast functions through regulation of activation and release (Breitkreutz, et al., 2013). In addition, BM plays an important role during the remodeling process after injury and damage to BM by cancer leads to cell activation in the stroma (Mueller and Fusenig, 2004).
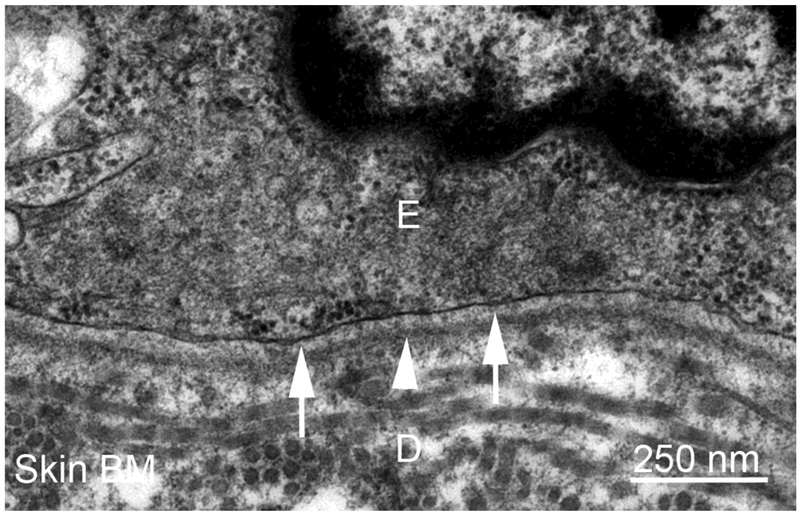
Fig. 4.
Transmission electron micrograph of rabbit inner thigh skin basement membrane (BM) at 40,000X magnification. The overlying basal keratinocyte adheres to the dermis (D) via the basement membrane (BM) composed of lamina lucida (arrows) and lamina densa (arrowhead). The BM in skin also regulates growth factor-mediated interactions between the epithelium and skin fibroblasts in the dermis. Note that the basal epithelial cell membrane in skin is much more prominent than in the cornea.
Skin BM components, such as perlecan, collagen type IV and collagen type VII, are produced by dermal fibroblasts and epidermal keratinocytes. Other components, like laminin-511 and laminin-332, are primarily synthesized by keratinocytes, although the main source of nidogens is thought to be dermal fibroblasts (Bechtel, et al., 2012, Fleischmajer, et al., 1995). Additionally, dermal fibroblasts transiently synthesize laminin-211 during wound healing in adult skin (Sugawara, et al., 2008).
The upper layer epidermis is connected to the BM by hemidesmosomes containing plectin and bullous pemphigoid antigen 1 (BPAG1) proteins (Sterk, et al., 2000). These proteins are linked to alpha 6/beta 4, (Sonnenberg, et al., 1991) CD151 (Sterk, et al., 2002) and collagen type XVII (Qiao, et al., 2009). Integrin alpha6/beta 4 also binds to laminin-332, the only integrin associated with keratins (Aumailley, et al., 2005) . The BM is connected to the dermis beneath by loop structures of collagen type VII and anchoring fibrils. Also, anchoring fibril-collagen type VII tightly binds to collagen type I and type III fibrils in the dermis (Villone, et al., 2008). Together, these bridges are essential to maintenance of the structural and functional integrity of skin. Defects in the skin BM or BM-associated molecules is often associated with severe or lethal disease ( Sterk, et al., 2002; Aumailley, et al., 2005,).
Mice lacking nidogen-1 and nidogen-2 live to birth and have skin that appear grossly normal (Bader, et al., 2005). But the ultrastructure of the skin reveals abnormal basal cells with micro-blistering, microvascular aberrations, BM duplications and leakiness of small vessels (Mirancea, et al., 2007). These mice die from lung and heart abnormalities that are directly related to BM defects, but kidney BMs appear normal (Bader, et al., 2005).
Co-cultures of epidermal keratinocytes and dermal fibroblasts have been investigated extensively to study on skin physiology and repair. However, these approaches have major drawbacks that limit communications between two cell types that occur in vivo. Therefore, organotypic co-cultures have been used to provide a better understanding of cellular interactions and BM generation in skin (Fleischmajer, et al., 1995; Smola, et al., 1998). Thus, in these models, normal epidermal phenotype and BM structure is generated with cells from different sources and with several combinations of epithelial and fibroblastic cells. For example, normal BM structure and epidermal phenotype, including hair follicles, can be generated in organotypic co-culture (Limat, et al., 1996, Stark, et al., 1999). These systems serve as alternative approaches to study the functions of mutated BM components (Di Nunzio, et al., 2008, Fritsch, et al., 2009, Murauer, et al., 2011).
Transplantation models offer other strategies to study the regeneration of skin and BM in mice. Cultured mouse keratinocytes regain full differentiated function, including the production of BM, when transplanted on the backs of C3H mice (Breitkreutz, et al., 1984). Similarly, HaCat cells or keratinocytes from human skin transplanted on nude mice generate normal epidermal tissue and BMs when examined with immunohistochemistry for BM components and ultrastructure examined with TEM. In these studies, the first BM component to appear is laminin-332, followed by nidogens, laminin-511 and collagen type IV (Breitkreutz, et al., 1998, Breitkreutz, et al., 1997).
Skin BMs from histological specimens, transplantation models, and organotypic co-cultures appear structurally and functionally the closest in morphology to corneal epithelial BM (compared to other imaged organs), although at high magnification after identical fixation and processing a difference in morphology appears obvious and could relate to transparency in the cornea (compare Fig. 2 to Fig 4).
There are a number of skin disorders associated with skin blistering, including epidermolysis bullosa affecting at least 18 genes associated with the EBM and adhesion to the EBM (Uitto, et al., 2017), pemphigus, and bullous pemphigoid (Hammers and Stanley, 2016). Pemphigus and bullous pemphigoid are auto-antibody-mediated blistering diseases of the skin. In pemphigus, keratinocytes in epidermis and mucous membranes lose cell-cell adhesion, and in pemphigoid, the basal keratinocytes lose adhesion to their basement membrane. Detailed discussion of these disorders is beyond the scope of this review, but they have been instrumental in understanding the specific functions of many BM components.
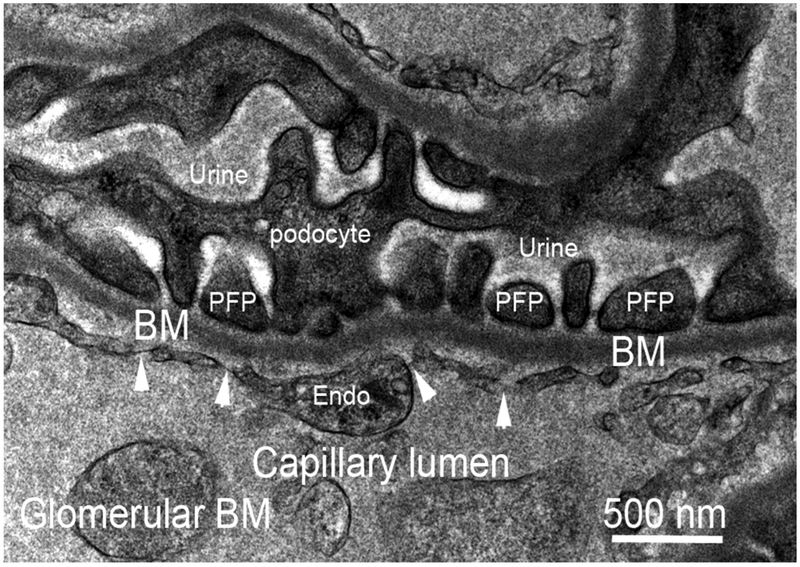
BM in Kidney
The glomerular basement membrane (GBM) lies between the glomerular endothelial cells and the podocytes (Fig. 5) and functions in the removal of waste and other molecules from blood plasma into the urine without the release of other plasma components such as albumin. The podocytes, which adhere to the GBM, play an active role in preventing plasma proteins from entering the urinary ultrafiltrate by providing a barrier comprising filtration slits between the podocyte foot processes (Fig. 5) (Reiser and Altintas, 2016). Unlike other BMs, the GBM is unusually thick and composed primarily of collagen type IV and laminins (Timpl, 1989). Mutations in these components cause filtration defects and result in severe renal disease (Miner, 2012). Agrin is the major heparan sulfate proteoglycan in GBM (Timpl, 1989) . This structure allows the passage of plasma water and small waste solutes but limits the flow of large plasma proteins such as albumin. Defects in one of these layers will result in high levels of albumin in the urine.
Fig. 5.
Transmission electron micrograph of glomerular basement membrane (BM) in rabbit kidney at 45,000X magnification. The BM that functions in the excretion of waste molecules from capillaries into the urine is a “double” BM that provides adhesion of capillary endothelial cells (endo) with fenestrations (arrowheads) on one side and podocyte foot plates (PFP) of podocytes on the other.
In adult GBM, laminin-521 is the major laminin. During GBM formation and maturation, however, laminins go through a transition from laminin-111 to laminin-511 and then to laminin-521(Miner, et al., 1997, Miner and Sanes, 1994) and genetic defects in this transition results in GBM breakdown. For example, in mice, a mutation in laminin α5 inhibits the laminin-111 to laminin-511 transition and results in the failure of glomerular vascularization(Miner and Li, 2000). Mutation in laminin β2 in humans or in mice results in a congenital nephrotic syndrome with neurological manifestations and it is known as Pierson syndrome (in humans) (Matejas, et al., 2010).
Collagen type IV plays a critical role in BM stability (Poschl, et al., 2004). Collagen also undergo developmental transitions in GBM during glomerulogenesis. Initially, GBM contains an α1/α2 network but when the glomerular capillaries begin to function, the podocytes secrete α3α4α5 trimers. Then, these components polymerize to form a collagen type IV network characteristic of the fully mature GBM (Abrahamson, 2009). Mutations in genes encoding any one of the collagen chains can cause defects in the GBM resulting in mild to severe disease. For example, ‘thin basement membrane disease’ has been found in 40 to 50% of patients having mutations in COL4A3 or COL4A4, which encode the α3 and α4 chains of collagen type IV, respectively (Voskarides, et al., 2007). Alport syndrome is a severe basement membrane disease, which eventually leads to kidney failure along with deafness and ocular abnormalities. The X-linked form is the most common version of Alport syndrome and it is caused by mutations in COL4A5 encoding the α5 chain of collagen type IV (Heidet, et al., 2000).
In mice, deletion of both nidogen-1 and nidogen-2 genes results in perinatal lethality. Nidogen-1 binds to both laminins and collagen type IV and, therefore, is an important component for BM formation. However, BM can form in the absence of both nidogens and the GBM can appear ultrastructurally normal. However, renal dysgenesis or hydronephrosis can be noted in the fully developed kidney (Bechtel, et al., 2012; Miosge, et al., 2002) . The absence of one or both nidogens does not alter basement membrane composition in adult murine kidney (Gersdorff, et al., 2007).
Agrin is the major heparan sulfate proteoglycan of the GBM (Groffen, et al., 1998, Timpl, 1989). As a heparan sulfate proteoglycan, and also due to the presence of sulfated glycosaminoglycan side chains, agrin has a high net negative charge. All BM, and particularly the GBM, have a net negative charge. Perlecan and agrin are thought to be the most important contributors to this negative charge (Kanwar, et al., 2007). It is thought that the net negative charge of the GBM is crucial for function, including the filtration of molecules by the glomerulus. Thus, studies show that molecules that are positively-charged cross the filtration barrier more easily than the neutral molecules, which in turn cross more easily than the negatively-charged molecules. For example, plasma albumin, which is negatively-charged, is repelled by the GBM. Defects in GBM allow albumin to pass the filtration barrier and results in high albumin content in urine. However, selective knockout of agrin had no effect on the glomerular filtration barrier in one study (Harvey, et al., 2007).
There are a number of diseases that affect the glomerular BM. In mature GBM, the major collagen type IV molecule is the alpha-3 alpha-4 alpha-5 isoform, associated with laminin-521 (alpha-5 beta-2 gamma-1), nidogen and agrin heparan sulfate proteoglycans. Several hereditary glomerular diseases are linked to structural anomalies of GBM tissue-specific components; for example, the alpha-3 alpha-4 alpha-5 isoform of collagen type IV in Alport syndrome and thin basement membrane nephropathy (benign familial hematuria), and laminin in Pierson syndrome (Gubler, 2008). Tumor necrosis factor-α has been shown to drive Alport glomerulosclerosis in mice by promoting podocyte apoptosis (Ryu, et al., 2012). Another example is the Goodpasture’s antigen associated with Goodpasture’s syndrome that is the NC1 domain of the alpha-3 chain of collagen type IV found in the glomerular BM (Derry and Pusey, 1994).
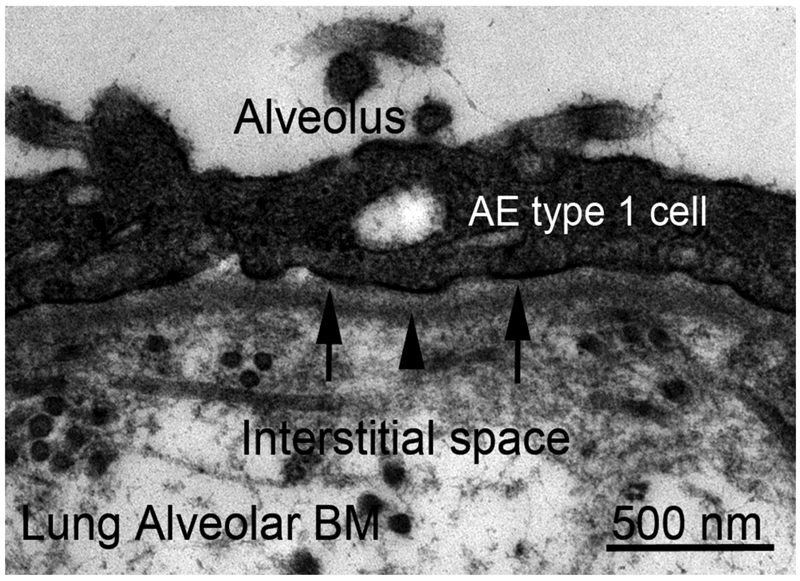
BM in Lung
The BMs of the alveolus functions in cell adhesion for alveolar epithelial and endothelial cells, to facilitate gas exchange between the alveolar space and the alveolar capillaries (West and Mathieu-Costello, 1999), to regulate cytokine and growth factor functions, and other alveolar cellular processes in the lung (Sannes and Wang, 1997). The polarity of the lung is maintained by the BMs and they act as physical barriers between epithelium, endothelium and mesenchymal tissues.
Pulmonary alveoli have been shown to have a thinner side and a thicker side (Vaccaro and Brody, 1981, Weibel, 1973). The thinner side consists of alveolar epithelium and capillary endothelium separated only by a common fused BM that is thought to facilitate gas exchange. The thicker side consists of alveolar epithelium and capillary endothelium, each with their respective BMs (alveolar BM [Fig. 6] and capillary BM, respectively) separated by connective tissues within the interstitial space (Vaccaro and Brody, 1981, Weibel, 1973). These two lung BMs appear to have similar ultrastructure when examined with standard TEM techniques. However, staining with ruthenium red demonstrated that the two lung BMs have different ultrastructural characteristics and that the type and distribution of proteoglycans differs between alveolar BM and capillary BM (Vaccaro and Brody, 1981). Otherwise, the component differences between these BMs have not been fully characterized. The integrity of the BMs maintains the normal lung architecture and the alveolar BM is crucial for restoration of alveolar epithelial homoeostasis following lung injury (Strieter and Mehrad, 2009).
Fig. 6.
Transmission electron micrograph of alveolar basement membrane (BM) of rabbit lung at 46,000X. Shown is the “thicker side” of the alveolus where the alveolar BM and capillary BM are separated by an interstitial space containing collagen fibrils and other extracellular matrix materials. The alveolar epithelial (AE) type 1 cell rests on the BM with lamina lucida (arrows) and lamina densa (arrowhead). On the “thinner side” of the alveolus (not shown) the alveolar BM and capillary BM fuse, at least focally, to form a single BM separating alveolar epithelial type 1 cells and capillary endothelial cells—a BM morphological variation that is thought to facilitate gas exchange between the alveolar space and the alveolar capillaries (Vaccaro and Brody, 1981).
Loss of alveolar BM/capillary BM integrity has been observed in idiopathic pulmonary fibrosis (IPF) (Chen, et al., 2016). Mechanisms underlying this disruption have not been well defined. Specific alveolar BM components have been described, including the Goodpasture’s antigen associated with Goodpasture’s syndrome that is the NC1 domain of the alpha-3 chain of collagen type IV, that is also found in the glomerular BM (Derry and Pusey, 1994). The absence of the basement membrane component nidogen-2, but not of nidogen-1, has been shown to result in increased lung metastases in mice (Mokkapati, et al., 2012).
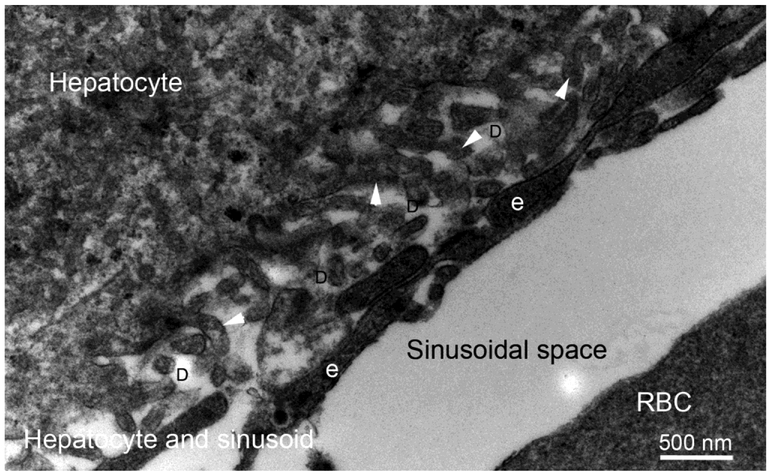
BM in the Liver
BMs are found in blood and lymphatic vessels and around the bile ducts in human liver (Hahn, et al., 1980; Mak and Mei, 2017). Their presence in the tubular regions, particularly between sinusoids lining cells and hepatocytes, is still controversial (Schaffner and Poper, 1963). Lack of a typical BM in the perisinusoidal space in normal liver (Fig. 7) is thought to allow the intimate contact between blood and parenchymal cells necessary for normal hepatocyte function. However, the appearance of a continuous perisinusoidal BM in experimental liver injury and in human liver fibrosis has been reported (Bucher, 1963; Mak and Mei, 2017). These disease-related changes may severely restrict the normal functions of the liver.
Fig. 7.
Transmission electron micrograph of rabbit liver hepatocyte, sinusoids and spaces of Disse at 30,000X magnification. Hepatocytes are organized into plates separated by the space of Disse (D) from vascular channels termed sinusoids. Hepatocyte processes (arrowheads) extend into the space of Disse. Sinusoids have a discontinuous, fenestrated endothelial cell lining. Of note, there is no basement membrane between either hepatocytes or endothelial cells and the space of Disse—allowing direct cellular contact that is thought to facilitate hepatocyte functions such as detoxification, modification, and excretion of exogenous and endogenous substances.
Thus, liver hepatocytes lack the typical electron dense structure of BM in other organs and contains non-BM constituents such as collagen type I and fibronectin, in addition to some typical BM constituents (Martinez-Hernandez and Amenta, 1995; Matsumoto, et al., 1999). Sinusoidal endothelial cells in liver can secrete collagen type IV, laminin, nidogen and perlecan (Wells, 2008). Collagen type IV, laminin and perlecan are also produced by perisinusoidal hepatic stellate cells (HSCs) (Wells, 2008). In the portal tracts, biliary epithelial cells are the principal cells producing collagen type IV, laminin, and perlecan, while portal fibroblasts and myofibroblasts, when generated, also contribute to their production. Expression of collagen type IV along with increased deposition of laminin in the space of Disse results in the formation of a perisinusoidal BM in liver fibrosis (Mak, et al., 2013). Laminin expression is not detected in the parenchyma of normal human liver, only in liver fibrogenesis, where β2 laminin chain may be deposited in the space Disse, along with collagen type IV and perlecan, forming a continuous basement membrane beneath the endothelium of liver sinusoids (Mak and Mei, 2017).
BM in other organs
Most other organs in a human or animal, including brain, heart, gut (with variation in the different segments of the small intestine and the large intestine), pancreas, gall bladder, and testis, have BMs that are similar in overall composition to those that have been described for cornea, skin, lung and kidney, but with tissue-specific alterations in BM components that facilitate the specific functions of these organs. A specific description of the differences in BM composition between these many different organs is beyond the scope of this review.
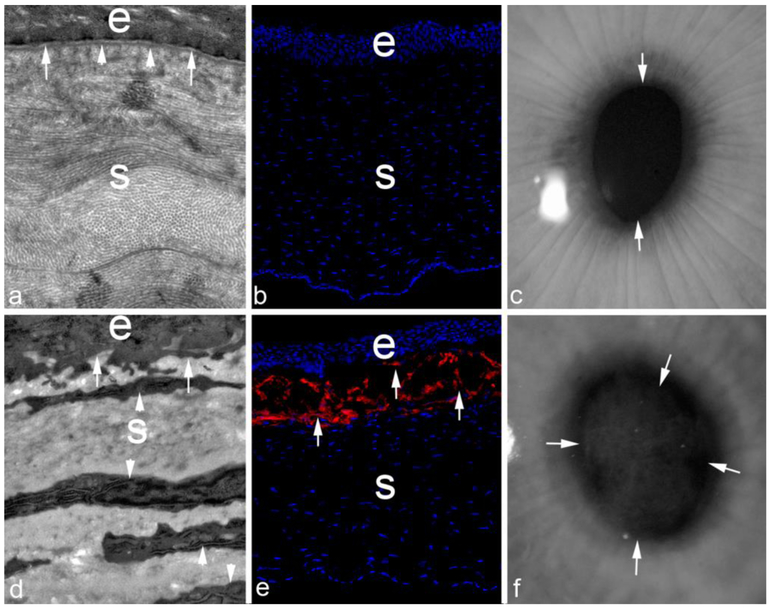
EBM injury, regeneration and fibrosis in different organs
Corneal EBM injury and regeneration, and its relationship to organ fibrosis, is one of the best-characterized systems. Whether the injured cornea heals with transparency or with fibrosis and transparency depends on the type and level of injury (Torricelli, et al., 2013b). Corneal stromal keratocytes are fibroblastic cells that are normally relatively quiescent and function to maintain the precise structure of the stromal extracellular matrix associated with transparency (Chaurasia, et al., 2009; Hassell and Birk, 2010; Ishizaki, et al., 1993; Jester, et al., 1999; Jester, et al., 1995; Kaur, et al., 2009). Corneal injuries “activate” keratocytes at the site of injury and in the proximate stroma to “corneal fibroblasts” that participate in the healing response and can differentiate into myofibroblasts when exposed to sustained transforming growth factor β1 or β2 (Jester, et al., 1987; Kaur, et al., 2009; Wilson, 2012). In vitro cell culture experiments have identified several key growth factors such as TGFβ1, TGFβ2, and PDGF that play critical roles in mediating keratocyte differentiation to wound healing corneal fibroblast and myofibroblast phenotypes (Jester, et al., 2002; Jester, Rodrigues and Herman, 1987; Tuli, et al., 2006; Wilson, 2012). In addition, after corneal injury, bone marrow-derived fibrocytes penetrate the corneal stroma and differentiate into myofibroblasts when TGFβ and PDGF are present in the stroma at sufficient and sustained levels (Barbosa, et al., 2010). It has been well documented that these key growth factors are produced in high levels by corneal epithelial cells but their penetration into the stroma is negligible when the EBM is intact (Fini, 1999, Torricelli, et al., 2013b, Wilson, 2012). The corneal epithelium, like other epithelial layers in animals, is continuously subjected to physical, chemical and biological insults. If an insult is sufficiently severe, the EBM is also injured, allowing the penetration of pro-fibrotic TGFβ, PDGF, and possibly other growth factors and cytokines, into the corneal stroma to initiate the development of corneal fibroblasts and myofibroblasts from local (keratocyte) and bone marrow-derived (fibrocyte) precursors (Torricelli, et al., 2013b, Wilson, 2012). If the EBM is promptly repaired, for example after most simple corneal abrasions, the penetration of TGFβ and PDGF into the stroma is consequently cut off and the developing myofibroblast precursors undergo IL-1-mediated apoptosis (Kaur, et al., 2009) before they become mature vimentin+ alpha-smooth muscle actin+ desmin+ myofibroblasts (that secrete large amounts disordered extracellular matrix) (Chaurasia, et al., 2009), keratocytes repopulate the anterior stroma, and transparency of the corneal stroma is maintained (Fig. 8A, B and C) . If, however, repair of the EBM is sufficiently delayed, then TGFβ and PDGF continue to penetrate the stroma at high levels, resulting in the development of large numbers of stromal myofibroblasts, and the prodigious amounts disordered extracellular matrix they produce, results in fibrosis and loss of transparency that is crucial for corneal function (Fig. 8D, E and F) (Torricelli, et al., 2013b, Wilson, 2012). Delayed regeneration of EBM can result from mechanical factors such as corneal stromal surface irregularity produced by injury, surgery, infection or disease (Netto, et al., 2006). Another mechanism for delayed EBM regeneration, however, is likely insufficient stromal keratocyte contributions of basement membrane components needed for full restoration of EBM structure and function (Santhanam, et al., 2017; Santhanam, et al., 2015; Torricelli, et al., 2015). Thus, keratocytes produce laminins, nidogen-1, nidogen-2, perlecan, and possibly other EBM components. The working hypothesis is that after corneal injury, the healed corneal epithelium lays down a self-polymerizing laminin nascent EBM and that this layer produces a barrier to the penetration of more posterior EBM components that must be provided, at least in part, by keratocytes (Santhanam, et al., 2017, Wilson, et al., 2017). If the original injury is sufficiently severe, resulting in substantial loss of adjacent keratocytes by apoptosis and/or necrosis (Marino, et al., 2017a; Mohan, et al., 2003; Wilson, et al., 1996) and, therefore, there are diminished keratocyte contributions of components to EBM repair, then defective regeneration of the EBM promotes the development and persistence of myofibroblasts via ongoing penetration of TGFβ and PDGF into the stroma. These persistent myofibroblasts produce the fibrosis in the anterior subepithelial stroma. After a period of time, importantly without recurrent injury and typically measured for the cornea in many months to years, the normal mature EBM may be regenerated—likely via keratocyte penetration of the layer of myofibroblasts and their disordered extracellular matrix—where the keratocytes coordinate with the overlying epithelium to facilitate EBM regeneration. Once the EBM is fully repaired, myofibroblasts, deprived of their ongoing source of TGFβ, undergo apoptosis (Wilson, et al., 2007). Subsequently, the anterior stroma is repopulated by keratocytes, which remove and reorganize the disordered extracellular matrix and restore corneal stromal transparency (Marino, et al., 2017b, Wilson, et al., 2017).
Fig. 8.
Regenerative vs. fibrotic repair of the rabbit cornea after injury. At one month after minor injuries to the rabbit cornea, such as epithelial abrasion or −4.5 diopter photorefractive keratectomy (PRK) that is shown (A to C), in which the EBM and a small amount of the anterior stroma is ablated with the excimer laser and relatively few stromal keratocytes die by apoptosis or necrosis, transmission electron microscopy (TEM) shows that the EBM regenerates normally (A, 22,000X mag., arrows are lamina lucida and arrowheads are lamina densa), keratocytes repopulate the anterior stroma (B, 400X mag., arrows) and few, and in this case no, myofibroblasts are detected by staining for the alpha-smooth muscle actin (SMA) myofibroblast marker (B, 400X mag. showing DAPI stained keratocytes in the stroma (s). The cornea overlying the pupil (arrows) is transparent and iris details are clear when photographed with a slit lamp at one month after −4.5D PRK (C, 20x mag.). After a more severe injury (such as high correction −9 diopter PRK) shown in D to F, the EBM is not regenerated at one month after surgery and no lamina lucida or lamina densa is detected (D, 22,000X mag., arrows note no EBM beneath the epithelium) and myofibroblasts (arrowheads) with large amounts of rough endoplasmic reticulum fill the anterior stroma of the cornea. Note in D the disorganization of the collagen in the stroma surrounding the myofibroblasts compared to A, where the collagen fibrils are uniform diameter and regularly packed—an important contributor to the transparency of the normal corneal stroma. After this level of injury (E, 400X mag.) the anterior stroma beneath the epithelium (the ongoing source of TGFβ that penetrates the stroma to maintain the viability of the myofibroblasts in the absence of normal EBM) has a layer of SMA+ myofibroblasts (arrows). A slit lamp photograph of the cornea at one month after surgery shows fibrosis (F, 20X mag., arrows delineate area of fibrosis that is also called haze) in the area of the previous PRK surgery. e is the epithelium and s is the stroma in panels A, B, D, and E.
The importance of the coordination and interplay between the epithelial cells, stromal cells, bone marrow-derived cells and the EBM in modulating transparency and fibrosis in the cornea at every stage of the corneal wound healing process, as well as in homeostasis in the normal uninjured cornea is remarkable and likely relevant to the interactions between epithelial cells, parenchymal cells, fibroblasts, endothelial cells, bone marrow-derived cells, and basement membranes that occur in other organs during homeostasis in normal tissues, and after injuries in which fibrosis may occur. Fibroblasts and other non-epithelial and non-parenchymal cells have been shown to produce basement membrane components in many other organs (El Ghalbzouri, et al., 2005; El Ghalbzouri and Ponec, 2004; Fleischmajer, et al., 1995; Fox, et al., 1991; Furuyama, et al., 1997; Marinkovich, et al., 1993; Simon-Assmann, et al., 1998; Smola, et al., 1998). Thus, keratinocyte-fibroblast interactions have been shown to be important in basement membrane generation in organotypic skin cultures (Smola, et al., 1998) . Similarly, assembly of the alvelolar basement membrane after lung injury is likely orchestrated by cooperation between alveolar epithelial cells and pulmonary fibroblasts (Furuyama, Kimata and Mochitate, 1997). In addition, fibrosis has been shown to resolve in other organs after removal of sources of chronic injury. For example, bleomycin-induced lung fibrosis in mice can reverse spontaneously after removal of the inciting agent (Cabrera, et al., 2013; Lawson, et al., 2005; Li, et al., 2011). In humans, skin fibrosis associated with systemic sclerosis can at least partially resolve following neutralization of the antifibrinolytic function of plasminogen activator inhibitor 1 (Lemaire, et al., 2016). Further research should be directed at fully understanding these critical cellular and extracellular matrix interactions that likely lie at the core of the development and resolution of fibrotic diseases that occur in many organs.
Acknowledgments
Supported in part by US Public Health Service grants RO1EY10056 (SEW) and P30-EY025585 from the National Eye Institute, National Institutes of Health, Bethesda, MD.
REFERNCES:
- Abrahamson DR (2009) Development of kidney glomerular endothelial cells and their role in basement membrane assembly. Organogenesis 5:275–287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arikawa-Hirasawa E, Watanabe H, Takami H, Hassell JR, Yamada Y (1999) Perlecan is essential for cartilage and cephalic development. Nat Genet 23:354–358 [DOI] [PubMed] [Google Scholar]
- Aumailley M, Battaglia C, Mayer U, Reinhardt D, Nischt R, Timpl R, Fox JW (1993) Nidogen mediates the formation of ternary complexes of basement membrane components. Kidney Int 43:7–12 [DOI] [PubMed] [Google Scholar]
- Aumailley M, Bruckner-Tuderman L, Carter WG, Deutzmann R, Edgar D, Ekblom P, Engel J, Engvall E, Hohenester E, Jones JC, Kleinman HK, Marinkovich MP, Martin GR, Mayer U, Meneguzzi G, Miner JH, Miyazaki K, Patarroyo M, Paulsson M, Quaranta V, Sanes JR, Sasaki T, Sekiguchi K, Sorokin LM, Talts JF, Tryggvason K, Uitto J, Virtanen I, von der Mark K, Wewer UM, Yamada Y, Yurchenco PD (2005) A simplified laminin nomenclature. Matrix biology : journal of the International Society for Matrix Biology 24:326–332 [DOI] [PubMed] [Google Scholar]
- Bader BL, Smyth N, Nedbal S, Miosge N, Baranowsky A, Mokkapati S, Murshed M, Nischt R (2005) Compound genetic ablation of nidogen 1 and 2 causes basement membrane defects and perinatal lethality in mice. Mol Cell Biol 25:6846–6856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbosa FL, Chaurasia SS, Cutler A, Asosingh K, Kaur H, de Medeiros FW, Agrawal V, Wilson SE (2010) Corneal myofibroblast generation from bone marrow-derived cells. Experimental eye research 91:92–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bechtel M, Keller MV, Bloch W, Sasaki T, Boukamp P, Zaucke F, Paulsson M, Nischt R (2012) Different domains in nidogen-1 and nidogen-2 drive basement membrane formation in skin organotypic cocultures. FASEB J 26:3637–3648 [DOI] [PubMed] [Google Scholar]
- Behrens DT, Villone D, Koch M, Brunner G, Sorokin L, Robenek H, Bruckner-Tuderman L, Bruckner P, Hansen U (2012) The epidermal basement membrane is a composite of separate laminin- or collagen IV-containing networks connected by aggregated perlecan, but not by nidogens. The Journal of biological chemistry 287:18700–18709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zvi A, Rodrigues MM, Krachmer JH, Fujikawa LS (1986) Immunohistochemical characterization of extracellular matrix in the developing human cornea. Current eye research 5:105–117 [DOI] [PubMed] [Google Scholar]
- Benya PD, Padilla SR (1986) Isolation and characterization of type VIII collagen synthesized by cultured rabbit corneal endothelial cells. A conventional structure replaces the interrupted-helix model. The Journal of biological chemistry 261:4160–4169 [PubMed] [Google Scholar]
- Bonod-Bidaud C, Roulet M, Hansen U, Elsheikh A, Malbouyres M, Ricard-Blum S, Faye C, Vaganay E, Rousselle P, Ruggiero F (2012) In vivo evidence for a bridging role of a collagen V subtype at the epidermis-dermis interface. J Invest Dermatol 132:1841–1849 [DOI] [PubMed] [Google Scholar]
- Boudreau NJ, Jones PL (1999) Extracellular matrix and integrin signalling: the shape of things to come. Biochem J 339 ( Pt 3):481–488 [PMC free article] [PubMed] [Google Scholar]
- Breitkreutz D, Bohnert A, Herzmann E, Bowden PE, Boukamp P, Fusenig NE (1984) Differentiation specific functions in cultured and transplanted mouse keratinocytes: environmental influences on ultrastructure and keratin expression. Differentiation 26:154–169 [DOI] [PubMed] [Google Scholar]
- Breitkreutz D, Koxholt I, Thiemann K, Nischt R (2013) Skin basement membrane: the foundation of epidermal integrity-BM functions and diverse roles of bridging molecules nidogen and perlecan. Biomed Res Int 2013:179784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitkreutz D, Schoop VM, Mirancea N, Baur M, Stark HJ, Fusenig NE (1998) Epidermal differentiation and basement membrane formation by HaCaT cells in surface transplants. Eur J Cell Biol 75:273–286 [DOI] [PubMed] [Google Scholar]
- Breitkreutz D, Stark HJ, Mirancea N, Tomakidi P, Steinbauer H, Fusenig NE (1997) Integrin and basement membrane normalization in mouse grafts of human keratinocytes--implications for epidermal homeostasis. Differentiation 61:195–209 [DOI] [PubMed] [Google Scholar]
- Bucher NL (1963) Regeneration of Mammalian Liver. Int Rev Cytol 15:245–300 [DOI] [PubMed] [Google Scholar]
- Cabrera S, Selman M, Lonzano-Bolanos A, Konishi K, Richards TJ, Kaminski N, Pardo A (2013) Gene expression profiles reveal molecular mechanisms involved in the progression and resolution of bleomycin-induced lung fibrosis. Am J Physiol Lung Cell Mol Physiol 304:L593–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron JD, Skubitz AP, Furcht LT (1991) Type IV collagen and corneal epithelial adhesion and migration. Effects of type IV collagen fragments and synthetic peptides on rabbit corneal epithelial cell adhesion and migration in vitro. Investigative ophthalmology & visual science 32:2766–2773 [PubMed] [Google Scholar]
- Carlin B, Jaffe R, Bender B, Chung AE (1981) Entactin, a novel basal lamina-associated sulfated glycoprotein. The Journal of biological chemistry 256:5209–5214 [PubMed] [Google Scholar]
- Carlson EC, Meezan E, Brendel K, Kenney MC (1981) Ultrastructural analyses of control and enzyme-treated isolated renal basement membranes. The Anatomical record 200:421–436 [DOI] [PubMed] [Google Scholar]
- Chaurasia SS, Kaur H, de Medeiros FW, Smith SD, Wilson SE (2009) Dynamics of the expression of intermediate filaments vimentin and desmin during myofibroblast differentiation after corneal injury. Experimental eye research 89:133–139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H, Qu J, Huang X, Kurundkar A, Zhu L, Yang N, Venado A, Ding Q, Liu G, Antony VB, Thannickal VJ, Zhou Y (2016) Mechanosensing by the alpha6-integrin confers an invasive fibroblast phenotype and mediates lung fibrosis. Nat Commun 7:12564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L, Hazlett LD (2001) Human corneal epithelial extracellular matrix perlecan serves as a site for Pseudomonas aeruginosa binding. Current eye research 22:19–27 [DOI] [PubMed] [Google Scholar]
- Chi HH, Teng CC, Katzin HM (1958) Histopathology of primary endothelial-epithelial dystrophy of the cornea. American journal of ophthalmology 45:518–535 [DOI] [PubMed] [Google Scholar]
- Chung AE, Freeman IL, Braginski JE (1977) A novel extracellular membrane elaborated by a mouse embryonal carcinoma-derived cell line. Biochemical and biophysical research communications 79:859–868 [DOI] [PubMed] [Google Scholar]
- Chung AE, Jaffe R, Freeman IL, Vergnes JP, Braginski JE, Carlin B (1979) Properties of a basement membrane-related glycoprotein synthesized in culture by a mouse embryonal carcinoma-derived cell line. Cell 16:277–287 [DOI] [PubMed] [Google Scholar]
- Costell M, Gustafsson E, Aszodi A, Morgelin M, Bloch W, Hunziker E, Addicks K, Timpl R, Fassler R (1999) Perlecan maintains the integrity of cartilage and some basement membranes. The Journal of cell biology 147:1109–1122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denzer AJ, Gesemann M, Schumacher B, Ruegg MA (1995) An amino-terminal extension is required for the secretion of chick agrin and its binding to extracellular matrix. The Journal of cell biology 131:1547–1560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derry CJ, Pusey CD (1994) Tissue-specific distribution of the Goodpasture antigen demonstrated by 2-D electrophoresis and western blotting. Nephrol Dial Transplant 9:355–361 [PubMed] [Google Scholar]
- Di Nunzio F, Maruggi G, Ferrari S, Di Iorio E, Poletti V, Garcia M, Del Rio M, De Luca M, Larcher F, Pellegrini G, Mavilio F (2008) Correction of laminin-5 deficiency in human epidermal stem cells by transcriptionally targeted lentiviral vectors. Mol Ther 16:1977–1985 [DOI] [PubMed] [Google Scholar]
- Dong S, Cole GJ, Halfter W (2003) Expression of collagen XVIII and localization of its glycosaminoglycan attachment sites. The Journal of biological chemistry 278:1700–1707 [DOI] [PubMed] [Google Scholar]
- El Ghalbzouri A, Jonkman MF, Dijkman R, Ponec M (2005) Basement membrane reconstruction in human skin equivalents is regulated by fibroblasts and/or exogenously activated keratinocytes. J Invest Dermatol 124:79–86 [DOI] [PubMed] [Google Scholar]
- El Ghalbzouri A, Ponec M (2004) Diffusible factors released by fibroblasts support epidermal morphogenesis and deposition of basement membrane components. Wound Repair Regen 12:359–367 [DOI] [PubMed] [Google Scholar]
- Ettner N, Gohring W, Sasaki T, Mann K, Timpl R (1998) The N-terminal globular domain of the laminin alpha1 chain binds to alpha1beta1 and alpha2beta1 integrins and to the heparan sulfate-containing domains of perlecan. FEBS Lett 430:217–221 [DOI] [PubMed] [Google Scholar]
- Filenius S, Hormia M, Rissanen J, Burgeson RE, Yamada Y, Araki-Sasaki K, Nakamura M, Virtanen I, Tervo T (2001) Laminin synthesis and the adhesion characteristics of immortalized human corneal epithelial cells to laminin isoforms. Experimental eye research 72:93–103 [DOI] [PubMed] [Google Scholar]
- Fini ME (1999) Keratocyte and fibroblast phenotypes in the repairing cornea. Prog Retin Eye Res 18:529–551 [DOI] [PubMed] [Google Scholar]
- Fleischmajer R, Schechter A, Bruns M, Perlish JS, Macdonald ED, Pan TC, Timpl R, Chu ML (1995) Skin fibroblasts are the only source of nidogen during early basal lamina formation in vitro. J Invest Dermatol 105:597–601 [DOI] [PubMed] [Google Scholar]
- Fox JW, Mayer U, Nischt R, Aumailley M, Reinhardt D, Wiedemann H, Mann K, Timpl R, Krieg T, Engel J, et al. (1991) Recombinant nidogen consists of three globular domains and mediates binding of laminin to collagen type IV. The EMBO journal 10:3137–3146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritsch A, Spassov S, Elfert S, Schlosser A, Gache Y, Meneguzzi G, Bruckner-Tuderman L (2009) Dominant-negative effects of COL7A1 mutations can be rescued by controlled overexpression of normal collagen VII. The Journal of biological chemistry 284:30248–30256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukai N, Eklund L, Marneros AG, Oh SP, Keene DR, Tamarkin L, Niemela M, Ilves M, Li E, Pihlajaniemi T, Olsen BR (2002) Lack of collagen XVIII/endostatin results in eye abnormalities. The EMBO journal 21:1535–1544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuyama A, Kimata K, Mochitate K (1997) Assembly of basement membrane in vitro by cooperation between alveolar epithelial cells and pulmonary fibroblasts. Cell Struct Funct 22:603–614 [DOI] [PubMed] [Google Scholar]
- Gersdorff N, Kohfeldt E, Sasaki T, Timpl R, Miosge N 2005. Laminin gamma3 chain binds to nidogen and is located in murine basement membranes. J Biol Chem 280:22146–53 [DOI] [PubMed] [Google Scholar]
- Gersdorff N, Otto S, Roediger M, Kruegel J, Miosge N 2007. The absence of one or both nidogens does not alter basement membrane composition in adult murine kidney. Histol Histopathol. 22:1077–84 [DOI] [PubMed] [Google Scholar]
- Gipson IK, Spurr-Michaud SJ, Tisdale AS (1988) Hemidesmosomes and anchoring fibril collagen appear synchronously during development and wound healing. Dev Biol 126:253–262 [DOI] [PubMed] [Google Scholar]
- Groffen AJ, Ruegg MA, Dijkman H, van de Velden TJ, Buskens CA, van den Born J, Assmann KJ, Monnens LA, Veerkamp JH, van den Heuvel LP (1998) Agrin is a major heparan sulfate proteoglycan in the human glomerular basement membrane. J Histochem Cytochem 46:19–27 [DOI] [PubMed] [Google Scholar]
- Gubler MC (2008) Inherited diseases of the glomerular basement membrane. Nat Clin Pract Nephrol 4:24–37 [DOI] [PubMed] [Google Scholar]
- Hahn E, Wick G, Pencev D, Timpl R (1980) Distribution of basement membrane proteins in normal and fibrotic human liver: collagen type IV, laminin, and fibronectin. Gut 21:63–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halfter W, Dong S, Schurer B, Cole GJ (1998) Collagen XVIII is a basement membrane heparan sulfate proteoglycan. The Journal of biological chemistry 273:25404–25412 [DOI] [PubMed] [Google Scholar]
- Halfter W, Oertle P, Monnier CA, Camenzind L, Reyes-Lua M, Hu H, Candiello J, Labilloy A, Balasubramani M, Henrich PB, Plodinec M (2015) New concepts in basement membrane biology. FEBS J 282:4466–4479 [DOI] [PubMed] [Google Scholar]
- Hammers CM, Stanley JR (2016) Mechanisms of Disease: Pemphigus and Bullous Pemphigoid. Annu Rev Pathol. 11:175–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey SJ, Jarad G, Cunningham J, Rops AL, van der Vlag J, Berden JH, Moeller MJ, Holzman LB, Burgess RW, Miner JH (2007) Disruption of glomerular basement membrane charge through podocyte-specific mutation of agrin does not alter glomerular permselectivity. The American journal of pathology 171:139–152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassell JR, Birk DE (2010) The molecular basis of corneal transparency. Experimental eye research 91:326–335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassell JR, Robey PG, Barrach HJ, Wilczek J, Rennard SI, Martin GR (1980) Isolation of a heparan sulfate-containing proteoglycan from basement membrane. Proc Natl Acad Sci U S A 77:4494–4498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassell JR, Schrecengost PK, Rada JA, SundarRaj N, Sossi G, Thoft RA (1992) Biosynthesis of stromal matrix proteoglycans and basement membrane components by human corneal fibroblasts. Investigative ophthalmology & visual science 33:547–557 [PubMed] [Google Scholar]
- Heidet L, Cai Y, Guicharnaud L, Antignac C, Gubler MC (2000) Glomerular expression of type IV collagen chains in normal and X-linked Alport syndrome kidneys. The American journal of pathology 156:1901–1910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho MS, Bose K, Mokkapati S, Nischt R, Smyth N (2008) Nidogens-Extracellular matrix linker molecules. Microsc Res Tech 71:387–395 [DOI] [PubMed] [Google Scholar]
- Inomata T, Ebihara N, Funaki T, Matsuda A, Watanabe Y, Ning L, Xu Z, Murakami A, Arikawa-Hirasawa E (2012) Perlecan-deficient mutation impairs corneal epithelial structure. Investigative ophthalmology & visual science 53:1277–1284 [DOI] [PubMed] [Google Scholar]
- Ishizaki M, Zhu G, Haseba T, Shafer SS, Kao WW (1993) Expression of collagen I, smooth muscle alpha-actin, and vimentin during the healing of alkali-burned and lacerated corneas. Investigative ophthalmology & visual science 34:3320–3328 [PubMed] [Google Scholar]
- Jester JV, Huang J, Barry-Lane PA, Kao WW, Petroll WM, Cavanagh HD (1999) Transforming growth factor(beta)-mediated corneal myofibroblast differentiation requires actin and fibronectin assembly. Investigative ophthalmology & visual science 40:1959–1967 [PubMed] [Google Scholar]
- Jester JV, Huang J, Petroll WM, Cavanagh HD (2002) TGFbeta induced myofibroblast differentiation of rabbit keratocytes requires synergistic TGFbeta, PDGF and integrin signaling. Experimental eye research 75:645–657 [DOI] [PubMed] [Google Scholar]
- Jester JV, Petroll WM, Barry PA, Cavanagh HD (1995) Temporal, 3-dimensional, cellular anatomy of corneal wound tissue. Journal of anatomy 186 ( Pt 2):301–311 [PMC free article] [PubMed] [Google Scholar]
- Jester JV, Rodrigues MM, Herman IM (1987) Characterization of avascular corneal wound healing fibroblasts. New insights into the myofibroblast. The American journal of pathology 127:140–148 [PMC free article] [PubMed] [Google Scholar]
- Johnson DH, Bourne WM, Campbell RJ (1982) The ultrastructure of Descemet’s membrane. II. Aphakic bullous keratopathy. Archives of ophthalmology 100:1948–1951 [DOI] [PubMed] [Google Scholar]
- Kabosova A, Azar DT, Bannikov GA, Campbell KP, Durbeej M, Ghohestani RF, Jones JC, Kenney MC, Koch M, Ninomiya Y, Patton BL, Paulsson M, Sado Y, Sage EH, Sasaki T, Sorokin LM, Steiner-Champliaud MF, Sun TT, Sundarraj N, Timpl R, Virtanen I, Ljubimov AV (2007) Compositional differences between infant and adult human corneal basement membranes. Investigative ophthalmology & visual science 48:4989–4999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanwar YS, Danesh FR, Chugh SS (2007) Contribution of proteoglycans towards the integrated functions of renal glomerular capillaries: a historical perspective. The American journal of pathology 171:9–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapoor R, Bornstein P, Sage EH (1986) Type VIII collagen from bovine Descemet’s membrane: structural characterization of a triple-helical domain. Biochemistry 25:3930–3937 [DOI] [PubMed] [Google Scholar]
- Kaur H, Chaurasia SS, Agrawal V, Suto C, Wilson SE (2009) Corneal myofibroblast viability: opposing effects of IL-1 and TGF beta1. Experimental eye research 89:152–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kefalides NA, Cameron JD, Tomichek EA, Yanoff M (1976) Biosynthesis of basement membrane collagen by rabbit corneal endothelium in vitro. The Journal of biological chemistry 251:730–733 [PubMed] [Google Scholar]
- Kefalides NA, Denduchis B (1969) Structural components of epithelial and endothelial basement membranes. Biochemistry 8:4613–4621 [DOI] [PubMed] [Google Scholar]
- Khoshnoodi J, Pedchenko V, Hudson BG (2008) Mammalian collagen IV. Microsc Res Tech 71:357–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimura N, Toyoshima T, Kojima T, Shimane M (1998) Entactin-2: a new member of basement membrane protein with high homology to entactin/nidogen. Exp Cell Res 241:36–45 [DOI] [PubMed] [Google Scholar]
- Kleinman HK, Martin GR (2005) Matrigel: basement membrane matrix with biological activity. Semin Cancer Biol 15:378–386 [DOI] [PubMed] [Google Scholar]
- Kleinman HK, McGarvey ML, Liotta LA, Robey PG, Tryggvason K, Martin GR (1982) Isolation and characterization of type IV procollagen, laminin, and heparan sulfate proteoglycan from the EHS sarcoma. Biochemistry 21:6188–6193 [DOI] [PubMed] [Google Scholar]
- Kruegel J, Miosge N 2012. Basement membrane components are key players in specialized extracellular matrices. Cell Mol Life Sci. 67:2879–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labermeier U, Kenney MC (1983) The presence of EC collagen and type IV collagen in bovine Descemet’s membranes. Biochemical and biophysical research communications 116:619–625 [DOI] [PubMed] [Google Scholar]
- Lawson WE, Polosukhin VV, Stathopoulos GT, Zoia O, Han W, Lane KB, Li B, Donnelly EF, Holburn GE, Lewis KG, Collins RD, Hull WM, Glasser SW, Whitsett JA, Blackwell TS (2005) Increased and prolonged pulmonary fibrosis in surfactant protein C-deficient mice following intratracheal bleomycin. The American journal of pathology 167:1267–1277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBleu VS, Macdonald B, Kalluri R (2007) Structure and function of basement membranes. Experimental biology and medicine 232:1121–1129 [DOI] [PubMed] [Google Scholar]
- Lemaire R, Burwell T, Sun H, Delaney T, Bakken J, Cheng L, Rebelatto MC, Czapiga M, de-Mendez I, Coyle AJ, Herbst R, Lafyatis R, Connor J (2016) Resolution of Skin Fibrosis by Neutralization of the Antifibrinolytic Function of Plasminogen Activator Inhibitor 1. Arthritis Rheumatol 68:473–483 [DOI] [PubMed] [Google Scholar]
- Li M, Krishnaveni MS, Li C, Zhou B, Xing Y, Banfalvi A, Li A, Lombardi V, Akbari O, Borok Z, Minoo P (2011) Epithelium-specific deletion of TGF-beta receptor type II protects mice from bleomycin-induced pulmonary fibrosis. J Clin Invest 121:277–287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limat A, Stockhammer E, Breitkreutz D, Schaffner T, Egelrud T, Salomon D, Fusenig NE, Braathen LR, Hunziker T (1996) Endogeneously regulated site-specific differentiation of human palmar skin keratinocytes in organotypic cocultures and in nude mouse transplants. Eur J Cell Biol 69:245–258 [PubMed] [Google Scholar]
- Lin HC, Chang JH, Jain S, Gabison EE, Kure T, Kato T, Fukai N, Azar DT (2001) Matrilysin cleavage of corneal collagen type XVIII NC1 domain and generation of a 28-kDa fragment. Investigative ophthalmology & visual science 42:2517–2524 [PubMed] [Google Scholar]
- Ljubimov AV, Burgeson RE, Butkowski RJ, Michael AF, Sun TT, Kenney MC (1995) Human corneal basement membrane heterogeneity: topographical differences in the expression of type IV collagen and laminin isoforms. Laboratory investigation; a journal of technical methods and pathology 72:461–473 [PubMed] [Google Scholar]
- Maatta M, Heljasvaara R, Pihlajaniemi T, Uusitalo M (2007) Collagen XVIII/endostatin shows a ubiquitous distribution in human ocular tissues and endostatin-containing fragments accumulate in ocular fluid samples. Graefe’s archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie 245:74–81 [DOI] [PubMed] [Google Scholar]
- Mak KM, Chen LL, Lee TF (2013) Codistribution of collagen type IV and laminin in liver fibrosis of elderly cadavers: immunohistochemical marker of perisinusoidal basement membrane formation. Anat Rec (Hoboken) 296:953–964 [DOI] [PubMed] [Google Scholar]
- Mak KM, Mei R (2017) Basement Membrane Type IV Collagen and Laminin: An Overview of Their Biology and Value as Fibrosis Biomarkers of Liver Disease. Anat Rec (Hoboken) 300:1371–1390 [DOI] [PubMed] [Google Scholar]
- Marinkovich MP, Keene DR, Rimberg CS, Burgeson RE (1993) Cellular origin of the dermal epidermal basement membrane. Dev Dyn 197:255–267 [DOI] [PubMed] [Google Scholar]
- Marino GK, Santhiago MR, Santhanam A, Lassance L, Thangavadivel S, Medeiros CS, Bose K, Tam KP, Wilson SE (2017a) Epithelial basement membrane injury and regeneration modulates corneal fibrosis after pseudomonas corneal ulcers in rabbits. Experimental eye research 161:101–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marino GK, Santhiago MR, Santhanam A, Torricelli AAM, Wilson SE (2017b) Regeneration of Defective Epithelial Basement Membrane and Restoration of Corneal Transparency After Photorefractive Keratectomy. J Refract Surg 33:337–346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marneros AG, Keene DR, Hansen U, Fukai N, Moulton K, Goletz PL, Moiseyev G, Pawlyk BS, Halfter W, Dong S, Shibata M, Li T, Crouch RK, Bruckner P, Olsen BR (2004) Collagen XVIII/endostatin is essential for vision and retinal pigment epithelial function. The EMBO journal 23:89–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marneros AG, Olsen BR (2003) Age-dependent iris abnormalities in collagen XVIII/endostatin deficient mice with similarities to human pigment dispersion syndrome. Investigative ophthalmology & visual science 44:2367–2372 [DOI] [PubMed] [Google Scholar]
- Martinez-Hernandez A, Amenta PS (1995) The extracellular matrix in hepatic regeneration. FASEB J 9:1401–1410 [DOI] [PubMed] [Google Scholar]
- Matejas V, Hinkes B, Alkandari F, Al-Gazali L, Annexstad E, Aytac MB, Barrow M, Blahova K, Bockenhauer D, Cheong HI, Maruniak-Chudek I, Cochat P, Dotsch J, Gajjar P, Hennekam RC, Janssen F, Kagan M, Kariminejad A, Kemper MJ, Koenig J, Kogan J, Kroes HY, Kuwertz-Broking E, Lewanda AF, Medeira A, Muscheites J, Niaudet P, Pierson M, Saggar A, Seaver L, Suri M, Tsygin A, Wuhl E, Zurowska A, Uebe S, Hildebrandt F, Antignac C, Zenker M (2010) Mutations in the human laminin beta2 (LAMB2) gene and the associated phenotypic spectrum. Human mutation 31:992–1002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumoto S, Yamamoto K, Nagano T, Okamoto R, Ibuki N, Tagashira M, Tsuji T (1999) Immunohistochemical study on phenotypical changes of hepatocytes in liver disease with reference to extracellular matrix composition. Liver 19:32–38 [DOI] [PubMed] [Google Scholar]
- May CA (2012) Distribution of nidogen in the murine eye and ocular phenotype of the nidogen-1 knockout mouse. ISRN ophthalmology 2012:378641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medeiros CS, Lassance L, Saikia P, Wilson SE (2018). Posterior stromal keratocyte apoptosis triggered by mechanical endothelial injury and nidogen-1 production in the cornea. Exp. Eye Res. 172:30–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menzel O, Bekkeheien RC, Reymond A, Fukai N, Boye E, Kosztolanyi G, Aftimos S, Deutsch S, Scott HS, Olsen BR, Antonarakis SE, Guipponi M (2004) Knobloch syndrome: novel mutations in COL18A1, evidence for genetic heterogeneity, and a functionally impaired polymorphism in endostatin. Human mutation 23:77–84 [DOI] [PubMed] [Google Scholar]
- Michelacci YM (2003) Collagens and proteoglycans of the corneal extracellular matrix. Brazilian journal of medical and biological research = Revista brasileira de pesquisas medicas e biologicas 36:1037–1046 [DOI] [PubMed] [Google Scholar]
- Miner JH (2012) The glomerular basement membrane. Exp Cell Res 318:973–978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miner JH, Li C (2000) Defective glomerulogenesis in the absence of laminin alpha5 demonstrates a developmental role for the kidney glomerular basement membrane. Dev Biol 217:278–289 [DOI] [PubMed] [Google Scholar]
- Miner JH, Patton BL, Lentz SI, Gilbert DJ, Snider WD, Jenkins NA, Copeland NG, Sanes JR (1997) The laminin alpha chains: expression, developmental transitions, and chromosomal locations of alpha1–5, identification of heterotrimeric laminins 8–11, and cloning of a novel alpha3 isoform. The Journal of cell biology 137:685–701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miner JH, Sanes JR (1994) Collagen IV alpha 3, alpha 4, and alpha 5 chains in rodent basal laminae: sequence, distribution, association with laminins, and developmental switches. The Journal of cell biology 127:879–891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miner JH, Yurchenco PD (2004) Laminin functions in tissue morphogenesis. Annu Rev Cell Dev Biol 20:255–284 [DOI] [PubMed] [Google Scholar]
- Miosge N, Sasaki T, Timpl R (2002) Evidence of nidogen-2 compensation for nidogen-1 deficiency in transgenic mice. Matrix biology : journal of the International Society for Matrix Biology 21:611–621 [DOI] [PubMed] [Google Scholar]
- Miosge N, Simniok T, Sprysch P, Herken R (2003) The collagen type XVIII endostatin domain is co-localized with perlecan in basement membranes in vivo. J Histochem Cytochem 51:285–296 [DOI] [PubMed] [Google Scholar]
- Mirancea N, Hausser I, Metze D, Stark HJ, Boukamp P, Breitkreutz D (2007) Junctional basement membrane anomalies of skin and mucosa in lipoid proteinosis (hyalinosis cutis et mucosae). J Dermatol Sci 45:175–185 [DOI] [PubMed] [Google Scholar]
- Mohan RR, Hutcheon AE, Choi R, Hong J, Lee J, Mohan RR, Ambrosio R Jr., Zieske JD, Wilson SE (2003) Apoptosis, necrosis, proliferation, and myofibroblast generation in the stroma following LASIK and PRK. Experimental eye research 76:71–87 [DOI] [PubMed] [Google Scholar]
- Mokkapati S, Bechtel M, Reibetanz M, Miosge N, Nischt R (2012) Absence of the basement membrane component nidogen 2, but not of nidogen 1, results in increased lung metastasis in mice. J Histochem Cytochem. 60:280–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller MM, Fusenig NE (2004) Friends or foes - bipolar effects of the tumour stroma in cancer. Nat Rev Cancer 4:839–849 [DOI] [PubMed] [Google Scholar]
- Murauer EM, Gache Y, Gratz IK, Klausegger A, Muss W, Gruber C, Meneguzzi G, Hintner H, Bauer JW (2011) Functional correction of type VII collagen expression in dystrophic epidermolysis bullosa. J Invest Dermatol 131:74–83 [DOI] [PubMed] [Google Scholar]
- Murphy C, Alvarado J, Juster R (1984) Prenatal and postnatal growth of the human Descemet’s membrane. Investigative ophthalmology & visual science 25:1402–1415 [PubMed] [Google Scholar]
- Netto MV, Mohan RR, Sinha S, Sharma A, Dupps W, Wilson SE (2006) Stromal haze, myofibroblasts, and surface irregularity after PRK. Experimental eye research 82:788–797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nystrom A, Bornert O, Kuhl T (2017) Cell therapy for basement membrane-linked diseases. Matrix biology : journal of the International Society for Matrix Biology 57–58:124–139 [DOI] [PubMed] [Google Scholar]
- Orkin RW, Gehron P, McGoodwin EB, Martin GR, Valentine T, Swarm R (1977) A murine tumor producing a matrix of basement membrane. J Exp Med 145:204–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulsson M (1988) The role of Ca2+ binding in the self-aggregation of laminin-nidogen complexes. The Journal of biological chemistry 263:5425–5430 [PubMed] [Google Scholar]
- Poschl E, Schlotzer-Schrehardt U, Brachvogel B, Saito K, Ninomiya Y, Mayer U (2004) Collagen IV is essential for basement membrane stability but dispensable for initiation of its assembly during early development. Development 131:1619–1628 [DOI] [PubMed] [Google Scholar]
- Qiao H, Shibaki A, Long HA, Wang G, Li Q, Nishie W, Abe R, Akiyama M, Shimizu H, McMillan JR (2009) Collagen XVII participates in keratinocyte adhesion to collagen IV, and in p38MAPK-dependent migration and cell signaling. J Invest Dermatol 129:2288–2295 [DOI] [PubMed] [Google Scholar]
- Reiser J, Altintas MM.(2016) Podocytes. F1000Res. 28:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryu M, Mulay SR, Miosge N, Gross O, Anders HJ (2012) Tumour necrosis factor-α drives Alport glomerulosclerosis in mice by promoting podocyte apoptosis. J Pathol. 226:120–31 [DOI] [PubMed] [Google Scholar]
- Saarela J, Ylikarppa R, Rehn M, Purmonen S, Pihlajaniemi T (1998) Complete primary structure of two variant forms of human type XVIII collagen and tissue-specific differences in the expression of the corresponding transcripts. Matrix biology : journal of the International Society for Matrix Biology 16:319–328 [DOI] [PubMed] [Google Scholar]
- Sage H, Pritzl P, Bornstein P (1981) Secretory phenotypes of endothelial cells in culture: comparison of aortic, venous, capillary, and corneal endothelium. Arteriosclerosis 1:427–442 [DOI] [PubMed] [Google Scholar]
- Salmivirta K, Talts JF, Olsson M, Sasaki T, Timpl R, Ekblom P (2002) Binding of mouse nidogen-2 to basement membrane components and cells and its expression in embryonic and adult tissues suggest complementary functions of the two nidogens. Exp Cell Res 279:188–201 [DOI] [PubMed] [Google Scholar]
- Sannes PL, Wang J (1997) Basement membranes and pulmonary development. Exp Lung Res. 23:101–8 [DOI] [PubMed] [Google Scholar]
- Santhanam A, Marino GK, Torricelli AA, Wilson SE (2017) EBM regeneration and changes in EBM component mRNA expression in stromal cells after corneal injury. Molecular vision 23:39–51 [PMC free article] [PubMed] [Google Scholar]
- Santhanam A, Torricelli AA, Wu J, Marino GK, Wilson SE (2015) Differential expression of epithelial basement membrane components nidogens and perlecan in corneal stromal cells in vitro. Molecular vision 21:1318–1327 [PMC free article] [PubMed] [Google Scholar]
- Sawada H (1982) The fine structure of the bovine Descemet’s membrane with special reference to biochemical nature. Cell and tissue research 226:241–255 [DOI] [PubMed] [Google Scholar]
- Schaffner F, Poper H (1963) Capillarization of hepatic sinusoids in man. Gastroenterology 44:239–242 [PubMed] [Google Scholar]
- Schubert D, Kimura H (1991) Substratum-growth factor collaborations are required for the mitogenic activities of activin and FGF on embryonal carcinoma cells. The Journal of cell biology 114:841–846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuttleworth CA (1997) Type VIII collagen. The international journal of biochemistry & cell biology 29:1145–1148 [DOI] [PubMed] [Google Scholar]
- Simon-Assmann P, Lefebvre O, Bellissent-Waydelich A, Olsen J, Orian-Rousseau V, De Arcangelis A (1998) The laminins: role in intestinal morphogenesis and differentiation. Ann N Y Acad Sci 859:46–64 [DOI] [PubMed] [Google Scholar]
- Smola H, Stark HJ, Thiekotter G, Mirancea N, Krieg T, Fusenig NE (1998) Dynamics of basement membrane formation by keratinocyte-fibroblast interactions in organotypic skin culture. Exp Cell Res 239:399–410 [DOI] [PubMed] [Google Scholar]
- Smyth N, Vatansever HS, Murray P, Meyer M, Frie C, Paulsson M, Edgar D (1999) Absence of basement membranes after targeting the LAMC1 gene results in embryonic lethality due to failure of endoderm differentiation. The Journal of cell biology 144:151–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnenberg A, Calafat J, Janssen H, Daams H, van der Raaij-Helmer LM, Falcioni R, Kennel SJ, Aplin JD, Baker J, Loizidou M, et al. (1991) Integrin alpha 6/beta 4 complex is located in hemidesmosomes, suggesting a major role in epidermal cell-basement membrane adhesion. The Journal of cell biology 113:907–917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark HJ, Baur M, Breitkreutz D, Mirancea N, Fusenig NE (1999) Organotypic keratinocyte cocultures in defined medium with regular epidermal morphogenesis and differentiation. J Invest Dermatol 112:681–691 [DOI] [PubMed] [Google Scholar]
- Sterk LM, Geuijen CA, Oomen LC, Calafat J, Janssen H, Sonnenberg A (2000) The tetraspan molecule CD151, a novel constituent of hemidesmosomes, associates with the integrin alpha6beta4 and may regulate the spatial organization of hemidesmosomes. The Journal of cell biology 149:969–982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterk LM, Geuijen CA, van den Berg JG, Claessen N, Weening JJ, Sonnenberg A (2002) Association of the tetraspanin CD151 with the laminin-binding integrins alpha3beta1, alpha6beta1, alpha6beta4 and alpha7beta1 in cells in culture and in vivo. J Cell Sci 115:1161–1173 [DOI] [PubMed] [Google Scholar]
- Strieter RM, Mehrad B (2009) New mechanisms of pulmonary fibrosis. Chest 136:1364–1370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugawara K, Tsuruta D, Ishii M, Jones JC, Kobayashi H (2008) Laminin-332 and −511 in skin. Exp Dermatol 17:473–480 [DOI] [PubMed] [Google Scholar]
- Suzuki OT, Sertie AL, Der Kaloustian VM, Kok F, Carpenter M, Murray J, Czeizel AE, Kliemann SE, Rosemberg S, Monteiro M, Olsen BR, Passos-Bueno MR (2002) Molecular analysis of collagen XVIII reveals novel mutations, presence of a third isoform, and possible genetic heterogeneity in Knobloch syndrome. American journal of human genetics 71:1320–1329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tervo K, Tervo T, van Setten GB, Virtanen I (1991) Integrins in human corneal epithelium. Cornea 10:461–465 [DOI] [PubMed] [Google Scholar]
- Tiedemann K, Sasaki T, Gustafsson E, Gohring W, Batge B, Notbohm H, Timpl R, Wedel T, Schlotzer-Schrehardt U, Reinhardt DP (2005) Microfibrils at basement membrane zones interact with perlecan via fibrillin-1. The Journal of biological chemistry 280:11404–11412 [DOI] [PubMed] [Google Scholar]
- Timpl R (1989) Structure and biological activity of basement membrane proteins. Eur J Biochem 180:487–502 [DOI] [PubMed] [Google Scholar]
- Timpl R, Brown JC (1996) Supramolecular assembly of basement membranes. Bioessays 18:123–132 [DOI] [PubMed] [Google Scholar]
- Timpl R, Rohde H, Robey PG, Rennard SI, Foidart JM, Martin GR (1979) Laminin--a glycoprotein from basement membranes. The Journal of biological chemistry 254:9933–9937 [PubMed] [Google Scholar]
- Torricelli AA, Marino GK, Santhanam A, Wu J, Singh A, Wilson SE (2015) Epithelial basement membrane proteins perlecan and nidogen-2 are up-regulated in stromal cells after epithelial injury in human corneas. Experimental eye research 134:33–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torricelli AA, Singh V, Agrawal V, Santhiago MR, Wilson SE (2013a) Transmission electron microscopy analysis of epithelial basement membrane repair in rabbit corneas with haze. Investigative ophthalmology & visual science 54:4026–4033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torricelli AA, Singh V, Santhiago MR, Wilson SE (2013b) The corneal epithelial basement membrane: structure, function, and disease. Investigative ophthalmology & visual science 54:6390–6400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsen G, Halfter W, Kroger S, Cole GJ (1995) Agrin is a heparan sulfate proteoglycan. The Journal of biological chemistry 270:3392–3399 [DOI] [PubMed] [Google Scholar]
- Tuli SS, Liu R, Chen C, Blalock TD, Goldstein M, Schultz GS (2006) Immunohistochemical localization of EGF, TGF-alpha, TGF-beta, and their receptors in rat corneas during healing of excimer laser ablation. Current eye research 31:709–719 [DOI] [PubMed] [Google Scholar]
- Tuori A, Uusitalo H, Burgeson RE, Terttunen J, Virtanen I (1996) The immunohistochemical composition of the human corneal basement membrane. Cornea 15:286–294 [DOI] [PubMed] [Google Scholar]
- Uitto J, Has C, Vahidnezhad H, Youssefian L, Bruckner-Tuderman L (2017) Molecular pathology of the basement membrane zone in heritable blistering diseases:: The paradigm of epidermolysis bullosa. Matrix Biol. 57–58:76–85 [DOI] [PubMed] [Google Scholar]
- Vaccaro CA, Brody JS (1981) Structural features of alveolar wall basement membrane in the adult rat lung. The Journal of cell biology 91:427–437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villone D, Fritsch A, Koch M, Bruckner-Tuderman L, Hansen U, Bruckner P (2008) Supramolecular interactions in the dermo-epidermal junction zone: anchoring fibril-collagen VII tightly binds to banded collagen fibrils. The Journal of biological chemistry 283:24506–24513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virtanen I, Tervo K, Korhonen M, Paallysaho T, Tervo T (1992) Integrins as receptors for extracellular matrix proteins in human cornea. Acta ophthalmologica Supplement 18–21 [DOI] [PubMed] [Google Scholar]
- Voskarides K, Damianou L, Neocleous V, Zouvani I, Christodoulidou S, Hadjiconstantinou V, Ioannou K, Athanasiou Y, Patsias C, Alexopoulos E, Pierides A, Kyriacou K, Deltas C (2007) COL4A3/COL4A4 mutations producing focal segmental glomerulosclerosis and renal failure in thin basement membrane nephropathy. Journal of the American Society of Nephrology : JASN 18:3004–3016 [DOI] [PubMed] [Google Scholar]
- Weibel ER (1973) Morphological basis of alveolar-capillary gas exchange. Physiol Rev 53:419–495 [DOI] [PubMed] [Google Scholar]
- Wells RG (2008) Cellular sources of extracellular matrix in hepatic fibrosis. Clin Liver Dis 12:759–768, viii [DOI] [PMC free article] [PubMed] [Google Scholar]
- West JB, Mathieu-Costello O (1999) Structure, strength, failure, and remodeling of the pulmonary blood-gas barrier. Annu Rev Physiol. 61:543–72. [DOI] [PubMed] [Google Scholar]
- Wilson SE (2012) Corneal myofibroblast biology and pathobiology: generation, persistence, and transparency. Experimental eye research 99:78–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson SE, Chaurasia SS, Medeiros FW (2007) Apoptosis in the initiation, modulation and termination of the corneal wound healing response. Experimental eye research 85:305–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson SE, He YG, Weng J, Li Q, McDowall AW, Vital M, Chwang EL (1996) Epithelial injury induces keratocyte apoptosis: hypothesized role for the interleukin-1 system in the modulation of corneal tissue organization and wound healing. Experimental eye research 62:325–327 [DOI] [PubMed] [Google Scholar]
- Wilson SE, Marino GK, Torricelli AAM, Medeiros CS (2017) Injury and defective regeneration of the epithelial basement membrane in corneal fibrosis: A paradigm for fibrosis in other organs? Matrix biology : journal of the International Society for Matrix Biology 64:17–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yurchenco PD, Tsilibary EC, Charonis AS, Furthmayr H (1986) Models for the self-assembly of basement membrane. J Histochem Cytochem 34:93–102 [DOI] [PubMed] [Google Scholar]
- Zhang J, Patel DV (2015) The pathophysiology of Fuchs’ endothelial dystrophy--a review of molecular and cellular insights. Experimental eye research 130:97–105 [DOI] [PubMed] [Google Scholar]