Abstract
Background
Cup malposition is a common cause of impingement, limitation of ROM, acceleration of bearing wear, liner fracture, and instability in THA. Previous studies of the safe zone based on plain radiographs have limitations inherent to measuring angles from two-dimensional projections. The current study uses CT to measure component position in stable and unstable hips to assess the presence of a safe zone for cup position in THA.
Questions/purposes
(1) Does acetabular component orientation, when measured on CT, differ in stable components and those revised for recurrent instability? (2) Do CT data support historic safe zone definitions for component orientation in THA?
Methods
We identified 34 hips that had undergone revision of the acetabulum for recurrent instability that also had a CT scan of the pelvis between August 2003 and February 2017. We also identified 175 patients with stable hip replacements who also had a CT study for preoperative planning and intraoperative navigation of the contralateral side. For each CT study, one observer analyzed major factors including acetabular orientation, femoral anteversion, combined anteversion (the sum of femoral and anatomic anteversion), pelvic tilt, total offset difference, head diameter, age, sex, and body mass index. These measures were then compared among stable hips, hips with cup revision for anterior instability, and hips with cup revision for posterior instability. We used a clinically relevant measurement of operative anteversion and inclination as opposed to the historic use of radiographic anteversion and inclination. The percentage of unstable hips in the historic Lewinnek safe zone was calculated, and a new safe zone was proposed based on an area with no unstable hips.
Results
Anteriorly unstable hips compared with stable hips had higher operative anteversion of the cup (44° ± 12° versus 31° ± 11°, respectively; mean difference, 13°; 95% confidence interval [CI], 5°-21°; p = 0.003), tilt-adjusted operative anteversion of the cup (40° ± 6° versus 26° ± 10°, respectively; mean difference, 14°; 95% CI, 10°-18°; p < 0.001), and combined tilt-adjusted anteversion of the cup (64° ± 10° versus 54° ± 19°, respectively; mean difference, 10°; 95% CI, 1°-19°; p = 0.028). Posteriorly unstable hips compared with stable hips had lower operative anteversion of the cup (19° ± 15° versus 31° ± 11°, respectively; mean difference, -12°; 95% CI, -5° to -18°; p = 0.001), tilt-adjusted operative anteversion of the cup (19° ± 13° versus 26° ± 10°, respectively; mean difference, -8°; 95% CI, -14° to -2°; p = 0.014), pelvic tilt (0° ± 6° versus 4° ± 6°, respectively; mean difference, -4°; 95% CI, -7° to -1°; p = 0.007), and anatomic cup anteversion (25° ± 18° versus 34° ± 12°, respectively; mean difference, -9°; 95% CI, -1° to -17°; p = 0.033). Thirty-two percent of the unstable hips were located in the Lewinnek safe zone (11 of 34; 10 posterior dislocations, one anterior dislocation). In addition, a safe zone with no unstable hips was identified within 43° ± 12° of operative inclination and 31° ± 8° of tilt-adjusted operative anteversion.
Conclusions
The current study supports the notion of a safe zone for acetabular component orientation based on CT. However, the results demonstrate that the historic Lewinnek safe zone is not a reliable predictor of future stability. Analysis of tilt-adjusted operative anteversion and operative inclination demonstrates a new safe zone where no hips were revised for recurrent instability that is narrower for tilt-adjusted operative anteversion than for operative inclination. Tilt-adjusted operative anteversion is significantly different between stable and unstable hips, and surgeons should therefore prioritize assessment of preoperative pelvic tilt and accurate placement in operative anteversion. With improvements in patient-specific cup orientation goals and acetabular component placement, further refinement of a safe zone with CT data may reduce the incidence of cup malposition and its associated complications.
Level of Evidence:
Level III, diagnostic study.
Introduction
Acetabular cup malposition represents a common cause of complications after THA [13], contributing to impingement, limitation of ROM, acceleration of bearing wear, and liner fracture [7, 14, 25]. In addition, malposition of the acetabular component is a prime cause of [13] hip instability, which is the most common cause for revision in the United States [25]. The first concept of a safe zone for acetabular component orientation, 40° ± 10° of inclination and 15° ± 10° of anteversion, introduced by Lewinnek et al. [15] in 1978 as well as various safe zones on plain radiographs [5, 6, 9, 15, 19], have been commonly referenced in clinical practice or studies. However, several investigators [8, 11, 31, 35] have questioned whether the historic concept of a safe zone is clinically useful. Historic safe zones also do not take into account individual patient morphology that may alter component-positioning goals such as variation in pelvic tilt, which has been shown to directly alter the functional orientation of the acetabular component [17].
Measurement of cup position in clinical practice typically is performed using plain radiographs. Inclination, or abduction, can easily be measured on plain radiographs, but anteversion is more difficult. Several factors are responsible, including difficulty identifying retroversion, the need for complicated calculations or conversion tables, and the wide variability of the patient’s pelvic orientation when radiographs are taken. In addition, accuracy of radiographic measurements can be affected by magnification and the deviation or unknown location of the central x-ray beam in relation to the cup. Finally, three different definitions [23] (operative, radiographic, and anatomic) and two reference planes (anterior pelvic plane [3] [APP] and functional coronal plane [19]) have been used to measure and report position of the acetabular component. As a result of limitations inherent to analysis of plain radiographs, CT scans and three-dimensional reconstructions have increasingly been used as imaging techniques to measure the true value of acetabular component orientation [24, 37] or to validate the radiographic methods using CT as the reference standard [24].
We therefore sought to determine: (1) Does acetabular component orientation, when measured on CT, differ in stable components and those revised for recurrent instability? (2) Do CT data support historic safe zone definitions for component orientation in THA?
Patients and Methods
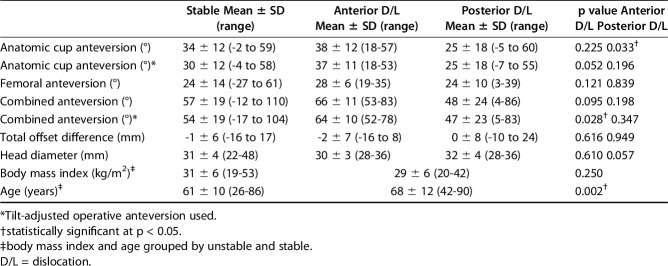
We identified 34 hips in 34 patients who had a CT study before undergoing revision of the acetabulum for recurrent instability. These cases represent every hip that we could identify by operating room and imaging logs at the New England Baptist Hospital that was treated by cup revision for recurrent instability between August 2003 and February 2017 and that had a CT study that allowed measurement of component position. Fifty-three percent (18) of the 34 hips in this group were in female patients, and the mean age at the time of revision was 68 ± 12 years (range, 42–90 years). There were 12 anterior and 22 posterior dislocations. We also identified a control group of 175 randomly chosen patients who had a stable hip replacement who presented for treatment by the senior author (SBM) and who had a CT study for preoperative planning and intraoperative navigation of the contralateral side during the period from 2003 to 2016 [12, 27]. In this group, 58% (101) of the hips were in female patients, and the mean age at the time of surgery was 61 ± 10 years (range, 26–86 years). Mean body mass index was 29 ± 6 kg/m2 (range, 20–42 kg/m2) in the unstable group and 31 ± 6 kg/m2 (range, 19–53 kg/m2) in the stable group. Hips with lipped liners were excluded because of difficulty in measuring the angle of the liner [2]. There were no differences in sex (p = 0.747) or body mass index (p = 0.250) between the stable and unstable groups. Patients with recurrent instability were on average 7 years older than those with stable hips (95% confidence interval [CI], 3–12; p = 0.002) (Table 1). The protocol was approved by the New England Baptist Hospital institutional review board.
Table 1.
Measurements of other variables in between the stable and unstable groups
The CT studies were performed using a spiral 32-slice CT scanner (Optima 660 or Lightspeed 32; General Electric, Boston, MA, USA) with the patient in the supine position. Scans were acquired in the supine position in a matrix of 512 x 512 with a display field of view of 36 auto mA used with a minimal value set at 100, maximum 560, kV 120. The protocol includes scans of the region from the level of the fourth lumbar vertebra proximally through the proximal femur with images through the distal femoral condyles. For each CT study, acetabular component orientation, pelvic tilt, and femoral anteversion were calculated using validated software [10] (HipXpert; Surgical Planning Associates, Boston, MA, USA), whereas total offset difference and head diameter were measured using an open DICOM viewer (OsiriX Lite, www.osirix-viewer.com).
To calculate cup orientation, a three-dimensional (3-D) model of the pelvis was created using the data and the APP coordinate system landmarks were identified (Fig. 1). The APP [33] is defined by three reference points: the two anterosuperior iliac spines and the anterior surface of the pubic symphysis. Next, using multiplanar views, points on the acetabular rim were identified to calculate a vector orthogonal to the open plane of the acetabulum (Fig. 2). The 3-D orientation of the cup opening plane in the APP coordinate space was calculated using the operative anteversion and inclination angles defined by Murray [23] (Fig. 3). In addition, supine pelvic tilt was calculated by measuring the angle between the APP coordinate system and the CT coordinate system. Pelvic tilt was positive if the anterosuperior iliac spines were anterior to the pubic symphysis and negative if the anterosuperior iliac spines were posterior to the pubic symphysis (Fig. 4). Tilt-adjusted operative anteversion was calculated as operative anteversion minus pelvic tilt. One observer measured all cases (SBM).
Fig. 1 A-B.
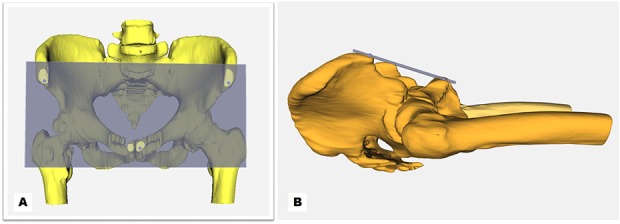
A 3-D CT model of the pelvis showing the anterior pelvic reference plane for measuring the position of the acetabular component: (A) frontal image; (B) lateral image.
Fig. 2 A-D.
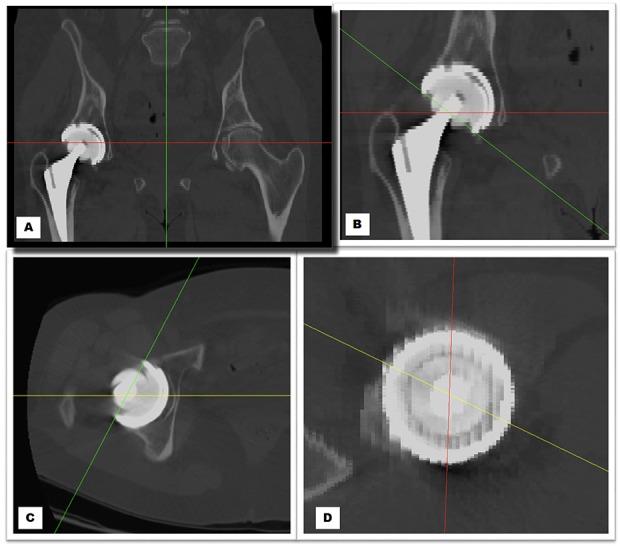
CT images demonstrating the method for measuring cup orientation on multiplanar views: (A) both hip images; (B) coronal image of the right hip; (C) sagittal image of the right hip; (D) axial image of the right hip.
Fig. 3.
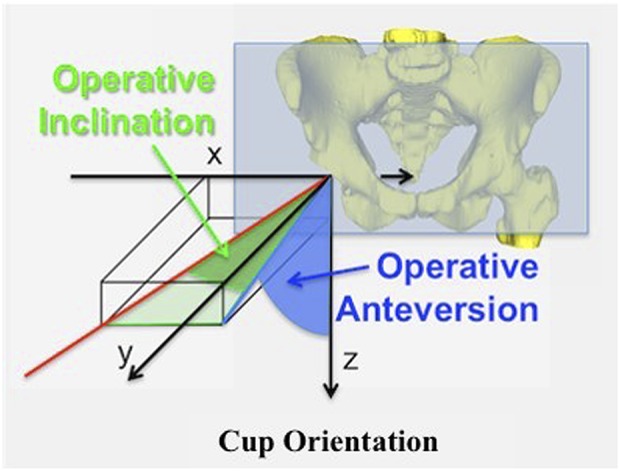
This figure depicts the 3-D orientation of the cup plane using the operative inclination and anteversion angles defined by Murray [23].
Fig. 4.
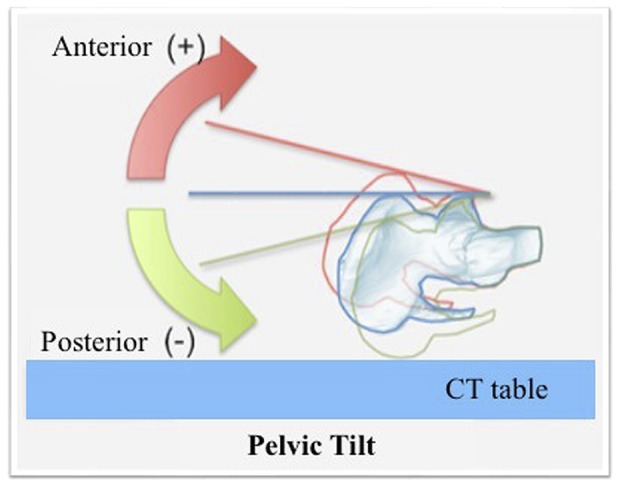
A snapshot image depicting AP supine pelvic tilt on CT.
Femoral anteversion was assessed by the technique described by Sugano et al. [21, 28]. Because operative anteversion is calculated in the sagittal plane, the cup orientation values were converted to anatomic anteversion, which is measured in the transverse plane, so that anatomic acetabular anteversion [23] and femoral anteversion could be added to calculate combined anteversion. With respect to offset, comparing just the femoral side would not be helpful because it does not account for medialization of the socket. Therefore, we compared total offset differences between the stable and unstable groups, measured from the medial border of the teardrop to the tip of the greater trochanter, on both sides using the modified technique described by Loughead et al. [16].
To determine the validity of an historic safe zone, we selected the historic “safe zone” of Lewinnek et al. because that study introduced the concept of a safe zone and is the most commonly referenced safe zone. To do this, we converted our cup orientations in the operative definition to cup orientation in the radiographic definition [23] used by Lewinnek et al. We then plotted the recurrently unstable hips in our study against the Lewinnek safe zone and calculated the percent of hips within that safe zone.
For descriptive analysis, mean values and differences were expressed in degrees and SDs. The distributions of variables with n < 30 were tested for normality using the Shapiro-Wilk test. If a variable met the criteria for normal distribution, differences in values between them were analyzed with use of a two-tailed independent t-test. Otherwise, we used the nonparametric Mann-Whitney U test. Results with p values of < 0.05 were considered significant. All statistical analyses were performed with XLSTAT® statistical software (Release 19.02; Addinsoft, New York, NY, USA).
Results
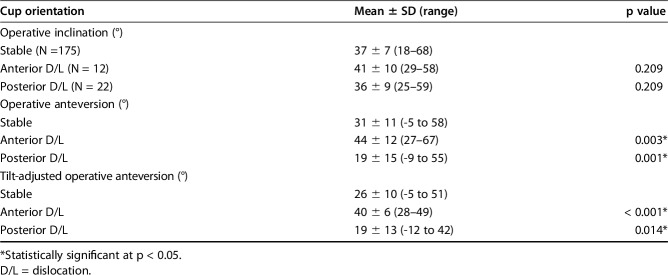
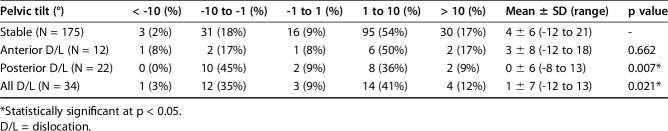
We found substantial differences in anteversion and tilt-adjusted anteversion between stable hips and both posteriorly and anteriorly dislocating recurrently unstable hips. Anteriorly unstable hips compared with stable hips had higher operative anteversion of the cup (44° ± 12° versus 31° ± 11°, respectively; mean difference, 13°; 95% CI, 5°-21°; p = 0.003) and tilt-adjusted operative anteversion of the cup (40° ± 6° versus 26° ± 10°, respectively; mean difference, 14°; 95% CI, 10°-18°; p < 0.001). Posteriorly unstable hips compared with stable hips had lower operative anteversion of the cup (19° ± 15° versus 31° ± 11°, respectively; mean difference, -12°; 95% CI, -5° to -18°; p = 0.001) and tilt-adjusted operative anteversion of the cup (19° ± 13° versus 26° ± 10°, respectively; mean difference, -8°; 95% CI, -14° to -2°; p = 0.014) (Table 2). There was no difference in operative inclination among stable, posteriorly dislocating, and anteriorly dislocating hips. A wide range of supine pelvic tilt was observed in both the stable and unstable groups, and pelvic tilt was lower in posteriorly dislocating unstable hips than in stable hips (0° ± 6° versus 4° ± 6°, respectively; mean difference, -4°; 95% CI, -7° to -1°; p = 0.007) (Table 3). Combined anteversion of the femur and acetabulum was higher in anteriorly unstable hips than stable hips (64° ± 10° versus 54° ± 19°, respectively; mean difference, 10°; 95% CI, 1°-19°; p = 0.028). No difference was found between stable hips and anteriorly dislocating hips in pelvic tilt. No difference was found between stable and posterior or anteriorly dislocating hips in femoral anteversion (Tables 1, 2).
Table 2.
Measurement of cup orientation between the stable and unstable groups
Table 3.
The distribution of supine pelvic tilt values
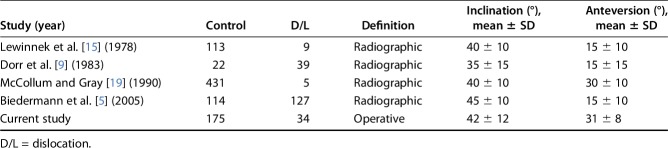
We found no evidence from CT data to support the Lewinnek safe zone but were able to identify a revised safe zone using operative definitions. Eleven of 34 (32%) recurrently unstable hips were located within the Lewinnek safe zone of 40° ± 10° of radiographic inclination and 15° ± 10° of radiographic anteversion, representing 10 of 22 (45%) posteriorly dislocating hips and one of 12 (8%) anteriorly dislocating hips (Fig. 5). In our study, all cups revised for recurrent instability had < 31° or > 56° of operative inclination or < 23° or > 39° of tilt-adjusted operative anteversion. Further analysis revealed a zone in which no dislocation had occurred (Fig. 6). Based on the positions of the hips that dislocated, a safe zone was determined to be 43° ± 12° of operative inclination and 31° ± 8° of tilt-adjusted operative anteversion where no hip was revised on the acetabular side for recurrent instability.
Fig. 5.
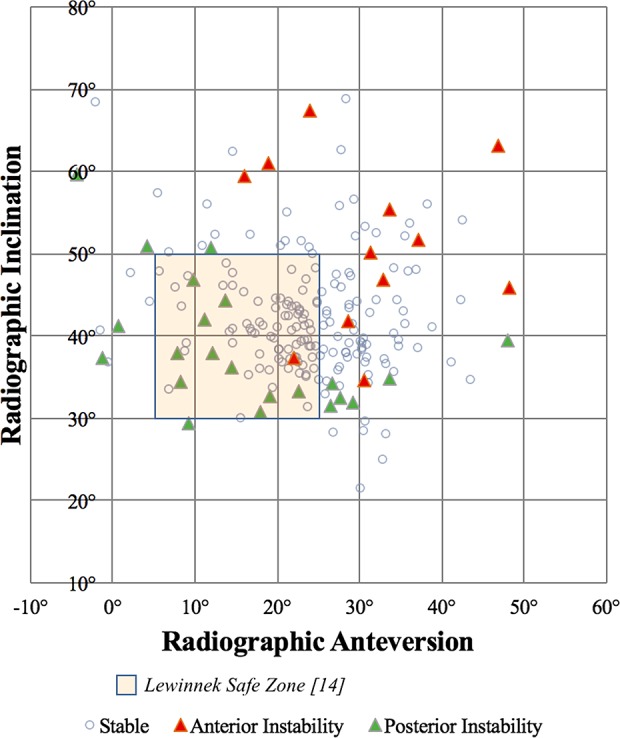
A scatterplot depicting cup position in the radiographic definition and the Lewinnek safe zone boundary.
Fig. 6.
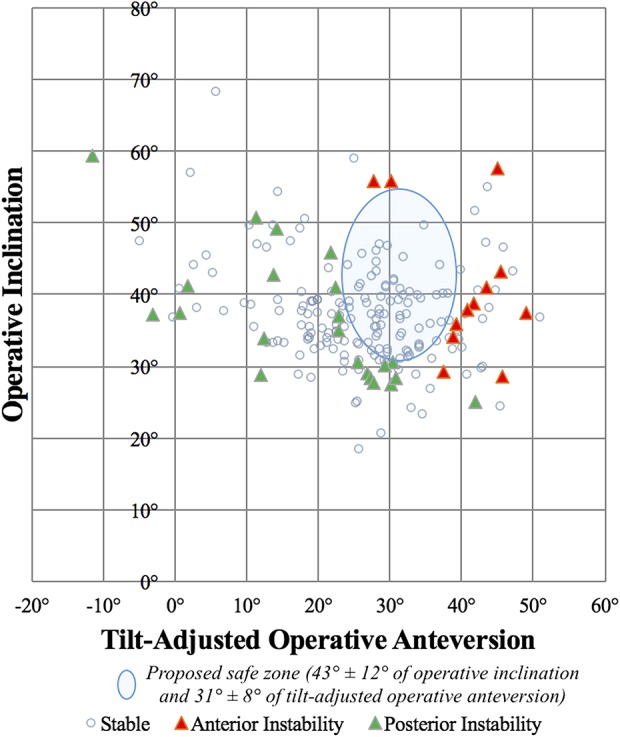
A scatterplot depicting cup position in the operative definition (tilt-adjusted) and the proposed safe zone of the current study.
Discussion
Defining a reliable safe zone of acetabular component positioning remains one of the major goals of THA research, because acetabular component malpositioning is a prime contributor to hip instability, the most common cause of revisions in the United States [25]. Many studies have used radiographic [6, 9, 13, 15, 19] and simulation [4, 26, 34, 36] techniques to assess the relationship between component orientation and joint stability. However, these studies that are based on radiographs are limited by issues of accuracy resulting from multiple unknown parameters of the pelvis image and have not taken into account femoral anteversion or combined anteversion [6, 9, 15, 19, 24, 29, 30]. In the current study, CT eliminates the inaccuracy of radiographic measurement and allows for direct measurement of acetabular component position, pelvic tilt in the supine position, and femoral anteversion. The current study identifies a new safe zone and shows that cup anteversion is a critical parameter. The study also demonstrates that the Lewinnek zone is not safe.
The current study is limited in several ways. It is a retrospective study, and CT studies of cups revised for recurrent instability are rare, naturally leading to smaller numbers for analysis. Larger numbers, especially in anterior dislocating hips, could lead to a better understanding of additional variables. Additionally, it would be of interest to better separate the groups by age, sex, body mass index, and surgical exposure of the index procedure and with a more in-depth understanding of spinopelvic attitude and flexibility. The mean age of the recurrently unstable group (68 years) and the stable group (61 years) limits the ability to stratify results by age or extrapolate to younger patients. The patients in this study came from a referral hospital in New England that does not represent the demographics of the United States at large, limiting extrapolation to other patient populations, and so care should be taken before applying these study results to the care of different patient populations. Because no information is known about why the study participants received CT scans, it is possible that these patients differ from the revision population as a whole if clinicians are more likely to order a CT scan when suspecting misplaced components. No data are available on the approaches of the original procedure or other confounding factors such as spine pathology beyond the static spine-pelvis measurement of pelvic tilt in the supine position. Despite these limitations, we believe that it is unlikely that these cases represented “out of the ordinary” revisions because prerevision CT studies for objective assessment of component position are generally becoming more common in clinical practice at our institution.
In our study population, the use of operative definition measures allowed for the identification of a clinically relevant safe zone with no dislocations. In common with other studies, we found little clinical relevance of the Lewinnek safe zone when compared with our CT data, because approximately one-third of the dislocations were within the Lewinnek safe zone [1, 8]. In addition, our data show a wider range of anteversion than inclination in both the study and control groups, indicating that surgeons may be more accurate in inclination than anteversion.
Our current study measured cup positions in operative definitions both because these are the common definitions used for surgical navigation systems and because operative anteversion is measured in the flexion/extension plane, the same plane in which pelvic tilt is measured (Fig. 4). In practice, cup orientation can be easily mathematically converted from one definition to another as desired. We incorporated pelvic tilt, which affects the relationship of the anterior pelvic plane to the functional coronal plane by up to 20° or more in some patients [3, 24, 38]. These measurements were in keeping with other recent studies [17, 20, 33] and have further highlighted the importance of the functional orientation of the acetabular component. We observed substantial individual variability of pelvic tilt in our study (Table 3) and consequently reported tilt-adjusted anteversion in the safe zone in this study to incorporate pelvic tilt as a patient-specific variable in cup positioning. Although we did not note significant change in pelvic tilt as a result of THA in a prior study [22], the spine-pelvic relationship is dynamic and can potentially change over time, so it is important to remember that measurement of pelvic tilt in the supine, sitting, standing, or crouched position is just a single measurement in an arc of motion at a single point in time. Our study confirmed that there are differences between the placement of stable and unstable cups as measured by CT and reported the data in the clinically useful operative definition [3].
Recently several authors have proposed redefining a safe zone for THA. Abdel et al. [1] and Timperley et al. [32] suggested that there is no safe zone for acetabular component positioning based on plain radiographic assessment. Tiberi et al. [31] suggested that the functional acetabular component safe zone may need to be individualized because substantial changes in cup orientation occur in many patients during different movements. McCarthy et al. [18] demonstrated that the true acetabular safe zone is much smaller than previously believed and varies considerably between patients. The results of these studies suggest that correct cup positioning is likely ultimately patient-specific and may require individualized preoperative planning. In the current study, not all malpositioned cups dislocated, but all cups in hips treated by cup revision for recurrent instability in this study were malpositioned. Although some prior studies have suggested a square-shaped safe zone [6, 9, 15, 19] (Table 4), such a shape could be anticipated to be unlikely given the motion of the joint and the shape of the components. Yoon et al. [35] demonstrated that given the impingement mechanism, it would be more reasonable to consider the safe zone as being circular (or nearly so) as supported by simulations of impingement and studies of actual dislocation risk. Our study showed a safe zone defined as an oval pattern (Fig. 6). Furthermore, the safe zone appears to be narrower for anteversion and wider for inclination than previously suggested [6, 9, 15, 19]. Our clinical results are concordant with the simulation results of Elkins et al. [11] who demonstrated, using a finite element analysis model, that ideal cup position was more restrictive than the historically defined safe zones and was substantially more sensitive to cup anteversion than to cup inclination. Our study and that of Danoff et al. [8] both suggest that the range of the acetabular safe zone may be different between inclination and anteversion. For a given cup, operative anteversion is always greater than radiographic anteversion and the difference may be large (commonly 8° or 9° depending on the cup inclination), whereas the difference between operative and radiographic inclination is much smaller [33].
Table 4.
Safe zones for acetabular cup position in clinical studies
In summary, both posteriorly and anteriorly dislocating, recurrently unstable hips treated by cup revision in this study differ from the control group in operative anteversion and tilt-adjusted operative anteversion, but not operative inclination when measured on CT. Furthermore, 32% of the dislocating hips were located in the Lewinnek safe zone, suggesting that although the Lewinnek study has been important in introducing the concept, the zone defined in that study should not be used in clinical practice. Our study data reinforce the clinical need to redefine the safe zone and identify a safe zone in operative measures that take into account patient-specific pelvic tilt. That malposition in operative anteversion (both with and without adjusting for pelvic tilt) was associated with recurrent instability highlights the need for increased clinical focus on the accuracy of cup anteversion in clinical practice and for additional studies using CT-based measurement to redefine the safe zone.
Acknowledgments
We thank Lisa Kamens RT, head CT technologist at New England Baptist Hospital, and all of the surgeons who cared for the patients who were analyzed in this study. This work was conducted with support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR001102) and financial contributions from Harvard University and its affiliated academic healthcare centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, or the National Institutes of Health.
Footnotes
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at The New England Baptist Hospital, Boston, MA, USA
References
- 1.Abdel MP, von Roth P, Jennings MT, Hanssen AD, Pagnano MW. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin Orthop Relat Res. 2016;474:386–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arora V, Hannan R, Beaver R, Fletcher T, Harvie P. A cadaver study validating CT assessment of acetabular component orientation: the Perth CT hip protocol. Skeletal Radiol. 2017;46:177–183. [DOI] [PubMed] [Google Scholar]
- 3.Babisch JW, Layher F, Amiot LP. The rationale for tilt-adjusted acetabular cup navigation. J Bone Joint Surg Am. 2008;90:357–365. [DOI] [PubMed] [Google Scholar]
- 4.Barrack RL, Lavernia C, Ries M, Thornberry R, Tozakoglou E. Virtual reality computer animation of the effect of component position and design on stability after total hip arthroplasty. Orthop Clin North Am. 2001;32:569–577, vii. [DOI] [PubMed] [Google Scholar]
- 5.Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stöckl B. Reducing the risk of dislocation after total hip arthroplasty. Bone Joint J. 2005;87:762–769. [DOI] [PubMed] [Google Scholar]
- 6.Bono JV, Sanford L, Toussaint JT. Severe polyethylene wear in total hip arthroplasty. Observations from retrieved AML PLUS hip implants with an ACS polyethylene liner. J Arthroplasty. 1994;9:119–125. [DOI] [PubMed] [Google Scholar]
- 7.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128–133. [DOI] [PubMed] [Google Scholar]
- 8.Danoff JR, Bobman JT, Cunn G, Murtaugh T, Gorroochurn P, Geller JA, Macaulay W. Redefining the acetabular component safe zone for posterior approach total hip arthroplasty. J Arthroplasty. 2016;31:506–511. [DOI] [PubMed] [Google Scholar]
- 9.Dorr LD, Wolf AW, Chandler R, Conaty JP. Classification and treatment of dislocations of total hip arthroplasty. Clin Orthop Relat Res. 1983;173:151–158. [PubMed] [Google Scholar]
- 10.Ecker TM, Tannast M, Murphy SB. Computed tomography-based surgical navigation for hip arthroplasty. Clin Orthop Relat Res. 2007;465:100–105. [DOI] [PubMed] [Google Scholar]
- 11.Elkins JM, Callaghan JJ, Brown TD. The 2014 Frank Stinchfield Award: The ‘landing zone' for wear and stability in total hip arthroplasty is smaller than we thought: a computational analysis. Clin Orthop Relat Res. 2015;473:441–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huppertz A, Radmer S, Asbach P, Juran R, Schwenke C, Diederichs G, Hamm B, Sparmann M. Computed tomography for preoperative planning in minimal-invasive total hip arthroplasty: radiation exposure and cost analysis. Eur J Radiol. 2011;78:406–413. [DOI] [PubMed] [Google Scholar]
- 13.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002;17:282–288. [DOI] [PubMed] [Google Scholar]
- 14.Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13:530–534. [DOI] [PubMed] [Google Scholar]
- 15.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 16.Loughead JM, Chesney D, Holland JP, McCaskie AW. Comparison of offset in Birmingham hip resurfacing and hybrid total hip arthroplasty. J Bone Joint Surg Br. 2005;87:163–166. [DOI] [PubMed] [Google Scholar]
- 17.Malik A, Wan Z, Jaramaz B, Bowman G, Dorr LD. A validation model for measurement of acetabular component position. J Arthroplasty. 2010;25:812–819. [DOI] [PubMed] [Google Scholar]
- 18.McCarthy TF, Alipit V, Nevelos J, Elmallah RK, Mont MA. Acetabular cup anteversion and inclination in hip range of motion to impingement. J Arthroplasty. 2016;31:264–268. [DOI] [PubMed] [Google Scholar]
- 19.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop Relat Res. 1990;261:159–170. [PubMed] [Google Scholar]
- 20.Miki H, Kyo T, Sugano N. Anatomical hip range of motion after implantation during total hip arthroplasty with a large change in pelvic inclination. J Arthroplasty. 2012;27:1641–1650.e1641. [DOI] [PubMed] [Google Scholar]
- 21.Murphy SB, Simon SR, Kijewski PK, Wilkinson RH, Griscom NT. Femoral anteversion. J Bone Joint Surg Am. 1987;69:1169–1176. [PubMed] [Google Scholar]
- 22.Murphy WS, Klingenstein G, Murphy SB, Zheng G. Pelvic tilt is minimally changed by total hip arthroplasty. Clin Orthop Relat Res. 2013;471:417–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232. [DOI] [PubMed] [Google Scholar]
- 24.Nomura T, Naito M, Nakamura Y, Ida T, Kuroda D, Kobayashi T, Sakamoto T, Seo H. An analysis of the best method for evaluating anteversion of the acetabular component after total hip replacement on plain radiographs. Bone Joint J. 2014;96:597–603. [DOI] [PubMed] [Google Scholar]
- 25.Sculco PK, Austin MS, Lavernia CJ, Rosenberg AG, Sierra RJ. Preventing leg length discrepancy and instability after total hip arthroplasty. Instr Course Lect. 2016;65:225–241. [PubMed] [Google Scholar]
- 26.Seki M, Yuasa N, Ohkuni K. Analysis of optimal range of socket orientations in total hip arthroplasty with use of computer-aided design simulation. J Orthop Res. 1998;16:513–517. [DOI] [PubMed] [Google Scholar]
- 27.Steppacher SD, Kowal JH, Murphy SB. Improving cup positioning using a mechanical navigation instrument. Clin Orthop Relat Res. 2011;469:423–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sugano N, Noble PC, Kamaric E. A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr. 1998;22:610–614. [DOI] [PubMed] [Google Scholar]
- 29.Tannast M, Langlotz U, Siebenrock KA, Wiese M, Bernsmann K, Langlotz F. Anatomic referencing of cup orientation in total hip arthroplasty. Clin Orthop Relat Res. 2005;436:144–150. [DOI] [PubMed] [Google Scholar]
- 30.Tannast M, Murphy SB, Langlotz F, Anderson SE, Siebenrock KA. Estimation of pelvic tilt on anteroposterior x-rays—a comparison of six parameters. Skeletal Radiol. 2006;35:149–155. [DOI] [PubMed] [Google Scholar]
- 31.Tiberi JV, 3rd, Antoci V, Malchau H, Rubash HE, Freiberg AA, Kwon YM. What is the fate of total hip arthroplasty (THA) acetabular component orientation when evaluated in the standing position? J Arthroplasty. 2015;30:1555–1560. [DOI] [PubMed] [Google Scholar]
- 32.Timperley AJ, Biau D, Chew D, Whitehouse SL. Dislocation after total hip replacement—there is no such thing as a safe zone for socket placement with the posterior approach. Hip Int. 2016;26:121–127. [DOI] [PubMed] [Google Scholar]
- 33.Wan Z, Malik A, Jaramaz B, Chao L, Dorr LD. Imaging and navigation measurement of acetabular component position in THA. Clin Orthop Relat Res. 2009;467:32–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–821. [DOI] [PubMed] [Google Scholar]
- 35.Yoon YS, Hodgson AJ, Tonetti J, Masri BA, Duncan CP. Resolving inconsistencies in defining the target orientation for the acetabular cup angles in total hip arthroplasty. Clin Biomech (Bristol, Avon). 2008;23:253–259. [DOI] [PubMed] [Google Scholar]
- 36.Yoshimine F. The safe-zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements. J Biomech. 2006;39:1315–1323. [DOI] [PubMed] [Google Scholar]
- 37.Zheng G, Zhang X, Steppacher SD, Murphy SB, Siebenrock KA, Tannast M. HipMatch: an object-oriented cross-platform program for accurate determination of cup orientation using 2D-3D registration of single standard x-ray radiograph and a CT volume. Comput Methods Programs Biomed. 2009;95:236–248. [DOI] [PubMed] [Google Scholar]
- 38.Zhu J, Wan Z, Dorr LD. Quantification of pelvic tilt in total hip arthroplasty. Clin Orthop Relat Res. 2010;468:571–575. [DOI] [PMC free article] [PubMed] [Google Scholar]