Abstract
Background: Patient portals have shown potential for increasing health care quality and efficiency. Internet access and other factors influencing patient portal use could worsen health disparities.
Methods: Observational study of adults with 1 or more visits to the outpatient clinics of an urban public health care system from 2012 to 2015. We used mixed effects logistic regression to evaluate the association between broadband internet access and (1) patient portal initiation (whether a patient logged in at least 1 time) and (2) messaging, controlling for demographic and neighborhood characteristics.
Results: There were 243 248 adults with 1 or more visits during 2012–2015 and 70 835 (29.1%) initiated portal use. Portal initiation was 34.1% for whites, 23.4% for blacks, and 23.8% for Hispanics, and was lower for Medicaid (26.5%), Medicare (23.4%), and uninsured patients (17.4%) than commercially insured patients (39.3%). In multivariate analysis, both initiation of portal use (odds ratio [OR] = 1.24 per quintile, 95% confidence interval [CI], 1.23–1.24, P < .0001) and sending messages to providers (OR = 1.15, 95%CI, 1.09–1.14, P < .0001) were associated with neighborhood broadband internet access.
Conclusions: The majority of adults with outpatient visits to a large urban health care system did not use the patient portal, and initiation of use was lower for racial and ethnic minorities, persons of lower socioeconomic status, and those without neighborhood broadband internet access. These results suggest the emergence of a digital divide in patient portal use. Given the scale of investment in patient portals and other internet-dependent health information technologies, efforts are urgently needed to address this growing inequality.
Keywords: internet, health disparities, digital divide, personal health record, patient portals
BACKGROUND
The patient portal is an electronic system through which patients can interact with their health care system, health care providers, and/or their own health information. Also described as personal health records (PHRs), these technologies can be tethered (tied to the electronic health record [EHR]) or untethered.1 Patient portal features vary by vendor and by institution-specific design features, but typically include administrative (eg, appointment scheduling and bill payment) and clinical (eg, secure messaging, health monitoring, health information resources, and lab and other test reports) functions.1–4
Patient portals have shown potential for increasing the quality and efficiency of health care, but a digital divide in home internet access has the potential to severely limit the benefits of patient portal implementation.5–8 Federal Meaningful Use incentives introduced by the Health Information Technology for Economic and Clinical Health Act and additional policies, and programs stemming from the Affordable Care Act of 2009 have led to increased adoption and use of health information technology overall.9–11 Early research demonstrated largely positive results of this investment, and most provider organizations have received incentive payments for promoting and using PHRs.12,13 Less is known about adoption and use of patient portals among patients from vulnerable and disadvantaged backgrounds.4 Prior research has shown lower enrollment for racial and ethnic minorities.7,14–17 Still, patients from diverse backgrounds demonstrate consistent interest in using technology to improve their health and health care experiences.18,19 One prior study of insured patients found that the lack of home internet access affects the uptake of patient portal outreach efforts,14 and other work has found that internet access is as much as 50% lower for patients living with chronic illnesses.20 This lack of access influencing uptake can broaden the digital divide as technological advances continue to support health care processes, with potentially negative consequences for individuals, institutions, and public health.21
Although 87% of Americans now report using the internet, more than a third do not have broadband internet access at home.22 The Federal Communications Commission (FCC) defines broadband as “high-speed internet access that is always on and faster than traditional dial-up access” and can include digital subscriber line, cable modem, fiber, wireless, or satellite. Barriers to patient portal uptake and use, in particular if linked to low rates of broadband internet access, could severely constrain the value of patient portal technology and place public and safety-net care providers and already vulnerable patients at a severe disadvantage.
Differences in health literacy and technological literacy are also significantly associated with disparities in the use of patient portals across categories of use (registration, active use, e-mails, refill requests, etc.).16 Even among those with internet access, patients who have not mastered the use of a mouse and keyboard would certainly be less likely to use a patient portal. Non-adopters of patient portals also tend to have more limited access to a broad range of technology beyond computers and the internet (eg, iPad, smartphone, etc.).2 In order to better understand the possible emergence of systematic disparities in the use of patient portals, we examined differences in initiation and use according to sex, race/ethnicity, age, insurance status, and broadband internet access.
METHODS
This was a retrospective, observational study combining data from the EHR with data from government agencies. This study was approved by the MetroHealth System Institutional Review Board. EHR data were queried to collect demographic and clinical information on all adult patients (age ≥ 18 years) seen in the outpatient clinics of a single integrated public health care system from 2012 to 2015. The system includes a large tertiary-care hospital, a level-1 trauma center, and more than 17 primary care clinics located across Cuyahoga County, Ohio. The health care system uses the EpicCareTM EHR system and has achieved the Healthcare Information Management Systems Society Analytics Stage 7 Electronic Medical Record Adoption Model, the highest level of EHR adoption, in its hospital and all outpatient clinics. As a result, the study site is among the top 3% of health care systems in the nation for information technology implementation and use.
Usage logs from the tethered patient portal were queried to construct 2 primary outcome variables: (1) portal initiation, determined by whether patients logged into the patient portal, and (2) messaging. The messaging index is a composite indicator of patient portal messaging activity created from the subset of activities eligible to meet the “Use Secure Electronic Messaging” requirement of Stage 2 Meaningful Use, which include requesting an appointment, requesting a refill, sending a clinical message, requesting advice, or replying to a message.23 Usage logs are comprehensive, tracking all clicks and activities, and we further examined patterns of use according to patient characteristics.
Patient addresses were geocoded to census tracts from the 2010 US Census. Data from the FCC 2013 Form 477 were obtained on broadband internet use; these data are made available at the census-tract level.25 A 5-category ordinal variable (0–20%, 20–40%, 40–60%, 60–80%, 80–100%) was created from the FCC data to describe the level of household broadband connections within a neighborhood. Neighborhood median income (by census block group) and a composite neighborhood-level education variable (representing average years of education of persons in the block group) were obtained from the American Community Survey. Block group–level data on income and education were selected because prior studies indicated that this is an appropriate size geographic area for such measures, and our own inspection of the local data indicated considerable variation at the broader census-tract level.26 EHR problem list diagnoses were used to calculate the Charlson index of medical comorbidity for each patient.27
In the bivariate analysis (Figure 1 ), in order to understand the potential for broadband inequality to constrain patient portal use at a larger unit of geography than the census tract, a zip code–level variable was created. Because the FCC does not report broadband data at the zip code level, zip code tabulation areas (ZCTAs) were used to approximate zip codes; ZCTAs follow census block boundaries and therefore approximated zip codes for the areas in which patients in this study resided.28 While there are important limitations of zip codes and ZCTAs in spatial analysis of disease data,29 it has been noted that use of zip code–level data can often be useful.28 This larger geography is appropriate, because internet service providers routinely use zip codes when making internet infrastructure and marketing decisions, and zip code–level data have been the focus of prior research on broadband internet availability.30
Figure 1.
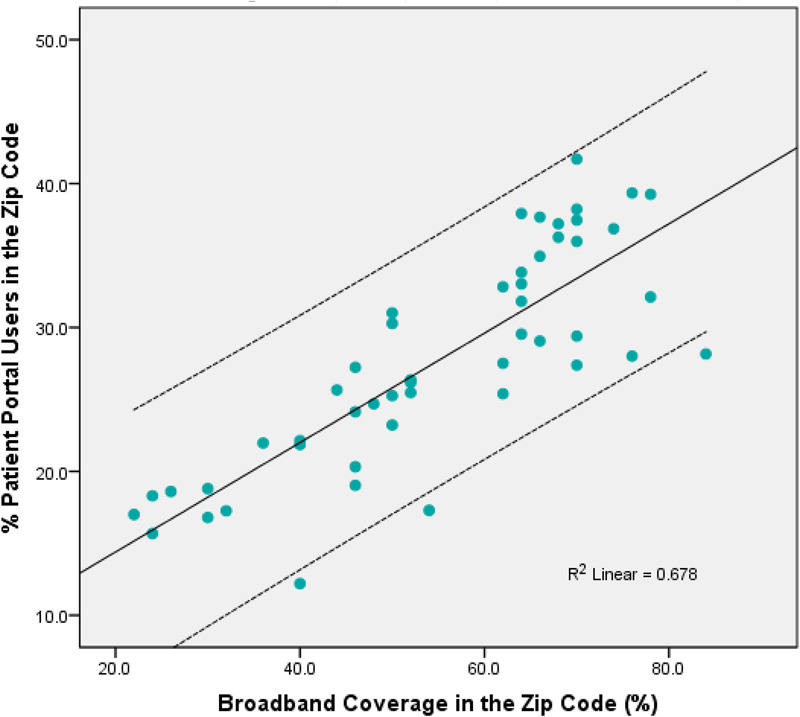
Patient portal use by broadband internet connection at the zip code (ZCTA) level (N = 243 248, ZCTAs = 50)
Analysis
Percentages were compared across groups to determine the extent of differences in patient portal use and specific portal activities. Bivariate correlation analysis was conducted to understand the covariation between broadband internet use and patient portal uptake. Multivariate mixed effects logistic regression modeling techniques were used to estimate Model 1, for all patients, the odds of using the patient portal, and Model 2, for patient portal users, the odds of sending a message to a provider. Sending a message to a provider can be viewed as a more advanced task that is less likely to be completed at the time of immediate PHR signup, and thus is an additional indicator of possible disparities in adoption and use of the patient portal.
Bootstrapped 95% bias-corrected confidence intervals were calculated for the model odds ratio estimates. Models included a random intercept in order to account for subject clustering within neighborhoods. We define α = 0.05 for our level of significance in all statistical tests. Missing data were handled using list-wise deletion. All statistical tests are 2-tailed. SAS version 9.2 was used for all analyses.31
RESULTS
Between 2012 and 2015, a total of 243 248 adult patients made at least 1 outpatient visit to the health system and were included; of these, 70 835 (29.1%) initiated use of the patient portal (defined by whether the patient or a proxy had logged in to the system at least once). During 2015, these users logged a total of 3 290 652 hits (clicks) throughout the patient portal system, for a total 51.9 hits per patient per year. The population was diverse by race/ethnicity: 52.4% white, 35.9% black, 5.4% Hispanic, 2.8% other, 3.6% unknown; and insurance status: 38.9% Medicaid, 15.6% Medicare, 33.2% commercial, 12.3% uninsured. Minority patients were less likely to begin using the patient portal, with uptake at 34.1% for whites, 23.4% for blacks, and 23.8% for Hispanics (P < .0001) (Table 1). Uptake was lower for Medicaid (26.5%), Medicare (23.4%), and uninsured patients (17.4%) than for commercially insured patients (39.3%) (P < .0001).
Table 1.
Population and patient portal user demographic characteristics
| Variable | All Patientsa | Portal Usersb | Portal Non-Users |
|---|---|---|---|
| N (%) | N (%) | N (%) | |
| Total Population | 243 249 (100) | 70 835 (29.1) | 172 413 (70.9) |
| Sex | |||
| Male | 103 142 (42.4) | 22 802 (32.2) | 80 340 (46.6) |
| Female | 140 106 (57.6) | 48 033 (67.8) | 92 073 (53.4) |
| Age | |||
| 18–64 | 207 417 (85.3) | 62 647 (88.4) | 144 769 (84.0) |
| 65–79 | 26 943 (11.1) | 6760 (9.5) | 20 183 (11.7) |
| ≥80 | 8889 (3.6) | 1428 (2.0) | 7461 (4.3) |
| Race | |||
| Black | 87 235 (35.9) | 20 394 (28.8) | 66 841 (38.8) |
| White | 127 471 (52.4) | 43 465 (61.4) | 84 006 (48.7) |
| Hispanic | 13 096 (5.5) | 3116 (4.4) | 9979 (5.8) |
| Other | 5965 (2.6) | 2023 (2.9) | 4744 (2.8) |
| Unknown | 8680 (3.6) | 1837 (2.6) | 6843 (4.0) |
| Primary Insurance | |||
| Medicaid | 94 566 (38.9) | 25 040 (35.3) | 69 526 (40.3) |
| Medicare | 37 916 (15.6) | 8865 (12.5) | 29 051 (16.8) |
| Commercial | 80 763 (33.2) | 31 706 (44.8) | 49 057 (28.5) |
| Uninsured | 30 004 (12.3) | 5224 (7.4) | 24 779 (14.4) |
| Incomec | $37 121 | $42 384 | $34 591 |
| Years of Educationc | 12.9 | 13.1 | 12.8 |
aWith 1 or more visits between January 1, 2012, and August 31, 2015.
bAt least 1 logon to the patient portal since January 1, 2012.
cBlock group median.
Among patient portal users, reading messages was the most common activity (86.0% overall), followed by viewing test results (81.5%) and requesting advice (39.4%) (Table 2). Differences in patient portal activity were similar to differences in patient portal initiation. By race and ethnicity, a higher percentage of white patients read messages, replied to messages, requested advice, and requested refills. However, a higher percentage of black patients scheduled appointments (Table 2). Notably, patient portal users age ≥ 80 (or their proxies) had high levels of requesting advice (43.4%) and viewing lab results (87.7%).
Table 2.
Frequency of patient portal activities by user characteristics (N = 63 387)a
| Variable | Request Appointment | View Lab Results | Request Refill | Request Advice | Read Message | Reply to Message |
|---|---|---|---|---|---|---|
| All Users | 22.6 | 81.5 | 18.7 | 39.4 | 86.0 | 28.9 |
| Sex | ||||||
| Male | 19.7 | 77.7 | 18.7 | 39.4 | 84.2 | 25.3 |
| Female | 23.9 | 83.3 | 18.7 | 40.7 | 86.9 | 30.5 |
| Age | ||||||
| 18–64 | 23.0 | 81.4 | 18.4 | 38.8 | 85.7 | 28.6 |
| 65–79 | 19.8 | 82.5 | 21.1 | 44.4 | 89.5 | 31.4 |
| ≥80 | 16.4 | 79.7 | 18.9 | 43.4 | 87.7 | 26.6 |
| Race | ||||||
| Black | 25.3 | 81.3 | 18.0 | 34.8 | 81.6 | 25.6 |
| White | 21.8 | 81.7 | 19.9 | 42.4 | 88.6 | 31.3 |
| Hispanic | 21.9 | 80.7 | 13.4 | 32.9 | 79.9 | 22.0 |
| Other | 16.6 | 82.5 | 11.5 | 30.8 | 82.9 | 20.9 |
| Primary Insurance | ||||||
| Medicaid | 24.3 | 80.7 | 17.3 | 33.8 | 81.8 | 24.5 |
| Medicare | 22.0 | 82.6 | 22.3 | 44.1 | 87.8 | 31.0 |
| Commercial | 22.0 | 82.7 | 19.2 | 43.3 | 89.0 | 32.4 |
| Uninsured | 18.5 | 75.4 | 15.0 | 30.6 | 82.8 | 21.4 |
aUse in a 1-year period (September 1, 2014, to August 31, 2015). All values represent percents.
Figure 1 displays the association between household broadband internet usage (at the zip code level) and patient portal initiation (first login). There is a strong linear association, with broadband internet usage explaining 68% (R2 = .68) of the variation in patient portal usage. As the percentage of home broadband internet connections in a census tract increases, so does the percentage of patients using the patient portal. In neighborhoods with 0–20% of residents having home broadband connections, just 17.5% used the patient portal, compared with 22.5% in the 20–40% connected neighborhoods, 29.8% in the 40–60% connected neighborhoods, 36.3% in the 60–80% connected neighborhoods, and 34.8% in the 80–100% connected neighborhoods.
Multivariate results describing the associations between patient characteristics, broadband internet usage, neighborhood socioeconomic status, and patient portal initiation and messaging outcomes are presented in Table 3. Older patients, male patients, blacks, Hispanics, those on Medicaid, and uninsured patients had substantially lower odds of ever initiating patient portal use (Table 3, Model 1) and ever messaging their providers via the patient portal (Table 3, Model 2). Home broadband internet was associated with both initiating patient portal use (OR = 1.10, 95% CI, 1.07–1.12, P < .0001) (Table 3, Model 1) and messaging providers (OR = 1.04, 95% CI, 1.01–1.07, P < .001) (Table 3, Model 2). In separate multivariate analyses adjusting for everything except income and education, an increase of a single quintile on the broadband internet usage measure was associated with 1.23 higher odds of using the patient portal (95% CI, 1.21–1.25, P < .0001) and 1.12 higher odds of messaging a provider (OR = 1.12, 95% CI, 1.09–1.14, P < .0001).
Table 3.
Results of mixed effects logistic regression models with random intercept
| Model 1: Personal Health Record First Sign-in (N = 204 882) |
Model 2: Sending a Message via the Personal Health Record (N = 60 723) |
|||
|---|---|---|---|---|
| Variable | Odds ratio (95% CI) | P-value | Odds ratio (95% CI) | P-value |
| Age | 0.99 (0.99–0.99) | <.0001 | 1.00 (1.00–1.00) | 0.1663 |
| Sex (female) | 1.75 (1.71–1.79) | <.0001 | 1.21 (1.17–1.25) | <.0001 |
| African Americana | 0.67 (0.65–0.69) | <.0001 | 0.83 (0.79–0.87) | <.0001 |
| Hispanica | 0.65 (0.62–0.68) | <.0001 | 0.79 (0.64–0.76) | <.0001 |
| Other Racea | 0.90 (0.84–0.96) | 0.0010 | 0.71 (0.65–0.80) | <.0001 |
| Unknown Racea | 0.69 (0.65–0.73) | <.0001 | 0.80 (0.72–0.89) | <.0001 |
| Medicaidb | 0.57 (0.55–0.58) | <.0001 | 0.70 (0.68–0.74) | 0.0034 |
| Medicareb | 0.37 (0.36–0.39) | <.0001 | 0.62 (0.59v0.67) | <.0001 |
| Uninsuredb | 0.45 (0.43–0.46) | <.0001 | 0.68 (0.63–0.72) | 0.0004 |
| Total Number of Visits | 1.05 (1.05–1.05) | <.0001 | 1.03 (1.03–1.03) | <.0001 |
| Charlson Comorbidity Index | 1.00 (0.99–1.01) | 0.6526 | 1.03 (1.01–1.04) | 0.0055 |
| Broadband Internet Access (tract) (per 20% increase) | 1.10 (1.07–1.12) | <.0001 | 1.04 (1.01–1.07) | 0.0050 |
| Years of Education (block group) | 1.10 (1.08–1.12) | <.0001 | 1.09 (1.07–1.12) | 0.0077 |
| Income (block group)c | 1.10 (1.07–1.14) | <.0001 | 1.00 (0.96–1.04) | 0.8641 |
| c-statistic = 0.726 | c-statistic = 0.639 | |||
aWhite is the reference category for race. bCommercial insurance is the reference category. cIncome scaling was normalized by dividing by the median.
DISCUSSION
We found that the majority of patients at an urban public health care system did not use the system’s patient portal. In addition, a major factor associated with accessing the patient portal was living in a neighborhood where most residents have access to home broadband internet. Elderly, underinsured, and minority patients were less likely to live in areas with a preponderance of home broadband internet or to access the patient portal. While prior studies have theorized a digital divide in the use of patient portals,14,21 this was largest, most diverse study to examine the association between broadband internet access and patient portal use, and the first to use a comprehensive dataset of usage logs combined with neighborhood data from public sources.
Federal efforts to improve health care through technology (including the Affordable Care Act and the Health Information Technology for Economic and Clinical Health Act) include patient portals and EHRs, telemonitoring, teleconferencing, and other strategies to use technology to improve patient education, engagement, and support while also working to address growing provider shortages.9,32–34 Highly reliable high-speed broadband access is required for these technologies to reach both providers and patients, with ideal bandwidths of at least 10 megabits per second, although a basic PHR could operate at lower speeds.32 Our findings indicate that 3 years after a patient portal rollout at a high-performing public health care system, an important disparity has appeared for persons without home broadband internet access. This evidence suggests that internet access disparities may constrain the projected benefits of patient portal use. Published analysis has estimated total PHR/patient portal benefits at greater than $21 billion annually.35 However, that analysis assumed that 80% of health care patients would have access 10 years after rollout.35 Given the results reported above, such beneficial levels of Meaningful Use36 will be extremely difficult if not impossible to achieve for health care organizations that serve communities with limited rates of home broadband internet usage. Providers who serve communities on the disconnected side of the digital divide face a steep barrier in their attempts to reach Meaningful Use thresholds and to break even on costly patient portal investments. In addition, there are potentially serious consequences for health outcomes and care engagement.
While there is a limited number of large, diverse, and rigorous studies on the efficacy of patient portals,12 preliminary evidence in some health conditions shows potential for positive clinical outcomes using patient portals as a part of disease management. For example, although a randomized controlled trial of hypertension found little evidence of patient portal benefit,37 a more general study found improvements in health care quality.5 Further studies have found evidence of clinical benefit in diabetes,6 anti-retroviral therapy for HIV-positive veterans,7 and preventive service use among persons with serious mental illness,3 as well as improvements in vaccination and preventive screenings.8 Therefore, in the context of growing evidence of patient portal benefits, the digital divide problem is even more concerning.
Individuals without internet access are systematically denied the benefits of patient portal use, including ease of scheduling appointments and ongoing interactions with care providers via the electronic system. Access to broadband internet has become a social determinant of health. The neighborhood-level measure in our study could be seen as a marker for the absence of any kind of home internet access. Researchers have long recognized the lack of access in rural communities, yet continue to underestimate the effects of access inequality that still exists in urban areas.32,38 Across locations, patients with chronic illnesses are less likely to have internet access, yet they utilize the internet more frequently to seek out health information when internet access is available.20,39 Recent data demonstrate that disparities in broadband access persist based on education level (95% for college, 66% for less than high school), household income (97% for incomes over $75K/year, 74% for incomes less than $30K/year), and age (96% of 18- to 29-year-olds, 58% of those age ≥ 65).38
The local context of internet connectedness in northeast Ohio is informative. According to the 2015 American Community Survey, for Cleveland households with incomes under $20 000/year (making up 38% of the city’s population), only 57% had home internet service through any source, mobile, dial-up, or broadband. A 2012 phone survey of 1261 Cleveland area residents found that for those making less than $20 000/year, only 57% had any access to the internet, 32% had broadband access, and just 10% had smartphone internet access.40,41 Among those using the internet, the most frequent category of use was health information (64% of those surveyed).41
Recent policy shifts have identified mechanisms through which large segments of disconnected patients could gain internet access. This includes the FCC’s movement toward a policy change that would allow consumers to divert the “Lifeline” subsidy to pay for internet access,24 service provider offerings such as AT&T’s agreement to provide $10 per month internet access to eligible low-income households in 21 states until 2020 (https://www.att.com/shop/internet/access/#/), and the Comcast Internet Essentials program (https://www.internetessentials.com/). Such efforts are emblematic of the changes needed to combat the growing digital divide in patient portal use. Research has suggested that a lack of market competition is another important factor in the affordability of broadband internet in some racial ethnic minority communities, and further policy efforts to increase quality and competition may be necessary.42
The multivariate provider messaging results presented in Table 3 have further importance in demonstrating that even after initial patient portal login, patients from disadvantaged backgrounds and communities face a persistent challenge in receiving value from the patient portal. Other researchers have suggested that differences in patients’ digital and computer literacy are behind the disparity.14,43 Expanding community-based training programs, designing technologies accessible to a wide range of users, and educating patients on how to use health information technology at health clinics are possible mechanisms that could combat emerging disparities.13,44,45
The rise in smartphone use might seem to eliminate some of the challenges presented by limits to home and neighborhood broadband access, yet recent data demonstrate that 15% of smartphone owners have no access to the internet other than their data plan.46 Low-income, low-education, and non-white individuals are more likely to be smartphone dependent and more likely to reach their plan’s data cap and have their phone cut off due to financial challenges.46 In a supplemental analysis, we further examined the patient portal logs from 63 387 users in the most recent 12 months of data from the study, and just 6223 (10.2%) had used a mobile device to access the patient portal, suggesting that smartphones are not meaningfully bridging the observed digital divide. These preliminary findings on mobile patient portal usage suggest the need for further analysis to examine barriers to, facilitators of, and potential disparities in the use of patient portals on mobile phones.
Limitations
Our study has some important limitations. First, we analyzed data from a single urban public health care system in northeast Ohio. Therefore, our findings have limited generalizability, especially to rural areas and smaller communities. Second, the FCC measure of broadband internet was available only at the neighborhood (census tract) level and is only as accurate as the data reported to the FCC by internet service providers. We were thus unable to determine internet usage at the individual patient level. Neighborhoods with higher levels of internet access tend to be of higher socioeconomic status, and likely have other important resources and facilitators of patient portal use. Third, the data for this study come from a health care system that has reached Healthcare Information Management Systems Society Stage 7 and therefore has a robust informatics infrastructure. The experience of provider organizations with less advanced technology resources is likely to be different in important ways. Fourth, we did not examine patterns of use for children or patterns of proxy usage. Fifth, there are a number of variables not measured in this study that could have a powerful influence on whether someone uses the patient portal. These include individual concerns about privacy, basic computer and digital literacy skills, and patient preferences for in-person support from providers.47–49 Such preferences might be mediators between internet access, measured at the neighborhood level, and patient portal use. We did not model the frequency of patient portal use, and examination of frequency of use could reveal additional disparities. Lastly, at the time of this analysis, the patient portal was not available in Spanish or other languages. Participants with preferred languages other than English are even less likely to use patient portals, and our electronic record system does not include an accurate measure of English proficiency.50
CONCLUSIONS
Our study found that for patients at one urban hospital system, differences in home broadband internet access demonstrate a clear negative association with patient portal initiation and use. Overall, patient portal initiation was modest and activity was systematically lower for blacks, Hispanics, older adults, and persons of low socioeconomic status (Medicaid and uninsured). Additional research is needed to examine the extent to which internet access constraints affect patients’ ability to access and utilize health services. The potential of new health information technologies like the patient portal to improve health is hampered by structural disadvantages, and internet access has emerged as an important social determinant of health. Policy changes and reforms are necessary to combat this emerging inequality.
References
- 1. Kaelber DC, Jha AK, Johnston D, Middleton B, Bates DW. A research agenda for personal health records (PHRs). J Am Med Inform Assoc. 2008;156:729–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Emani S, Yamin CK, Peters E et al. Patient perceptions of a personal health record: a test of the diffusion of innovation model. J Med Internet Res. 2012;146:e150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Druss BG, Ji X, Glick G, Silke A. Randomized trial of an electronic personal health record for patients with serious mental illnesses. Am J Psychiatry. 2014;1714:360–68. [DOI] [PubMed] [Google Scholar]
- 4. Archer N, Fevrier-Thomas U, Lokker C, McKibbon KA, Straus S. Personal health records: a scoping review. J Am Med Inform Assoc. 2011;184:515–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhou YY, Kanter MH, Wang JJ, Garrido T. Improved quality at Kaiser Permanente through e-mail between physicians and patients. Health Affairs. 2010;297:1370–75. [DOI] [PubMed] [Google Scholar]
- 6. Lau M, Campbell H, Tang T, Thompson DJ, Elliott T. Impact of patient use of an online patient portal on diabetes outcomes. Can J Diab. 2014;381:17–21. [DOI] [PubMed] [Google Scholar]
- 7. McInnes DK, Shimada SL, Rao SR et al. Personal health record use and its association with antiretroviral adherence: survey and medical record data from 1871 US veterans infected with HIV. AIDS Behav. 2013;179:3091–100. [DOI] [PubMed] [Google Scholar]
- 8. Wright A, Poon EG, Wald J et al. Randomized controlled trial of health maintenance reminders provided directly to patients through an electronic PHR. J General Int Med. 2012;271:85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pearson TL. Telehealth: aiding navigation through the perfect storm of diabetes care in the era of health care reform. Diabetes Spectrum. 2013;264:221–25. [Google Scholar]
- 10. Blumenthal D. Launching HIteCH. New Engl J Med. 2010;3625:382–85. [DOI] [PubMed] [Google Scholar]
- 11. Stark P. Congressional intent for the HITECH Act. Am J Managed Care. 2010;16(12 Suppl HIT):SP24–28. [PubMed] [Google Scholar]
- 12. Buntin MB, Burke MF, Hoaglin MC, Blumenthal D. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Affairs. 2011;303:464–71. [DOI] [PubMed] [Google Scholar]
- 13. Lyles C, Schillinger D, Sarkar U. Connecting the dots: health information technology expansion and health disparities. PLoS Med. 2015;127:e1001852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Roblin DW, Houston TK, Allison JJ, Joski PJ, Becker ER. Disparities in use of a personal health record in a managed care organization. J Am Med Inform Assoc. 2009;165:683–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Goel MS, Brown TL, Williams A, Hasnain-Wynia R, Thompson JA, Baker DW. Disparities in enrollment and use of an electronic patient portal. J General Int Med. 2011;2610:1112–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sarkar U, Karter AJ, Liu JY et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc. 2011;183:318–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McInnes DK, Solomon JL, Shimada SL et al. Development and evaluation of an internet and personal health record training program for low-income patients with HIV or hepatitis C. Med Care. 2013;51:S62–66. [DOI] [PubMed] [Google Scholar]
- 18. Schickedanz A, Huang D, Lopez A et al. Access, interest, and attitudes toward electronic communication for health care among patients in the medical safety net. J General Int Med. 2013;287:914–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dhanireddy S, Walker J, Reisch L, Oster N, Delbanco T, Elmore JG. The urban underserved: attitudes towards gaining full access to electronic medical records. Health Expect. 2014;175:724–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fox S, Purcell K. Chronic Disease and the Internet. Washington, DC: Pew Internet & American Life Project; 2010. [Google Scholar]
- 21. Yamin CK, Emani S, Williams DH et al. The digital divide in adoption and use of a personal health record. Arch Int Med. 2011;1716:568–74. [DOI] [PubMed] [Google Scholar]
- 22. Horrigan JB, Duggan M. Home Broadband 2015. Washington, DC: Pew Research Center; 2015. http://www.pewinternet.org/2015/12/22/2015/Home-Broadband-2015/. Accessed December 2016. [Google Scholar]
- 23. Centers for Medicare & Medicaid Services. Stage 2 Eligible Professional Meaningful Use Core Measures Measure 17. Baltimore, MD; 2012. [Google Scholar]
- 24. Federal Communications Commission Lifeline and Link Up Reform and Modernization. FCC15–71. 2015. https://apps.fcc.gov/edocs_public/attachmatch/FCC-15-71A1_Rcd.pdf. Accessed December 2016. [Google Scholar]
- 25. Federal Communications Commission Form 477 Census Tract Data on Internet Access Services. 2013. https://www.fcc.gov/general/broadband-deployment-data-fcc-form-477. Accessed December 2016. [Google Scholar]
- 26. Krieger N, Chen JT, Waterman PD, Soobader M-J, Subramanian S, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: The Public Health Disparities Geocoding Project (US). J Epidemiol Commun Health. 2003;573:186–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. D’Hoore W, Bouckaert A, Tilquin C. Practical considerations on the use of the Charlson comorbidity index with administrative data bases. J Clin Epidemiol. 1996;4912:1429–33. [DOI] [PubMed] [Google Scholar]
- 28. Grubesic TH. Zip codes and spatial analysis: problems and prospects. Socio-Econ Planning Sci. 2008;422:129–49. [Google Scholar]
- 29. Grubesic TH, Matisziw TC. On the use of ZIP codes and ZIP code tabulation areas (ZCTAs) for the spatial analysis of epidemiological data. Int J Health Geographics. 2006;51:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Grubesic TH. A spatial taxonomy of broadband regions in the United States. Inform Econ Policy. 2006;184:423–48. [Google Scholar]
- 31. Institute S. SAS/STAT 9.2 User’s Guide. Cary, NC: SAS Institute; 2008. [Google Scholar]
- 32. Steele R, Lo A. Telehealth and ubiquitous computing for bandwidth-constrained rural and remote areas. Personal Ubiquitous Comput. 2013;173:533–43. [Google Scholar]
- 33. Kvedar J, Coye MJ, Everett W. Connected health: a review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Affairs. 2014;332:194–99. [DOI] [PubMed] [Google Scholar]
- 34. Cebul RD, Love TE, Jain AK, Hebert CJ. Electronic health records and quality of diabetes care. New Engl J Med. 2011;3659:825–33. [DOI] [PubMed] [Google Scholar]
- 35. Kaelber D, Pan EC. The value of personal health record (PHR) systems. AMIA Annual Symposium Proceedings. American Medical Informatics Association; 2008;(2008):343–47. [PMC free article] [PubMed] [Google Scholar]
- 36. Kannry J, Beuria P, Wang E, Nissim J. Personal health records: meaningful use, but for whom? Mount Sinai J Med. 2012;795:593–602. [DOI] [PubMed] [Google Scholar]
- 37. Wagner PJ, Dias J, Howard S et al. Personal health records and hypertension control: a randomized trial. J Am Med Inform Assoc. 2012;194:626–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Perrin A, Duggan M. Americans’ Internet Access: 2000–2015. Pew Research Center; 2015:26 http://www.pewinternet.org/2015/06/26/americans-internet-access-2000-2015/. Accessed December 2016. [Google Scholar]
- 39. Zickuhr K, Smith A. Digital Differences: Pew Internet and American Life Project. 2012. http://pewinternet. org/Reports/2012/Digital-differences.aspx. Accessed February 2014. [Google Scholar]
- 40. Smith A. US Smartphone Use in 2015. Pew Research Center; 2015:1 http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/. Accessed December 2016. [Google Scholar]
- 41. Tolbert C, Mossberger K. Executive Summary: Cuyahoga County Survey of Internet Access and Use. 2013. http://connectyourcommunity.org/wp-content/uploads/2015/11/Cuyahoga-County-Survey-of-Internet-Access-and-Use.pdf. Accessed December 2016. [Google Scholar]
- 42. Prieger JE, Hu W-M. The broadband digital divide and the nexus of race, competition, and quality. Inform Econ Policy. 2008;202:150–67. [Google Scholar]
- 43. Miller DP Jr, Latulipe C, Melius KA, Quandt SA, Arcury TA. Primary care providers’ views of patient portals: interview study of perceived benefits and consequences. J Med Internet Res. 2016;181: e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Jacobs G, Castek J, Pizzolato D, Pendell KD, Withers E, Reder S. Community Connections: Digital Literacy Acquisition Policy Brief. 2015. http://archives.pdx.edu/ds/psu/16518. Accessed December 2016. [Google Scholar]
- 45. Harris K, Castek J, Jacobs G, Hill L, Pizzolato D. Community Digital Inclusion Partnerships with Healthcare Providers. Net Inclusion 2016: The National Digital Inclusion Summit. Kansas City, MO; 2016. [Google Scholar]
- 46. Smith A, Page D. US Smartphone Use in 2015. Washington, DC: Pew Internet & American Life Project; 2015. [Google Scholar]
- 47. Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;132:121–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lyles CR, Allen JY, Poole D, Tieu L, Kanter MH, Garrido T. “I Want to Keep the Personal Relationship With My Doctor”: understanding barriers to portal use among African Americans and Latinos. J Med Internet Res. 2016;1810:e263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Tieu L, Schillinger D, Sarkar U et al. Online patient websites for electronic health record access among vulnerable populations: portals to nowhere? J Am Med Inform Assoc. 2016;0:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ancker JS, Barrón Y, Rockoff ML et al. Use of an electronic patient portal among disadvantaged populations. J General Int Med. 2011;2610:1117–23. [DOI] [PMC free article] [PubMed] [Google Scholar]


