Abstract
Background
The United States has a growing opioid epidemic impacting all aspects of health care including orthopaedic surgery. Septic arthritis of the knee is a condition commonly encountered by orthopaedic surgeons related to opioid and injection drug use (IDU). Changes in the frequency of hospitalizations for IDU-related septic arthritis and differences in septic arthritis patient outcomes according to IDU status in the setting of the burgeoning opioid epidemic are unknown.
Questions/purposes
(1) What proportion of patients with septic arthritis of the knee use injection drugs? (2) Are there any differences in complications, reoperations, length of stay, and leaving against medical advice among patients with septic arthritis of the knee with and without IDU? (3) What are the age and racial trends in IDU-related septic arthritis of the knee from 2000 to 2013?
Methods
The Healthcare Cost and Utilization Project, Nationwide Inpatient Sample database of years 2000 to 2013 was utilized for patients between ages 15 and 64 years with a principal discharge diagnosis of native septic arthritis of the lower leg, the vast majority of which represents the knee. The Nationwide Inpatient Sample is the largest publicly available healthcare database in the United States that can show nationally representative clinical trends and outcomes. Septic arthritis was classified as related or unrelated to IDU based on previously published algorithms using billing codes. Patients with IDU-related septic arthritis were more likely to be black or Hispanic, younger, and use Medicare, Medicaid, or self-payment as their primary payment method. The yearly proportion of patients with septic arthritis who used injection drugs was determined. Hospitalization outcomes including length of stay, leaving against medical advice, number of procedures, and mortality rates were compared after adjusting for age, gender, and race in multivariable regression analyses. The yearly change in proportion of IDU-related septic arthritis in each age, race, and gender group was compared over the study period.
Results
The proportion of patients with IDU-related septic arthritis increased from 5% in 2000 to 11% in 2013. After adjusting for age, gender, and race, patients with IDU-related septic arthritis were more likely to die during hospitalization (adjusted odds ratio [AOR], 2.86; 95% confidence interval [CI], 1.51-5.39; p < 0.001) and undergo repeat arthroscopic (AOR, 1.24; 95% CI, 1.06-1.45; p = 0.007) or open irrigation and débridement (AOR, 1.68; 95% CI, 1.28-2.19; p < 0.001). Patients with IDU-related septic arthritis were more likely to leave against medical advice (AOR, 7.13; 95% CI, 5.56-9.15; p < 0.001) and also had an additional 5 days in length of stay (95% CI, 4.1-5.5; p < 0.001) on average compared with patients with septic arthritis unrelated to IDU. There was an increasing proportion of patients with IDU-related septic arthritis who were aged 15 to 34 years and 55 to 64 years from 2000 to 2013.
Conclusions
IDU is increasingly the cause of septic knee admissions and is associated with higher rates of mortality, reoperations, resource utilization, and leaving against medical advice. Orthopaedic surgeons must adequately screen for IDU among patients with septic arthritis and monitor them closely for reoperation with a low threshold to reaspirate a knee in the postoperative period. Future studies should determine the current use and potential benefits of a multidisciplinary approach, including addiction specialists, to aid in the management of the increasing number of these patients.
Level of Evidence
Level III, therapeutic study.
Introduction
Septic arthritis, the infection of one or more joints, is a condition commonly encountered by orthopaedic surgeons across all subspecialties. It is a condition associated with considerable morbidity and mortality [13] with total hospital charges at USD 759 million in the United States in 2012 [21]. High-risk populations include children, older patients, people with prosthetic joints, and people who inject drugs [6, 19]. Injection drug use (IDU)-related septic arthritis occurs either through local extension of infected skin and soft tissue near the insertion site of needles or from hematogenous seeding of joints [5, 10, 17, 18].
In light of the burgeoning opioid epidemic, trends in healthcare utilization for people with IDU-related septic arthritis is of increasing interest to the orthopaedic community [8, 16, 24]. Relative rates of complications, reoperations, and leaving against medical advice as well as the length of stay for patients diagnosed with septic arthritis with and without IDU are highly relevant but largely unknown. Intrigued by these questions, we analyzed data from a large, deidentified healthcare database with the goals of describing trends in hospital utilization for IDU-related septic arthritis of the knee, which is the most commonly affected joint in both children and adults for bacterial and mycobacterial arthritis [22].
We therefore asked: (1) What proportion of patients hospitalized with septic arthritis of the knee are people who use drugs and how has this proportion changed over time? (2) Are there any differences in complications, reoperations, length of stay, and leaving against medical advice among patients with septic arthritis of the knee with and without IDU? (3) What are age and racial trends associated with IDU-related patients with septic arthritis of the knee from 2000 to 2013?
Patients and Methods
Database
We implemented a cross-sectional, comparative analysis of data from the Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample (NIS) database from years 2000 to 2013. The HCUP includes a variety of databases managed by the Agency for Healthcare Research and Quality (AHRQ). The NIS is the largest publicly available inpatient healthcare database in the United States with > 8 million annual inpatient observations [3]. It is a stratified systematic random sample of approximately 20% of discharges from US community hospitals (nongovernmental, but including tertiary centers), excluding rehabilitation and long-term acute care hospitals. Data include diagnoses and procedural codes (International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM]), patient demographics, discharge status, demographics, and length of stay. The database has a nationally representative cohort with inclusion of a variety of hospitalization indicators, facilitating research on a broad range of topics including medical practice patterns and outcomes of treatments. Age was divided into groups 15 to 34, 35 to 54, and 55 to 64 years, whereas race was divided into six categories as reported by hospitals: white, black, Hispanic, Asian or Pacific Islander, Native American, and other.
Classification of Septic Arthritis of the Knee
We included patients with a principal diagnosis of septic arthritis of the lower extremity (ICD-9-CM 711.06) between ages 15 and 64 years at the time of admission from January 1, 2000, to December 31, 2013. We used only a principal diagnosis code of septic arthritis of the lower extremity to maximize the precision of our case definition [11, 12]. We excluded patients with a history of arthroplasty (ICD-9-CM V43.65). Although this ICD-9-CM code refers to the lower leg, because there is a separate ICD-9-CM code for septic arthritis of the ankle and foot (ICD-9-CM 711.07), the vast majority of these diagnoses represents septic arthritis of the knee, and throughout this article, we refer to septic arthritis of the knee.
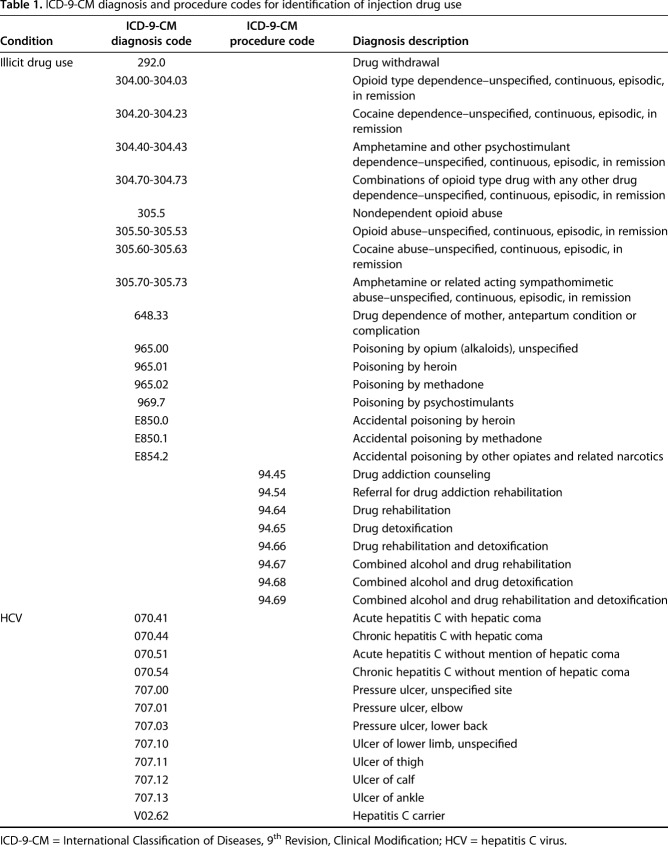
Classification of IDU-related Septic Arthritis of the Knee
The term IDU includes any use of illicit or nonprescription drugs. Typically, this includes opioids, cocaine, and methamphetamines. There is no validated method of which we are aware to identify people who use or inject drugs using ICD-9-CM codes. Specifically, ICD-9-CM codes do not differentiate among ways of use (eg, smoke, snort, or injection). However, several researchers have developed algorithms using ICD-9-CM codes to approximate use of drugs in patients admitted to the hospital. We used one such algorithm [25] for identifying IDU-related septic arthritis (Table 1) that seeks to identify people who use drugs based on the ICD-9-CM diagnosis codes for illicit drug use and hepatitis C virus, which are commonly present in patients with IDU. Hospitalizations were then either classified as septic arthritis of the knee related to IDU or not related to IDU.
Table 1.
ICD-9-CM diagnosis and procedure codes for identification of injection drug use
Patient Population
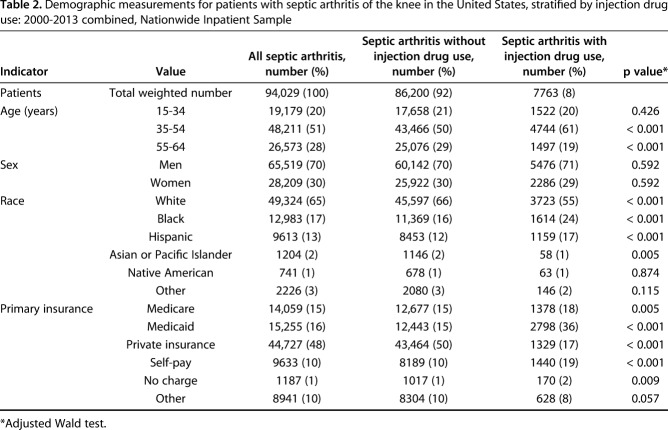
We identified 19,860 patients with a principal diagnosis of septic arthritis of the knee from 2000 to 2013, an estimate of 94,028 (95% confidence interval [CI], 90,631-97,426) patients nationwide (Table 2). In 2013 alone, there were 6995 patients with septic arthritis nationally (see Appendix, Supplemental Digital Content) for patients aged 15 to 64 years, corresponding to 3.3 patients per 100,000 person-years [23]. Overall, the median (interquartile range) age was 48 (37-56) years and 70% of hospitalizations were for male patients. Nearly 95% of hospitalizations were from patients of white, black, or Hispanic races.
Table 2.
Demographic measurements for patients with septic arthritis of the knee in the United States, stratified by injection drug use: 2000-2013 combined, Nationwide Inpatient Sample
Patients with IDU-related septic arthritis were more likely to be aged 35 to 54 years and less likely to be aged 55 to 64 years. A higher proportion of patients with IDU-related septic arthritis were black or Hispanic. Patients with IDU-related septic arthritis were more likely to use Medicare, Medicaid, or self-payment as their primary insurance and to have no charges for the hospitalization. Only 17% of patients with IDU-related septic arthritis used private insurance compared with 50% of people with septic arthritis unrelated to IDU (Table 2).
Outcomes of Interest
We calculated the yearly and overall proportion of hospitalizations that were IDU-related in two populations, namely patients with septic arthritis of the knee and all patients in the NIS database from 2000 to 2013.
The main hospitalization outcomes included length of stay, total charges, the proportion of patients who left against medical advice, the proportion of patients undergoing repeat arthroscopy and arthrotomy, and mortality. For arthroscopy, we used ICD-9-CM codes 80.26, 80.46, 80.60, 80.76, 80.86, and 80.96; for arthrotomy, we used ICD-9-CM codes 80.06 and 80.16.
To compare the age and racial trends of patients with septic arthritis of the knee with and without IDU, we determined the yearly proportion of patients within each age and race category. We implemented a trend analysis of these proportions from 2000 to 2013 to determine any changes in the distribution of different age or racial groups within patients with septic arthritis with and without IDU.
Statistical Analysis
Adjusted Wald tests were used to test for differences between patients with septic arthritis with and without IDU in demographics and hospitalization outcomes. Linear regression was used to test for trends in the proportions of various demographic groups among IDU-related septic arthritis discharges with the year of hospitalization as the independent variable. Logistic regression was used to determine the odds ratios for comparing the likelihood of leaving against medical advice, performing surgical procedures, and dying based on one’s IDU status. We used multivariable analysis for both linear and logistic regressions to adjust for age, gender, and race to compute adjusted differences and adjusted odds ratios (AORs). We confirmed the goodness of fit of all logistic models using the Hosmer-Lemeshow test (p < 0.05). Statistical significance was set at p < 0.05 (two-sided). Nineteen percent of the patients were missing the race categorization, and those observations were excluded from analyses concerning race. All analyses were carried out using Stata version 12 (Stata Corp, College Station, TX, USA), and figures were produced using R 3.2.3 (R Development Core Team, Vienna, Austria). To calculate national estimates and standard errors, data were analyzed using appropriate discharge and trend weights provided by the HCUP [7]. HCUP-NIS hospital data were used to calculate appropriate standard errors when working with subsets of data only concerning patients with septic arthritis [1, 2].
Our study was exempt from the Tufts Health Sciences institutional review board because this was research not involving human subjects.
Results
Proportion of Patients With Septic Arthritis Related to IDU
Over the 14 years of this study, 8% (95% CI, 7.7%-8.8%) of patients with septic arthritis of the knee had IDU-related septic arthritis (7763 patients; 95% CI, 7176-8349). From 2000 to 2013, the proportion of patients with septic arthritis who used injection drugs increased from 5% (95% CI, 3.7%-6.6%) to 11% (95% CI, 9.0%-12.3%), and the proportion of all hospitalizations that were considered IDU also increased from 4% (95% CI, 3.9%-4.7%) to approximately 7% (95% CI, 6.7%-7.1%) (Fig. 1). Over the 14 years, patients with septic arthritis had 44% higher odds of IDU (AOR, 1.44; 95% CI, 1.36-1.54) relative to all hospitalized patients within the NIS. In proportion, 8% (95% CI, 7.7%-8.8%) of patients with septic arthritis were IDU-related, whereas among all hospitalizations, nearly 6% (95% CI, 5.6%-6.0%) were IDU-related over the 14 years.
Fig. 1.
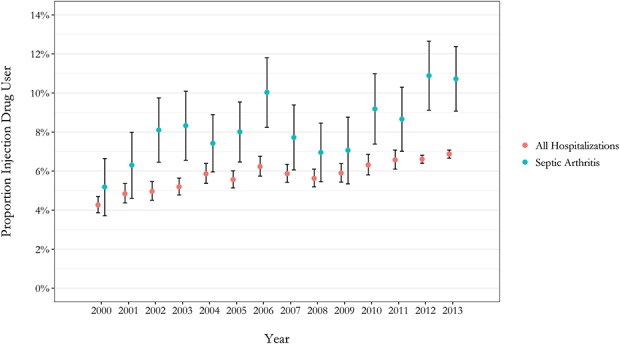
The proportion of patients with septic arthritis of the knee and the proportion of all hospitalized patients in the NIS classified as people who inject drugs in the United States from 2000 to 2013 is shown.
Complications, Reoperations, Leaving Against Medical Advice, and Length of Stay
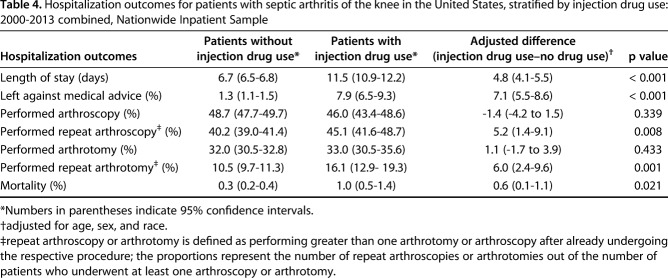
After controlling for potential confounding variables such as age, gender, and race, we found 1.0% of patients with septic arthritis related to IDU and 0.3% of patients with septic arthritis without IDU died during hospitalization, demonstrating that IDU was associated with higher odds of death during hospitalization (AOR, 2.86; 95% CI, 1.51-5.39; p < 0.001). After controlling for the aforementioned potential confounders, we found no difference between patients with septic arthritis with and without IDU as far as undergoing arthroscopy (AOR, 0.95; 95% CI, 0.84-1.06; p = 0.341) or arthrotomy (AOR, 1.05; 95% CI, 0.93-1.19; p = 0.428) (Table 3). However, if they had either procedure, patients with IDU-related septic arthritis were more likely to undergo a second arthroscopy (AOR, 1.24; 95% CI, 1.06-1.45; p = 0.007) or arthrotomy (AOR, 1.68; 95% CI, 1.28-2.19; p < 0.001). Patients with septic arthritis with IDU had 7.13 times the odds of leaving against medical advice relative to patients with septic arthritis without IDU (95% CI, 5.56-9.15). A total of 8% (95% CI, 6.5%-9.3%) of patients with IDU-related septic arthritis and 1.3% (95% CI, 1.1%-1.5%) of patients without IDU-related septic arthritis left against medical advice. The mean length of stay was approximately 12 days for patients with IDU-related septic arthritis compared with 7 days for patients without IDU, showing a difference on average of 5 additional days (95% CI, 4.1-5.5) (Table 4).
Table 3.
Association of injection drug use with hospitalization outcomes among patients with septic arthritis of the knee, United States: 2000-2013, Nationwide Inpatient Sample
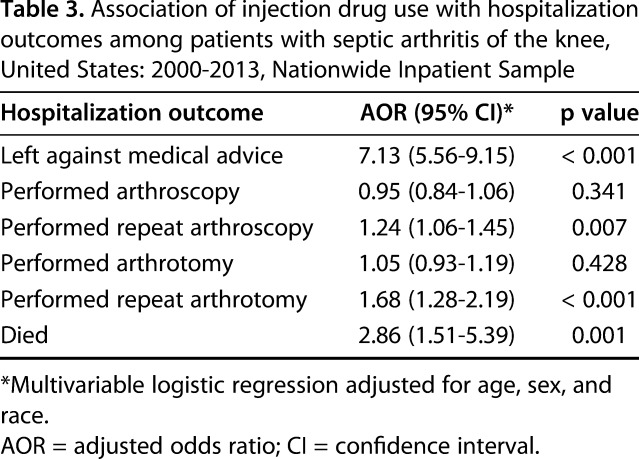
Table 4.
Hospitalization outcomes for patients with septic arthritis of the knee in the United States, stratified by injection drug use: 2000-2013 combined, Nationwide Inpatient Sample
Age and Racial Trends
Over the same time period, there was a decrease in the proportion of patients without IDU who were aged 15 to 34 and 35 to 54 years as well as an increase in the 55- to 64-year age group. Accordingly, the mean age of patients with septic arthritis without IDU increased from just under 44 years (95% CI, 40.7-46.8) in 2000 to over 47 years (95% CI, 46.5-48.0) in 2013. In contrast, among patients with IDU-related septic arthritis, there was an increase in the proportion of patients in age groups 15 to 34 and 55 to 64 years. Native Americans were the only race group that had an increase in their proportion among patients with IDU-related septic arthritis (Appendix, Supplemental Digital Content).
Discussion
Septic arthritis is a common orthopaedic condition with considerable morbidity and mortality. This study demonstrates rising hospitalizations from IDU-related septic arthritis in the context of the opioid epidemic in terms of prevalence, complications, reoperations, mortality, and epidemiology. From 2000 to 2013, the proportion of patients with septic arthritis related to IDU more than doubled, and patients with septic arthritis with IDU had a higher likelihood of death during hospitalization, reoperations, and leaving against medical advice.
We acknowledge several limitations related to the use of a large administrative database. Our results rely on accurate coding at the hospital level, which can involve misclassifications or omissions. One such misclassification includes the categorization of race, which comes from hospital administrative records as identified by clinicians and not self-identified by patients. Although such nonrandom errors may disproportionately affect demographic distributions and hospitalization outcomes, the use of weighted results remedies these shortcomings. In regard to the NIS, its large sampling size and stratified cluster sampling methods make it a robust database that has been widely used in nationally representative studies; however, one key limitation is the inability to track individual patients through readmissions or the long-term course of their diagnosis. Furthermore, the categorization of patients as people who use drugs is subject to inaccuracies, but the use of algorithms from recent studies [25] allowed us to distinguish IDU to our best current ability. Indeed, because drug use is often underdiagnosed, we are likely underestimating the true burden of hospitalizations from IDU-related septic arthritis. In addition, the cross-sectional study design made it difficult to quantify the relative risk of developing septic arthritis among people who use drugs or track the long-term outcomes of the patient population. Further research with prospective cohorts is needed to characterize progression of disease and long-term outcomes and to help establish temporal causality.
There could also be potential limitations associated with our multivariable regressions. Although we controlled for key demographic factors such as age, gender, and race, other factors such as socioeconomic status, homelessness, or smoking status could also have a role in the outcomes discussed. Although the NIS has potential indicators of one’s socioeconomic status such as the estimated median household income for the zip code of the patient’s address, including it as a covariate in our models decreased the precision of the models considerably and the CIs became quite unstable. We also considered expected primary insurance as another potential covariate, but we considered it to be (1) not necessarily a strong indicator of one's affluence; and (2) the complexity of insurance coding, especially considering the interstate differences in coding insurance status, within the NIS could introduce inaccuracies to the model. Considering these factors, we decided not to include these variables in our models. Regarding homelessness and smoking status, these are often not reflected in billing frequently and, as such, not accurate markers of true homelessness or smoking status within the NIS. These indicators would be better captured through research methods including patient interviews. Although these factors could have under- or overestimated the magnitude of certain coefficients, it is unlikely that the primary findings of this study will change considerably. Future research with more detailed patient demographic data can investigate the effect of these covariates.
We observed that a greater proportion of patients with septic arthritis also had used injectable drugs over the 14-year span of this study. The mechanism for IDU leading to septic arthritis has been well described and is likely a result of bacteria injected through nonsterile needles, bacterial contamination of drugs, or systemic spread of local cellulitis at the injection site. Bacteria then deposit in joints and lead to local inflammation and bone destruction. Because people who use drugs are more likely also to have conditions like immune deficiency and malnutrition, it is thought that they serve as vulnerable hosts who (1) fail to suppress incoming pathogens and (2) provide the space necessary for their growth, particularly in joints [20]. These mechanisms are reflected within our study showing the elevated rate of IDU among patients with septic arthritis compared with all hospitalized patients within NIS. Indeed, recent research has recognized and discussed the impact of the opioid epidemic on orthopaedic surgery as the medical specialty with the third highest opioid prescriptions in the United States [15]. Current guidelines specific for orthopaedics are sparse, but generally include better identifying patients at risk of opioid addiction, more carefully determining those truly needing opioids, and setting patient expectations for pain management and prescription administration [15].
In addition to the rising prevalence, our findings suggested that patients with IDU-related septic arthritis had a higher rate of mortality, reoperation, leaving against medical advice, and a longer length of stay relative to patients with septic arthritis without IDU. The higher likelihood of receiving greater than one arthroscopy and/or arthrotomy and a higher mortality rate both indicate that patients with IDU-related septic arthritis have a much more complex clinical management course and have a heavier burden of disease relative to patients with septic arthritis without IDU. Higher rates of postoperative complications and reinfection for patients with IDU have been demonstrated in other pathologies associated with IDU such as infective endocarditis [9]. This is further complicated by nearly 8% of patients with IDU-related septic arthritis leaving against medical advice, which is approximately six times greater than the rate for patients without IDU and other musculoskeletal infections [14]. The risks of undertreated septic arthritis are further bone destruction, systemic spread of the infection leading to sepsis, and other more serious morbidities such as epidural abscesses and bacterial endocarditis. Based on these study results and the current lack of guidelines for treating IDU-related septic arthritis, orthopaedic surgeons should monitor patients with IDU-related septic arthritis more closely for reoperation with a low threshold to reaspirate a knee in the postoperative period as a result of the higher risk of complications and reoperations. Future studies can evaluate the effectiveness of a total synovectomy as an initial débridement in these populations and investigate the perihospital and posthospitalization courses of people with IDU-related septic arthritis, because their disease course after discharge may also markedly differ from patients without IDU.
The changing demographics of patients with IDU-related septic arthritis with an increasing proportion of younger (15-34 years of age) and older patients (55-64 years of age) need to be carefully considered in conjunction with the rising proportion of patients with septic arthritis with IDU so that these populations are adequately screened for within orthopaedic clinics treating patients with septic arthritis. These patients should also be adequately screened for in prescribing opioids for both secondary prevention and harm reduction using existing guidelines for all clinicians [4, 26].
Our results highlight the impact of the opioid epidemic on the orthopaedic patient population, specifically for patients with septic arthritis of the knee. Orthopaedic surgeons must be vigilant regarding this epidemic on two fronts, to (1) avoid aggravating the epidemic any further by prescribing opioids only when truly necessary and (2) managing patients with a history of IDU more adequately both in terms of acute treatment and long-term management. As a practice that often involves patients who go through a tremendous amount of pain, orthopaedic surgeons may find it difficult to adequately manage pain without exposing their patients to the risk of opioid addiction. Furthermore, although some guidance material for prescribing opioids exists [4, 15, 26], there is little guidance for the treatment of orthopaedic patients already dependent on opioids, who can present quite differently in the clinic as demonstrated. With the development of new guidelines, orthopaedic surgeons should receive additional training in these areas as part of their continuing medical education so that they can screen for IDU among patients with septic arthritis and treat adequately using those guidelines. Orthopaedic surgeons should also engage in future research to evaluate the current use and potential benefits of a multidisciplinary approach, including collaboration with addiction specialists, to aid in the management of the increasing number of these patients.
Acknowledgments
We thank the Tufts Medical Center Department of Orthopaedics for making the Nationwide Inpatient Sample available for this study.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Tufts University School of Medicine and Tufts Medical Center, Boston, MA, USA.
References
- 1.Agency for Healthcare Research and Quality. HCUP Methods Series: Calculating National Nationwide Inpatient Sample (NIS) Variance for Data Years 2011 and Earlier. 2003. Available at: https://www.hcup-us.ahrq.gov/reports/methods/2003_02.jsp. Accessed February 12, 2018.
- 2.Agency for Healthcare Research and Quality. HCUP Methods Series: Calculating National Nationwide Inpatient Sample (NIS) Variance for Data Years 2012 and Later. 2015. Available at: https://www.hcup-us.ahrq.gov/reports/methods/2015_09.jsp. Accessed February 12, 2018.
- 3.Agency for Healthcare Research and Quality. Overview of the National (Nationwide) Inpatient Sample (NIS). 2016. Available at: https://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed February 12, 2018.
- 4.Alford DP, Zisblatt L, Ng P, Hayes SM, Peloquin S, Hardesty I, White JL. SCOPE of pain: an evaluation of an opioid risk evaluation and mitigation strategy continuing education program. Pain Med. 2016;17:52–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andersen K, Bennedbaek FN, Hansen BL. [Septic arthritis in intravenous drug abuse] [in German]. Ugeskr Laeger. 1994;156:3876–3880. [PubMed] [Google Scholar]
- 6.Gupta MN, Sturrock RD, Field M. A prospective 2-year study of 75 patients with adult-onset septic arthritis. Rheumatology (Oxford). 2001;40:24–30. [DOI] [PubMed] [Google Scholar]
- 7.Healthcare Cost and Utilization Project. Using the HCUP National Inpatient Sample to Estimate Trends. 2006. Available at: https://www.hcup-us.ahrq.gov/reports/methods/methods.jsp. Accessed February 12, 2018. [Google Scholar]
- 8.Jones CM, Christensen A, Gladden RM. Increases in prescription opioid injection abuse among treatment admissions in the United States, 2004-2013. Drug Alcohol Depend. 2017;176:89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim JB, Ejiofor JI, Yammine M, Ando M, Camuso JM, Youngster I, Nelson SB, Kim AY, Melnitchouk SI, Rawn JD, MacGillivray TE, Cohn LH, Byrne JG, Sundt TM., 3rd Surgical outcomes of infective endocarditis among intravenous drug users. J Thorac Cardiovasc Surg. 2016;152:832–841.e1. [DOI] [PubMed] [Google Scholar]
- 10.Larney S, Peacock A, Mathers BM, Hickman M, Degenhardt L. A systematic review of injecting-related injury and disease among people who inject drugs. Drug Alcohol Depend. 2017;171:39–49. [DOI] [PubMed] [Google Scholar]
- 11.Lim SY, Lu N, Oza A, Fisher M, Rai SK, Menendez ME, Choi HK. Trends in gout and rheumatoid arthritis hospitalizations in the United States, 1993-2011. JAMA. 2016;315:2345–2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lu N, Rai SK, Terkeltaub R, Kim SC, Menendez ME, Choi HK. Racial disparities in the risk of Stevens–Johnson syndrome and toxic epidermal necrolysis as urate-lowering drug adverse events in the United States. Semin Arthritis Rheum. 2016;46:253–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mathews CJ, Weston VC, Jones A, Field M, Coakley G. Bacterial septic arthritis in adults. Lancet. 2010;375:846–855. [DOI] [PubMed] [Google Scholar]
- 14.Menendez ME, van Dijk CN, Ring D. Who leaves the hospital against medical advice in the orthopaedic setting? Clin Orthop Relat Res. 2015;473:1140–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morris BJ, Mir HR. The opioid epidemic: impact on orthopaedic surgery. J Am Acad Orthop Surg. 2015;23:267–271. [DOI] [PubMed] [Google Scholar]
- 16.Okie S. A flood of opioids, a rising tide of deaths. N Engl J Med. 2010;363:1981–1985. [DOI] [PubMed] [Google Scholar]
- 17.Peterson TC, Pearson C, Zekaj M, Hudson I, Fakhouri G, Vaidya R. Septic arthritis in intravenous drug abusers: a historical comparison of habits and pathogens. J Emerg Med. 2014;47:723–728. [DOI] [PubMed] [Google Scholar]
- 18.Roy S, Ninkovic J, Banerjee S, Charboneau RG, Das S, Dutta R, Kirchner VA, Koodie L, Ma J, Meng J, Barke RA. Opioid drug abuse and modulation of immune function: consequences in the susceptibility to opportunistic infections. J Neuroimmune Pharmacol. 2011;6:442–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharp JT, Lidsky MD, Duffy J, Duncan MW. Infectious arthritis. Arch Intern Med. 1979;139:1125–1130. [PubMed] [Google Scholar]
- 20.Shirtliff ME, Mader JT. Acute septic arthritis. Clin Microbiol Rev. 2002;15:527–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh JA, Yu S. The burden of septic arthritis on the US inpatient care: a national study. PLoS One. 2017;12:e0182577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith JW, Chalupa P, Shabaz Hasan M. Infectious arthritis: clinical features, laboratory findings and treatment. Clin Microbiol Infect. 2006;12:309–314. [DOI] [PubMed] [Google Scholar]
- 23.US Census Bureau. Annual Estimates of the Resident Population for the United States, Regions, States, and Puerto Rico: April 1, 2010 to July 1, 2016. Available at: https://www.census.gov/data/tables/2017/demo/popest/nation-total.html. Accessed May 12, 2017.
- 24.Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies–tackling the opioid-overdose epidemic. N Engl J Med. 2014;370:2063–2066. [DOI] [PubMed] [Google Scholar]
- 25.Wurcel AG, Anderson JE, Chui KK, Skinner S, Knox TA, Snydman DR, Stopka TJ. Increasing infectious endocarditis admissions among young people who inject drugs. Open Forum Infect Dis. 2016;3:ofw157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zisblatt L, Hayes SM, Lazure P, Hardesty I, White JL, Alford DP. Safe and competent opioid prescribing education: Increasing dissemination with a train-the-trainer program. Subst Abus. 2017;38:168–176. [DOI] [PubMed] [Google Scholar]