Abstract
Background
The Medicare Access and CHIP Reauthorization Act of 2015 provides the framework to link reimbursement for providers based on outcome metrics. Concerns exist that the lack of risk adjustment for patients undergoing revision TKA for an infection may cause problems with access to care.
Questions/purposes
(1) After controlling for confounding variables, do patients undergoing revision TKA for infection have higher 30-day readmission, reoperation, and mortality rates than those undergoing revision TKA for aseptic causes? (2) Compared with patients undergoing revision TKA who are believed not to have infections, are patients undergoing revision for infected TKAs at increased risk for complications?
Methods
We queried the American College of Surgeons National Surgical Quality Improvement Program database for patients undergoing revision TKA from 2012 to 2015 identified by Current Procedural Terminology (CPT) codes 27486, 27487, and 27488. Of the 10,848 patients identified, four were excluded with a diagnosis of malignancy (International Classification of Diseases, 9th Revision code 170.7, 170.9, 171.8, or 198.5). This validated, national database records short-term outcome data for inpatient procedures and does not rely on administrative coding data. Demographic variables, comorbidities, and outcomes were compared between patients believed to have infected TKAs and those undergoing revision for aseptic causes. A multivariate logistic regression analysis was performed to identify independent factors associated with complications, readmissions, reoperations, and mortality.
Results
After controlling for demographic factors and medical comorbidities, TKA revision for infection was independently associated with complications (odds ratio [OR], 3.736; 95% confidence interval [CI], 3.198-4.365; p < 0.001), 30-day readmission (OR, 1.455; 95% CI, 1.207-1.755; p < 0.001), 30-day reoperation (OR, 1.614; 95% CI, 1.278-2.037; p < 0.001), and 30-day mortality (OR, 3.337; 95% CI, 1.213-9.180; p = 0.020). Patients with infected TKA had higher rates of postoperative infection (OR, 3.818; 95% CI, 3.082-4.728; p < 0.001), renal failure (OR, 36.709; 95% CI, 8.255-163.231; p < 0.001), sepsis (OR, 7.582; 95% CI, 5.529-10.397; p < 0.001), and septic shock (OR, 3.031; 95% CI, 1.376-6.675; p = 0.006).
Conclusions
Policymakers should be aware of the higher rate of mortality, readmissions, reoperations, and complications in patients with infected TKA. Without appropriate risk adjustment or excluding these patients all together from alternative payment and quality reporting models, fewer providers will be incentivized to care for patients with infected TKA.
Level of Evidence
Level III, therapeutic study.
Introduction
Healthcare expenditures continue to rise in the United States and are projected to exceed 20% of the gross domestic product by 2025 [17]. To help curb these costs, recent health reform efforts have shifted the focus from volume to value in an attempt to improve the quality of care while reducing costs [24]. Congress has passed legislation including the Affordable Care Act and the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) to provide the framework to link reimbursement for providers based on outcome metrics. The Centers for Medicare & Medicaid Services (CMS) have developed programs such as the Merit-based Incentive Payment System (MIPS) and the Hospital Readmissions Reduction Program to focus on value-driven care [7, 8]. Because the economic and clinical burden of revision TKA is projected to increase [4, 6, 20], it has become a target for cost reduction for payers such as the CMS. Since alternative payment models have become popular to reduce episode-of-care costs in primary arthroplasty [5, 14-16, 23], some centers are now participating in bundled payment arrangements for revision TKA [9]. A recent survey of adult reconstruction surgeons, however, reports that the top concern regarding bundled payment models is problems with access to care for patients who utilize more resources [18]. Although patients undergoing revision TKA for infection have been shown to have markedly increased hospital costs than revision TKA for aseptic causes in smaller institutional studies that are now two decades old [13, 27], the independent effect of infection on complication, readmission, mortality, and reoperation has yet to be assessed on a national level.
Concerns exist with regard to the lack of risk adjustment in these payment and quality reporting models. In current reimbursement models, patients undergoing a revision for an infected TKA are included in the same diagnosis-related group with the same inpatient facility fee as patients undergoing revision TKA for aseptic reasons. Providers participating in an alternative payment model for revision TKA are also financially responsible for readmissions and reoperations after discharge from the hospital. Without appropriate risk adjustment or exclusion of patients with infected TKA in value-based payment models, surgeons and hospitals may be disincentivized to care for patients with periprosthetic joint infection (PJI) of the knee.
The purpose of this study is to answer the following questions: (1) After controlling for confounding variables, do patients undergoing revision TKA for infection have higher 30-day readmission, reoperation, and mortality rates than those undergoing revision TKA for aseptic causes? (2) Compared with patients undergoing revision TKA who are believed not to have infections, are patients undergoing revision for infected TKAs at increased risk for complications?
Patients and Methods
We retrospectively queried the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database for all patients who underwent revision TKA from January 1, 2012, to December 31, 2015. The NSQIP database is a validated, national database including cases from > 650 hospitals [1, 3]. Although other national databases using CMS or insurance claims data provide for a large sample size, many rely solely on administrative coding for their results. Although the NSQIP database only reports 30-day outcomes, each chart is specifically reviewed for accuracy by a trained data abstractor and does not rely on coding and billing information to report their results.
Patients in the database were identified for the study based on primary procedure Current Procedural Terminology (CPT) codes 27486 (single-component revision), 27487 (both-component revision), and 27488 (explantation and placement of a spacer). Patients having a diagnosis of infection were also identified based on principal International Classification of Diseases, 9th Revision diagnosis codes 996.6x and 711.xx. Patients were excluded from the study if their primary diagnosis for the procedure was for malignancy (170.7, 170.9, 171.8, or 198.5). Patients undergoing revision for any other diagnosis code were considered as undergoing aseptic revisions. This study was exempt from institutional review board approval because all data were deidentified. No external funding was received for this study.
Demographic variables, medical comorbidities as well as 30-day complication, readmission, and mortality rates were noted from the database. We defined hypoalbuminemia as any patient with a preoperative albumin < 3.5 g/dL and preoperative kidney disease as any patient with a preoperative creatinine > 1.5 mg/L. Complications, reoperations, and readmissions within 30 days of surgery were noted. We defined complications within 30 days of surgery according to the NSQIP as any patient having a recorded surgical site infection, pneumonia, respiratory complication requiring reintubation, pulmonary embolism, deep venous thrombosis (DVT), renal insufficiency or failure, stroke, cardiac arrest, myocardial infarction, sepsis, or septic shock. Although the NSQIP database includes rates of urinary tract infection and bleeding requiring a transfusion, we have excluded these variables in our analysis because they are minor complications. We defined postoperative infection as a superficial surgical site infection, deep surgical site infection, or wound dehiscence. Complete NSQIP methodology has been reported previously [2].
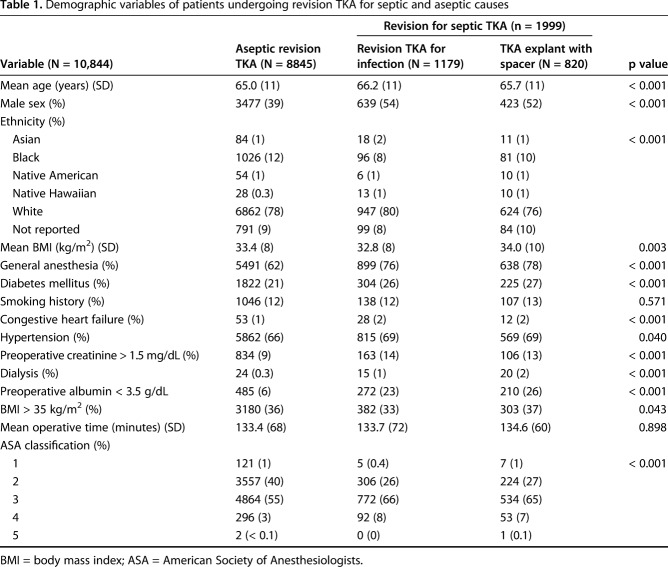
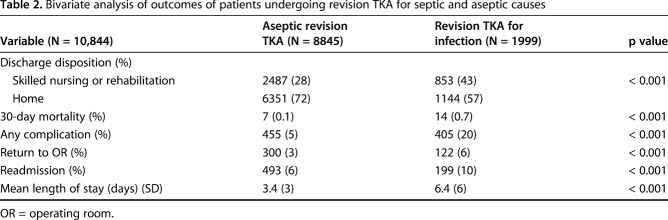
There were 10,848 patients undergoing revision TKA from 2012 to 2015. Four patients were excluded based on diagnosis codes for malignancy, leaving 10,844 patients for analysis. Of these, 1999 patients (18%) underwent revision TKA for infection, including 820 patients (8%) coded as explantation with placement of an antibiotic spacer. Patients undergoing revision TKA for aseptic causes had a lower mean age than the revision TKA for infection and TKA explant groups (65 years [SD 11 years] versus 66 years [SD 11 years] versus 66 years [11 years], p < 0.001). They were also a healthier cohort with lower rates of diabetes mellitus (1822 of 8845 [21%] versus 304 of 1179 [26%] versus 225 of 820 [27%], p < 0.001), hypoalbuminemia (485 of 8845 [6%] versus 272 of 1179 [23%] versus 210 of 820 [26%], p < 0.001), and kidney disease (834 of 8845 [9%] versus 163 of 1179 [14%] versus 106 of 820 [13%], p < 0.001; Table 1). Patients undergoing revision TKA for infection were more likely to be discharged to a rehabilitation facility (853 of 1999 [43%] versus 2487 of 8845 [28%], p < 0.001) and had a longer mean length of stay (6.4 [SD 6 days] versus 3.4 [SD 3 days] days, p < 0.001) than aseptic patients undergoing revision TKA. Infected patients undergoing revision TKA also had higher 30-day mortality (14 of 1999 [0.7%] versus seven of 8845 [0.1%], p < 0.001), reoperation (122 of 1999 [6%] versus 300 of 8845 [3%], p < 0.001), and readmission (199 of 1999 [10%] versus 493 of 8845 [6%], p < 0.001) rates than patients undergoing TKA for aseptic reasons (Table 2). 1
Table 1.
Demographic variables of patients undergoing revision TKA for septic and aseptic causes
Table 2.
Bivariate analysis of outcomes of patients undergoing revision TKA for septic and aseptic causes
Statistical Analysis
We first conducted an a priori power analysis to determine the appropriate sample size. We sought to power our study to answer whether patients undergoing revision TKA for infection had a higher 30-day complication rate than those patients undergoing revision TKA for aseptic causes. Based on a prior published complication rate among patients undergoing revision TKA at 8%, with 20% of patients undergoing TKA revised for infection, to detect a 2% difference in complication rate, with a type I error rate of 0.05, we would need a sample size of 10,584 patients to achieve a power of 0.80 [12].
Data analysis was first performed comparing who underwent revision TKA for aseptic causes with those undergoing revision TKA for infection. Categorical variables were analyzed using a chi square test. When observed or expected values were < 5, we performed a Fisher’s exact test. Continuous variables such as age and body mass index were analyzed using an unpaired, two-tailed, Student’s t-test. When comparing three groups (aseptic revision TKA, septic revision TKA, and TKA explant with antibiotic spacer), a one-way analysis of variance was performed. Statistical significance was set at p < 0.05. We then performed a multivariate logistic regression analysis to identify independent factors associated with 30-day complications, readmissions, and mortality. Statistical analysis was performed using Microsoft Excel (Bellevue, WA, USA) and IBM SPSS Version 24.0 (Armonk, NY, USA).
Results
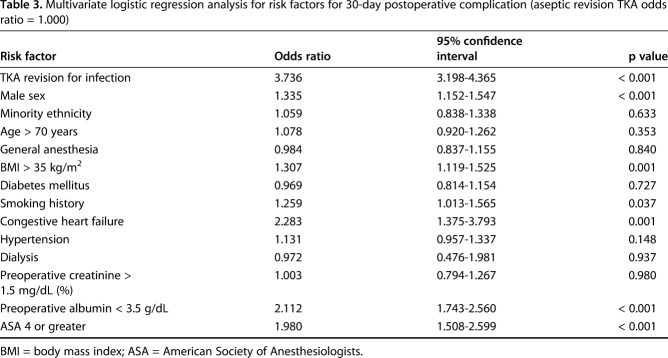
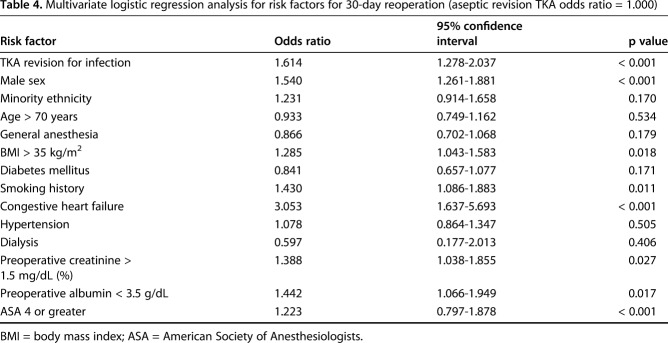
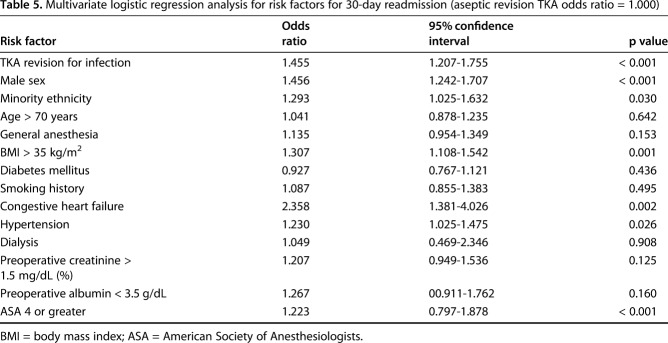
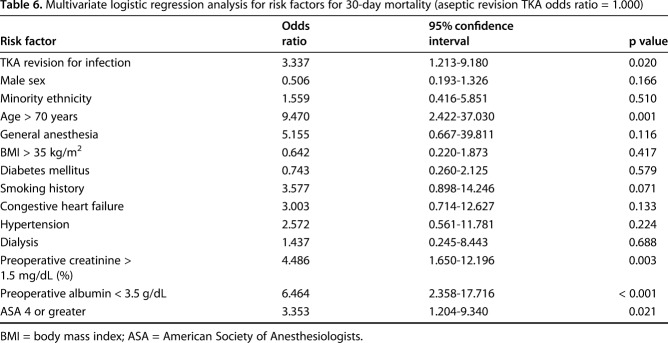
After controlling for demographic factors and medical comorbidities, TKA revision for infection was independently associated with complications (Table 3) (odds ratio [OR], 3.736; 95% confidence interval [CI], 3.198-4.365; p < 0.001), 30-day reoperation (OR, 1.614; 95% CI, 1.278-2.037; p < 0.001) (Table 4), 30-day readmission (OR, 1.455; 95% CI, 1.207-1.755; p < 0.001) (Table 5), and 30-day mortality (OR, 3.337; 95% CI, 1.213-9.180; p = 0.020) (Table 6).
Table 3.
Multivariate logistic regression analysis for risk factors for 30-day postoperative complication (aseptic revision TKA odds ratio = 1.000)
Table 4.
Multivariate logistic regression analysis for risk factors for 30-day reoperation (aseptic revision TKA odds ratio = 1.000)
Table 5.
Multivariate logistic regression analysis for risk factors for 30-day readmission (aseptic revision TKA odds ratio = 1.000)
Table 6.
Multivariate logistic regression analysis for risk factors for 30-day mortality (aseptic revision TKA odds ratio = 1.000)
Patients undergoing explanation of TKA and placement of a spacer had higher 30-day complication (OR, 4.064; 95% CI, 3.321-4.974; p < 0.001), mortality (OR, 4.681; 95% CI, 1.496-14.648; p = 0.008), and readmission (OR, 1.334; 95% CI, 1.023-1.740; p = 0.033) rates when compared with patients undergoing revision TKA for aseptic causes. There was no difference in reoperation rates (OR, 1.176; 95% CI, 0.819-1.688; p = 0.380). Similarly, patients undergoing a revision TKA excluding spacers also had higher 30-day complication (OR, 3.515; 95% CI, 2.925-4.224; p < 0.001), reoperation (OR, 1.925; 95% CI, 1.478-2.507; p < 0.001), and readmission rates (OR, 1.542; 95% CI, 1.236-1.923; p < 0.001) when compared with patients undergoing revision TKA for aseptic causes. There was no difference in mortality rates (OR, 2.473; 95% CI, 0.761-8.036; p = 0.132).
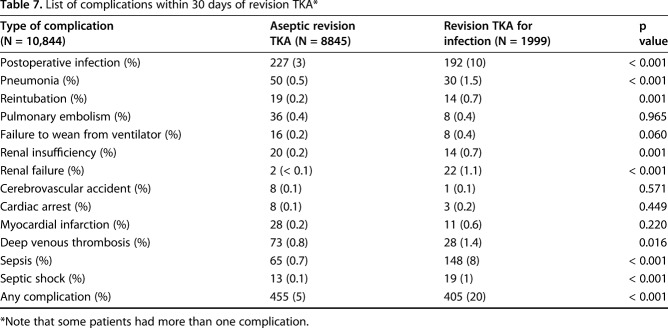
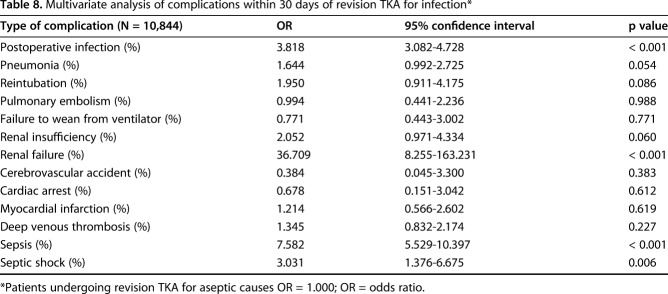
When compared with patients undergoing revision TKA for aseptic causes, patients undergoing revision TKA for infection had higher rates of postoperative infection (OR, 3.818; 95% CI, 3.082-4.728; p < 0.001), renal failure (OR, 36.709; 95% CI, 8.255-163.231; p < 0.001), sepsis (OR, 7.582; 95% CI, 5.529-10.397; p < 0.001), and septic shock (OR, 3.031; 95% CI, 1.376-6.675; p = 0.006) (Tables 7, 8). When controlling for confounding demographic variables and medical comorbidities, there was no difference in the rate of DVT (OR, 1.345; 95% CI, 0.832-2.174; p = 0.227), pulmonary embolism (OR, 0.994; 95% CI, 0.441-2.236; p = 0.988), or myocardial infarction (OR, 1.214; 95% CI, 0.566-2.602; p = 0.619).
Table 7.
List of complications within 30 days of revision TKA*
Table 8.
Multivariate analysis of complications within 30 days of revision TKA for infection*
Discussion
To reward quality and to lower the cost of care, providers are now responsible for reporting outcome metrics through MACRA and the MIPS program [6]. Some institutions have also elected to participate in a voluntary bundled payment model with the CMS for revision TKA to maximize reimbursement [9]. However, concerns exist about access to care in these value-based programs for patients with higher cost arthroplasty who may use more resources in an episode of care [11, 18]. In current reimbursement models, payers do not differentiate between patients undergoing revision TKA for infection and those undergoing revision TKA for aseptic causes. Providers are financially incentivized to care for healthier patients who undergo aseptic revision TKA and are currently disincentivized to care for patients with an infected TKA without proper risk adjustment. We hope our study can impact policymakers in adjusting reimbursement for facilities and surgeons that care for patients with an infected TKA. Therefore, we sought to find out if patients undergoing revision TKA for infection utilize more resources in a 30-day episode of care than those undergoing revision TKA for aseptic causes.
There are several limitations to this study. Like with many large databases, big data studies rely heavily on accuracy of coding. The NSQIP database, however, has advantages over other administrative databases by using certified data collectors abstracting data from each medical record. Random audits have found discrepancy rates of < 2% within each site [2]. Because of variations in surgeon and hospital billing, there are no specific CPT codes to separately analyze patients who underwent irrigation and débridement with polyethylene liner exchange, single-stage revision TKA, or second-stage reimplantation after spacer placement. Our infected revision TKA cohort did attempt to capture all of these patients using diagnosis and procedural codes. Finally, we did not have cost or reimbursement data for analysis and had to use 30-day outcomes such as readmission and discharge disposition as proxies for higher episode-of-care costs. Further study is needed to quantify the financial burden of infected TKA revisions on episode-of-care costs.
Not surprisingly, our results showed that patients undergoing revision TKA for infection had a longer length of stay, were more likely to be discharged to a rehabilitation facility, and had higher readmission, complication, reoperation, and mortality rates than patients undergoing aseptic revision. The short-term, 30-day outcomes for revision TKA in our series are comparable to other large database studies [12, 19, 21]; however, these studies did not specifically look at infection as a risk factor. Although studies have identified poor outcomes after revision of infected TKA, policymakers rarely generalize results from institutional studies. We present a large series of patients from a validated, national database of > 600 hospitals demonstrating poorer outcomes after revision TKA for infection. Infected patients undergoing TKA require long-term IV access, antibiotic infusion, and often have activity and weightbearing restrictions, all of which account for increased resource utilization. Interestingly, when separating patients by surgical procedure, those who underwent explantation and placement of an antibiotic spacer had the worst outcomes. These patients’ poor prognoses are likely the result of the physiologic burden of an active PJI, but may also be related to patient comorbidities that could push the surgeon toward explantation. In our series, some may argue that the increased resource utilization for infected patients undergoing TKA revision is the result of the comorbidity profile of this group. Infected patients undergoing TKA did have higher rates of renal disease, malnutrition, heart failure, and diabetes, all of which have been shown to have increased complication rates after arthroplasty [25, 26]. When controlling for demographics and comorbidities, however, infected patients undergoing revision TKA had higher rates of complications, readmission, reoperation, and mortality. Value-based models that incentivize providers based on outcomes instead of volume [22] should account for infected patients undergoing revision TKA, who have an inherently higher risk of complications and resource utilization in an episode of care. Our data agree with prior studies demonstrating the increased clinical and financial burden of infected revision TKA [13, 27]. Although some of these clinical risk factors are modifiable in primary TKA, a patient undergoing joint débridement or resection arthroplasty for PJI may not be able to spend weeks or months improving his or her medical condition in advance of what sometimes is urgent surgery. Such patients should also be counseled preoperatively about the inherent high risk of the procedure.
When analyzing differences in specific complications, patients with infected TKAs undergoing revision had higher risks of sepsis, wound infection, shock, and renal failure than patients undergoing revision TKA in the absence of infection. These results could be explained by prior studies that have shown that infected patients undergoing revision TKA have greater hemodynamic variation and blood loss than aseptic patients [28]. Other studies have linked PJI to higher rates of DVT in patients undergoing revision arthroplasty [10], but we found no increase when controlling for other confounding variables. Although we excluded minor complications such as urinary tract infection that would likely only have a negligible effect on episode-of-care costs, infected patients undergoing revision TKA have higher rates of serious complications, many of which require prolonged hospital admission and utilization of healthcare resources.
Patients undergoing revision TKA for infection have higher 30-day complication, readmission, reoperation, and mortality rates than aseptic patients undergoing revision TKA. Without risk adjustment to current alternative payment and quality reporting models to carve out treatment of PJI as a different category in a revision bundle, there will be a financial disincentive to care for infected patients undergoing TKA, which may ultimately lead to loss of access to care for patients. We hope our large series from a validated, national database can help influence policymakers to adjust reimbursement for providers caring for patients with infected TKA or exclude them from value-based payment models.
Footnotes
Each author certifies that neither he, nor any member of his immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
This work was performed at Thomas Jefferson University Hospital, Rothman Institute, Philadelphia, PA, USA.
The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
References
- 1.American College of Surgeons. ACS National Surgical Quality Improvement Program (ACS NSQIP). Available at: http://site.acsnsqip.org/participants/. Accessed August 22, 2017.
- 2.American College of Surgeons. Data collection, analysis, and reporting. Available at: https://www.facs.org/quality-programs/acs-nsqip/program-specifics/data. Accessed August 22, 2017.
- 3.American College of Surgeons. NSQIP participant use data file. 2015. Available at: https://www.facs.org/quality-programs/acs-nsqip/program-specifics/participant-use. Accessed August 22, 2017.
- 4.Bhandari M, Smith J, Miller LE, Block JE. Clinical and economic burden of revision knee arthroplasty. Clin Med Insights Arthritis Musculoskelet Disord. 2012;5:89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bolz NJ, Iorio R. Bundled payments: our experience at an academic medical center. J Arthroplasty. 2016;31:932–935. [DOI] [PubMed] [Google Scholar]
- 6.Casalino LP. The Medicare Access and CHIP Reauthorization Act and the corporate transformation of American medicine. Health Aff (Millwood). 2017;36:865–869. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Medicare & Medicaid Services. Quality Payment Program. The Merit-based Incentive Program. 2016. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/Merit-based-Incentive-Payment-System-MIPS-Overview-slides.pdf. Accessed August 22, 2017.
- 8.Centers for Medicare & Medicaid Services. Readmissions Reduction Program. 2016. Available at: https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Accessed August 22, 2017.
- 9.Courtney PM, Ashley BS, Hume EL, Kamath AF. Are bundled payments a viable reimbursement model in revision hip and knee arthroplasty? Clin Orthop Relat Res. 2016;474:2714–2721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Courtney PM, Boniello AJ, Sheth NP, Levine BR, Paprosky WG. Are revision hip arthroplasty patients at higher risk for venous thromboembolic events than primary hip arthroplasty patients? J Arthroplasty. 2017. Jul 25. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Courtney PM, Edmiston T, Batko B, Levine BR. Can bundled payments be successful in the Medicaid population for primary joint arthroplasty? J Arthroplasty. 2017. May 25. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Dieterich JD, Fields AC, Moucha CS. Short term outcomes of revision total knee arthroplasty. J Arthroplasty. 2014;29:2163–2166. [DOI] [PubMed] [Google Scholar]
- 13.Hebert CK, Williams RE, Levy RS, Barrack RL. Cost of treating an infected total knee replacement. Clin Orthop Relat Res. 1996;331:140–145. [DOI] [PubMed] [Google Scholar]
- 14.Iorio R. Strategies and tactics for successful implementation of bundled payments: bundled payment for care improvement at a large, urban, academic medical center. J Arthroplasty. 2015;30:349–350. [DOI] [PubMed] [Google Scholar]
- 15.Iorio R, Bosco J, Slover J, Sayeed Y, Zuckerman JD. Single institution early experience with the bundled payments for care improvement initiative. J Bone Joint Surg Am. 2017;99:e2. [DOI] [PubMed] [Google Scholar]
- 16.Iorio R, Clair AJ, Slover J, Zuckerman JD. Early results of CMS bundled payment initiative for a 90 day total joint replacement episode of care. J Arthroplasty. 2016;31:343–350. [DOI] [PubMed] [Google Scholar]
- 17.Keehan SP, Poisal JA, Cuckler GA, Sisko AM, Smith SD, Madison AJ, Stone DA, Wolfe CJ, Lizonitz JM. National health expenditure projections, 2015–25: economy, prices, and aging expected to shape spending and enrollment. Health Aff (Millwood). 2016;35:1522–1531. [DOI] [PubMed] [Google Scholar]
- 18.Kamath AF, Courtney PM, Bozic KJ, Mehta S, Parsley BS, Froimson MI. Bundled payment in total joint care: survey of AAHKS membership attitudes and experience with alternative payment models. J Arthroplasty. 2015;30:2045–2056. [DOI] [PubMed] [Google Scholar]
- 19.Keswani A, Lovy AJ, Robinson J, Levy R, Chen D, Moucha CS. Risk factors predict increased length of stay and readmission rates in revision joint arthroplasty. J Arthroplasty. 2016;31:603–608. [DOI] [PubMed] [Google Scholar]
- 20.Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96:624–630. [DOI] [PubMed] [Google Scholar]
- 21.Liodakis E, Bergeron SG, Zukor DJ, Huk OL, Epure LM, Antoniou J. Perioperative complications and length of stay after revision total hip and knee arthroplasties: an analysis of the NSQIP database. J Arthroplasty. 2015;30:1868–1871. [DOI] [PubMed] [Google Scholar]
- 22.Malinak J, Press MJ, Rajkumar R, Conway PH. Principles for provider incentives in CMS' alternative payment models. Healthc (Amst). 2017;5:9–11. [DOI] [PubMed] [Google Scholar]
- 23.Mechanic RE. Mandatory Medicare bundled payments: is it ready for prime time. N Engl J Med. 2015;373:1291. [DOI] [PubMed] [Google Scholar]
- 24.Miller HD. From volume to value: better ways to pay for health care. Health Aff (Millwood). 2009;28:1418–1428. [DOI] [PubMed] [Google Scholar]
- 25.Nelson CL, Elkassabany NM, Kamath AF, Liu J. Low albumin levels, more than morbid obesity, are associated with complications after TKA. Clin Orthop Relat Res. 2015;473:3163–3172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rozell JC, Courtney PM, Dattilo JR, Wu CH, Lee GC. Late complications following elective primary total hip and knee arthroplasty: who, when, and how? J Arthroplasty. 2017;32:719–723. [DOI] [PubMed] [Google Scholar]
- 27.Sculco TP. The economic impact of infected total joint arthroplasty. Instr Course Lect. 1993;42:349–351. [PubMed] [Google Scholar]
- 28.Shon OJ, Lee DC, Ryu SM, Ahn HS. Comparison of difference in hematologic and hemodynamic outcomes between primary total knee arthroplasty and revision of infected total knee arthroplasty. Knee Surg Relat Res. 2016;28:130–136. [DOI] [PMC free article] [PubMed] [Google Scholar]