Rotator cuff tears are a common cause of shoulder pain and dysfunction. For patients who do not improve with nonoperative treatment, surgery often is indicated. While primary repair of the rotator cuff suffices for many patients, repair is not always possible. Factors that increase the chances of an irreparable tear include large size, increasing number of tendons involved, chronic retraction and scarring, and poor tissue quality resulting from atrophy and fatty infiltration. Treatment options for patients with irreparable tears include simple débridement, margin convergence, superior capsular reconstruction, tendon transfer, and reverse shoulder arthroplasty, among others. As the number of treatment options continues to grow, the best indications have become an increasing topic of debate.
In this Clinical Faceoff, I will discuss surgical options for irreparable rotator cuff tears with two clinical experts on the topic: Dr. Bassam Elhassan from the Mayo Clinic and Dr. Joshua S. Dines from the Hospital for Special Surgery. Dr. Elhassan has completed fellowships in shoulder, elbow, and hand surgery. Although he treats nearly every surgical condition of the shoulder, he has extensive clinical and academic experience with tendon transfers about the shoulder. Following residency, Dr. Dines completed a fellowship in sports medicine and shoulder surgery. He has years of experience treating rotator cuff injuries (repairable and irreparable) of the shoulder. Both of our debaters are clear thought leaders on this common but difficult topic.
Clinical Scenario
A 59-year-old right-hand-dominant woman who is a recreational swimmer and tennis player has been diagnosed with an acute, massive (supraspinatus and infraspinatus), rotator cuff tear after a fall 3 months ago. She has persistent pain, decreased motion, and weakness despite nonoperative treatment. Passive ROM is full; however, active ROM is limited to 45° of forward elevation (vs. 170° on contralateral side) and 30° of external rotation (vs. 60° on contralateral side). She has pain and weakness with elevation and external rotation but full internal rotation strength. Based on the examination and MRI, the injury involves the entire supraspinatus and most of the infraspinatus. The subscapularis and teres minor both appear intact. After reviewing the MRI, it is determined that the supraspinatus tear cannot be repaired (Fig. 1). She does not have glenohumeral joint arthritis (Fig. 2) and the shoulder was asymptomatic prior to this injury.
Fig. 1.

In this coronal T2-weighted MRI of the right shoulder, a full-thickness tear of the supraspinatus (SS) near the musculotendinous junction is demonstrated. The remaining tendon stump is retracted medial to the glenoid.
Fig. 2.
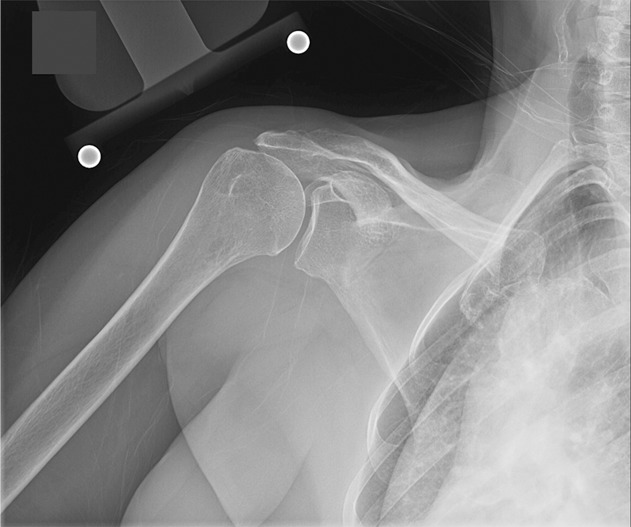
The glenohumeral joint space is well preserved without any evidence of chronic joint degeneration on this anterior to posterior radiograph of the right shoulder.
Christopher L. Camp MD: Based on the history, imaging, and the arthroscopic photo that shows full-thickness musculotendinous junction tears of the supraspinatus and infraspinatus with retraction medial to the glenoid and no evidence of arthritis, (Fig. 3) what treatment option is likely to provide this patient with the highest degree of function following surgery and why?
Fig. 3.
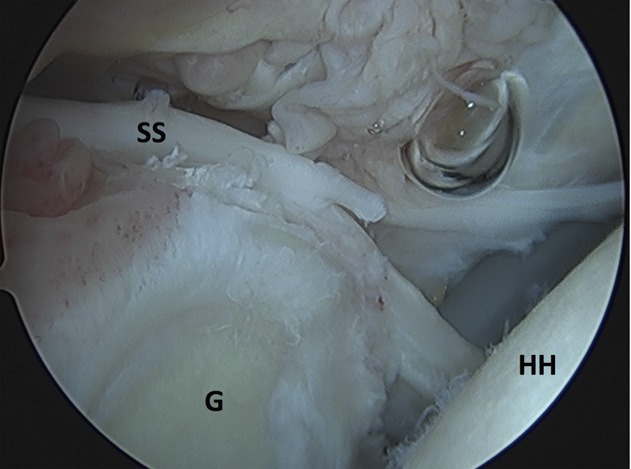
While viewing from a posterior arthroscopy portal using a standard 30° arthroscope with the patient in the beach chair position, the full-thickness nature of the rotator cuff is appreciated. The remaining supraspinatus (SS) tendon is retracted medial to the glenoid (G). The chondral surfaces of the glenoid and humeral head (HH) are well preserved.
Bassem Elhassan MD: I would offer the patient an arthroscopic lower trapezius transfer to reconstruct her irreparable posterior-superior rotator cuff tear. Since the infraspinatus is disrupted, and the supraspinatus is irreparable, the patient will benefit from an alternative motor to drive and improve her shoulder external rotation, and to restore the force couple of the shoulder. Because the line of pull of the lower trapezius transfer matches the line of pull of the infraspinatus and supraspinatus, I feel it is the best option to restore the force couple of the shoulder, maximize ROM, and decrease pain [3].
Joshua S. Dines MD: Dr. Elhassan has done outstanding work defining the indications of and techniques for a successful lower trapezius transfer. And I agree with him that it is likely a more-appropriate tendon transfer than, for example, the latissimus dorsi. Unfortunately, despite the biomechanical advantages of the lower trapezius transfer compared to other tendon transfers, the clinical results may not support the claim that a tendon transfer would provide this patient with the highest degree of function following surgery. One study demonstrated mean gains of 50° of forward elevation and 30° of external rotation for this technique, and unfortunately, worse results were observed in patients with < 60° of preoperative elevation [5]. This patient likely would be in the group that would experience less improvement with a lower trapezius transfer. As a result, my preferred approach would be a superior capsular reconstruction using a dermal allograft fixed to the glenoid and humeral head with suture anchors. In the initial series reporting results of superior capsular reconstruction, many patients with pseudoparalysis of the shoulder achieved full forward elevation, with an overall mean of 148° [8]. In patients in whom the graft healed, average postoperative American Shoulder and Elbow Score (ASES) score was 96 and even in the few patients whose graft tore, the ASES score still improved to an average of 77. Based on these data, I think that superior capsular reconstruction would provide this patient with the most predictable improvements in shoulder pain and function.
Dr. Camp: If superior capsular reconstruction ultimately provides an unsatisfactory clinical result for the patient in terms of pain and function, what are the other options for this patient moving forward?
Dr. Dines: Superior capsular reconstruction is an excellent option for young, active patients with irreparable rotator cuff tears without arthritis for 3 reasons: (1) The procedure may be performed arthroscopically, and surgeons who are comfortable performing arthroscopic rotator cuff repairs should be able to perform this procedure with relative ease; (2) it has an excellent early clinical track record in both Japan [8] and the United States [4], and, perhaps most importantly, (3) it doesn’t burn any bridges with regards to what could be done if it does not adequately improve the patient’s pain and function. Aside from superior capsular reconstruction, other options in this setting might include débridement with or without biceps tenodesis, partial tendon repair, tendon transfers (latissimus dorsi or lower trapezius), balloon spacer insertion, or reverse total shoulder arthroplasty. Having had a previous superior capsular reconstruction would not contraindicate any of these procedures, and it is unlikely that any of these procedures would be compromised by a prior superior capsular reconstruction.
Dr. Elhassan: These are all great thoughts, and while I agree with his first two points, a large degree of uncertainty remains regarding the final point (that superior capsular reconstruction doesn’t burn any bridges). Currently, we have few data on the clinical outcomes of superior capsular reconstruction, and the few studies that have been published report only short-term followup [4, 8]. As a result, the long-term durability, function, complication profile, and impact on future surgery following failed superior capsular reconstruction remain unknown. Therefore, I submit that while reliable salvage options following failed superior capsular reconstruction would include tendon transfer and/or reverse shoulder arthroplasty, we do not yet know if the results of procedures likely to be impaired by the prior superior capsular reconstruction.
Dr. Camp: Excellent point, Dr. Elhassan. We do lack long-term data on superior capsular reconstruction. But on the flip side, how durable are tendon transfers in young, active patients, and what happens if they go bad?
Dr. Elhassan: At the Mayo Clinic, we have seen some younger patients who have continued to experience pain relief and maintained their improved ROM following tendon transfers at 10 years followup. Likewise, Gerber and colleagues [6] found that these patients maintain improvements in functional outcome scores, ROM, and strength up to 15 years after surgery (minimum followup 10 years) [6]. To date, I have performed more than 100 lower trapezius transfers with few complications and a low risk of reoperation [5].
Ultimately, the most common reason for subsequent surgery following tendon transfer is progressive arthritis in patients who had arthritic changes prior to surgery. In this select group of patients, conversion to a reverse shoulder arthroplasty is a relatively straightforward procedure to perform, but this is certainly not without its risks. Additionally, if the tendon transfer was adequately healed, it will allow for continued external rotation following arthroplasty without additional transfers.
Dr. Dines: Dr. Elhassan raises an excellent point. A successful tendon transfer providing external rotation would be helpful to have in place should a patient undergo reverse shoulder replacement in the future. Unfortunately, a number of complications can occur after tendon transfers, which make them a somewhat less-attractive option to me; these include hematoma compressing the axillary nerve resulting in surgical release, deltoid insufficiency even after repair, adhesive capsulitis, and traumatic failure of the tendon [3]. For me, one of the main benefits of the superior capsular reconstruction over tendon transfers when treating this extremely challenging problem is that those kinds of complications haven’t been reported following superior capsular reconstruction.
Dr. Camp: What is the learning curve for these procedures (superior capsular reconstruction and tendon transfers), and do you think specialized training is required before someone adopts them in practice?
Dr. Dines: While both superior capsular reconstruction and tendon transfers can work well in the clinical situation we are discussing, the main reason I favor superior capsular reconstruction over tendon transfer directly relates to the learning curve and relative technical difficulty of the two procedures. As I earlier mentioned, superior capsular reconstruction is done entirely arthroscopically with the same instruments and implants used for arthroscopic rotator cuff repair. Once the graft is fixed medially to the glenoid, the procedure is akin to a standard rotator cuff repair. Admittedly, shuttling the graft into the shoulder and fixing it to the glenoid is not something that most sports or shoulder surgeons do regularly, but there are several technique articles that provide technical pearls to make the process easier [1, 2, 7]. I think the learning curve, assuming one is comfortable performing arthroscopic rotator cuff repairs, is likely less than five procedures. This contrasts with the learning curve associated with tendon transfers.
The anatomy that a surgeon encounters during a superior capsular reconstruction is familiar. This is not the case with tendon transfers, where a portion of the procedure is done through an open approach over the posterior aspect of the shoulder/scapula. This is an area not commonly operated on by most orthopaedic surgeons, which can cause some trepidation. Surgical dissection in that area requires a review of the anatomy, and, in addition, practice sessions with cadaveric specimens. Once the tendon (either lower trapezius or latissimus) is harvested, it needs to be transferred, which also has a learning curve to it. At the very least, in my opinion, the learning curve for tendon transfers is steeper than for superior capsular reconstruction, and the ability to perform a tendon transfer likely requires specialized training.
Dr. Elhassan: For surgeons who are comfortable in shoulder arthroscopy, it is relatively easy to learn how to perform arthroscopic lower trapezius transfer. This is completely different than performing latissimus transfer. With the latter, good knowledge of the anatomy of the latissimus and comfort in dissecting neurovascular pedicle and mobilization of the muscle should be gained before performing the transfer. However, this is not the case for the lower trapezius transfer. Harvesting generally takes no more than 10 minutes in my hands when using standard, anatomically defined landmarks that are familiar to all surgeons [5]. For those who don’t have as much experience, the harvest may take longer initially, but it can generally be performed in 15 to 20 minutes once you are familiar and comfortable with the technique. For instance, fellows who train with us can typically perform the harvesting independently in approximately 15 minutes after 10 to 15 procedures. The Achilles’ tendon preparation, passage, and fixation are generally straightforward, because the subacromial space is generally wide open in the setting of massive rotator cuff tear. This also facilitates preparation of the tuberosity for the tendon attachment. Finally, attaching the tendon allograft to the lower trapezius is akin to other standard open tendon repairs commonly performed by orthopaedic surgeons (such as quadriceps, patellar, or Achilles tendon repairs).
Footnotes
A note from the Editor-in-Chief: We are pleased to present to readers of Clinical Orthopaedics and Related Research® another installment of Clinical Faceoff, a regular feature. This section is a point-counterpoint discussion between recognized experts in their fields on a controversial topic. We welcome reader feedback on all of our columns and articles; please send your comments to eic@clinorthop.org.
The authors certify that neither they, nor any members of their immediate families, have any commercial associations (such as consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
The opinions expressed are those of the writers and do not reflect the opinion or policy of CORR® or The Association of Bone and Joint Surgeons®.
References
- 1.Adams CR, Denard PJ, Brady PC, Hartzler RU, Burkhart SS. The arthroscopic superior capsular reconstruction. Am J Orthop (Belle Mead NJ). 2016;45:320–324. [PubMed] [Google Scholar]
- 2.Burkhart SS, Denard PJ, Adams CR, Brady PC, Hartzler RU. Arthroscopic superior capsular reconstruction for massive irreparable rotator cuff repair. Arthrosc Tech. 2016;5:e1407–e1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clark NJ, Elhassan BT. The role of tendon transfers for irreparable rotator cuff tears. Curr. Rev Musculoskelet Med. 2018;11:141–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Denard PJ, Brady PC, Adams CR, Tokish JM, Burkhart SS. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy. 2018;34:93–99. [DOI] [PubMed] [Google Scholar]
- 5.Elhassan BT, Wagner ER, Werthel J-D. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tear. J Shoulder Elb Surg. 2016;25:1346–1353. [DOI] [PubMed] [Google Scholar]
- 6.Gerber C, Rahm SA, Catanzaro S, Farshad M, Moor BK. Latissimus dorsi tendon transfer for treatment of irreparable posterosuperior rotator cuff tears: long-term results at a minimum follow-up of ten years. J Bone Joint Surg Am. 2013;95:1920–1926. [DOI] [PubMed] [Google Scholar]
- 7.Hirahara AM, Adams CR. Arthroscopic superior capsular reconstruction for treatment of massive irreparable rotator cuff tears. Arthrosc Tech. 2015;4:e637-641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mihata T, Lee TQ, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, Kinoshita M. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. [DOI] [PubMed] [Google Scholar]


