Abstract
Background
Patellofemoral pain is one of the most common forms of knee arthralgia in adolescent females. Unlike in adults, in whom the etiology of patellofemoral pain is considered to be multifactorial (eg, altered bone shape and musculoskeletal dynamics), the etiology of adolescent patellofemoral pain has been historically attributed to overuse. Although it is highly plausible that adolescent patellofemoral pain results from excessive maltracking, as suggested by recent research, an increase in patellar, relative to femoral, size could also contribute to patellofemoral pain through altered cartilage stresses/strains, resulting in overloading of the subchondral bone. Because the role of bone morphology in the genesis of patellofemoral pain in adolescent females remains largely unknown, research is needed in this area to improve our understanding of patellofemoral pain and advance diagnosis/treatment.
Questions/purposes
(1) Are patellar volume and width increased, and femoral trochlear width decreased, in female adolescents with patellofemoral pain compared with asymptomatic females? (2) Are measures of patellofemoral size correlated with patellofemoral tracking?
Methods
Twenty adolescent females with patellofemoral pain (age, 13.7 ± 1.3 years) and 20 asymptomatic female control participants (age, 13.6 ± 1.3 years) were enrolled in this case-control institutional review board-approved study. This study focused on a strict definition of patellofemoral pain, peripatellar pain in the absence of other structural pathologic conditions (eg, tendinitis, ligament injury, Osgood-Schlatter disease) or a history of dislocations/trauma. Control participants with no history of patellofemoral pain or other lower extremity pathology were matched for age (within 6 months) and body mass index (within 5 kg/m2). Participants self-referred and were recruited through clinicaltrails.gov, printed advertisements, and word of mouth. Three-dimensional (3-D), static, T1-weighted, gradient recalled echo MR images were acquired, from which 3-D patellofemoral models were created. Patellar volume and width, patellar-to-femoral volume and width ratios, and femoral trochlear width were compared across cohorts. In addition, 3-D patellofemoral tracking was quantified from dynamic MR images captured during cyclical flexion-extension volitional movements of the lower extremity. The size measures and ratios were correlated to patellofemoral tracking.
Results
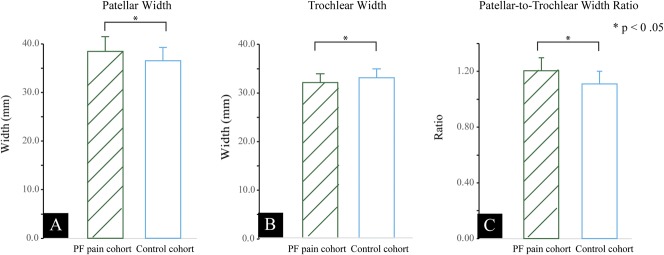
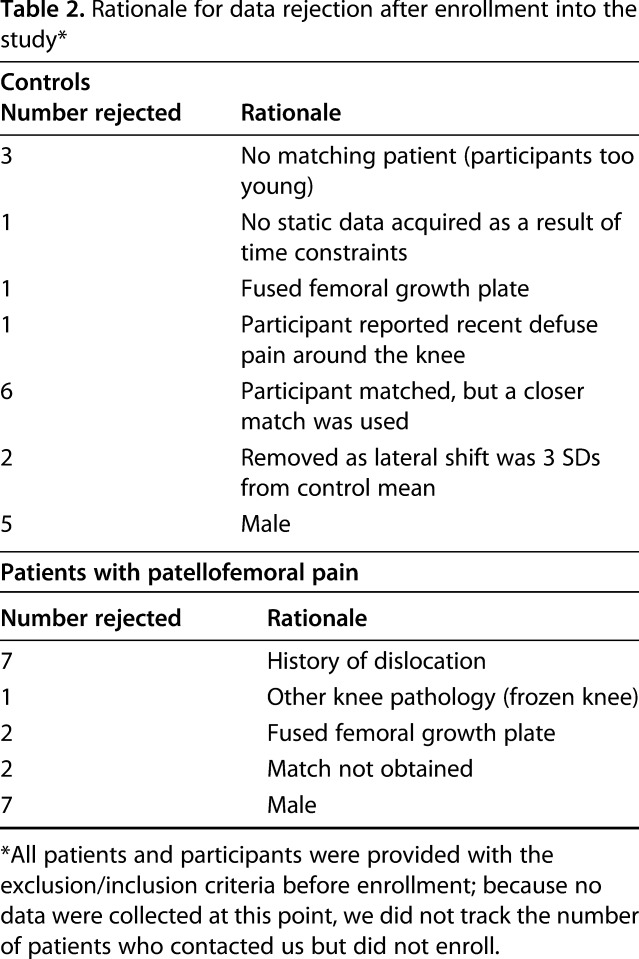
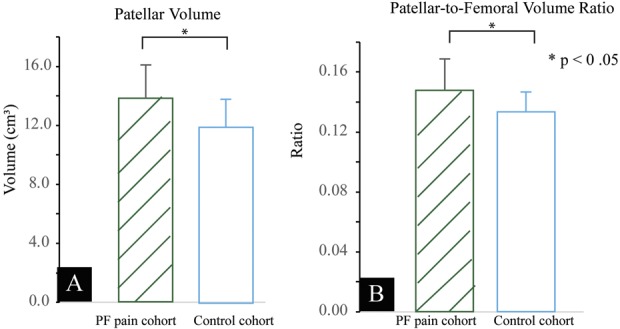
Compared with control participants, the cohort with patellofemoral pain had greater patellar volume (13,792 ± 2256 versus 11,930 ± 1902 mm3; 95% confidence interval [CI], 1336 mm3; p = 0.004; d = 0.89) and width (38.4 ± 3.0 versus 36.5 ± 2.7 mm; 95% CI, 1.8 mm; p = 0.021; d = 0.67). The femoral trochlear width was smaller (32.0 ± 1.8 versus 32.9 ± 1.8 mm; p = 0.043, d = 0.54). The patellar-to-femoral volume ratio and the patellar-to-trochlear width ratio were greater in adolescents with patellofemoral pain (0.15 ± 0.02 versus 0.13 ± 0.01, p = 0.006, d = 0.83 and 1.20 ± 0.09 versus 1.11 ± 0.09, p = 0.001, d = 1.02). No correlations were found between patellar size and patellofemoral tracking (r < 0.375, p > 0.103).
Conclusions
In adolescent females with patellofemoral pain, the increased patellar volume/width and patellar-to-trochlear width ratio, along with the decreased femoral trochlear width, may initiate a pathway to pain through improper engagement of the patella within the femoral trochlea. Specifically, the mean differences between cohorts in patellar and femoral trochlear width (1.9 mm and 0.9 mm) are 58% and 37% of the mean patellar and femoral cartilage thickness in females, respectively, as reported in the literature. Further studies are needed to fully elucidate the mechanism of pain.
Level of Evidence
Level III, prognostic study.
Introduction
Idiopathic patellofemoral (PF) pain is one of the most common causes of knee arthralgia in active adolescent females [1, 3, 26, 31], who are 25% to 50% more likely to be affected than adolescent males [3, 26, 38]. Historically, PF pain during adolescence was considered a self-limiting condition, primarily as a result of overuse [10, 18]. However, recent observational studies suggest that adolescent PF pain is chronic and activity-limiting in some patients [25, 27, 29]. Rathleff et al. [27] estimate that 71% of adolescents with PF pain report a decrease or cessation of sports participation over a 2-year period. Adolescents with PF pain have a morbidity comparable to that of adolescents with ACL injuries, yet the former are less likely to experience symptom resolution compared with ACL injuries or knee pain from other sources [16, 27, 30]. This pain not only affects their physical well-being, but also can have negative social, educational, and economic consequences [4, 20, 40]. Thus, there has been a renewed effort to understand the etiology of PF pain as a result of its high prevalence and poor long-term prognosis during adolescence.
Recent research has begun to look past the simplified theory of overuse toward other paradigms that may explain the mechanism of adolescent PF pain [5, 14, 24, 28, 41]. These studies provide evidence that pathologic neuromuscular control [24, 28], anthropomorphic variables [14, 41], and patellar maltracking [5] are associated with PF pain in the adolescent. The latter study [5] established that dynamic lateral maltracking is the predominant kinematic abnormality in adolescent females with PF pain. Although it is highly plausible that PF pain in adolescent patients with “extreme lateral” maltracking [5] results from pathologic knee kinematics, it is less likely to be the only source of pain in patients with less pronounced kinematic abnormalities. In such cases, an increase in patellar size (eg, patellar volume, patellar width) could limit the 3-D patellar mobility within the groove, through increased contact forces, while increasing the likelihood of patellofemoral pain. Furthermore, PF cartilage has a mean 3.25 mm thickness in adult females [8]. As such, a small increase in patellar volume/width or a small decrease in femoral trochlear width would likely result in large changes to contact stress/strain, increasing the likelihood of PF pain. An improved understanding of the morphologic changes associated with PF pain in adolescents will help advance our treatment of this condition in this unique population.
Adolescence [11] is a developmental period with rapid bone growth and vast biologic changes [19]. The shape and size of immature bone are highly responsive to its loading environment, because mechanical forces influence both osteogenesis and bone remodeling [15]. An imbalance of forces may lead to incongruous bone growth or changes in bone morphology [13, 34, 42]. Although previous studies in adolescents have reported on anthropomorphic variables (eg, lower leg alignment), tibial tubercle-trochlear groove distances, static patellar alignment (eg, Q-angle), and dynamic tracking, we found no studies that investigated changes in PF morphology associated with isolated PF pain in the adolescent population [5, 14, 41].
The purpose of this case-control study was to determine if PF morphology, specifically bone volume and width, is associated with PF pain and PF maltracking in adolescent females. We evaluated the following questions: (1) Are patellar volume and width increased, and femoral trochlear width decreased, in adolescents with PF pain compared with age-matched female control participants without PF pain? (2) Are measures of PF size correlated with PF tracking?
Patients and Methods
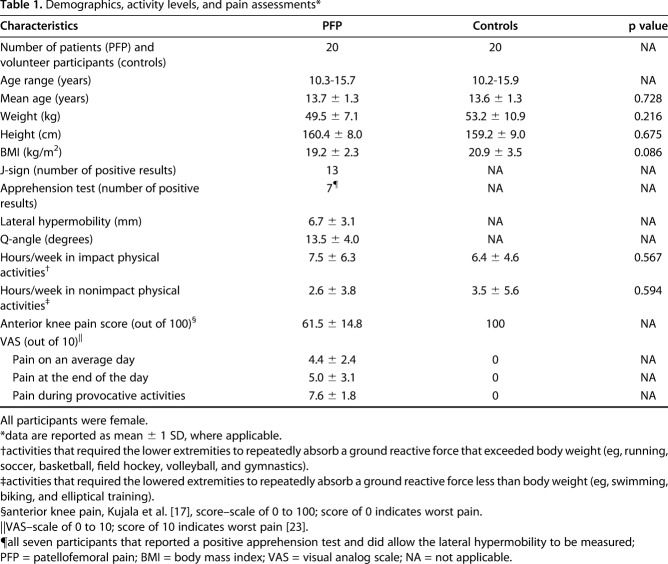
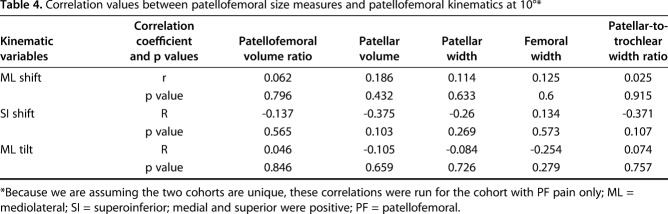
Overall, this study contained data for single knees from 20 female participants with PF pain (age, 13.7 ± 1.3 years) and 20 asymptomatic female control participants (age, 13.6 ± 1.3 years), a sample of convenience (Table 1). Data collection occurred from May 2008 to December 2017 as part of an ongoing institutional review board-approved protocol. In total 39 data sets were collected for each cohort, but the final analysis was limited to 20 per cohort (Table 2). This single-center case-control study was conducted at the Clinical Center of the National Institutes of Health. Previous research [5] included a subset of the current cohort (eight of 20 patients with PF pain and 10 of 20 control participants). This previous study reported PF kinematics (tracking) in adolescent females with and without PF pain. The current study only uses the tracking data as part of a secondary correlation and discriminant analyses.
Table 1.
Demographics, activity levels, and pain assessments*
Table 2.
Rationale for data rejection after enrollment into the study*
Participant Recruitment
All participants entered the study through self-referral. The recruitment tools used were clinicaltrials.gov, flyers, and word of mouth. The flyers were provided at local orthopaedic sports medicine practices, physical therapy clinics, and primary care offices to help recruit patients with PF pain. All asymptomatic volunteer adolescent females (control participants) were matched to patients with PF pain for age (within 6 months) and body mass index (BMI) within 5 kg/m2 (Table 1). The inclusion criterion for the PF pain cohort was a clinical diagnosis of idiopathic anterior, peripatellar pain lasting for > 6 months. Exclusion criteria for both cohorts included a history of patellar dislocation, lower limb trauma (serious lower limb injuries requiring medical attention such as contusions, sprains, or other lower leg injuries/pathologies), or previous lower limb surgery. These exclusion criteria extended to both legs with the exception that patients with PF pain who had previous dislocation of or arthroscopy on the nonstudy leg were not excluded. In addition, individuals from both cohorts were excluded if they could not undergo an MR imaging examination, had fused femoral growth plates (based on 3-D gradient recall echo [GRE] fat-sat MR images), had generalized clinical hypermobility (Beighton score of > 5 [37]), or had a diagnostic history of a hypermobility syndrome (such as Ehlers-Danlos syndrome). For individuals with bilateral PF pain, we used the data for the knee with the most severe pain rating based on a visual analog score (VAS [23]) for activities that typically invoke pain. For control participants, we randomly selected the knee studied.
Before data collection, participants provided signed assent, and an accompanying legal guardian provided signed consent. An in-house physiatrist conducted a history and physical examination for each participant along with a focused knee evaluation. A physical activity questionnaire was acquired (RMS, FTS, AS, VRC); the Kujala score [17] and VAS for pain during a typical day, at the end of the day, and during activities that caused pain were obtained. In addition, the presence/absence of a J-sign was evaluated; the Q-angle was measured, and lateral hypermobility was quantified.
There were no differences in demographics between the cohorts (Table 1). Additionally, there were no differences between cohorts in hours spent in impact and nonimpact physical activities.
MR Data Collection and Analysis
We used static and dynamic MR images to quantify the PF bone morphology (patellar volume, patellar width, and femoral trochlear width) and tracking. The morphology measures were selected because they influence the congruence of the patella within the femoral sulcus.
For static imaging, participants were supine on the MR plinth (3T Verio; Philips Electronics, Eindhoven, The Netherlands) with the lower extremity cushioned in an anatomically neutral position and the knee centered in an eight-channel knee coil. Static, 3-D, high-resolution GRE and GRE-fat-saturated (0.27 x 0.27 x 1.0 mm, 512 x 512 pixels) along with proton density-weighted (0.27 x 0.27 x 1.2 mm, 512 x 512 pixels) MR images were acquired. The on-call radiologist reviewed all static images for any undiagnosed knee pathology that was not detected during the intact history and physical.
Patellar volumes were acquired from the 3-D static images (Fig. 1). Using a custom automatic segmentation algorithm that was based on guided recursive ray tracing (MIPAV; NIH, Bethesda, MD, USA), we created anatomic contours or a “cloud of points” for each bone. Although this automatic segmentation had an accuracy of less than 0.29 mm [6], the unfused growth plates created focal errors for specific data sets. Thus, to ensure model accuracy, one author (RMS) edited the automatic contours using MIPAV. The senior author (FTS), who had > 10 years of experience in creating bone models, reviewed all bone outlines before their use in later analyses. The final cloud of points was imported into Geomagic Studio (Geomagic Inc, Morrisville, NC, USA) and was digitally wrapped and smoothed (0.2 mm) to produce a final patellar model for analysis. The bone volume was calculated directly from the final 3-D models (Fig. 1). To remove the potential influence of the participant’s overall size, we calculated the patellar-to-distal femoral volume (PF volume) ratio for each individual. A distal femoral bone model was created for each participant in an identical manner to the patella. For consistency, we trimmed each femoral model at 5 mm above the level of the laterosuperior aspect of the articular femoral cartilage (Fig. 2), because the 3-D static MR images did not capture the entire femur, and then calculated the volume as we did with the patella.
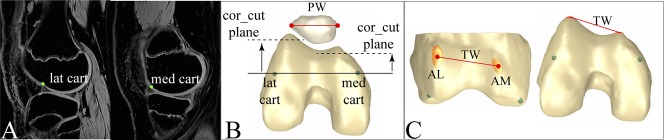
Fig. 1 A-C.
Patellar-to-trochlear width ratio was calculated from the 3-D model. (A) The point of transition from anterior to posterior cartilage on the medial and lateral femoral cartilage extremes (med cart and lat cart, respectively) were located on the bone within the MR images using the 3-D viewing tool in MIPAV (NIH, Bethesda, MD, USA). (B) These medial and lateral transition points from the static images were transferred to the 3-D bone model. A coronal plane (cor_cut plane), relative to the imaging coordinate system, was then rotated about the imager’s superoinferior axis until it contained the mediolateral transition points. This defined the oblique coronal cut plane. (C) This cutting plane was translated anteriorly and used to trim the most anterior sections of the lateral and medial femoral condyles. The center of these regions (anterolateral [AL] and anteromedial [AM]) defined the trochlear width (TW). Patellar width (PW) was calculated as the mediolateral distance using a bounding box. This bounding box was defined relative to the imaging coordinate system.
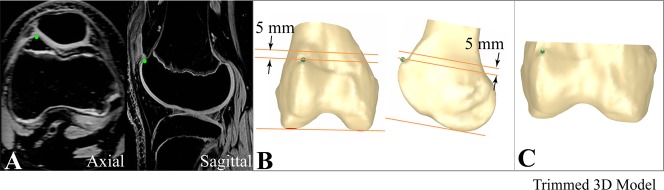
Fig. 2 A-C.
Distal femoral volume was calculated from the distal femur model. (A) The most superior aspect of the lateral cartilage was located on the 3-D GRE fat-saturated images using the triplanar view in MIPAV (NIH, Bethesda, MD, USA). (B) The point on the bone denoting the superolateral cartilage was transferred to the 3-D femoral bone model in Geomagic (Geomagic Inc, Morrisville, NC, USA). The cut plane was defined in the imaging coordinate system. An oblique-axial plane was rotated about the AP axis such that it contained the two most distal points on the femur and was 5 mm superior to the most superolateral cartilage point. This 5-mm shift ensured that the entire posterior aspect of the femoral condyles was included. (C) The model was trimmed at the cutting plane and the volume calculated in Geomagic.
We quantified measures of PF width from the 3-D models in Geomagic. We defined patellar width as the mediolateral size of a bounding box containing the patella. We measured femoral trochlear width using the distance between the most anterior aspect of the lateral and medial femoral condyles on the subchondral surface (Fig. 1). Like with the volume, the patellar-to-trochlear width ratio was calculated.
All measures were based in the imaging coordinate system. Performing the analysis in a bone-based coordinate system is much more time-intensive and potentially less precise, because creating such coordinate systems requires interpretation of the images. Furthermore, our methodology for aligning participants within the scanner creates consistent alignment of the femur relative to the imaging coordinate system. Only 2.6° of rotation about two axes is required to align the femoral coordinate system to the imaging based coordinate system [36]. Lastly, none of the patients with PF pain demonstrated severe lateral tilt; thus, patellar rotation within the imaging coordinate system did not influence the measures of patellar width. All researchers were blind to the individual’s cohort during the data analysis stage.
Dynamic patellar tracking and knee angle were acquired using dynamic cine phase-contrast MR imaging, identical to our previous work [5]. This technique is accurate to 0.3 mm for tracking 3-D in vivo bone motion [2]. For the cine phase-contrast data collection, which was acquired during the same visit as the static data, participants were supine in the MR scanner with their knee flexed and supported on cushioned blocks within a custom knee coil holder. Cine phase-contrast images were captured while the participants cyclically flexed and extended their lower leg from approximately 40° flexion to full extension to the beat of an audible metronome (two beats per cycle) at 30 cycles per minute. To create precise coordinate systems, dynamic multiplane axial cine MR data (anatomic images only) were also captured during the movement. The 3-D patellar tracking was derived by integrating the cine phase-contrast data and then expressed in terms of anatomic coordinates fixed in each bone [32].
Sources of Bias
The authors acknowledge that individual participation was limited to adolescents within a close geographic area (District of Columbia-Maryland-Virginia) as a result of travel requirements to the National Institutes of Health Clinical Center. Nevertheless, the investigators utilized all available resources to ensure open advertisements (print, digital, word of mouth, and doctor-patient networks).
Statistical Analysis
The difference in patellar volume was our primary research question. As such, an a priori power analysis (G*Power Version 3.1; Heinrich-Heine-Universität, Düsseldorf, Germany) determined that 17 individuals were needed in each cohort for a 15% patellar volume difference between cohorts with α = 0.05 and a power of 80%. This estimate was based on the mean volume of five patellae from adolescent participants that were manually segmented before this study [6].
All statistical analyses were performed using SPSS Statistics, Version 22 (IBM Corp, Armonk, NY, USA). A one-tailed Student’s t-test defined if the 3-D patellar volumes and width measures were increased in the cohort with PF pain. To further explore differences between cohorts, a discriminant analysis was completed to determine if any single size measure could distinguish cohort membership. A second discriminant analysis was completed to determine if the accuracy of predicting cohort membership improved by adding either mediolateral patellar shift or tilt to the analysis. Effect size was measured using Cohen’s d statistic [7]. Using a Pearson’s correlation (r), bone volume and width measures were correlated to the PF mediolateral shift, superoinferior shift, and mediolateral tilt at 10° knee angle. We selected this subset of kinematic variables to limit the number of correlations. Full extension was selected, because maltracking in patients with PF pain is typically more evident when the knee is fully extended with active quadriceps. A knee angle of 10° measured on MR images equates to a 0° knee angle as measured clinically using the hip, knee, and ankle centers [12]. A two-tailed Student’s t test provided statistical analysis of demographic variables (age, height, weight, BMI).
Results
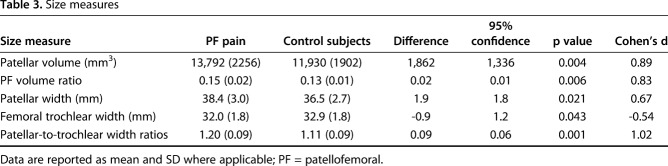
Individuals with PF pain had larger patellar volume relative to control participants (mean difference ± 95% confidence interval = 1862 ± 1336 mm3, p = 0.004, d = 0.89; Fig. 3A; Table 3). The mean (± 1 SD) patellar volumes for the PF pain and control cohorts were 13,792 ± 2256 and 11,930 ± 1902 mm3. The PF volume ratio was greater in individuals with PF pain (mean difference = 0.02 ± 0.01, p = 0.006, d = 0.83; Fig. 3B; Table 3). The mean ratios for the PF pain and control cohorts were 0.15 ± 0.02 and 0.13 ± 0.01, respectively. Seven of the 20 knees in the PF pain cohort demonstrated an extreme PF volume ratio (equal to or greater than 2 SDs of the control mean). The patellar-to-trochlear width ratio was greater in adolescents with PF pain compared with control participants (mean difference = 0.09 ± .06, p = 0.001; Fig. 4A; Table 3). The mean ratios for the PF pain and control cohorts were 1.20 ± 0.09 and 1.11 ± 0.09, respectively (Table 3). In evaluating the individual components of this ratio, the patellar width was larger (mean difference = 1.9 ± 1.8 mm, p = 0.021, d = 0.67; Table 3) and the femoral trochlear width was smaller (mean difference = 0.9 ± 1.2 mm, p = 0.043, d = 0.54; Fig. 4B; Table 3) in patients with PF pain. These patellar and femoral widths were 38.4 ± 3.0 and 36.5 ± 2.7 mm and 32.0 ± 1.8 and 32.9 ± 1.8 mm in the PF pain and control cohorts, respectively (Table 3).
Fig. 3 A-B.
(A) Patellar volume and (B) patellar-to-femoral volume ratio are larger in the cohort with PF pain.
Table 3.
Size measures
Fig. 4 A-C.
(A) Patellar width, (B) trochlear width, and (C) patellar-to-femoral width ratio are larger in the cohort with PF pain.
The patellar-to-trochlear width ratio (Fig. 4C) was the most accurate size variable in discriminating between the groups (75% and 65% accuracy for the PF pain and control cohorts, respectively). When the patellar-to-femoral volume ratio is combined with the PF mediolateral position at full extension, the accuracy in discriminating between the study groups is optimal: 80% and 100% for the PF pain and control cohorts (Fig. 5). There were no correlations (Table 4) between the patellar tracking variables of interest (mediolateral displacement, superoinferior displacement, and mediolateral tilt) and measures of size (volume and width) for the cohort with PF pain.
Fig. 5.
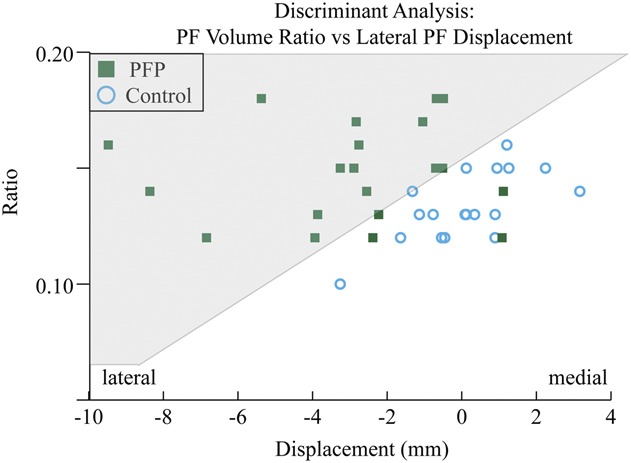
Discriminant analysis: the PF volume ratio is plotted relative to the mediolateral displacement. The gray area indicates the region containing individuals with PF pain. Four of our younger control participants were unable to perform the repetitive motion, required for the dynamic acquisition, well enough for us to obtain analyzable data. Thus, for the discriminant analysis, the missing data were replaced by the mean control mediolateral displacement (0.12 mm).
Table 4.
Correlation values between patellofemoral size measures and patellofemoral kinematics at 10°*
The PF pain cohort was laterally shifted (3.0 mm) relative to the control participants at full extension (p < 0.001, d =1.29) with seven individuals falling into the “extreme maltracking” category [5]. No other kinematic variables (PF superior and anterior displacement; and flexion, medial tilt, and varus rotation) demonstrated differences between the cohorts.
Discussion
This study expands our understanding of the etiology of adolescent PF pain by suggesting an alternate, and possibly complementary, pathway to PF pain, one that begins with pathologic patellar and femoral size. The leading model for the development of adult PF pain is that maltracking initiates pathologic cartilage contact, which overloads the subchondral bone and fosters pain [22], yet this kinematic pathway to pain has not been fully substantiated. Because bone remodeling is heightened during early to mid-adolescence [34], adolescents are particularly susceptible to pathologic bone morphology in the presence of imbalanced forces. Therefore, the presence of increased patellar size and decreased femoral trochlear width is likely inherent risk factors for the development of PF pain, opening avenues for exploring new preemptive and corrective interventions.
This study had limitations. We used single knees with unfused femurs in a cohort of early to mid-adolescent females with isolated, idiopathic PF pain. Thus, the results cannot be generalized to males with PF pain and to other individuals with known etiologies of PF pain (eg, dislocation, trauma, etc). However, this was a study with cohort homogeneity and close matching between cohorts (to within 6 months of age and a BMI within 5 kg/m2). All participants entered the study through self-referral, which may have limited the population to more highly motivated individuals. The pain levels, across our population of patients with PF pain, were quite broad, which may have produced different results than studying a group of patients with a more homogenous report of pain (eg, very mild pain, extreme pain). Although this study was adequately powered for the primary question regarding patellar volume, the correlation analyses may have been limited by the current sample size. At the present time, measuring patellar volume is time-intensive using MR techniques; however, new automatic segmentation techniques are becoming available [6]. Given that our understanding of the etiology of PF pain is still evolving, the theories regarding increased patellar size and pathologic kinematics require further research to substantiate their links to altered PF contact, overloaded subchondral bone, and pain.
The increased patellar bone volume in the current study contrasts with the findings of Yilmaz et al. [43] who found a smaller patellar volume in adolescents with a history of patellar dislocation (presence or absence of PF pain was not reported). Biomechanically, it is plausible that a smaller, more mobile patella has a greater tendency to dislocate, similar to THA wherein a smaller femoral head component is thought to foster dislocation [39]. The divergent results between the current study and the previous study, which focused on dislocators [43], may also have arisen from uncontrolled confounding variables in the previous study such as the control group being diagnosed with unspecified knee pain and being older with a higher percentage of males relative to the patient cohort [43]. Ultimately, this substantial difference between the dislocation and isolated PF pain adolescent cohorts suggests that isolated PF pain and dislocation are unique pathologies with separate etiologies.
Coupling the increased patellar-to-trochlear width ratio and the narrower femoral trochlear width in the current PF pain cohort with past work provides a potential explanation for the greater prevalence of PF pain in females [3, 26, 38]. Although the differences in these variables appeared small (1.9 ± 1.8 mm and 0.9 ± 1.2 mm), when compared with typical cartilage thickness (2.7 mm and 3.25 mm in young adult females [8]) and lateral maltracking in adolescent females (3.2 mm [5]), they are quite substantial. The cohort with PF pain not only demonstrated a narrower trochlear width, but also a larger patellar-to-trochlea width ratio. This larger patellae within a smaller femoral groove, as present in the current PF pain cohort, has a greater likelihood of imbalanced contact patterns and increased stress/strain when it is engaged within the trochlea. Furthermore, with a patella that is too wide for its trochlea, the most lateral or medial cartilaginous surfaces of the patella may become incongruent with the femoral trochlea during functional activities, creating stress concentrations. Coupling this with previous research [9, 21] demonstrating that women have a proportionately narrower distal femur suggests that the narrower femoral trochlear width in females is an intrinsic factor, predisposing females to PF pain. If future research provides continued support for these findings, then females, particularly young athletes who demonstrate increased patellar size or a narrow femoral trochlea before pain, can be directed to training programs to mitigate the effects of adolescent knee pain. Alternatively, for those who already have pain, but have not found relief with conservative treatment, surgical interventions targeting the size abnormalities may reduce or eliminate symptoms in females with PF pain.
Although the kinematics were not a focus of this research, they do help put into context the current results regarding PF size. When the patellar-to-femoral volume ratio is combined with the PF mediolateral position at full extension, the accuracy in discriminating between the study groups is optimized (80% and 100% discriminant accuracy for the PF pain and control cohorts). This high level of accuracy along with a lack of correlation between the PF size measures and tracking indicates the presence of two unique initiators for the pathway to PF pain. Two patients in the current study demonstrated both extreme patellar volume and extreme lateral maltracking, thus these pathways are also not mutually exclusive. These two potential pathways (maltracking and pathologic size) do not exclude other causes of pain given that PF pain is considered a multifactorial disorder [22]. The concept of multiple pathways of pain, that are potentially additive in certain individuals, is supported by the recent studies defining the presence of subgroups within the populations of individuals with PF pain [33, 35].
In conclusion, to our knowledge, this study is the first to demonstrate that adolescent females with isolated PF pain have increased patellar volume and increased patellar-to-trochlear width ratios. An increased PF volume and patellar-to-trochlear width ratio may lead to improper patellar engagement within the femoral trochlea, altered contact locations, and increased PF contact stress. This in turn would overload the subchondral bone and lead to PF pain. The presence of open physes and bone plasticity during adolescence makes bone morphology a potentially important etiologic factor in adolescent idiopathic PF pain. Future prospective studies are warranted to delineate whether an increased patellar volume is the origin or effect of imbalanced forces, PF maltracking, and/or increased physical activity.
Acknowledgments
We thank Katharine E. Alter MD, Natalia Alexandridi, Victor R. Carlson MD, Aricia Shen, Sara Sadeghi, Ruida Cheng, and the Diagnostic Radiology Department (CC, NIH) for their help and support on this project.
Footnotes
One or more of the authors (RMS, FTS) has received funding from the Intramural Research Program of the National Institutes of Health Clinical Center (Bethesda, MD, USA). One of the authors (RMS) certifies that he received funding support through the National Institutes of Health (NIH) Medical Research Scholars Program, a public-private partnership supported jointly by the NIH and generous contributions to the Foundation for the NIH, the Doris Duke Charitable Foundation, the American Association for Dental Research, the Colgate-Palmolive Company, Genentech, and other private donors.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Functional and Applied Biomechanics Section, Rehabilitation Medicine Department, National Institutes of Health, Bethesda, MD, USA.
References
- 1.Beasley MA, Stracciolini A, Tyson KD, Stein CJ. Knee injury patterns in young Irish dancers. Med Probl Perform Art. 2014;29:70–73. [DOI] [PubMed] [Google Scholar]
- 2.Behnam AJ, Herzka DA, Sheehan FT. Assessing the accuracy and precision of musculoskeletal motion tracking using cine-PC MRI on a 3.0T platform. J Biomech. 2011;44:193–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20:725–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boykin RE, McFeely ED, Shearer D, Frank JS, Harrod CC, Nasreddine AY, Kocher MS. Correlation between the Child Health Questionnaire and the International Knee Documentation Committee score in pediatric and adolescent patients with an anterior cruciate ligament tear. J Pediatr Orthop. 2013;33:216–220. [DOI] [PubMed] [Google Scholar]
- 5.Carlson VR, Boden BP, Sheehan FT. Patellofemoral kinematics and tibial tuberosity-trochlear groove distances in female adolescents with patellofemoral pain. Am J Sports Med. 2017;45:1102–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng RD, Jackson JN, McCreedy ES, Gandler W, Eijkenboom JJFA, van Middelkoop M, McAuliffe MJ, Sheehan FT. Patellar segmentation from 3D magnetic resonance images using guided recursive ray-tracing for edge pattern detection. Proc SPIE. 2016;9788. [Google Scholar]
- 7.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ, USA: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 8.Coleman JL, Widmyer MR, Leddy HA, Utturkar GM, Spritzer CE, Moorman CT, 3rd, Guilak F, DeFrate LE. Diurnal variations in articular cartilage thickness and strain in the human knee. J Biomech. 2013;46:541–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dargel J, Michael JW, Feiser J, Ivo R, Koebke J. Human knee joint anatomy revisited: morphometry in the light of sex-specific total knee arthroplasty. J Arthroplasty. 2011;26:346–353. [DOI] [PubMed] [Google Scholar]
- 10.Fairbank JC, Pynsent PB, van Poortvliet JA, Phillips H. Mechanical factors in the incidence of knee pain in adolescents and young adults. J Bone Joint Surg Br. 1984;66:685–693. [DOI] [PubMed] [Google Scholar]
- 11.Findley S. Age limits and adolescents. Paediatrics & Child Health. 2003;8:577–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Freedman BR, Sheehan FT. Predicting three-dimensional patellofemoral kinematics from static imaging-based alignment measures. J Orthop Res. 2013;31:441–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guevara JM, Moncayo MA, Vaca-Gonzalez JJ, Gutierrez ML, Barrera LA, Garzon-Alvarado DA. Growth plate stress distribution implications during bone development: a simple framework computational approach. Comput Methods Programs Biomed. 2015;118:59–68. [DOI] [PubMed] [Google Scholar]
- 14.Herbst KA, Barber Foss KD, Fader L, Hewett TE, Witvrouw E, Stanfield D, Myer GD. Hip strength is greater in athletes who subsequently develop patellofemoral pain. Am J Sports Med. 2015;43:2747–2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Julián-Almárcegui C, Gómez-Cabello A, Huybrechts I, González-Agüero A, Kaufman JM, Casajús JA, Vicente-Rodríguez G. Combined effects of interaction between physical activity and nutrition on bone health in children and adolescents: a systematic review. Nutr Rev. 2015;73:127–139. [DOI] [PubMed] [Google Scholar]
- 16.Kastelein M, Luijsterburg PAJ, Heintjes EM, van Middelkoop M, Verhaar JAN, Koes BW, Bierma-Zeinstra SMA. The 6-year trajectory of non-traumatic knee symptoms (including patellofemoral pain) in adolescents and young adults in general practice: a study of clinical predictors. Br J Sports Med. 2014;49:400–405. [DOI] [PubMed] [Google Scholar]
- 17.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–163. [DOI] [PubMed] [Google Scholar]
- 18.Maffulli N, Longo UG, Spiezia F, Denaro V. Aetiology and prevention of injuries in elite young athletes. Med Sport Sci. 2011;56:187–200. [DOI] [PubMed] [Google Scholar]
- 19.National Research Council, Institute of Medicine. Adolescent development and the biology of puberty: summary of a workshop on new research. In: Kipke MD, ed. Adolescent Development and the Biology of Puberty: Summary of a Workshop on New Research. Washington, DC, USA: The National Academies Press; 1999. [PubMed] [Google Scholar]
- 20.Newcomer RR, Perna FM. Features of posttraumatic distress among adolescent athletes. J Athl Train. 2003;38:163–166. [PMC free article] [PubMed] [Google Scholar]
- 21.Pinskerova V, Nemec K, Landor I. Gender differences in the morphology of the trochlea and the distal femur. Knee Surg Sports Traumatol Arthrosc. 2014;22:2342–2349. [DOI] [PubMed] [Google Scholar]
- 22.Powers CM, Bolgla LA, Callaghan MJ, Collins N, Sheehan FT. Patellofemoral pain: proximal, distal, and local factors, 2nd International Research Retreat. J Orthop Sports Phys Ther. 2012;42:A1–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17:45–56. [DOI] [PubMed] [Google Scholar]
- 24.Quatman-Yates CC, Myer GD, Ford KR, Hewett TE. A longitudinal evaluation of maturational effects on lower extremity strength in female adolescent athletes. Pediatr Phys Ther. 2013;25:271–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rathleff CR, Olesen JL, Roos EM, Rasmussen S, Rathleff MS. Half of 12-15-year-olds with knee pain still have pain after one year. Dan Med J. 2013;60:A4725. [PubMed] [Google Scholar]
- 26.Rathleff MS. High prevalence of daily and multi-site pin—a cross-sectional population-based study among 3000 Danish adolescents. BMC Pediatr. 2013;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rathleff MS, Rathleff CR, Olesen JL, Rasmussen S, Roos EM. Is knee pain during adolescence a self-limiting condition? Prognosis of Patellofemoral pain and other types of knee pain. Am J Sports Med. 2016;44:1165–1171. [DOI] [PubMed] [Google Scholar]
- 28.Rathleff MS, Samani A, Olesen JL, Roos EM, Rasmussen S, Christensen BH, Madeleine P. Neuromuscular activity and knee kinematics in adolescents with patellofemoral pain. Med Sci Sports Exerc. 2013;45:1730–1739. [DOI] [PubMed] [Google Scholar]
- 29.Roth-Isigkeit A, Thyen U, Stöven H, Schwarzenberger J, Schmucker P. Pain among children and adolescents: restrictions in daily living and triggering factors. Pediatrics. 2005;115:e152–e162. [DOI] [PubMed] [Google Scholar]
- 30.Rothermich MA, Nepple JJ, Raup VT, O'Donnell JC, Luhmann SJ. A comparative analysis of International Knee Documentation Committee scores for common pediatric and adolescent knee injuries. J Pediatr Orthop. 2016;36:274–277. [DOI] [PubMed] [Google Scholar]
- 31.Sanchis-Alfonso V, McConnell J, Monllau JC, Fulkerson JP. Diagnosis and treatment of anterior knee pain. Journal of ISAKOS: Joint Disorders & Orthopaedic Sports Medicine. 2016;1:161–173. [Google Scholar]
- 32.Seisler AR, Sheehan FT. Normative three-dimensional patellofemoral and tibiofemoral kinematics: a dynamic, in vivo study. IEEE Trans Biomed Eng. 2007;54:1333–1341. [DOI] [PubMed] [Google Scholar]
- 33.Selfe J, Callaghan M, Witvrouw E, Richards J, Dey MP, Sutton C, Dixon J, Martin D, Stokes M, Janssen J, Ritchie E, Turner D. Targeted interventions for patellofemoral pain syndrome (TIPPS): classification of clinical subgroups. BMJ Open. 2013;3:e003795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sheehan FT, Brainerd EL, Troy KL, Shefelbine SJ, Ronsky JL. Advancing quantitative techniques to improve understanding of the skeletal structure-function relationship. J Neuroeng Rehabil. 2018;15:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sheehan FT, Derasari A, Fine KM, Brindle TJ, Alter KE. Q-angle and J-sign: indicative of maltracking subgroups in patellofemoral pain. Clin Orthop Relat Res. 2009;468:266–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shibanuma N, Sheehan FT, Stanhope SJ. Limb positioning is critical for defining patellofemoral alignment and femoral shape. Clin Orthop Relat Res. 2005;434:198–206. [DOI] [PubMed] [Google Scholar]
- 37.Smits-Engelsman B, Klerks M, Kirby A. Beighton score: a valid measure for generalized hypermobility in children. J Pediatr. 2011;158:119–123. e114. [DOI] [PubMed] [Google Scholar]
- 38.Stracciolini A, Casciano R, Levey Friedman H, Stein CJ, Meehan WP, 3rd, Micheli LJ. Pediatric sports injuries: a comparison of males versus females. Am J Sports Med. 2014;42:965–972. [DOI] [PubMed] [Google Scholar]
- 39.Tansey RJ, Green GL, Haddad FS. Large diameter heads: is bigger always better? Semin Arthroplasty. 2015;26:16–19. [Google Scholar]
- 40.Weiss MR. Psychological aspects of sport-injury rehabilitation: a developmental perspective. J Athl Train. 2003;38:172–175. [PMC free article] [PubMed] [Google Scholar]
- 41.Witvrouw E, Lysens R, Bellemans J, Cambier D, Guy V. Intrinsic risk factors for the development of anterior knee pain in an athletic population. Am J Sports Med. 2000;28:480–489. [DOI] [PubMed] [Google Scholar]
- 42.Yadav P, Shefelbine SJ, Gutierrez-Farewik EM. Effect of growth plate geometry and growth direction on prediction of proximal femoral morphology. J Biomech. 2016;49:1613–1619. [DOI] [PubMed] [Google Scholar]
- 43.Yilmaz B, Cicek ED, Sirin E, Ozdemir G, Karakus O, Muratli HH. A magnetic resonance imaging study of abnormalities of the patella and patellar tendon that predispose children to acute patellofemoral dislocation. Clin Imaging. 2017;42:83–87. [DOI] [PubMed] [Google Scholar]