Short abstract
Small incision refractive lenticule extraction (SMILE) is a femtosecond laser technique to correct myopia and myopic astigmatism. Herein, we report a technique where intrastromal lenticule obtained from the SMILE procedure served as a graft for lamellar keratoplasty in the management of a limbal dermoid. An 18-year-old woman presented to the clinic with a corneal-limbal mass in the right eye. Slit-lamp examination revealed a vascularized circular mass of approximately 6 mm × 5 mm, which was attached at 7 o’clock in the inferotemporal region of the corneal limbus; this suggested limbal dermoid. Anterior segment optical coherence tomography revealed superficial involvement of the cornea. The patient was treated with excision and lamellar keratoplasty by using femtosecond intrastromal lenticule. The lenticule was sutured over the cornea with 10-0 interrupted nylon sutures. On postoperative follow-up, best-corrected visual acuity was 20/20; there was no corneal neovascularization and no sign of rejection. This case of limbal dermoid was managed by simple surgical excision and lamellar keratoplasty with a SMILE-extracted lenticule. This method may serve as an alternative surgical approach for management of limbal dermoid.
Keywords: Lenticule, small incision refractive lenticule, limbal dermoid, lamellar keratoplasty, dermoid cyst, corneal transplantation, limbus corneae
Introduction
Limbal dermoid is a common benign neoplasm of the corneal limbus.1 Generally, it arises in the inferior portion of the temporal quadrant, and can lead to astigmatism, cosmetic difficulties, and increasing astigmatism, as well as vision disturbances in conjunction with lesions.2,3 Various surgical procedures have been described, based on the site, depth, and size of these lesions, including simple excision, amniotic membrane transplantation, simple keratectomy with corneal tattooing, and lamellar keratoplasty (LKP) or penetrating keratoplasty (PKP) with corneal-limbal scleral donor graft transplantation.4–6 The established procedure for management of limbal dermoid is simple excision, whereas LKP is an alternative method.6 Worldwide, there is an extreme need for corneal grafts, particularly in developing countries; the lack of readily available grafts is a limitation of LKP.7
Small incision refractive lenticule extraction (SMILE) is an innovative femtosecond laser refractive procedure that is used for the correction of myopia and myopic astigmatism by extraction of the intrastromal corneal lenticule.8 Pradhan et al.9 described the first human implantation of allogenic lenticule; they reported successful implantation of an intrastromal lenticule, which was obtained from a myopic donor via the SMILE procedure, for the correction of hyperopia. Here, we describe a technique that consists of limbal dermoid excision combined with LKP—using lenticule from the SMILE procedure—for the treatment of limbal dermoid in a young female.
Case report
Informed written consent was obtained from the patient for the publication of this case report and all accompanying images. As this case report and review of the literature are intended for informational and educational purposes, our institution did not require ethical approval.
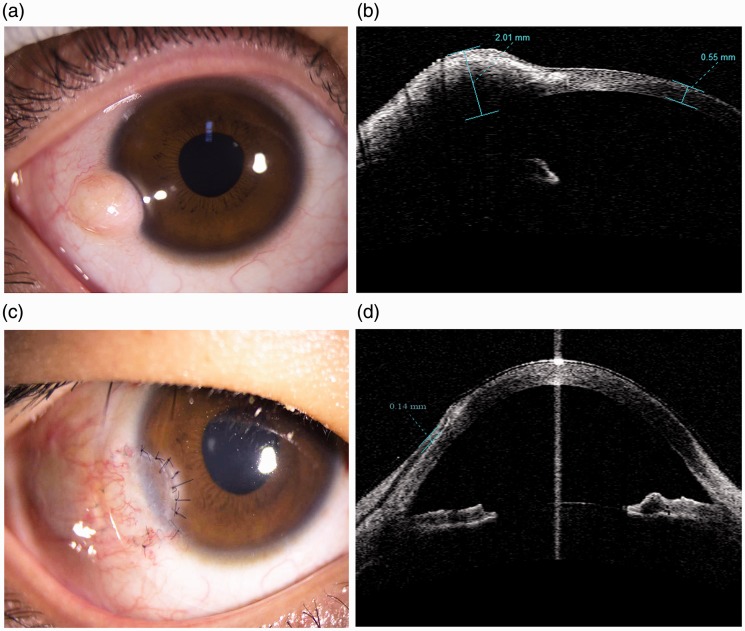
An 18-year-old woman presented at the Department of Ophthalmology, First Hospital of Jilin University, with a history of a corneal-limbal mass in the right eye; the mass had been present since birth, and had gradually increased in size. The patient did not experience any pain, but reported a mild foreign body sensation. Slit-lamp biomicroscopy (SL 130 Slit Lamp; Carl Zeiss, Germany) showed a vascularized circular opaque mass of approximately 6 mm × 5 mm, fixed at 7 o’clock in the inferotemporal region of the corneal limbus in the right eye (OD) (Figure 1a). The mass did not interfere with the visual axis. Uncorrected visual acuity (UCVA) was 20/80 in the right eye and the manifest refractive correction was -1.75 Dcyl ax 40 with a best-corrected visual acuity (BCVA) of 20/20 on the Snellen chart. The patient had normal eye movements in both eyes and all other ocular parameters were normal. Anterior segment optical coherence tomography (Visante, Anterior Segment Imaging, Carl Zeiss Meditec, Germany) showed superficial corneal involvement with a depth of one-third of the corneal thickness (Figure 1b). The patient was clinically diagnosed with a grade I limbal dermoid, which was later confirmed by histological examination. Because of the patient’s desire to remove the lesion for cosmetic purposes, surgical excision was performed, followed by intraoperative LKP with intrastromal lenticule obtained from the SMILE procedure.
Figure 1.
Images of the right eye of an 18-year-old female patient who presented with limbal dermoid and underwent dermoid excision with lamellar keratoplasty, using a lenticule obtained by small incision lenticule extraction: (a) preoperative slit-lamp biomicroscopy of the right eye, showing a mass of approximately 6 mm × 5 mm present in the corneal-limbal area; (b) preoperative anterior optical coherence tomography of right eye, displaying superficial involvement of the cornea; (c) slit-lamp biomicroscopy of the right eye at 3 weeks postoperatively, showing that there is no sign of rejection, the graft remains in position, and sutures remain intact; (d) anterior optical coherence tomography of the right eye at 3 weeks postoperatively, demonstrating graft thickness of 0.14 mm.
Under topical anesthesia (several drops of lidocaine), the edge of the limbal dermoid was marked with a fine pen to differentiate the conjunctival and corneal portions of the dermoid. The conjunctiva was then dissected by using a pair of blunt Westcott scissors under subconjunctival anesthesia (2% lidocaine containing 1:100 000 epinephrine), in order to expose the bare sclera around the mass. Lamellar dissection of the corneal-limbal dermoid was performed by using a surgical blade knife. After complete excision and removal of the dermoid, longitudinal planar dissection of the remaining dermoid fibers from the cornea was performed with a surgical blade knife. Minimal cauterization was performed at sites of bleeding.
As an elective procedure, the lenticule was obtained from SMILE procedure by using the VisuMax FS laser (Carl Zeiss, Meditec AG, Jena, Germany) from a myopic donor with a refractive correction spherical equivalent of -8.50 D, thus ensuring donor lenticule central thickness ≥100 µm. The optical zone and cap thickness were 6.5 mm and 120 µm, respectively. Additionally, the donor was negative for syphilis, hepatitis, human immunodeficiency virus, corneal disease, infection, and malignancy. The donor had no past history of ocular surgery. The lenticule thus obtained was trimmed to match the size of the corneal defect and then sutured to the recipient with interrupted 10-0 nylon sutures. First, the 12-o’clock and 6-o’clock cardinal sutures were placed, immediately followed by 3-o’clock and 9-o’clock cardinal sutures. No sutures approached or intersected the visual axis. The exposed sclera was covered with adjacent conjunctiva and sutured to the edge of the graft by using Ethicon 10-0 nylon suture (Johnson & Johnson Health Care Systems, New Brunswick, NJ, USA). Finally, the cornea was enclosed with a therapeutic contact lens; tobramycin plus dexamethasone eye ointment (S.A. Alcon-Couvereur N.V., Purrs, Belgium) was applied within the conjunctival sac. The excised lesion was sent for histologic examination.
Postoperatively, topical antibiotic (0.3% ofloxacin [Allergan, Irvine, CA, USA], four times per day for 4 months) and topical steroid medication (1% prednisolone acetate [Allergan], four times per day for 1 month; subsequently, 0.1% fluorometholone, four times per day for 1 month, gradually tapered over 2 months) were used. At every follow-up, the patient showed no steroid-related complications.
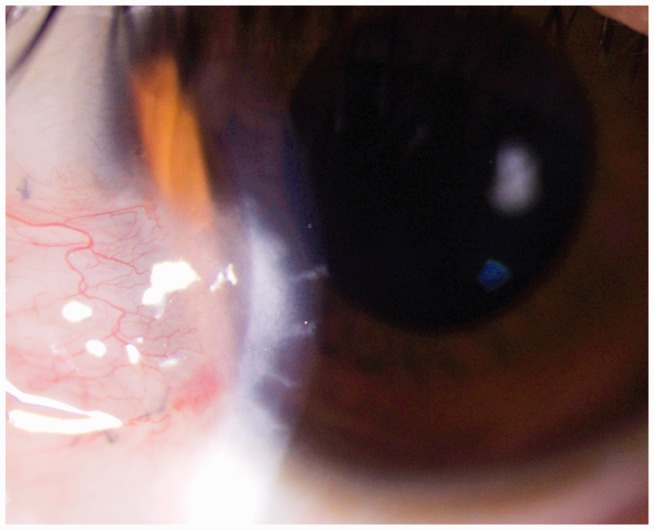
On postoperative day 1, there were no complaints; slit-lamp examination showed conjunctival congestion and the graft was in position with intact sutures. Complete epithelialization was achieved during the first postoperative week. On postoperative day 21, the patient experienced mild foreign body sensation; sutures remained intact (Figure 1c) and anterior OCT revealed that the total graft thickness was 0.14 mm (Figure 1d). At 3 months postoperatively, corneal sutures were removed. At 4 months postoperatively, BCVA was 20/20 (refractive correction -1.50 Dcy ax 40) with no sign of rejection or corneal neovascularization (Figure 2). The patient was assessed every month for 12 months. There was no evidence of corneal melting or infection during follow-up. The patient regularly attended follow-up examinations and was satisfied with the cosmetic outcome after the procedure.
Figure 2.
The final corneal image after removal of all corneal sutures at 4 months postoperatively, showing corneal stability and no sign of rejection.
Discussion
Limbal dermoids are ocular choristomas comprising tissues of ectodermal and mesodermal origin, which present as small lesions to large masses in the epibulbar area.10 Limbal dermoids are categorized into three grades. Grade I limbal dermoids include superficial lesions less than 5 mm, which are confined to the limbus. Grade II limbal dermoids include larger lesions extending to the corneal stroma, deep to Descemet’s membrane without involvement of the membrane. Grade III limbal dermoids, the least common form, include larger lesions involving the entire cornea, as well as those extending deep to the structures of anterior chamber.5 Limbal dermoids require surgical excision for cosmetic reasons, as well as for vision impairment. Management depends on various factors such as the site, depth, and size of the lesion.5 Simple excision of a limbal dermoid may lead to corneal vascularization, persistent epithelial defect, scar development, and pseudo-pterygium formation, as well as conjunctival symblepharon.4,11 LKP is an alternative for simple excision or keratectomy with a low incidence of postoperative complications, including corneal opacity, neovascularization, and pseudo-pterygium.6 Although LKP is an alternative for the surgical management of limbal dermoids, it presents some disadvantages, including graft rejection, infection, requirement for increased surgical skills, high cost, and the need for a donor cornea.6 Worldwide, the cornea is the most common organ transplanted; recent 10-year data have shown that more than 8000 keratoplasties are performed in China each year.7 However, there is a great scarcity of corneal donors for LKP in developing nations, such as China.
SMILE is a novel surgical procedure for the correction of myopia and myopic astigmatism without the use of a corneal flap. SMILE has been used widely because of its brilliant effectiveness, safety, and predictability.8 Re-implantation of SMILE-extracted lenticule has been used in the management of various clinical conditions, including presbyopia, hyperopia, corneal ulcers, microperforations, corneal thinning, and corneal dystrophy.9,12–14 Lenticules extracted by the SMILE procedure are high-quality, clear tissues because patients who undergo SMILE are generally younger than typical corneal donors. Therefore, the extracted lenticule can be used as a graft in LKP for the treatment of a patient with limbal dermoid, in order to reduce the shortage of corneal graft, as well as to ensure a cost-effective approach.
Management of limbal dermoid by using an intrastromal SMILE-extracted lenticule has been recently reported, combined with corneal tattooing and the aid of fibrin glue.15 Although corneal tattooing is considered a safe and effective procedure, various complications have been reported, such as severe toxic reaction, corneal melting, granulomatous keratitis, persistent epithelial defects, ulceration, iridocyclitis, wound dehiscence, Tenon’s cyst, and corneal epithelial erosion.16–20 Despite viral inactivation techniques used in commercially available fibrin glue, transmission of infectious agents, such as parvovirus B19 (HPV B19) and prions, remains the chief concern.21 Moreover, fibrin glue is inaccessible in various developing countries; in those where it is accessible, its cost is greater than most patients can afford and the quality of local glue is unsatisfactory.
In the present report, we have described a technique of simple dermoid excision and LPK, which used SMILE-extracted lenticule with interrupted 10-0 nylon sutures, in a patient with grade I limbal dermoid. Simple dermoid excision was performed; then, the lenticule was trimmed and sutured with interrupted 10-0 nylon sutures. The use of sutures minimizes the risk of recurrent graft loss, corneal epithelial erosion, granulomatous keratitis, and Tenon’s cyst, all of which are more common when using a sutureless technique with fibrin glue. Graft dehiscence is a severe complication of techniques that involve fibrin glue. Regarding visual acuity, the patient’s preoperative and postoperative BCVAs were 20/20, with respective refractive correction of -1.75 Dcyl ax 40 and -1.50 Dcy ax 40. There was a postoperative reduction in astigmatism. In the present case, the surgical result was superior to those of previous corrective surgeries. However, this approach may require longer operative time and better surgical skills. Additionally, our patient received the lenticule without any added cost.
Importantly, this technique was performed in a tertiary care hospital where a SMILE facility was available and the donor lenticule was easily accessible. Thus, the restricted availability of the donor lenticule—primarily within tertiary care hospitals that perform SMILE procedures—is a major limitation of this technique. However, these lenticules can be stored for short durations in corneal storage media, and for longer durations through cryopreservation; thus, the lenticule may be supplied to other surgical facilities through the use of eye banks.
In summary, LKP with SMILE-extracted intrastromal lenticule is an alternative approach for the management of limbal dermoid. This can reduce the donor shortages and high cost of donor corneas in developing nations; moreover, it results in good cosmetic and functional outcomes. However, further studies and long-term follow-up analyses are needed.
Declaration of conflicting interest
The authors declare that there is no conflict of interest
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Sunderraj PP, Viswanathan RK, Balachander R. Neoplasms of the limbus. Indian J Ophthalmol 1991; 39: 168–169. [PubMed] [Google Scholar]
- 2.Nevares RL, Mulliken JB, Robb RM. Ocular dermoids. Plast Reconstr Surg 1988; 82: 959–964. [DOI] [PubMed] [Google Scholar]
- 3.Scott JA, Tan DT. Therapeutic lamellar keratoplasty for limbal dermoids. Ophthalmology 2001; 108: 1858–1867. [DOI] [PubMed] [Google Scholar]
- 4.Panton RW, Sugar J. Excision of limbal dermoids. Ophthalmic Surg 1991; 22: 85–89. [PubMed] [Google Scholar]
- 5.Pirouzian A, Ly H, Holz H, et al. Fibrin-glue assisted multilayered amniotic membrane transplantation in surgical management of pediatric corneal limbal dermoid: a novel approach. Graefes Arch Clin Exp Ophthalmol 2011; 249: 261–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cha DM, Shin KH, Kim KH, et al. Simple keratectomy and corneal tattooing for limbal dermoids: results of a 3-year study. Int J Ophthalmol 2013; 6: 463–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hong J, Shi W, Liu Z, et al. Limitations of Keratoplasty in China: a survey analysis. PLoS One 2015; 10: e0132268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yu Y, Zhang W, Cheng X, et al. Impact of treatment decentration on higher-order aberrations after SMILE. J Ophthalmol 2017; 2017: 9575723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pradhan KR, Reinstein DZ, Carp GI, et al. Femtosecond laser-assisted keyhole endokeratophakia: correction of hyperopia by implantation of an allogeneic lenticule obtained by SMILE from a myopic donor. J Refract Surg 2013; 29: 777–782. [DOI] [PubMed] [Google Scholar]
- 10.Mansour AM, Barber JC, Reinecke RD, et al. Ocular choristomas. Surv Ophthalmol 1989; 33: 339–358. [DOI] [PubMed] [Google Scholar]
- 11.Panda A, Ghose S, Khokhar S, et al . Surgical outcomes of Epibulbar dermoids. J Pediatr Ophthalmol Strabismus 2002; 39: 20–25. [DOI] [PubMed] [Google Scholar]
- 12.Jacob S, Kumar DA, Agarwal A, et al. Preliminary evidence of successful near vision enhancement with a new technique: presbyopic allogenic refractive lenticule (PEARL) corneal inlay using a SMILE lenticule. J Refract Surg 2017; 33: 224–229. [DOI] [PubMed] [Google Scholar]
- 13.Zhao J, Sun L, Shen Y, et al. Using donor lenticules obtained through SMILE for an epikeratophakia technique combined with phototherapeutic keratectomy. J Refract Surg 2016; 32: 840–845. [DOI] [PubMed] [Google Scholar]
- 14.Bhandari V, Ganesh S, Brar S, et al. Application of the SMILE-derived glued lenticule patch graft in microperforations and partial-thickness corneal defects. Cornea 2016; 35: 408–412. [DOI] [PubMed] [Google Scholar]
- 15.Jacob S, Narasimhan S, Agarwal A, et al. Combined interface tattooing and fibrin glue-assisted sutureless corneal resurfacing with donor lenticule obtained from small-incision lenticule extraction for limbal dermoid. J Cataract Refract Surg 2017; 43: 1371–1375. [DOI] [PubMed] [Google Scholar]
- 16.Mannis MJ, Eghbali K, Schwab IR. Keratopigmentation: a review of corneal tattooing. Cornea 1999; 18: 633–637. [PubMed] [Google Scholar]
- 17.van der Velden/Samderubun EM, Kok JH. Dermatography as a modern treatment for coloring leucoma corneae. Cornea 1994; 13: 349–353. [DOI] [PubMed] [Google Scholar]
- 18.Sharma A, Gupta P, Dogra MR, et al. Granulomatous keratitis following corneal tattooing. Indian J Ophthalmol 2003; 51: 265–267. [PubMed] [Google Scholar]
- 19.Panda A, Mohan M, Chawdhary S. Corneal tattooing–experiences with “lamellar pocket procedure”. Indian J Ophthalmol 1984; 32: 408–411. [PubMed] [Google Scholar]
- 20.Cagatay HH, Gokce G, Ekinci M, et al. Long-term comparison of fibrin tissue glue and vicryl suture in conjunctival autografting for pterygium surgery. Postgrad Med 2014; 126: 97–103. [DOI] [PubMed] [Google Scholar]
- 21.Hino M, Ishiko O, Honda KI. Transmission of symptomatic parvovirus B19 infection by fibrin sealant used during surgery. Br J Haematol 2000; 108: 194–195. [DOI] [PubMed] [Google Scholar]