Abstract
Background
Persons with speech, language, and/or voice disabilities (collectively referred to as communication disabilities (CD)) represent 10% of the US population, yet their healthcare outcomes have not been described. Generally, research shows that persons with disabilities have poorer health and healthcare outcomes than their non-disabled peers.
Objectives
To examine the health and healthcare outcomes of persons with CD compared to persons without CD.
Design
Retrospective cohort study of the 2012 National Health Interview Survey, which contained the first supplemental questions on CD. We compared proportional differences in outcomes; logistic and ordered logistic regression assessed the outcome measures across CD categories, controlling for demographics, non-communication disabilities, and chronic conditions. Findings are weighted to permit national inferences.
Participants
Adults (≥ 18 years old) were divided into 4 mutually exclusive groups: people with voice disabilities only; speech/language disabilities only; speech/language and voice disabilities; and people without CD.
Main Measures
Chronic health conditions; self-rated health; access to care; unmet needs for care; healthcare utilization.
Key Results
Adults with CD more frequently had ≥ 1 chronic condition (voice 67.9%, speech/language 68.6%, speech/language and voice 79.9%, no CD 50.1%, p < 0.001) and reported fair/poor health (voice 19.5%, speech/language 32.5%, speech/language and voice 48.3%, no CD 11.2%, p < 0.001) compared to those without CD. Adults with CD more frequently utilized healthcare compared to those without CD. However, persons with CD endorsed greater difficulties accessing care than those without CD, including identifying a usual source of care, trouble finding a physician, and delaying or foregoing care (e.g., delayed due to availability of care: voice 26.1%, speech/language 37.2%, speech/language and voice 30.8% no CD 16.1%, p < 0.001).
Conclusions
Persons with CD are medically complex and experience greater challenges accessing healthcare than persons without CD. Healthcare providers need support and tools to provide equitable care that addresses the medical needs of persons with CD.
Electronic supplementary material
The online version of this article (10.1007/s11606-018-4625-1) contains supplementary material, which is available to authorized users.
KEY WORDS: communication disabilities, chronic conditions, health care utilization, access to care, unmet needs for care
BACKGROUND
Persons with speech, language, and/or voice disabilities (collectively referred to as communication disabilities (CD)) represent 10% of the US population.1 CD can arise from a multitude of conditions (e.g., aphasia due to stroke, developmental stutter or dysfluency, aphonia from total laryngectomy) and result in patients having difficulty expressing and/or comprehending language. Given the rising rates of disability and the aging population, the proportion of persons with CD in the population is likely to increase.2
An expanding body of evidence suggests that people with disabilities experience poorer health and healthcare outcomes than those without disabilities,3, 4 yet few studies to date have examined health and healthcare outcomes for adults with CD. In a study of Medicare recipients, Hoffman et al. reported low satisfaction with healthcare and patient-provider communication among persons with CD.5 These findings have been echoed in qualitative studies describing poor patient-provider communication among patients with CD as a major contributor to low satisfaction.6–10 Bartlett et al. observed that patients with CD were three times more likely to experience adverse medical events during hospital stays compared to patients without CD.11 Outside of these reports, little is known about the overall health and healthcare outcomes of people with CD. Yet, healthcare providers need baseline information on these outcomes to address the needs of this growing population that reports poor experiences with healthcare delivery.
In 2012, the National Health Interview Survey (NHIS) included supplemental questions about CD.12 This was the first health-related national survey to collect such information. Therefore, the purpose of this paper is to leverage this unique dataset to examine the health and healthcare outcomes of people with CD compared to people without CD in the USA. We pay particular attention to self-rated health, chronic conditions, and healthcare access and utilization. Based on the literature discussed above and our clinical experiences, we anticipate that people with CD will fare worse in these domains than their peers without CD.
METHODS
Data Source and Subjects
For this retrospective cohort study, we used the 2012 National Health Interview Survey (NHIS). The NHIS is an annual in-person survey administered by the U.S. Census Bureau of community-dwelling civilians in households in the USA that addresses numerous health and healthcare topics.12 Surveyors asked a set of core survey questions on health conditions, behaviors, and healthcare access/utilization for each member of the sampled families. Additionally, they gathered information on one randomly sampled adult within each family unit. The NHIS is publicly available; the Institutional Review Board at Tufts University categorized this study as exempt from review.
The 2012 NHIS Sample Adult questionnaire contained the supplementary questions on CD. The Sample Adult file contains information on a total of 34,525 adults ≥ 18 years old, representing a final response rate of 61.2%.12 Full information on the supplemental CD questions was available for 33,166 adults (96%), which comprised the cohort used in this analysis.
Communication Disabilities Definitions
Respondents were categorized as having a communication disabilities (CD) based on an affirmative response to questions regarding difficulties or problems with their voice, speech, or language during the past 12 months. Respondents answering “no” to those all of these questions were categorized as not having a CD. Respondents who refused or were uncertain were coded as missing (n = 49) and were excluded from the final analysis.
We created a mutually exclusive variable to define CD groups: people with (1) voice disabilities only (2) speech and/or language (SL) disabilities only, and (3) speech and/or language and voice (SLV) disabilities. We categorized voice disabilities separately from SL disabilities because the duration of these problems is significantly shorter (56 days in a year as compared to 142 and 195 days for respondents with speech or language disabilities).4 Consequently, it would be expected that voice disabilities are less likely to impact a respondent’s health and health outcomes compared to speech or language disabilities.
Study Outcomes
Health
We examined respondents’ self-reports of having 8 conditions: hypertension, stroke, emphysema, asthma, cancer, arthritis, diabetes, and cardiac disease. We summarized these reports into no conditions, 1 condition, or ≥ 2 condition. Self-rated health was categorized as poor/fair, good, or very good/excellent.
Access to Healthcare
We included two measures of usual sources of care: having a usual place of care (1) when sick or in need of medical advice and (2) when routine or preventative care was needed. We coded respondents who reported the hospital Emergency Department as their usual source of care as not having usual sources of care.
Unmet Needs for Healthcare
Separate measures identify respondents who reported difficulty finding physicians or delaying or foregoing care due to cost. We categorized respondents as delaying care due to availability problems if they reported difficulty scheduling appointments, waiting too long to get an appointment or at the doctor’s office, clinics not open when the respondent was available, or the respondent not having transportation to the clinic in the previous 12 months. Participants were coded as having foregone healthcare services if they reported being unable to afford prescription medications, mental healthcare, dental care, eyeglasses, specialist visits, or follow-up care.
Healthcare Utilization
Self-reported inpatient hospital stays, emergency department visits, and office-based visits over the past 12 months were measured using NHIS-defined categories. Inpatient hospital or emergency department visits were categorized into no stays/visits, 1 stay/visit, or more than 1 stay/visit because these were relatively rare events. The more frequently occurring outpatient visits were categorized into no visits, 1–3 visits, or ≥ 4 visits.
Other Measures
Self-reported race/ethnicity, marital status, educational attainment, sex, region of residence, and age were used as controls. Poverty status was measured as the family-sized adjusted income; publicly available imputations from the National Center for Health Statistics were used to account for non-response. Self-reported health insurance was categorized as uninsured, any private insurance, or public insurance only. We controlled for the following non-communication disabilities: physical, cognitive, visual, hearing, instrumental activities of daily living (IADL), and activities of daily living (ADL) disabilities.
Data Analysis
Analyses were conducted in 2016–2017 using Stata (version 11.0; Stata Corp.; College Station, TX),13 accounting for the Sample Adult weight and complex survey design. Statistical significance was defined as p < 0.05. We examined the unadjusted association between outcomes and CD using Pearson’s chi-squared test. Next, we used logistic and ordered logistic regressions (odds ratios (ORs)) to assess the outcome measures described above on CD, controlling for demographics and non-communication disabilities. Post-hoc analyses revealed that ordered logistic regressions violated the assumption of parallel lines; models that relaxed this assumption were substantively similar in magnitude, direction, and statistical significance.14 For ease of interpretation, we show the ordered logistic regression models here. For healthcare-related outcomes, we additionally controlled for chronic conditions. Other disability types were included as a control measure because a substantive body of literature has shown a significant overlap between these disability types and poor health and healthcare outcomes.15, 16 Models including other disability types revealed few differences (details available upon request). We chose to present the models controlling for other disability types to more conservatively assess the impact of CD on outcomes.
RESULTS
Of the 33,166 adults included in the sample, 6.3% of adults endorsed voice disabilities, 2.2% endorsed SL disabilities, and 1.3% endorsed SLV disabilities (Table 1). People without CD and those with voice disabilities were more frequently married, employed, and female than their counterparts with SL disabilities. Adults with SL and SLV disabilities more frequently reported public only health insurance and other co-occurring disabilities than did their peers without CD. Of note, 14.8% of persons without CD endorsed a non-communication disability vs. 23.8%, 53.5%, and 64.7% of persons with Voice, SL, and SLV disabilities, respectively.
Table 1.
Characteristics of Persons with and Without Communication Disabilities
| No comm. disability | Voice only disability | Speech/language (SL) disability | Speech/language + voice (SLV) disability | |
|---|---|---|---|---|
| % (n) | % (n) | % (n) | % (n) | |
| Total (n = 33,166) | 90.2 (29,820) | 6.3 (2160) | 2.2 (723) | 1.3 (463) |
| Female* | 51.1 (16,429) | 66.2 (1457) | 47.7 (363) | 48.5 (251) |
| Age (years; mean (SD))* | 46.4 (17.7) | 48.8 (18.8) | 45.0 (19.2) | 49.6 (20.9) |
| 18–24 | 12.7 (2930) | 11.9 (214) | 21.4 (95) | 16.6 (47) |
| 25–34 | 18.0 (5451) | 15.7 (324) | 14.2 (113) | 11.2 (48) |
| 35–44 | 17.3 (5111) | 14.3 (304) | 12.9 (98) | 11.1 (51) |
| 45–54 | 18.6 (5146) | 18.8 (351) | 16.8 (119) | 18.0 (82) |
| 55–64 | 16.2 (5016) | 16.4 (386) | 17.5 (146) | 18.4 (102) |
| ≥ 65 | 17.2 (6166) | 22.9 (581) | 17.2 (152) | 24.7 (133) |
| Race/ethnicity* | ||||
| Hispanic | 15.3 (5228) | 9.2 (230) | 15.3 (128) | 14.8 (75) |
| White, non-Hispanic | 66.8 (17,872) | 76.6 (1527) | 66.2 (411) | 66.8 (274) |
| Black, non-Hispanic | 11.6 (4457) | 10.8 (312) | 14.0 (148) | 14.4 (91) |
| Other, Non-Hispanic | 6.3 (2263) | 3.4 (91) | 4.5 (36) | 4.0 (23) |
| Marital status* | 54.1 (13,276) | 50.3 (860) | 36.5 (214) | 37.1 (133) |
| Employment status* | 62.3 (17,792) | 57.2 (1148) | 38.3 (274) | 35.9 (143) |
| Educational attainment* | ||||
| Less than high school | 13.7 (4642) | 11.6 (279) | 22.0 (194) | 27.9 (134) |
| High school graduate | 26.2 (7724) | 22.8 (525) | 30.6 (207) | 32.4 (141) |
| Some college | 20.4 (5901) | 22.5 (478) | 22.1 (155) | 22.7 (97) |
| College degree | 39.8 (11,553) | 43.1 (878) | 25.3 (167) | 17.1 (91) |
| Poverty status (imputed)* | ||||
| < 100% FPL | 13.4 (4993) | 12.8 (373) | 24.6 (213) | 25.4 (135) |
| 100–199% FPL | 19.0 (5412) | 19.3 (406) | 25.8 (167) | 27.9 (112) |
| 200–399% FPL | 29.9 (7552) | 30.5 (574) | 27.6 (166) | 30.3 (110) |
| ≥ 400% FPL | 37.7 (8775) | 37.4 (603) | 21.9 (113) | 16.3 (65) |
| Health insurance* | ||||
| Any private | 66.6 (18,575) | 69.7 (1397) | 49.0 (312) | 44.5 (192) |
| Public only | 16.3 (5830) | 17.7 (465) | 32.2 (271) | 39.9 (209) |
| Uninsured | 17.0 (5415) | 12.7 (298) | 18.8 (140) | 15.7 (62) |
| Region of residence* | ||||
| Northeast | 18.4 (5030) | 16.5 (339) | 16.6 (100) | 11.9 (54) |
| Midwest | 22.3 (6086) | 28.3 (556) | 24.2 (152) | 23.6 (92) |
| South | 36.5 (10,870) | 36.1 (757) | 37.3 (279) | 39.7 (181) |
| West | 22.8 (7834) | 19.2 (508) | 21.9 (192) | 24.8 (136) |
| Non-communication disabilities | ||||
| Any disability* | 14.8 (5067) | 23.8 (619) | 53.5 (422) | 64.7 (331) |
| Physical* | 8.1 (2956) | 15.8 (416) | 29.7 (239) | 47.0 (247) |
| Cognitive* | 3.9 (1284) | 7.1 (189) | 35.0 (278) | 41.1 (199) |
| Visual* | 2.9 (1018) | 5.7 (146) | 10.1 (86) | 23.6 (113) |
| Deaf or hard of hearing* | 4.5 (1472) | 7.0 (185) | 14.9 (118) | 22.4 (106) |
| IADL* | 4.2 (1516) | 7.7 (219) | 25.8 (201) | 37.5 (193) |
| ADL* | 2.1 (735) | 4.4 (114) | 14.0 (96) | 27.4 (128) |
Poverty status was imputed by the National Center for Health Statistics. N’s reflect the sample sizes that were not imputed
SL speech/language disability, SLV speech/language + voice disability, SD standard deviation, FPL federal poverty line, IADL instrumental activities of daily living, ADL activities of daily living
*p < 0.001
Health Outcomes
Adults with CD reported higher prevalence of any chronic conditions compared to persons without CD (Voice 67.9%, SL 68.6%, SLV 79.9%, no CD 49.9%, p < 0.001; Table 2, eTable 1). Only 25% of adults without CD reported ≥ 2 chronic conditions compared to 40% of people with Voice, 44% adults with SL, and 63% of adults with SLV disabilities (p < 0.001). Persons with CD were more likely to report additional chronic conditions compared to those without a CD, controlling for the measures in Table 1 (AOR (95% CI): Voice 1.9 (1.7–2.2), SL 1.7 (1.3–2.2), SLV 2.7 (1.9–3.8)).
Table 2.
Disability, Number of Chronic Conditions, and Self-rated Health Among Persons with Communication Disabilities Compared to Persons Without Communication Disabilities (n = 33,166)
| No comm. disabilities | Voice only disability | Speech/language (SL) disability | Speech/language + voice (SLV) disability | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % (n) |
% (n) |
p valuea | AOR (95% CI)b |
% (n) |
p valuea | AOR (95% CI)b |
% (n) |
p valuea | AOR (95% CI)b | |
| Self-rated healthc | ||||||||||
| Fair/poor |
11.2 (3948) |
19.5 (493) |
< 0.001 |
0.7 (0.6–0.8) |
32.5 (263) |
< 0.001 |
0.8 (0.7–1.0) |
48.3 (241) |
< 0.001 |
0.5 (0.4–0.7) |
| Good |
26.5 (8275) |
28.0 (639) |
0.001 |
27.4 (202) |
< 0.001 |
28.8 (141) |
< 0.001 | |||
| Very good/excellent |
62.3 (17,597) |
52.5 (1028) |
< 0.001 |
40.1 (258) |
< 0.001 |
23.0 (81) |
< 0.001 | |||
| Number of chronic conditionsc | ||||||||||
| None |
50.1 (14,209) |
32.1 (598) |
< 0.001 |
1.9 (1.7–2.2) |
31.4 (207) |
< 0.001 |
1.7 (1.3–2.2) |
20.1 (77) |
< 0.001 |
2.7 (1.9–3.8) |
| One |
25.0 (7472) |
27.5 (580) |
< 0.001 |
24.5 (177) |
0.002 |
17.2 (80) |
0.014 | |||
| ≥ 2 |
24.9 (8139) |
40.4 (982) |
< 0.001 |
44.1 (339) |
< 0.001 |
62.7 (306) |
< 0.001 | |||
SL speech/language disability, SLV speech/language + voice disability, AOR adjusted odds ratios, CI confidence interval
aBivariate comparison of the communication disability group to the group with no communication disabilities
bComparison of the communication disability group to the group with no communication disability, controlling for race/ethnicity, marital status, employment status, educational attainment, poverty status, region of residence, sex, age, health insurance, and non-communication disabilities
cNumber of chronic conditions and self-rated health were assessed using ordered logistic regression; adjusted odds ratios and 95% CIs are shown
Adults with CD were more likely to report fair/poor health compared to those without CD (Voice 19.5%, SL 32.5%, SLV 48.3%; no CD 11.2%; p < 0.001; Table 2). After controlling for the characteristics in Table 1, adults with CD were less likely to rate their health highly compared to adults without CD (AOR (95% CI): Voice 0.7 (0.6–0.8), SLV 0.5 (0.4–0.7)).
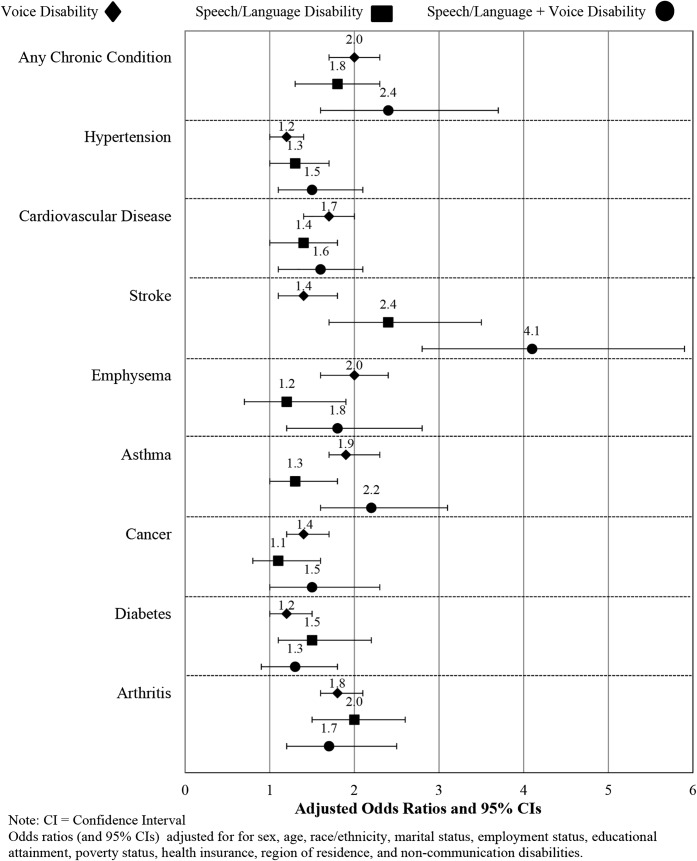
People across all CD types reported stroke, emphysema, and asthma more frequently than their peers without CD (eTable 1). Cardiovascular disease and diabetes were also more frequently reported by people with rather than without CD. Persons with Voice and SLV were 1.2–4.1 times more likely to report each of the specific chronic conditions compared to persons without CD, controlling for the measures in Table 1 (Fig. 1). Similarly, persons with SL CD were 1.3–2.4 times more likely to report the same chronic conditions as those without CD.
Fig. 1.
Forest plot of adjusted odds ratios (and 95% CI) of chronic conditions by communication disability groups, compared to persons without communication disabilities
Healthcare Outcomes
Adults with CD more frequently had ≥ 1 hospital stays and ≥ 1 emergency department visits than their peers without CD (≥ 1 hospital stay: Voice 14.0%, SL 17.1%, SLV 22.6%, no CD 8.5%. p < 0.001; ≥ 1 emergency department visits: Voice 27.5%, SL 38.1%, SLV 43.3%, no CD 18.1%, p < 0.001) (Table 3). Similarly, persons with CD more frequently had ≥ 1 office-based visits compared to people without CD (Voice 91.0%, SL 83.5%, SLV 86.3%, no CD 79.5%, p < 0.001) (Table 3). In analyses adjusted for the demographics and presence of non-communication disabilities described in Table 1, adults with CD had higher odds of more hospital stays (AOR (95% CI): Voice 1.3 (1.0–1.5)) and emergency department visits (AORs (95% CI): Voice 1.4 (1.2–1.6), SL 1.5 (1.1–1.9), SLV 1.5 (1.1–2.0)) compared to people without CD. Adults with Voice CD were 1.6 (95% CI 1.4–1.8) times more likely to have additional office-based visits than their peers without CD, accounting for the measures in Table 1. Persons with SL and SLV disabilities more frequently reported ≥ 4 visits (SL 48.3%; SLV 61.3%) compared to people without CD (34.8%, p < 0.001). However, these findings were not significant in multivariate results.
Table 3.
Healthcare Utilization for Persons with Communication Disorders Compared to Persons Without Communication Disorders (n = 33,166)
| No comm. disorder | Voice only disability | Speech/language (SL) disability | Speech/language + voice (SLV) disability | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % (n) |
% (n) |
p valuea | AOR (95% CI)b |
% (n) |
p valuea | AOR (95% CI)b |
% (n) |
p valuea | AOR (95% CI)b |
|
| Inpatient hospital stays | ||||||||||
| No stays |
91.5 (27,091) |
86.0 (1834) |
< 0.001 |
1.3 (1.0–1.5) |
82.9 (594) |
< 0.001 |
1.1 (0.8–1.6) |
77.4 (342) |
< 0.001 |
1.2 (0.8–1.7) |
| 1 stay |
6.3 (2001) |
9.4 (211) |
< 0.001 |
10.6 (81) |
< 0.001 |
11.3 (58) |
< 0.001 | |||
| ≥ 2 stays |
2.1 (728) |
4.5 (115) |
< 0.001 |
6.5 (48) |
< 0.001 |
11.3 (63) |
< 0.001 | |||
| Emergency department visits | ||||||||||
| No visits |
81.9 (24,158) |
72.5 (1505) |
< 0.001 |
1.4 (1.2–1.6) |
61.9 (442) |
< 0.001 |
1.5 (1.1–1.9) |
56.6 (256) |
< 0.001 |
1.5 (1.1–2.0) |
| 1 visit |
11.9 (3648) |
15.9 (381) |
< 0.001 |
19.7 (140) |
< 0.001 |
17.2 (82) |
< 0.001 | |||
| ≥ 2 visits |
6.2 (2014) |
11.6 (274) |
< 0.001 |
18.4 (141) |
< 0.001 |
26.2 (125) |
< 0.001 | |||
| Office-based visits | ||||||||||
| No visits |
20.5 (6193) |
9.0 (200) |
< 0.001 |
1.6 (1.4–1.8) |
16.5 (122) |
< 0.001 |
1.0 (0.8–1.2) |
13.7 (49) |
< 0.001 |
1.1 (0.8–1.5) |
| 1–3 visits |
44.7 (12,971) |
37.8 (764) |
< 0.001 |
35.2 (231) |
0.915 |
25.1 (108) |
0.452 | |||
| ≥ 4 visits |
34.8 (10,656) |
53.3 (1196) |
< 0.001 |
48.3 (370) |
< 0.001 |
61.3 (306) |
< 0.001 | |||
SL speech/language disability, SLV speech/language + voice disability, AOR adjusted odds ratios; CI confidence interval
aBivariate comparison of the communication disability group to the group with no communication disabilities
bOdds ratios comparing communication disability group to the group with no communication disability from ordered logistic regression analyses controlling for race/ethnicity, marital status, employment status, educational attainment, poverty status, region of residence, sex, age, health insurance, chronic conditions, and non-communication disabilities
cAdjusted odds ratios from logistic regression comparing each of the communication disability groups to the group with no communication disability are shown in Fig. 2
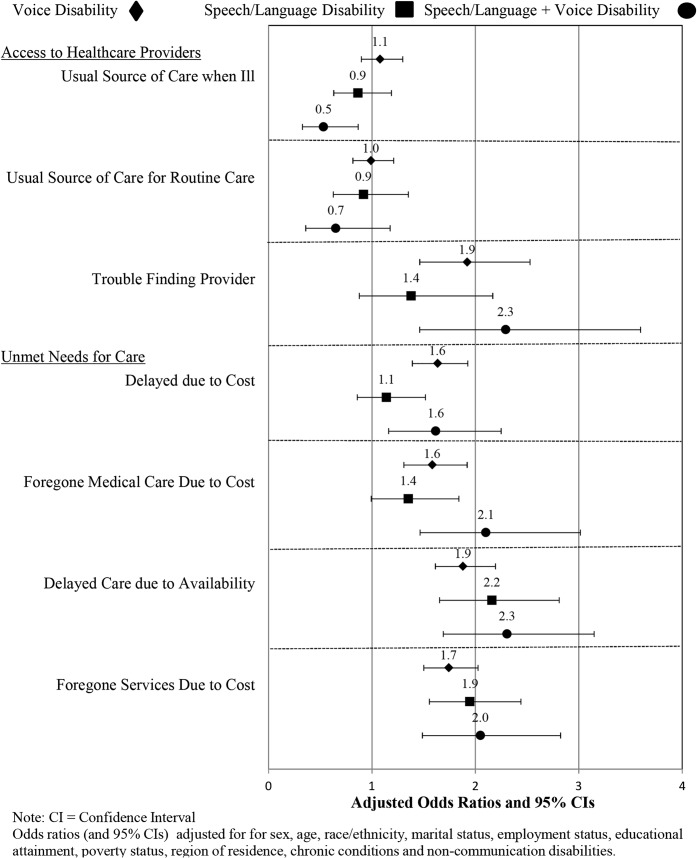
All persons with CD in this cohort endorsed higher rates of “trouble finding a provider” for healthcare (Fig. 2; e Table 2), although the confidence intervals for the adjusted odds ratios were only significant for persons with Voice and SLV disabilities (AOR (95% CI): Voice 1.9 (1.5–2.5), SL 1.4 (0.9–2.2), SLV 2.3 (1.5–3.6)). Persons with CD had different experiences in identifying usual sources of care for ill or routine care. For those measures, persons with Voice and SL disabilities endorsed similar experiences to persons without CD while persons with SLV disabilities had significantly greater difficulties identifying a usual source of care when ill (usual source of care when ill: AOR (95% CI): Voice 1.1 (0.9–1.3)), SL 0.9 (0.6–1.2), SLV 0.5 (0.3–0.9)).
Fig. 2.
Forest plot of adjusted odds ratios (and 95% CI) of access to care by communication disability groups, compared to persons without communication disabilities
Persons with CD more frequently reported unmet needs for care than persons without CD (for example, delayed healthcare due to cost: Voice 16.4%; SL: 17.0%; SLV: 23.9%; no CD: 10.4%, p < 0.001 for pairwise comparisons; delayed due to availability: Voice: 18.9%; SL: 25.2%; SLV: 30.8%; no CD: 9.4%, p < 0.001 for pairwise comparisons). All CD groups reported greater unmet needs for care, with adjusted odds ranging from 1.6 (95% CI 1.3–1.9, foregone medical care due to cost) to 2.3 (95% CI 1.7–3.1, delayed care due to availability).
DISCUSSION
This study provides the first descriptions of health and healthcare outcomes among persons with CD in the U.S. We observed that persons with CD are generally more medically complex and have greater challenges accessing care than people without CD, despite controlling for demographics, other non-communication disability types, and chronic conditions.
Persons with CD were as likely as those without CD to have usual sources of care for routine care and illness. Despite this, they frequently reported unmet healthcare needs due to cost, lack of availability, and difficulty finding healthcare providers. These challenges may be related to the fact that this is an unhealthy population with low financial resources and high rates of public insurance, which is not accepted by all providers. Communication barriers amplify these difficulties. Patients with hearing disabilities report challenges scheduling appointments over the phone.17 Similarly, patients with CD report frequently switching healthcare providers as a consequence of communication challenges with providers and staff.6 The negative effects of communication challenges are unsurprising given that it is well-documented that people with limited English proficiency, a population that also presents with communication challenges, also face multiple barriers to accessing care.18
Persons with CD have high rates of healthcare utilization, despite reporting difficulty finding providers and having unmet care needs. Approximately 50% of people with CD reported having ≥ 4 office-based visits in the previous year. A quarter of those with SLV disabilities had ≥ 2 emergency department visits and 22% had ≥ 1 inpatient hospital stay in the past year. The frequency of interactions with healthcare settings highlights the need for healthcare providers and systems to be prepared for communicating with and providing care for patients with CD.
Despite previous studies that show that voice disabilities are less severe than SL disabilities, we found that adults with voice disabilities, both alone and accompanied by SL disabilities, were more likely to report chronic conditions and greater challenges accessing care compared to those without CD. This is a critical finding, as 7% of the US population reports voice disabilities.1 Other studies have found that persons with voice disabilities report lower quality of life and health compared to those without voice disabilities.19 Further research is needed to understand what factors contribute to lower quality of health care, health, and access for this relatively large portion of the US population.
The results of this study are consistent with research findings in other disability populations. A study comparing people without disabilities to people with either cognitive or physical disabilities found that those with disabilities had higher rates of chronic conditions and were less likely to rate their health as good; however, they were more likely to have usual sources of care.15 While the prevalence of co-occurring disabilities among the group of people with CD is high, we found that disparities in health and healthcare outcomes based on CD persisted compared to people without CD. This suggests that there is something particular about CD that contributes to differences in health and healthcare utilization.
Providing care for patients with CD is inherently difficult due to communication challenges. The Joint Commission names those with CD as a population at high risk for ineffective communication and calls for healthcare systems and clinicians to provide additional supports to ensure effective communication and high-quality healthcare.20 Additionally, Section 1557 of the Patient Protection and Affordable Care Act mandates that hospitals and clinics provide patients with disabilities “auxiliary aids and services” to ensure equitable access to healthcare communication.21 Unfortunately, providers receive little, if any, training or support in this area.22 Clinical encounters with people with CD often take longer (due to communication barriers and the fact that they have higher rates of multiple chronic conditions) and tools and strategies to ensure effective communication may not be evident. For example, research has shown that people with CD have improved comprehension and participation in conversations when communication partners use strategies such as writing down key words while speaking or using visual aids.23 Yet, a study of video-recorded clinical encounters revealed that clinicians rarely, if ever, used evidence-based communication strategies with patients with language disabilities.8 Providing clinicians the right supports and tools to effectively communicate with patients with CD has the potential to significantly improve the quality of care provided to this vulnerable population.
The 2012 NHIS was the first national survey of health and healthcare to specifically query CD. Our results reveal the presence of significant disparities in health and healthcare delivery among persons with CD and strongly suggests that questions about CD be included on future national surveys. This will support longitudinal tracking, which is critical to identifying trends in health and healthcare outcomes for patients with CD and supporting positive health and healthcare outcomes.
Limitations
The NHIS is cross-sectional by design and, thus, it is not possible to determine the causality of chronic conditions and the presence of CD. Certain CD are more likely to result from chronic conditions. For example, the high rates of stroke in those with SL disabilities is not surprising given that approximately 1 million people in the USA are living with aphasia, a language disorder most often caused by stroke.24 Regardless of the cause of the specific CD, we found that the majority of those with CD (68 to 80%) live with at least one chronic condition that requires continued medical intervention. Therefore, providing effective healthcare that is sensitive to the needs of this population is paramount to ensuring that patients with CD achieve the most optimal health possible.
CONCLUSIONS
Persons with CD are an understudied and overlooked population in our healthcare system, even though they represent 10% of the US population, have high rates of healthcare utilization, and experience significant disparities in health and healthcare outcomes. Moving the needle to improve the health of our nation necessitates that our healthcare providers and systems be prepared to provide high-quality patient-centered healthcare to patients with CD.
Electronic Supplementary Material
(DOCX 32 kb)
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
References
- 1.Morris MA, Meier SK, Griffin JM, Branda ME, Phelan SM. Prevalence and etiologies of adult communication disabilities in the united states: Results from the 2012 national health interview survey. Disability and Health Journal. 2016;9(1):140–144. doi: 10.1016/j.dhjo.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine . Workshop on disability in america: A new look: Summary and background papers. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- 3.Havercamp SM, Scandlin D, Roth M. Health disparities among adults with developmental disabilities, adults with other disabilities, and adults not reporting disability in north carolina. Public Health Rep. 2004;119(4):418–426. doi: 10.1016/j.phr.2004.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krahn GL, Walker DK, Correa-De-Araujo R. Persons with disabilities as an unrecognized health disparity population. Am J Public Health. 2015;105(S2):S198–S206. doi: 10.2105/AJPH.2014.302182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoffman JM, Yorkston KM, Shumway-Cook A, Ciol MA, Dudgeon BJ, Chan L. Effect of communication disability on satisfaction with health care: A survey of medicare beneficiaries. American Journal of Speech-Language Pathology. 2005;14(3):221–228. doi: 10.1044/1058-0360(2005/022). [DOI] [PubMed] [Google Scholar]
- 6.Morris MA, Dudgeon BJ, Yorkston K. A qualitative study of adult AAC users’ experiences communicating with medical providers. Disability and Rehabilitation: Assistive Technology. 2013;8(6):472–481. doi: 10.3109/17483107.2012.746398. [DOI] [PubMed] [Google Scholar]
- 7.Murphy J. Perceptions of communication between people with communication disability and general practice staff. Health Expectations. 2006;9(1):49–59. doi: 10.1111/j.1369-7625.2006.00366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morris MA, Clayman ML, Peters KJ, Leppin AL, LeBlanc A. Patient-centered communication strategies for patients with aphasia: Discrepancies between what patients want and what physicians do. Disability and health journal. 2015;8(2):208–215. doi: 10.1016/j.dhjo.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 9.Nicolaidis C, Raymaker D, McDonald K, et al. Comparison of healthcare experiences in autistic and non-autistic adults: A cross-sectional online survey facilitated by an academic-community partnership. Journal of general internal medicine. 2013;28(6):761–769. doi: 10.1007/s11606-012-2262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nordehn G, Meredith A, Bye L. A preliminary investigation of barriers to achieving patient-centered communication with patients who have stroke-related communication disorders. Topics in Stroke Rehabilitation. 2006;13(1):68–77. doi: 10.1310/5K2W-P6CD-EFDF-8HG4. [DOI] [PubMed] [Google Scholar]
- 11.Bartlett G, Blais R, Tamblyn R, Clermont RJ, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555–1562. doi: 10.1503/cmaj.070690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics . Data file documentation, national health interview survey, 2012 (machine reaable data file and documentation) Hyattsville: National Center for Health Statistics, Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 13.StataCorp L. Stata 15.1 for windows. . 2017.
- 14.Williams R. Generalized order logit/partial proprotional odds models for ordinal dependent variables. The Stata Journal. 2006;6(1):58–82. doi: 10.1177/1536867X0600600104. [DOI] [Google Scholar]
- 15.Reichard A, Stolzle H, Fox MH. Health disparities among adults with physical disabilities or cognitive limitations compared to individuals with no disabilities in the united states. Disability and Health Journal. 2011;4(2):59–67. doi: 10.1016/j.dhjo.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Reichard A, Gulley SP, Rasch EK, Chan L. Diagnosis isn’t enough: Understanding the connections between high health care utilization, chronic conditions and disabilities among US working age adults. Disability and health journal. 2015;8(4):535–546. doi: 10.1016/j.dhjo.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iezzoni LI, O’Day BL, Killeen M, Harker H. Communicating about health care: Observations from persons who are deaf or hard of hearing. Ann Intern Med. 2004;140(5):356–362. doi: 10.7326/0003-4819-140-5-200403020-00011. [DOI] [PubMed] [Google Scholar]
- 18.Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured: Findings from a national sample. Med Care. 2002;40(1):52–59. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Merrill RM, Anderson AE, Sloan A. Quality of life indicators according to voice disorders and voice-related conditions. Laryngoscope. 2011;121(9):2004–2010. doi: 10.1002/lary.21895. [DOI] [PubMed] [Google Scholar]
- 20.The Joint Commission . Advancing effective communication, cultural competence, and patient- and family-centered care: A roadmap for hospitals. Oakbrook Terrace: The Joint Commission; 2010. [Google Scholar]
- 21.Nondiscrimination in health programs and activities, final rule. Fed Regist. 2016;81(96):31375–31473. [PubMed]
- 22.Burns MI, Baylor CR, Morris MA, McNalley TE, Yorkston KM. Training healthcare providers in patient–provider communication: What speech-language pathology and medical education can learn from one another. Aphasiology. 2012;26(5):673–688. doi: 10.1080/02687038.2012.676864. [DOI] [Google Scholar]
- 23.Simmons-Mackie N, Raymer A, Armstrong E, Holland A, Cherney LR. Communication partner training in aphasia: A systematic review. Arch Phys Med Rehabil. 2010;91(12):1814–1837. doi: 10.1016/j.apmr.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 24.National Institute on Deafness and Other Communication Disorders. Aphasia. https://www.nidcd.nih.gov/health/aphasia. Updated 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 32 kb)