Abstract
Introduction:
As a new healthcare market force and first point of contact, family physicians (FPs) play a key role in healthcare delivery system. It is vital to understand issues that affect performance and satisfaction with their practices and working environment. The objectives of this study are to assess the level of professional satisfaction and to compare and identify the factors potentially associated with professional satisfaction/dissatisfaction among FPs of two regions.
Materials and Methods:
A comparative cross-sectional study on FPs working in primary healthcare centers under Ministry of Health was conducted in two regions (Jeddah and Eastern region) to assess job satisfaction and dissatisfaction among them. Validated close-ended questionnaire was emailed. Overall satisfaction along with the associated factors was identified. Chi-square and multivariate regression analyses were performed to test the association between job satisfaction and predictors.
Results:
A total of 237 FPs completed the survey and an overall 62% of them were satisfied. Male doctors were less in number yet more satisfied (71%). FPs of eastern region were slightly more satisfied (63.4%) when compared with 59.2% of Jeddah. Factors significantly associated with professional dissatisfaction included FPs having the opinion that they were not respected by community members [odds ratio (OR) 2.7, confidence interval (CI): 1.24–5.97, P = 0.012] and FPs’ own perception of being inferior to other specialties (OR 13.59, CI: 4.98–37.07, P < 0.001).
Conclusion:
More than half of the FPs were professionally satisfied; however, the majority had perception of being inferior to other specialties. Improving self-esteem, working environment, and addressing other identified factors for dissatisfaction can help FPs overcome their stresses, leading to better healthcare delivery.
Keywords: Family physician, job satisfaction, primary healthcare center, stress
Introduction
Healthcare delivery has changed dramatically in the past few decades, focusing mainly on community-oriented primary healthcare approach.[1] The main primary healthcare providers in any setting remain to be the family physicians (FPs). FPs’ role varies from providing coordinated and continuous primary healthcare, health education, counseling, and so on.[2] Recently, a visible undesirable change is seen in the way FPs deliver healthcare. The main reason identified in the studies is low satisfaction level of the FPs.[3,4] As a frontline healthcare provider to the community, it becomes particularly important to recognize factors affecting their job satisfaction.[2,3]
Retaining a suitable and competent workforce is important for better functioning of any organization.[4] Sometimes, it becomes difficult to realize the factors for increased turnover of the workforce. Dissatisfied employees are more likely to show intention to leave their job and this intent is associated with actual turnover.[3,4,5,6] Studies show that job satisfaction could function as a buffer against conditions favoring increased turnover.[7,8] If due attention is given to job satisfaction of the employees, it may prevent staff shortage and reduce mental stress.[6]
Insufficient number of trained physicians and increasing demand make it more difficult to promote professional job satisfaction.[7] Studies identify four major job stressors including demands of the job with less reward and patients’ expectations, interference with family life, constant interruptions at work and home, and administration of practice.[9] Job dissatisfaction among doctors not only affects patient's quality of care but also their own mental health.[9,10,11] Resulting in more medical errors decreased patient satisfaction, ultimately putting patients at risk.[12,13,14,15]
As a general perception, doctors are assumed to have a tough, demanding, and challenging life. That is why physician's job satisfaction was not considered as a topic worth discussing.[15] However, recent studies have highlighted high level of job dissatisfaction and stress among doctors affecting quality of care.[16,17] Around 38% Canadian doctors described “medical practice” itself as extremely stressful, as one has to deal with difficult cases, aggressive patients, and their attendants.[18] Modern changes in the healthcare system, increase in the workload, reduced physician's autonomy, and respect are some of the main reasons for dissatisfaction.[13,14] Job dissatisfaction is directly related to burnout among physicians.[16]
With the paradigm shift toward primary healthcare, the level of satisfaction should be assessed.[2,13] FPs are the first line of contact between the health department and population. The level of their professional satisfaction directly affects patient's care. In this study, we aimed to access the perceptions and satisfaction level of the FPs in primary healthcare centers (PHCCs) working under Ministry of Health of two regions, that is, Jeddah and Eastern region. Literature search shows no such comparative study has been conducted in PHCCs. Moreover, we tried to identify the reasons for job satisfaction and dissatisfaction among them which is affecting their performance and keeping them under constant stress/pressure. The findings of this study would help overcome the issues faced by the physicians at their work places and in improving strategies and policies to overcome these issues. Indirectly it would improve quality of patient care and patient's satisfaction.
Materials and Methods
A comparative cross-sectional mailed questionnaire-based survey was conducted in different PHCCs having FPs present in Jeddah and Eastern region working under Ministry of Health. All FPs fulfilling the inclusion criteria working in the selected PHCCs were included in the study. The duration of this study was 9 months, that is, from 1st January 2017 to 1st October 2017. Jeddah region included Jeddah city and its peripheral towns/areas. Eastern region included Damman, Al-Khober, Al-Qatif, Al-Jubail, and Safwa. There were total of 116 FPs in Jeddah region and 180 in Eastern region (inside included cities).
We selected PHCCs using cluster sampling technique (one cluster of PHCCs of Jeddah and other of Eastern region). We emailed questionnaire to all the FPs working in these two regions and fulfilling inclusion criteria. Follow-up was done by reminding them through SMS and telephone calls. However, the response rate was less from Eastern region FPs (was around 74.4%, n = 134) when compared with 89% (n = 103) of Jeddah region.
A validated close-ended structured questionnaire was adopted from previous studies conducted in Pakistan,[2] the United States,[15,17] and Canada.[11,18] Data were collected and compiled in soft and hard copies. Data analysis was done using SPSS 22 (IBM SPSS Statistics for Windows, Version 22.0; IBM Corp., Armonk, NY, USA). Categorical variables were used for descriptive epidemiology. Chi-square was used to find association between categorical variables and professional satisfaction. Multivariate regression was performed to determine significant predictors of satisfaction in physicians. Significant variables in bivariate analysis were included as covariates in multivariate logistic regression model [using a backward stepwise (likelihood ratio) method] to evaluate the predictors for FPs’ dissatisfaction. In logistic regression, dissatisfied FPs were our referent group and were compared through odds ratio (OR) with FPs who claimed to be satisfied. To generate the best fit model, eight independent variables have been entered and total of seven steps have been run. P value <0.05 was considered significant.
FPs of the two regions having at least 6 months’ experience were included in this study. Only four FPs of Jeddah and nine FPs of Eastern region were having less than 6 months experience, and hence were excluded. FPs are specialist/consultant doctors who have finished and cleared exit examination after 4 years of postgraduate residency training in Family Medicine. All the general practitioners (general practitioners are simple undergraduate doctors with no postgraduate training in Family Medicine) were also excluded.
Ethical approval was taken from ethical committee of Ministry of Health (H-02-J-002-076) and Directorate of Health Affairs, Jeddah and Eastern region. Physicians were ensured about the confidentiality of data.
Results
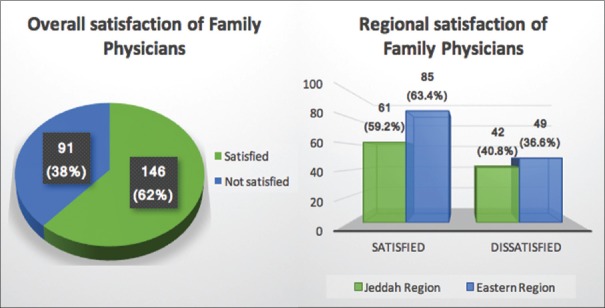
The mean age of FPs working in Ministry of Health PHCCs was 37.8 ± 5.7 years. Of the 237 doctors, 67.1% (n = 159) were females. The majority of doctors were married (n = 206, 86.9%). Most of the study participants (n = 195, 82.1%) had less than 10 years of experience as FP. The mean daily working hours of FPs were 5.79 ± 3.19 h with mean daily out patient department of 24 ± 8 patients. FPs of Eastern region were slightly more satisfied (63%) when compared with Jeddah region (59%); however, this difference was not statistically significant (P = 0.509). Overall and regional satisfaction of the FPs is shown in Figure 1.
Figure 1.
Overall and regional satisfaction of family physicians (n = 237)
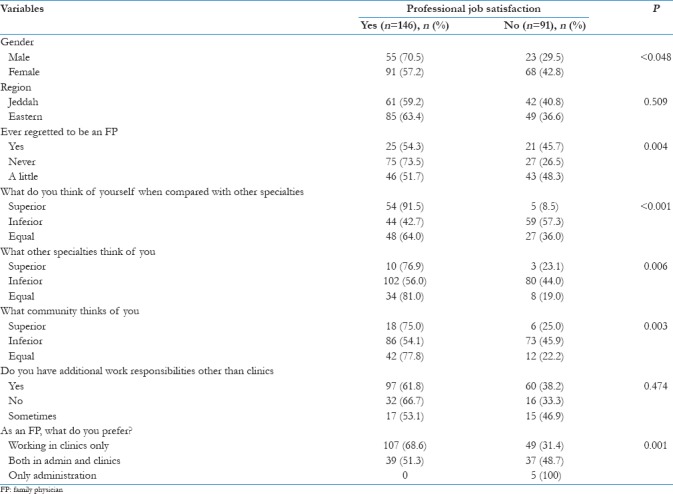
Male doctors were less in number yet more satisfied (n = 55, 70.5%) when compared with female doctors (n = 91, 57.2%). Most study participants think themselves inferior to other specialties. Similarly, the majority perceived that the community and doctors of other specialties all consider them as an inferior specialty [Table 1]. The majority satisfied FPs did not desire any additional administrative work (n = 155, P < 0.001). Teaching/training postgraduate residents was the only additional duty in which around 61% (n = 144) FPs showed interest.
Table 1.
Professional job satisfaction status (n=237)
Additional work responsibilities for the FPs included working as a technical director of PHCC, quality coordinator, teaching/training supervisor, and head of department of public health administration/health supervisory sector. Most FPs had a combination of responsibilities from the above-mentioned list.
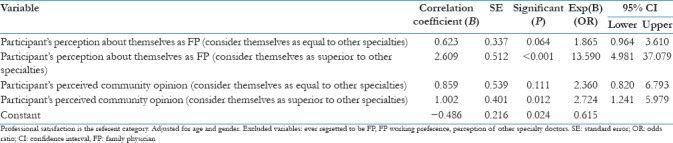
Multivariate regression analysis was conducted to highlight potential risk factors for the overall satisfaction of FPs. In the final model, factors significantly associated with professional dissatisfaction included the FPs were of the opinion that they were not respected by community members. If community perception regarding FPs is moved from inferior to superior, FPs’ satisfaction is around three times improved [OR 2.7, confidence interval (CI): 1.24–5.97, P = 0.012]. Similarly, FPs who consider themselves inferior to other specialties were around 13 times dissatisfied when compared with FPs who think themselves superior to other specialties (OR 13.59, CI: 4.98–37.07, P < 0.001) [Table 2].
Table 2.
Multivariate regression analysis predicting factors for satisfaction (n=237)
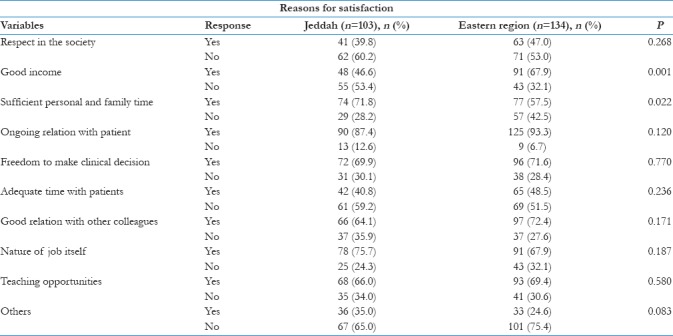
Sufficient personal and family time, ongoing relation with patient, freedom in clinical decisions, good relation with other colleagues, and sufficient teaching opportunities were highlighted as main reasons for their job satisfaction in both regions. Other reasons for satisfaction are enlisted in Table 3.
Table 3.
Comparison between regions highlighting reasons for satisfaction (n=237)
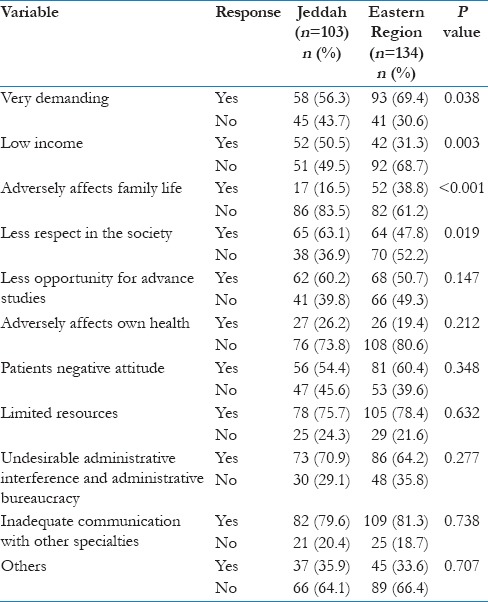
A demanding field with increased patient load, interfering administration, having less respect in the society, and less opportunities for advance studies were highlighted as main reasons for their job dissatisfaction. Other reasons for dissatisfaction are given in Table 4.
Table 4.
Comparison between regions highlighting reasons for dissatisfaction (n=237)
Discussion
The findings of this study have given an insight into the factors associated with the satisfaction of FPs working in PHCCs of two regions. As the PHCC is the first line of contact between the patients and doctors, it was of considerable importance that level of job satisfaction of FPs be assessed. This is not the first study that addresses job satisfaction in Saudi Arabia per se;[19,20] however, this is the first survey of its kind that assesses the level of job satisfaction in FPs of two different regions/provinces.
The overall level of job satisfaction was seen in 62% FPs which is comparable to some regional[2,21,22] as well as studies conducted in the United States[5] and Canada.[18] Satisfaction of FPs suggests that they have adjusted well to the changing landscape of medical practice. However, a study conducted in Al-Madina Munawara, Saudi Arabia, demonstrated overall physician's satisfaction to be 48% much less than our study.[20] This study highlighted male FPs being more satisfied when compared with female doctors. Similar findings of lower job satisfaction in female physicians in other parts of Saudi Arabia were pointed out by Al Juhani and Kishk.[20] Possible explanation could be the fact that females usually experience more conflict between their work and personal life.
FPs of Eastern region were slightly more satisfied (63%) when compared with Jeddah (59%). Possible explanation for better satisfaction can be more freedom in making clinical decisions, spending more time with patients which make their relationship stronger, and geographical diversity of Eastern region. Moreover, Eastern region has continuous physician competency program involving FPs; also, coaching and mentoring for FPs with continuous meetings and wide spread of family medicine approach practice in PHCC lead to better satisfaction. Findings of study conducted by Fahrenkopf et al.[15] and Burke and Richardsen[18] complement the findings of our study.
The majority (79%) of our study participants had no regret being an FP. This was consistent with US[17] and Canadian[18] doctors where most of the physicians (84% and 78%, respectively) were satisfied, and if given the chance most of them were willing to select the same specialty next time. This increased liking and change in doctor's attitude toward family medicine is due to less hectic job, no emergency calls/duties, and suitable timings especially for females. Current trends of adopting family medicine and changes in healthcare delivery are unlikely to disrupt the FP workforce.[17] However, a study conducted in Pakistan highlighted a number of doctors regretting being working in PHCC.[2] Posted to far-flung areas with lack of facilities provided to doctors and aggressiveness of uneducated patients/attendants were few reasons for regret.[2] Some older FPs even though working in developed countries, but in the rural areas, were also less satisfied.[17,18]
Participants of studies conducted in Pakistan,[2,21] India,[22] and other developing countries[11] consider limited earning potential when compared with other specialties, lack of recognition, and respect from not only the community but also by other specialty doctors as factors significantly associated with professional dissatisfaction. In our study too, the main predictors for dissatisfaction were more or less the same, considering themselves inferior to other specialties and wrong perception that the community also believes them to be inferior. Pride at work, specialty, and self-esteem of FPs need to be improved. Along with this, community's perception needs to be changed too. This could be attributed to the wrong perception by most of the specialist or consultant doctors working in hospitals thinking themselves as superior. These findings were not consistent with the developed countries where every doctor is given the same respect.[17,18]
Less professional growth opportunities, demanding patient care, and work/patient overload were the most frequently encountered domains identified for physician's dissatisfaction in most national and international studies.[19,20,21,22,23] Our study participants also reported the contribution of the unmet need for career advancement and lack of adequate resources for patient care as possible explanations for low job satisfaction. Another factor highlighted in many studies[21,22,24] was low income, which was not considered a reason for dissatisfaction in our FPs.
Studies conducted in different states of the United States[17,25] identified in detail the different causes of professional dissatisfaction, including administrative interference resulting in many obstacles in providing quality of care, difficult interface, and time-consuming data entry of electronic health record especially for senior physicians. Electronic record was not being maintained in our PHCCs, yet it was not considered as an obstacle here. Lack of autonomy and work control, and relationship with colleagues were few other reasons for dissatisfaction identified in the United States.[25] FPs of our study also pointed repeated interference by administration and decisions taken by administrative bureaucracy without involving workforce to be contributors of dissatisfaction.
Additional responsibilities other than examining patients seemed to be part of FPs’ work. The majority of FPs were performing duties in administration like technical director of PHCC, quality coordinator, working in public health administration, and teaching postgraduate trainees. Although FPs were fulfilling these responsibilities, majority did not desire to perform extra duties. This extra administrative workload leads to physician's burnout.[16] However, teaching/training postgraduate trainees was one area where around 60% of FPs showed interest. Similar findings were reported in the studies conducted in Canada[26] and Japan.[27] Consultant FPs should be encouraged by facilitating them to teach the future generation.
The limitation of this study was low response rate from FPs of Eastern region which might have affected the comparison. Although a sample of FPs was selected from diverse geographical area, the doctors in our sample were not representative of all FPs working in Saudi Arabia.
Conclusion
Most of the FPs of both the regions were generally satisfied, with majority having perception of being inferior to other specialties. Improving self-esteem, working environment, and addressing other identified factors for dissatisfaction can help FPs overcome their stresses leading to better healthcare delivery.
It was recommended that healthcare policy makers need to implement immediate, extensive, and decisive measures. These improvements in health reforms and policies can help in elevating the job satisfaction level. Future exploration on work–life balance among FPs aiming to improve career and lifestyle harmony should be carried out.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We would like to acknowledge Mrs. Etidal Abdullah Alshumrani and Mrs. Mona Ahmed Shamia for help in “data collection.”
References
- 1.International Conference on Primary Health Care. Declaration of Alma-Ata. WHO Chron. 1978;32:428–30. [PubMed] [Google Scholar]
- 2.Ashraf H, Shah N, Anwer F, Akhtar H, Abro MA, Khan A, et al. Professional satisfaction of family physicians in Pakistan – Results of a cross-sectional postal survey. J Pak Med Assoc. 2014;64:442–6. [PubMed] [Google Scholar]
- 3.Misra-Hebert AD, Kay R, Stoller JK. A review of physician turnover: Rates, causes, and consequences. Am J Med Qual. 2004;19:56–66. doi: 10.1177/106286060401900203. [DOI] [PubMed] [Google Scholar]
- 4.Buchbinder SB, Wilson M, Melick CF, Powe NR. Primary care physician job satisfaction and turnover. Am J Manag Care. 2001;7:701–13. [PubMed] [Google Scholar]
- 5.Parsons SK, Simmons WP, Penn K, Furlough M. Determinants of satisfaction and turnover among nursing assistants. The results of a statewide survey. J Gerontol Nurs. 2003;29:51–8. doi: 10.3928/0098-9134-20030301-11. [DOI] [PubMed] [Google Scholar]
- 6.Seston E, Hassell K, Ferguson J, Hann M. Exploring the relationship between pharmacists’ job satisfaction, intention to quit the profession, and actual quitting. Res Social Adm Pharm. 2009;5:121–32. doi: 10.1016/j.sapharm.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 7.Peterson LE, Eden A, Cochrane A, Hagen M. Physician satisfaction with and practice changes resulting from American board of family medicine maintenance of certification performance in practice modules. J Contin Educ Health Prof. 2016;36:55–60. doi: 10.1097/CEH.0000000000000022. [DOI] [PubMed] [Google Scholar]
- 8.Honarvar B, Lankarani KB, Ghahramani S, Akbari M, Tabrizi R, Bagheri Z, et al. Satisfaction and dissatisfaction toward urban family physician program: A population based study in Shiraz, Southern Iran. Int J Prev Med. 2016;7:3. doi: 10.4103/2008-7802.173793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindsay E, Wooltorton E, Hendry P, Williams K, Wells G. Family physicians’ continuing professional development activities: Current practices and potential for new options. Can Med Educ J. 2016;7:e38–46. [PMC free article] [PubMed] [Google Scholar]
- 10.Young R, Webb A, Lackan N, Marchand L. Family medicine residency educational characteristics and career satisfaction in recent graduates. Fam Med. 2008;40:484–91. [PubMed] [Google Scholar]
- 11.Thind A, Freeman T, Thorpe C, Burt A, Stewart M. Family physicians’ satisfaction with current practice: What is the role of their interactions with specialists? Healthc Policy. 2009;4:e145–58. [PMC free article] [PubMed] [Google Scholar]
- 12.Libert Y, Canivet D, Ménard C, Van Achte L, Farvacques C, Merckaert I, et al. Predictors of physicians’ satisfaction with their management of uncertainty during a decision-making encounter with a simulated advanced stage cancer patient. Patient Educ Couns. 2016;99:1121–9. doi: 10.1016/j.pec.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 13.Linzer M, Poplau S, Brown R, Grossman E, Varkey A, Yale S, et al. Do work condition interventions affect quality and errors in primary care? Results from the healthy work place study. J Gen Intern Med. 2017;32:56–61. doi: 10.1007/s11606-016-3856-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harms R. Physicians, professionalism and organizational efforts to improve quality – A systems perspective. WMJ. 2004;103:63–4. [PubMed] [Google Scholar]
- 15.Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VW, et al. Rates of medication errors among depressed and burnt out residents: Prospective cohort study. BMJ. 2008;336:488–91. doi: 10.1136/bmj.39469.763218.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bawakid K, Abdulrashid O, Mandoura N, Shah HBU, Ibrahim A, Akkad NM, et al. Burnout of physicians working in primary health care centers under ministry of health Jeddah, Saudi Arabia. Cureus. 2017;9:e1877. doi: 10.7759/cureus.1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hueston WJ. Family physicians’ satisfaction with practice. Arch Fam Med. 1998;7:242–7. doi: 10.1001/archfami.7.3.242. [DOI] [PubMed] [Google Scholar]
- 18.Burke RJ, Richardsen AM. Sources of satisfaction and stress among Canadian physicians. Psychol Rep. 1990;67:1335–44. doi: 10.2466/pr0.1990.67.3f.1335. [DOI] [PubMed] [Google Scholar]
- 19.Kalantan KA, Al-Taweel AA, Abdul Ghani H. Factors influencing job satisfaction among primary health care (PHC) physicians in Riyadh, Saudi Arabia. Ann Saudi Med. 1999;19:424–6. doi: 10.5144/0256-4947.1999.424. [DOI] [PubMed] [Google Scholar]
- 20.Al Juhani AM, Kishk NA. Job satisfaction among primary health care physicians and nurses in Al-Madinah Al-Munawwara. J Egypt Public Health Assoc. 2006;81:165–80. [PubMed] [Google Scholar]
- 21.Shakir S, Ghazali A, Shah IA, Zaidi SA, Tahir MH. Job satisfaction among doctors working at teaching hospital of Bahawalpur, Pakistan. J Ayub Med Coll Abbottabad. 2007;19:42–5. [PubMed] [Google Scholar]
- 22.Kaur S, Sharma R, Talwar R, Verma A, Singh S. A study of job satisfaction and work environment perception among doctors in a tertiary hospital in Delhi. Indian J Med Sci. 2009;63:139–44. [PubMed] [Google Scholar]
- 23.Vernooij-Dasssen MJ, Faber MJ, Olde Rikkert MG, Koopmans RT, van Achterberg T, Braat DD, et al. Dementia care and labour market: The role of job satisfaction. Aging Ment Health. 2009;13:383–90. doi: 10.1080/13607860902861043. [DOI] [PubMed] [Google Scholar]
- 24.Hann M, Reeves D, Sibbald B. Relationships between job satisfaction, intentions to leave family practice and actually leaving among family physicians in England. Eur J Public Health. 2011;21:499–503. doi: 10.1093/eurpub/ckq005. [DOI] [PubMed] [Google Scholar]
- 25.Hier DB, Rothschild A, LeMaistre A, Keeler J. Differing faculty and housestaff acceptance of an electronic health record. Int J Med Inform. 2005;74:657–62. doi: 10.1016/j.ijmedinf.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 26.Thommasen HV, Lavanchy M, Connelly I, Berkowitz J, Grzybowski S. Mental health, job satisfaction, and intention to relocate. Opinions of physicians in rural British Columbia. Can Fam Physician. 2001;47:737–44. [PMC free article] [PubMed] [Google Scholar]
- 27.Tokuda Y, Hayano K, Ozaki M, Bito S, Yanai H, Koizumi S, et al. The interrelationships between working conditions, job satisfaction, burnout and mental health among hospital physicians in Japan: A path analysis. Ind Health. 2009;47:166–72. doi: 10.2486/indhealth.47.166. [DOI] [PubMed] [Google Scholar]