Abstract
Background
Dislocation is one of the most common complications after revision THA. Dual-mobility constructs and large femoral heads (ie, 40 mm) are two contemporary, nonconstrained bearing options used in revision THA to minimize the risk of dislocation; however, it is not currently established if there is a clear benefit to using dual-mobility constructs over large femoral heads in the revision setting.
Questions/purposes
We sought to determine if dual-mobility constructs would provide a reduction in dislocation, rerevision for dislocation, and reoperation or other complications as compared with large femoral heads in revision THA.
Methods
From 2011 to 2014, a series of 355 THAs underwent revision for any reason and received either a dual-mobility construct (146 THAs) or a 40-mm large femoral head (209 THAs). Indications for either construct were based on surgeon judgment; however, there is a preference to use dual-mobility constructs in patients believed to be at higher risk of dislocation. In the dual-mobility group, 20 of 146 (14%) were excluded because of loss of followup before 2 years or because they had a dual-mobility shell cemented into a preexisting acetabular component. In the large head group, 33 of 209 (16%) were lost to followup before 2 years. Followup in the dual-mobility group was 3.3 ± 0.8 years and followup in the large head group was 3.9 ± 0.9 years. Primary endpoints included dislocation, rerevisions for dislocation, and reoperations, which were determined through our institution’s total joint registry and verified by individual patient chart review. Age and body mass index were not different with the numbers available between the groups, but there was a slight predominance of females in the dual-mobility group (52% [66 of 126] female) versus the 40-mm large head group (41% [72 of 176] female) (p = 0.05). Notably, 33% (41 of 126) of patients receiving the dual-mobility constructs had the index revision THA done for a diagnosis of recurrent dislocation versus 9% (17 of 176) in the 40-mm large head group. Mean effective head size in the dual-mobility group was 47 mm (range, 38–58 mm).
Results
The subsequent frequency of dislocation in the dual-mobility construct group was less (3% [four of 126] dual-mobility versus 10% [17 of 176] in the 40-mm large head group; hazard ratio, 3.2 [1.1-9.4]; p = 0.03). Rerevision for dislocation in the dual-mobility construct group was less frequent (1% [one of 126] dual-mobility versus 6% [10 of 176] in the 40-mm large head group; hazard ratio, 7.1 [0.9-55.6]; p = 0.03). Reoperation for any cause in the dual-mobility construct group was less frequent (6% [eight of 126] dual-mobility versus 15% [27 of 176] in the 40-mm large head group; hazard ratio, 2.5 [1.1-5.5]; p = 0.02); there were no differences between the groups in terms of the overall percentage of complications in each group.
Conclusions
When compared with patients treated with a 40-mm large femoral head, patients undergoing revision THA who received a dual-mobility construct had a lower risk of subsequent dislocation, rerevision for dislocation, and reoperation for any reason in the first several years postoperatively. Those findings were present despite selection bias in this study to use the dual-mobility construct in patients at the highest risk for subsequent dislocation. Given the lower risk of subsequent dislocation, rerevision, and reoperation with the dual-mobility construct, some surgeons may wish to consider whether the role of dual-mobility should be judiciously expanded in contemporary revision THA.
Level of Evidence:
Level III, therapeutic study.
Introduction
THA is a successful and cost-effective operation, offering pain relief and improved function to patients with end-stage arthritis [4, 11]. Reported incidence of dislocation after primary THA varies from 0.2% to 10% and from 10% to 28% after revision THA [3, 16-18]. Jo et al. [9] found that in patients specifically revised for instability, risk of redislocation increased by approximately 2% yearly, reaching 34% by 15 years. In addition, Abdel et al. [1] recently showed that the majority (58% [120 of 206]) of dislocated primary THAs had a socket within the Lewinnek safe zone, indicating that instability is multifactorial.
Although most dislocations can be treated by closed reduction [6, 24], operative intervention sometimes is called for and may involve correcting component malposition, addressing soft tissue tension, and selecting components that reduce the likelihood of dislocation [2, 3, 6, 10, 14, 16, 24]. Although multiple studies have shown a low risk of dislocation in patients treated with dual-mobility constructs in both primary and revision THAs [15, 21, 22], there also are series showing that large femoral heads can reduce the risk of dislocation both in the primary and revision settings [5, 7, 8]. However, to our knowledge, there are no studies that directly compare these two nonconstrained implant options in revision THA.
We therefore sought to determine if dual-mobility constructs would provide a reduction in dislocation, rerevision for dislocation, and reoperation or other complications as compared with large femoral heads in revision THA.
Patients and Methods
A series of 355 revision THAs using either the Modular Dual MobilityTM system (Stryker, Mahwah, NJ, USA; ie, dual-mobility group) or 40-mm femoral heads (ie, large femoral head group) from 2011 to 2014 were identified from our total joint registry that follows all arthroplasties at our institution at 1 year, 2 years, 5 years, and every 5 years thereafter. Although 36-mm heads are frequently used at our institution and are generally accepted to fall under the umbrella of “large heads,” 40-mm heads are the largest commonly used head and therefore thought to give the best comparison to dual-mobility constructs in terms of optimal implant characteristics when addressing instability. Of the 355, 302 patients had a minimum of 2-year followup (85%). There were 126 in the dual-mobility group and 176 in the large femoral head group. For these patients, mean followup in the dual-mobility group was 3.3 ± 0.8 years and mean followup in the large head group was 3.9 ± 0.9 years. Patients were excluded if they had a dual-mobility liner cemented into a preexisting acetabular component at the time of the revision THA. Institutional review board approval was obtained before initiation of this retrospective, comparative study.
The primary outcome was postoperative dislocation after the revision THA requiring closed reduction, open reduction, or rerevision THA. Secondary outcomes included rerevision for dislocation, reoperation for any cause, and overall complications. The data were gathered from our longitudinally maintained total joint registry and individual patient chart reviews were carried out by a single investigator (MAH) who was not the primary surgeon for any patient included in this study.
Radiographic analysis was carried out by a single investigator (MAH) using AP pelvis and crosstable lateral views of the hip. This was performed after index revision on all patients. Radiographic calibration was done using femoral head size obtained from operative reports, and this magnification factor was used in subsequent measurements. Acetabular inclination, leg length discrepancy, and offset were measured on the AP pelvis radiographs. Anteversion was measured on crosstable lateral radiographs using the ischiolateral method as described by Tiberi et al. [20]. Inclination and anteversion measurements were then compared between the dual-mobility and large femoral head groups.
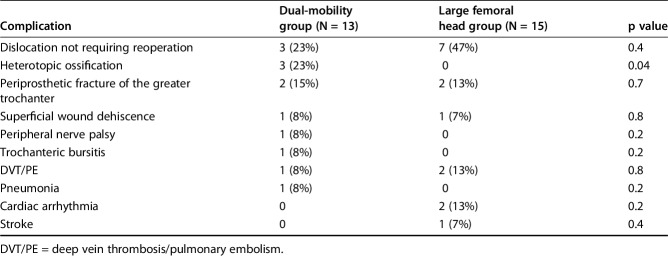
Mean age and body mass index were not different with the numbers available between the groups (Table 1). There were more women in the dual-mobility group (52% [66 of 126] versus 41% [72 of 176] in the large head group; p = 0.05).
Table 1.
Demographic parameters
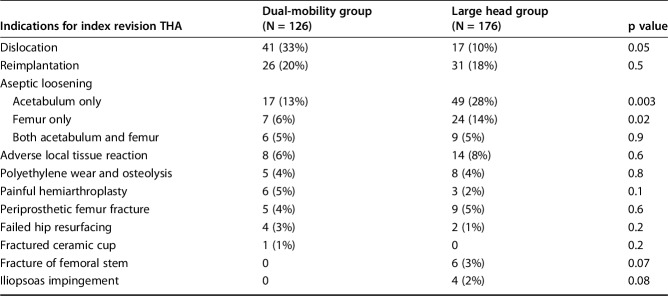
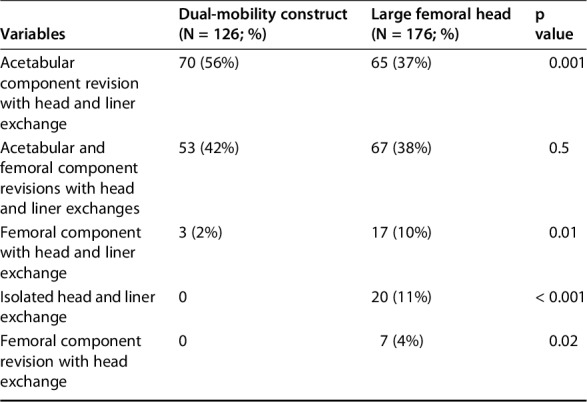
Twelve surgeons at our institution performed these revisions. Notably, 41 of 126 (33%) of the patients in the dual-mobility group had instability as an indication for the revision procedure, whereas only 15 of 176 (9%) of the large femoral head group had an initial indication of instability for revision (p = 0.05) (Table 2). In the dual-mobility group, 70 patients had acetabular revisions, 53 patients had acetabular and femoral components revised, whereas three had femoral revision with head and liner exchange. It should be noted, patients who already have a Stryker Tritanium™ shell (Stryker, Mahwah, NJ, USA) in place can receive a dual-mobility construct without removing the shell. In the large head group, 67 had acetabular and femoral component revisions, 65 had acetabular components revised alone, 19 had head and liner exchange alone, 17 had femoral components revised with a head and liner exchange, and one had proximal body and femoral head exchange (Table 3). The average number of previous surgeries in both groups was two (mean difference 0.27 [-0.07 to 0.61], p = 0.1).
Table 2.
Indications for index revision
Table 3.
Components revised at index revision THA
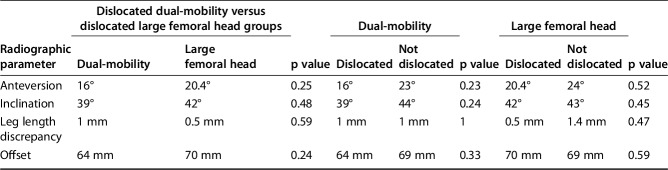
Radiographic analysis revealed a mean anteversion of 16° in patients receiving a dual-mobility construct who dislocated versus 23° in patients who did not (mean difference 6.9 [-10.3 to 24.2], p = 0.23). In this group, mean inclination was 39° in those who dislocated versus 44° in those who did not (mean difference 4.4 [-7.4 to 16.2], p = 0.24). The mean leg length discrepancy was 1 mm in both groups (mean difference -0.0 [-10.1 to 10.1], p = 1), and mean offset was 64 mm in those who dislocated versus 69 mm in those who did not (mean difference 4.3 [-9.3 to 18], p = 0.33). In the large femoral head group, mean anteversion was 20° in patients who dislocated versus 25° in patients who did not (mean difference 3.9 [-1.5 to 9.3], p = 0.52). In this group, mean inclination was 42° in those who dislocated versus 43° in those who did not (mean difference 1.4 [-2.3 to 5.1], p = 0.45), mean leg length discrepancy was 3.2 mm versus 1.3 mm (mean difference 1 [-2.4 to 4.3], p = 0.47), and mean offset was 70 mm in those who dislocated versus 69 mm in those who did not (mean difference -1.2 [-5.6 to 3.2], p = 0.6). There were no differences in the mean of these parameters in patients who dislocated and did not dislocate in each group. Additionally, all values fell within 2 SDs of mean values, demonstrating the absence of extreme outliers in any group (Table 4).
Table 4.
Radiographic analysis of dual-mobility versus large femoral head (ie, 40 mm) groups
Statistical Analysis
Continuous variables were given as mean and SD and compared using two-tailed t-tests. Discrete variables are given as proportions and these are analyzed with a chi-square test or Fisher’s exact test. Significance was set at a p value of < 0.05. Statistical analysis was carried out utilizing StatPlus software Version 5.9.4.1 (AnalystSoft Inc, Walnut, CA, USA).
Results
Risk of Dislocation
The incidence of postoperative dislocation was 3% in the dual-mobility group (four of 126 patients) compared with 10% in the large femoral head group (17 of 176 patients; hazard ratio, 3.2 [1.1-9.4]; p = 0.03) (Fig. 1). There was no association with type of surgical approach (Table 5).
Fig. 1.
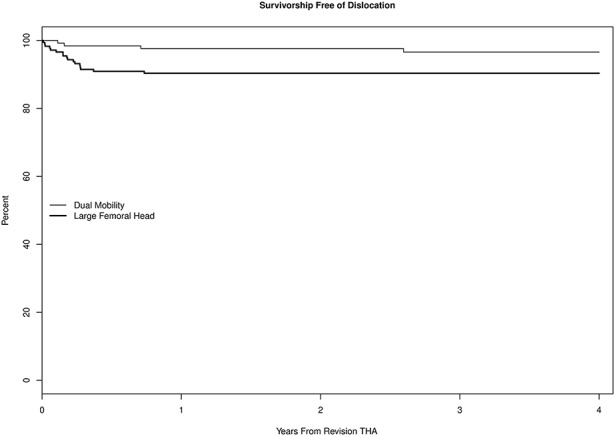
Survival free of dislocation is demonstrated. The majority of dislocations occurred within the first year of rerevision.
Table 5.
Surgical approach in patients who dislocated after revision THA
Of the four patients who dislocated after revision in the dual-mobility group, two of 41 (5%) had initially undergone revision for an indication of instability and two of 85 (2%) had initially undergone revision for other indications. No intraprosthetic dislocations were observed, and no patients underwent open reduction. Of the 17 patients who dislocated after revision in the large head group, one had been revised for instability and 16 had been revised for other indications (p = 0.09).
Rerevisions for Dislocations
Rerevision for dislocation in the dual-mobility construct group was less frequent (1% [one of 126] dual-mobility versus 6% [10 of 176] in the 40-mm large head group; hazard ratio, 7.1 (0.9-55.6); p = 0.03) (Fig. 2). Of the four patients who dislocated in the dual-mobility group, one had rerevision for dislocation. This patient went on to resection arthroplasty. Of the 17 patients in the large head group who experienced a dislocation after revision, 10 patients went on to rerevision. These patients went on to constrained liners (n = 7), dual-mobility constructs (n = 2), and resection arthroplasty (n = 1). At latest followup, none of the patients rerevised to either a dual-mobility construct or a constrained liner had further instability. Patients in both groups who did not undergo rerevision THA were treated with closed reduction, and they reported no further instability.
Fig. 2.
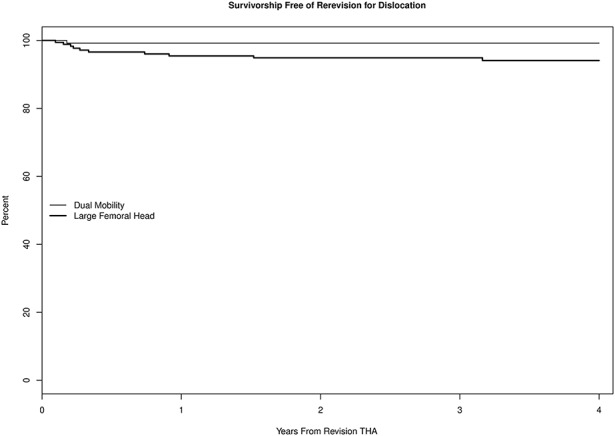
Survivorship free of rerevision is demonstrated for both groups. In the dual-mobility group, rerevision occurred early and then plateaued, whereas the larger femoral head group showed decreased survivorship over time out to 4 years.
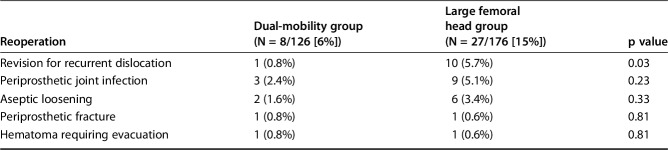
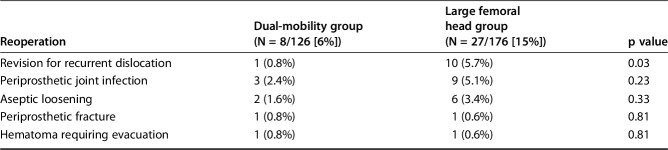
Reoperation for Any Cause and Complications
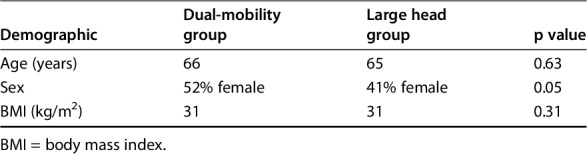
Reoperation for any cause in the dual-mobility construct group was less frequent (6% [eight of 126] dual-mobility versus 15% [27 of 176] in the 40-mm large head group; hazard ratio, 2.5 [1.1-5.5]; p = 0.02) (Table 6; Fig. 3). The overall frequency of complications was 10% (13 of 126) in the dual-mobility group versus 8% (15 of 176) in the large femoral head group (p = 0.6) (Table 7).
Table 6.
All-cause reoperation
Fig. 3.
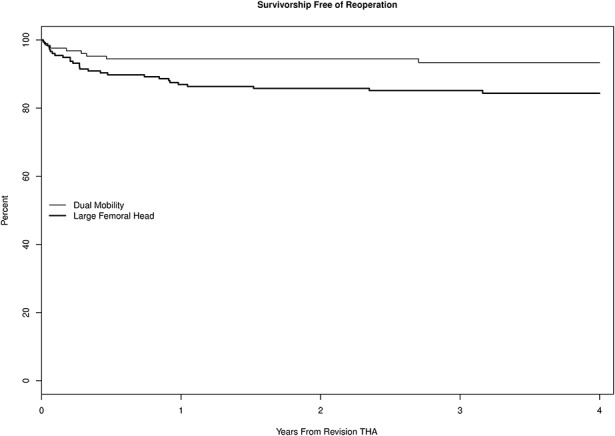
Survivorship free of reoperation for any reason is shown. Both groups underwent the majority of reoperations within the first year after surgery. Likewise, after the first year, both continue to have gradually decreased survivorship out to 4 years.
Table 7.
Overall complication rate
Discussion
Dislocation after both primary and revision THAs continues to be one of the most common postoperative complications and causes for revision surgery. Dislocation after revision THA may be as high as 28% [3, 16-18]. Patients undergoing revision THA often have abductor dysfunction or greater trochanteric osteolysis, which may compromise the abductor mechanism and increase the risk of postoperative instability. The use of constrained acetabular components decreases the risk of postoperative instability but leads to an increased risk of mechanical failure with midterm followup [25]. Alternatives to constrained liners include dual-mobility constructs and large-diameter femoral heads. Previous randomized controlled trials have demonstrated a decrease in the risk of dislocation with the use of large-diameter femoral heads versus traditional smaller diameter femoral heads [8]. Dual-mobility constructs have also reduced the risk of dislocation in both the primary and revision settings [12, 15, 21-23]. However, it is currently not clear whether dual-mobility constructs with a larger potentially effective head size have greater stability than large 40-mm femoral heads. We therefore compared these two approaches in the context of a retrospective analysis of data drawn from a large, longitudinally maintained institutional registry.
There are several limitations of this study. First, there was a 15% loss to followup; however, there was no differential loss to followup between the two groups. Still, it is possible a number of dislocations, rerevisions, and reoperations were not captured in the current study as a result of this loss of followup. Second, this was conducted retrospectively and therefore is vulnerable to several kinds of bias, most notably selection bias, although the bias that we have identified (using the dual-mobility constructs in the highest risk patients) did not result in more dislocations in that cohort. Dual-mobility constructs generally are selected for patients in whom instability is more likely and who also tend to be younger and more active. This may impact the generalizability of this study. As a result of the retrospective nature of the study, combined anteversion was unable to be calculated for each patient because CT scans are not routinely obtained after primary or revision arthroplasty. Additionally, information on abductor function and bone loss was not uniformly collected and therefore could not be included in analysis. Lastly, we focused on the outcomes of dislocation, rerevision for dislocation, and reoperation for any cause and did not analyze functional scores.
In this contemporary study of patients undergoing revision THA for a variety of reasons, there were fewer patients who dislocated postoperatively when revised to a dual-mobility construct compared with those revised with a large 40-mm femoral head. This is consistent with other studies demonstrating low dislocation rates in patients who underwent revision THA with a dual-mobility construct [15, 19, 22, 23]. Wegrzyn et al. [23] treated 980 patients with dual-mobility constructs during revision THAs. At a mean of 7 years of followup, the authors found a cumulative incidence of dislocation of 1.5%. Two-thirds of the patients in this study who dislocated had no identifiable component malposition. Similarly, Vasukutty et al. [21] found an incidence of dislocation of 2% at a mean followup of 48 months in patients who received a dual-mobility construct during their revision THA. This study demonstrates that when compared with the largest commonly used femoral head size (40 mm), dual-mobility constructs may offer not only a lower risk of dislocation, but also a lower risk of rerevision and reoperation for any reason.
Among those patients who did dislocate after their revision THA, the subsequent frequency of rerevision was lower in the dual-mobility group than in the large femoral head group. The three patients who were successfully closed reduced in the dual-mobility group had no further instability episodes at latest followup. The patient who had rerevision went on to resection arthroplasty for deep prosthetic infection. In the large head group, there were no further dislocations at latest followup for patients revised to either a constrained liner or a dual-mobility construct. Garbuz et al. [7] found a frequency of dislocation after revision THA to large femoral heads of 1.1% with no rerevision in that group, which contrasts with our findings of 10% dislocation in the large head group and 59% going on to rerevision. Our frequency of redislocation after revision to a dual-mobility construct of 3% at a mean of 3.6-year followup is consistent with the risk of dislocation as determined by others when using these constructs for revision THA, which varied from 1.5% to 4.8% [12, 15, 19, 22, 23]. Our findings suggest the incidence of rerevision after revision to large femoral heads may be higher than currently found in the literature.
The overall frequency of reoperation of 6% in the dual-mobility group versus 15% in the large femoral head group is particularly important to note in today’s healthcare environment where readmission and reoperations are under greater scrutiny. Revision for instability made up 37% of the patients in the large head group, whereas the remainder had infection, fracture, aseptic loosening, or hardware failure. One patient in the dual-mobility construct group who dislocated after revision surgery went on to resection arthroplasty, as previously noted, whereas the other indications for reoperations were infection, fracture, or aseptic loosening. Our overall frequency of reoperation was approximately half of that reported by Simian et al. [19], who found an overall frequency of reoperation of 11% in their recent study of dual-mobility constructs for revision THA. In that small cohort of patients, a higher percentage of reoperation for infection occurred than in the present investigation [19]. In our analysis, neither surgical approach nor sex appeared to influence the likelihood of dislocation after our revision THAs. Berry [2] demonstrated that female patients are twice as likely to dislocate their THA as male patients. This knowledge may account for the gender imbalance between the two cohorts in our study because our dual-mobility cohort had both more patients with an index diagnosis of recurrent dislocation and more patients who were female. Knowing that female patients undergoing revision THA are at particularly high risk of dislocation, it is likely that there was some surgeon bias toward using dual-mobility constructs in these higher risk patients. Our radiographic analysis showed similar component position between patients who did and did not dislocate. Moreover, there was similar radiographic positioning between the dual-mobility and large femoral head groups in our study. Notably, patients who did and did not dislocate in both groups had inclination and anteversion angles within the Lewinnek “safe zone” of 40° ± 10° and 15° ± 10°, respectively [13]. These findings are in agreement of those by Abdel et al. [1] who demonstrated that a majority of dislocating THAs was within these traditionally accepted “safe” parameters.
In conclusion, this large retrospective study of more than 300 revision THAs showed that patients who received a dual-mobility construct, as compared with patients treated with a 40-mm large femoral head, had a lower risk of subsequent dislocation, rerevision for dislocation, and reoperation for any reason in the first several years postoperatively. Those findings were present despite a selection bias in this study to use the dual-mobility construct in patients at the highest risk for subsequent dislocation. Given the lower risk of subsequent dislocation, rerevision, and reoperation with the dual-mobility construct, some surgeons may wish to consider whether the role of dual-mobility constructs should be judiciously expanded in contemporary revision THA.
Acknowledgments
We thank Dirk R. Larson MS, for his help with statistical analysis.
Footnotes
One of the authors (MPA) is a paid consultant for Stryker (Kalamazoo, MI, USA). One of the authors (MJT) has received personal fees from DJO Global (Vista, CA, USA), outside the submitted work. One of the authors (ADH) has received hip royalties from Stryker (Kalamazoo, MI, USA), outside the submitted work. One of the authors (MWP) has received royalties from DePuy Synthes (Warsaw, IN, USA) and Stryker and is a paid consultant for Pacira Pharmaceuticals, Inc (San Diego, CA, USA) and PixarBio (Salem, NH, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Abdel MP, von Roth P, Jennings MT, Hanssen AD, Pagnano MW. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin Orthop Relat Res. 2016;474:386–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berry DJ. Unstable total hip arthroplasty: detailed overview. Instr Course Lect. 2001;50:265–274. [PubMed] [Google Scholar]
- 3.Carter AH, Sheehan EC, Mortazavi SM, Purtill JJ, Sharkey PF, Parvizi J. Revision for recurrent instability: what are the predictors of failure? J Arthroplasty. 2011;26(Suppl):46–52. [DOI] [PubMed] [Google Scholar]
- 4.Chang RW, Pellisier JM, Hazen GB. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA. 1996;275:858–865. [PubMed] [Google Scholar]
- 5.Cinotti G, Lucioli N, Malagoli A, Calderoli C, Cassese F. Do large femoral heads reduce the risks of impingement in total hip arthroplasty with optimal and non-optimal cup positioning? Int Orthop. 2011;35:317–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daly PJ, Morrey BF. Operative correction of an unstable total hip arthroplasty. J Bone Joint Surg Am. 1992;74:1334–1343. [PubMed] [Google Scholar]
- 7.Garbuz DS, Masri BA, Duncan CP, Greidanus NV, Bohm ER, Petrak MJ, Della Valle CJ, Gross AE. The Frank Stinchfield Award: Dislocation in revision THA: do large heads (36 and 40 mm) result in reduced dislocation rates in a randomized clinical trial? Clin Orthop Relat Res. 2012;470:351–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Howie DW, Holubowycz OT, Middleton R. Large femoral heads decrease the incidence of dislocation after total hip arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2012;94:1095–1102. [DOI] [PubMed] [Google Scholar]
- 9.Jo S, Jimenez Almonte JH, Sierra RJ. The cumulative risk of re-dislocation after revision THA performed for instability increases close to 35% at 15 years. J Arthroplasty. 2015;30:1177–1182. [DOI] [PubMed] [Google Scholar]
- 10.Kaplan SJ, Thomas WH, Poss R. Trochanteric advancement for recurrent dislocation after total hip arthroplasty. J Arthroplasty. 1987;2:119–124. [DOI] [PubMed] [Google Scholar]
- 11.Lavernia CJ, Iacobelli DA, Brooks L, Villa JM. The cost-utility of total hip arthroplasty: earlier intervention, improved economics. J Arthroplasty. 2015;30:945–949. [DOI] [PubMed] [Google Scholar]
- 12.Leiber-Wackenheim F, Brunschweiler B, Ehlinger M, Gabrion A, Mertl P. Treatment of recurrent THR dislocation using of a cementless dual-mobility cup: a 59 cases series with a mean 8 years' follow-up. Orthop Traumatol Surg Res. 2011;97:8–13. [DOI] [PubMed] [Google Scholar]
- 13.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 14.McGann WA, Welch RB. Treatment of the unstable total hip arthroplasty using modularity, soft tissue, and allograft reconstruction. J Arthroplasty. 2001;16(Suppl 1):19–23. [DOI] [PubMed] [Google Scholar]
- 15.Mertl P, Combes A, Leiber-Wackenheim F, Fessy MH, Girard J, Migaud H. Recurrence of dislocation following total hip arthroplasty revision using dual mobility cups was rare in 180 hips followed over 7 years. HSS J. 2012;8:251–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parvizi J, Picinic E, Sharkey PF. Revision total hip arthroplasty for instability: surgical techniques and principles. J Bone Joint Surg Am. 2008;90:1134–1142. [PubMed] [Google Scholar]
- 17.Patel PD, Potts A, Froimson MI. The dislocating hip arthroplasty: prevention and treatment. J Arthroplasty. 2007;22(Suppl 1):86–90. [DOI] [PubMed] [Google Scholar]
- 18.Sikes CV, Lai LP, Schreiber M, Mont MA, Jinnah RH, Seyler TM. Instability after total hip arthroplasty: treatment with large femoral heads vs constrained liners. J Arthroplasty. 2008;23(Suppl):59–63. [DOI] [PubMed] [Google Scholar]
- 19.Simian E, Chatellard R, Druon J, Berhouet J, Rosset P. Dual mobility cup in revision total hip arthroplasty: dislocation rate and survival after 5 years. Orthop Traumatol Surg Res. 2015;101:577–581. [DOI] [PubMed] [Google Scholar]
- 20.Tiberi JV, Pulos N, Kertzner M, Schmalzried TP. A more reliable method to assess acetabular component position. Clin Orthop Relat Res. 2012;470:471–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vasukutty NL, Middleton RG, Matthews EC, Young PS, Uzoigwe CE, Minhas TH. The double-mobility acetabular component in revision total hip replacement: the United Kingdom experience. J Bone Joint Surg Br. 2012;94:603–608. [DOI] [PubMed] [Google Scholar]
- 22.Vigdorchik JM, D'Apuzzo MR, Markel DC, Malkani AL, Raterman S, Sharpe KP, Cornell CN, Westrich GH. Lack of early dislocation following total hip arthroplasty with a new dual mobility acetabular design. Hip Int. 2015;25:34–38. [DOI] [PubMed] [Google Scholar]
- 23.Wegrzyn J, Tebaa E, Jacquel A, Carret JP, Bejui-Hugues J, Pibarot V. Can dual mobility cups prevent dislocation in all situations after revision total hip arthroplasty? J Arthroplasty. 2015;30:631–640. [DOI] [PubMed] [Google Scholar]
- 24.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306. [PubMed] [Google Scholar]
- 25.Yang C, Goodman SB. Outcome and complications of constrained acetabular components. Orthopedics. 2009;32:115. [PubMed] [Google Scholar]