Abstract
Background
Revision THA to treat recurrent instability can itself be complicated by recurrent instability, and when this occurs, this problem is difficult to treat. Some patients’ THAs will continue to dislocate despite use of a constrained liner. One option in this difficult-to-treat group is conversion to a dual-mobility (DM) construct, but there are few data on this approach.
Questions/purposes
(1) What were the Harris hip scores in a small group of patients whose constrained liners were converted to DM constructs to treat recurrent dislocation? (2) What were the redislocation, rerevision, and DM construct retention rates in these patients?
Methods
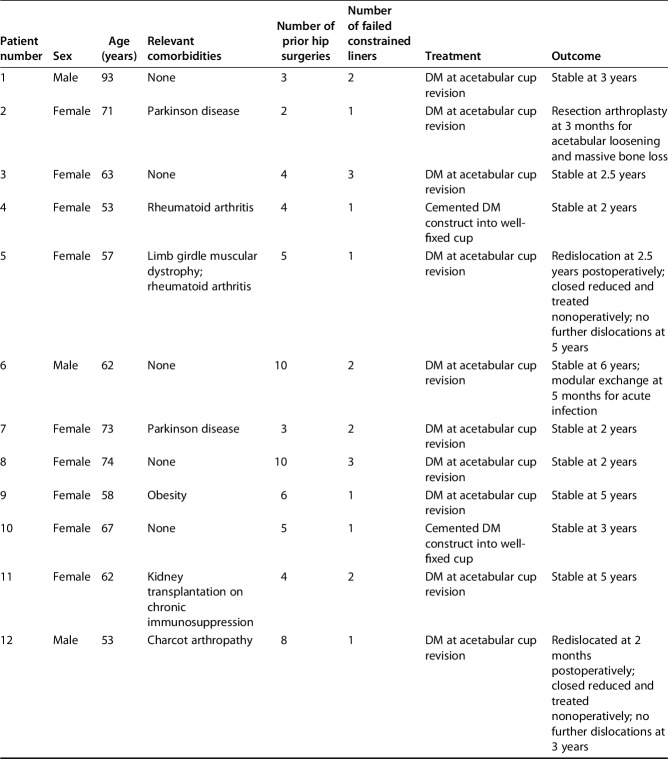
We conducted a retrospective analysis of a longitudinally maintained institutional database maintained by individuals other than the treating surgeons to identify patients undergoing conversion of constrained liners to DM constructs in revision THA from 2011 to 2014. We identified 16 patients who underwent revision of dislocated constrained liners to DM constructs. Two patients died before 2-year followup, leaving 14 patients available for followup at a minimum of 24 months and a median of 37 months (range, 24–71 months). Indications for conversion to DM constructs included patients with dislocation of multiple prior constrained liners, patients with at least partial abductor functioning and soft tissue tensioning, and patients at very high risk for recurrent instability as an alternative to resection arthroplasty. Ten patients (10 of 14) underwent DM conversion at the time of cup revision, whereas four patients (four of 14) had a DM construct cemented into a preexisting cup. Median age was 65 years (range, 53–93 years). Median number of prior hip surgeries was five (range, three to 10) and seven patients (seven of 14) had dislocated more than one constrained liner.
Results
Harris hip score improved from a median of 57 (range, 55–67) to 84 (range, 68–96) postoperatively (p < 0.001). Three patients (three of 14) experienced a redislocation. Two (two of 14) of these patients were closed reduced and treated successfully nonoperatively; one (one of 14) patient experienced an intraprosthetic dislocation and underwent modular exchange. One patient (one of 14) underwent early resection arthroplasty for acetabular loosening after complex acetabular reconstruction. Overall, all other patients (13 of 14) retained a DM construct at final followup.
Conclusions
Conversion to a DM construct shows promise as a salvage option in high-risk, multiply operated on patients with dislocated constrained liners undergoing revision THA for recurrent instability. The ability to close reduce a dislocated DM construct is a distinct advantage over constrained liners. However, longer followup is required given that three of 14 redislocated, and one of those underwent revision for persistent instability at short-term followup.
Level of Evidence:
Level IV, therapeutic study.
Introduction
Rerecurrent instability is a challenging complication after revision THA for instability [2, 10, 18, 19, 26]. A recent report indicated that cumulative risk of redislocation after revision THA for recurrent instability was 35% at 15 years [10]. There are multiple surgical options to address an unstable prosthesis including abductor repairs or reconstructions, conversion to hemiarthroplasty [15], large-diameter femoral heads [1, 19, 26], acetabular revision [18], increased hip offset [18], constrained liners [4–7, 9, 13, 19, 24], and dual-mobility (DM) constructs [3, 8, 12, 16, 17, 20, 21, 24, 25]. One of the more commonly utilized techniques to treat or prevent recurrent dislocation, especially in multiply operated on patients with deficient abductor mechanisms, is constrained liners [4-7, 9, 13, 19, 23]. However, there are some inherent disadvantages with the use of constrained liners: limited ROM before prosthetic impingement and increased stress at the locking mechanism and at the prosthesis-bone interface [7, 9, 11]. This may lead to increased risk of liner breakage, intraprosthetic dislocation, or component loosening [9]. In high-risk patients undergoing constrained liner implantation for recurrent THA dislocation, as many as 31% of patients experience constrained liner dislocations [2, 4, 6, 9]. Furthermore, if a constrained liner dislocates, treatment almost always necessitates open reduction [22].
Furthermore, there is little information on how to treat patients who have dislocated one or more constrained liners secondary to recurrent instability; resection arthroplasty may be the final and only salvage option [15]. To date, we are unaware of any studies analyzing the outcomes of revising a dislocated constrained liner to a DM construct as an alternative option to treat a patient with recurrent THA dislocations. Potential advantages of DM components include the biomechanical advantage of an effective large-diameter femoral head to increase the jump distance and impingement-free arc of motion [1]. DM constructs provide an alternative method by reducing impingement-induced dislocations, a failure mode to which constrained liners are particularly susceptible. Moreover, not adding additional constraint, especially at the time of new acetabular component placement, theoretically reduces the risk of acetabular component loosening [7]. Finally, the potential ability to reduce a dislocated DM component without open hip surgery may be an advantage in these high-risk patients [16].
We therefore asked: (1) What were the Harris hip scores in a small group of patients whose constrained liners were converted to DM constructs to treat recurrent dislocation? (2) What were the redislocation, rerevision, and DM construct retention rates in these patients?
Patients and Methods
After approval from the institutional review board, we identified 16 patients who underwent conversion of a dislocated constrained liner to a DM construct at a single tertiary care academic institution from 2011 to 2014 through an institutional total joint registry maintained by persons other than the treating surgeons. Through individual chart analysis, analysis of operative reports, and review of preoperative and postoperative radiographs by an individual not involved in the surgical treatment (BPC), 16 patients who had a dislocated constrained liner converted to DM constructs in revision THA were confirmed. Two patients died before 2-year followup, leaving 14 patients for analysis at a minimum clinical followup of 24 months and a median followup of 37 months (range, 24-71 months). Median age was 65 years (range, 53-93 years) and median body mass index was 28 kg/m2 (range, 17–39 kg/m2). Three patients (three of 14) had a previously diagnosed progressive neuromuscular disorder. Median number of prior hip surgeries was five (range, three to 10 surgeries). Seven patients (seven of 14) had dislocated more than one constrained liner secondary to instability (Table 1).
Table 1.
Demographics, treatment, and outcomes of patients undergoing revision THA with failed constrained liners resulting from recurrent instability with implantation of dual-mobility components
The decision to utilize a DM construct versus another prosthetic-stabilizing strategy was decided on by the surgeon after careful consideration of numerous factors including patient age, gender, activity level, number and type of prior hip operations, quality of the abductor mechanism as assessed by physical and radiographic examination, and the currently implanted components. In general, indications for conversion of dislocated constrained liners to DM constructs were (1) dislocation of multiple prior constrained liners with an attempt to reduce prosthetic impingement and impart a different mechanism of hip stability; (2) at least partial soft tissue tension and abductor mechanism present; and (3) salvage in extremely high-risk patients as an alternative to or last option before resection arthroplasty. A relative contraindication was the complete absence of proximal bone or an abductor mechanism, but conversion to a DM construct can still be considered in these patients who meet one of the aforementioned considerations.
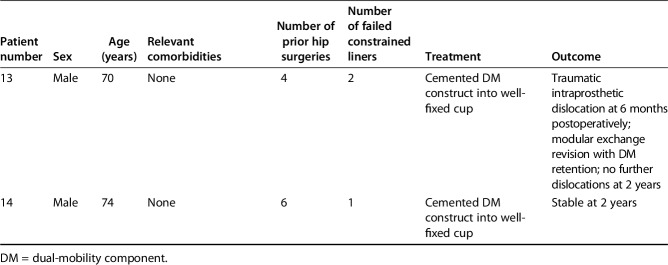
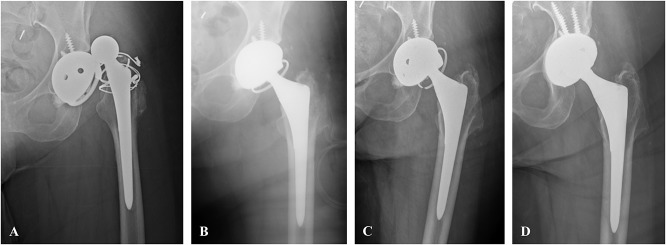
All revision THAs were performed by seven surgeons experienced in primary and revision THA at a single academic center. The decision to utilize a DM component versus another prosthetic-stabilizing strategy was decided on by the surgeon after careful consideration of numerous factors including patient age, gender, activity level, number and type of prior hip operations, quality of the abductor mechanism, and the currently implanted components. The posterolateral approach was utilized in seven THAs (seven of 14) and the anterolateral interval was utilized in seven THAs (seven of 14). The last constrained liner in place at the time of failure included: six (six of 14) Trident® Osteonics constrained liners (Stryker Orthopaedics, Mahwah, NJ, USA), six (six of 14) Trilogy® Longevity® Constrained liners (Zimmer, Warsaw, IN, USA), one (one of 14) Freedom® constrained liner (Biomet, Warsaw, IN, USA), and one (one of 14) unknown type of constrained liner that was implanted at an outside hospital for which records could not be obtained. The Modular Dual Mobility (Stryker Orthopaedics) DM construct was utilized in all patients. Ten patients (10 of 14) underwent cup revision at the same time as conversion to DM (Fig. 1) when revision was needed to accommodate the DM construct (eight hips) or cup malposition was thought to be contributing to instability (two hips). Four patients (four of 14) underwent modular exchange with a cemented DM construct into a well-fixed cup (Fig. 2).
Fig. 1 A-D.
Patient 11 (Table 1) is a 67-year-old woman who had a failed Zimmer Trilogy® Longevity® Constrained liner placed for recurrent instability, as seen on the AP radiograph (A). She was revised to a Trident® Osteonics constrained liner (B), which subsequently failed as well (C). She then underwent acetabular revision with implantation of DM components (D). She has a stable hip without subsequent dislocations at 5 years postoperatively.
Fig. 2 A-F.

Patient 1 is a 76-year-old man who sustained a first dislocation 10 years after primary THA. He was revised after failed nonoperative treatment to a cemented Trident® Osteonics constrained liner (A) that subsequently failed at 2 years with breakage of the locking mechanism. (B). He was rerevised to another constrained liner (C), which also failed at 2 years (D). Closed reduction attempts were unsuccessful (E). He then underwent acetabular revision with conversion to DM components (F) and remained dislocation-free at final followup 3 years after his last revision.
Results
Harris hip score (HHS) improved from a median of 57 (range, 55–67) to 84 (range, 68–96) postoperatively (p < 0.001).
Three patients (three of 14) experienced redislocation at 2, 6, and 30 months. Two (two of 14) of these patients, including one patient with progressive limb muscular dystrophy and one patient with Charcot arthropathy of the hip, were closed reduced and treated nonoperatively; neither patient experienced redislocation at 2 and 3 years postdislocation. One (one of 14) of these patients experienced a traumatic intraprosthetic dislocation with dissociation of the polyethylene liner from the femoral head. This was treated with modular exchange of the polyethylene liner and reduction; this patient had no further instability 2 years after dislocation. Two patients (two of 14) were rerevised at final followup. One patient (one of 14) with progressive Parkinson disease who underwent DM construct placement at the time of acetabular revision underwent resection arthroplasty for acetabular loosening and massive acetabular bone loss in the setting of a minimally ambulatory patient. One patient (one of 14) underwent irrigation and débridement and modular exchange of the DM construct for acute deep periprosthetic infection 5 months after revision THA; the patient retained the DM components without issues with instability or further infection. Thirteen of the 14 patients retained DM constructs at final clinical followup. There were no other reoperations.
Discussion
Recurrent instability remains a challenging problem after revision THA with a recent study reporting a 35% redislocation rate after revision THA for instability at 15 years [10]. In patients who have undergone multiple prior procedures, surgical options are limited. Constrained liners are an option for patients with recurrent instability in revision THA, but their results are mixed [4-7, 11, 13, 19, 23]. We recently reported a dislocation rate of 31% in such patients undergoing modular exchange with implantation of one type of constrained liner for treatment of recurrent prosthetic instability [4]. The goal of the current study was to analyze the HHS, redislocation, and the likelihood of component retention among patients whose dislocating constrained components were treated with DM constructs.
We acknowledge several limitations to the current study. First, there is a small number of patients with short-term (minimum 2 years) followup. More patients in this series may sustain redislocations if followed for a longer period of time. Furthermore, although all patients were high-risk patients who had sustained multiple dislocations and dislocated at least one constrained liner, the patient population, past constrained liners, and surgical treatment at DM revision (cup revision versus modular exchange) were nonuniform in this study. Because several surgical approaches including a repeat constrained liner and resection arthroplasty were utilized on patients with dislocated constrained liners during this timeframe, this case series is subject to selection bias. However, we recognize potential selection bias in these specific patients and have attempted to outline our indications for conversion of dislocated constrained liners to DM constructs. Finally, there is also the potential for assessment bias because some patients may have experienced complications and presented to an outside institution.
Mean HHS improved preoperatively from 60 to 85 at latest followup. Several studies have reported reliable results and outcomes with the use of DM constructs in primary and revision THA [8, 20, 25]. In a series of 36 patients undergoing revision THA considered at high risk for recurrent dislocation, Plummer et al. [16] reported improved HHS by a mean of 45 points with a final mean of 90. DM constructs utilized in revision THA can reliably improve patients’ pain and functioning. Although there are no specific studies measuring patients’ pain and function levels after resection arthroplasty to the authors’ knowledge, we believe this clinical improvement and clinical function at final followup are superior to resection arthroplasty.
In this series, three patients experienced redislocations (three of 14). Two of these three patients had progressive neurologic disorders affecting the hip (Table 1). However, only one patient (one of 14) underwent operative management of a DM construct dislocation; this was secondary to a traumatic intraprosthetic dislocation, a rare complication of DM constructs [14, 25]. All patients in this patient cohort who experienced repeat dislocation retained DM constructs. Simian et al. [20] reported a 1.4% dislocation rate in patients undergoing revision THA, mainly for aseptic loosening and without a history of hip instability, with DM constructs. In a study of 994 revision THAs for all indications, Wegryzn et al. [25] reported an overall dislocation rate of 1.5% and the intraprosthetic dislocation rate was 0.2%. Several reports indicate an up to 30% dislocation rate of constrained liners in multiply operated on patients at high risk for recurrent dislocation [4, 6]. DM constructs and constrained liners have different mechanisms to impart hip stability. In theory, constrained liners restrict the hip into the socket by prosthetic design in an attempt to compensate for deficient soft tissue tension. Large femoral head components such as DM constructs prevent impingement-induced dislocation by increasing impingement-free ROM and the jump distance [1, 8, 19, 26]. Although these failure modes are not always so discrete or mutually exclusive, it makes sense to attempt an alternative method of hip stabilization in the event of one or multiple failures of the other approach. To the authors’ knowledge, this is the first study directly analyzing the outcomes of converting dislocated constrained liners to DM constructs. In this series of extremely high-risk patients, only one patient (one of 14) required revision for recurrent instability; that patient retained the DM construct 2 years postrevision without recurrent instability.
One of the purported advantages of DM constructs in this high-risk patient population, many of whom also have comorbidities that may predispose them to dislocations such as neuromuscular diseases, is the ability to close reduce and conservatively treat redislocations (Table 1). Although there are case reports of closed reducing unbroken, dislocated constrained liners [22], the majority of dislocated constrained liners either have broken locking mechanisms or cannot be closed reduced (Fig. 1) [4, 6, 7, 22, 23]. Plummer et al. [16] reported one dislocation and two cemented DM dissociations requiring revision at a mean of 2.4 years followup in 36 patients considered high risk for dislocation undergoing revision THA with DM constructs; similar to this study, the dislocation was closed reduced and successfully managed nonoperatively. Three patients in their series were revised for constrained liner dislocations, none of which redislocated. In patients at high risk of dislocation despite multiple failed surgical attempts to obtain a stable prosthetic hip, DM constructs not only allow enhanced stability, but also allow the option of treating repeat dislocations with closed reduction and bracing rather than necessitating urgent surgical intervention as is often the case in most dislocated constrained liners.
The treatment of recurrent instability after revision THA for instability remains a challenge, especially in patients with several risk factors for redislocation who have undergone multiple prior surgeries in an attempt to achieve prosthetic stability. Dislocation of constrained liners can occur in up to 30% of patients [4, 6, 7, 9, 23] and dislocated constrained liners typically result in urgent surgical intervention secondary to broken locking mechanisms and/or the inability to close reduce a dislocation. In this small, short-term analysis, revision of dislocated constrained liners to a DM construct in these high-risk patients may represent a reasonable option of achieving prosthetic stability through a different mechanism. The option of closed reducing repeat dislocations in extremely high-risk patients with underlying neuromuscular disorders after multiple failed surgical attempts to achieve hip stability is attractive. Longer followup of this series and larger cohorts will be required to demonstrate the durability of this approach.
Footnotes
The authors’ institution has received royalties from DePuy (Warsaw, IN, USA), DJO Global (Vista, CA, USA), and Zimmer Biomet (Warsaw, IN, USA); however, no funding was relevant to the present research.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Berry DJ, von Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2456–2463. [DOI] [PubMed] [Google Scholar]
- 2.Carter AH, Sheehan EC, Mortazavi SM, Purtill JJ, Sharkey PF, Parvizi J. Revision for recurrent instability: what are the predictors of failure? J Arthroplasty. 2011;26:46–52. [DOI] [PubMed] [Google Scholar]
- 3.Carulli C, Macera A, Matassi F, Civinini R, Innocenti M. The use of a dual mobility cup in the management of recurrent dislocations of hip hemiarthroplasty. J Orthop Traumatol. 2016;17:131–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chalmers BP, Arsoy D, Sierra RJ, Lewallen DG, Trousdale RT. High failure rate of modular exchange with a specific design of a constrained liner in high-risk patients undergoing revision total hip arthroplasty. J Arthroplasty. 2015;31:1963–1969. [DOI] [PubMed] [Google Scholar]
- 5.Clavé A, Maurer D, Tristan L, Dubrana F, Lefèvre C, Pandit H. Midterm survivorship of the Lefèvre constrained liner: a consecutive multisurgeon series of 166 cases. J Arthroplasty. 2016;31:1970–1978. [DOI] [PubMed] [Google Scholar]
- 6.Della Valle CJ, Chang D, Sporer S, Berger RA, Rosenberg AG, Paprosky WG. High failure rate of a constrained acetabular liner in revision total hip arthroplasty. J Arthroplasty. 2005;20:103–107. [DOI] [PubMed] [Google Scholar]
- 7.Fricka KB, Marshall A, Paprosky WG. Constrained liners in revision total hip arthroplasty: an overuse syndrome. In the affirmative. J Arthroplasty. 2006;21:121–125. [DOI] [PubMed] [Google Scholar]
- 8.Grazioli A, Ek ET, Rüdiger HA. Biomechanical concept and clinical outcome of dual mobility cups. Int Orthop. 2012;36:2411–2418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guyen O, Lewallen DG, Cabanela ME. Modes of failure of Osteonics constrained tripolar implants: a retrospective analysis of forty-three failed implants. J Bone Joint Surg Am. 2008;90:1553–1560. [DOI] [PubMed] [Google Scholar]
- 10.Jo S, Jimenez Almonte JH, Sierra RJ. The cumulative risk of re-dislocation after revision THA performed for instability increases close to 35% at 15 years. J Arthroplasty. 2015;30:1177–1182. [DOI] [PubMed] [Google Scholar]
- 11.Khoury JI, Malkani AL, Adler EM, Markel DC. Constrained acetabular liners cemented into cages during total hip revision arthroplasty. J Arthroplasty. 2010;25:901–905. [DOI] [PubMed] [Google Scholar]
- 12.Ko LM, Hozack WJ. The dual mobility cup: what problems does it solve? Bone Joint J. 2016;98:60–63. [DOI] [PubMed] [Google Scholar]
- 13.Munro JT, Vioreanu MH, Masri BA, Duncan CP. Acetabular liner with focal constraint to prevent dislocation after THA. Clin Orthop Relat Res. 2013;471:3883–3890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Odland AN, Sierra RJ. Intraprosthetic dislocation of a contemporary dual-mobility design used during conversion THA. Orthopedics. 2014;37:e1124–1128. [DOI] [PubMed] [Google Scholar]
- 15.Parvizi J, Morrey BF. Bipolar hip arthroplasty as a salvage treatment for instability of the hip. J Bone Joint Surg Am. 2000;82:1132–1139. [DOI] [PubMed] [Google Scholar]
- 16.Plummer DR, Christy JM, Sporer SM, Paprosky WG, Della Valle CJ. Dual-mobility articulations for patients at high risk for dislocation. J Arthroplasty. 2016;31:131–135. [DOI] [PubMed] [Google Scholar]
- 17.Prudhon JL, Ferreira A, Verdier R. Dual mobility cup: dislocation rate and survivorship at ten years of follow-up. Int Orthop. 2013;37:2345–2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salassa T, Hoeffel D, Mehle S, Tatman P, Gioe TJ. Efficacy of revision surgery for the dislocating total hip arthroplasty: report from a large community registry. Clin Orthop Relat Res. 2014;472:962–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sikes C Van, Lai LP, Schreiber M, Mont MA, Jinnah RH, Seyler TM. Instability after total hip arthroplasty. Treatment with large femoral heads vs constrained liners. J Arthroplasty. 2008;23:59–63. [DOI] [PubMed] [Google Scholar]
- 20.Simian E, Chatellard R, Druon J, Berhouet J, Rosset P. Dual mobility cup in revision total hip arthroplasty: dislocation rate and survival after 5 years. Orthop Traumatol Surg Res. 2015;101:577–581. [DOI] [PubMed] [Google Scholar]
- 21.Snir N, Park BK, Garofolo G, Marwin SE. Revision of failed hip resurfacing and large metal-on-metal total hip arthroplasty using dual-mobility components. Orthopedics. 2015;38:369–374. [DOI] [PubMed] [Google Scholar]
- 22.Sonohata M, Waewsawangwong W, Goodman SB. Successful closed reduction of a dislocated constrained total hip arthroplasty: a case report and literature review. Open Orthop J. 2012;6:211–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Su EP, Pellicci PM. The role of constrained liners in total hip arthroplasty. Clin Orthop Relat Res. 2004;420:122–129. [DOI] [PubMed] [Google Scholar]
- 24.van Heumen M, Heesterbeek PJ, Swierstra BA, Van Hellemondt GG, Goosen JH. Dual mobility acetabular component in revision total hip arthroplasty for persistent dislocation: no dislocations in 50 hips after 1-5 years. J Orthop Traumatol. 2015;16:15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wegrzyn J, Tebaa E, Jacquel A, Carret JP, Béjui-Hugues J, Pibarot V. Can dual mobility cups prevent dislocation in all situations after revision total hip arthroplasty? J Arthroplasty. 2015;30:631–640. [DOI] [PubMed] [Google Scholar]
- 26.Wetters NG, Murray TG, Moric M, Sporer SM, Paprosky WG, Della Valle CJ. Risk factors for dislocation after revision total hip arthroplasty. Clin Orthop Relat Res. 2012;471:410–416. [DOI] [PMC free article] [PubMed] [Google Scholar]