Abstract
Background
Emergency department (ED) visits after elective surgical procedures are a potential target for interventions to reduce healthcare costs. More than 1 million total joint arthroplasties (TJAs) are performed each year with postsurgical ED utilization estimated in the range of 10%.
Questions/purposes
We asked whether (1) outpatient orthopaedic care was associated with reduced ED utilization and (2) whether there were identifiable factors associated with ED utilization within the first 30 and 90 days after TJA.
Methods
An analysis of adult TRICARE beneficiaries who underwent TJA (2006-2014) was performed. TRICARE is the insurance program of the Department of Defense, covering > 9 million beneficiaries. ED use within 90 days of surgery was the primary outcome and postoperative outpatient orthopaedic care the primary explanatory variable. Patient demographics (age, sex, race, beneficiary category), clinical characteristics (length of hospital stay, prior comorbidities, complications), and environment of care were used as covariates. Logistic regression adjusted for all covariates was performed to determine factors associated with ED use.
Results
We found that orthopaedic outpatient care (odds ratio [OR], 0.73; 95% confidence interval [CI], 0.68-0.77) was associated with lower odds of ED use within 90 days. We also found that index hospital length of stay (OR, 1.07; 95% CI, 1.04-1.10), medical comorbidities (OR, 1.16; 95% CI, 1.08-1.24), and complications (OR, 2.47; 95% CI, 2.24-2.72) were associated with higher odds of ED use.
Conclusions
When considering that at 90 days, only 3928 patients sustained a complication, a substantial number of ED visits (11,486 of 15,414 [75%]) after TJA may be avoidable. Enhancing access to appropriate outpatient care with improved discharge planning may reduce ED use after TJA. Further research should be directed toward unpacking the situations, outside of complications, that drive patients to access the ED and devise interventions that could mitigate such behavior.
Level of Evidence
Level III, therapeutic study.
Introduction
In surgical care, emergency department (ED) visits represent either a postsurgical adverse event or a discontinuity in appropriate postoperative management; they may add substantial cost to the patient and healthcare system [10, 17]. Moreover, with the advent of risk-based reimbursement programs and penalties for hospital readmission, the financial responsibility associated with ED visits after surgery has largely shifted to the healthcare organizations and surgeons providing care [5, 19].
THA and TKA account for a substantial amount of healthcare expenditures with more than 1 million procedures performed annually at a cost of nearly USD 19 billion [2]. Moreover, although these procedures are frequently performed in Medicare patients, the fastest growing population receiving joint arthroplasty is now younger than age 65 years. Joint replacements have been prime targets for both bundled payment initiatives and readmission penalties in recent years [5, 9-12, 17, 18]. The proportion of patients readmitted after THA and TKA has been reported to be 5% to 10% and the risk factors associated with these events have been characterized [1, 11, 12, 17, 18]. However, the association of orthopaedic outpatient care with ED utilization within the 90-day period after joint arthroplasty has not been extensively studied. We believe that outpatient orthopaedic visits can be viewed as a surrogate for continuity of care after hospital discharge and may be associated with a reduction in the need for patients to access ED services.
In this context, we used insurance claims data to answer two questions. We asked whether (1) outpatient orthopaedic care was associated with reduced ED utilization and (2) whether there were identifiable factors associated with ED utilization within the first 30 and 90 days after TJA.
Patients and Methods
For this analysis, we used TRICARE insurance claims data (2006–2014), which are maintained by the Military Health System Data Repository. TRICARE is the healthcare program of the Department of Defense that is responsible for providing healthcare coverage to active-duty and retired uniformed services personnel and their families. Currently, the program provides coverage to nearly 9.5 million individuals through military and civilian hospitals across the United States [3, 4, 14, 20]. This system is independent of Veterans Administration hospitals and military healthcare facilities in combat theaters. Prior studies have used TRICARE data to study healthcare outcomes in trauma, surgical, and medical conditions and the demographic profile of this population broadly resembles that of the US population younger than age 65 years [3, 4, 14-16]. Before commencement, this study received an exempt determination from the Partners Human Research Committee. All data were deidentified.
Claims were queried for adult patients (18-64 years) with a primary procedure code for primary THA and TKA (International Classification of Diseases, 9th Revision [ICD-9] 81.51 and 81.54) between 2006 and 2014. We excluded patients older than 65 years of age and those who were Medicare-eligible. This approach allowed complete case ascertainment because any services billed to Medicare and not TRICARE would not be captured in our data set.
Patients included in the analysis had their claims abstracted for demographics (age, race, sex, sponsor rank, and beneficiary category), clinical characteristics (Charlson comorbidity index [CCI] [6], length of stay [LOS], index surgical procedure, and complications), and healthcare use (orthopaedic outpatient care visits and ED visits) within 90 days of the date of surgery. TRICARE documents outpatient care services through provider/specialty-specific taxonomy codes for care delivered in both military and civilian settings. Taxonomy codes specific to orthopaedic surgery outpatient care (see Appendix, Supplemental Digital Content 1) were used to survey for use of these services within 90 days of the surgical intervention.
Race was categorized as white, black, Asian, and other based on patient self-report. When race information was missing, we used reweighted estimating equations, an effective method to reduce bias introduced by missing race information [8]. In this approach, we calculated the probability of reported race using a logistic regression model, and we applied the inverse of this predicted probability as a survey weight in the adjusted analyses.
We divided the CCI into three categories (0, 1, > 1). Complications within 30 and 90 days after discharge were identified using a previously published ICD-9-based algorithm [3, 14], which captured infectious, wound-related, cardiovascular, neurologic, urologic, and respiratory complications.
The primary independent variables were 30- and 90-day orthopaedic outpatient visits, whether scheduled or unscheduled. ED visits within the first 30 and 90 days after discharge were established as the primary dependent variable. Secondary independent variables consisted of age, race, sex, CCI, LOS, and the development of postsurgical complications.
We calculated the incidence of ED visits, complications, and outpatient orthopaedic visits at the 30- and 90-day intervals. The top five diagnoses, by ICD-9 code, associated with ED and orthopaedic outpatient visits were also evaluated.
We used multivariable logistic regression models, adjusted for demographic and clinical characteristics, to identify factors associated with ED use at 30- and 90-day intervals. The interaction between race and sponsor rank was controlled for in all statistical testing. Sensitivity analyses based on the same parameters but excluding active-duty personnel and a complete case assessment limited to individuals with a reported race were also performed to confirm the applicability of these findings to the general population.
All statistical analyses were conducted using Stata, Version 14.1 (StataCorp, College Station, TX, USA), and statistical significance was set at odds ratios (ORs) with 95% confidence intervals (CIs) exclusive of 1.0. Data analysis was performed between September 10, 2017, and March 17, 2018.
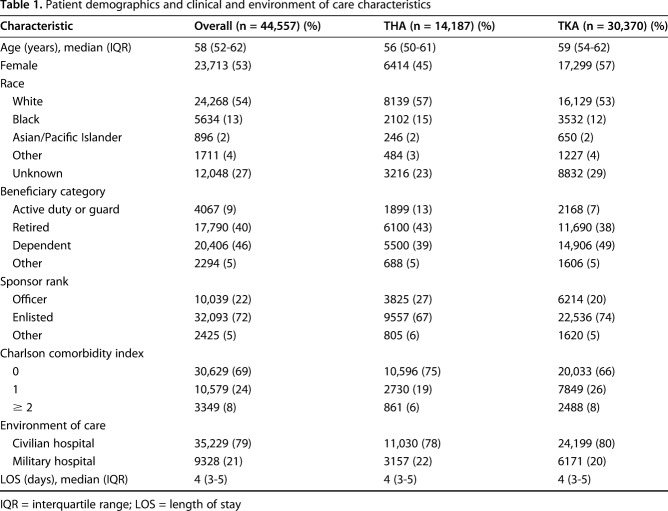
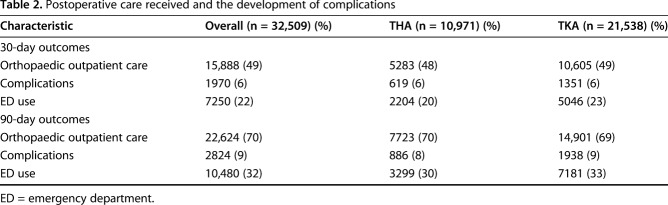
From 2006 to 2014, 44,557 patients met our inclusion criteria. Of these, 14,187 underwent THA and 30,370 underwent TKA. The median age of the cohort was 58 years (interquartile range [IQR], 52-62 years; Table 1). Most patients undergoing both THA (78% [11,030 of 14,187]) and TKA (80% [24,199 of 30,370]) received the index procedure at a civilian hospital. For both cohorts, the median LOS was 4 days. The proportion of patients who received outpatient orthopaedic care after hospital discharge was 46% (20,445 of 44,557) within 30 days and 67% (29,744 of 44,557) at 90 days (Table 2). The overall complication rate was 6% (2710 of 44,557) and 9% (3928 of 44,557) at 30 and 90 days, respectively.
Table 1.
Patient demographics and clinical and environment of care characteristics
Table 2.
Postoperative care received and the development of complications
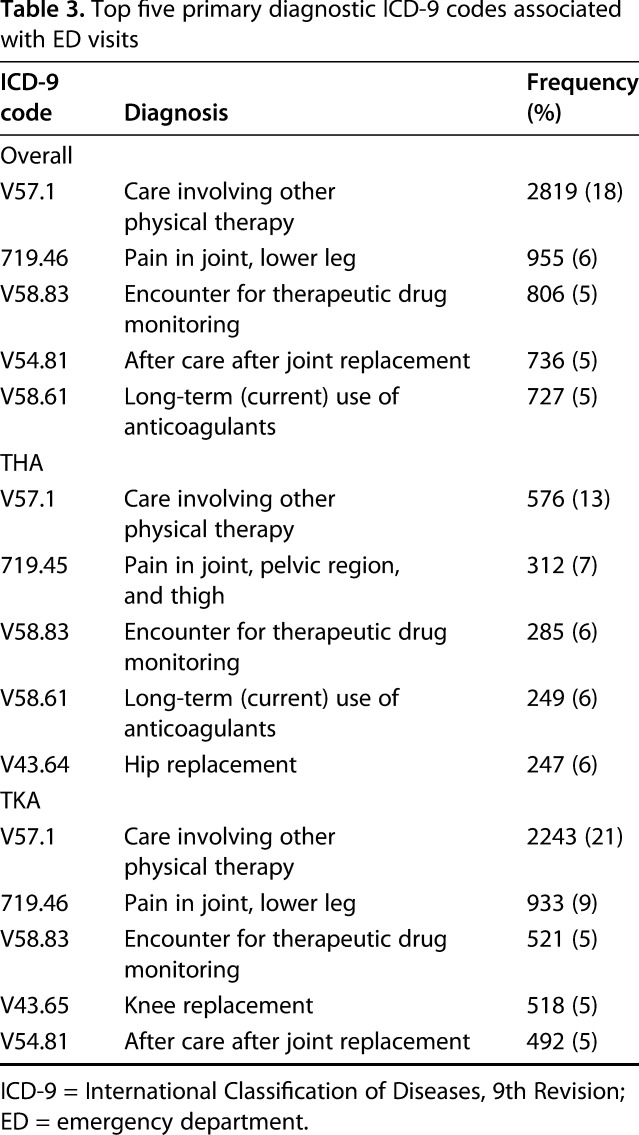
We found that 24% (10,661 of 44,557) of patients visited the ED within 30 days of discharge and 35% (15,414 of 44,557) were seen in the ED within 90 days (Fig. 1). The most common ICD-9 diagnosis associated with ED use within the study period was V57.1: care involving other physical therapy (18% [2819/15,414]; Table 3). Pain was the second most common primary diagnosis (6% [955 of 15,414]). Encounters for therapeutic drug monitoring (806 of 15,414) and long-term use of anticoagulants (727 of 15,414) each accounted for 5% of the diagnoses associated with ED utilization.
Fig. 1.
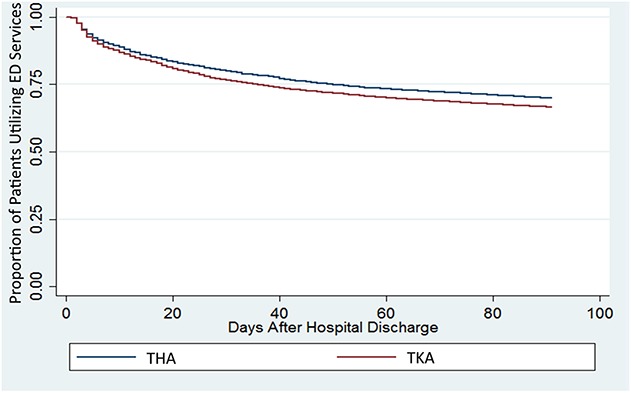
The proportion of patients using ED services within 90 days of postsurgical discharge after THA or TKA is shown.
Table 3.
Top five primary diagnostic ICD-9 codes associated with ED visits
The most commonly encountered codes associated with the use of orthopaedic outpatient care (19,355 of 29,744 [65%]) were nonspecific or associated with aftercare (v54.81, v43.65, 799.89). Codes for joint pain (719.46; 2134 of 29,744 [7%]) and joint osteoarthritis (715.16; 2056 of 29,744 [7%]) were also among the most frequently documented reasons for outpatient orthopaedic visits.
Results
Association Between Outpatient Orthopaedic Care and 30- and 90-day ED Use
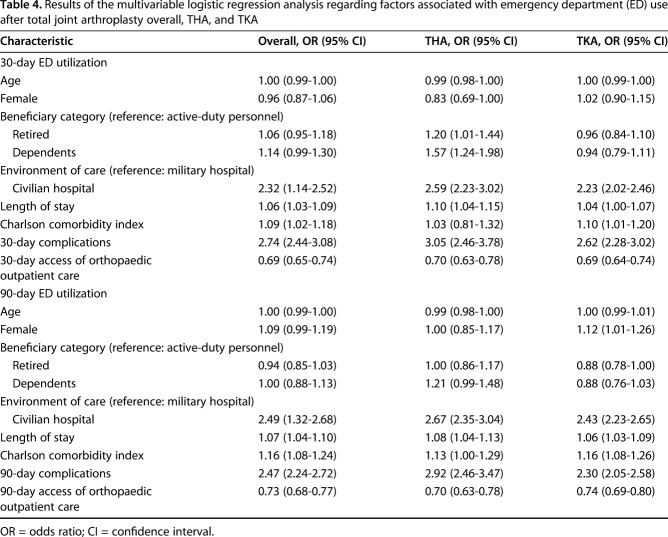
After controlling for potential confounding variables such as age, medical comorbidities, and the environment of care, we found that outpatient orthopaedic care was associated with reduced ED utilization over both the 30- and 90-day postoperative periods (Table 4). In the 30-day period, accessing outpatient orthopaedic care resulted in a 31% reduction in the odds of ED utilization (OR, 0.69; 95% CI, 0.65-0.74), whereas at 90 days, there was a 27% reduction in the odds of ED use (OR, 0.73; 95% CI, 0.68-0.77). This was unchanged in the sensitivity tests that limited consideration solely to nonactive-duty individuals (see Appendix, Supplemental Digital Content 2) as well as in the complete case assessment (30-day OR, 0.68, 95% CI, 0.64-0.71; 90-day OR, 0.71; 95% CI, 0.68-0.75).
Table 4.
Results of the multivariable logistic regression analysis regarding factors associated with emergency department (ED) use after total joint arthroplasty overall, THA, and TKA
Factors Associated With 30- and 90-day ED Use After TJA
After controlling for potential confounding variables such as patient age, comorbidities, and the environment of care (Table 4), we found that overall, care at civilian hospitals (OR, 2.32; 95% CI, 1.14-2.52), longer LOS (OR, 1.06; 95% CI, 1.03-1.09), increased CCI (OR, 1.09; 95% CI, 1.02-1.18), and development of complications (OR, 2.74; 95% CI, 2.44-3.08) were associated with a higher likelihood of ED use at 30 days. These findings remained apparent for the 90-day period as well: care at civilian hospitals (OR, 2.49; 95% CI, 1.32-2.68), longer LOS (OR, 1.07; 95% CI, 1.04-1.10), increased CCI (OR, 1.16; 95% CI, 1.08-1.24), and development of complications (OR, 2.47; 95% CI, 2.24-2.72). These findings were also unchanged in the sensitivity analyses performed. When the interaction between race and sponsor rank was accounted for, there was no significant association for race and ED utilization at 30 (OR, 1.25; 95% CI, 0.99-1.58) or 90 days (OR, 1.06; 95% CI, 0.87-1.29).
Discussion
In the current healthcare environment, stakeholders and payers have made a concerted effort to contain healthcare spending and improve efficiency [5, 9, 10, 19]. Outside of treatment for postoperative complications, or as a means of facilitating readmission, utilization of the ED after surgery is expensive and frequently an inefficient use of healthcare resources [1, 10, 17]. As a proxy for continuity of care after surgery, we believe that access of outpatient orthopaedic services can effectively mitigate the need for patients to seek treatment in the ED. Although prior research has focused on characterizing clinical and sociodemographic characteristics associated with ED use after TJA [1, 7, 17, 18], the ability of orthopaedic outpatient care to reduce such behavior has not been extensively studied. In this study, we found that orthopaedic outpatient care decreased the likelihood of ED utilization at both 30 and 90 days after surgery. Furthermore, we also determined that a number of clinical characteristics, including index hospital LOS, medical comorbidities, and the development of complications, increased the potential for patients to return to the ED.
We recognize that this study contains several limitations. Foremost, this analysis was performed using TRICARE, which provides care to military service members, retirees, and their dependents. Approximately 21% (9328 of 44,557) of the population was also treated at a Department of Defense healthcare facility. The extent to which healthcare delivery differs within this population may impair the translational capacity of our results. For example, the index hospital LOS reported for our population was slightly longer than in other contemporary work, the percentage of patients utilizing the ED was higher, and some of the diagnoses associated with ED use were different than those reported elsewhere [1, 7, 11, 12, 17, 18]. As a claims-based study, we may more reliably identify ED visits than investigations that rely on statewide or hospital registries. Although we did adjust for LOS in our analyses, we cannot characterize the extent to which underlying differences in ED utilization practices could influence the generalizability of these findings. We also recognize that our determinations derive from a retrospective review of claims data. The original purpose of these data was for adjudication of healthcare claims and remuneration rather than research. The capacity to establish firm clinical recommendations and determine causality is thus limited. Moreover, our reliance on claims restricts the ability to obtain nuanced information, including discharge plans, ease of patient access to outpatient care services as well as severity and duration of symptoms that prompted a return to the ED. ED diagnoses alone are insufficient to understand the clinical picture that culminated in a decision to access the ED. Although useful to suggest opportunities for further study, additional research using more clinically granular data would be necessary to generate appropriate interventions capable of reducing ED utilization.
Furthermore, we cannot detail why only 67% of our study population had received documented outpatient orthopaedic care at 90 days after surgery. We relied on TRICARE-provided taxonomy codes to identify receipt of outpatient orthopaedic services. Some patients may have been directed to or chose to followup with primary care providers. Others may have received outpatient orthopaedic care that was not reported to the insurer. The use of orthopaedic services not reported to TRICARE would be missed, and thus the use of outpatient services could be underestimated to some extent. The extent of this phenomenon cannot be quantified nor can its potential impact on our study findings. Another limitation of this study could include the military affiliation of some patients, which might also influence the generalizability of study results. We seek to emphasize that TRICARE data have been widely used for surgical and nonsurgical research in the past with the population demographics of beneficiaries found to approximate those of the US general population younger than 65 years [3, 4, 13-15]. To further address this concern, we performed a sensitivity analysis that excluded any active-duty personnel. Importantly, the results of the sensitivity tests did not differ from the overall analysis. Given the age limitations associated with this study, which were necessary to ensure accurate documentation of surgical and outpatient services, we realize that the findings may not be completely translatable to the Medicare population.
Several studies have previously considered readmission after joint replacement, but relatively few have focused on ED utilization in the absence of readmissions. Using statewide registries, Trimba et al. [18] found that joint pain or limb swelling was the most common cause for accessing the ED after a joint replacement. Similar findings were reported in the work of Finnegan et al. [7] and the single-center study of Sibia et al. [17]. Interestingly, in the work of Sibia and colleagues, medication-related issues were the second most frequent cause of an unplanned ED visit [17]. Although Finnegan et al. theorized that improvements in postoperative care could mitigate the need for ED utilization after joint replacement [7], none of these studies evaluated the association between orthopaedic outpatient care and return visits to the ED. The top five diagnoses associated with an ED visit in our study represent inadequate pain control, the need for physical therapy, and the management of anticoagulants. In this context, the need for physical therapy suggests an inability to mobilize effectively or to be sufficiently functional in the postdischarge environment. The nature of our analysis prevented us from ascertaining the exact clinical circumstance surrounding ED use. However, based on the consideration of primary ED diagnosis codes, many of these encounters could have been managed in the outpatient setting with the appropriate care resources. When considering that at 90 days only 3928 patients sustained a complication, a substantial number of ED visits (11,486 of 15,414 [75%]) appears to be avoidable.
Prior work has investigated clinical and sociodemographic characteristics associated with ED utilization after TJA [1, 7, 11, 17, 18]. Perhaps not surprisingly, as encountered in this study, one of the main drivers of unplanned ED visits is the development of postoperative complications [1, 17, 18]. Outside of this, increased medical comorbidities and a patient’s body mass index have also been associated with the likelihood of an unplanned return to the ED and readmission [7, 12, 17, 18]. Finnegan et al. reported that Medicare or Medicaid insurance were also associated with ED use after TJA [7]. The TRICARE population enjoys universal healthcare coverage irrespective of vocation, work status, or educational level [13-15], which eliminates our ability to consider such factors in the present work. Although Adelani et al. [1] and Finnegan et al. [7] both reported black race to be associated with ED utilization after joint replacement, we did not encounter a significant association once we accounted for other sociodemographic characteristics in our cohort. This may reflect the fact that other sociodemographic factors, including insurance status, ability to navigate the healthcare system, and healthcare segregation, are often confounded by race.
In conclusion, this study found that accessing orthopaedic outpatient care effectively reduced the likelihood of ED utilization within the 90-day period after joint replacement. Our findings have immediate implications for clinical practice and are of clear interest to surgical providers, hospitals, patients, and third-party payers. They indicate that proper coordination and communication regarding postdischarge services may reduce ED use after discharge. The large sample size, the fact that patients are drawn from centers across the United States, and the diverse demographic, educational, vocational, and functional characteristics of the population insured through TRICARE [4, 13-16] may allow the results presented here to be more readily translated to clinical practice, but further research is clearly required. The need for a more granular assessment of the scenarios leading to ED visits is suggested by our work and this could be addressed using a prospective, mixed-methods design. Additionally, a study into specific interventions that ensure access to postoperative outpatient care, improve discharge instruction comprehension, and access to postoperative care resources could actualize benefits that are presently only suggested in our study findings.
Footnotes
This research was supported by a grant (Principal Investigators: TK, AHH) from the Department of Defense and the Henry M. Jackson Foundation of the Department of Defense. The following authors receive partial salary support from the Comparative Effectiveness and Provider Induced Demand Collaboration grant: MAC, LMP, DJS, TK, AHH, AJS. One or more of the authors certify that he (MAC, DJS, AHH, AJS) or she (LMP, TK), or a member of his or her immediate family, has received or may receive payments or benefits, during the study period, in the amount of USD 10,000 to USD 100,000 from the Henry M. Jackson Foundation of the Department of Defense (Bethesda, MD, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Adelani MA, Keller MR, Barrack RL, Olsen MA.the impact of hospital volume on racial differences in complications, readmissions, and emergency department visits following total joint arthroplasty. J Arthroplasty. 2018;33:309–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Table 105: Cost of hospital discharges with common hospital operating room procedures in nonfederal community hospitals, by age and selected principle procedure: United States. In: Health, United States, 2014. With a special feature on adults aged 55-64. Available at: http://www.cdc.gov/nchs/data/hus/hus14.pdf#105. Accessed November 14, 2017.
- 3.Chaudhary MA, Schoenfeld AJ, Harlow AF, Ranjit R, Chowdhury R, Sharma M, Nitzschke S, Koehlmoos T, Haider AH. Incidence and predictors of opioid prescription at discharge after traumatic injury. JAMA Surg. 2017;152:930–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaudhary MA, Sharma M, Scully RE, Sturgeon DJ, Koehlmoos T, Haider AH, Schoenfeld AJ. Universal insurance and an equal access healthcare system eliminate disparities for black patients after traumatic injury. Surgery. 2018;163:651–656. [DOI] [PubMed] [Google Scholar]
- 5.Chen LM, Meara E, Birkmeyer JD. Medicare's bundled payments for care improvement (BPCI) initiative: expanding enrollment suggests potential for large impact. Am J Manag Care. 2015;21:814. [PMC free article] [PubMed] [Google Scholar]
- 6.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. [DOI] [PubMed] [Google Scholar]
- 7.Finnegan MA, Shaffer R, Remington A, Kwong J, Curtin C, Hernandez-Boussard T. Emergency department visits following elective total hip and knee replacement surgery: identifying gaps in continuity of care. J Bone Joint Surg Am. 2017;99:1005–1012. [DOI] [PubMed] [Google Scholar]
- 8.Henry AJ, Hevelone ND, Lipsitz S, Nguyen LL. Comparative methods for handling missing data in large databases. J Vasc Surg. 2013;58:1353–1359. [DOI] [PubMed] [Google Scholar]
- 9.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA. 2013;309:342–343. [DOI] [PubMed] [Google Scholar]
- 10.Kocher KE, Nallamothu BK, Birkmeyer JD, Dimick JB. Emergency department visits after surgery are common for Medicare patients, suggesting opportunities to improve care. Health Aff (Millwood). 2013;32:1600–1607. [DOI] [PubMed] [Google Scholar]
- 11.Raines BT, Ponce BA, Reed RD, Richman JS, Hawn MT. Hospital acquired conditions are the strongest predictor for early readmission: an analysis of 26,710 arthroplasties. J Arthroplasty. 2015;30:1299–1307. [DOI] [PubMed] [Google Scholar]
- 12.Ricciardi BF, Oi KK, Daines SB, Lee Y-Y, Joseph AD, Westrich GH. Patient and perioperative variables affecting 30-day readmission for surgical complications after hip and knee arthroplasties: a matched cohort study. J Arthroplasty. 2017;32:1074–1079. [DOI] [PubMed] [Google Scholar]
- 13.Schoenfeld AJ, Goodman GP, Burks R, Black MA, Nelson JH, Belmont PJ., Jr The influence of musculoskeletal conditions, behavioral health diagnoses, and demographic factors on injury-related outcome in a high-demand population. J Bone Joint Surg Am. 2014;96:e106. [DOI] [PubMed] [Google Scholar]
- 14.Schoenfeld AJ, Jiang W, Harris MB, Cooper Z, Koehlmoos T, Learn PA, Weissman JS, Haider AH. Association between race and postoperative outcomes in a universally insured population versus patients in the state of California. Ann Surg. 2017;266:267–273. [DOI] [PubMed] [Google Scholar]
- 15.Schoenfeld AJ, Makanji H, Jiang W, Koehlmoos T, Bono CM, Haider AH. is there variation in procedural utilization for lumbar spine disorders between a fee-for-service and salaried healthcare system? Clin Orthop Relat Res. 2017;475:2838–2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scully RE, Schoenfeld AJ, Jiang W, Lipsitz S, Chaudhary MA, Learn PA, Koehlmoos T, Haider AH, Nguyen LL. Defining optimal length of opioid pain medication prescription after common surgical procedures. JAMA Surg. 2018;153:37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sibia US, Mandelblatt AE, Callanan MA, MacDonald JH, King PJ. Incidence, risk factors, and costs for hospital returns after total joint arthroplasties. J Arthroplasty. 2017;32:381–385. [DOI] [PubMed] [Google Scholar]
- 18.Trimba R, Laughlin RT, Krishnamurthy A, Ross JS, Fox JP. Hospital-based acute care after total hip and knee arthroplasty: implications for quality measurement. J Arthroplasty. 2016;31:573–578. [DOI] [PubMed] [Google Scholar]
- 19.Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19:47–59. [PMC free article] [PubMed] [Google Scholar]
- 20.Zogg CK, Jiang W, Chaudhary MA, Scott JW, Shah AA, Lipsitz SR, Weissman JS, Cooper Z, Salim A, Nitzschke SL, Nguyen LL, Helmchen LA, Kimsey L, Olaiya ST, Learn PA, Haider AH. Racial disparities in emergency general surgery: do differences in outcomes persist among universally insured military patients? J Trauma Acute Care Surg. 2016;80:764–777. [DOI] [PubMed] [Google Scholar]