Abstract
Background
Implicit attitudes are outside of conscious awareness and are thought to affect automatic responses outside of one’s deliberate control, with the potential to impact physician-patient relationships.
Objective
To measure the nature and extent of implicit biases towards depression in internal medicine and psychiatry residents.
Design
Descriptive and comparative study.
Participants
Fifty-one residents from three internal medicine programs and 35 residents from three psychiatry programs located in two states.
Interventions
Participants were sent a link to voluntarily participate in four online implicit association tests. Residents’ identities were anonymous.
Main Measures
Four implicit association tests to measure the association of (1) attitude (good/bad), (2) permanence, (3) controllability, and (4) etiology with depression/physical illness.
Key Results
Internal medicine residents demonstrated a significant association between depression and negative attitudes (t(38) = 6.01, p < .001, Cohen’s d = .95), uncontrollability (t(35) = 4.80, p < .001, Cohen’s d = .79), temporariness (t(37) = 2.94, p = .006, Cohen’s d = .48), and a psychologic etiology (t(1) = 6.91, p < .001, Cohen’s d = 1.24). Psychiatry residents only demonstrated an association between depression and a psychologic etiology (t(2) = 4.79, p < .001, Cohen’s d = 4.5). When comparing the two specialties, internal medicine and psychiatry differed on two of the IATs. Internal medicine residents were more likely to associate negative attitudes with depression than psychiatry residents (t(63) = 4.66, p < .001, Cohen’s d = 1.18) and to associate depression with being uncontrollable (t(57) = 3.17, p = .002, Cohen’s d = .81).
Conclusions
Internal medicine residents demonstrated biases in their attitudes towards depression and significantly differed in some areas from psychiatry residents. This pilot study needs to be replicated to confirm our findings and further work needs to be done to determine the effect of these attitudes on the provision of clinical care.
Introduction
People with behavioral health problems experience worsened health outcomes and shortened life expectancies1 for a variety of reasons, including suicide and accidents,2 disparities in access to care,3 the impact of psychiatric medications,4 and risky personal practices such as smoking and exercise avoidance.4 Self-stigma, social stigma, and health care provider stigma can also impact health outcomes by influencing treatment seeking behaviors in those with mental illnesses or substance abuse issues.5 Stigma on the part of health care providers, including physicians, may also affect clinical decision making in ways that are not yet fully understood.6–9
Physician stigma towards mental illness stems from both implicit and explicit attitudes. Implicit attitudes result in primarily automatic responses and tend to predict spontaneous and nonverbal behaviors10 while explicit attitudes are conscious thoughts that are associated with controlled behaviors and are influenced by social demands.11 Studies have demonstrated that expressions of prejudice or stereotypes associated with explicit attitudes may be modified or controlled with education, motivation, skill, and cognitive resources,11 but implicit attitudes may not be as easily identified and targeted.
There is evidence that negative explicit attitudes impact clinical decision making at least to some extent. For example, in one study, health care providers (both primary care and mental health) who endorsed more stigmatizing explicit attitudes about mental illness were likely to be more pessimistic about patients’ likelihood of adhering to treatment and consequently were less likely to refer patients to a specialist or refill their prescription.12 In another study, family physicians demonstrated a reluctance to investigate physical symptoms in patients with a history of depression, perhaps because they attributed the symptoms to the mental illness rather than a biological condition.13 In two qualitative studies of emergency department clinicians, participants described a fear of people with mental health issues, reported some stigmatizing attitudes, and showed evidence of diagnostic overshadowing (the misattribution of physical symptoms to mental illness).14, 15
While no study has yet explored the impact of implicit attitudes on clinical decision making, several recent studies have explored the prevalence of implicit attitudes towards mental illness in psychiatrists and other mental health providers. For example, practicing and resident psychiatrists were found to have little or no negative associations with schizophrenia.16 Another study looked at attitudes towards schizophrenia and found that just prior to their psychiatric rotation, Japanese medical residents associated the traditional term for schizophrenia (“Seishin-Bunretsu-Byo”) with violence. After their rotation, the residents had come to associate the new term for schizophrenia (“Togo-Shitcho-Sho”) which was introduced to destigmatize the condition, with violence as well.17 Finally, Peris et al.18 found that negative implicit attitudes towards people with mental illness in clinicians with mental health training predicted over-diagnosis of people (defined in this study as assigning diagnoses beyond the correct one) with mental illnesses, while explicit biases predicted the prognosis a clinician would assign a patient.
Together, these studies demonstrate the presence of biases towards mental illness even in those providers who have trained specifically to treat them (i.e., psychiatrists and other mental health providers), and begin to suggest that such biases may impact clinical decision making. What is not known is how prevalent these biases are in primary care physicians. This is an important gap in the literature, as more than half of outpatient primary care visits for somatic complaints are associated with anxiety and depression.19 Thus, the purpose of this study was to (1) measure the implicit attitudes of internal medicine and psychiatry residents towards depression and 2) to determine whether internal medicine and psychiatry residents show differences in their implicit bias towards depression.
Methods
Study Design
This was a descriptive and comparative study involving three internal medicine residency programs and three psychiatry residency programs in two states. This study was determined to be exempt from oversight by the Institutional Review Boards of Louisiana State University Health Sciences Center and University of Southern California Keck School of Medicine. The study was funded in part by grants from the Southern Group on Educational Affairs and the Western Group on Educational Affairs.
Participants
We made the decision to include two different specialties and to make the study anonymous and voluntary to attract a wider variety of residents to participate. Internal medicine residents, PGY 1–3, who were part of the three internal medicine programs during the 2015-2016 year were invited to participate. Psychiatry residents, PGY 1-4, from the 2015–2016 year (plus incoming 2016-2017 PGY 1’s) in three different programs were eligible and were invited to participate. Two of the internal medicine programs and two of the psychiatry programs were located in urban Louisiana cities. The third internal medicine and psychiatry programs that were included were in California. An email from the respective program directors contained a link to four online implicit association tests and was sent to all eligible residents (N = 185 internal medicine and 116 psychiatry). Participation was voluntary and no incentives were offered.
Implicit Attitude Measures
The purpose of the Implicit Association Test (IAT)20 is to reveal automatic, unconscious associations between particular concepts (e.g., depression) and different labels (e.g., bad) by measuring reaction times during a sorting task (for a more detailed description of the IAT procedure, see Greenwald and Binaji20). Four IATs were created for the purpose of this study based on the work of Monteith.11 These IATs were designed to assess the extent to which residents associated a patient’s condition of depression with the affective valence of the condition (good/bad) (IAT 1), the controllability of the condition (IAT 2), the etiology of the condition (IAT 3), and the temporal stability of the condition (IAT 4). Table 1 contains the labels that were used in each IAT.
Table 1.
Words that were used within the implicit association tests
| Depression | Sadness, hopeless, tearful, despondent, depressed | |
| Physical illness | Nausea, fever, shortness of breath, edema, jaundice | |
| Good | IAT 1 | Positive, pleasant, enjoy, glorious, wonderful |
| Bad | Horrible, depraved, terrible, unpleasant, despise | |
| Controllable | IAT 2 | Avoidable, preventable, manageable, well behaved |
| Uncontrollable | Unavoidable, inevitable, unmanageable, irrepressible | |
| Psychological | IAT 3 | Stress, mental, emotional, psychosomatic, feelings |
| Biological | Genes, physiology, brain, physical, hereditary | |
| Permanent | IAT 4 | Stable, constant, persistent, chronic, prolonged |
| Temporary | Impermanent, variable, short-term, brief, occasional | |
Each IAT was scored by combining the response latencies for each combination of categories into an IAT score that can range from –2 to 2. The IAT score is essentially a measure of the effect size between response latencies to different sets of stimuli.21 The assumption behind this scoring is that faster reaction times to one pairing compared to the other reflect an automatic preference for that pairing and thus an implicit association between the two concepts.. Scores of greater magnitude (whether positive or negative) represent a stronger association. In our study, a positive IAT score associated depression with having a bad attitude (IAT 1), being uncontrollable (IAT 2), having a psychological etiology (IAT 3), and being impermanent (IAT 4) whereas a negative score associated physical illness with those same characteristics.
Data Collection
Residents were sent an email requesting that they participate in the study. The IAT’s were hosted by Project Implicit’sR website and residents had to participate using a desk top computer. The tests could not be done from a phone or tablet. Participation was voluntary and no demographic data were collected to ensure anonymity.
Data Analysis
Computation of the IAT scores for each of the four tests was done by Project ImplicitR, based on an algorithm developed by Greenwald, Nosek, and Banaji.22 One-sample t tests were computed to determine whether mean IAT scores within each type of residency differed significantly from zero, and independent samples t tests were used to determine whether the two residencies differed significantly from each other by mean IAT scores. Cohen’s d effect sizes were calculated for all inferential statistics.
Results
Of the 185 internal medicine and 116 psychiatry residents invited to participate, 51 (28%) and 35 (30%) respectively completed the study. For each IAT, any individual with an error rate of more than 40% or unusually fast (10% or more of responses < 300 ms) or slow (10% or more of responses > 2000 ms) response times was excluded from analyses.23 This resulted in the removal of 20 participants from IAT 1, 27 participants from IATs 2 and 3, and 14 participants from IAT 4. By using the more stringent criteria for inclusion, we only included people who completed the task appropriately. Our data was analyzed with and without those outliers and the results were the same, but with the excluded participants, the standard deviations were smaller and the results stronger. The results of all IATs are summarized in Figure 1.
Figure 1.
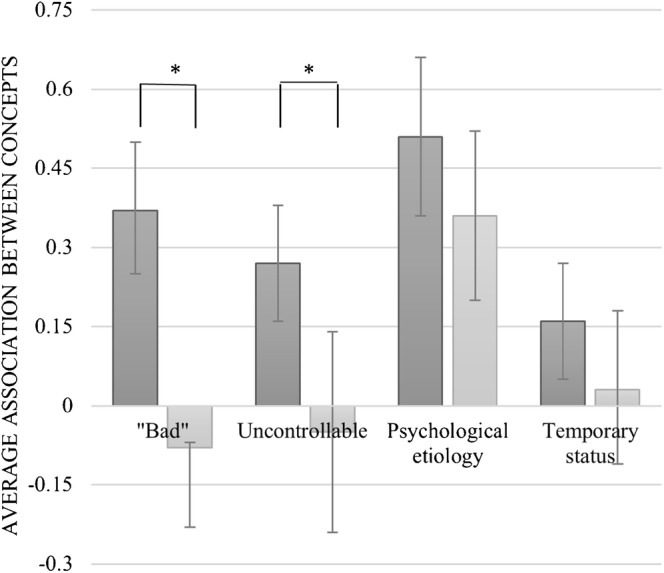
Summary of IAT results comparing internal medicine and psychiatry resident attitudes towards depression.  Internal Medicine residents.
Internal Medicine residents.  Psychiatry residents. *p < 0.001 when comparing the two specialties’ average IAT values. A positive score shows an association between descriptor and depression, while a negative score shows an association between descriptor and physical illness.
Psychiatry residents. *p < 0.001 when comparing the two specialties’ average IAT values. A positive score shows an association between descriptor and depression, while a negative score shows an association between descriptor and physical illness.
For the IAT that measured the association of attitudes, positive or negative, with physical illness and depression (IAT 1), 39 internal medicine residents and 26 psychiatry residents were included in the analysis. Compared to a score of zero (representing no association), internal medicine residents showed a significant association of depression with “negative words” (M = .37, SD = .39, t(38) = 6.01, p < .001, 95% CI .25 to .50, Cohen’s d = .95), while psychiatry residents did not (M = − .08, SD = .37, t(25) = − 1.05, p = .30, 95% CI − .23 to − .07, Cohen’s d = − .22). Internal medicine residents were significantly more likely to associate more positive words with physical illness and more negative words with depression than were psychiatry residents (t(63) = 4.66, p < .001, Cohen’s d = 1.18).
For the IAT that measured the association of controllable and uncontrollable words with physical illness and depression (IAT 2), 36 internal medicine residents and 23 psychiatry residents were included. Compared to a score of zero (representing no association), internal medicine residents showed a significant association between depression and uncontrollability (M = .27, SD = .34, t(35) = 4.80, p < .001, 95% CI .16 to .38, Cohen’s d = .79) while psychiatry residents did not (M = − .05, SD = .44, t(22) = − .55, p = .59, 95% CI − .24 to .14, Cohen’s d = − .11. Internal medicine residents were significantly more likely to associate physical illness with “controllable” and depression with “uncontrollable” than were psychiatry residents (t(57) = 3.17, p = .002, Cohen’s d = .81).
For the IAT that measured associations of depression and physical illness with biological or psychological etiology, 30 internal medicine residents and 20 psychiatry residents were included. There was no significant difference between the two groups of residents (t(48) = 1.36, p = .18, Cohen’s d = .51), and both significantly associated physical illness with “biological” and depression with “psychological” etiologies (internal medicine M = .51, SD = .41, t(29) = 6.91, p < .001, 95% CI .36 to .66, Cohen’s d = 1.24 and psychiatry M = .36, SD = .08, t(19) = 4.79, p < .001, 95% CI .20 to .52, Cohen’s d = 4.5).
For the IAT that looked at associations between depression and physical illness and the permanence of the condition, 38 internal medicine residents and 27 psychiatry residents were included. The two groups of residents did not differ significantly on this IAT (t(63) = 1.47, p = .15, Cohen’s d = .37); however, internal medicine residents did show a significant association between physical illness with permanence/depression with temporariness (M = .16, SD = .33, t(37) = 2.94, p = .006, 95% CI .05 to .27, Cohen’s d = .48) while psychiatry residents showed no such association (M = .03, SD = .37, t(26) = .44, p = .67, 95% CI − .11 to .18, Cohen’s d = .08).
Discussion
Our findings as they relate to psychiatry residents are similar to the work of Dabby,16 who measured implicit attitudes towards people with mental illness. Practicing psychiatrists and psychiatry residents in that study did not differ from each other and their mean IAT scores did not demonstrate a meaningful effect size. Although there have been reports of mental health personnel, and psychiatrists in particular, harboring explicitly stigmatizing attitudes towards people with mental illness, including depression,24, 25 there was no evidence of it when measured implicitly in our study. Personality assessments of people who go into psychiatry have demonstrated a higher degree of openness (defined as an attentiveness to inner feelings, intellectual curiosity and independence of judgment)26 and compassion27 which could help explain the lack of automatic bias towards depression we found in this study.
In a unique contribution to the literature, our study showed that our internal medicine residents demonstrated an automatic preference in all four of the IAT’s, though to varying degrees. They associated depression with negative words and a psychologic etiology, as well as with being uncontrollable and temporary. The first IAT measured negative and positive attitudes towards depression, and the association of negative words with depression is clearly undesirable. However, the concepts of controllability, permanence, and etiology (IAT’s 2, 3, and 4) don’t necessarily convey a negative judgment. The fact that internal medicine residents see the condition of depression as a temporary state could be interpreted to convey hope, while the fact that they see it as uncontrollable could be a reflection on their own sense of impotence at knowing how to appropriately treat it, rather than a reflection on or judgment of the patients. The concept that both groups agreed on was their shared interpretation of depression as more psychological than biological in its etiology which suggests perhaps their beliefs about depression as a reflection of the mind, rather than the brain.
At this point, it is unknown whether the implicit biases found in internal medicine residents in this small pilot study are generalizable outside of the studied population. There is no evidence from other studies with which to compare these results. Furthermore, our study does not shed light on whether or not these biases may impact clinical care decisions. Indeed, there is often little correlation between people’s explicit attitudes or behaviors and their implicit attitudes.11 On the other hand, some evidence does suggest that implicit attitudes (or biases) can correlate with potential differences in care.28 However, our study does not make this link, and our findings could be explained in part by the participants’ level of discomfort with a condition they do not feel competent to assess and treat. More work should be done before drawing conclusions as to the meaning and impact of these findings. However, as reported, the unconscious attitudes demonstrated in this study may contribute to the perceived stigma some patients report when trying to access health care29 and the perception by some patients that they should not disclose their depressive symptoms to primary care providers.30
Future research should investigate both the prevalence and effects of automatic attitudes towards depression in the primary care setting. Also, investigation into ways to minimize the effects of implicit biases should be explored and interventions piloted. Residency programs could consider adding training to their curricula about implicit biases and their potential effect on patients. Although education alone is insufficient to change implicit attitudes, awareness can help one overcome the potential for bias in decision making.28
We had results from three different programs of each specialty in two different states, but the limitation of low response rates reduced generalizability. The study should therefore be viewed as a pilot that opens the discussion about implicit attitudes, but conclusions or generalizability of the findings are not possible at this time.
In summary, this is the first study to look at internal medicine resident implicit attitudes towards depression, and comparing those implicit attitudes between internal medicine residents and psychiatry residents. Differences between specialties were found; however, more work needs to be done to confirm these differences and to explore the impact of these differences on the provision of clinical care.
ACKNOWLEDGEMENTS
This project was supported by funding from both the Association of American Medical Colleges (AAMC) Southern Group on Educational Affairs and the Western Group on Educational Affairs. The authors thank them for their support.
Compliance with ethical standards
Conflict of interest
The authors declare that they do not have a conflict of interest.
Prior presentations
This work was presented at the University of Southern California, Keck School of Medicine, Innovations in Medical Education conference in February, 2017 and the Southern Group on Educational Affairs regional conference in April 2018.
References
- 1.Chang C-K, Hayes RD, Perera G, et al. Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS ONE. 2011;6(5):e19590. doi: 10.1371/journal.pone.0019590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lawrence D, Kisely S, Pais J. The epidemiology of excess mortality in people with mental illness. Can J Psychiatry. 2010;55(12):752–760. doi: 10.1177/070674371005501202. [DOI] [PubMed] [Google Scholar]
- 4.Parks J, Svendsen D, Singer P, et al. Morbidity and Mortality in People with Serious Mental Illness. Alexandria, VA; 2006; Tech No. 13.
- 5.Henderson C, Evans-Lacko S, Thornicroft G. Mental illness stigma, help seeking, and public health programs. Am J Public Health. 2013;103(5):777–780. doi: 10.2105/AJPH.2012.301056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petersen LA, Normand S-LT, Druss BG, Rosenheck RA. Process of care and outcome after acute myocardial infarction for patients with mental illness in the VA health care system: are there disparities? Health Serv Res. 2003;38(1 Pt 1):41–63. doi: 10.1111/1475-6773.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leucht S, Burkard T, Henderson J, Maj M, Sartorius N. Physical illness and schizophrenia: a review of the literature. Acta Psychiatr Scand. 2007;116(5):317–333. doi: 10.1111/j.1600-0447.2007.01095.x. [DOI] [PubMed] [Google Scholar]
- 8.Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340(8):618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 9.Barney LJ, Griffiths KM, Jorm AF, Christensen H. Stigma about depression and its impact on help-seeking intentions. Aust N Z J Psychiatry. 2006;40(1):51–54. doi: 10.1080/j.1440-1614.2006.01741.x. [DOI] [PubMed] [Google Scholar]
- 10.Sriram N, Greenwald AG. The brief implicit association test. Exp Psychol. 2009;56(4):283–294. doi: 10.1027/1618-3169.56.4.283. [DOI] [PubMed] [Google Scholar]
- 11.Monteith LL, Pettit JW. Implicit and explicit stigmatizing attitudes and stereotypes about depression. Journal of Social and Clinical Psychology. 2011;30(5):484–505. doi: 10.1521/jscp.2011.30.5.484. [DOI] [Google Scholar]
- 12.Corrigan P, Mittal D, Reaves C, Haynes T, Han X, Morris S, Sullivan G. Mental health stigma and primary health care decisions. Psychiatry Res. 2014;218:35–38. doi: 10.1016/j.psychres.2014.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Graber M, Bergus G, Dawson J, Wood G, Levy B, Levin I. Effect of a patient’s psychiatric history on physician’s estimation of probability of disease. J Gen Intern Med. 2000;15:204–206. doi: 10.1046/j.1525-1497.2000.04399.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van Nieuwenhuizen A, Henderson C, Kassam A, Graham T. Emergency department staff views and experiences on diagnostic overshadowing related to people with mental illness. Epidemiology and Psychiatric Services. 2013;22(3):255–262. doi: 10.1017/S2045796012000571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shefer G, Henderson C, Howard L, Murray J, Thornicroft G. Diagnostic overshadowing and other challenges involved in the diagnostic process of patients with mental illness who present in emergency departments with physical symptoms—a qualitative study. PLoS One. 2014;9911:e111682. doi: 10.1371/journal.pone.0111682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dabby L, Tranulis C, Kirmayer LJ. Explicit and implicit attitudes of Canadian psychiatrists toward people with mental illness. Can J Psychiatry. 2015;60(10):451–459. doi: 10.1177/070674371506001006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Omori A, Tateno A, Ideno T, et al. Influence of contact with schizophrenia on implicit attitudes towards schizophrenia patients held by clinical residents. BMC Psychiatry. 2012;12:205. doi: 10.1186/1471-244X-12-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peris TS, Teachman BA, Nosek BA. Implicit and explicit stigma of mental illness: links to clinical care. J Nerv Ment Dis. 2008;196(10):752–760. doi: 10.1097/NMD.0b013e3181879dfd. [DOI] [PubMed] [Google Scholar]
- 19.Kroenke K. The interface between physical and psychological symptoms. Primary care companion. J Clin Psychiatry. 2003;5(suppl 7):11–18. [Google Scholar]
- 20.Greenwald AG, McGhee DE, Schwartz JL. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998;74(6):1464–1480. doi: 10.1037/0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- 21.Baker TK, Smith GS, Jacobs NN, et al. A deeper look at implicit weight bias in medical students. Adv in Health Sci Educ. 2017;22:889–900. doi: 10.1007/s10459-016-9718-1. [DOI] [PubMed] [Google Scholar]
- 22.Greenwald AG, Nosek BA, Banaji MR. Understanding and using the implicit association test: I. An improved scoring algorithm. J Pers Soc Psychol. 2003;85(2):197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- 23.Teachman BA, Wilson JG, Komarovskaya I. Implicit and explicit stigma of mental illness in diagnosed and healthy samples. Journal of Social and Clinical Psychology. 2006;25(1):75–95. doi: 10.1521/jscp.2006.25.1.75. [DOI] [Google Scholar]
- 24.Henderson C, Noblett J, Parke H, et al. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry. 2014;1(6):467–482. doi: 10.1016/S2215-0366(14)00023-6. [DOI] [PubMed] [Google Scholar]
- 25.Schulze B. Stigma and mental health professionals: a review of the evidence on an intricate relationship. Int Rev Psychiatry. 2007;19(2):137–155. doi: 10.1080/09540260701278929. [DOI] [PubMed] [Google Scholar]
- 26.Maron BA, Fein S, Maron BJ, Hillel AT, El Baghdadi MM, Rodenhauser P. Ability of prospective assessment of personality profiles to predict the practice specialty of medical students. Proc (Bayl Univ Med Cent). 2007;20(1):22–26. doi: 10.1080/08998280.2007.11928228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sievert M, Zwir I, Cloninger KM, Lester N, Rozsa S, Cloninger CR. The influence of temperament and character profiles on specialty choice and well-being in medical residents. PeerJ. 2016;4:e2319. doi: 10.7717/peerj.2319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chapman E, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. JGIM. 2013;28(11):1504–10. doi: 10.1007/s11606-013-2441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ostrow L, Manderscheid R, Mojtabai R. Stigma and difficulty accessing medical care in a sample of adults with serious mental illness. J Health Care Poor Underserved. 2014;25(4):1956–1965. doi: 10.1353/hpu.2014.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Keller AO, Valdez CR, Schwei RJ, Jacobs EA. Disclosure of depression in primary care: a qualitative study of women’s perceptions. Womens Health Issues. 2016;26(5):529–536. doi: 10.1016/j.whi.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


