Abstract
Hepatic encephalopathy (HE) markedly reduces an individual's quality of life as measured by established scoring systems. However, the experiences of having HE that can be assumed to cause the loss of quality of life have not yet been examined. This study aimed to explore how individuals with cirrhosis experienced overt HE by means of an in-depth interview with a tailored semistructured interview guide and qualitative analysis. Eight patients with cirrhosis who had clinically recovered from disorientation, somnolence, and stupor due to episodic HE Grade II or III were interviewed. The collected data were analyzed using systematic text condensation, as described by K. Malterud (2012). The analysis process identified 4 themes, “multiple losses,” “anxiety,” “dependence on others,” and “social isolation,” which described the experiences of HE both during an episode and in recovery. We believe that these findings provide an important contribution to gain a deeper understanding of the widespread loss of quality of life caused by HE. Management of these individuals should involve procedures and attitudes targeted against the described experiences. However, more research is needed about the individuals' experiences of HE to further detail such efforts.
Hepatic encephalopathy (HE) is a reversible cerebral dysfunction with a wide spectrum of nonspecific neurological and psychiatric disturbances. It manifests as a continuum and can be categorized into several stages, from subtle cognitive changes measurable only using psychometric methods (minimal HE) to stages with clinically evident personality changes (Grade I), disorientation and asterixis (Grade II), somnolence and stupor (Grade III), and coma (Grade IV) (Conn et al., 1977).
It is estimated that HE Grade II and above (“overt”) will occur in 30%–40% of patients with cirrhosis at some time during their clinical course, as well as repeatedly in most cases of survivors. Minimal HE is most likely present at any time in more than half of patients with cirrhosis, and half of these patients will subsequently experience overt HE (Lauridsen, Jepsen, & Vilstrup, 2011; Sharma & Sharma, 2015).
Background
Hepatic encephalopathy is a prevalent and very serious complication of cirrhosis (Conn, 1993) and a common cause of hospital admissions and readmissions (Sørensen et al., 2003; Zhou, Zhang, & Qiao, 2014). The cognitive dysfunction related to HE can affect patients' ability to maintain personal hygiene and perform basic activities of daily living. In addition, HE can affect the ability to drive and work, which may lead to a negative impact on patients' finances and socioeconomic status (Bajaj et al., 2011; Chaney, Werner, & Kipple, 2015). Overall, HE is currently the most debilitating manifestation of cirrhosis affecting patients, healthcare providers, and the healthcare system.
Studies have shown that health-related quality of life is significantly impaired in patients with cirrhosis (Abdi, Daryani, Khorvash, & Yousefi, 2015; Younossi & Henry, 2015). In addition, it is well established that patients with HE have a very poor quality of life, as consistently described by quality-of-life scoring systems that show most of the physical, mental, and social domains are severely compromised (Agrawal, Umapathy, & Dhiman, 2015; Barboza et al., 2016; Groeneweg et al., 1998; Marchesini et al., 2001; Orr et al., 2014). The reasons for these profound damages on patients' lives have thus far not been identified and are not particularly seen from the patient-experienced perspective (i.e., the “insider” perspective). With this background, the aim of this study was to systematically examine how patients with cirrhosis experience overt HE.
Methods
Study Design and Sample
A qualitative approach was selected as appropriate because the research aim sought to provide a comprehensive description of the study participants' lived experiences of HE (Davidsen, 2013; Polit, Beck, & Hungler, 2001). The participants were consecutively recruited from the Department of Hepatology and Gastroenterology at Aarhus University Hospital.
Inclusion criteria included patients with an established diagnosis of liver cirrhosis undergoing treatment and follow-up who had recovered from an episode of HE Grade II or III for which they had been hospitalized within the last 6 weeks. Furthermore, the participants should be native Danish speakers. Because of the diagnostic difficulties regarding minimal HE, we did not include such patients in this study (Lauridsen et al., 2011). Also, because of the uncertain memory function during HE Grade IV, such patients were not included. The diagnosis of HE as well as a complete clinical recovery was ascertained by specialized hepatologists. Exclusion criteria were dementia or mental illness and competing causes for cerebral involvement, such as heart or lung failure (Lauridsen & Bajaj, 2015). The inclusion period was 4 weeks in the spring of 2015.
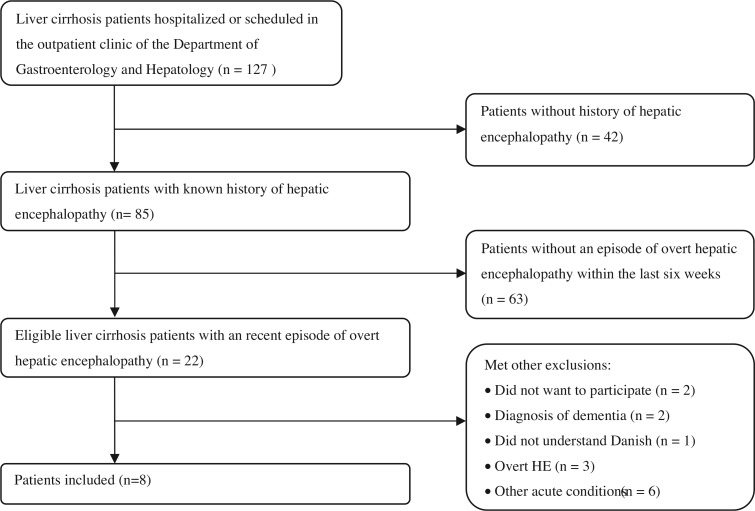
Ten participants were invited to participate. Eight patients accepted and two declined because of fatigue. The mean time since the last hospitalization caused by HE was 27 days. All the participants had experienced two or more episodes of overt HE (Grades II–IV). At the time of the interview, four patients received prophylactic treatment in the form of lactulose (all four), rifaximin add-on (two patients), and oral branched-chain amino acids add-on (one patient). The participant flow is illustrated in Figure 1. Table 1 shows participants' demographic and clinical characteristics.
FIGURE 1.
Flow chart of participant inclusion.
TABLE 1. Demographic and Clinical Characteristics of Participants.
| Variable | Cirrhosis Patients (n = 8) |
|---|---|
| Clinical features | |
| Age, mean (range) (years) | 61 (51–72) |
| Women | 62% |
| Etiology of cirrhosis | |
| Alcoholic | 50% |
| Cryptogenic | 25% |
| Autoimmune hepatitis | 25% |
| Severity of cirrhosis | |
| Child Pugh score (mean and range) | 7 (5–11) |
| Model of end-stage liver disease (mean and range) | 10 (7–19) |
| History of hepatic encephalopathy | |
| 2 episodes | 25% |
| >2 episodes | 75% |
| Family status | |
| Single/divorced/widower | 38% |
| Married/cohabiting | 62% |
| Occupation | |
| Sick leave | 25% |
| Unemployed | 38% |
| Disability pensioner | 12% |
| Retired | 25% |
Data Collection
The interviews were performed when participants had appointments at the hospital for planned procedures (four patients) or at the outpatient clinic (four patients). Before the interviews, the participants were informed about the aim of the study. Each interview lasted for at least 30 minutes and was performed in a secluded room by the same interviewer, who had no previous relationship with the patients. Patients were interviewed until no additional or new information regarding HE was identified. This was consistent with an understanding of data saturation within qualitative studies (Lincoln & Guba, 1985; Patton, 2002). All interviews were taped and transcribed verbatim by the interviewer. A total of 63 pages emerged after the transcription.
Interview Guide
To obtain an in-depth knowledge of the participants' experiences, an HE-targeted interview guide was developed. The interviews were semistructured, and topics and questions for the interviews were determined in advance but the structure was open, allowing the patients to provide detailed narratives about their experiences of HE (Kvale & Brinkmann, 2009). The interview guide consisted of both broad and specific questions that centered on HE, its patterns, consequences, and recovery as experienced by the patients. The guide reflected the aim of the study and included three main topics inspired by the literature on cirrhosis patients' quality of life (Table 2). The questions were open-ended, so that the participants were able to express their personal and individual experiences and concerns relating to the three topics. This allowed the participants to contribute as much detailed information as they desired, and it also allowed the interviewer to ask probing questions as a follow-up (Kvale & Brinkmann, 2009). At the end of each interview, participants were given the opportunity to provide additional comments. The interview guide was piloted twice, which involved minor linguistic corrections.
TABLE 2. Interview Guide With Topics for the Interviews.
| Main Topics | Items of Discussion |
|---|---|
| Introduction | Aim of the study |
| Pattern of hepatic encephalopathy (HE) | When was the last time you had an episode of HE? Can you remember what happened? How did you react? How would you experience an episode of HE? |
| Consequences of HE | How does HE affect your daily life? Have you experienced any changes in needs during or after an episode of HE? Is something more important to you now? |
| Recovery of HE | How does it affect you that HE is recurrent? How often do you think about it? When did you last think about it and why? How do you feel, when you think about it? |
| Additional comments | Is there anything you would like to add? |
Analysis
The interviews were analyzed because of the principles of systematic text condensation, as described by Malterud, who developed this method from inspiration by Giorgi's psychological phenomenological approach (Malterud, 2012). This method involves four steps. The first step refers to obtaining an overall sense of the data, while the other phases represent the deeper analysis.
First, each interview transcription was read repeatedly to establish an overview of the data and to obtain an overall impression of the entire material. Special attention was paid to the participants' experiences that illustrated a variation of the aspects of HE, and preliminary themes were considered as a starting point to organize the data.
In the second step, the interview transcriptions were systematically reviewed line by line to identify meaning units (i.e., text fragments that expressed aspects of how cirrhosis patients experience HE). Every meaning unit was marked with a label to identify how the meaning units could be classified and grouped under new headings that related to the previous themes. This involved an iterative process of adjusting headings and labels.
The third step of the analysis implied a reduction of the interview transcriptions. First, the meaning units were temporarily removed from their original contexts and organized into thematic groups across the individual patients. Next, the meaning units were reduced by text condensation (i.e., creating a reduced text that was close to the patients' own expressions). These text condensations served as a point of departure for the analysis in progress. During this process, subgroups were identified to explore the depth, nuances, and complexity of the patients' experiences. To stay close to the original data, the condensations were illustrated by relevant quotations.
The fourth step involved a recontextualization of the data. This was obtained by synthesizing the content of each thematic group into new descriptions and concepts that reflected important aspects of the patients' experiences of HE. Finally, all interview transcriptions were read again to ensure the validity and accuracy with the entire original data set. In addition, a systematic search for data from the interview transcriptions that might challenge the results was performed (Malterud, 2012). Table 3 illustrates the steps of the analysis.
TABLE 3. Illustration of the Analytical Steps.
| Preliminary Themes | Meaning Units | Condensation | Final Theme |
|---|---|---|---|
| Consequences for daily life | It all happened so fast. Now life is boring. I'm stuck at home with nothing to do. I need help to get up in the morning, during the day, and when I go to bed. My wife goes to work every day as normal, I just sit at home. I eat 30 pills every day! I can't go outside because I get dizzy. I used to drive my car and go to work, but now I can't. I will never go back to work. I'm not fired yet but I'm going to be. | The consequences of HE means a changed and reduced life. This is experienced as difficult and involves feelings of loss of identity and brought feelings of sadness accompanied by sense of reduced meaning with life. | Multiple losses |
Ethical Considerations
All participating patients were given verbal and written information regarding the aim of the study and its voluntary nature prior to the interview. The study was reviewed by the Central Denmark Region Committee on Biomedical and Research Ethics. No formal approval was required because of its nonbiomedical character. The study was performed according to the Declaration of Helsinki.
Findings
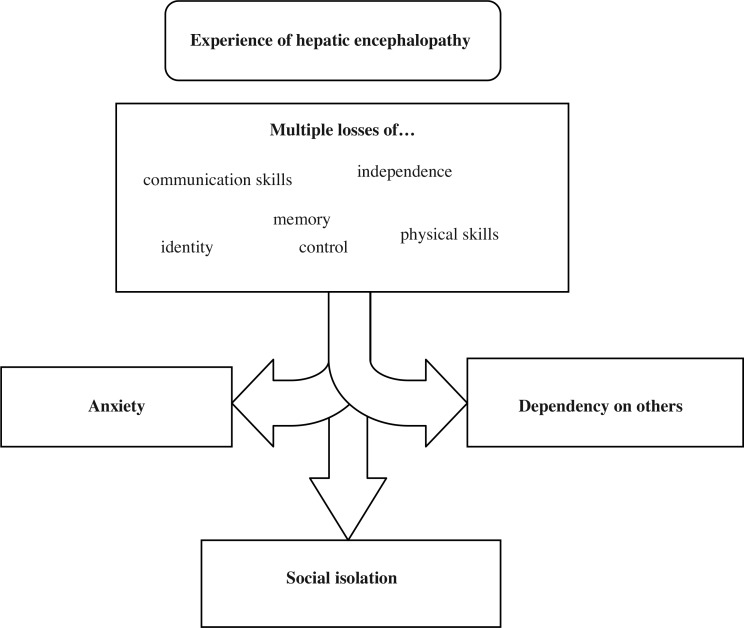
The analysis process identified four themes which described the experience of HE both during an episode and in recovery. The prevailing theme “multiple losses” describes the participants' loss of memory, physical and communicative abilities, control, and identity. This main theme led to the three other identified themes: “anxiety,” “dependency of others,” and “social isolation” (Figure 2). The themes are strongly interrelated. Within each theme, the memories of episodes with HE are presented first followed by the actual experiences in recovery. Quotes selected from the original data are provided as examples to illustrate the identified meanings (Malterud, 2012).
FIGURE 2.
Themes revealed by systematic text condensation. Four themes describe the experience of hepatic encephalopathy during an episode and in recovery. The main theme of “multiple losses” led to three other identified themes: “anxiety,” “dependency of others,” and “social isolation.”
Multiple Losses
All of the participants were experiencing or had experienced the same type of essential losses; however, they were expressed in different ways and affected the participants differently.
The participants had experienced loss of communication skills during an episode of overt HE. They could sense that what they were saying only made sense to themselves and not to other people. However, it was impossible for them to correct themselves:
Around Christmas and New Year I was hospitalized with my first episode of HE. I thought I answered the doctor correctly, but it was gibberish... I thought I said it right, but I didn't... It was nonsense. It was simple questions like what day is it, when is your birthday. My brain told me to say some nonsense because it felt right.
At the same time, the participants also experienced problems with expressing their needs. It made life difficult for them. They also experienced a loss of physical skills and thus dependency on others. This led to a loss of independence:
I can remember once I have been in liver coma. I had to go to the toilet... Normally I'm able to do that, but this time I could not figure out how to do it. Then, I called for a nurse and she said: “You are able to do it yourself.” However, in that situation, I didn't know what I was supposed to do, I could not figure it out. It was scary and frightening.
A loss of independence created frustration, feelings of uselessness, and sadness due to a sense of a loss of control. Hepatic encephalopathy also led to situations where the participants felt that they were no longer themselves. This resulted in the feeling of a loss of identity:
I could not remember how old I was or my social security number. I was really sad and upset. I kept asking the doctor if he thought I ever would become normal again, and he answered. “Yes, you will.” I asked him, “Are you sure, what if the treatment does not work?” Then, he answered: “Then, we will try something else.”
Even when recovering, HE patients experienced losses. Thus, after hospitalization, some participants experienced difficulties with concentration and memory. They described how embarrassing they felt when they discovered that they repeatedly forgot ordinary things or names:
Anyway, it was still a problem when I got home. I can't remember. My memory is not good anymore. My memory is bad after an episode of HE.
The participants were aware of the difficulties they were experiencing in relationship to HE. Apart from the frustration of not being able to accomplish basic activities of daily living and remembering things, they were embarrassed about their failure and felt incompetent and clumsy, which made them angry with themselves:
Sometimes, I pour the coffee into the cup, open the refrigerator and put the coffee in there. Then, I go back to the living room to sit on the couch. It is such an idiotic thing to do.
Many of the participants felt that they had lost their previous lives and that the life they now lived was very different and not as good as the life before they had HE. Participants perceived this as difficult and it involved a feeling of a loss of identity. The loss of their previous lives elicited feelings of sadness accompanied by a sense of reduced meaning with life (see Table 3).
Anxiety
Hepatic encephalopathy was described by all participants as terrifying and a cause of anxiety. The anxiety appeared both during and after an episode of HE.
During an episode of HE, the participants were disorientated and confused and could not understand what was happening around them. Participants decried the fear and anxiety that they felt when they found themselves somewhere between consciousness and unconsciousness:
I was so terrified. I could see a man and I could hear a woman's voice, but I could not see her. She shouted at me, “Now you really need to keep your hands away from the instruments.” She was talking very loudly and in an aggressive tone. However, how else are you going to stop a person who is hurting herself? I was terrified and frightened... The first thought that went through my mind was, “What am I doing here? Have I been in an accident?” I was so scared... I looked at him and wanted him to tell me why I was lying here, but I could not say anything. He did not say anything, because he did not know that I wanted him to tell me.
The lack of knowledge of why the participants reacted the way that they did and the inability to communicate caused a loss of control and thus anxiety. The patients wanted the healthcare providers to reassure them and inform them about their situation, but they had experienced problems with communicating this to the healthcare providers.
The participants also experienced anxiety associated with HE as a result of their sudden functional limitations:
I was really, really sad this time because I was disorientated and could not do anything. I could not write, I could not eat by myself, I could not go to the bathroom on my own, and it was difficult for me to talk. HE had a huge impact on me this time; it was really frightening to experience. I was completely beside myself. Deep down I knew it was me, but it was like I could not do anything. It made me anxious.
When recovering from HE, participants wished to know how long the episode of HE had lasted, as well as what had happened during the episode. Without this knowledge, they felt insecure. In addition, they were constantly afraid of recurrence. They tried to sense when a new episode of HE was on the way, and they were terrified if they suddenly could not remember words or perform basic everyday life activities:
I was scared all the time. What would happen the next time I had trouble finding the words? Is it now a new episode of HE? I could not keep calm. I was afraid and stressed all the time. I think I was close to a mental breakdown. When I had experienced several episodes of HE, I began to talk to a psychologist, and that was a great help for me.
Dependency of Others
The decreased ability to perform basic activities was a major concern to the participants. During episodes of HE, they experienced dependency for care and treatment, as well as a need for protection and support from relatives and healthcare providers. Participants received help in private and intimate situations, such as going to the toilet or maintaining personal hygiene. It was frustrating for the participants and far from their former life. For some, it was difficult to accept:
It is so degrading to have people to help you. It is so degrading for a man—then there is not much man left in you... I would not wish for you to try it.
Participants also described the loss of independence when they had recovered from HE. They described that they could no longer do what they wanted. This made the participants feel isolated and reminded them of their vulnerable situation:
When I have to eat, the food must be cut up. Cut up just as for small children. And then I eat with a spoon... I cannot just go on vacation. I cannot just this or that because I need help every day of the year. Then, you're stuck.
Most participants reported that they were more dependent on their spouses after HE. This resulted in an uneven balance in the matrimonial relationship, resulting in ambiguous feelings. On the one hand, it meant a lot to them that their spouse helped them; on the other hand, it was difficult for the participants to see what they no longer were able to do themselves. It made the participants feel like a burden:
Then, you grow fonder of your spouse who has been there for 40 years now. She does a great job. I can sit in my chair and see her work. I cannot help with anything anymore. It is really annoying.
Social Isolation
The episode of HE and its recovery phase resulted in an inability or limited capacity to participate in social events and socialize with relatives. Thus, participation in activities once enjoyed was affected by HE, leading to social isolation:
I have been involved in music associations, running clubs and so on. However, now I cannot handle it anymore. Now I sit at home doing nothing. I cannot even use the computer to look at Facebook or anything. The worst thing is that you get used to it. I'm used to sleeping for many hours in the day because I have nothing else to do.
Reduced participation in social events and a reluctance to ask for assistance from relatives resulted in self-imposed isolation as the participants sought to protect themselves by keeping their distance. In addition, they did not want to be seen as a nuisance or a burden to others:
I do not go to parties anymore. I don't want to because I need people to help me. I don't like to. So it (HE) leads to a kind of isolation.
Stigmatization was a significant part of their experience of social isolation. Participants were afraid to talk about their disease because they did not want to be labelled as alcoholics due to the general lack of knowledge of liver cirrhosis. Similarly, participants were afraid to talk to relatives about their episodes of HE, as they feared to be viewed as mentally ill. This resulted in participants not feeling that they had anyone to talk to:
The liver cirrhosis I could not understand because I've never drank. And it is said that liver cirrhosis is due to drinking. I heard that a lot. Therefore, I stopped saying that I have cirrhosis because then I don't have to constantly defend myself... You do not meet anyone you can really talk to about this. And HE... For others, it will be like you have been mentally ill for a period, but now it's over.
Discussion
This is the first qualitative study to investigate how patients with cirrhosis experience HE. These results clearly indicate that HE depreciated the participants' lives by their experiences of losses, anxiety, dependency, and isolation. We used a qualitative design to uncover these patterns of experience to create a new understanding of why and how HE affects the patients' quality of life as measured using quantitative standardized questionnaire studies reporting to what extent HE negatively affects the physical and mental domains of life (Arguedas, DeLawrence, & McGuire, 2003; Groeneweg et al., 1998).
Encephalopathy is a broad term used to describe a cerebral dysfunction with an altered mental state (Katramadon & Varelas, 2010), usually in the absence of structural brain disease. We have not been able to find literature about the experience of encephalopathy of different etiologies. Thus, we do not know whether the clearly categorized findings of our study are specific for HE or are general traits of other types of encephalopathy.
The World Health Organization classifies HE as a delirium (World Health Organization, 1992). In qualitative studies, delirious patients have described emotional suffering from anxiety, fear of recurrence, and embarrassment of having hallucinated and suspicious of healthcare providers (Laitinen, 1996; Partridge, Martin, Harari, & Dhesi, 2013). This is, to a certain extent, consistent with the findings from our study. However, as expected, participants with HE did not complain about hallucinations (Rosenberg, Renvillard, & Hjerrild, 2013), making HE distinct from other delirious states. Likewise, our HE participants described a sustained great impact on them and their lives after recovery, which was not found in delirium.
The participants described that during HE, they were aware that something unpleasant was happening with and around them. However, their loss of communication skills prohibited them from expressing themselves, resulting in anxiety. In the recovery phase, the anxiety was maintained by the participants' fear of HE recurrence. It has been shown that people with cirrhosis have a poor understanding of their disease and lack adequate knowledge about complications (Valery et al., 2015). However, it has also been shown that simple educational intervention highly improves this situation (Volk, Fisher, & Fontana, 2013). Such education may involve so-called therapeutic communication, in which patients may talk about their experience (McCurren & Cronin, 2003). Such communications also enable the healthcare providers to cope with and plan for future HE episodes.
Another consistent finding was that HE resulted in an increased dependency on others. The mental impairments of HE combined with the complex management of the physical aspects of cirrhosis indicated that these individuals are faced with specific and high levels of supportive care needs (Rakoski et al., 2012). However, in contrast to, for example, heart failure and chronic obstructive pulmonary disease, supportive care standards are not yet established, which may be rooted in the traditional focus on the physical aspects of disease.
In addition, the social life of HE patients was seriously impeded. They no longer mastered or wished to participate in social activities, and they fell into social isolation, which was deepened by their feelings of stigmatization by suspicions of being alcoholics or mentally ill. This result was consistent with the findings that the majority of cirrhosis patients feel stigmatized by their disease, leading to depression, low social support, and a poor quality of life (Vaughn-Sandler, Sherman, Aronsohn, & Volk, 2014). This was not limited to the participants' social surroundings. Even among healthcare providers, cirrhosis may be considered a condition ranking lower than depression, schizophrenia, and AIDS (Album & Westin, 2008). These aspects should be included in patient-staff education.
Study Limitations
There are limitations of this study. First, the interviews occurred at the hospital or outpatient clinic; the environment might not be convenient from the participants' perspective, which may have affected their responses. The timing of the interview may also have had an effect on the data. The participants were interviewed immediately after they had agreed to participate. More time for the interview preparation may have led the participants to reflect more deeply on their experiences or to provide additional knowledge. However, the participants were able to provide concrete examples of their experience of HE. Second, although the included participants had experienced a recent episode of overt HE, some responses may be subject to recall bias, and it may have been difficult for the participants to fully separate their experiences of different episodes and grades of HE. Third, the participants were selected from one University Hospital, and this may not provide variations of data; however, within this methodology, variation is not related to demographic characteristics but to variations of experiences (Norlyk & Harder, 2010; Todres, 2005). Fourth, the present sample size is small, but this sample size corresponds with the notion that in qualitative studies, sampling is not about size but about quality (Kvale & Brinkmann, 2009; Patton, 2002). Although the results cannot be fully generalized, we believe our study to be a useful contribution to the sparse knowledge on individuals' experiences of HE; this may motivate further studies in this field. The interview guide we developed and used in this study might be useful to enable comparisons among future interview studies.
Implications for Practice
There has not been much focus on interventions for the practice to improve' life after HE beyond medical therapy. However, our study emphasizes the need and probable utility of disease education of HE patients based on therapeutic communication. This requires that healthcare providers working with cirrhosis patients have specialist knowledge on the prevention and care of HE.
The experience of isolation and stigmatization found in this study needs to be addressed. Thus, social groups could be facilitated to help support patients and their relatives. Likewise, an assessment of the patients' supportive care needs by questionnaire is essential to explore their supportive care concerns. It would increase the likelihood of appropriate and comprehensive need identification and may be useful in clinical practice to tailor interventions most effectively.
Conclusion
This study adds a new dimension to the existing knowledge of how HE is experienced by individuals both during an episode and in recovery. The qualitative design has identified a previously unknown understanding of the impact of HE on patients. The results indicate that HE affects the participants' lives by multiple losses, anxiety, dependency, and isolation. Therefore, of importance for daily clinical practice, the management of HE needs targeted attention and adequate treatment, to improve the care and quality of life of individuals living with cirrhosis.
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- Abdi F., Daryani N. E., Khorvash F., Yousefi Z. (2015). Experience of individuals with liver cirrhosis. A qualitative study. Gastroenterology Nursing, 38(4), 252–257. [DOI] [PubMed] [Google Scholar]
- Agrawal S., Umapathy S., Dhiman R. K. (2015). Minimal hepatic encephalopathy impairs quality of life. Journal of Clinical and Experimental Hepatology, 5(Suppl. 1), 42–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Album D., Westin S. (2008). Do diseases have a prestige hierarchy? A survey among physicians and medical students. Social Science & Medicine, 66(1), 182–188. [DOI] [PubMed] [Google Scholar]
- Arguedas M. R., DeLawrence T. G., McGuire B. M. (2003). Influence of hepatic encephalopathy on health-related quality of life in patients with cirrhosis. Digestive Diseases and Sciences, 48(8), 1622–1626. [DOI] [PubMed] [Google Scholar]
- Bajaj J. S., Wade J. B., Gibson D. P., Heuman D. M., Thacker L. R., Sterling R. K. (2011). The multi-dimensional burden of cirrhosis and hepatic encephalopathy on patients and caregivers. American Journal of Gastroenterology, 106(9), 1646–1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barboza K. C., Salinas L. M., Sahebjam F., Jesudian A. B., Weisberg I. L., Sigal S. H. (2016). Impact of depressive symptoms and hepatic encephalopathy on health-related quality of life in cirrhotic hepatitis C patients. Metabolic Brain Disease, 31(4), 869–880. [DOI] [PubMed] [Google Scholar]
- Chaney A., Werner K. T., Kipple T. (2015). Primary care management of hepatic encephalopathy: a common cirrhosis complication. Journal of Nursing Practice, 11(3), 300–306. [Google Scholar]
- Conn H. O. (1993). Hepatic encephalopathy. In Schiff L., Schiff E. R. (Eds.), Diseases of the liver (7th ed., pp. 1036–1060). Philadelphia, PA: Lippincott. [Google Scholar]
- Conn H. O., Leevy C. M., Vlachevic Z. R., Rodgers J. B., Maddrey W. C., Seeff L., Levy L. L. (1977). A comparison of lactulose and neomycin in the treatment of portal-systemic encephalopathy: A double-blind controlled trial. Gastroenterology, 72(4), 573–583. [PubMed] [Google Scholar]
- Davidsen A. S. (2013). Phenomenological approaches in psychology and health sciences. Qualitative Research in Psychology, 10(3), 318–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groeneweg M., Quero J. C., De Bruijn I., Hartmann I. J., Essink-Bot M. L., Hop W. C., Schalm S. W. (1998). Subclinical hepatic encephalopathy impairs daily functioning. Hepatology, 28(1), 45–49. [DOI] [PubMed] [Google Scholar]
- Katramadon A., Varelas P. (2010). Encephalopathy. In Torbey M. (Ed.), Neurocritical care (pp. 220–226). New York, NY: Cambridge University Press. [Google Scholar]
- Kvale S., Brinkmann S. (2009). InterViews: Learning the craft of qualitative research interviewing (2nd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Laitinen H. (1996). Patients' experience of confusion in the intensive care unit follow cardiac surgery. Intensive & Critical Care Nursing, 12(2), 79–83. [DOI] [PubMed] [Google Scholar]
- Lauridsen M. M., Bajaj J. S. (2015). Hepatic encephalopathy treatment and its effect on driving abilities: A continental divide. Journal of Hepatology, 63(1), 287–288. [DOI] [PubMed] [Google Scholar]
- Lauridsen M. M., Jepsen P., Vilstrup H. (2011). Critical flicker frequency and continuous reaction times for the diagnosis of minimal hepatic encephalopathy: a comparative study of 154 patients with liver disease. Metabolic Brain Disease, 26(2), 135–139. [DOI] [PubMed] [Google Scholar]
- Lincoln Y. S., Guba E. G. (1985). Naturalistic inquiry. Newbury Park, CA: Sage. [Google Scholar]
- Malterud K. (2012). Systematic text condensation: A strategy for qualitative analysis. Scandinavian Journal of Public Health, 40(8), 795–805. [DOI] [PubMed] [Google Scholar]
- Marchesini G., Bianchi G., Amodio P., Salerno F., Merli M., Panella C., Abbiati R. (2001). Factors associated with poor health-related quality of life of patients with cirrhosis. Gastroenterology, 120(1), 170–180. [DOI] [PubMed] [Google Scholar]
- McCurren C., Cronin S. N. (2003). Delirium: Elders tell their stories and guide nursing practice. Medsurg Nursing, 12(5), 318–323. [PubMed] [Google Scholar]
- Norlyk A., Harder I. (2010). What makes a phenomenological study phenomenological? An analysis of peer-reviewed empirical nursing studies. Qualitative Health Research, 20(3), 420–431. [DOI] [PubMed] [Google Scholar]
- Orr J. G., Homer T., Ternent L., Newton J., McNeil C. J., Hudson M., Jones D. E. J. (2014). Health related quality of life in people with advanced chronic liver disease. Journal of Hepatology, 61(5), 1158–1165. [DOI] [PubMed] [Google Scholar]
- Partridge J. S. L., Martin F., Harari D., Dhesi J. K. (2013). The delirium experience: What is the effect on patients, relatives and staff and what can be done to modify this? International Journal of Geriatric Psychiatry, 28(8), 804–812. [DOI] [PubMed] [Google Scholar]
- Patton M. Q. (Ed). (2002). Qualitative research & evaluation methods (3rd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Polit D. F., Beck C. T., Hungler B. P. (Eds.). (2001). Essentials of nursing research: Methods, appraisal, and utilization (5th ed.). Philadelphia, PA: Lippincott. [Google Scholar]
- Rakoski M. O., McCammon R. J., Piette J. D., Iwashyna T. J., Marrero J. A., Lok A. S., Volk M. L. (2012). Burden of cirrhosis on older Americans and their families: Analysis of the health and retirement study. Hepatology, 55(1), 184–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg R., Renvillard S. G., Hjerrild S. (2013). Organic delirious states and other psychiatric disorders: Lessons for the hepatologists. Metabolic Brain Disease, 28(2), 235–238. [DOI] [PubMed] [Google Scholar]
- Sharma P., Sharma B. C. (2015). Management of overt hepatic encephalopathy. Journal of Clinical and Experimental Hepatology, 5(Suppl. 1), 82–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sørensen H. T., Thulstrup A. M., Mellemkjar L., Jepsen P., Christensen E., Olsen J. H., Vilstrup H. (2003). Long-term survival and cause-specific mortality in patients with cirrhosis of the liver: A nationwide cohort study in Denmark. Journal of Clinical Epidemiology, 56(6), 88–93. [DOI] [PubMed] [Google Scholar]
- Todres L. (2005). Clarifying the life-world: Descriptive phenomenology. In Holloway I. (Ed.), Qualitative research in health care (pp. 104–124). London: Open University Press. [Google Scholar]
- Valery P. C., Powell E., Moses N., Volk M. L., McPhail S. M., Clark P. J., Martin J. (2015). Systematic review: Unmet supportive care needs in people diagnosed with chronic liver disease. BMJ Open, 5(4), e007451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughn-Sandler V., Sherman C., Aronsohn A., Volk M. L. (2014). Consequences of perceived stigma among patients with cirrhosis. Digestive Diseases and Sciences, 59(3), 681–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volk M. L., Fisher N., Fontana R. J. (2013). Patient knowledge about disease self-management in cirrhosis. American Journal of Gastroenterology, 108(3), 302–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Younossi Z., Henry L. (2015). Overall health-related quality of life in patients with end-stage liver disease. Clinical Liver Disease, 6(1), 9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (1992). The ICD-10 classification of mental and behavioural disorders. Clinical descriptions and diagnostic guidelines. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Zhou W. C., Zhang Q. B., Qiao L. (2014). Pathogenesis of liver cirrhosis. World Journal of Gastroenterology, 20(23), 7312–7324. [DOI] [PMC free article] [PubMed] [Google Scholar]