Abstract
Background:
Achilles tendon (AT) ruptures are one of the most common tendon ruptures, but there have been no studies investigating these injuries in the United States (US) using data representative of the entire US population.
Purpose/Hypothesis:
The purpose of this study was to determine the incidence and risk factors for AT ruptures in the US. We hypothesized that male sex, older age, and sport participation would increase the risk for AT ruptures.
Study Design:
Descriptive epidemiology study.
Methods:
All patients presenting to an emergency department with ruptured AT in the US from 2012 through 2016 were selected from the National Electronic Injury Surveillance System (NEISS) database. Incidence was calculated for sex, race, and age. AT ruptures were characterized based on the mechanism of injury, with subanalyses performed on sport-related AT ruptures to examine sex-, race-, and age-related differences.
Results:
From 2012 to 2016, a significant increase in the incidence of AT ruptures was observed, from 1.8 per 100,000 person-years in 2012 to 2.5 per 100,000 person-years in 2016 (P < .01), for an overall incidence of 2.1 per 100,000 person-years. The majority of AT ruptures occurred in male compared with female patients, with an incidence rate ratio of 3.5 (P < .01). The largest overall incidence of AT ruptures occurred in those aged 20-39 years for male patients (5.6/100,000 person-years) and in those aged 40-59 years for female patients (1.2/100,000 person-years). The largest rise in the incidence of AT ruptures during the study period was observed in patients aged 40-59 years (78% increase). The most common injury mechanism was participation in a sport or recreational activity (81.9% of all injuries), with basketball being the most common overall cause of AT ruptures.
Conclusion:
While AT ruptures in the US most commonly occur in young male patients (20-39 years old), the largest rise in the incidence was observed in middle-aged patients (40-59 years old), with participation in recreational sports being the most likely mechanism. Recognizing high-risk patients can help physicians counsel them and recommend strategies for injury prevention.
Keywords: Achilles tendon, tendon rupture, epidemiology, database, NEISS, basketball
An acute rupture of the Achilles tendon (AT) is one of the most common tendon injuries in the adult population, with incidences ranging between 7 and 40 per 100,000 person-years.3,7,15,20–22,32,40 Acute ruptures of the AT can be caused by sudden excessive loading, cumulative degeneration, or less commonly as a manifestation of systemic disease.17 Despite the fact that a majority of patients who sustain acute AT ruptures do not report prodromal symptoms, histological studies have shown most patients to have evidence of cumulative degenerative changes.2,11 Aside from degeneration, other factors increasing the risk of ruptures are anabolic steroids, fluoroquinolone usage, and local corticosteroid injections.16,35
The incidence of AT ruptures has increased over the past decade. It is believed that increased participation in physical activity by older patients is contributory to this rising incidence.5,21 Studies have shown that a majority of AT ruptures occur during sport participation and primarily in middle-aged men, leading to the consensus that male recreational athletes are most at risk for these injuries.4,13,15,21,32
Presently, the majority of studies investigating the incidence of AT ruptures have been performed outside of the United States (US), and the limited number of studies performed in the US have analyzed samples not representative of the entire US population.‡ Therefore, little is known about the true epidemiology of AT ruptures in the general population of the US. The purpose of this study was to utilize the National Electronic Injury Surveillance System (NEISS) database, which is representative of cases from emergency departments (EDs) in the US, to determine the incidence and risk factors for AT ruptures. We hypothesized that male sex, older age, and participation in sports will place patients at an increased risk of AT ruptures.
Methods
Data Collection
This was a retrospective study using data from the NEISS, which is a public database operated by the US Consumer Product Safety Commission (CPSC). The NEISS database contains deidentified public data, and institutional review board approval is not required to analyze the data, per 45 Code of Federal Regulations 46.102. The NEISS database receives information on all injury-related visits to EDs from 100 hospitals. These hospitals are a stratified sample of all the hospitals containing EDs in the US and its territories. This includes both adult and children’s hospitals as well as trauma centers and community hospitals in both rural and urban areas. Each case is assigned a statistical weight based on the inverse probability of being selected. The CPSC annually ensures the accuracy of the sample by using a new sampling frame each year to allow for NEISS sample weights to reflect the total number of ED visits that occur nationally during a specific year. Variables included in the database for each case are the treatment date, patient age, sex, race, diagnostic category, body part injured, patient disposition, place of injury, and 2 descriptive narrative fields. The NEISS database has been used to analyze injury epidemiology with US population census data, for which the dataset is specifically configured.6,9,12,24,30
To isolate all potential AT ruptures, the NEISS database was queried for all lower leg injuries (code 36) diagnosed as a ruptured tendon, ligament, or muscle (code 64) from 2012 to 2016. Injury narratives were reviewed to only select cases with a clear diagnosis of an AT rupture or tear. All cases in which the narratives described an alternative diagnosis (eg, tendinitis) were excluded. After screening, 15% of the original cases (854/5564) met inclusion criteria.
For sport-related AT ruptures, cases were queried using the location variable for injuries that occurred at a place of sport/recreation. After this, the remaining cases were individually checked to include any other case that was sport related but not categorized as an injury occurring at a place of sport/recreation.
Statistical Analysis
To determine incidence rates, The US Census Bureau’s34 population statistics were used to calculate person-years at risk according to sex, age, and race. For ease of calculation, patients were divided into 20-year age groups. The incidence of AT ruptures was calculated using NEISS sample weights. The injury incidence was reported per 100,000 person-years at risk to standardize injury rates and allow for an easier comparison between other injury types; 95% CIs were calculated for all national incidence estimates. The incidence rate ratio (IRR) was used to compare the incidence rate among subgroups, using a reference subgroup’s incidence as the denominator.
Analysis of variance and chi-square analysis were used for the comparison of continuous and categorical data, respectively. Z test column proportions were used for post hoc analysis after chi-square analysis. P values were adjusted using the Bonferroni method. Analyses were performed using Excel (Microsoft), SPSS version 24 (IBM), and OpenEpi version 3.02 (Emory University). Statistical significance was defined as a P value <.05.
Results
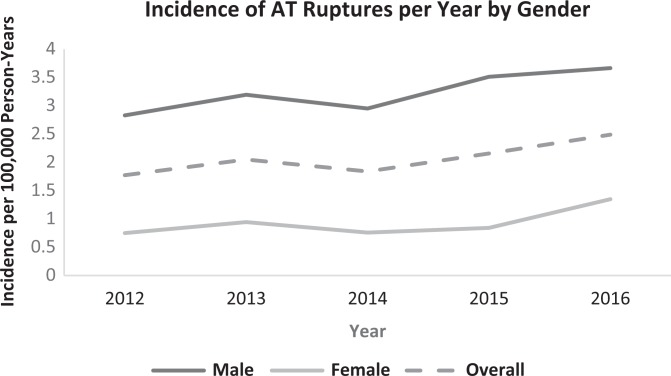
Between 2012 and 2016, 854 AT ruptures were identified, representing a national estimate of 32,906 ruptures. During this time, there was a significant increase in the incidence of AT ruptures from 1.8 (95% CI, 1.7-1.8) per 100,000 person-years in 2012 to 2.5 (95% CI, 2.4-2.5) per 100,000 person-years in 2016 (P < .01), for an overall incidence of 2.1 (95% CI, 2.0-2.1) per 100,000 person-years (Figure 1).
Figure 1.
Annual incidence of Achilles tendon (AT) ruptures from 2012 to 2016 by sex.
Sex
Male patients accounted for 25,374 weighted AT ruptures (77.1%), while female patients accounted for 7533 (22.9%). The overall incidence of AT ruptures for male and female patients was 3.2 (95% CI, 3.20-3.27) and 0.9 (95% CI, 0.90-0.95) per 100,000 person-years, respectively (Figure 1). An IRR of 3.5 (95% CI, 3.4-3.6; P < .01) demonstrated AT ruptures in male patients to be significantly greater than in female patients.
Age
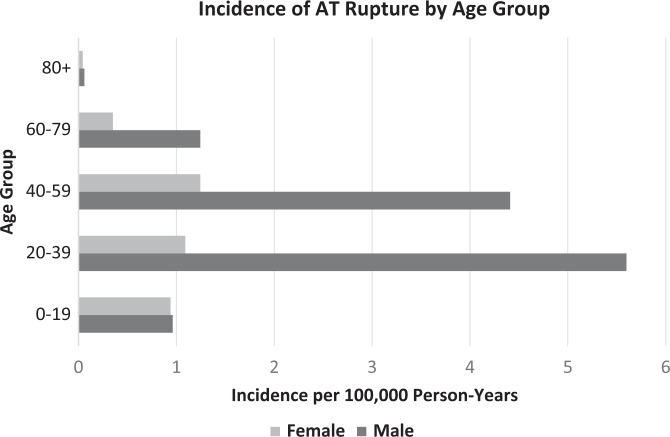
The age of patients ranged from 7 to 85 years, for an overall mean of 37.5 ± 13.9 years. The mean age for male and female patients was 38.0 ± 13.9 years and 36.2 ± 16.9 years (P < .01), respectively. The largest incidence of AT ruptures occurred between ages 20-39 years for male patients, with 5.6 (95% CI, 5.5-5.7) per 100,000 person-years, and between ages 40-59 years for female patients, with 1.2 (95% CI, 1.2-1.3) per 100,000 person-years (Figure 2).
Figure 2.
Overall incidence of Achilles tendon (AT) ruptures from 2012 to 2016 by age group.
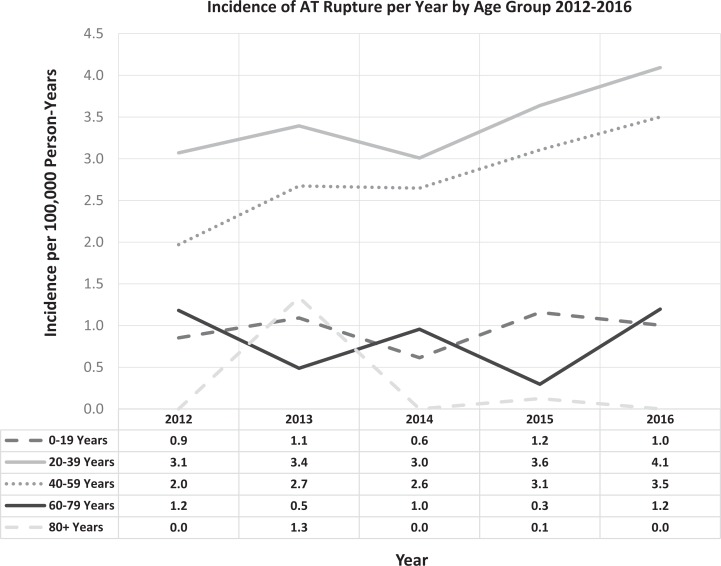
The largest rise in the incidence of AT ruptures during the study period was observed in patients aged 40-59 years, increasing by 78% (2.0-3.5/100,000 person-years), followed by a 33% increase in those aged 20-39 years (3.1-4.1/100,000 person-years) (Figure 3).
Figure 3.
Annual incidence of Achilles tendon (AT) ruptures from 2012 to 2016 by age group.
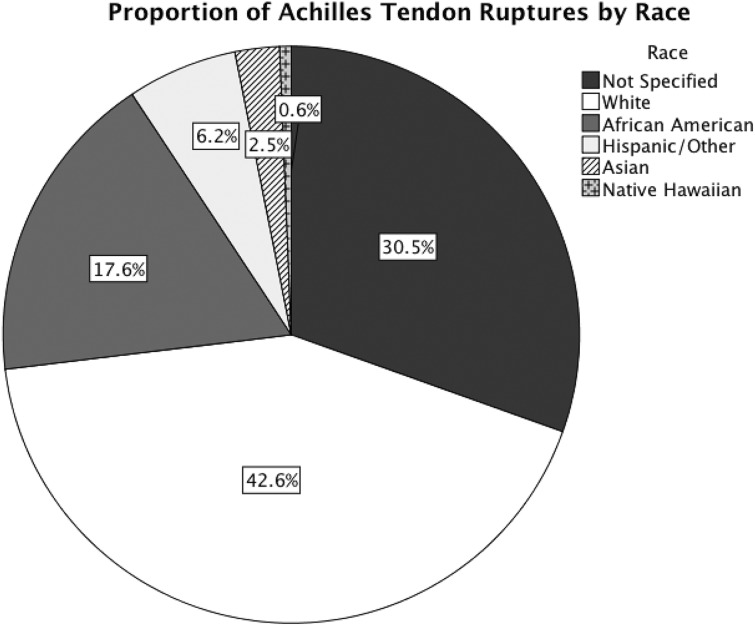
Race
Race was available for 69.5% of AT ruptures. White patients accounted for 14,027 estimated cases (42.6%), representing the largest proportion of patients presenting to the ED for AT ruptures, followed by African Americans (n = 5790, 17.6%) (Figure 4).
Figure 4.
Distribution of Achilles tendon ruptures in the United States from 2012 to 2016 by race.
The incidence rate for AT ruptures was highest for Native Hawaiians/Pacific Islanders at 5.6 (95% CI, 4.9-6.4) per 100,000 person-years, followed by 2.5 (95% CI, 2.4-2.5) for African Americans, 1.2 (95% CI, 1.18-1.21) for whites, 0.8 (95% CI, 0.8-0.9) for Asians, and 0.6 (95% CI, 0.57-0.63) for Hispanics. When comparing AT ruptures to white patients, the IRR was 4.7 (95% CI, 4.1-5.4) for Native Hawaiians/Pacific Islanders, 2.0 (95% CI, 2.0-2.1) for African Americans, 0.7 (95% CI, 0.6-0.7) for Asians, and 0.5 (95% CI, 0.48-0.51) for Hispanics (P < .01). Basketball accounted for the largest proportion of AT ruptures in white patients (46.5%), African Americans (79.7%), and Asians (51.9%). In Hispanics, soccer accounted for the largest percentage of AT ruptures (55.2%), and hiking/running/stretching accounted for the largest proportion of injuries in Native Hawaiians/Pacific Islanders (35.4%). The mean age was 38.6 ± 16.0 years for white patients, 33.5 ± 11.9 years for African Americans, 34.9 ± 11.2 years for Hispanics, 33.3 ± 9.6 years for Asians, and 45.7 ± 4.6 years for Native Hawaiians/Pacific Islanders.
Location
The majority of AT ruptures occurred at a sporting venue (47.7%). This was followed by “location–not specified” (37.2%), home (8.7%), school (2.4%), a public place (2.3%), and the street (1.7%). The mean age for patients sustaining an AT rupture differed between locations; the age of patients injured at school (18.4 ± 8.7 years) was lower compared with those injured at a sporting venue (36.6 ± 12.9 years), home (43.3 ± 8.7 years), a public place (41.9 ± 16.0 years), and the street (49.2 ± 15.0 years) (P < .01).
Mechanism
The injury mechanism was reported for 100% of the cases. The most common injury mechanism was participation in a sport or recreational activity, accounting for 81.9% of injuries. Basketball was the most common cause of AT ruptures for all patients younger than 60 years (Table 1). Of all injuries related to sport participation, basketball (42.6%), soccer (9.9%), football (8.4%), tennis (6.9%), and running/hiking/stretching (5.8%) were the most common.
TABLE 1.
Top 5 Injury Mechanisms for Achilles Tendon Ruptures by Age Group
| Rank | 0-19 Years | 20-39 Years | 40-59 Years | 60-79 Years | ≥80 Years | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mechanism | n (%) | Mechanism | n (%) | Mechanism | n (%) | Mechanism | n (%) | Mechanism | n (%) | |
| 1 | Basketball | 780 (20.0) | Basketball | 6838 (46.2) | Basketball | 3616 (30.5) | Tennis | 385 (17.7) | Running/hiking/stretching | 79 (45.7) |
| 2 | Football | 459 (11.7) | Soccer | 1243 (8.4) | Stair related | 1341 (11.3) | Stair related | 285 (13.1) | Golf | 79 (45.7) |
| 3 | Running/hiking/stretching | 335 (8.6) | Football | 1180 (8.0) | Running/hiking/stretching | 1218 (10.3) | Running/hiking/stretching | 269 (12.4) | Sink related | 15 (8.7) |
| 4 | Bicycling | 247 (6.3) | Running/hiking/stretching | 1072 (7.2) | Soccer | 952 (8.0) | Ball sport/other (ie, kickball, etc) | 112 (5.1) | ||
| 5 | Soccer | 240 (6.1) | Volleyball | 585 (3.9) | Tennis | 396 (3.3) | Door related | 103 (4.7) | ||
Patients aged 20-39 years sustained the most sport-related AT ruptures (54.4%), followed by those aged 40-59 years (32.5%) and those aged 0-19 years (8.5%). Volleyball made up the largest proportion of sport-related AT ruptures in female patients (15.2%), while basketball was the most common sport-related mechanism in male patients (46.9%) (Table 2).
TABLE 2.
Top 5 Injury Mechanisms for Achilles Tendon Ruptures by Sex
| Rank | Female | Male | ||
|---|---|---|---|---|
| Mechanism | % | Mechanism | % | |
| 1 | Volleyball | 15.2 | Basketball | 46.9 |
| 2 | Basketball | 14.8 | Soccer | 10.6 |
| 3 | Track and field | 9.8 | Football | 9.0 |
| 4 | Gymnastics | 8.9 | Tennis | 7.4 |
| 5 | Running/hiking/stretching | 8.5 | Running/hiking/stretching | 5.4 |
Discussion
To our knowledge, this is the largest epidemiological study of AT ruptures in the US (1.6 billion person-years at risk) and the first to assess a patient demographic sample representative of the US population. A total of 5564 (unweighted) cases of lower leg tendon/muscle injuries presented to EDs included in the NEISS database, with 15% (854/5564) of these injuries having a diagnosis of an AT rupture. Between 2012 and 2016, we found a significant increase in the incidence of AT ruptures from 1.8 to 2.5 per 100,000 person-years, with the largest rise observed in those aged 40-59 years. Male patients aged 20-39 years participating in sports were at the greatest risk for injuries. By race, Native Hawaiians/Pacific Islanders had the highest incidence of AT ruptures.
A majority of studies investigating the incidence of AT ruptures have been conducted in Europe.13,15,21,22 Few have been performed in the US, and those studies were limited by their study populations.4,7,32,41 Investigations by White et al41 and Davis et al4 were both confined to US military cadets. Raikin et al32 retrospectively analyzed 400 adult patients at a single institution, resulting in selection bias, both geographically and socioeconomically. Conversely, we identified 854 AT ruptures, representing a weighted total of 32,906 ruptures, from a sample that is representative of the entire nation and therefore more representative of the true incidence of AT ruptures in the US.
Erickson et al7 assessed the incidence of nontraumatic AT ruptures among a US Medicare population between 2005 and 2011. They reported an incidence of 6.7 to 10.8 AT tears per 100,000 person-years, which is more than double the incidence observed in the present study (1.8-2.5/100,000 person-years). This discrepancy may be explained by the study population, of which a majority of the patients were older than 65 years. To the contrary, children and adolescents were included in the present study and may have contributed to a decrease in the overall incidence, as AT ruptures are less common in this age group.37 Additionally, the NEISS database does not account for patients with AT ruptures who present to providers outside of the ED, including primary care physicians and athletic trainers. Another discrepancy was that Erickson et al7 found no difference in the incidence of AT ruptures between sexes, while we observed an IRR of 3.5 (95% CI, 3.4-3.6) between male and female patients. Because they focused on nontraumatic AT ruptures in Medicare patients, Erickson et al7 may have underrepresented the middle-aged male “weekend warriors” most at risk for AT ruptures.
From 2012 through 2016, the number of AT ruptures increased by 39%, mirroring the rise in the incidence observed in other studies.15,17,21,32,33 The largest cross-sectional study examining trends in the incidence of AT ruptures was performed by Lantto et al21 in Oulu, Finland; these authors found a 900% increase in the incidence of AT ruptures from 1979 to 2011. AT ruptures in male patients aged 60-69 years participating in sports had the largest rise in incidence in that study. The authors speculated that the increase observed in this population was caused by the growing popularity of recreational activities and the building of multiple sport halls in the city, although they were unable to support this. In the present study, male patients aged 40-59 years experienced the largest increase in AT ruptures. Similar to what has been observed in Finland, the rise in AT ruptures in the US is likely related to the increase in activity levels and sport participation by older adults.5,18 Other potential reasons to consider include increased utilization of the ED as well as improved awareness and detection of AT ruptures by ED physicians.
Among all age groups, the highest incidence of AT ruptures was found in male patients aged 20-39 years. Our findings suggest that those with AT ruptures in the US may be younger than their counterparts in other countries, where the highest incidence has been observed in those older than 40 years.13,15 Despite the scarcity of literature comparing the incidence and characteristics of AT ruptures between different countries, assumptions can be made, which include higher body mass indexes (BMIs) in North American patients compared with those in Europe. While the NEISS database did not report patients’ BMI, other studies have noted an increased risk of AT ruptures in those with a BMI larger than 25 kg/m2, with a previous study showing only 23% of the patients sustaining AT ruptures in the US to have a normal BMI.19,32 Additionally, despite recent increases in the activity levels of US residents, older adults still may be less active compared with their counterparts in Scandinavian countries and therefore at a lower risk for AT ruptures.10
Native Hawaiians/Pacific Islanders were found to have the highest incidence of AT ruptures and an IRR of 4.7 compared with white patients. To our knowledge, this is the first report showing the aforementioned population to be at a heightened risk for AT ruptures. The increased incidence in this population may be because of widespread participation in outdoor activities in the Hawaiian Islands, as the most common mechanism of injury in this population was running/hiking/stretching. Additionally, compared with other patients, Native Hawaiians/Pacific Islanders were significantly older, with a mean age of 45.7 years. Previous studies have reported African Americans to be the most at risk for all tendon ruptures, including the AT.4,29,41 Owens et al29 investigated racial differences among major tendon ruptures occurring in the military and observed an IRR of 3.4 for AT ruptures in African Americans compared with white patients. Our results are in line with this finding, with an observed IRR of 2.0. Multiple explanations for a predisposition in African Americans have been proposed. The AT in African Americans has been shown to differ in its biomechanical properties, with decreased elasticity and increased stiffness compared with the AT in white patients.8 Another reason may be differences in body weight, as African Americans have higher average BMIs compared with white patients in the US.38 We also must consider the possibility that the increased incidence observed in the aforementioned populations is related to socioeconomic issues that cause them to present more frequently to the ED rather than seeking care at more traditional office-based practices.
During sports and recreational activities, tendons are subjected to large forces and are responsible for transmitting them to the skeletal system. Excessive eccentric muscle activation is largely responsible for tendon ruptures. The risk of ruptures has been shown to increase during plyometric activities (eg, jumping), when a large eccentric force is followed by a large concentric contraction.27 To this end, we found 81.9% of all ruptures to be sport/exercise related, which is a slightly larger proportion than in other studies.21,26 The distribution of sport-related AT ruptures may vary according to recreational cultures. In the present study, basketball, soccer, tennis, football, and running/hiking/stretching were the most common sports that resulted in AT ruptures. In Finland, volleyball, badminton, and soccer have been shown to be responsible for the largest proportion of sport-related AT ruptures, and Denmark highlighted badminton, soccer, handball, and volleyball.13,21,22 Despite these differences, a similarity among all of these sports is the requirement and frequency of rapid changes in direction and jumping, which are actions that put one at risk for AT ruptures, given the mechanics of such activities, as mentioned above.17
In every age group younger than 60 years, basketball was the most common cause of AT ruptures (42.6% of all AT ruptures), with the largest proportion of basketball-related AT ruptures occurring in those aged 20-39 years and patients of African American race.38 Despite a majority of basketball-related AT ruptures occurring in recreational athletes, AT ruptures in National Basketball Association (NBA) players are also common and can have devastating outcomes compared with other injuries, with 40% of players not returning to play in the NBA after an AT rupture.1,23 Similar findings have been reported in National Football League (NFL) players, with 32% of players unable to return to play after an AT rupture.31 Given the decreased athletic requirements of recreational athletes, “weekend warrior” patients may have more optimistic return-to-play rates. In a recent meta-analysis of 85 studies that addressed return-to-play rates after an AT rupture, Zellers et al42 reported that 80% of athletes returned to play after an AT rupture. Despite a large proportion of these athletes returning to play, patients should be counseled that a smaller percentage of athletes return to the same level of play/performance, and to do so may require ongoing follow-up and rehabilitation.
Although the NEISS has been used to characterize the epidemiology of other injuries in the US and is an established database for epidemiological research, there are limitations.6,25,28,36,39 The database does not account for patients who received care outside of EDs, such as at outpatient clinics, urgent care centers, and high school/collegiate athletic training rooms. Therefore, the incidence observed in this study is likely an underestimate of the true incidence, and selection bias may exist with regard to which patients present to the ED. Additionally, because data regarding race were unknown for 30.5% of participants, the race-specific incidence rates were likely underestimated. Similarly, the location of injury was unreported in 37% of the cases. Although we speculate a similar distribution of injury locations among the cases in which location was not identified, this cannot be confirmed. While this limitation does not take away from the major findings of the study, our findings regarding injury location should be read with caution.
Furthermore, the diagnoses reported in the NEISS database are unable to be confirmed, and the included narratives are sometimes inconsistent and do not provide uniform information on injury data, such as an athlete’s level of play, if the injury occurred during competition or practice, and if the injury was a primary injury or recurrent. Finally, the low incidence of AT ruptures in certain age groups, specifically in those older than 80 years, makes it difficult to accurately assess injury trends among such patients. Despite these limited weaknesses, the NEISS is a nationwide database consisting of a heterogeneous patient population with significant external validity. For this reason, we believe that it demonstrates the most accurate incidence rate of AT ruptures in the US compared with previous studies on more limited populations.4,7,32
In summary, our findings indicate that AT ruptures account for thousands of injuries in the US annually, with certain subgroups being at an increased risk, including male patients, those older than 20 years, and those participating in sports/recreational activities. There should be awareness of these at-risk populations to assist providers with identifying those most likely presenting with AT ruptures and to aid with counseling those patients suffering from an AT rupture.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: B.D.O. is a paid consultant for DePuy, Medical Device Business Services, Rotation Medical, Sanofi-Aventis, Linvatec, and the Musculoskeletal Transplant Foundation; has received honoraria from Vericel; has received hospitality payments from DePuy, Medical Device Business Services, and Linvatec; and is a paid associate editor for The American Journal of Sports Medicine. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Amin NH, Old AB, Tabb LP, Garg R, Toossi N, Cerynik DL. Performance outcomes after repair of complete Achilles tendon ruptures in National Basketball Association players. Am J Sports Med. 2013;41(8):1864–1868. [DOI] [PubMed] [Google Scholar]
- 2. Burry HC, Pool CJ. Central degeneration of the Achilles tendon. Rheumatology. 1973;12(4):177–181. [Google Scholar]
- 3. Clayton RAE, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008;39(12):1338–1344. [DOI] [PubMed] [Google Scholar]
- 4. Davis JJ, Mason KT, Clark DA. Achilles tendon ruptures stratified by age, race, and cause of injury among active duty U.S. military members. Mil Med. 1999;164(12):872–873. [PubMed] [Google Scholar]
- 5. DeFroda SF, Feller R, Klinge SA. Surgical management of the aging athlete. Curr Sports Med Rep. 2016;15(6):426–432. [DOI] [PubMed] [Google Scholar]
- 6. Diamond PT, Gale SD. Head injuries in men’s and women’s lacrosse: a 10 year analysis of the NEISS database. Brain Inj. 2001;15(6):537–544. [DOI] [PubMed] [Google Scholar]
- 7. Erickson BJ, Cvetanovich GL, Nwachukwu BU, et al. Trends in the management of Achilles tendon ruptures in the United States Medicare population, 2005-2011. Orthop J Sports Med. 2014;2(9):2325967114549948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fukashiro S, Abe T, Shibayama A, Brechue WF. Comparison of viscoelastic characteristics in triceps surae between black and white athletes. Acta Physiol Scand. 2002;175(3):183–187. [DOI] [PubMed] [Google Scholar]
- 9. Gil JA, Defroda SF, Kriz P, Owens BD. Epidemiology of snow skiing- versus snowboarding-related concussions presenting to the emergency department in the United States from 2010 to 2014. Clin J Sport Med. 2017;27(5):499–502. [DOI] [PubMed] [Google Scholar]
- 10. Hallal PC, Andersen LB, Bull FC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–257. [DOI] [PubMed] [Google Scholar]
- 11. Hoffmann A, Mamisch N, Buck FM, Espinosa N, Pfirrmann CWA, Zanetti M. Oedema and fatty degeneration of the soleus and gastrocnemius muscles on MR images in patients with Achilles tendon abnormalities. Eur Radiol. 2011;21(9):1996–2003. [DOI] [PubMed] [Google Scholar]
- 12. Hojjat H, Svider PF, Lin HS, et al. Adding injury to insult: a national analysis of combat sport-related facial injury. Ann Otol Rhinol Laryngol. 2016;125(8):652–659. [DOI] [PubMed] [Google Scholar]
- 13. Houshian S, Tscherning T, Riegels-Nielsen P. The epidemiology of Achilles tendon rupture in a Danish county. Injury. 1998;29(9):651–654. [DOI] [PubMed] [Google Scholar]
- 14. Hsu AR, Jones CP, Cohen BE, Davis WH, Ellington JK, Anderson RB. Clinical outcomes and complications of percutaneous Achilles repair system versus open technique for acute Achilles tendon ruptures. Foot Ankle Int. 2015;36(11):1279–1286. [DOI] [PubMed] [Google Scholar]
- 15. Huttunen TT, Kannus P, Rolf C, Felländer-Tsai L, Mattila VM. Acute Achilles tendon ruptures: incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med. 2014;42(10):2419–2423. [DOI] [PubMed] [Google Scholar]
- 16. Inhofe PD, Grana WA, Egle D, Min KW, Tomasek J. The effects of anabolic steroids on rat tendon: an ultrastructural, biomechanical, and biochemical analysis. Am J Sports Med. 1995;23(2):227–232. [DOI] [PubMed] [Google Scholar]
- 17. Järvinen TAH, Kannus P, Maffulli N, Khan KM. Achilles tendon disorders: etiology and epidemiology. Foot Ankle Clin. 2005;10(2):255–266. [DOI] [PubMed] [Google Scholar]
- 18. Krolo I, Visković K, Ikić D, Klarić-Custović R, Marotti M, Cicvara T. The risk of sports activities: the injuries of the Achilles tendon in sportsmen. Coll Antropol. 2007;31(1):275–278. [PubMed] [Google Scholar]
- 19. Krul AJ, Daanen HAM, Choi H. Self-reported and measured weight, height and body mass index (BMI) in Italy, the Netherlands and North America. Eur J Public Health. 2011;21(4):414–419. [DOI] [PubMed] [Google Scholar]
- 20. Kujala UM, Sarna S, Kaprio J. Cumulative incidence of Achilles tendon rupture and tendinopathy in male former elite athletes. Clin J Sport Med. 2005;15(3):133–135. [DOI] [PubMed] [Google Scholar]
- 21. Lantto I, Heikkinen J, Flinkkilä T, Ohtonen P, Leppilahti J. Epidemiology of Achilles tendon ruptures: increasing incidence over a 33-year period. Scand J Med Sci Sports. 2015;25(1):e133–e138. [DOI] [PubMed] [Google Scholar]
- 22. Leppilahti J, Puranen J, Orava S. Incidence of Achilles tendon rupture. Acta Orthop Scand. 1996;67(3):277–279. [DOI] [PubMed] [Google Scholar]
- 23. Minhas SV, Kester BS, Larkin KE, Hsu WK. The effect of an orthopaedic surgical procedure in the National Basketball Association. Am J Sports Med. 2016;44(4):1056–1061. [DOI] [PubMed] [Google Scholar]
- 24. Myers RJ, Linakis SW, Mello MJ, Linakis JG. Competitive wrestling-related injuries in school aged athletes in U.S. emergency departments. West J Emerg Med. 2010;11(5):442–449. [PMC free article] [PubMed] [Google Scholar]
- 25. Nelson NG, McKenzie LB. Mountain biking-related injuries treated in emergency departments in the United States, 1994-2007. Am J Sports Med. 2011;39(2):404–409. [DOI] [PubMed] [Google Scholar]
- 26. Nillius SA, Nilsson BE, Westlin NE. The incidence of Achilles tendon rupture. Acta Orthop Scand. 1976;47(1):118–121. [DOI] [PubMed] [Google Scholar]
- 27. O’Brien M. Functional anatomy and physiology of tendons. Clin Sports Med. 1992;11(3):505–520. [PubMed] [Google Scholar]
- 28. Ootes D, Lambers KT, Ring DC. The epidemiology of upper extremity injuries presenting to the emergency department in the United States. Hand (N Y). 2012;7(1):18–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Owens B, Mountcastle S, White D. Racial differences in tendon rupture incidence. Int J Sports Med. 2007;28(7):617–620. [DOI] [PubMed] [Google Scholar]
- 30. Pappas E. Boxing, wrestling, and martial arts related injuries treated in emergency departments in the United States, 2002-2005. J Sports Sci Med. 2007;6(CSSI-2):58–61. [PMC free article] [PubMed] [Google Scholar]
- 31. Parekh SG, Wray WH, Brimmo O, Sennett BJ, Wapner KL. Epidemiology and outcomes of Achilles tendon ruptures in the National Football League. Foot Ankle Spec. 2009;2(6):283–286. [DOI] [PubMed] [Google Scholar]
- 32. Raikin SM, Garras DN, Krapchev PV. Achilles tendon injuries in a United States population. Foot Ankle Int. 2013;34(4):475–480. [DOI] [PubMed] [Google Scholar]
- 33. Schepsis AA, Jones H, Haas AL. Achilles tendon disorders in athletes. Am J Sports Med. 2002;30(2):287–305. [DOI] [PubMed] [Google Scholar]
- 34. US Census Bureau. United States census. Available at: https://www.census.gov/quickfacts/fact/table/US/PST045216%0A https://www.census.gov/quickfacts/fact/map/US/PST045216%0A http://www.census.gov/quickfacts/table/PST045215/27053/accessible. Accessed March 18, 2018.
- 35. van der Linden PD, Sturkenboom MC, Herings RM, Leufkens HM, Rowlands S, Stricker BH. Increased risk of Achilles tendon rupture with quinolone antibacterial use, especially in elderly patients taking oral corticosteroids. Arch Intern Med. 2003;163(15):1801–1807. [DOI] [PubMed] [Google Scholar]
- 36. Van Tassel D, Owens BD, Pointer L, Moriatis Wolf J. Incidence of clavicle fractures in sports: analysis of the NEISS database. Int J Sports Med. 2014;35(1):83–86. [DOI] [PubMed] [Google Scholar]
- 37. Vasileff WK, Moutzouros V. Unrecognized pediatric partial Achilles tendon injury followed by traumatic completion: a case report and literature review. J Foot Ankle Surg. 2014;53(4):485–488. [DOI] [PubMed] [Google Scholar]
- 38. Wang Y, Beydoun MA. The obesity epidemic in the United States: gender, age, socioeconomic, racial/ethnic, and geographic characteristics. A systematic review and meta-regression analysis. Epidemiol Rev. 2007;29(1):6–28. [DOI] [PubMed] [Google Scholar]
- 39. Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92(13):2279–2284. [DOI] [PubMed] [Google Scholar]
- 40. Weinfeld SB. Achilles tendon disorders. Med Clin North Am. 2014;98(2):331–338. [DOI] [PubMed] [Google Scholar]
- 41. White DW, Wenke JC, Mosely DS, Mountcastle SB, Basamania CJ. Incidence of major tendon ruptures and anterior cruciate ligament tears in US Army soldiers. Am J Sports Med. 2007;35(8):1308–1314. [DOI] [PubMed] [Google Scholar]
- 42. Zellers JA, Carmont MR, Silbernagel KG. Return to play post-Achilles tendon rupture: a systematic review and meta-analysis of rate and measures of return to play. Br J Sports Med. 2016;50(21):1325–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]