Short abstract
Objective
Ultrasonography is an efficient technique for detecting fatty liver. Its sensitivity and specificity in detecting moderate to severe fatty liver are comparable to those of histology. Fatty liver is associated with abnormal lipid and lipoprotein metabolism and insulin resistance, metabolic syndrome, cardiovascular/renal disease, type 2 diabetes, and other conditions. This study was performed to compare the serum lipid profiles and serum glutamic pyruvic transaminase (GPT), glutamic oxaloacetic transaminase (GOT), and glycosylated hemoglobin (HbA1c) levels in patients diagnosed with fatty liver on ultrasonography versus controls without fatty liver and evaluate the clinical relevance of an ultrasound diagnosis of fatty liver in routine health checkups.
Methods
This hospital-based cross-sectional study included 390 patients who underwent health checkups; 226 were diagnosed with fatty liver (cases) and 164 were not (controls). The lipid profile, serum GOT and GPT levels, and HbA1c level were compared between the cases and controls.
Results
The cases had considerably higher levels of lipids, liver enzymes (serum GOT and GPT), and HbA1c than controls.
Conclusion
Ultrasonography is a noninvasive simple tool for early detection of fatty liver in asymptomatic patients and can help clinicians achieve early detection of metabolic syndrome.
Keywords: Fatty liver, NAFLD, correlation of fatty liver with lipid profile, liver enzymes and HbA1c, NAFLD and insulin resistance, NAFLD and metabolic syndrome
Introduction
Ultrasonography is a very efficient and widely available technique for the detection of fatty liver. The overall sensitivity and specificity of ultrasound in detection of moderate to severe fatty liver have been shown to be accurate and comparable to those of histology (gold standard).1–3 Fatty liver (i.e., hepatic steatosis) in non-alcoholic individuals is rapidly becoming a major public health challenge;4 however, its natural history and determinants remain incompletely understood because of limitations in diagnostic technologies, and this condition is often asymptomatic until the very late stages. Severe complications can occur because of the risk of progression to more advanced stages, including liver fibrosis and cirrhosis, making early noninvasive detection of fatty liver disease by ultrasonography very clinically important.2,4,5 Non-alcoholic fatty liver disease (NAFLD) is a spectrum of diseases ranging from simple steatosis (fatty liver) to non-alcoholic steatohepatitis, fibrosis, and ultimately liver cirrhosis. Abnormalities in lipid and lipoprotein metabolism and abnormal insulin resistance are associated with fatty liver and are also considered to be important pathways for the development of metabolic syndrome-related diseases such as atherosclerosis, cardiovascular disease (CVD), and NAFLD.6
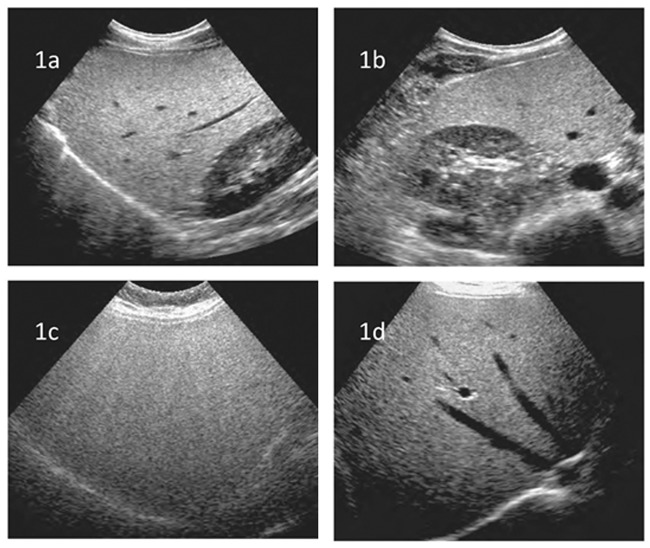
Conventional B-mode ultrasonography is the most common technique used to assess the presence of fatty liver in clinical settings and population studies. Fatty liver is diagnosed based on the following ultrasound parameters: parenchymal brightness, liver-to-kidney contrast, deep beam attenuation, bright vessel walls, and gallbladder wall definition.7 Qualitative grades are conveniently labeled mild, moderate, or severe or grade 0 to 3 (with 0 being normal). Grade 1 (mild) (Figure 1) is represented by a slight diffuse increase in fine echoes in the hepatic parenchyma with normal visualization of the diaphragm and intrahepatic vessel borders. Grade 2 (moderate) is represented by a moderate diffuse increase in fine echoes with slightly impaired visualization of the intrahepatic vessels and diaphragm. Grade 3 (marked) (Figure 1) is represented by a marked increase in fine echoes with poor or no visualization of the intrahepatic vessel borders, diaphragm, and posterior portion of the right lobe of the liver.8
Figure 1.
Ultrasound findings. (a, b) B-mode ultrasound images of the liver show a mild increase in liver echogenicity compared with the kidney. (c, d) B-mode ultrasound images of the liver show grade III diffuse fatty infiltration with a marked increase in liver echogenicity relative to the kidney and no visualization of the intrahepatic vessel borders, diaphragm, and posterior portion of the right lobe of the liver.
This study was performed to compare the serum lipid profiles, serum glutamic pyruvic transaminase (GPT) and glutamic oxaloacetic transaminase (GOT) levels, and glycosylated hemoglobin (HbA1c) level between patients with and without fatty liver on ultrasonography and to determine whether statistical significance exists between fatty liver detected on routine health checkup scans and these laboratory parameters. Overall, the goal was to prove the clinical relevance of ultrasound reporting of fatty liver in routine health checkups.
Materials and methods
This retrospective hospital-based cross-sectional study involved patients who had presented for a master health checkup. Of all patients who had been investigated by ultrasonography, those with fatty liver were defined as cases and those without fatty liver were defined as controls. The lipid profile [i.e., total cholesterol, triglycerides, high-density lipoprotein (HDL), and low-density lipoprotein (LDL)] was obtained for all patients. The serum GOT [aspartate transaminase (AST)], serum GPT [alanine transaminase (ALT)], and HbA1c levels were available in various proportions of patients. The lipid profiles, serum GOT and GPT, and HbA1c were compared between cases and controls. The p value was calculated using the chi-square test, and p < 0.05 was considered statistically significant. The unpaired t-test was performed, and odds ratios were calculated.
Because this was a retrospective study and no new tests were performed or changes to existing investigation protocols were made (whether ultrasonography or blood tests), ethics committee approval was not considered essential. Written consent for the investigations are available from the medical record division. No consent was obtained for inclusion in the study because of its retrospective design.
Results
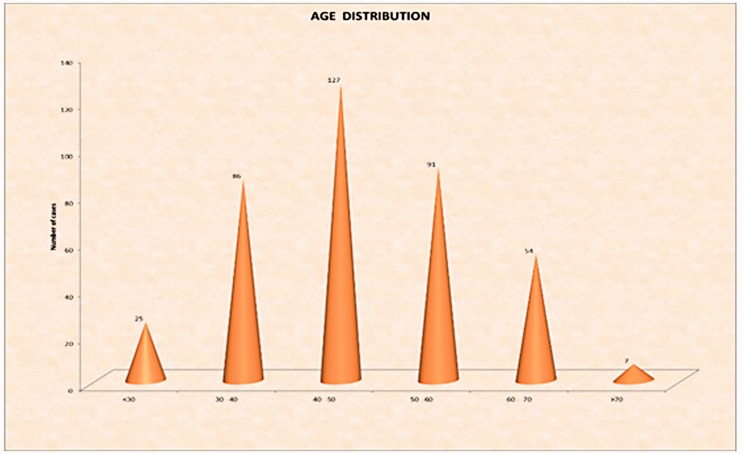
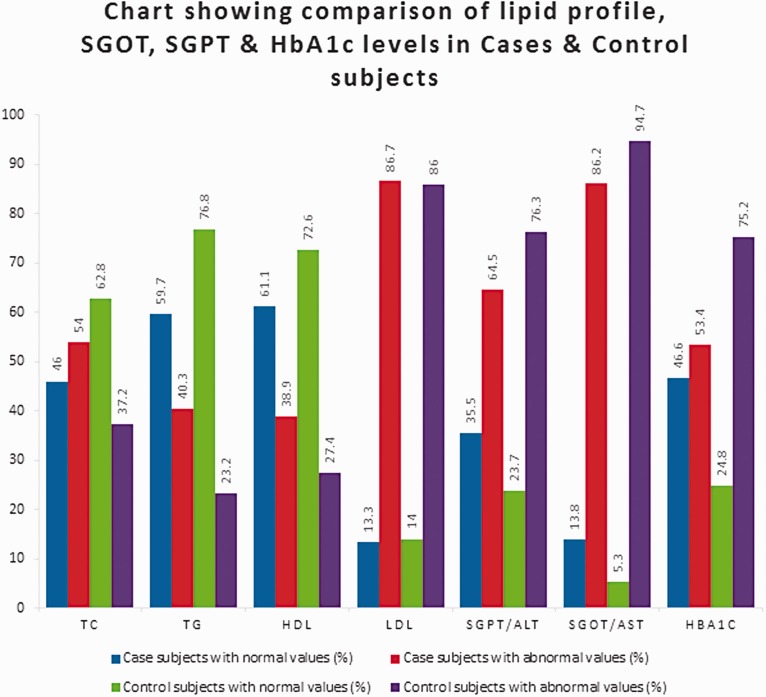
In total, 390 patients were investigated by ultrasonography. Of these patients, 226 were diagnosed with fatty liver, and the remaining 164 patients with a normal hepatic echopattern served as controls. The serum GOT and GPT levels were available in 261 and 266 patients, respectively. The HbA1c level was available in 311 patients. The mean age of the cases and controls was 49.73 and 44.86 years, respectively (p < 0.001 [very highly significant (VHS)]). Most cases were in the 40- to 60-year age group (p < 0.001 VHS) (Figure 2). Male and female patients comprised 37.6% and 62.4% of the cases, respectively, and 50.0% each of the controls (p = 0.015 [significant (SIG)]). The lipid, liver enzyme, and HbA1c levels were significantly higher in the cases than controls (Figure 3 and Table 1). The serum total cholesterol and triglyceride levels were high in 54.0% and 40.3% of cases and 37.2% and 23.2% of controls, respectively (p < 0.001). Low serum HDL levels were seen in 38.9% of cases and 27.4% of controls (p < 0.001). High serum GPT, GOT, and HbA1c levels were seen in 13.8%, 35.5%, and 46.6% of cases and 5.3%, 23.7%, and 24.8% of controls, respectively. However, the rise in LDL levels in cases (86.7%) compared with controls (86.0%) was not statistically significant.
Figure 2.
Column chart showing age distribution in the case and control groups (X2 =25.756, p < 0.001).
Figure 3.
Column chart showing distribution of lipid profile and serum GOT, GPT, and HbA1c levels in cases and controls. TC, total cholesterol; TG, triglycerides; HDL, high-density lipoprotein; LDL, low-density lipoprotein; GOT/AST, glutamic oxaloacetic transaminase/aspartate transaminase; GPT/ALP, glutamic pyruvic transaminase/alanine transaminase; HbA1c, glycosylated hemoglobin.
Table 1.
Group statistics of variables in case and control groups with unpaired t-test and odds ratio estimation.
| Group | n | Mean | SD | t-test |
Odds ratio for abnormal/below-normal values |
|||
|---|---|---|---|---|---|---|---|---|
| Value |
95% CI |
|||||||
| Lower | Upper | |||||||
| Total cholesterol (serum) | Cases | 226 | 205.075 | 49.574 | 2.755 | 0.505 | 0.335 | 0.761 |
| Controls | 164 | 192.634 | 34.956 | p = 0.006 HS | ||||
| Triglycerides | Cases | 226 | 161.867 | 140.419 | 3.555 | 0.447 | 0.285 | 0.701 |
| Controls | 164 | 120.268 | 61.231 | p < 0.001 VHS | ||||
| HDL cholesterol | Cases | 226 | 44.648 | 11.211 | 4.089 | 0.593 | 0.384 | 0.916 |
| Controls | 164 | 50.063 | 14.946 | p < 0.001 VHS | ||||
| LDL cholesterol | Cases | 226 | 146.944 | 38.539 | 3.173 | 0.938 | 0.523 | 1.684 |
| Controls | 164 | 135.074 | 33.387 | p = 0.002 HS | ||||
| GOT (AST) | Cases | 167 | 28.371 | 17.102 | 2.295 | 0.352 | 0.129 | 0.959 |
| Controls | 94 | 23.968 | 9.725 | p = 0.023 SIG | ||||
| GPT (ALT) | Cases | 169 | 39.373 | 24.614 | 2.326 | 0.564 | 0.321 | 0.992 |
| Controls | 97 | 32.361 | 21.898 | p = 0.021 SIG | ||||
| HbA1c | Cases | 174 | 6.483 | 1.506 | 3.419 | 0.379 | 0.232 | 0.618 |
| Controls | 137 | 5.951 | 1.152 | p < 0.001 VHS | ||||
SD, standard deviation; CI, confidence interval; HDL, high-density lipoprotein; LDL, low-density lipoprotein; GOT, glutamic oxaloacetic transaminase; GPT, glutamic pyruvic transaminase; HbA1c, glycosylated hemoglobin; VHS, very highly significant; HS, highly significant; SIG, significant.
Discussion
With the rising prevalence of obesity, the proportion of fatty liver has increased in both Eastern and Western countries.4 Fatty liver can progress to steatohepatitis, cirrhosis, and even hepatocellular carcinoma if not diagnosed promptly. Previous studies conducted in Western countries have demonstrated that the risk factors for fatty liver disease include age, sex, and metabolic factors such as central obesity; a higher body mass index, fasting blood glucose level, insulin level, triglyceride level, and cholesterol level; and lower HDL level.5 NAFLD is a broad term for a wide disease spectrum ranging from NAFLD to non-alcoholic steatohepatitis, fibrosis, and ultimately cirrhosis in the absence of significant alcohol intake. Moreover, previous studies have demonstrated that the development of hepatocellular carcinoma in patients with hepatic steatosis can occur in the absence of liver cirrhosis. In asymptomatic non-alcoholic patients with hepatic steatosis detected by ultrasonography, it is important to check for metabolic risk factors such as dyslipidemia, obesity, and glucose intolerance by biochemical analysis for early diagnosis of metabolic syndrome.5 NAFLD affects almost 30% of the population in Western countries and has become the most common cause of chronic parenchymal liver disease.9 Obesity is considered a high-risk factor for fatty liver, and the prevalence of NAFLD is >90% with up to 5% of patients having clinically unsuspected cirrhosis. Fatty liver is not only a hepatic manifestation of metabolic syndrome but can also promote the development of metabolic-related extrahepatic complications such as CVD, type 2 diabetes, chronic kidney disease, hypothyroidism, polycystic ovarian syndrome, osteoporosis, and colorectal cancer. Increasing evidence is showing that patients with fatty liver disease have a significantly higher risk of CVD than the general population of the same age and sex.5,10–12
Our study is in agreement with several previous studies showing a higher prevalence of fatty liver in men than women, with the prevalence peaking at 40 years of age and remaining relatively constant up to the seventh decade of life.13 NAFLD appears to be the most common cause of elevated serum GPT and GOT levels.14 NAFLD is not an isolated or random event in metabolic syndrome but is a hepatic component of metabolic syndrome12 and represents an important self-governing risk factor for diabetes, CVD, chronic renal disease, and all components of metabolic syndrome. In patients with NAFLD, overproduction of several atherogenic factors such as cytokines and lipoproteins occurs with influx of free fatty acids from the adipose tissue to the liver, contributing to an increase in the liver fat concentration. Alterations in the triacylglycerol content are seen in about 74% to 90% of patients undergoing liver biopsy.12 Insulin resistance is now considered characteristic of NAFLD, contributing to the development of type 2 diabetes; hence, fatty liver is associated with abnormal HbA1c levels. Increased free fatty acid flux from fatty tissue to non-adipose organs because of deranged fat metabolism can contribute to hepatic triglyceride accumulation, resulting in impaired glucose metabolism and insulin sensitivity in the muscle and liver.15 Thus, fatty liver is associated with increased serum LDL and triglyceride levels combined with decreased HDL levels, all of which are independent risk factors for CVD. NAFLD is thus independently associated with an increased risk of CVD in patients without diabetes and in those with type 1 and 2 diabetes.6,16,17 Our results corroborate these findings because we found that elevated liver enzymes, a deranged lipid profile, and abnormal insulin resistance manifesting as high HbA1c levels are associated with fatty liver even in asymptomatic patients presenting for routine health checkups.
Fatty liver disease is not uncommon in non-obese Asian patients. A rising prevalence of metabolic syndrome12 and a higher risk of CVD and type 2 diabetes have been reported in South Asian countries despite the fact that these patients have a lower body mass index than their European and American counterparts.18 The use of blood tests, mainly measurement of the ALT level, as a screening tool can be erroneous because the ALT level may be normal in 69% of patients with increased liver fat.12 Consequently, the development of a feasible noninvasive screening marker is needed to identify high-risk groups of patients with fatty liver in the general population. Such patients are easily overlooked if there is a lack of clinical suspicion. Because it is inexpensive and readily available in all rural centers in India, ultrasound fits the role of being the most suitable investigation technique for mass population screening of fatty liver. Further metabolic tests can then be performed in individuals found to have fatty liver.
Study limitations
The correlation of LDL levels between cases and controls was not statistically significant. We assume that if the study had been performed in a larger sample size, we may have been able to prove a statistically significant association between LDL and fatty liver.
Conclusion
Most patients with fatty liver are asymptomatic; symptoms occur only in the advanced stages of the disease. Knowledge of the diagnosis, risk factors, and management of NAFLD is poor, even among general practitioners; thus, a significant proportion of patients with high-risk NAFLD are missed. Over-reliance on measurement of transaminases to diagnose fatty liver disease risks underdiagnosing NAFLD. Although liver biopsy is the gold standard method for diagnosis of fatty liver, it cannot be performed in the entire general population. Ultrasonography, which is a noninvasive and simple tool, can be used for the early detection of fatty liver in asymptomatic patients. This technique can also serve as an indicator of future comorbidities and can help clinicians to suggest blood investigations and counsel patients regarding further management or preventive measures.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Adams LA, Talwalkar JA. Diagnostic evaluation of nonalcoholic fatty liver disease. J Clin Gastroenterol 2006; 40(Suppl 1): S34–S38. [DOI] [PubMed] [Google Scholar]
- 2.Wieckowska A, Feldstein AE. Diagnosis of nonalcoholic fatty liver disease: invasive versus noninvasive. Semin Liver Dis 2008; 28: 386–395. [DOI] [PubMed] [Google Scholar]
- 3.Hernaez R, Lazo M, Bonekamp S, et al. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Hepatology 2011; 54: 1082–1090. DOI: 10.1002/hep.24452 PMID: 21618575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of nonalcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther 2011; 34: 274–285. DOI: 10.1111/j.1365-2036.2011.04724.x PMID: 21623852. [DOI] [PubMed] [Google Scholar]
- 5.Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American gastroenterological association, American association for the study of liver diseases, and American college of gastroenterology. Gastroenterology 2012; 142: 1592–1609. DOI: 10.1053/j.gastro.2012.04.001 PMID: 22656328. [DOI] [PubMed] [Google Scholar]
- 6.Fon Tacer K, Rozman D. Nonalcoholic fatty liver disease: focus on lipoprotein and lipid deregulation. J Lipids 2011; 2011: 783976. DOI: 10.1155/2011/783976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dasarathy S, Dasarathy J, Khiyami A, et al. Validity of real time ultrasound in the diagnosis of hepatic steatosis: a prospective study. J Hepatol 2009; 51: 1061–1067. DOI: 10.1016/j.jhep.2009.09.001 PMID: 19846234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shannon A, Alkhouri N, Carter-Kent C, et al. Ultrasonographic quantitative estimation of hepatic steatosis in children With NAFLD. J Pediatr Gastroenterol Nutr 2011; 53: 190–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hyysalo J, Mannisto VT, Zhou Y, et al. A population-based study on the prevalence of NASH using scores validated against liver histology. J Hepatol 2014; 60: 839–846. DOI: 10.1016/j.jhep.2013.12.009 PMID: 24333862. [DOI] [PubMed] [Google Scholar]
- 10.Pais R, Charlotte F, Fedchuk L, et al. A systematic review of follow-up biopsies reveals disease progression in patients with non-alcoholic fatty liver. J Hepatol 2013; 59: 550–556. DOI: 10.1016/j.jhep.2013.04.027. [DOI] [PubMed] [Google Scholar]
- 11.Sanyal AJ. and American Gastroenterological Association. AGA technical review on nonalcoholic fatty liver disease. Gastroenterology 2002; 123: 1705–1725. PMID: 12404245. [DOI] [PubMed] [Google Scholar]
- 12.Tarantino G, Finelli C. What about non-alcoholic fatty liver disease as a new criterion to define metabolic syndrome? World J Gastroenterol 2013; 19: 3375–3384. DOI: 10.3748/wjg.v19.i22.3375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong VW, Chu WC, Wong GL, et al. Prevalence of non-alcoholic fatty liver disease and advanced fibrosis in Hong Kong Chinese: a population study using proton-magnetic resonance spectroscopy and transient elastography. Gut 2012; 61: 409–415. DOI: 10.1136/gutjnl-2011-300342 PMID: 21846782. [DOI] [PubMed] [Google Scholar]
- 14.Chen CH, Huang MH, Yang JC, et al. Prevalence and etiology of elevated serum alanine aminotransferase level in an adult population in Taiwan. J Gastroenterol Hepatol 2007; 22: 1482–1489. PMID: 17716352. [DOI] [PubMed] [Google Scholar]
- 15.Bugianesi E, McCullough AJ, Marchesini G. Insulin resistance: a metabolic pathway to chronic liver disease. Hepatology 2005; 42: 987–1000. DOI 10.1002/hep.20920. [DOI] [PubMed] [Google Scholar]
- 16.Calori G, Lattuada G, Ragogna F, et al. Fatty liver index and mortality: the Cremona study in the 15th year of follow-up. Hepatology 2011; 54: 145–152. DOI: 10.1002/hep.24356 PMID: 21488080. [DOI] [PubMed] [Google Scholar]
- 17.Treeprasertsuk S, Leverage S, Adams LA, et al. The Framingham risk score and heart disease in nonalcoholic fatty liver disease. Liver Int 2012; 32: 945–950. DOI: 10.1111/j.1478-3231.2011.02753.x PMID: 22299674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palaniappan LP, Wong EC, Shin JJ, et al. Asian Americans have greater prevalence of metabolic syndrome despite lower body mass index. Int J Obes (Lond) 2011; 35: 393–400. DOI: 10.1038/ijo.2010.152 PMID: 20680014. [DOI] [PMC free article] [PubMed] [Google Scholar]