Abstract
Background
Given that the pelvis is the pedestal on which the spine lies, its morphology has been observed to be associated with specific sagittal spinal shapes and should therefore be taken into account when dealing with pathologic conditions of the spine. However, the exact relationship between the pelvic morphology and lumbar lordosis still remains poorly defined. We hypothesized that the shape of the lumbar lordosis and its relationship with the pelvis could be described using anatomic parameters, independently of posture.
Questions/purposes
(1) What is the variation of lumbar segmental lordosis in an asymptomatic adult population? (2) Is there an association between increasing magnitude of pelvic incidence (PI) and segmental lordosis? (3) How does the position of the apex of lordosis change with increasing magnitude of PI value?
Methods
This retrospective study used data drawn from a longitudinally maintained database; between March 2014 and January 2015, 119 asymptomatic volunteers between 18 and 79 years old were enrolled in the study. Mean age was 51 years; there were 81 women and 38 men. Both segmental and cumulative lordosis were measured and used to describe the shape of the lumbar spine. We defined cumulative lordosis as the angle between L1 and S1, proximal lordosis as the angle between L1 and the superior endplate of L4, and distal lordosis as the angle between the superior endplates of L4 and S1. PI is defined as the angle between the line passing through the center of the femoral head and the center of the sacral endplate and a line perpendicular to the sacral endplate. Pearson’s correlation was performed to analyze the relationship among PI, proximal and distal lordosis. Stratification by PI was performed (low, < 45°; average, 45°-60°; and high, > 60°) and the proportions of distal and proximal lordosis were then compared using an analysis of variance test.
Results
In the whole cohort, proximal lordosis accounted for 38% of total lordosis, whereas distal lordosis accounted for 62%. PI revealed a positive correlation with proximal lordosis (r = 0.546; p < 0.001). However, there was no correlation with distal lordosis (r = 0.087; p = 0.346). Stratification by PI showed that proximal lordosis increased across PI groups (16.6° [± 10] versus 21.6° [± 9] versus 30.1° [± 9]; p < 0.001), whereas distal lordosis remained relatively constant (34.8° [± 8] versus 36.7° [± 7] versus 35.9° [± 10]; p = 0.581). Apex position was overall more proximal as PI increased (r = -0.199; p = 0.034).
Conclusions
Our study demonstrated that PI influences only the proximal part of the lordosis, but not the distal part in an asymptomatic adult population. The proximal part of the lumbar spine had the most variability across individuals and appeared to accommodate to pelvic morphology (incidence). Further studies using a larger cohort size are encouraged not only to refine this relationship, but also to investigate the effect of restoration of normal lordotic shape of the lumbar spine on the functional outcomes after spinal fusion.
Clinical Relevance
Our findings may be useful for surgical planning in an era of patient-specific care. The findings suggest that surgeons should aim for a patient-specific lumbar shape rather than simple global lordosis matched to the PI.
Introduction
In the past two decades, the role of sagittal alignment in pathologic conditions has been repeatedly demonstrated. One of the main parameters used to assess the role of the pelvis in sagittal alignment is the pelvic incidence (PI). This parameter reflects the sagittal orientation of the sacral endplate within the pelvis with regard to the femoral heads (Fig. 1). It is now established that sagittal alignment is correlated to health-related quality-of-life scores (HRQoL) [2, 5, 7, 10]. In adult spinal deformity, previous studies have highlighted that postoperative residual sagittal malalignment results in lower HRQoL, higher revision rates, and residual pain [5, 7]. In degenerative conditions, it has been shown that the correction of sagittal malalignment, quantified by the pelvic incidence-lumbar lordosis (PI-LL) mismatch, is a predictor of success after short-segment fusions [2, 10]. On the other hand, a greater postoperative PI-LL mismatch leads to a higher risk of adjacent-segment disease and decreased HRQoL scores [12, 14].
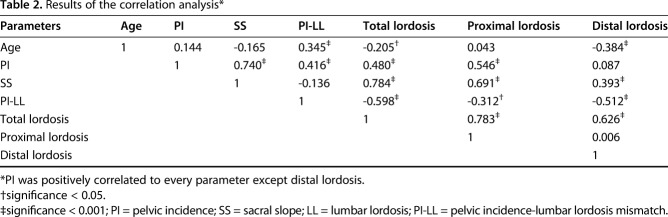
Fig. 1.
List detailing radiographic parameters. Total lordosis was defined as the angle between the superior endplate of L1 and the superior endplate of S1. Proximal lordosis was defined as the angle between the superior endplate of L1 to the superior endplate of L4. Distal lordosis was defined as the angle between the superior endplate of L4 and the superior endplate of S1. Segmental lordosis was defined as the sagittal angle between the superior endplate at a given level and the superior endplate of the level below. The thoracolumbar junction was the angle between the superior endplate of T10 and the inferior endplate of L2. Cumulative lordosis was defined as the sagittal angle between the superior endplate at a given level and the superior endplate of S1. The apex of lordosis was calculated according to the tangential radiographic assessment of the lumbar lordosis method [6].
The relationship between pelvic morphology and the spine has been well established [4, 9]. A chain of correlation exists among PI, pelvic tilt, sacral slope, and lumbar lordosis. Because the sacral slope is the pedestal of lumbar lordosis, as sacral slope becomes more vertical, lumbar lordosis will increase accordingly; thus, sacrum orientation will mediate the overall shape of the lumbar spine. Although sacral slope represents the connection between the pelvis and lumbar lordosis, PI quantifies anatomic pelvis morphology, defining sacrum orientation within the pelvis. Because PI is an anatomic parameter, it does not change with sagittal pelvis rotation. In the past, the values of lumbar lordosis and PI have been demonstrated to show a strong positive association [4].
However, the relationship between pelvic morphology and the detailed contour of the lumbar lordosis remains unclear. Been et al. [3] demonstrated that the lordosis within each lumbar level was not homogenous, but the authors did not investigate the potential influence of the pelvis. Laouissat et al. [8] and Roussouly et al. [13] presented the variation in lumbar, sagittal shape in the normative population. They proposed a classification based on the sacral slope and the apex position of lordosis and defined five morphologic types. With their method, they divided the lordosis into an upper and lower arc, separated by a horizontal line, with the lower arc equal to the sacral slope. They demonstrated that higher values of PI, and in turn, higher sacral slope, are strongly associated with larger lumbar lordosis in the distal segments (L4-L5, L5-S1). In other words, the distal lumbar lordosis showed a variation across the PI spectrum. They concluded that the PI was the best parameter to describe lordosis shape. It appears that taking the horizontal plane as a reference is a major limitation. Spinal conditions are likely to induce several changes in spinal alignment, and pelvic position (tilt) will therefore change to compensate for spinal malalignment. It is thus misleading to use this classification in the setting of spinal pathology. To the best of our knowledge, the independent impact of pelvic morphology on the distribution of lumbar lordosis has not been clarified based on previous work.
In this study, we asked: (1) What is the variation of lumbar segmental lordosis in an asymptomatic adult population? (2) Is there an association between increasing magnitude of PI and segmental lordosis? (3) How does the position of the apex of lordosis change with increasing magnitude of PI value?
Patients and Methods
After institutional review board approval, we conducted a retrospective review of a longitudinally maintained database of asymptomatic volunteers ages 18 and 79 years with no neck, back, or leg pain from March 2014 to January 2015. Individuals with a history of prior spine surgery, previous hip or knee arthroplasty, or lower limb realignment (because of trauma or osteotomy) were excluded from the study as were patients with disabling back pain, degenerative spine conditions requiring intervention (physical therapy, corticosteroid injection), patients who could not walk, and those with a history of neuromuscular or inflammatory conditions and pregnancy. Informed consent was obtained from each individual before study enrollment. In total, 119 asymptomatic volunteers were recruited at a single center (Washington University School of Medicine, St Louis, MO, USA). Mean age was 50.7 years old (± 17; range, 22-78 years). There were 81 women and 38 men (sex ratio = 2.1:1).
Demographic parameters were collected: weight, height, and age. Standing full-body biplanar (AP and lateral) low-dose radiographs were taken (EOS Imaging, Paris, France). For radiographic acquisition, individuals were asked to stand naturally and then place their fists on their shoulders with mild shoulder flexion.
Two trained independent observers (RL, JCE) measured radiographic parameters using validated software (Spineview; ENSAM Laboratory of Biomechanics, Paris, France) [11]. The two observers evaluated all radiographs and reached consensus for every measurement. They measured the segmental lordosis, defined as the angle between the superior endplate at a given level and the superior endplate of the level below; as well as the cumulative lordosis, defined as the angle between the superior endplate at a given level and the superior endplate of S1. The total lordosis was defined as the angle between the superior endplate of L1 and the superior endplate of S1. The proximal lordosis was the angle between the superior endplate of L1 to the superior endplate of L4. The distal lordosis was the angle between the superior endplate of L4 and the superior endplate of S1. The thoracolumbar junction was assessed by the angle between the superior endplate of T10 and the inferior endplate of L2. Pelvic parameters were also measured (PI, pelvic tilt, and sacral slope). The lordosis apex was defined using the tangential radiographic assessment of the lumbar lordosis method [6]. To calculate the apex, first a line was drawn from the posterosuperior aspect of L1 to the posterosuperior aspect of S1. Subsequently, the perpendicular distance connecting the midpoint of the posterior wall of the vertebrae to the L1-S1 line was measured. The vertebral level with the greatest distance was then defined as the apex (Fig. 1).
Primary and Secondary Study Outcome Variables
To answer the first research question, the distribution of lordosis was assessed with the measurement of the segmental lordosis at each level of the lumbar spine. The influence of PI on the shape of the lumbar spine (question 2) was assessed with correlation analysis between PI value and proximal and distal lordosis. Further analysis involved stratification of our cohort into three groups by the PI value (low PI, < 45°; average PI, 45°–60°; high PI < 60°). Finally, the position of the apex of lordosis was measured and compared across three PI groups.
Statistical Analysis
We performed statistical analyses with SPSS (IBM, Chicago, IL, USA). Data are presented as mean ± SD. Comparison of means was performed using an analysis of variance. Post hoc analysis was performed using a Bonferroni correction. We assessed the relationship between parameters with Pearson correlation tests. The relationship of the proximal and distal lordosis with PI was analyzed using a linear stepwise regression through the origin. Stepwise multilinear regression was performed to assess the association of PI and age with the proximal and distal lordosis. For discrete values, comparisons were performed with a chi-square test. For all statistical tests, the significance threshold was set at p < 0.05.
Results
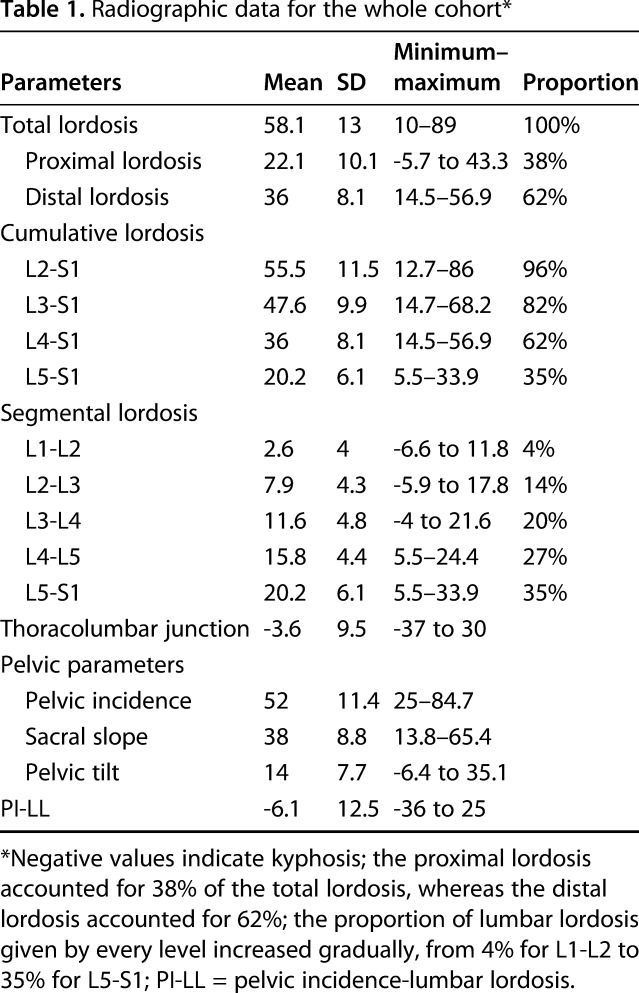
Variation of Lumbar Segmental Lordosis in Asymptomatic Adults
The mean lordosis was 58.1° (± 13; Table 1). The mean proximal lordosis was 22.1° (± 10.1°) and accounted for 38% of the total lordosis, whereas the mean distal lordosis was 36° (± 8.1) and accounted for 62% of the total lordosis. The proportion of lumbar lordosis given by every level increased gradually, from 4% for L1-L2 to 35% for L5-S1.
Table 1.
Radiographic data for the whole cohort*
Influence of PI Value on Segmental Lordosis
PI was correlated to proximal lordosis (r = 0.546; p < 0.001) (Fig. 2) but not to distal lordosis (r = 0.087; p = 0.346; Table 2). The proximal lordosis increased throughout the PI groups (17° [± 10] versus 22° [± 9] versus 30° [± 9], respectively; p < 0.001; Table 3), whereas the distal lordosis did not vary (35° [± 8] versus 37° [± 7] versus 36° [± 10], respectively; p = 0.581; Fig. 3). Post hoc analysis (Bonferroni) showed that proximal lordosis was different between PI groups (low PI versus average PI, 17° versus 22°, p = 0.03 [95% confidence interval {CI}, 0.3°-9.8°°]; low PI versus high PI, 17° versus 30°, p < 0.001 [95% CI, 7.7°-19.3°]; and average PI versus high PI, 22° versus 30° [95% CI, 3.3°-13.6°], p < 0.001). There was no difference between PI groups regarding distal lordosis (low PI versus average PI, 35° versus 37° [95% CI, -6.1° to 2.5°], p = 0.90; low PI versus high PI, 35° versus 36° [95% CI, -6.3° to 4.1°], p = 0.99; and average PI versus high PI, 37° versus 36° [95% CI, -3.8° to 5.4°], p = 0.99). Linear regression showed that PI represented 43% of the proximal lordosis (r2 = 0.879, proximal lordosis = 0.428 x PI, p < 0.001) (Fig. 4). After exploring other variables such as age, we found that only PI was associated with proximal lordosis (p < 0.001). On the other hand, only age was associated to distal lordosis (p = 0.02).
Fig. 2.
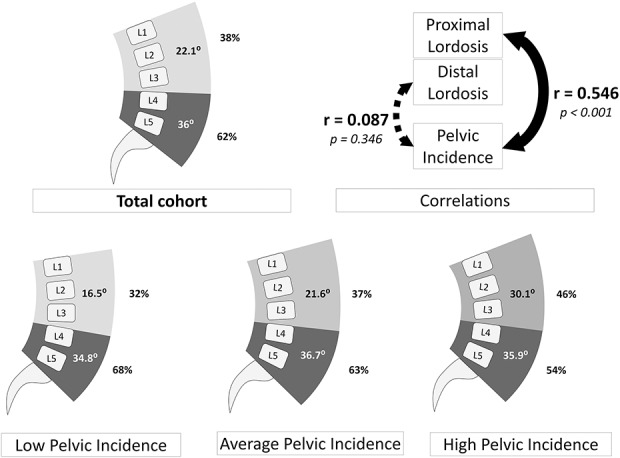
This figure represents the shape of the lumbar spine and segmental lordosis in the whole cohort and according to stratification by PI. The proximal lordosis increased with PI, whereas the distal part remained constant. There was a correlation between PI and proximal lordosis.
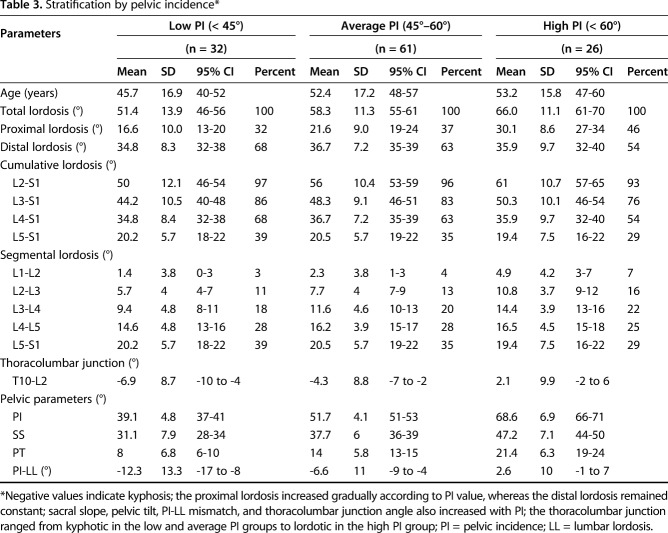
Table 2.
Results of the correlation analysis*
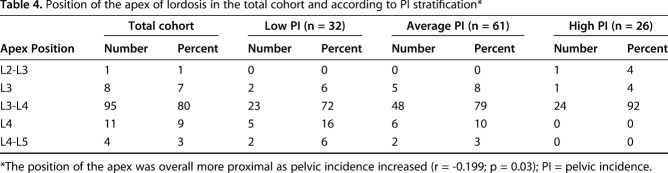
Table 3.
Stratification by pelvic incidence*
Fig. 3.
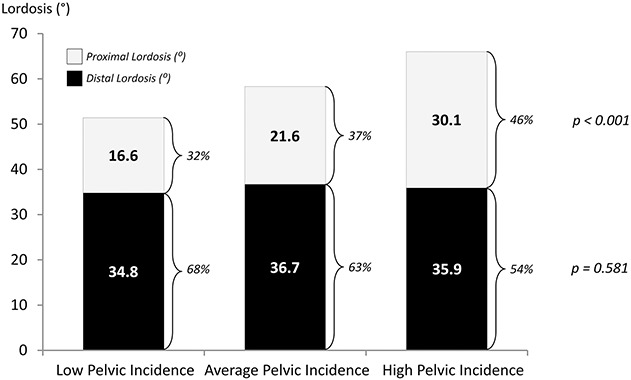
This bar plot shows the proportion of proximal and distal lordosis by PI groups. The proximal lordosis increased throughout PI groups, whereas the distal part remained constant.
Fig. 4.
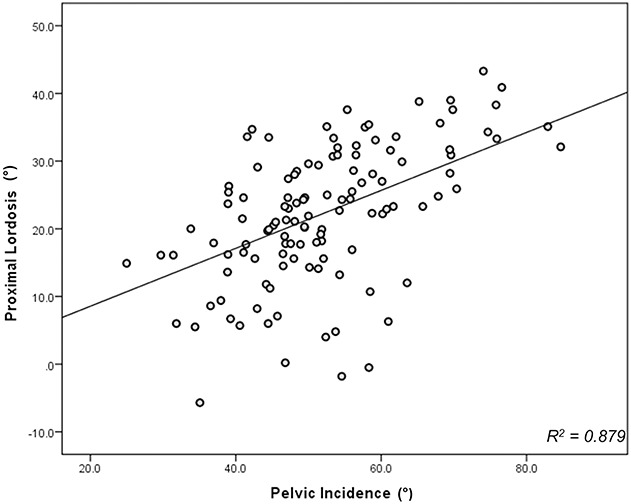
This plot shows the linear regression for prediction of proximal lordosis with PI. It shows that PI accounted for 43% of the proximal lordosis (proximal lordosis = 0.428 x PI; r2 = 0.879; p < 0.001).
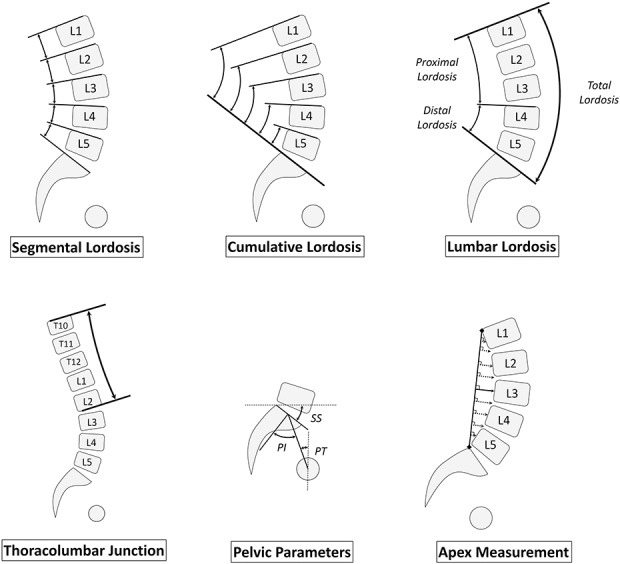
Lordosis Apex Position Change and PI Value
There was a correlation between PI and the apex position (r = -0.199; p = 0.034), meaning that as PI increased, the location of the apex was increasingly proximal. In the low PI group, the apex position was L3 in two of 32 patients, L3-L4 in 23 patients, L4 in five patients, and L4-L5 in two patients. In the average PI group, the apex position was L3 in five of 61 patients, L3-L4 in 48 patients, L4 in six patients, and L4-L5 in two patients. Finally, in the high PI group, the apex position was L2-L3 in one of 26 patients, L3 in one patient, and L3-L4 in 24 patients (Table 4).
Table 4.
Position of the apex of lordosis in the total cohort and according to PI stratification*
Discussion
Because spinal fusion aims to restore the natural profile of the spine, a deeper understanding of the distribution of lordosis across the entire lumbar spine is needed. Most of the studies investigating the relationship between the pelvis and lumbar spine did not explore the shape of the lumbar spine in relation to PI [4, 9]. The present study provided a cohort of 119 asymptomatic individuals to identify the relationship between pelvic morphology and the shape of the lumbar lordosis. We were able to demonstrate an association between the segmental lordosis, particularly in the proximal portion, with the pelvic anatomy. Patients with larger PI revealed accompanying larger proximal lordosis in the lumbar region.
The present study has several limitations. First, the cohort size is limited and a larger series may provide a more detailed analysis of the relationship between pelvic morphology and lumbar lordosis. Second, including more PI groups and assessing the influence of age and sex could be of interest but would require a larger cohort. Finally, this analysis was conducted in two dimensions (sagittal only) and did not investigate the potential association between the lower limbs and lordosis shape. Despite a limited sample, we were able to find relationships between pelvic anatomy and lumbar spine shape.
Our results suggest that lordosis is not homogenously distributed across the different lumbar levels. The L4-S1 segment was overall responsible for 62% of lordosis, whereas the three other levels accounted for 38%. These results are in line with those reported by Been et al. [3]. Segmental lordosis has previously been explored by Anwar et al. [1]. They reported their results on a much younger cohort than ours with a mean age of 17 years. With a mean age of 51 years old, our cohort is likely more representative of the patients seen in the setting of adult spinal deformity. In addition, the cohort of Anwar et al. [1] was mainly composed of women (sex ratio 8:1), whereas our 2:1 sex ratio is likely more representative of the expected patient population with adult spinal deformity. However, our results are in line with theirs. We found that as PI increased, proximal levels were recruited to increase lordosis. The lordosis within the proximal portion of the lumbar spine increased throughout the different PI. In patients with high PI, proximal lordosis was responsible for almost half of the total lordosis.
We found that the lordosis within L4-S1 was nearly constant and independent of the PI (Fig. 5). The L4-S1 lordosis was approximately 35° in the three different groups and was not correlated to PI. Contrary to the present notion, this finding implies that the shape of the global lordosis cannot be characterized by the distal lordosis. These results contradict those reported by Laouissat et al. [8] and Roussouly et al. [13]. In their studies, they postulated for the lower arc to show more variation across their cohort, and they based their classification on this parameter. As defined by the authors, the lower arc was the lordosis measured between a horizontal line located at the apex and the superior endplate of S1. We based our analysis on anatomic landmarks, which seems more reasonable because measuring the distal lordosis by taking the horizontal plane as a reference makes it a positional parameter. Because the relationship between PI and sacral slope is static, individuals with a larger PI will have an increased inclination of the sacral slope. Consequently, a forward rotation is induced in the entire spine. The magnitude of the lower arc will then increase, whereas the distal lordosis (within L4-S1) will not necessarily change. Given that the spine may rotate in pathologic conditions, the use of a positional parameter is then questionable. A pathologic decrease of lumbar lordosis will induce pelvic retroversion and therefore an increase in pelvic tilt as a compensatory mechanism for loss of spinal curvature. Following the geometric relationship between pelvic parameters, an increase of pelvic tilt is necessarily associated with a decrease in sacral slope. These compensatory mechanisms within the pelvis will lead to a decrease in the lower arc of lordosis as defined by Roussouly et al. [13], whereas the driver of the deformity is not necessarily located in the distal lordosis. Using this classification may therefore be misleading in patients with spinal pathology because it may fail to determine the location of the loss of lordosis and reconstruction.
Fig. 5 A-C.
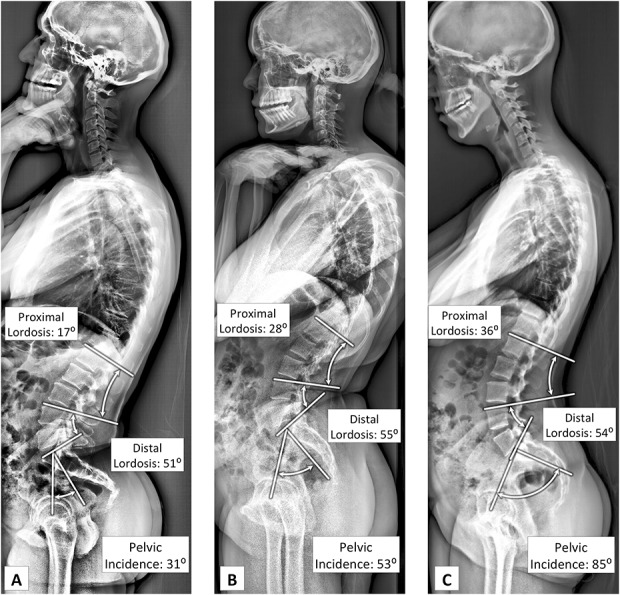
Herein are presented clinical examples of segmental lordosis according to PI. In patients with low (A) and average (B) PI, the main part of the lordosis occurs within the distal vertebrae, whereas in patients with high PI (C), almost 40% of the total lordosis is located within the proximal vertebrae. Of note, the distal lordosis was almost constant in these three patients, independent of the PI value.
Our results suggest that an increase of PI is associated with a proximal migration of the apex. There was a correlation between PI and apex position (eg, larger PI was associated with more proximal location of the apex of lordosis). Although this relationship was weak, we believe this finding can serve as a guideline on the location of restoration of lordosis (distal over proximal location) in the setting of realignment surgery. The apex was in the distal lordosis in 22% of the patients with a low PI, whereas none of the patients with a high PI had the apex located in the distal lordosis. These results correspond with those reported by Roussouly et al. [13] and support that an increase of PI is associated with an increase of proximal lordosis; as the proportion of lordosis resulting from the proximal lumbar spine increases, the apex will necessarily migrate proximally.
Using anatomic landmarks, we were able to define normative values of segmental lordosis at each level according to PI. Surgeons may be able to analyze the segmental lordosis and accurately determine the levels involved in the malalignment. Lumbar spine fusions may be able to be planned with a more accurate approach that allows personalized realignment considering segmental angular goals based on pelvic morphology. PI strongly influences the proximal portion of lumbar lordosis. Although distal lordosis is responsible for the major part of the total lordosis, it remains constant across individuals and independent of the PI. The proximal portion exhibits the most variability to adjust the total lumbar lordosis to pelvic anatomy. The normative values provided by this study allow accurate analysis of sagittal malalignment and identification of the location of the deformity. Surgeons should consider the distribution of the segmental lumbar lordosis while planning its restoration in realignment surgery when seeking to restore a proper lumbar shape rather than just the global lordosis. Focusing on the value of segmental lordosis at each level, further research could investigate the consequences of different spinal conditions on lordosis shape. Such an investigation would enable an understanding of the mechanisms of decreasing lordosis in both patients with degenerative spine and those with adult spine deformity. For example, in degenerative spondylolisthesis it is still unclear if the loss of lordosis only occurs at the listhesis level or if it extends to other levels. Furthermore, in long fusions, this could elucidate the effect of a proper segmental lordosis restoration versus restoration of the overall lordosis. It is still unclear what should be the ideal shape of a fused spine, but this study provides the basis to investigate this particular question and its impact on long-term function as well as junctional disease.
Acknowledgments
We thank George Beyer for contributing to the language editing of our manuscript.
Footnotes
One of the authors (LGL) reports personal fees from Medtronic (Minneapolis, MN, USA), grants and personal fees from DePuy-Synthes Spine (Raynham, MA, USA), personal fees from K2M (Leesburg, VA, USA), nonfinancial support from Broadwater (New York, NY, USA), nonfinancial support from the Seattle Science Foundation (Seattle, WA, USA), grants and nonfinancial support from the Scoliosis Research Society (Milwaukee, WI, USA), nonfinancial support from Stryker Spine (Allendale, NJ, USA), nonfinancial support from The Spinal Research Foundation (New York, NY, USA), grants from EOS (Paris, France), grants from the Setting Scoliosis Straight Foundation (New York, NY, USA), personal fees from Fox Rothschild LLC (New York, NY, USA), personal fees from Quality Medical Publishing (St Louis, MO, USA), other from the Evans Family Donation (New York, NY, USA), other from the Fox Family Foundation (St Louis, MO, USA), and grants and nonfinancial support from AO Spine (Geneva, Switzerland), outside the submitted work. One of the authors (FJS) reports grants from NuVasive (San Diego, CA, USA), grants from K2M, grants from DePuy Synthes (Raynham, MA, USA), personal fees from K2M, personal fees from NuVasive, personal fees from Medicrea (Rillieux la Pape, France), personal fees from Zimmer Biomet (Warsaw, IN, USA), personal fees from MSD (Kenilworth, NJ, USA), other from Nemaris Inc (New York, NY, USA), and grants from Stryker (Allendale, NJ, USA), outside the submitted work. One of the authors (HJK) reports personal fees from K2M, personal fees from Zimmer Biomet, other from AO Spine, grants from ISSGF (New York, NY, USA), and other from Stryker (Leesburg, VA, USA), outside the submitted work. One of the authors (VL) reports grants from SRS (Milwaukee, WI, USA), grants from NuVasive, grants from DePuy (Raynham, MA, USA), grants and personal fees from K2M, grants from Stryker, personal fees from DePuy Spine (Raynham, MA, USA), personal fees from MSD, personal fees from NuVasive, and other from Nemaris Inc (New York, NY, USA), outside the submitted work.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Hospital for Special Surgery, New York, NY, USA.
References
- 1.Anwar HA, Butler JS, Yarashi T, Rajakulendran K, Molloy S. Segmental pelvic correlation (SPeC): a novel approach to understanding sagittal plane spinal alignment. Spine J. 2015;15:2518–2523. [DOI] [PubMed] [Google Scholar]
- 2.Aoki Y, Nakajima A, Takahashi H, Sonobe M, Terajima F, Saito M, Takahashi K, Ohtori S, Watanabe A, Nakajima T, Takazawa M, Orita S, Eguchi Y, Nakagawa K. Influence of pelvic incidence-lumbar lordosis mismatch on surgical outcomes of short-segment transforaminal lumbar interbody fusion. BMC Musculoskelet Disord. 2015;16:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Been E, Barash A, Marom A, Kramer PA. Vertebral bodies or discs: which contributes more to human-like lumbar lordosis? Clin Orthop Relat Res. 2010;468:1822–1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupère G, Pélissier J. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15:415–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976). 2005;30:682–688. [DOI] [PubMed] [Google Scholar]
- 6.Hong JY, Suh SW, Modi HN, Hur CY, Song HR, Park JH. Reliability analysis for radiographic measures of lumbar lordosis in adult scoliosis: a case–control study comparing 6 methods. Eur Spine J. 2010;19:1551–1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lafage V, Schwab F, Patel A, Hawkinson N, Farcy J-P. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 2009;34:E599–606. [DOI] [PubMed] [Google Scholar]
- 8.Laouissat F, Sebaaly A, Gehrchen M, Roussouly P. Classification of normal sagittal spine alignment: refounding the Roussouly classification. Eur Spine J. 2017. Apr 28. 10.1007/s00586-017-5111-x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matsumoto T, Okuda S, Maeno T, Yamashita T, Yamasaki R, Sugiura T, Iwasaki M. Spinopelvic sagittal imbalance as a risk factor for adjacent-segment disease after single-segment posterior lumbar interbody fusion. J Neurosurg Spine. 2017;26:435–440. [DOI] [PubMed] [Google Scholar]
- 11.Rillardon L, Levassor N, Guigui P, Wodecki P, Cardinne L, Templier A, Skalli W. [Validation of a tool to measure pelvic and spinal parameters of sagittal balance] [in French]. Rev Chir Orthop Reparatrice Appar Mot. 2003;89:218–227. [PubMed] [Google Scholar]
- 12.Rothenfluh DA, Mueller DA, Rothenfluh E, Min K. Pelvic incidence-lumbar lordosis mismatch predisposes to adjacent segment disease after lumbar spinal fusion. Eur Spine J. 2015;24:1251–1258. [DOI] [PubMed] [Google Scholar]
- 13.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976). 2005;30:346–353. [DOI] [PubMed] [Google Scholar]
- 14.Tempel ZJ, Gandhoke GS, Bolinger BD, Khattar NK, Parry PV, Chang YF, Okonkwo DO, Kanter AS. The influence of pelvic incidence and lumbar lordosis mismatch on development of symptomatic adjacent level disease following single-level transforaminal lumbar interbody fusion. Neurosurgery. 2017;80:880–886. [DOI] [PubMed] [Google Scholar]