Abstract
Introduction
A lot of different techniques have been proposed in order to manage abduction limitation secondary to sixth nerve palsy; however, anterior segment ischemia remains a concern. The aim of this study was to evaluate the results of augmented vertical recti muscle transposition (VRT) with partial recession of medial rectus muscle (MR) for complete, chronic sixth nerve palsy, a new modified technique that could also minimize the risk for anterior segment ischemia (ASI).
Methods
In this nonrandomized 8-year (2009–2017) retrospective review, 20 patients with complete sixth nerve palsy and contracted MR were enrolled. All of them underwent augmented VRT and partial recession of the MR, following a new proposed surgical technique. Only the central part of the MR tendon and belly was recessed by 6.5 mm, leaving 1.5 mm of the upper pole and 1.5 mm of the lower pole of the muscle intact, preserving the circulation of two anterior ciliary arteries.
Results
Twenty patients with a mean age of 43 years (range 12–71), all unilateral cases, were enrolled in this study. The mean preoperative deviation was 64.25 ± 10.9 prism diopters (PD) base out (range 50 to 90). In 17 cases (88%), the postoperative deviation was within 10 PD of orthotropia. Two patients (10%) had residual esotropia (15 PD and 20 PD, respectively), and one patient (5%) had 10 PD of hypotropia. The mean preoperative abduction limitation of −5.9 improved to −3.1 (p < 0.0001). None of the cases presented with ASI (success rate 100%).
Conclusion
Partial recession of the MR preserving the two anterior ciliary arteries (Kozeis modified technique) with augmented vertical recti muscle transposition is an effective procedure, with a high success rate and is probably less risky for ASI.
Keywords: Anterior segment ischemia, Sixth nerve palsy, Surgery
Introduction
By definition, patients with complete sixth nerve palsy present with esotropia, limitation of abduction, diplopia in primary position and abnormal head posture in many cases. Various surgical procedures have been described to manage this condition, including partial or full vertical recti muscles transposition (VRT), with and without weakening of the medial rectus muscle (MR) of the affected eye. Full VRT with Foster’s augmented sutures, is among the most effective treatments [1], especially in severe and long-standing cases, being combined with MR weakening, due to the contracture of this muscle. However, simultaneous operation on MR and both vertical recti muscles in the same eye carries a high risk for ASI [2].
In this study, we describe a new technique (Kozeis modified technique) of MR weakening (by partial recession) plus augmented full transposition of vertical recti muscles, in order to maintain a high surgical success rate and to possibly minimize the risks for ASI in complete sixth nerve palsy.
Methods
In this nonrandomized 8-year (2009–2017) retrospective review, 20 patients with complete sixth nerve palsy and contracted MR were enrolled. Eight were males and 12 females, with a mean age of 43 years (range 12–71), and unilateral complete sixth nerve palsy with contracted MR. The study was not registered as a clinical trial since it is a nonrandomized retrospective review, but it was conducted according to the tenets of the Declaration of Helsinki and was approved by the Ophthalmica Eye Institute Ethics Committee. The inclusion criteria of the study are presented in Table 1. All patients signed an informed consent preoperatively. Complete sixth nerve palsy was defined as the deficient abduction beyond the midline and included a positive forced duction test. According to our records, the etiology of the palsy was classified as traumatic (7), tumor-related (4), vascular (7) and viral (2).
Table 1.
Inclusion criteria for patients with complete sixth nerve palsy
| Inclusion criteria |
|---|
| Complete sixth nerve palsy |
| Stable strabismus angle > 6 months |
| No previous operation/Botox |
| No medications influencing the muscular tone |
| Forced duction test (+) |
| Best corrected visual acuity of the affected eye better than 6/60 |
| Postoperative follow up ≥ 12 months |
All patients were operated upon at least 6 months from the onset of the nerve palsy, by one surgeon, the senior author (NK).
Patients who had at least 12 months of follow-up were included in the analysis. Patients with prior strabismus surgery or on medications affecting the muscular tone were excluded. The pre- and postoperative deviation was measured by using the prism cover–uncover test asking the patient to fix at a 3-m far target. The pre- and postoperative abduction limitation was also graded from −8 (no abduction at all), −4 (abduction up to midline), to 0 (full abduction). The collected and analyzed data is presented in Table 2.
Table 2.
Demographic and clinical characteristics of patients included in the study
| Demographics | Clinical findings | |||||||
|---|---|---|---|---|---|---|---|---|
| ID | Age of operation (years) |
Sex | Causes | Preoperative angle of deviation in PD | Last postoperative angle of deviation in PD | Preoperative abduction limitation | Last postoperative abduction limitation | Slit lamp examination and fundoscopy for signs of ASI |
| 1 | 12 | F | Viral | 55 | 8 | −5 | −3 | No ASI |
| 2 | 71 | F | Vascular | 60 | 7 | −5 | −3 | No ASI |
| 3 | 65 | M | Vascular | 55 | 6 | −5 | −2 | No ASI |
| 4 | 16 | F | Viral | 50 | 6 | −5 | −2 | No ASI |
| 5 | 60 | F | Vascular | 70 | 9 | −6 | −4 | No ASI |
| 6 | 58 | F | Vascular | 65 | 7 | −6 | −3 | No ASI |
| 7 | 66 | M | Vascular | 65 | 6 | −6 | −2 | No ASI |
| 8 | 67 | M | Vascular | 55 | 7 | −5 | −2 | No ASI |
| 9 | 58 | M | Vascular | 50 | 7 | −5 | −2 | No ASI |
| 10 | 55 | M | Traumatic | 70 | 8 | −7 | −4 | No ASI |
| 11 | 35 | F | Traumatic | 90 | 20 | −8 | −4 | No ASI |
| 12 | 24 | M | Traumatic | 60 | 6 | −6 | −3 | No ASI |
| 13 | 31 | F | Traumatic | 80 | 15 | −8 | −4 | No ASI |
| 14 | 27 | F | Traumatic | 55 | 8 | −5 | −2 | No ASI |
| 15 | 40 | M | Traumatic | 65 | 8 | −6 | −3 | No ASI |
| 16 | 33 | F | Traumatic | 65 | 10 | −5 | −4 | No ASI |
| 17 | 25 | F | Tumor | 55 | 10 | −5 | −3 | No ASI |
| 18 | 36 | F | Tumor | 80 | 7 | −7 | −4 | No ASI |
| 19 | 41 | M | Tumor | 80 | 6 | −7 | −4 | No ASI |
| 20 | 43 | F | Tumor | 60 | 6 | −6 | −4 | No ASI |
PD prism diopters, ASI anterior segment ischemia
The angle of deviation pre- and postoperatively was estimated by cover–uncover test with far target at 3 m. Post-op angle ≤ 10 PD was considered a success
Complete sixth nerve palsy was defined as the inability to abduct more than the midline (primary position). The abduction was scored as: −8 complete inability for abduction, −4 partial ability for abduction, up to primary position, 0 ability for full abduction
The postoperative follow up was undertaken at: 1st day, 1st week, 1st month, 6 months, 12 months
Patients with residual esotropia appeared with no problems in their everyday life. They were helped with prismatic correction incorporated into far-distance glasses, as well as the patient with the vertical deviation
Surgical Technique
Augmented VRT was performed according to the technique described by Foster [1]. According to our modified technique, the MR of the affected eye was undermined, avoiding cauterization of the anterior ciliary vessels. The width of the MR tendon insertion was measured and a 6/0 double-ended vicryl suture (spatulated needle) was put along the central part of the MR tendon and secured by four knots, leaving intact a 1.5-mm width of the upper tendon insertion pole and 1.5-mm width of the lower tendon insertion pole of the MR, preserving the anterior ciliary circulation. Then, the central part of the MR tendon and belly (secured by the 6/0 vicryl suture) was recessed by 6.5 mm and sutured on the sclera (Images 1, 2). The conjunctiva was closed with an 8/0 vicryl suture (interrupted fashion). Local tobramycin and dexamethasone drops three times a day (tid) for 4 weeks were prescribed postoperatively.
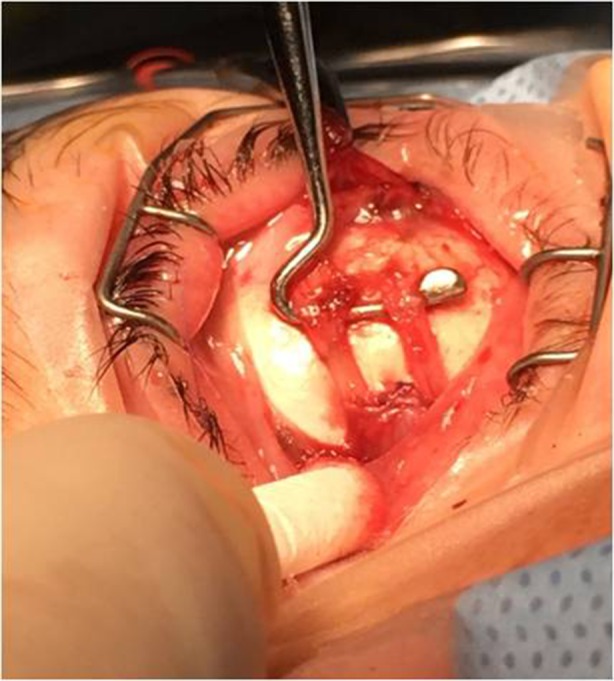
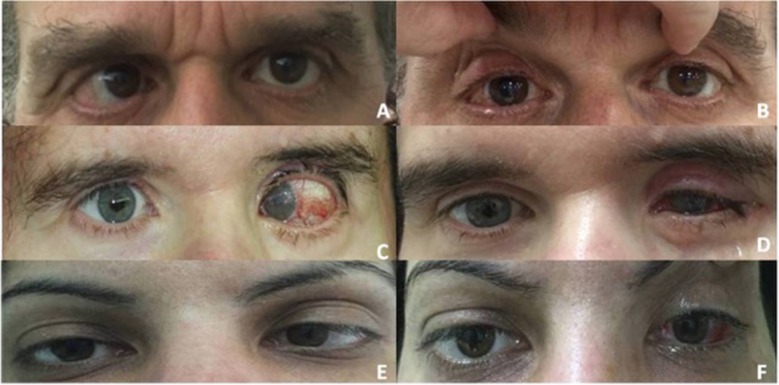
Image 1 Representation of the medial rectus muscle (MR) recession procedure: the central part of the MR tendon and belly are recessed and sutured onto the sclera, leaving intact a 1.5-mm width of the upper and lower tendon insertion pole. (MR shown on the hook in image)
Image 2 Eye position pre- (a–e) and postoperatively (b–f) in three patients. a, b Male patient with right sixth nerve palsy. c, d Female patient with left sixth nerve palsy shown on these images who had an additional lid surgery to treat lagophthalmos (due to coexistence of seventh nerve palsy) and is one of the two cases with the residual esotropia. e, f Female patient with left sixth nerve palsy
All patients were followed postoperatively on a regular basis: on the 1st day, 1st week, 1st month, 6th month and 12th month. A complete eye examination and a full ocular motility assessment was performed on all of the follow-up appointments.
Statistical Analysis
The Shapiro–Wilk test and the Wilcoxon test were used to further analyze the results. p values ≤ 0.05 were considered as statistically significant and postoperative alignment within 10 prism diopters (PD) of orthotropia suggested a successful surgical result. Normality of the data was tested and subsequently, a Wilcoxon test was performed to assess for significant differences between pre-operative and postoperative measurements of abduction limitation and deviation.
Results
Twenty patients (8 males and 12 females) with unilateral complete sixth nerve palsy were enrolled in the study. The most common cause of sixth nerve palsy in this study was trauma (35%) and vascular diseases (35%). The etiology and the rest of pre- and postoperative data are summarized in Table 2.
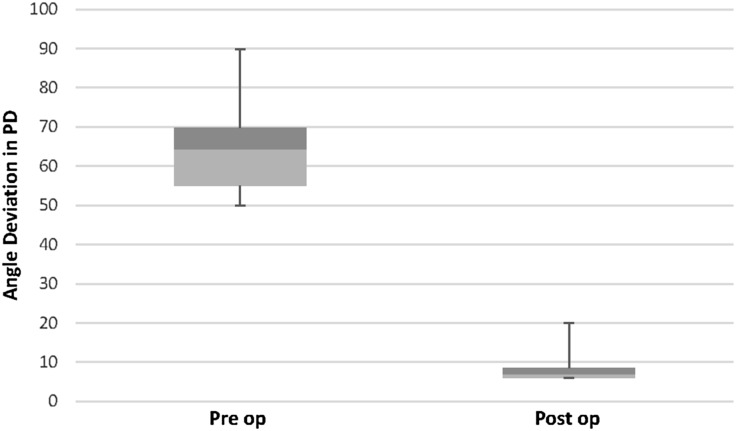
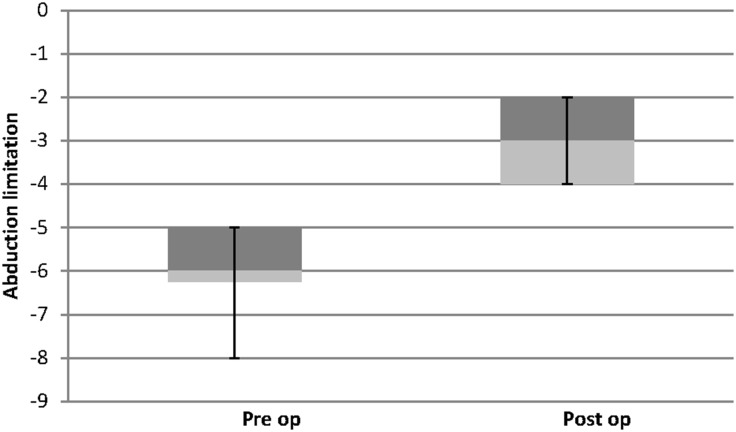
Mean esotropia in the primary position improved from 64.25 ± 10.9 PD preoperatively to 8.35 ± 3.5 PD postoperatively (p < 0.0001; Fig. 1). Seventeen patients (88%) were within 10 PD of orthotropia. Two patients (10%) ended up with undercorrection (patients 11 and 13 with residual angles of 20 and 15 PD base out, respectively); in both cases, the preoperative angle of deviation was ≥ 80 PD. New-onset vertical deviation in primary position was observed in one patient (5%) who ended up with hypotropia (angle of 10 PD base out). The abduction deficit was also improved from a mean −5.9 ± 1.02 to −3.1 ± 0.85 (p < 0.0001; Fig. 2). We also compared the postoperative results of the subgroups, according to their aetiology; however, no statistical difference was found.
Fig. 1.
Surgical results: Angle deviation preoperatively (Pre op) and postoperatively (Post op) representing esotropia and a significant improvement in deviation is indicated. PD: prism diopters Box and whisker diagram: The bottom and top of the box represent the 25th and 75th percentile (the lower and upper quartiles, respectively); the band near the middle of the box is the 50th percentile (the median). The ends of the whiskers represent the minimum and maximum of all the data
Fig. 2.
Surgical results: This figure summarizes the abduction limitation preoperatively (Pre op) and postoperatively (Post op). Negative values represent abduction deficit. Box and whisker diagram: The bottom and top of the box represent the 25th and 75th percentile (the lower and upper quartiles, respectively); the band near the middle of the box is the 50th percentile (the median). The ends of the whiskers represent the minimum and maximum of all the data
Discussion
Various procedures have been described to manage complete sixth nerve palsy [3, 4]. VRT procedure is the surgical technique of choice in these cases, aiming to improve the eye alignment in the primary position, the binocular field of vision and the abduction deficit.
Augmented full-tendon VRT, described by Foster [1], was proved to be effective in order to enhance the abduction and became the most preferable technique.
Rosenbaum reviewed the results of VRT with posterior fixation, orbital fixation and partial VRT in patients with sixth nerve palsy and Duane syndrome [5]. He concluded that a marked improvement in the range of binocular single vision could be achieved in patients that had undergone VRT with posterior fixation.
Guyton also described a vessel-sparing, “crossed adjustable” VRT that allows adjustment of both the superior and inferior recti muscles, not needing further augmentation [6]. However, many patients with abduction limitation develop tightness or contracture of the MR over time and that could guard the results. These patients need a further MR-weakening surgical procedure [5].
Although this is an option, surgery on multiple recti muscles on the same eye carries a theoretical increase in the risk of anterior segment ischemia (ASI) [7].
Looking for solutions, Johnston and Crouch first proposed that it might be possible to gain the benefits of transposition surgery by transposing only the superior rectus muscle (SRT; with or without MR recession), reducing the amount of surgery and the theoretical risk of ASI [8]. This technique became popular during the last few years.
Hunter adopted this technique by adding an MR recession on an adjustable suture [9].
Other authors have proposed VRT surgery combined with botulinum toxin (BTX) injection on the ipsilateral MR, to weaken its action [10]. However, the risk of ASI in full MR tendon recession combined with VRT, the unpredictable success rate in severe cases of sixth nerve palsy in SRT (combined or not) and the unpredictable results in BTX use compelled us to explore other solutions.
Our new modified technique weakens the MR (by recessing only the central part of the muscle’s belly—which mainly drives the muscle’s action) and preserves the anterior ciliary circulation.
Etiology that could lead to complete sixth nerve palsy varies a lot. In our study, the most common causes were trauma and vascular diseases (diabetes mellitus, etc.), which was compatible with other studies [11]. Our success rate (related to deviation) was 88%. Most of other techniques led to poorer results [12–14]. The mean final reduction of the preoperative esotropic deviation was 56 PD.
In previous studies, exotropic shift was reported, but in some of them, patients had undergone previous surgery [6, 12, 14–16]. On the contrary, in our study group, none of the patients had previous eye surgery and none of them appeared with postoperative exotropia, probably due to this fact.
In our current study, the mean abduction deficit improved from −5.9 preoperatively to −3.1 postoperatively. These results are very comparable with other studies [11–13]. Two of our patients who had residual esotropia in the primary position of gaze (15 and 20 PD base out) were managed successfully with prismatic correction incorporated into far-distance glasses. None of them had diplopia in near vision.
No significant limitation of adduction was observed in our study, compared to other studies, where MR weakening techniques (surgical or BTX) led to limitation of adduction [14, 15]. This could be possibly related to partial MR recession in our technique.
The undesired postoperative vertical deviation is not uncommon (5–30%). The real mechanism of this complication remains not well understood, although various theories have been proposed [17, 18]. To prevent this, various intraoperative manipulations like adjustable suture techniques [6], modification of the Foster technique using a single posterior fixation suture [19], intraoperative manipulations to take care of torsion and vertical deviations have been proposed [18, 20, 21].
Only one of our patients (5%) appeared with postoperative hypotropia of 10 PD in the operated eye, which was successfully managed with prismatic correction on distance glasses.
None of our patients presented with ASI, probably due to preservation of the anterior ciliary circulation. However, a larger sample and iris angiography is needed to objectively confirm that.
Limitations of the study should be considered: (a) the postoperative nature of the study, (b) the relatively small sample and (c) the lack of iris angiography to objectively prove the absence of ASI. Iris angiography was not performed in our sample because many of our patients were either too young or with multiple health problems. Due to that, parents and doctors (neurologists and neurosurgeons) did not consent to proceed in many of our cases. The number of the remaining participants then was too small.
To the best of our knowledge, our study is the first which describes this new technique and reports its long-term results. Our technique improves significantly the initial angle of deviation and the limitation of the abduction and probably minimizes the risk for ASI by preserving the anterior ciliary circulation. However, the latter remains to be objectively proved with iris angiography in larger samples.
Conclusion
The augmented VRT with partial recession of the MR (Kozeis modified technique) has a high success rate in improving the initial angle of deviation, the abduction deficit and possibly minimizes the risk for ASI in complete forms of sixth nerve palsy. However, the latter should be objectively proved with iris angiography in larger samples. The technique could be performed in patients with complete and chronic sixth nerve palsy as an alternative to other previously described techniques.
Acknowledgements
We would like to thank the participants of the study.
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole and have given their approval for this version to be published.
Disclosures
The authors Nikolaos Kozeis, Magdalini Triantafylla, Aspasia Adamopoulou, Stergiani Veliki, Athina Kozei, and Straton Tyradellis have nothing to disclose.
Compliance with Ethics Guidelines
The study was conducted according to the tenets of the Declaration of Helsinki and was approved by the Ophthalmica Eye Institute Ethics Committee. All patients signed an informed consent preoperatively.
Data Availability
All data generated or analyzed during this study are included in this published article as supplementary information files.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Footnotes
Enhanced digital content
To view enhanced digital content for this article, go to 10.6084/m9.figshare.6994781.
Contributor Information
Nikolaos Kozeis, Email: kozeis@ophthalmica.gr.
Athina Kozei, Email: kozeiathina@gmail.com.
References
- 1.Foster RS. Vertical muscle transposition augmented with lateral fixation. J AAPOS. 1997;1:20–30. doi: 10.1016/S1091-8531(97)90019-7. [DOI] [PubMed] [Google Scholar]
- 2.Saunders RA, Phillips MS. Anterior segment ischemia after three rectus muscle surgery. Ophthalmology. 1988;95:533–537. doi: 10.1016/S0161-6420(88)33154-4. [DOI] [PubMed] [Google Scholar]
- 3.Muraki S, Nishida Y, Ohji M. Surgical results of a muscle transposition procedure for abducens palsy without tenotomy and muscle splitting. Am J Ophthalmol. 2013;156(4):819–824. doi: 10.1016/j.ajo.2013.05.020. [DOI] [PubMed] [Google Scholar]
- 4.Lee YH, Lambert SR. Outcomes after superior rectus transposition and medial rectus recession versus vertical recti transposition for sixth nerve palsy. Am J Ophthalmol. 2017;177:100–105. doi: 10.1016/j.ajo.2017.02.019. [DOI] [PubMed] [Google Scholar]
- 5.Lecture Costenbader. The efficacy of rectus muscle transposition surgery in esotropic Duane syndrome and VI nerve palsy. J AAPOS. 2004;8(5):409–419. doi: 10.1016/j.jaapos.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 6.Phamonvaechavan P, Anwar D, Guyton DL. Adjustable suture technique for enhanced transposition surgery for extra ocular muscles. J AAPOS. 2010;14(5):399–405. doi: 10.1016/j.jaapos.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Murdock TJL, Kushner BJ. Anterior segment ischemia after surgery on 2 vertical rectus muscles augmented with lateral fixation sutures. J AAPOS. 2001;5(5):323–324. doi: 10.1067/mpa.2001.118668. [DOI] [PubMed] [Google Scholar]
- 8.Johnston SC, Courch ERC, Jr, Crouch ER. An innovative approach to transposition surgery is effective in treatment of Duane’s syndrome with esotropia. Invest Ophthalmol Vis Sci. 2006;47:2475. [Google Scholar]
- 9.Mehendale Reshma A, Dagi Linda R, Carolyn Wu, Ledoux Danielle, Johnston Suzanne, Hunter David G. Superior rectus transposition combined with medial rectus recession for Duane syndrome and sixth nerve palsy. Arch Ophthalmol. 2012;130(2):195–201. doi: 10.1001/archophthalmol.2011.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scott AB, Kraft SP. Botulinum toxin injection in the management of lateral rectus paresis. Ophthalmology. 1985;92:676–683. doi: 10.1016/S0161-6420(85)33982-9. [DOI] [PubMed] [Google Scholar]
- 11.Rosenbaum AL, Kushner BJ, Kirschen D. Vertical rectus transposition and botulinum toxin (oculinum) to medial rectus for abducens palsy. Arch Ophthalmol. 1989;107:820–823. doi: 10.1001/archopht.1989.01070010842025. [DOI] [PubMed] [Google Scholar]
- 12.Fitzsmons R, Lee JP, Elston J. Treatment of sixth nerve palsy in adults with combined botulinum toxin chemodenervation and surgery. Ophthalmology. 1988;95:1535–1542. doi: 10.1016/S0161-6420(88)32976-3. [DOI] [PubMed] [Google Scholar]
- 13.Flanders M, Qahtani F, Gans M, Beneish R. Vertical rectus muscle transposition and botulinum toxin for complete sixth nerve palsy. Can J Ophthalmol. 2001;36:18–25. doi: 10.1016/S0008-4182(01)80062-4. [DOI] [PubMed] [Google Scholar]
- 14.Nabie R, Andalib D. Augmented vertical recti transposition with intraoperative botulinum toxin for complete and chronic sixth nerve palsy Eye. 2017;31:148–151. doi: 10.1038/eye.2016.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Armenia JV, Sigal MB. Abducens paralysis repaired with muscle transposition and intraoperative botulinum toxin. Ann Ophthalmol. 1987;19(416–618):422. [PubMed] [Google Scholar]
- 16.Leiba H, Wirth GM, Amstuz C, Landau K. Long-term result of vertical transposition and botulinum toxin for sixth nerve palsy. J AAPOS. 2010;14:498–501. doi: 10.1016/j.jaapos.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 17.Bansal S, Khan J, Marsh IB. Unaugmented vertical muscle transposition surgery for chronic sixth nerve paralysis. Strabismus. 2006;14:177–181. doi: 10.1080/09273970601026201. [DOI] [PubMed] [Google Scholar]
- 18.Laby DM, Rosenbaum AL. Adjustable vertical rectus muscle transposition surgery. J Pediatr Ophthalmol Strabismus. 1994;31:75–78. doi: 10.3928/0191-3913-19940301-03. [DOI] [PubMed] [Google Scholar]
- 19.Holmes JM, Hatt SR, Leske DA. Intraoperative monitoring of torsion to prevent vertical deviations during augmented vertical rectus transposition surgery. J AAPOS. 2012;16:136–140. doi: 10.1016/j.jaapos.2011.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Struck MC. Augmented vertical rectus transposition surgery with single posterior fixation suture: modification of foster technique. J AAPOS. 2009;13:343–349. doi: 10.1016/j.jaapos.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 21.Ruth AL, Velez FG, Rosenbaum AL. Management of vertical deviation after vertical rectus transposition surgery. J AAPOS. 2009;13:16–19. doi: 10.1016/j.jaapos.2008.08.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article as supplementary information files.