Abstract
Background
Patients with comparable severities of developmental dysplasia of the hip (DDH) may variably progress to osteoarthritis (OA) over time. Although joint congruency may be associated with OA progression in patients with DDH, it has only been assessed subjectively. We assessed the gap between the rotational centers of the acetabulum and femoral head (center gap) as a possible predictive measure of OA progression in patients with DDH.
Questions/purposes
In patients with bilateral DDH, we asked: (1) What is the probability of OA progression (Tönnis grade) or symptom development (pain) in the asymptomatic contralateral hip of patients with DDH undergoing unilateral joint-preserving surgery? (2) Is the center gap measurement associated with OA progression or symptom development in these hips? (3) Is the center gap measurement correlated with previous radiographic parameters?
Methods
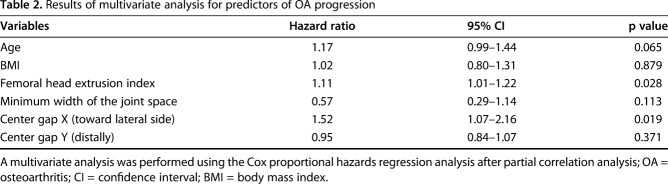
A total of 297 patients (319 hips) underwent unilateral eccentric rotational acetabular osteotomy at our institution between July 1989 and December 1999. We performed no other joint-preserving surgery to treat patients with DDH during this timeframe. The inclusion criteria for the study were patients younger than 55 years of age, the contralateral hip classified as Tönnis Grade 0, no previous surgical interventions, and asymptomatic at the time of eccentric rotational acetabular osteotomy (155 patients, 155 hips). The exclusion criteria were a contralateral hip without dysplasia (four patients, four hips), loss to followup before 10 years (42 patients, 42 hips [27%]), or missing medical records or radiographs (21 patients, 21 hips [14%]). The remaining 88 patients (88 hips; 11 males and 77 females) with a mean age of 39 years (range, 17–53 years) and mean followup of 20 years (range, 10-27 years) were analyzed. From the institutional database, radiographic parameters including the center gap in the AP view were assessed using radiographs at the time of eccentric rotational acetabular osteotomy, and the Tönnis grade was recorded 1 year postoperatively and annually thereafter retrospectively. We defined migration of the rotational center of the femoral head based on the rotational center of the acetabulum in the horizontal plane as center gap X (mm) and in the vertical plane as center gap Y (mm) and defined the absolute value between the centers as center gap distance (mm). Using κ statistics, intra- and interobserver reliabilities were determined to be 0.896 and 0.857 for center gap X, 0.912 and 0.874 for center gap Y, and 0.912 and 0.901 for the center gap distance, respectively. When patients reported any contralateral ipsilateral hip pain during clinic visits, the hip was considered symptomatic. Kaplan-Meier survivorship analyses were performed with OA progression or symptom development in the nonoperative hip as the endpoint. Multivariate analyses were performed to assess risk factors for each outcome using the Cox proportional hazards model. Correlation analyses between the center gap and other parameters including lateral center-edge angle, femoral head extrusion index, acetabular depth-to-width index, femoral head lateralization, minimum width of the joint space, head sphericity, and joint congruency were performed using Pearson’s correlation coefficient.
Results
At 20 years postoperatively, the probability of OA progression in the nonoperative hip was 13% (95% confidence interval [CI], 7.1–22.1) and the probability of symptom development was 34% (95% CI, 24.7–46.1). The center gap X measurements in the groups with OA progression (lateral 2.0 ± 2.1 [SD] mm) or symptom development (lateral 0.9 ± 2.4 mm) took a more lateral direction than those in the group without OA progression (medial 0.4 ± 2.1 mm) or symptom development (medial 0.5 ± 2.0 mm) (OA progression, p < 0.001; symptom development, p = 0.005). The center gap Y measurements in the groups with OA progression (distal 2.7 ± 7.1 mm) or symptom development (distal 2.1 ± 6.0 mm) took a more distal direction than those in the group without OA progression (proximal 1.6 ± 6.2 mm) or symptom development (proximal 2.5 ± 6.1 mm) (OA progression, p = 0.027; symptom development, p = 0.001). Independent risk factors for OA progression were the femoral head extrusion index (hazard ratio [HR], 1.11; 95% CI, 1.01–1.22; p = 0.028) and the center gap X (HR, 1.52; 95% CI, 1.07–2.16; p = 0.019), whereas no independent risk factors for symptom development were found. The center gap in the horizontal plane had no correlations with any other radiographic parameter studied.
Conclusions
The center gap in the horizontal plane had a modest association with OA progression in this group of patients with DDH. Future studies are needed to determine the normal value of the center gap for patients without DDH and to assess the center gap in lateral radiographic views.
Level of Evidence
Level IV, prognostic study.
Introduction
Developmental dysplasia of the hip (DDH) is a risk factor for the development of secondary hip osteoarthritis (OA) [6, 11, 17, 22]. However, there is some controversy whether the lateral center-edge angle [4, 21] is predictive of OA progression [16] or not [9]. In our daily clinical practice we often encounter patients with relatively similar grades of DDH severity who demonstrate a wide disparity of OA progression during long-term followup.
Wyles et al. [22] demonstrated that for a patient with DDH who recently developed Tönnis Grade 1 degenerative change [20], the probability of undergoing THA in 10 years is approximately one in three. Consequently, for joint-preserving surgery in DDH, it is important to detect those patients whose hips are at risk for progressive arthritic changes. In a retrospective case study of contralateral hips in 398 patients with THA, Amstutz and Le Duff [2] demonstrated that the minimum width of the joint space was an additional risk factor for OA progression in patients with DDH. However, the mean followup of 11 years was relatively short for observing the natural history. We presumed that joint congruency was also a radiographic predictor of OA progression in patients with DDH; research has shown that joint congruency assessed using a subjective classification system [23] is associated with conversion to THA after eccentric rotational acetabular osteotomy [12] as a joint-preserving surgery for DDH [1]. The appearance of joint congruency reflects the difference in curvature between the acetabulum and the femoral head. Okuzu et al. [18], in their CT imaging study in 207 female patients with DDH, indicated that the more severe the hip subluxation, the smaller the radius of curvature of the acetabulum. However, no study has assessed the difference in curvature between the acetabulum and the femoral head. To obtain a more objective measure of joint congruency, we propose a measurement of the gap between the rotational centers of the acetabulum and the femoral head as a new radiographic parameter termed the “center gap.”
We sought to answer the following questions: (1) What is the probability of OA progression (Tönnis grade) or symptom development (pain) in the asymptomatic contralateral hip of patients with DDH undergoing unilateral joint-preserving surgery? (2) Is the center gap measurement associated with OA progression or symptom development in these hips? (3) Is the center gap measurement correlated with previous radiographic parameters?
Patients and Methods
This was a retrospective case series. After we obtained institutional review board approval, we searched our surgical database and retrospectively identified a total of 297 patients (319 hips) who had undergone unilateral eccentric rotational acetabular osteotomy at our institution between July 1989 and December 1999. All of these procedures were performed by the senior author (YH). We performed no other joint-preserving surgery to treat patients with DDH during the timeframe. Medical charts and pertinent radiographs were not always available before July 1989. We excluded 22 patients who underwent bilateral eccentric rotational acetabular osteotomies during that timeframe. We studied the hips that were contralateral to the eccentric rotational acetabular osteotomy.
We included 155 patients (155 hips) who were younger than 55 years of age [22] with a contralateral hip classified as Tönnis Grade 0 who had no previous surgical interventions and who were asymptomatic at the time of eccentric rotational acetabular osteotomy. The exclusion criteria were the absence of dysplasia in the contralateral hip (defined as a lateral center-edge angle > 25°; four patients, four hips) [21, 22], loss to followup before 10 years (42 patients, 42 hips [27%]), or missing medical records or radiographs (21 patients, 21 hips [14%]). The remaining 88 patients (88 hips) were analyzed in this study (Fig. 1). The patients had a mean age of 39 years (range, 17–53 years) and the mean followup was 20 years (range, 10-27 years) (Table 1). Most of the authors (DM, YH, TS, TA, YT, TK, YH) were involved in the followup of these patients. Among the excluded patients with followup periods of < 10 years (42 patients, 42 hips), 40 patients discontinued followup at our hospital because they resumed followup with other physicians and hospitals after the eccentric rotational acetabular osteotomy procedure. We postoperatively followed the remaining two patients; one was a 36-year-old woman with moderate contralateral DDH (lateral center-edge angle = 15°), and the other was a 39-year-old woman with mild contralateral DDH (lateral center-edge angle = 20°). However, they discontinued followup at 6.3 and 9.1 years postoperatively, respectively. During their followup periods, neither OA progression nor symptom development was observed.
Fig. 1.
The diagram demonstrates subsets of the study group.
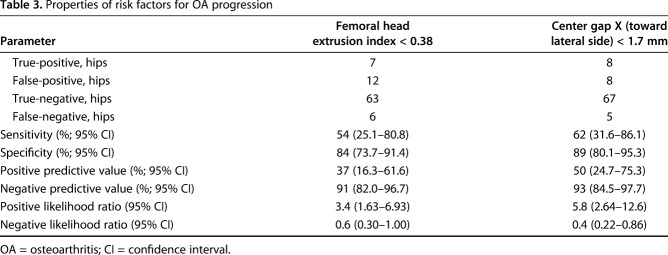
Table 1.
Patient demographic data
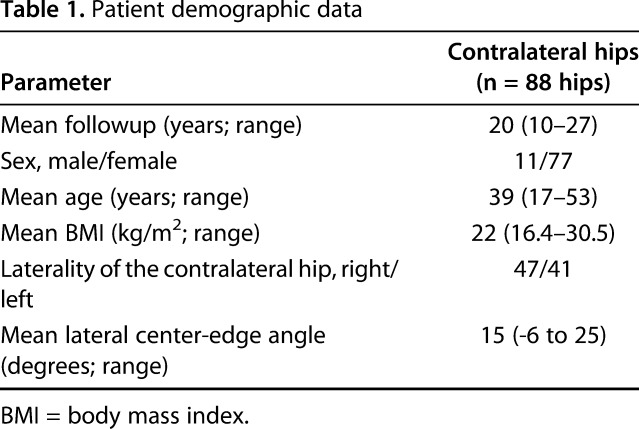
AP view radiographs of patients in the supine position were obtained at the time of eccentric rotational acetabular osteotomy, 1 year postoperatively, and annually thereafter from the institutional database. For AP view radiographs, both hips were neutrally rotated with 0° abduction. The Tönnis grade [20] of the contralateral hip was recorded using each followup radiograph, retrospectively. Other radiographic parameters including the center gap were assessed using radiographs at the time of eccentric rotational acetabular osteotomy. The previous radiographic parameters were as follows (Fig. 2): lateral center-edge angle (in degrees) [21], femoral head extrusion index [13], acetabular depth-to-width index [15], femoral head lateralization (mm) [4], minimum width of the joint space (mm), head sphericity (spherical or aspherical) [4], and joint congruency (excellent, good, fair, or poor) [23]. Two authors (DM, TA) independently evaluated these parameters and Tönnis grade using a medical computer system (NeoChart Hospital Information System; Fujitsu, Tokyo, Japan). Using κ statistics, interobserver variabilities were determined to be 0.741, 0.875, 0.967, 0.915, 0.923, 0.945, 0.911, and 0.819 for Tönnis grade, lateral center-edge angle, femoral head extrusion index, acetabular depth-to-width index, femoral head lateralization, minimum width of the joint space, head sphericity, and joint congruency, respectively.
Fig. 2 A-D.
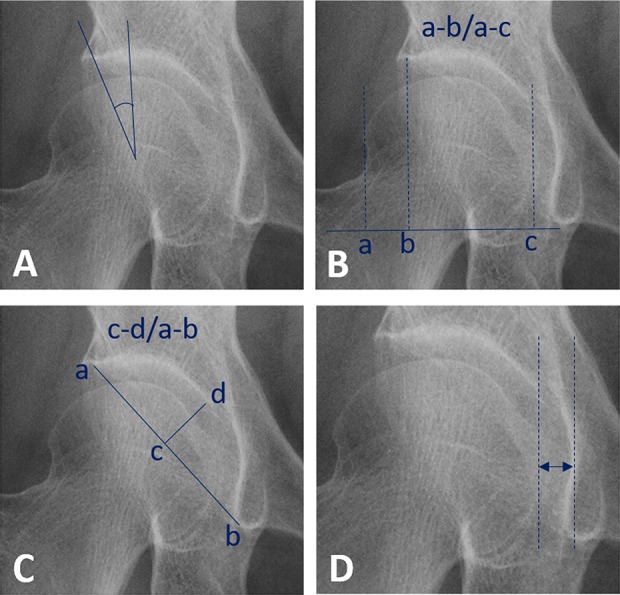
Some previous radiographic parameters on the AP view radiograph are shown. (A) Lateral center-edge angle; (B) femoral head extrusion index; (C) acetabular depth-to-width index; and (D) femoral head lateralization are illustrated.
The center gap was investigated using Roman Version 1.70 software computer digitizer facilities (Institute of Orthopedics, Oswestry, UK) [8]. After normalization using the measure on radiographs, distances in the horizontal and vertical planes and the absolute value between rotational centers of the acetabulum and femoral head were measured (Fig. 3). We defined migration of the rotational center of the femoral head based on the rotational center of the acetabulum in the horizontal plane as center gap X (mm) and in the vertical plane as center gap Y (mm) and defined the absolute value between the centers as center gap distance (mm). Using κ statistics, intra- and interobserver variabilities were determined to be 0.896 and 0.857 for center gap X, 0.912 and 0.874 for center gap Y, and 0.912 and 0.901 for the center gap distance, respectively.
Fig. 3 A-D.
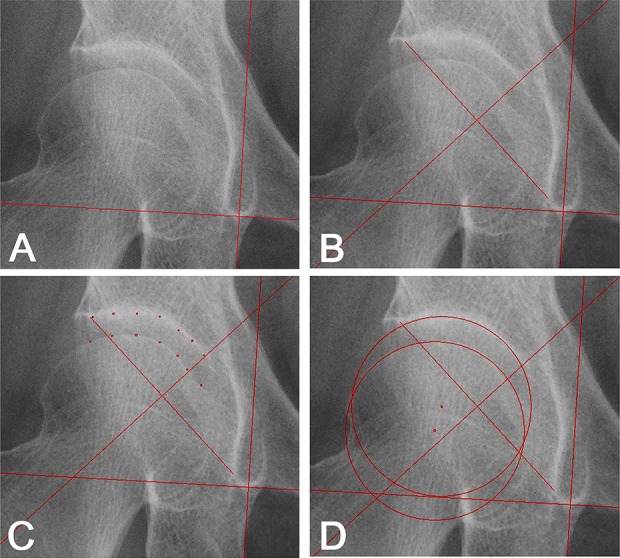
The center gap measurement method is shown. (A) A vertical line is drawn based on the horizontal line connecting the inferior ends of the left- and right-sided teardrops. (B) A perpendicular bisector of a line segment is drawn connecting the inferior and superior edges of the acetabulum. (C) Seven points on the joint surface except the fossa in the superior half of the acetabulum that is separated by the perpendicular bisector are plotted. The surface of the femoral head is plotted using seven points within the same region as the acetabulum. (D) Circles of the acetabulum and femoral head are automatically constructed by the interpolation of those seven points. Distances in the horizontal and vertical planes and the absolute value between the centers are measured digitally. All measurements are normalized using the known diameter of the measure on radiographs.
We considered progression from Tönnis Grade 0 to 2 or 3 to be OA progression [3]. We also assessed symptom development at time points on followup radiographs according to the pain subscale of the Harris hip score (HHS) [10] from medical charts. When patients reported slight or occasional contralateral hip pain that equaled 40 points on the pain subscale of the HHS, the hip was considered symptomatic. These assessments were completed on all 88 patients (88 hips).
Survivorship analyses using the Kaplan-Meier method with OA progression or symptomatic hip as the endpoint were performed, and probabilities of OA progression and symptomatic hip were calculated at 5, 10, 15, and 20 years. All contralateral hips were included in survivorship analyses at 5 and 10 years postoperatively, and a total of 85 patients (97%) were analyzed at 15 years postoperatively and 50 (57%) patients were analyzed at 20 years postoperatively.
To assess risk factors for each outcome, we performed preliminary univariate analyses using the unpaired Student’s t-tests or chi-square and Fisher’s exact tests for all variables; these included sex; age; body mass index (BMI); laterality of the contralateral hip; previous radiographic parameters mentioned; and center gap X, Y, and distance. After extracting variables with a p value < 0.2, we performed partial correlation analyses for variables that had a strong correlation with an r value > 0.6 between each other. Regarding OA progression, age, BMI, femoral head extrusion index, minimum width of the joint space, and center gap X and Y were included for multivariate analysis using the Cox proportional hazards model. Regarding symptom development, BMI, femoral head extrusion index, femoral head lateralization, and center gap X and Y were included for the analysis. The thresholds for independent risk factors were determined by the Youden index (J = sensitivity + specificity − 1) based on its correspondence with OA progression. Furthermore, to evaluate the role of the center gap measurement, the relationship of center gaps X, Y, and distance with previous radiographic parameters was assessed by correlation analyses using the Pearson’s correlation coefficient. We used SPSS Version 21 (IBM Corp, Armonk, NY, USA) for all statistical analyses. Statistical significance was accepted for p values < 0.05.
Results
Probability of OA Progression and Symptom Development in Contralateral DDH
The probability of OA progression was 0% at 5 years, 0% at 10 years, 7% (95% confidence interval [CI], 3.3–15.2) at 15 years, and 13% (95% CI, 7.1–22.1) at 20 years postoperatively. In the 13 patients (15%) who eventually had OA progression in their contralateral hips, the mean duration from the unilateral eccentric rotational acetabular osteotomy to OA progression in the contralateral hip was 16 years (range, 11–25 years). All contralateral hips of these patients were symptomatic at their final followup, and the mean duration from the onset of symptoms to OA progression was 4 years (range, -3 to 9 years). Two hips had OA progression before symptom development. The probability of symptom development (pain on the HHS pain scale) was 0% at 5 years, 7% (95% CI, 3.2–14.7) at 10 years, 18% (95% CI, 11.0–27.5) at 15 years, and 34% (95% CI, 24.7–46.1) at 20 years postoperatively. In the 30 patients (34%) who eventually had a symptomatic contralateral hip, the mean duration from the unilateral eccentric rotational acetabular osteotomy to a symptomatic contralateral hip was 15 years (range, 8–22 years). Among the contralateral hips of these patients, we observed OA progression in 13 hips (43%).
Center Gap Association With OA Progression or Symptom Development
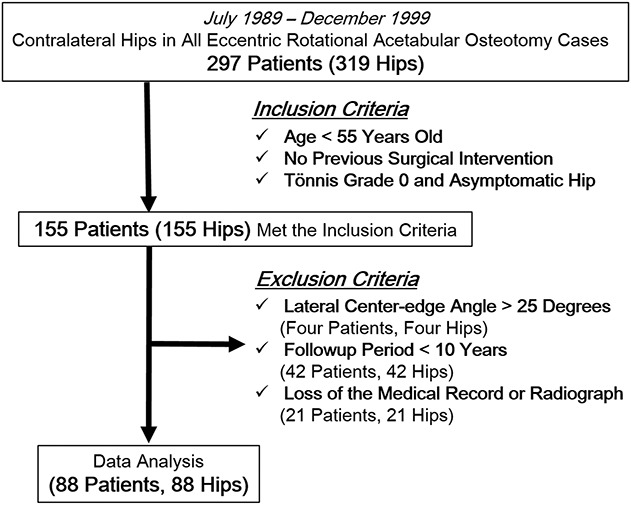
After controlling for potential confounding variables such as sex, laterality of the contralateral hip, lateral center-edge angle, acetabular depth-to-width index, femoral head lateralization, head sphericity, joint congruency, and center gap distance, we found the femoral head extrusion index (hazard ratio [HR], 1.11; 95% CI, 1.01–1.22; p = 0.028) and center gap X (HR, 1.52; 95% CI, 1.07–2.16; p = 0.019) were independent risk factors for OA progression using the Cox proportional hazards regression analysis (Table 2). However, after controlling for potential confounding variables, we found no independent risk factors for symptom development.
Table 2.
Results of multivariate analysis for predictors of OA progression
For OA progression from Tönnis Grade 0 to 2 or 3, threshold values of the femoral head extrusion index and center gap X were 0.38 and lateral 1.7 mm, respectively. For a combination of the femoral head extrusion index or the center gap X, the sensitivity, specificity, and positive predictive value were 77% (95% CI, 46.2–95.0), 76% (95% CI, 64.7–85.1), and 36% (95% CI, 18.6–55.9), respectively. For a combination of the femoral head extrusion index and the center gap X, the sensitivity, specificity, and positive predictive value were 39% (95% CI, 13.9–68.4), 97% (95% CI, 90.7–99.7), and 71% (95% CI, 29.0–96.3), respectively (Table 3).
Table 3.
Properties of risk factors for OA progression
The center gap X measurements in the groups with OA progression (lateral 2.0 ± 2.1 [SD] mm) or symptom development (lateral 0.9 ± 2.4 mm) took a more lateral direction than those in the group without OA progression (medial 0.4 ± 2.1 mm) or symptom development (medial 0.5 ± 2.0 mm) (OA progression, p < 0.001; symptom development, p = 0.005) (Fig. 4). The center gap Y measurements in the groups with OA progression (distal 2.7 ± 7.1 mm) or symptom development (distal 2.1 ± 6.0 mm) took a more distal direction than those in the group without OA progression (proximal 1.6 ± 6.2 mm) or symptom development (proximal 2.5 ± 6.1 mm) (OA progression, p = 0.027; symptom development, p = 0.001). However, no differences in the center gap distance were observed between the groups with OA progression (6.8 ± 4.3 mm) or symptom development (5.7 ± 3.9 mm) and without OA progression (5.3 ± 4.3 mm) or symptom development (5.4 ± 4.5 mm) (OA progression, p = 0.261; symptom development, p = 0.781) (Fig. 5).
Fig. 4 A-F.
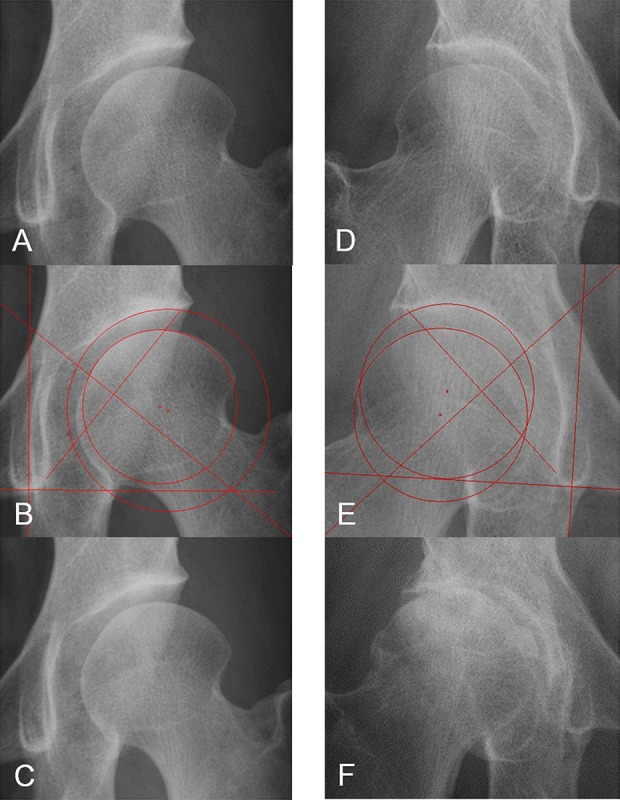
(A) The case is a 34-year-old woman without OA progression. A hip radiograph of the contralateral side in the AP view at the time of eccentric rotational acetabular osteotomy shows severe DDH with a lateral center-edge angle of 13°. (B) The center gap X is calculated to be medial 2 mm. (C) OA progression is not observed 22 years postoperatively. (D) The case is a 43-year-old woman with OA progression. A hip radiograph of the contralateral side in the AP view at the time of eccentric rotational acetabular osteotomy shows mild DDH with a lateral center-edge angle of 23°. (E) The center gap X is calculated to be lateral 1.8 mm. (F) OA progression is observed at 18 years postoperatively.
Fig. 5 A-B.
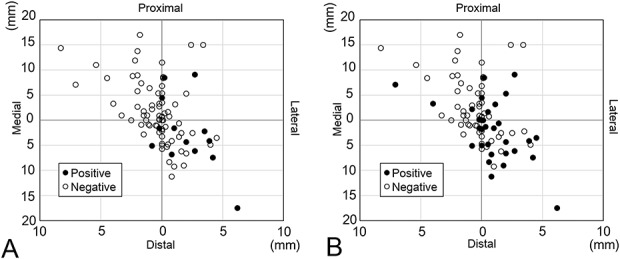
Scatter diagrams of the center gap in the AP view at the time of eccentric rotational acetabular osteotomy are demonstrated. (A) The endpoint is OA progression. (B) The endpoint is a symptomatic hip.
Relationships Between the Center Gap and Previous Radiographic Parameters
The center gap X and center gap distance had no correlations with any other measured radiographic parameter. Conversely, the center gap Y was correlated with the femoral head extrusion index (r = 0.236, p = 0.027) and acetabular depth-to-width index (r = -0.222, p = 0.037) as radiographic features of DDH and with joint congruency as a subjective radiographic assessment (r = 0.304, p = 0.004).
Discussion
DDH is commonly recognized as a structural hip morphology leading to premature degenerative changes [5, 11, 17, 22]. However, the long-term natural history of DDH is not sufficiently well understood, particularly regarding both OA and symptom progression. Furthermore, whether certain radiographic features of DDH are risk factors for OA progression remains controversial [9, 16]. The current study was undertaken to assess the long-term natural history of asymptomatic contralateral DDH without joint degeneration in patients undergoing eccentric rotational acetabular osteotomy and to analyze the potential of a new radiographic predictor of OA progression, the center gap, apart from other standard radiographic features of DDH [13, 15, 21].
There are some potential limitations of this study. First, the study used a relatively small cohort and lacked a control group. The true effect of each variable on OA progression and symptom development may have been under- or overestimated. Our results obtained from survivorship analyses with OA progression and symptom development showed wide CIs (> 10%) at 10, 15, and 20 years postoperatively. However, we feel these results are reliable because probabilities of both endpoints increased progressively over time. Furthermore, it is essential to perform a comparison with normal hips without DDH. Other than the patients included in this study, however, there were only five patients (three males and two females) without contralateral DDH who underwent eccentric rotational acetabular osteotomy during the same time. Further studies using larger cohorts, including patients with normal hip morphology, are required. Second, > 40% (63 of 155) of potentially eligible patients were excluded because of loss to followup before 10 years or missing records or radiographs. From medical chart review, although we could not estimate radiographic parameters, these patients were noted to be younger than our cohort, who had a mean age of 35 years (range, 17–52 years) at the time of eccentric rotational acetabular osteotomy (p = 0.033, unpaired Student’s t-test). Thus, it is possible that our results from survivorship analyses would differ from outcomes in these patients, because DDH severity or center gap in their contralateral hips might be worse than results shown in this study. Third, all of our patients were Japanese, who are shorter and lighter on average than their Western counterparts. Some previous studies reported that being overweight was a risk factor for OA progression [5, 19], and so our findings may or may not generalize to other patient populations and should be replicated in other populations. As well as body weight, differences in activity level and the nature of the patient’s work might influence the long-term natural history in the nonoperative hip. Unfortunately, however, we could not obtain reliable information from medical charts about these parameters. Furthermore, we should consider the effect of eccentric rotational acetabular osteotomy on the contralateral hip when we interpret our findings. Weight transfer on the nonoperative hip might reasonably be expected to improve after the operation. Fourth, the baseline of the contralateral hips was not the same. The natural history shown in this study may have been affected by degenerative changes in the cartilage or labrum that occurred before the first evaluation. Fifth, all measurements and estimations were performed only on AP view radiographs in the supine position because our indication for eccentric rotational acetabular osteotomy had been based on this radiographic view during the timeframe in question, although this limitation has been described in other previous studies [2, 22]. Unfortunately, standing AP radiographs, lateral radiographs, or CT scans of the contralateral hip were not available, and that information could also have influenced the study results [7]. Examinations with the patient standing are needed to assess the influence of stress loading on each radiographic parameter, including the center gap. Finally, we used Roman Version 1.70 software to measure the center gap in this study. The validity of Roman Version 1.70 software for rotational centers of the acetabulum and femoral head detected according to the method in this study has not been confirmed, because the software was originally designed to measure penetration of the femoral head into the acetabular component in THA [8]. However, this method is more objective and reliable than previous assessments of joint congruency [23] and can typically be performed in a relatively short time (approximately 3 minutes) without other mechanical devices.
At 20 years postoperatively, we found that the probability of OA progression in the nonoperative hip was 13% (95% CI, 7.1–22.1) and for symptom development it was 34% (95% CI, 24.7–46.1). There have been a few reports of the long-term natural history in patients with DDH. Results from Hisatome et al.’s [14] observational study of 61 patients with DDH with pre-OA or early OA contralateral to the side of a rotational acetabular osteotomy showed that 7.1% hips developed early OA at 10 years postoperatively. In an observational study of the contralateral side of 48 patients with DDH who underwent THA, Wyles et al. [22] demonstrated that 18% of patients with Tönnis Grade 0 developed Tönnis Grade 2 or 3 degenerative changes in the hip at 20 years postoperatively. The probability of OA progression obtained from our survivorship analyses was less compared with these previous reports. This may be attributable to the fact that our patients had no degenerative changes or pain in their contralateral hips at the first evaluation and that they were relatively young when unilateral eccentric rotational acetabular osteotomy was performed. The baseline of these contralateral hips was therefore presumably at an earlier stage than in those studies.
Our results demonstrated that the center gap X was an independent risk factor for OA progression in asymptomatic contralateral hips of patients with DDH undergoing eccentric rotational acetabular osteotomy. Although the sensitivity of center gap X for OA progression individually was not high (62%), the combination of the femoral head extrusion index or the center gap X may help us to detect those patients with early-stage DDH whose hip would possibly progress to a degenerative joint (sensitivity, 77%). Among this patient population, we could also distinguish patients at high risk for OA progression using the combination of the femoral head extrusion index and the center gap X (positive predictive value, 71%). Furthermore, the center gap X is easy for surgeons to use to determine whether there is a risk for OA progression because it is calculated as an objective numeric value. Conversely, a previous subjective classification system for joint congruency [23], albeit simple and easy to apply, may have the potential difficulty of determining the grade. In fact, it was demonstrated that the subjective classification system had a relatively low κ value in this study (interobserver variabilities, 0.819) and also in a previous study [1].
Our results obtained from correlation analyses showed that the center gap Y had a positive correlation with the femoral head extrusion index and a negative correlation with the acetabular depth-to-width index. Hence, DDH could affect migration of the center gap Y distally. Conversely, the center gap X had no correlation with previous radiographic parameters in our results. Thus, the center gap X represents a new radiographic parameter that was not assessed in prior DDH radiographic measurements, including joint congruency [23] as a subjective grade.
In conclusion, for a patient who has asymptomatic DDH without joint degeneration contralateral to the side undergoing eccentric rotational acetabular osteotomy, the probability of a symptomatic contralateral hip is 34% and 13% for OA progression at 20 years postoperatively. We propose that the center gap in the horizontal plane be considered as a new radiographic predictor of OA progression in DDH in addition to the femoral head extrusion index as a parameter of DDH severity. Further clinical studies for normal hips without DDH are warranted. Moreover, the center gap changes over time on nonoperative hips and those before and after eccentric rotational acetabular osteotomy on operative hips should also be analyzed. Although the center gap in the horizontal plane was moderately associated with OA progression in patients with DDH, the combination of the femoral head extrusion index and/or center gap in the horizontal plane was useful to predict the natural course of the asymptomatic hip in these patients.
Acknowledgments
This manuscript has been edited for English language, grammar, punctuation, and spelling by Enago, the editing brand of Crimson Interactive Pvt Ltd.
Footnotes
Each author certifies that neither he, nor any member of his immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This study was performed at the Department of Orthopedic Surgery, Nagoya University Graduate School of Medicine, Nagoya City, Aichi, Japan.
References
- 1.Amano T, Hasegawa Y, Seki T, Takegami Y, Murotani K, Ishiguro N. A pre-operative predictive score for the outcome eccentric of rotational acetabular osteotomy in the treatment of acetabular dysplasia and early osteoarthritis of the hip in adults. Bone Joint J. 2016;98:1326–1332. [DOI] [PubMed] [Google Scholar]
- 2.Amstutz HC, Le Duff MJ. The natural history of osteoarthritis: what happens to the other hip? Clin Orthop Relat Res. 2016;474:1802–1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chandrasekaran S, Darwish N, Gui C, Lodhia P, Suarez-Ahedo C, Domb BG. Outcomes of hip arthroscopy in patients with Tönnis grade-2 osteoarthritis at a mean 2-year follow-up: evaluation using a matched-pair analysis with Tönnis grade-0 and grade-1 cohorts. J Bone Joint Surg Am. 2016;98:973–982. [DOI] [PubMed] [Google Scholar]
- 4.Clohisy JC, Carlisle JC, Beaulé PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(Suppl 4):47–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper C, Inskip H, Croft P, Campbell L, Smith G, McLaren M, Coggon D. Individual risk factors for hip osteoarthritis: obesity, hip injury, and physical activity. Am J Epidemiol. 1998;147:516–522. [DOI] [PubMed] [Google Scholar]
- 6.Cooperman DR, Wallensten R, Stulberg SD. Acetabular dysplasia in the adult. Clin Orthop Relat Res. 1983;175:79–85. [PubMed] [Google Scholar]
- 7.Eijer H, Leunig M, Mahomed MN, Ganz R. Cross-table lateral radiographs for screening of anterior femoral head-neck offset in patients with femoro-acetabular impingement. Hip Int. 2001;11:37–41. [Google Scholar]
- 8.García-Rey E, García-Cimbrelo E, Cruz-Pardos A, Ortega-Chamarro J. New polyethylenes in total hip replacement: a prospective, comparative clinical study of two types of liner. J Bone Joint Surg Br. 2008;90:149–153. [DOI] [PubMed] [Google Scholar]
- 9.Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am. 2010;92:1162–1169. [DOI] [PubMed] [Google Scholar]
- 10.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 11.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33. [PubMed] [Google Scholar]
- 12.Hasegawa Y, Iwase T, Kitamura S, Yamauchi Ki K, Sakano S, Iwata H. Eccentric rotational acetabular osteotomy for acetabular dysplasia: follow-up of one hundred and thirty-two hips for five to ten years. J Bone Joint Surg Am. 2002;84:404–410. [PubMed] [Google Scholar]
- 13.Heyman CH, Herndon CH. Legg-Perthes disease; a method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950;32:767–778. [PubMed] [Google Scholar]
- 14.Hisatome T, Yasunaga Y, Tanaka R, Yamasaki T, Ishida O, Ochi M. Natural course of the minimally symptomatic nonoperated hip in patients with bilateral hip dysplasia treated with contralateral rotational acetabular osteotomy. J Orthop Sci. 2005;10:574–580. [DOI] [PubMed] [Google Scholar]
- 15.Jacobsen S. Adult hip dysplasia and osteoarthritis. Studies in radiology and clinical epidemiology. Acta Orthop Suppl. 2006;77:1–37. [PubMed] [Google Scholar]
- 16.Jessel RH, Zurakowski D, Zilkens C, Burstein D, Gray ML, Kim YJ. Radiographic and patient factors associated with pre-radiographic osteoarthritis in hip dysplasia. J Bone Joint Surg Am. 2009;91:1120–1129. [DOI] [PubMed] [Google Scholar]
- 17.Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985–989. [DOI] [PubMed] [Google Scholar]
- 18.Okuzu Y, Goto K, Kawata T, So K, Kuroda Y, Matsuda S. The relationship between subluxation percentage of the femoroacetabular joint and acetabular width in Asian women with developmental dysplasia of the hip. J Bone Joint Surg Am. 2017;99:e31. [DOI] [PubMed] [Google Scholar]
- 19.Oliveria SA, Felson DT, Cirillo PA, Reed JI, Walker AM. Body weight, body mass index, and incident symptomatic osteoarthritis of the hand, hip, and knee. Epidemiology. 1999;10:161–166. [PubMed] [Google Scholar]
- 20.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. [DOI] [PubMed] [Google Scholar]
- 21.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83(Suppl 58):1–135. [Google Scholar]
- 22.Wyles CC, Heidenreich MJ, Jeng J, Larson DR, Trousdale RT, Sierra RJ. The John Charnley Award: Redefining the natural history of osteoarthritis in patients with hip dysplasia and impingement. Clin Orthop Relat Res. 2017;475:336–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yasunaga Y, Ikuta Y, Kanazawa T, Takahashi K, Hisatome T. The state of the articular cartilage at the time of surgery as an indication for rotational acetabular osteotomy. J Bone Joint Surg Br. 2001;83:1001–1004. [DOI] [PubMed] [Google Scholar]