Abstract
Background
In traditional societies, patients who reach adulthood with developmental dysplasia of the hip (DDH) may be labeled “disabled” and may be considered “defective,” causing them psychologic pain and problems with social interactions. In some patriarchal societies, women disproportionately experience these problems, because they may be seen as insufficient in terms of marriage and sexual intercourse owing to hip-related limitations, and they may be married through arranged marriages to people who also have disabilities. This patriarchal structure limits the ways women can engage in society and may lower their quality of life (QOL). The degree to which THA can improve the lives of women in these specific ways in a patriarchal culture has not, to our knowledge, been studied.
Questions/purposes
(1) Does THA improve the social standing of young women with DDH in Turkey? (2) Does THA improve QOL of young women with DDH in Turkey? (3) Does THA improve pain and physical function in these patients?
Methods
This study was a retrospective, comparative study performed at Karabük University Research and Training Hospital in Karabük, Turkey, from 2012 to 2017. A total of 217 women with DDH were followed at our center between the study dates. All of these patients were evaluated for inclusion into the study. Among these, 175 women with DDH (aged 20-45 years) were included in the study according to inclusion/exclusion criteria. We offered THA to all patients in whom surgery was technically feasible; 84 chose to undergo THA, whereas 91 declined the procedure. Whether THA had any effects on the study questions was determined by comparison of the following findings at baseline and after intervention. The social standing of patients was assessed through their marital status and proportions of employment and depression; the patients’ QOL was assessed with the SF-36 at baseline for all patients and at 1 year postoperatively for those who underwent THA; and pain and dysfunction were evaluated by determination of the proportion of patients who had scoliosis, knee valgus, and knee and lumbar pain. At baseline, patients were not different in regard to all parameters except knee and lumbar pain, which were greater in those who had decided to undergo THA. The SF-36 scores of patients who underwent THA were compared with their postoperative scores as well as with the baseline scores of patients who did not undergo THA.
Results
In terms of measures of social standing, women who underwent THA appeared better at followup than did the patients who did not undergo THA. Those who underwent THA had higher percentages of marriage and employment and less depression. Regarding QOL, postintervention comparisons revealed that women who underwent THA had higher SF-36 scores compared with the initial results of women who did not have surgery. Compared with preoperative scores, the highest improvements were found in social role function (mean difference ± standard error [SE] = 58.64 ± 0.88; 95% confidence interval [CI], 56.91-60.37; p < 0.001) and mental health (mean difference ± SE = 53.00 ± 0.86; 95% CI, 51.31-54.69; p < 0.001) subdimensions of the SF-36. Finally, patients who underwent THA had improvements in pain and function as measured by Harris hip score than did patients who did not undergo THA. At initial evaluation, two groups were found to be similar in terms of Harris hip scores (THA: 61.6 ± 7.4 versus non-THA: 63.7 ± 7.6, p = 0.066), whereas the THA group was found to be superior at followup evaluation (THA: 83.5 ± 6.2 versus non-THA: 62.1 ± 7.8, p = 0.001).
Conclusions
Young women with DDH are severely affected by social and cultural norms in Turkey, which is an example of a patriarchal culture. We believe that in this setting, some patients who improve their appearance, gait, and physical function through THA may benefit from a better social perception and higher self-esteem, which may, in turn, increase their QOL and provide more freedom in terms of life choices.
Level of Evidence
Level III, therapeutic study.
Introduction
Developmental dysplasia of the hip (DDH) in more affluent countries usually is recognized soon after birth as a result of systematic screening. As a result, the occurrence of untreated dysplasia in young adults has dropped steadily over time [14]. However, screening and early treatment are often not available or utilized in other parts of the world, and patients affected by DDH may present for the first time as young adults [4]. Because the dysplasia in this setting is often severe, some of these patients have substantial physical disabilities with considerable pain and functional restrictions [6].
In addition to physical impairment, adult patients with DDH in some cultures are subjected to social and psychologic stresses, which diminish their quality of life [7]. Many traditional, patriarchal societies equate physical power with privilege [2]. In countries such as Turkey, which is an example of a relatively traditional, patriarchal culture, women are more severely affected by the physical issues related to DDH [3]. As DDH progresses, shortening and external rotation occur in the affected limb in addition to postural and symmetric abnormalities of the back, shoulders, waist, and hip. These changes affect appearance and may negatively impact a patient’s body image and self-esteem [11]. Furthermore, women with a more traditional perception of gender roles may see themselves as inadequate and may lose interest in social interactions [2]. In this setting, some are labeled “disabled” and may be considered “defective,” causing them psychologic pain and problems with social interactions. In some patriarchal societies, women disproportionately experience these problems, because they may be seen as insufficient in terms of marriage and sexual intercourse because of hip-related limitations, and they may be married through arranged marriages to people who also have disabilities [3]. Although it is fallacious to consider that a major aim of young women is to marry, it is also important to remember that marriage is an important step in life for many men and women; therefore, it is crucial to at least provide the chance to choose their spouse to women who are under patriarchal pressure [3]. This patriarchal structure may also limit the ways women can engage in society and may lower their quality of life (QOL). The degree to which THA can improve the lives of women in these specific ways in a patriarchal culture has not, to our knowledge, been studied. THA has been shown to improve QOL in patients with osteoarthritis secondary to DDH [5, 13, 15]. Our clinical experience led us to believe that these patients—especially women in traditional societies—may benefit from surgical intervention and improve their socioeconomic status even if functional gain is not expected.
In this study, we aimed to address the following questions: (1) Does THA improve the social standing of young women with DDH in Turkey? (2) Does THA improve QOL of young women with DDH in Turkey? (3) Does THA improve pain and physical function in these patients?
Patients and Methods
This retrospective, comparative study was performed from 2012 to 2017 at Karabük University Research and Training Hospital, which is located in Karabük, a small, relatively traditional and undeveloped city by Turkish standards. We obtained ethical approval and permission for the study from the Karabük University Clinical Research Ethical Committee. We adhered strictly to the conditions brought by the Helsinki Declaration and good clinical practice guidelines during the study. All patients provided written consent for this study.
To determine whether THA improved social standing, we compared the proportion of patients who were married, employed, and had depression in the THA and non-THA groups. The patients’ QOL was assessed with the SF-36 [1] at baseline for all patients and at 1 year postoperatively for those who underwent THA. To determine the effect of THA on pain and function, we compared the proportion of patients who had scoliosis, knee valgus deformity, and knee and lumbar pain in those with and without THA.
The study group consisted of women with DDH who attended followup studies at our center from 2012 to 2017. To be included in this study, the patient had to be a woman older than 18 years of age who had agreed to participate. In all, 217 patients in our clinic fulfilled these criteria at the time of the study and all (100%) accepted to participate in the study. Of these patients, 18 were excluded for having undergone surgery for DDH or other hip problems at a different center, four because they received a diagnosis of concurrent osteomyelitis, 17 for being absent during followup studies as a result of reasons such as relocation or changing their physician (five from the THA group, 12 from the non-THA group), and three were excluded because they were deemed inoperable (explained subsequently), resulting in the total number of exclusions being 42.
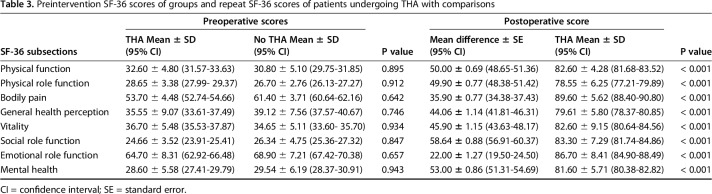
The final study group consisted of 175 women with DDH, of whom 84 (48%) underwent THA and 91 (52%) did not undergo surgical intervention. All patients’ radiographic images were evaluated, and physical examinations were performed. Two experienced orthopaedists (MA, EA) confirmed the diagnoses. The mean age of patients who underwent THA was 39 ± 3.5 years, and the mean age of patients who did not undergo surgery was 43 ± 1.5 years (p = 0.001; 95% confidence interval [CI], 4.793-3.207). The comparison of baseline characteristics of the study groups, including Crowe type, marital status, employment, depression diagnosis, comorbidities, smoking status, knee valgus deformity, educational status, and the presence/absence of lumbar and knee pain, showed the groups were similar regarding all parameters except knee and lumbar pain (Table 1).
Table 1.
Baseline characteristics and comparison of study groups
All patients decided, without outside interference, to undergo surgery. A panel of four experienced orthopaedists (TM, UD, AB, HY) and one anesthesiologist (AA) evaluated the medical suitability of patients for surgery. Three patients were deemed inoperable and were excluded from the study. The cause for inoperability was skeletal insufficiency in two and excessive loss of muscle mass in one patient.
The patients’ social standing was evaluated by determining the proportion of patients who were married, employed, and had depression diagnoses in each of the groups. A validated Turkish-language translation of the SF-36 [10] was used to assess health-related QOL at baseline and at 1 year postoperatively in the THA group and at baseline in the non-THA group. Pain and functional comparisons were performed by determining the proportion of patients who had knee pain, lumbar pain, knee valgus deformity, and scoliosis. The marital and employment status of patients were inquired by one of two nurses (HÇ, EA) and those who were married were asked whether their husband had any sort of physical disability. Evaluation of pain was performed by asking the patient whether they had pain that reduced their functional capacity in the week before inclusion into the study (in the non-THA group) or surgery (in the THA group) and the week before postintervention 1-year followup. The Harris hip scores (HHS) of all patients were also calculated [8]. The SF-36 questionnaire evaluates the patient’s health status in eight subsections: physical function, physical role function, bodily pain, general health perception, vitality, social role function, emotional role, and mental health. Each subsection is scored on a scale of 0 to 100; 0 equals severe disability and 100 equals no disability. In the present study, QOL was assessed by applying the SF-36 to the entire study group at the study’s inception. Patients who underwent THA repeated the test 1 year postoperatively. The average time of questionnaire completion was 45 minutes. All subsections of the SF-36 were similar among groups at baseline.
In patients who underwent THA, the procedure was performed with spinal anesthesia in 90% of the patients, whereas general anesthesia was used in the remaining 10% as a result of patient request. The operation was performed as follows: patients were placed in the lateral decubitus position, and a posterior approach was used. The trochanteric bursa was incised, the joint capsule was partially excised, and hip dislocation was performed. The femoral neck osteotomy was performed from the greater trochanter to 1 cm superior of the lesser trochanter. The true acetabulum was found and the joint capsule was completely excised. Before advancing to femoral shortening osteotomy, femoral reaming was performed. On average, a 1- to 2-cm transverse femoral cut was performed for femoral shortening. Afterward, the true acetabulum was reamed and the acetabulum was placed with press-fit and fixed with two or three screws. Both parts of the femur were pulled longitudinally and the overlap between proximal and distal parts was compared with results from presurgical physical examination and orthoroentgenograms to determine the correct shortening amount. The second femoral cut was performed in parallel with the first cut followed by reaming of the femur and insertion of an appropriate femoral stem. Neutral anteversion was applied. To prevent bone fissure, a cerclage wire was applied to the proximal femur. Joint movements and stability of the osteotomy were checked. A 3.5-mm plate-screw was applied in those with instability. Another cerclage wire was utilized for fixation in cases in which there was further suspicion of instability at the osteotomy line. Lateral rotators were fixed to the greater trochanter. Closing of the wound was performed appropriately.
Patients who chose not to undergo THA attended usual followup and were treated for pain during painful periods. Patients with pain were prescribed nonsteroidal antiinflammatory drugs and rest was suggested. If pain increased with walking, we suggested assistive devices and a followup 6 to 7 weeks later for pain evaluation was scheduled. Patients who had more pronounced lumbar pain (compared with hip pain) were given physical rehabilitation programs and directed to the physical therapy and rehabilitation department for close followup. The THA group attended postoperative followup (explained in detail later) and were treated for pain similarly to the non-THA group. We suggested that patients with excessive leg-length discrepancies use orthopaedic shoes with high soles. Those who had a body mass index > 25 kg/m2 were directed to the dietitian’s clinic. All patients with symptoms or signs of depression were referred to the psychiatry clinic.
The postoperative care of patients who underwent THA was performed as follows: patients were kept as inpatients at the hospital for 5 to 7 days. Mobilization was started in bed at postoperative Day 1 and extended to movements outside the bed at 2 to 3 days without applying weight to the surgical side. Patients were taught safe joint movements and isometric/isotonic quadriceps exercises and were asked to perform these movements at least two to three times a day while in bed. After discharge, the first followup was scheduled for postoperative Day 16 to 18, when radiographic imaging was performed and their sutures were also removed. The second followup was at postoperative Day 30 and the third at Day 45 when radiographic imaging and physical examinations were performed. The first time weight was applied to the operated extremity was between Days 45 and 50; those who had callus formation were permitted full weightbearing. By postoperative Day 60, all patients had at least started to apply partial weight to the operated side. After Day 60, followup visits were scheduled at intervals of 2 months for all patients. At the end of the first year, all patients who underwent THA attended repeat SF-36 evaluation.
Our primary study outcome was the change in social standing (marital status, employment, and depression). Secondary comparisons included changes in QOL (SF-36 score), pain and function (the proportion of patients who reported knee and lumbar pain and the presence of knee valgus deformity and scoliosis), and HHS.
To determine whether the groups were generally comparable, we evaluated patients’ Crowe type, comorbidities, marital status, employment status, depression, knee and lumbar pain, smoking status, the presence of knee valgus, scoliosis, and educational status. To minimize cotreatment bias, the followup of the non-THA group was performed as before and they were treated for pain, whereas the THA group attended postoperative followup and were also treated for pain similarly. To minimize assessment bias, the interviews of patients were performed by one of two nurses (HÇ, EA) who were not immediate healthcare providers of the patient.
All analyses were performed with SPSS, Version 20 (SPSS, Chicago, IL, USA). For the normality test, we used the Shapiro-Wilk test. Continuous variables are given as mean ± SD for normally distributed data and median (minimum–maximum) for nonnormally distributed data. We used the Mann-Whitney U test for between-group comparisons and analyzed categorical variables with the chi-square test. Before-and-after comparisons of categorical variables were made using the McNemar test. Using the nonparametric Wilcoxon test, we compared the patients’ QOL before and after THA. We accepted p ≤ 0.05 values as statistically significant.
Results
Social Standing
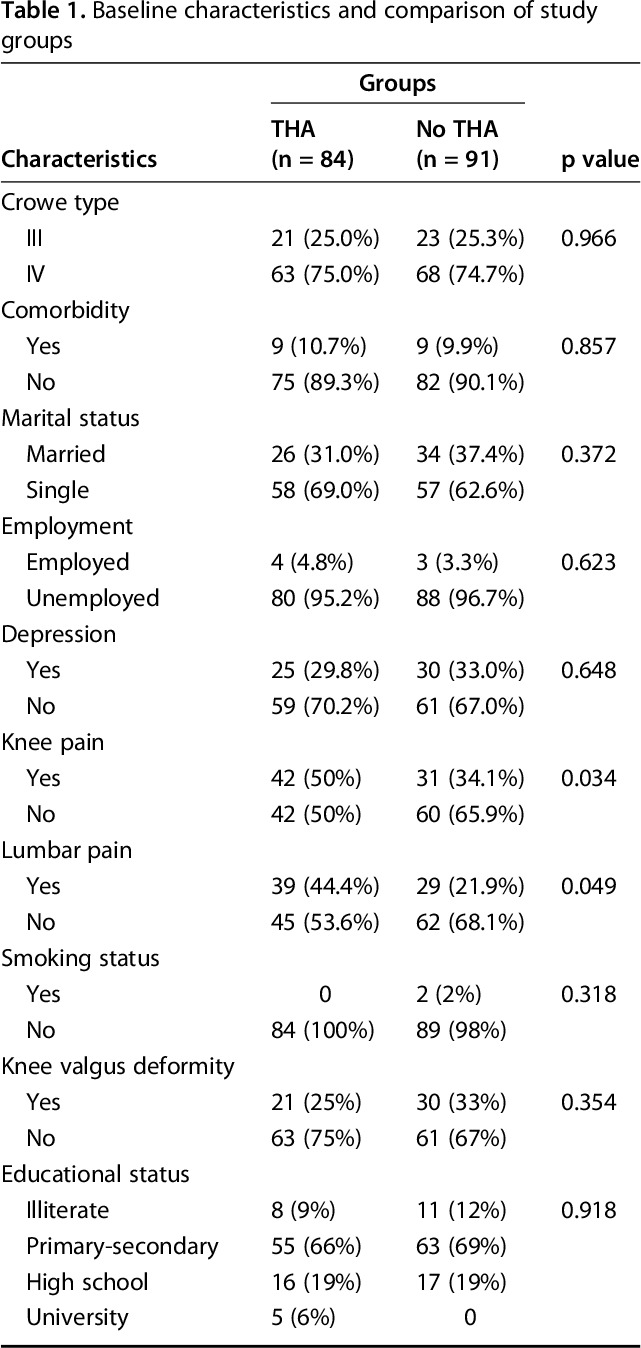
In terms of measures of social standing, women who underwent THA in this study appeared better at followup than did the patients who did not undergo THA. The percentage of patients who were married was higher in the group that underwent THA (51 of 84 [61%] versus 34 of 91 [37%], p = 0.002). In the followup period we observed an increase in the number of married women in the THA group (odds ratio [OR], 12.50; 95% CI, 3.12-108.89; p < 0.001), whereas there was no change in the non-THA group. We observed that 25 (30%) of the patients in the THA group married after the surgery. Furthermore, 17 of the 26 patients who were married before the surgery were married to persons who also had illnesses or complications that caused physical disabilities (coxarthrosis, polio sequelae, etc). However, no patients who married after THA had spouses with physical problems. Compared with those who did not receive surgery, patients who underwent THA had a higher percentage of employment (25% versus 5%, p < 0.001). Similar to marital status, there was an increase in the employment percentage of women who underwent THA (OR, 17.00; 95% CI, 2.66-710.46; p < 0.001), whereas no change was found among those without THA. In regard to depression diagnoses, the groups were similar at baseline (30% versus 33%, p < 0.001) (Table 1), whereas postinterventional comparison revealed that patients who did not undergo surgery had a higher percentage of clinical depression (1% versus 18%, p < 0.001) (Table 2). Also, we found that both groups had improvements regarding depression diagnosis (THA: p < 0.001, OR, not available; and non-THA: OR, 0.36, 95% CI, 0.14-0.85; p = 0.017).
Table 2.
Postintervention characteristics and comparison of study groups
Quality of Life
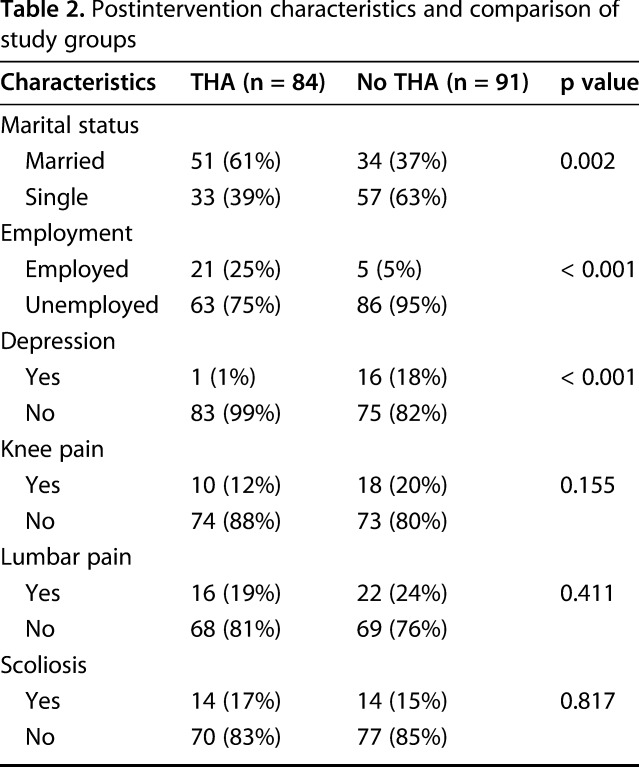
The SF-36 scores of those who underwent THA were higher than the scores of women who did not have surgery. All subsections of the SF-36 were higher in those who underwent THA. Compared with preoperative scores, the highest improvements were found in social role function (24.66 ± 3.52 versus 83.3 ± 7.29, mean difference = 58.64, p < 0.001) and mental health (28.60 ± 5.58 versus 81.60 ± 5.71, mean difference = 53.0, p < 0.001) subsections of the SF-36 (Table 3).
Table 3.
Preintervention SF-36 scores of groups and repeat SF-36 scores of patients undergoing THA with comparisons
Pain and Function
Finally, patients who underwent THA had greater improvements in self-reported pain presence/absence than did patients who did not undergo THA. Although 42 patients reported functionally limiting knee pain before THA, only 10 reported pain postoperatively (OR, 0.059; 95% CI, 0.007-0.229; p < 0.001). In terms of lumbar pain, comparisons showed considerable improvement in those who had undergone THA (OR, 0.207; 95% CI, 0.070-0.507; p = 0.001). When we compared the groups (THA versus non-THA) postoperatively for knee pain, lumbar pain, scoliosis, and knee valgus deformity, we found no differences (p > 0.05) (Table 2). At initial evaluation, two groups were found to be similar in terms of HHS (THA: 61.6 ± 7.4 versus non-THA: 63.7 ± 7.6, p = 0.066), whereas the THA group was found to be superior at followup evaluation (THA: 83.5 ± 6.2 versus non-THA: 62.1 ± 7.8, p = 0.001). In other words, although HHS improvements were observed in the THA group (mean difference ± standard error [SE] = 21.90 ± 1.03; 95% CI, 19.87-23.93; p < 0.001), there was no change in the non-THA group (mean difference ± SE= -1.6 ± 1.17; 95% CI, -3.90 to 0.70; p = 0.172).
Discussion
DDH is a debilitating condition that has severe consequences to the QOL of patients, especially if it has been unidentified or untreated until adulthood [7]. Young adults, especially women in patriarchal cultures, may experience the restrictions brought by the disease disproportionately, because they may be seen as disabled and insufficient in terms of social life and physical interactions including sexual intercourse [3]. THA is a procedure through which the appearance, gait, and physical function of patients with DDH may be restored to some degree, which may benefit patients in terms of QOL and social standing in some more traditional societies. To our knowledge, the effect of THA on social standing has not been investigated. In this study, we found that women who chose to undergo THA benefitted in terms of social standing (marriage, employment, and depression) and QOL (SF-36 scores).
Our patient group is a highly specific group, consisting of women with advanced, untreated DDH; therefore, our results only apply to these patients. Baseline analysis of groups showed that groups were not different in terms of social standing and physical problems, whereas there were differences between groups regarding pain and age. These differences may be regarded as limitations; however, the presence/absence of pain and its severity are varying parameters in DDH. We do not believe that higher proportions of patients with knee and lumbar pain in the THA group (50% versus 34% and 44% versus 22%) were the sole reason driving these patients’ decisions to undergo surgery. In terms of the baseline age difference between groups, the younger age of those who accepted to undergo surgery may have been associated with a desire to normalize appearance, gait, and physical problems before age became a problem for the decision to undergo surgery (younger patients may have been more eager to solve these problems before starting their career, marrying, or having children). All in all, these baseline differences are important limitations of the study. Second, the lack of postintervention SF-36 scores in the non-THA group may be considered a limitation. However, among non-THA patients, a small number attended postintervention SF-36 evaluation; thus, we decided to use their preintervention results rather than include results from a smaller portion of patients. Although it is very unlikely that there would be any major differences from baseline SF-36 values in the non-THA group, this is a limitation from a statistical perspective as a result of the chance for changes to occur over time. Also, ours is a single-center study and thus lacks comparisons with data from other areas. However, Karabük can be considered to be a city that conforms to the sociocultural median of Turkey. Therefore, our results apply to the large majority of Turkey and to countries and regions that are similar to Turkey in regard to sociocultural characteristics. We evaluated marital status as a primary parameter for social standing. This may not be true for all those who participated in the study because they may not be interested in marriage at all. However, 25 of those who underwent THA married after the procedure and the fact that none of these patients were married to persons with disabilities is very important regarding social freedom. Although this alone may not prove that they were not married through arranged marriages, the fact that 17 of the 26 who were married preoperatively were married to people with physical disabilities is highly suggestive of arranged marriages and shows that patients who underwent THA had more freedom regarding marital choice. Access to medical care for these patients may have also been a factor effective on the decision for surgery or marriage. However, Turkey provides universal health care free of charge; all evaluations, surgeries, and followup studies are free. Therefore, none of the patients should have declined surgery because of financial constraints.
We found substantial improvements in overall social function and status for the patients who underwent THA, even with a brief duration of followup. Patients with DDH who underwent THA were more likely to gain employment and to marry. Furthermore, the spouses of those who married after THA were free from physical disability, which shows much improved acceptance into society and possibly better chances for social interaction with those who—after surgery—do not see them as disabled. In regard to depression, the percentage of patients who were diagnosed with depression was substantially lower in those who underwent surgery compared with the non-THA group. In a study that evaluated the depression and anxiety levels of patients with DDH after THA, it was reported that depression and anxiety levels of patients decreased in direct proportion to perceived limb length discrepancy [11]. In other words—similar to our findings—cosmetic expectations had a direct impact on patients’ well-being, despite adjusting for pain and functional improvement.
In keeping with other studies, we found that patients undergoing THA for DDH experienced substantial improvement in QOL, as measured by the SF-36. We found that QOL was increased in those who underwent surgery compared with their baseline results and also the baseline results of those who did not undergo THA. There are only a few studies that report results from similar patient groups; Roidis et al. [12] reported an improvement in QOL after THA was performed for DDH. Knutsson and Engberg [9] also reported improvements in the general, physical, and psychosocial QOL of patients who underwent THA. Tellini et al. [15] reported that QOL was improved in patients who underwent hip replacement for DDH. Likewise, a study by Sanei et al. [13] showed that the mean SF-36 scores of patients with DDH increased from 27.41 to 79.12 points after THA, an immense improvement in QOL. In the present study, the increase in the scores of SF-36 subsections ranged from 22.0 to 58.64 points in patients who underwent THA. We also compared the SF-36 results of patients who underwent THA with those who did not. Although there was no difference between groups preoperatively, the THA group had substantial improvement in all SF-36 subsections postoperatively. Sanei et al. [13] observed the highest improvement in the pain subsection, whereas we found the highest improvement was in the social role function closely followed by the mental health subsection. Cultural differences and social expectations may have contributed to this difference. However, we believe that the relatively younger mean age in our study was a major factor; younger patients may experience more of the social and psychologic effects of DDH. Thus, the benefits of surgery may have been more pronounced in these subsections for our patients.
Other studies have shown improvements in pain and function after THA for DDH [8, 16], and our findings generally were consistent with the results of those studies. In addition, we observed a decrease in functionally limiting pain complaints in both groups. At baseline evaluation, patients in the THA group had more self-reported lumbar and knee pain than the non-THA group. This may have been a factor that could have directly affected the decision for surgery in these patients. Overall, the THA group had greater reduction of pain complaints after intervention.
In some traditional, patriarchal cultures, social standing, lifestyle, and QOL of young people—especially young women—is adversely affected by DDH. We found that THA in these patients was associated both with improvements in social standing and QOL compared with women whose DDH symptoms were managed without THA. These improvements may have been a function of cosmetic improvements (such as amelioration of leg length differences), functional improvements (improvement in gait), or other factors. In many more traditional cultures, social standing is of critical importance and should be considered and discussed in the context of surgical decision-making, because patients may have unstated expectations and concerns on those topics as they contemplate treatment options. In Turkey, a patriarchal culture, we found that young women who underwent THA for DDH appeared to derive not just pain-related and QOL benefits, but also improvements in social standing, which may have provided them more freedom in terms of life choices.
Acknowledgments
We thank Prof Dr Murat Altay, Prof Dr Erbil Aydın, Dr Hasan Yıldırım (our clinical supervisor), and anesthesiologist assistant Dr Alpay Ateş for their valuable contributions on diagnosis confirmation and operative decisions. We also thank our clinic nurses Elif Ateş and Hülya Çoban for their assistance to this study.
Footnotes
Each author certifies that neither he, nor any member of his immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
The work was performed at the Karabük Research and Training Hospital, Karabük, Turkey.
References
- 1.Brazier JE, Harper R, Jones NM, O'Cathain A, Thomas KJ, Usherwood T, Westlake L. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305:160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buz S. Feminist social work practice. Journal of Society & Social Work. 2009;20:53–65. [Google Scholar]
- 3.Buz S, Karabulut A. Orthopedically handicapped women: a study in the framework of gender. Igdir University Journal of Social Sciences. 2015;7:25–45. [Google Scholar]
- 4.Dezateux C, Rosendahl K. Developmental dysplasia of the hip. Lancet. 2007;369:1541–1552. [DOI] [PubMed] [Google Scholar]
- 5.Garbuz DS, Awwad MA, Duncan CP. Periacetabular osteotomy and total hip arthroplasty in patients older than 40 years. J Arthroplasty. 2008;23:960–963. [DOI] [PubMed] [Google Scholar]
- 6.Hartofilakidis G, Karachalios T, Stamos KG. Epidemiology, demographics, and natural history of congenital hip disease in adults. Orthopedics. 2000;23:823–827. [DOI] [PubMed] [Google Scholar]
- 7.Hartofilakidis G, Lampropoulou-Adamidou K. Lessons learned from study of congenital hip disease in adults. World J Orthop. 2016;7:785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jitesh Kumar J, Agarwal S, Sharma RK. Total hip replacement in Crowe type IV dysplastic hips—average 5 year follow-up and literature review. Acta Orthop Belg. 2016;82:539–548. [PubMed] [Google Scholar]
- 9.Knutsson S, Engberg IB. An evaluation of patients’ quality of life before, 6 weeks and 6 months after total hip replacement surgery. J Adv Nurs. 1999;30:1349–1359. [DOI] [PubMed] [Google Scholar]
- 10.Kocyigit H. Reliability and validity of the Turkish version of Short Form-36 (SF-36): a study in a group of patients will rheumatic diseases. Turk J Drugs Ther. 1999;12:102–106. [Google Scholar]
- 11.Liu R, Li Y, Fan L, Mu M, Wang K, Song W. Depression and anxiety before and after limb length discrepancy correction in patients with unilateral developmental dysplasia of the hip. J Psychosom Res. 2015;79:574–579. [DOI] [PubMed] [Google Scholar]
- 12.Roidis NT, Pollalis AP, Hartofilakidis GC. Total hip arthroplasty in young females with congenital dislocation of the hip, radically improves their long-term quality of life. J Arthroplasty. 2013;28:1206–1211. [DOI] [PubMed] [Google Scholar]
- 13.Sanei F, Jameh BAA, Irani A, Akbarzadeh BA, Ghoreishi M. Comparing the quality of life before and after total hip arthroplasty operation in patients with developmental dysplasia of the hip. Physical Treatments-Specific Physical Therapy Journal. 2016;5:219–224. [Google Scholar]
- 14.Shorter D, Hong T, Osborn DA. Cochrane Review: Screening programmes for developmental dysplasia of the hip in newborn infants. Evid Based Child Health. 2013;8:11–54. [DOI] [PubMed] [Google Scholar]
- 15.Tellini A, Ciccone V, Blonna D, Rossi R, Marmotti A, Castoldi F. Quality of life evaluation in patients affected by osteoarthritis secondary to congenital hip dysplasia after total hip replacement. J Orthop Traumatol. 2008;9:155–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu J, Wang Y, Pang J, Lü B, Huang C, Hao P, Tan B. [Effectiveness of total hip arthroplasty for severe developmental dysplasia of hip in adults] [in Chinese]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2014;28:335–338. [PubMed] [Google Scholar]