Abstract
Background:
Chronic obstructive pulmonary disease (COPD) is a major public health challenge in India with significant economic burden and healthcare utilization and contributes to patients’ daily life limitations. Health-related quality of life (HRQoL) reflects the health- and disease-related aspects of QoL. Limited studies have examined this dimension in healthcare settings. We explored the HRQoL among patients with COPD attending a tertiary care facility and the factors (enablers and constraints) influencing it.
Materials and Methods:
A parallel mixed-method study design was adopted to undertake the study. Data were collected from 110 patients with COPD attending the outpatient department of the tertiary care hospital at Bhubaneswar, Odisha, during June and July 2014. The translated and pretested version of St. George Respiratory Questionnaire (SGRQ) was used. In addition, in-depth interviews were held with 11 patients.
Results:
The overall HRQoL was significantly lower in females and patients from rural area. It declined with increasing age and was worst in patients age 70 years or above. Patients having two or more comorbid conditions had the poorest HRQoL. Reason for not using inhalers was mentioned to be perceived harm due to prolonged use. Family support and better financial condition were enablers while easy accessibility of healthcare facilities helped in early interventions.
Conclusion:
COPD has considerable negative impact on the QoL with advancing age and is worse among the geriatric age group population. Acute exacerbations impair HRQoL. The degree of severity of COPD could be determined by SGRQ which reflects the impairment of their HRQoL.
Keywords: Chronic obstructive pulmonary disease, health-related quality of life, St. George Respiratory Questionnaire, tertiary care hospital
Introduction
According to World Health Organization, globally chronic obstructive pulmonary disease (COPD) is a leading cause of mortality and morbidity.[1] COPD is a chronic respiratory disease characterized by a waning in lung function over a period of time, along with respiratory symptoms, primarily dyspnea, cough, and sputum production.[2] Consequently, COPD impacts on patients’ everyday life; it is linked with a significant economic burden which includes cost of hospitalization, wage loss due to work absence, and restricted physical ability.[3] Moreover, COPD being a chronic debilitating disease, patients are also confronted with daily life limitations, reduced daily activities (DAs), and reduced health-related quality of life (HRQoL) caused by complaints such as dyspnea, skeletal muscle dysfunction, and comorbidities.[4] According to recent reports, there is a continuous increase in COPD-related mortality. It is estimated that by the year 2020, COPD will be the third leading cause of death worldwide.[5]
According to the Center for Disease Control, HRQoL is an individual's or a group's perceived physical and mental health over time. HRQoL is defined as physical, psychological, and social domains of health that are unique to every individual.[6] It reflects the health and disease-related aspects of QoL. HRQoL measurements quantify the impact of disease, treatments, and tests on daily life and well-being in a formal and standardized way.[7] HRQoL has attracted considerable attention over the past decade as impaired health status is an important contributing factor of mortality, severity of disease and hospital admission, and response to diverse treatment options.[8,9] For patients with symptomatic COPD, information provided by the measures of HRQoL are way more informative and useful when compared with measures of lung function or exercise performance. Thus, inclusion of HRQoL assessment should be a fundamental measure of the conduct and interpretation of clinical studies.[10]
Worldwide studies have demonstrated the casual association between depression, anxiety, and HRQoL in patients with COPD.[11] A study done in Korea shows that HRQoL of patients with COPD over 40 years of age has significant association with disease severity and gender differences.[12] Another comparative study between patients with COPD and general population shows a significant difference in HRQoL. Another study on HRQoL among patients with COPD show a significant association between HRQoL, lung function, and dyspnea rating in patients with stable COPD.[13] A study by Menn et al. in 2010, among patients with severe COPD, shows that acute exacerbations seriously impair health status and QoL of patients.[14] A study in Germany among early working age population depicts that the relationship of HRQoL and COPD is largely influenced by common comorbidities.[4] A cross-sectional study by Weldam et al. exhibits the extent to which the interplay of illness perceptions, active coping, and depressive symptoms contribute to DAs and HRQoL in patients with COPD.[15] A study shows that lack of awareness among ex-smokers on the benefits of sustaining smoking cessation may be the main cause of their smoking relapse.[16] This study adds further that HRQoL is also affected by the duration of smoking cessation among patients with COPD. Studies on self-management education or daily practice of Spanish among patients with COPD show how to live a normal life and undertake the DAs, which otherwise are restricted due to physiological impairment, and to reduce severity of COPD by means of life style alternations.[17,18] High-intensity noninvasive ventilation is the most effective means of improving several physiological and clinical parameters in patients with chronic hypercapnia COPD.[19]
Studies estimated a significant difference in the mortality and morbidity associated with COPD Asian population when compared with developed countries. According to estimates, nearly 6%–8% of Indians are affected by COPD.[20,21] This rise in COPD-related burden will be most intense in Asian and African countries over the next two decades, mostly due to an increase in the prevalence of smoking.[22] Indoor air pollution, prior infection with tuberculosis, outdoor air pollution, and childhood respiratory infections are other important determinants for COPD in developing countries.[23]
Considering the above facts, this study was designed to explore the HRQoL among patients with COPD and the factors both enablers and constraints affecting it. Although many studies have reported impaired HRQoL in patients with COPD and poor HRQoL has been shown to be associated with different physiological factors, to the best of our knowledge, in Indian context, there is only one study from South India that found that patients with COPD had reduced quality life that was associated with duration of disease, severity of disease, and dyspnea.[24] To the best of the authors’ knowledge, there has been no study on the HRQoL among patients with COPD in the eastern India as well as in Odisha.
Situated on the eastern part of India, Odisha is a economically backward state with considerable population using traditional biomass fuel and exposure to indoor air pollution from domestic combustion of solid fuels; they use almost all forms of smoking products such as cigarettes and “bidis” contributing significantly to the risk of development of COPD. The COPD prevalence varies from 3% to 8% among Indian males and approximately 2.5% to 4.5% among Indian females.[25] It needs considerable attention to address the needs to improve the quality of care for these patients and delve deeper into the multiple aspects of the disease and its influence on the QoL. Taking all these points forward, this study is an attempt to look into the HRQoL among patients with COPD attending a chest clinic in an urban hospital in Odisha. The objective of this study is to assess the HRQoL among patients with COPD attending Capital Hospital Bhubaneswar, Odisha, India.
Materials and Methods
Study design and study setting
Bhubaneswar city is the state capital of Odisha, situated in the Khurda district of Odisha. Khurda district is the central district bounded by three districts, Cuttack on north side, Ganjam toward the south, and district Puri in the west. This district has a population of 1,877,395. The COPD scenario of the district is very critical and has increased since the past few years. All patients with COPD from the outdoor patient department (OPD) and indoor patient department (IPD) of chest and TB and medicine department were taken for the study. This is a cross-sectional study which includes a parallel mixed-method approach (using both quantitative and qualitative methods). The hospital is located in the capital city with all medical facilities catering to a population of Bhubaneswar and nearby locations within 100 km radius due to good communication facilities and due to free medicine supplies by the government.
Sampling and sample size
This study was undertaken during 1st June 2014 to 3rd August 2014 in Capital Hospital, Bhubaneswar, Odisha, India. Capital Hospital was selected purposely for this study. During these 2 months period of survey, 129 patients were reported to be diagnosed with COPD. All the patients above age 18 years were approached to participate in the study.
Methods of data collection
Quantitative data
St. George's Respiratory Questionnaire
The St. George Respiratory Questionnaire (SGRQ) is a standardized, self-administered questionnaire for measuring impaired health and perceived HRQoL in respiratory disease.[26] It contains 50 items with 76 weighted responses that cover three domains: symptoms – distress due to respiratory symptoms, activity – disturbances of physical activity, and impact – overall impact on daily life and well-being. Low scores indicate a better HRQoL. PW Jones has confirmed that the minimal important difference relevant to the patients is 4 on a scale of 0–100. According to the SGRQ guidelines, the score ranges from 0 to 100. If the score is 100, then HRQoL is worst, and if it is 0 it has a good score.[26]
A semi-structured questionnaire by SGRQ in English, translated to Odia script, was used for data collection. The tool was validated among 30 patients through pilot testing. Then necessary modifications and additions were done as per the study objectives. The questionnaire was administered through interview method after explaining and taking consent from concerned patients. The interview was done in a separate quite room keeping all the ethical consideration and privacy of the respondent confidential. Field staff checked the data immediately after the interviews to ensure accuracy and completeness of the filled-in questionnaires. A user-written computer program in SPSS and MS Excel was used for data entry and validation by trained data entry officers.
Qualitative data
We conducted in-depth interviews of 11 patients with COPD, both from IPD and OPD at Capital Hospital, Bhubaneswar. Each interview lasted from 45 to 60 min. The interviews were taped and translated in verbatim and analyzed using Thematic Framework Approach. The respondents were probed on their views regarding the different aspects of the disease such as (a) duration of the disease and frequency of exacerbations, (b) various symptoms of diseases such as shortness of breath, cough, exercise tolerance, musculoskeletal pain, and comorbidities if any, and impact on daily life (c) constraints and barriers on their health-seeking practices, (d) enablers or support systems and its effect, and (e) their perceived view on their health condition.
Data analysis
Descriptive statistics (i.e., means, standard deviations, and proportions) and bivariate analyses were used to describe the strength and association of sociodemographic characteristics, multimorbidity, and HRQoL among patients with COPD. All quantitative analyses were conducted using STATA software (version 11.2) manufactured by StataCorp. Qualitative analysis was done using thematic framework approach in which all the qualitative data collected are coded into separate thematic areas.
Ethical approval and participant consent
Ethical approval for the project was given by Institutional Ethical Committee of Indian Institute of Public Health, Bhubaneswar. Written informed consent was obtained from all participants after explaining them the objectives of the study and ensuring the anonymity of the data. Adherence to the guidelines of the Declaration of Helsinki was ensured at each step.
Results
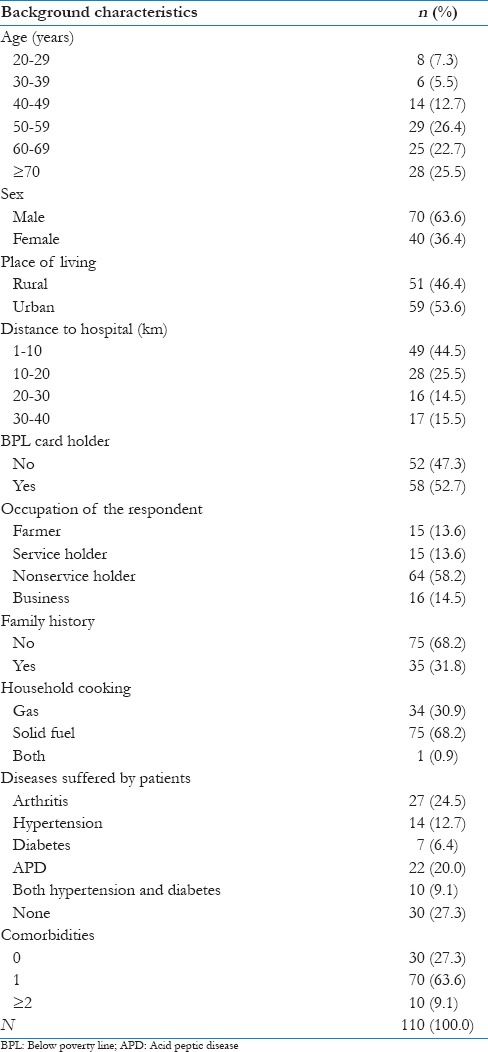
Of the 129 patients who agreed to participate in the survey, 110 patients completed the survey. The response rate was 85.2%. The sociodemographic characteristics of the patients are tabulated in Table 1.
Table 1.
Sociodemographic profile of chronic obstructive pulmonary disease patients, City Hospital, Bhubaneswar, 2014
Quantitative findings
The results from Table 1 depict that 75% of the patients were above 50 years of age; nearly 26% were in the age group of 50–59 years and 25% age 70 years or more. The minimum and maximum age was 22 and 86 years, respectively. Of 110 patients, 70 (63.6%) were male and 59 (53.6%) were from urban area. A total of 58 patients (52.7%) had below poverty line (BPL) card (which is an economic benchmark used by the Government of India to indicate economic disadvantage; the card is issued by them to get subsidized ration, etc.); 64 (58.2%) were nonservice holder. In all, 35 patients (31.8%) had positive family history of COPD; 75 patients (68.2%) were using solid fuel in house for cooking purpose. Of 110 patients, 27 (24.5%) patients suffer from arthritis. About 22 patients (20%) had acid peptic diseases (APD) and 12.7% had hypertension. The majority of the patient suffering with COPD presented with single comorbidity condition (70, 63.6%), while 10 patients had more than two comorbidities.
From Table 2, it can be seen that patients >70 years have a mean age of 68.7 years [standard deviation (SD) 11.4 years]. The mean overall QoL among female is 58.6 (SD 14.9) which is more than male 57.7 (SD 20.1). The mean overall QoL for patients living in rural area is 60.9 (SD 16.1). Patients with BPL card had a mean QoL score of 62.92 (SD 14.9). The QoL score increases rapidly across the numbers of comorbidities from no-comorbidity (mean: 47.3, SD 21.2) to two or more comorbidities (mean: 68.5, SD 14.5).
Table 2.
Component-wise QoL score by background characteristics among patients with chronic obstructive pulmonary disease, City Hospital, Bhubaneswar, 2014
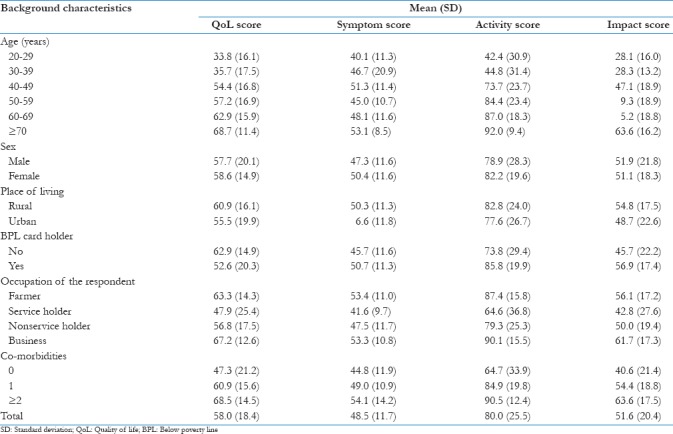
From the above table, it can be seen that patients >70 years have a mean age of symptom score of 53.1 (SD 8.5) and in the same age group the activity score with mean age is 92.0 (SD 9.4) and impact score 63.56 (SD 16.2). The mean symptom score of 50.38 (SD 11.6) and activity score of 82.2 (SD 19.6) among female are more than male. The mean symptom score for patients living in rural area is 50.3 (SD 11.2) and activity score 82.77 (24.0). Patients with BPL card had a mean activity score of 85.76 (SD 19.9) and impact score of 56.94 (SD 17.4). Symptom score, activity score, and impact increase with two or more comorbidities condition.
Qualitative findings
Few major themes emerged from the interviews. All the patients have been diagnosed with COPD for the past 3–12 years. Most of them have had acute episodes in the past 6 months and needed to be admitted to the in-patients department. Shortness of breath and cough were the two key symptoms that affected the daily life of patients. The majority of the respondents being daily wage earners, these symptoms prevented them from going to work and earning their livelihood. One of them being a betel shop owner said,
“Though I have to sit and work but because of shortness of breath and cough I am unable to converse with my customers and attend to them, hence I have to close my shop for days together and this shop is my only source of income.”
Another who is a domestic help said her job requires her to climb stairs and carry things, but because of shortness of breath she takes a long time to complete her work and “sits on the steps” frequently while climbing stairs. But those who were not employed and had less burden of daily work did not feel the shortness of breath to be a major issue. Low economic status of the patients was a key constraint. While most have been advised to use inhalers and all agreed that use of inhaler helped in alleviating symptoms, the major reason for non-use was the high cost of inhalers. One of the patients said,
“I am able to work comfortably after taking two sprays but I can’t take it daily as one inhaler costs 400 rupees and I can’t afford it, so I keep it only for very severe days.”
The other major reason for not using inhaler was the notion that long-term inhaler use could harm their health. One of them said,
“If I use it every day my breathlessness may subside but it may affect other parts of body, so my friends have said not to use it daily.”
Those who had less severe problem of shortness of breath were more worried about their comorbidities such as diabetes and coronary artery disease. Stable family support played a major positive role in disease coping and management. Those who had sympathetic family and friends were able to cope better with the disease and less anxious and worried about their condition. They took medications on time and had fewer incidences of exacerbations. Steady income and secure financial condition acted as an enabler in this disease management. Easy accessibility of hospital and better healthcare facilities helped in early interventions, fewer admissions into hospital, and reduced hospital days. Those of whom had mild shortness of breath and less frequent exacerbation rated their health as good and felt the disease did not have a major impact on their overall health. However, those who had moderate to severe shortness of breath and cough rated their health as bad and felt the disease to be a major hindrance in their life. They were more prone to feeling of sadness and anxiety.
Discussion
Studies showed that COPD is a major public health threat in India. Patients with COPD are challenged with restricted physical activities and reduced HRQoL. This is due to dyspnea and systemic effects such as skeletal muscle dysfunction and comorbidities. Multiple drivers interplay which enhances the complexity of living with COPD. In addition to physical functioning, it is worth exploring these drivers to get a holistic picture of the central issue.
In this study conducted at the Capital Hospital, Bhubaneswar, there was a predominance of COPD in males (64%) than females (36%). Similar results were reported in previous studies.[20,22,27] About 75% of our sample in the study were above the age of 50 years. An Indian Study on Epidemiology of Asthma, Respiratory Symptoms and Chronic Bronchitis in Adults (INSEARECH) involving a total of 85,105 men and 84,470 women from 12 urban and 11 rural showed that the overall prevalence of chronic bronchitis in adults >35 years was 3.49%.[27] Hence, with advancing years COPD is an important comorbidity. There was higher proportion of “non-service holders” (58%) among the sample, and almost 53% were BPL card holders and around 32% of the respondents had a positive family history of COPD.
Almost 50% of the world's total population use biomass fuel as the primary source of energy for domestic cooking, heating, and lighting.[28] Inferior quality stoves, in addition to poorly ventilated indoors, are used by women in rural areas for cooking purposes. Such an extent of exposure to biomass fuel combustion products makes women and household members vulnerable to COPD. The biomass smoke exposure is a risk factor for developing COPD in both women and men as demonstrated in a systematic review conducted by Kurmi et al.[23] In this study, almost 68% of the sample were using biomass fuel at their homes.[23] About 64% of the sample had single comorbid condition and arthritis was found to be the commonest among them (25%), followed by APD (20%).
The QoL scores of this study generally indicate the patients had poor health status. With regard to age, it is seen that HRQol score rises rapidly in the age group of 40–49 years and is highest in the age group above 70 years. Therefore, COPD has a substantial negative bearing on the QoL with advancing age and is worse among the geriatric age group population (68.7%). As shown in previous studies, in this study too the mean overall HRQol is higher among females than males. While respondents from the rural areas had poorer QoL than their urban counterparts, it could be attributed to the lack of easily accessible healthcare facilities and generally come to higher center only when the severity of disease increases. The distance from the available health facilities also attributed significantly to the QoL, with the patients within 10 km of the hospital having lower scores than those far away. The highest score being among people staying more than 30 km from that hospital. It again reinforces the need to have easy to reach healthcare facilities for improved QoL among patients with COPD. Among studies in the past, low socioeconomic status has been linked to poor QoL among patients with COPD. Likewise, our data also supported this finding. In this study, patients with low incomes (as BPL card holders in this study) had about a mean of 62.9. Hence, it is felt that augmenting socioeconomic status would help in coping the disease better and improve the QoL. Here, we found that patients having more than two comorbid conditions had the highest score (68.5), and it was lowest among those who did not have a single comorbidity.
This study has some limitations. It was a hospital-based survey, and as such the participants included in the study may be skewed toward the very sick patients. Considering the high cost associated with setting-based care, patients often do not access healthcare in low-income or developing countries until their clinical condition becomes very serious. This potentially limits the ability to generalize the results of this study to all patients with COPD. Other limitations of the study include time constraints; relatively small sample size; as this was a cross-sectional study, it was not possible to determine the causal association between risk factors and HRQoL; and patients taking alternative medicines.
As high morbidity and mortality are associated with COPD, an early recognition of symptoms is important. Our study reported that patients with COPD had an impaired QoL overall. HRQoL was impaired across all levels of severity of airway obstruction. HRQoL measures the personal and social context of the patients. According to this study, with an increase in age, that is above 50 years, the HRQoL reduced with impaired DAs. This may be due to smoking habits, air pollution, inhalation of irritants, and so on. Positive family history of patients with COPD shows a genetic relevance. Low-income group people have an impaired HRQoL who use solid fuels instead of gas which causes irritation and air way obstruction aggravating COPD.
Extrapulmonary comorbidities such as arthritis and APD have decreased their DAs; due to these comorbidities, the study shows that the QoL was impaired. In few cases, it was seen that patients were unable to do their routine DAs and few had to change their profession. Rural females in the age group above 60–70 years have high total score, that is, toward 100 which shows their HRQoL was impaired. This may be due to use of biomass fuels for domestic cooking, lack of education, lack of awareness, or lack of healthcare among rural females. It was seen that females were taken to the hospital only when the symptoms get worse and hamper their DAs. Social beliefs and use of alternative medicines (such as homeopathic, Ayurvedic) could be the other possible reasons. The findings of the study also show that there is a rapid increase in the number of patients with two or more comorbidities reducing their HRQoL.
Conclusion
This study concludes that QoL is impaired in patients with COPD which deteriorates with increasing severity of disease. Increasing severity increases the SGRQ scores, that is, the total and individual scores. Acute exacerbations impair HRQoL. The properties of SGRQ were good. The degree of patients with COPD could be determined by scores using SGRQ which reflects the impairment of their HRQoL. The study findings recommend that elderly population and their caretakers should be educated on improving the provision of fresh air within house. Health education to the population on symptoms appraisal, preventing late diagnosis, early treatment-seeking, and better adherence to treatment of respiratory illnesses to recover the physical domain of QoL might be helpful. The study further suggests for intervention-based large-scale studies on patients with COPD, advocacy, and research to strengthen policies and programs toward elderly.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. Chronic Respiratory Diseases. Burden of COPD; 2016. [Last accessed on 2017 May 29]. Available from: http://www.who.int/respiratory/copd/burden/en/ [Google Scholar]
- 2.Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS, GOLD Scientific Committee et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO global initiative for chronic obstructive lung disease (GOLD) workshop summary. Am J Respir Crit Care Med. 2001;163:1256–76. doi: 10.1164/ajrccm.163.5.2101039. [DOI] [PubMed] [Google Scholar]
- 3.Guarascio AJ, Ray SM, Finch CK, Self TH. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res. 2013;5:235–45. doi: 10.2147/CEOR.S34321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wacker ME, Hunger M, Karrasch S, Heinrich J, Peters A, Schulz H, et al. Health-related quality of life and chronic obstructive pulmonary disease in early stages – Longitudinal results from the population-based KORA cohort in a working age population. BMC Pulm Med. 2014;14:134. doi: 10.1186/1471-2466-14-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murray CJ, Lopez AD. Vol. 1. Boston: Harvard University Press; 1996. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Deceases, Injuries and Risk Factors in 1990 and Projected to 2010; pp. 1–35. [Google Scholar]
- 6.Testa MA, Simonson DC. Assessment of quality-of-life outcomes. N Engl J Med. 1996;334:835–40. doi: 10.1056/NEJM199603283341306. [DOI] [PubMed] [Google Scholar]
- 7.Post MW. Definitions of quality of life: What has happened and how to move on. Top Spinal Cord Inj Rehabil. 2014;20:167–80. doi: 10.1310/sci2003-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Testa MA, Simonson DC. Assessment of quality-of-life outcomes. N Engl J Med. 1996;334:835–40. doi: 10.1056/NEJM199603283341306. [DOI] [PubMed] [Google Scholar]
- 9.Gosker HR, Wouters EF, van der Vusse GJ, Schols AM. Skeletal muscle dysfunction in chronic obstructive pulmonary disease and chronic heart failure: Underlying mechanisms and therapy perspectives. Am J Clin Nutr. 2000;71:1033–47. doi: 10.1093/ajcn/71.5.1033. [DOI] [PubMed] [Google Scholar]
- 10.van der Molen T, Miravitlles M, Kocks JW. COPD management: Role of symptom assessment in routine clinical practice. Int J Chron Obstruct Pulmon Dis. 2013;8:461–71. doi: 10.2147/COPD.S49392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blakemore A, Dickens C, Guthrie E, Bower P, Kontopantelis E, Afzal C, et al. Depression and anxiety predict health-related quality of life in chronic obstructive pulmonary disease: Systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2014;9:501–12. doi: 10.2147/COPD.S58136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim SH, Oh YM, Jo MW. Health-related quality of life in chronic obstructive pulmonary disease patients in Korea. Health Qual Life Outcomes. 2014;12:57. doi: 10.1186/1477-7525-12-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Justine M, Tahirah F, Mohan V. Health-related quality of life, lung function and dyspnea rating in COPD patients. Monaldi Arch Chest Dis. 2013;79:116–20. doi: 10.4081/monaldi.2013.5209. [DOI] [PubMed] [Google Scholar]
- 14.Menn P, Weber N, Holle R. Health-related quality of life in patients with severe COPD hospitalized for exacerbations – Comparing EQ-5D, SF-12 and SGRQ. Health Qual Life Outcomes. 2010;8:39. doi: 10.1186/1477-7525-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weldam SW, Lammers JW, Decates RL, Schuurmans MJ. Daily activities and health-related quality of life in patients with chronic obstructive pulmonary disease: Psychological determinants: A cross-sectional study. Health Qual Life Outcomes. 2013;11:190. doi: 10.1186/1477-7525-11-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abu Hassan H, Abd Aziz N, Hassan Y, Hassan F. Does the duration of smoking cessation have an impact on hospital admission and health-related quality of life amongst COPD patients? Int J Chron Obstruct Pulmon Dis. 2014;9:493–8. doi: 10.2147/COPD.S56637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Monninkhof E, van der Valk P, van der Palen J, van Herwaarden C, Partridge MR, Zielhuis G, et al. Self-management education for patients with chronic obstructive pulmonary disease: A systematic review. Thorax. 2003;58:394–8. doi: 10.1136/thorax.58.5.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Almagro P, Castro A. Helping COPD patients change health behavior in order to improve their quality of life. Int J Chron Obstruct Pulmon Dis. 2013;8:335–45. doi: 10.2147/COPD.S34211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Storre JH, Matrosovich E, Ekkernkamp E, Walker DJ, Schmoor C, Dreher M, et al. Home mechanical ventilation for COPD: High-intensity versus target volume noninvasive ventilation. Respir Care. 2014;59:1389–97. doi: 10.4187/respcare.02941. [DOI] [PubMed] [Google Scholar]
- 20.Adeloye D, Chua S, Lee C, Basquill C, Papana A, Theodoratou E, et al. Global and regional estimates of COPD prevalence: Systematic review and meta-analysis. J Glob Health. 2015;5:020415. doi: 10.7189/jogh.05-020415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhome AB. COPD in India: Iceberg or volcano? J Thorac Dis. 2012;4:298–309. doi: 10.3978/j.issn.2072-1439.2012.03.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan-Yeung M, Aït-Khaled N, White N, Ip MS, Tan WC. The burden and impact of COPD in Asia and Africa. Int J Tuberc Lung Dis. 2004;8:2–14. [PubMed] [Google Scholar]
- 23.Kurmi OP, Semple S, Simkhada P, Smith WC, Ayres JG. COPD and chronic bronchitis risk of indoor air pollution from solid fuel: A systematic review and meta-analysis. Thorax. 2010;65:221–8. doi: 10.1136/thx.2009.124644. [DOI] [PubMed] [Google Scholar]
- 24.Shavro SA, Ezhilarasu P, Augustine J, Bechtel JJ, Christopher DJ. Correlation of health-related quality of life with other disease severity indices in Indian chronic obstructive pulmonary disease patients. Int J Chron Obstruct Pulmon Dis. 2012;7:291–6. doi: 10.2147/COPD.S26405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jindal SK, Aggarwal AN, Gupta D. A review of population studies from india to estimate national burden of chronic obstructive pulmonary disease and its association with smoking. Indian J Chest Dis Allied Sci. 2001;43:139–47. [PubMed] [Google Scholar]
- 26.Jones PW. St. George's Respiratory Questionnaire: MCID. COPD. 2005;2:75–9. doi: 10.1081/copd-200050513. [DOI] [PubMed] [Google Scholar]
- 27.Parasuramalu BG, Huliraj N, Prashanth Kumar SP, Gangaboraiah, Ramesh Masthi NR, Srinivasa Babu CR, et al. Prevalence of chronic obstructive pulmonary disease and its association with tobacco smoking and environmental tobacco smoke exposure among rural population. Indian J Public Health. 2014;58:45–9. doi: 10.4103/0019-557X.128166. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. Household Energy and Health Household Energy and Health. 2006. [Last accessed on 2017 Jun 23]. Available from: http://www.who.int/indoorair/publications/fuelforlife.pdf .


