Abstract
Background
Psychosocial factors are key determinants of health after upper extremity injuries. However, a systematic review is needed to understand which psychosocial factors are most consistently associated with disability and how the language, conceptualization, and types of measures used to assess disability impact these associations in upper extremity injuries.
Questions/purposes
(1) What factors are most consistently associated with disability after upper extremity injuries in adults? (2) What are the trends in types of outcome measures and conceptualization of disability in patients’ upper extremity injuries?
Methods
We searched multiple electronic databases (PubMED, OVIDSP, PsycInfo, Google Scholar, ISI Web of Science) between January 1, 1996, and December 31, 2016, using terms related to the “upper extremity”, “outcome measurement”, and “impairment, psychological, social or symptomatic” variables. We included all studies involving adult patients with any musculoskeletal injury and excluded those that did not use patient-reported outcome measures. We identified and screened 9339 studies. Of these, we retained 41 studies that involved conditions ranging from fractures to soft tissue injuries in various regions of the arm. We conducted quality assessment using a 10-item validated checklist and a five-tier strength of evidence assessment. We used the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) criteria and registered the review before performing our search (PROSPERO: CRD42017054048). None of the authors received any funding to perform this work.
Results
Disability after upper extremity injury was most consistently associated with depression (21 cohorts), catastrophic thinking (13 cohorts), anxiety (11 cohorts), pain self-efficacy (eight cohorts), and pain interference (seven cohorts). Social and demographic factors were also associated with disability. Measures of impairment such as ROM and injury severity were least associated with disability. There has been a gradual increase in use of region or condition-specific patient-reported outcome measures and measures of psychological, social, and symptomatic factors over a period since the introduction of the World Health Organization (WHO) International Classification of Functioning, Disability and Health (ICF) around 2000. Approximately 17% of studies (n = 454 of 2628) had instances of unclear, conflicting, or inappropriate terminology and 11% of studies (n = 257 of 2628) involved misrepresentations of outcome measures related to disability.
Conclusions
Psychologic and social factors are most consistently associated with disability than factors related to impairment. Further research involving the assessment of depression, anxiety, and coping strategies in cohorts with specific injuries may support decision-making regarding the provision of emotional support and psychologic therapies during recovery. Using the WHO ICF framework to conceptualize disability is key in increasing strength of evidence and allowing accurate comparisons of research in this field.
Level of Evidence
Level IV, therapeutic study.
Introduction
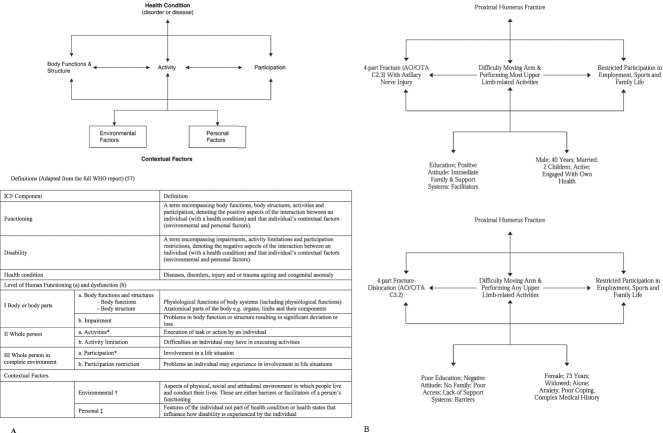
Understanding disability is fundamental in evaluating the outcomes of interventions after musculoskeletal injuries. The World Health Organization (WHO) International Classification of Functioning, Disability and Health (ICF) defines disability as a multidimensional construct involving a dynamic interaction between body functions and structures, activity limitations and participation restrictions, and environmental and personal factors associated with the relevant health condition (Fig. 1 A-B) [30, 53, 57]. Musculoskeletal injuries are often associated with substantial disability, affecting an individual’s quality of life (QoL) [4, 13, 27, 45]. Orthopaedic trauma to the upper extremity demonstrates greater disability and reduced health-related QoL indices compared with other body regions [13, 14]. The inability to feed, clean, and clothe, particularly when a dominant arm is involved, can be debilitating.
Fig. 1 A-B.
(A) A schematic is shown of the WHO ICF framework including ICF components and their definitions. *The activity and participation domains are organized into subdomains including: Learning and applying knowledge; General tasks and demands; Communication; Mobility; Self-care; Domestic life; Interpersonal international and relationships; Major life areas; Community, social and civic life. †The environmental domain is organized into subdomains including: Products and technology; Natural environment and human made changes to environment; Support and relationships; Attitudes; Services; Systems; Policies. ‡The personal domain is organized into subdomains including: Sex; Age; Race; Lifestyle habits; Coping styles; Social backgrounds; Education; Overall behavior patterns; Psychological assets. Adapted from: World Health Organization (Geneva) 2013. World Health Organization. How to use the ICF: A Practical Manual for Using the International Classification of Functioning. Available at: http://www.who.int/classifications/icf/en/. Accessed October 11, 2017. (B) Examples of the WHO ICF framework that was adapted to two different types of individual with a proximal humerus fracture. The examples include some features within each domain and are not intended to represent a complete overview of all subdomains. The direction of the arrows may differ depending on specific situations. Bidirectional arrows represent a two-way influence of one domain (or subdomain) on another.
There is growing recognition that the magnitude of disability correlates more with the subjective, psychosocial aspects of illness and pain (such as emotional distress and coping strategies) than objective measures of impairment and pathophysiology [17, 31, 33, 36, 54]. However, it is unclear which factors are most consistently associated with disability in orthopaedic trauma patients and what the strengths of these associations are. Furthermore, there is variability in the outcome measures used to assess disability, the manner in which the construct of disability is conceptualized, and the language used when defining the construct.
More than three decades since the introduction of the WHO ICF framework, there is still a level of misrepresentation and interchangeable use of terms related to disability and function despite the definitions being set out in the accompanying WHO manual [57]. The translation of research findings into the alleviation of posttraumatic disability requires a comprehensive summary of the factors associated with disability itself alongside clear and consistent language and conceptualization of the construct of disability.
We therefore performed a systematic review to answer the following questions: (1) What factors are most consistently associated with disability after upper extremity injuries in adults? (2) What are the trends in types of outcome measures used to represent disability and conceptualization of disability in patients with upper extremity injuries?
Materials and Methods
Search Strategy and Criteria
We used PubMED, OVIDSP, and PsycInfo electronic databases to identify all published studies from January 1, 1996, until December 31, 2016. We enlisted a librarian to determine a list of search terms and revised it as a multidisciplinary team. We combined terms related to “upper extremity”, “outcome measurement”, and “impairment, psychological, social and symptomatic variables” with the operator AND (Appendix, Supplemental Digital Content 1). The same search was used with additional electronic sources (Google Scholar, ISI Web of Science). No restrictions were set in the search fields and terms were identified in the title and/or abstract without limits. The review adheres to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) criteria [34] and the protocol is registered on the PROSPERO system (No. CRD42017054048).
All studies (Level I to Level IV) involving adult patients experiencing any musculoskeletal upper extremity injury condition for which they received operative and/or nonoperative interventions were eligible. Comparators were the outcome measures themselves and all outcomes were categorized into those assessing disability, impairment, psychologic, social, symptomatic, demographic, and other factors (Fig. 1 A-B). We followed strict identification and screening selection criteria (Fig. 2 A-B). We included only original research studies containing at least one patient-reported outcome measure (PROM) that could be equated to disability. We excluded studies focusing on clinometric features alone (eg, ROM, pathoanatomic or radiologic classification, clinical examination tests), single health components (eg, pain, depression, return to activity), and health behavior scales. Four investigators (PJ, A-MV, SG, CLO) performed identification and screening of titles and abstracts and two investigators (PJ, A-MV) conducted eligibility assessment. This phase entailed a closer inspection of abstracts and full-text review if there was any ambiguity in the abstract prose. The final set of full texts for inclusion was acquired and independently reviewed (PJ, A-MV, CF). Assessment for inclusion was performed together through discussion. We achieved a high level of consistency during the eligibility assessment and inclusion process, and consensus discussions were not required.
Fig. 2 A-B.
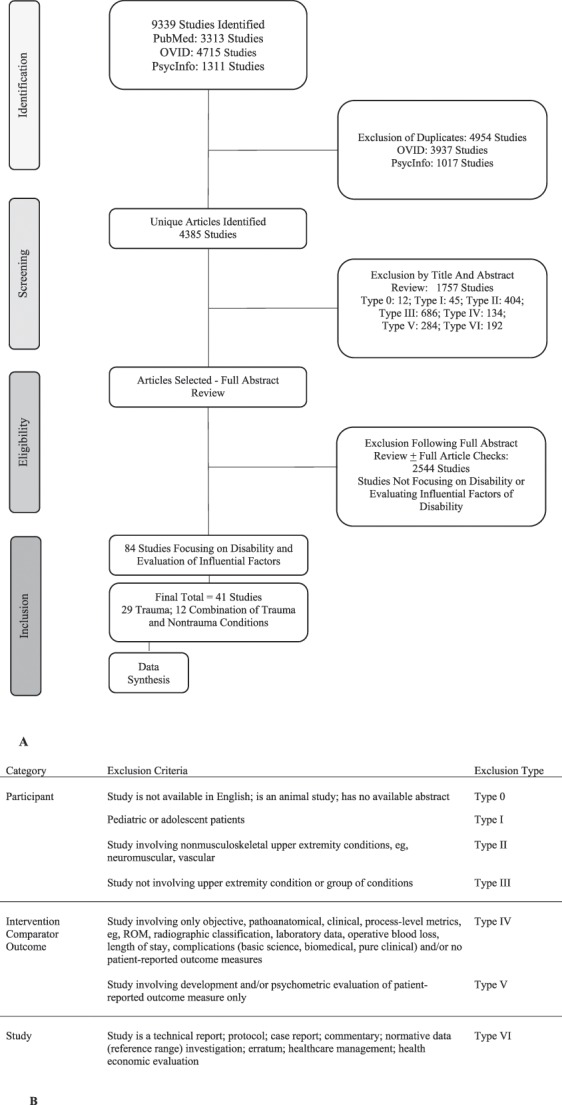
(A) A flowchart demonstrates the number of articles selected during the stages of identification, screening, eligibility, and inclusion following a search period from January 1, 1996, to December 31, 2016. (B) Screening and exclusion criteria are shown.
Quality assessment was conducted independently by three reviewers (PJ, A-MV, CF) using a 10-item checklist related to demographics, data collection, diagnosis, control group, participation/response rate, differences between responders and nonresponders, outcome measures, statistics, consent, and participant selection [23, 52]. This was a modified, population-specific version of established criteria used in previous systematic reviews of prognostic factors for patients with musculoskeletal disorders [23, 52]. The 10 items each had yes (+) and no (-) options, and we awarded a point (+) if there was sufficient information and no likelihood of potential bias. We calculated a quality score by counting all positively rated items (maximum score 10) and converted to a percentage total. An arbitrary classification was defined a priori as low (< 50%), moderate (50%-70%), and high quality (> 70%). Studies scoring > 50% were included in the strength of evidence evaluation. It was planned that any disagreements would be dealt with by reaching consensus with two additional authors (SG, MW) as required. However, a high level of consistency in agreement was present during quality assessment, and consensus discussions were not required.
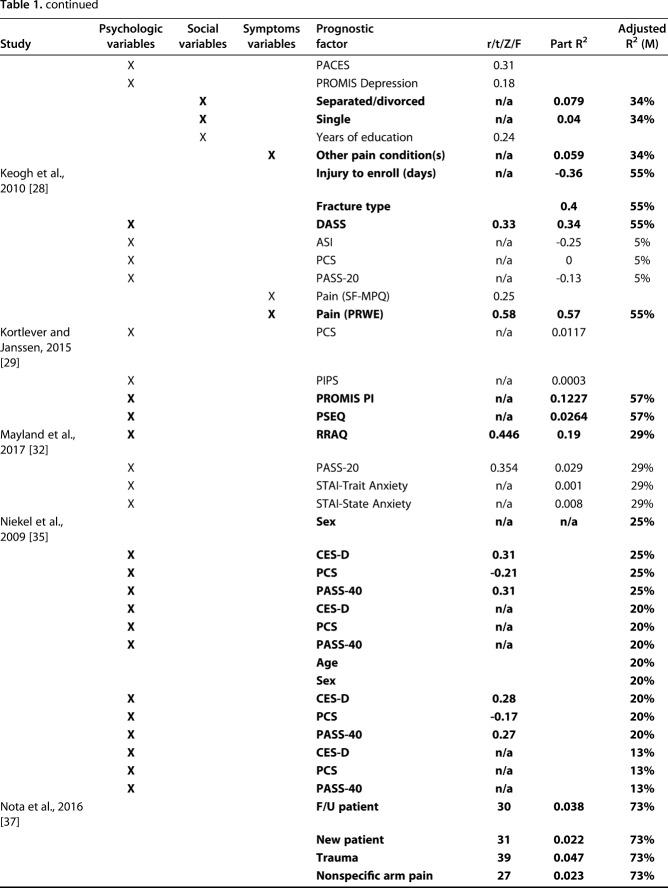
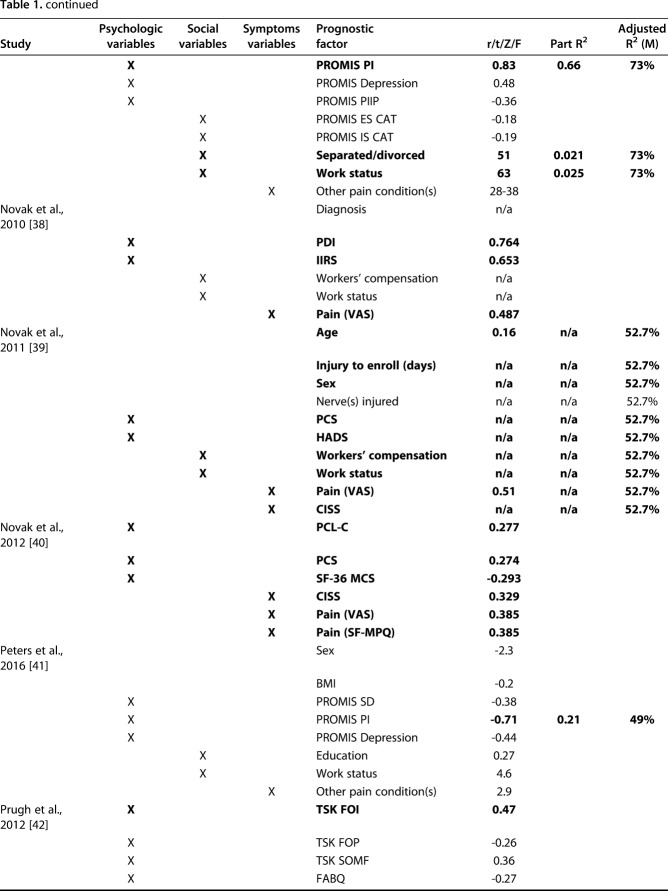
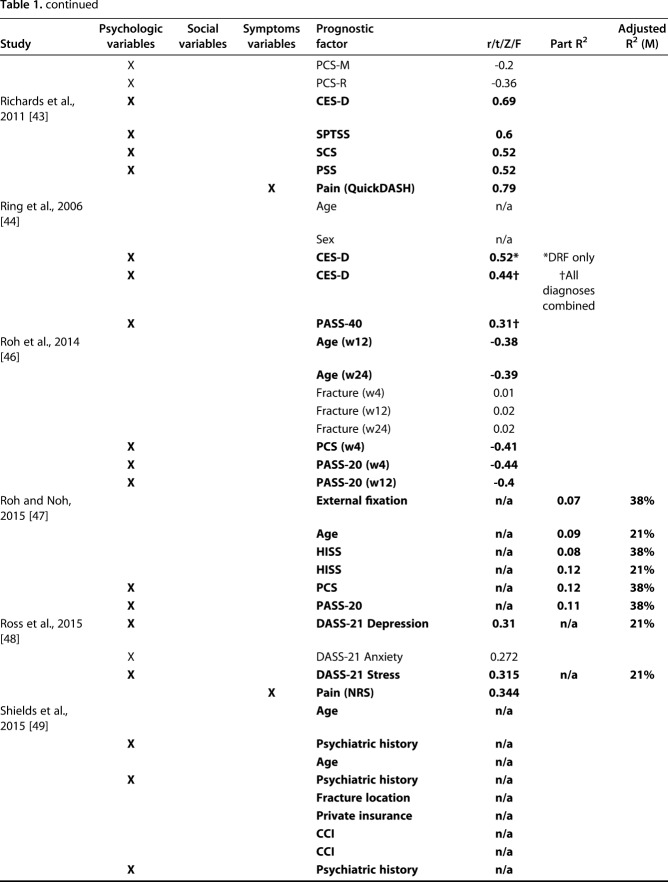
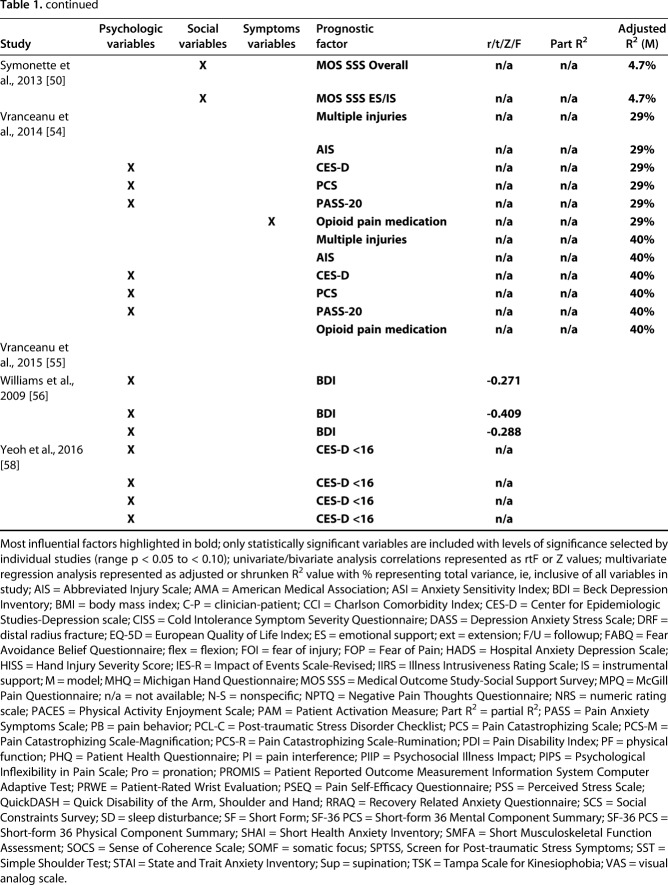
We independently extracted data and recorded information using an electronic database (Microsoft Excel Version 15.32; Microsoft Inc, Redmond, WA, USA). A definition of variables was used as a reference throughout the review process (Appendix, Supplemental Digital Content 2). Extracted information included the official publication date, level of evidence, study design, study population, trauma region, and outcome measures, scales, and metrics pertaining to the domains assessed (Table 1). The key disability-focused findings and clinical and/or research sequelae were recorded (Appendix, Supplemental Digital Content 3). The next stage involved assimilating key statistical data pertaining to factors associated with disability from the full publication including any linked supplementary files. We reported study populations involving traumatic and nontraumatic conditions with aggregated data on the combined cohort as such unless there were specific data on the relevant subpopulation with a trauma problem. Further documentation of key influential factors was performed, charting the outcome measure(s) used, relevant statistics, and clinical grading if available. Finally, we performed a distribution analysis of the total study set that cleared the screening phase.
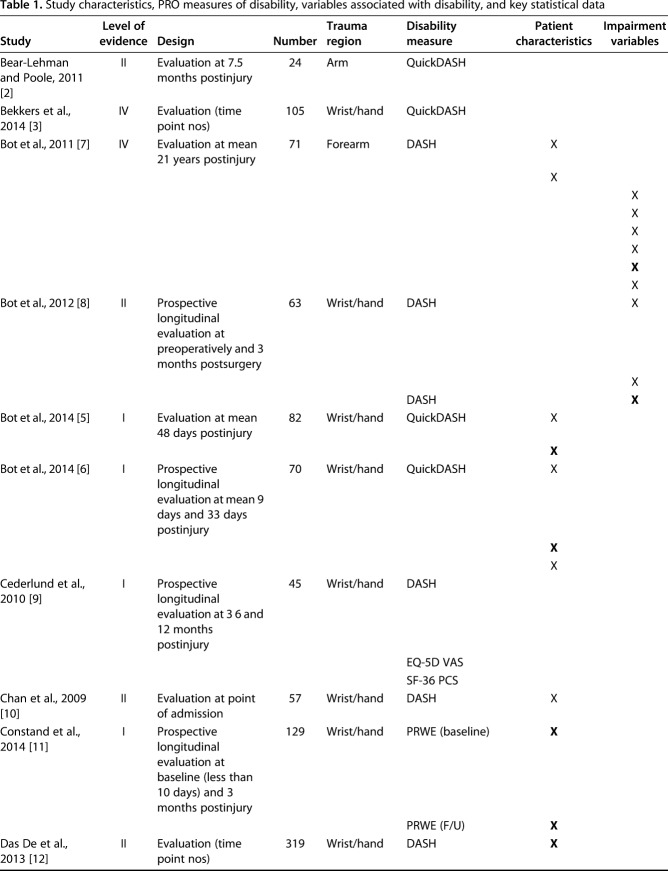
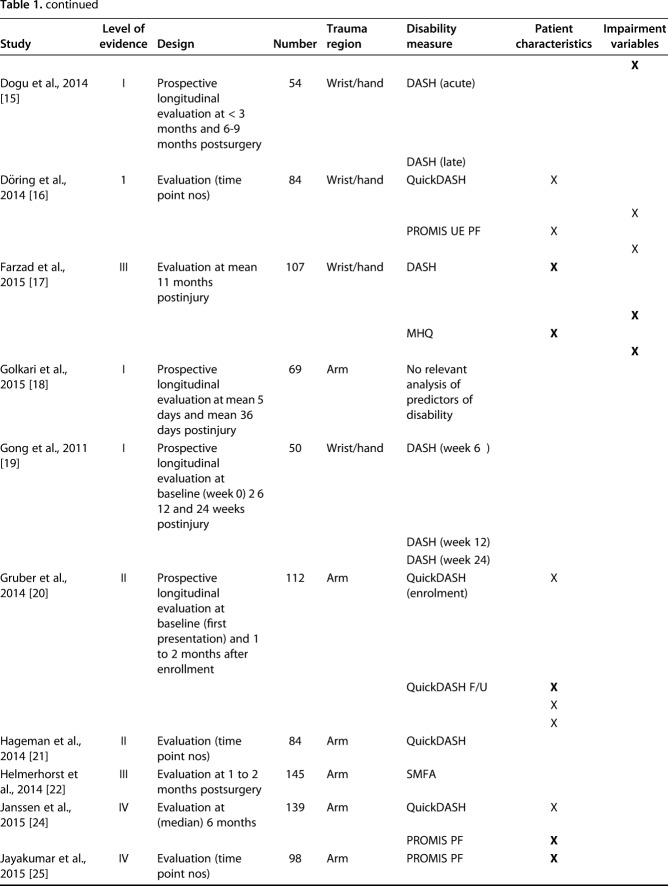
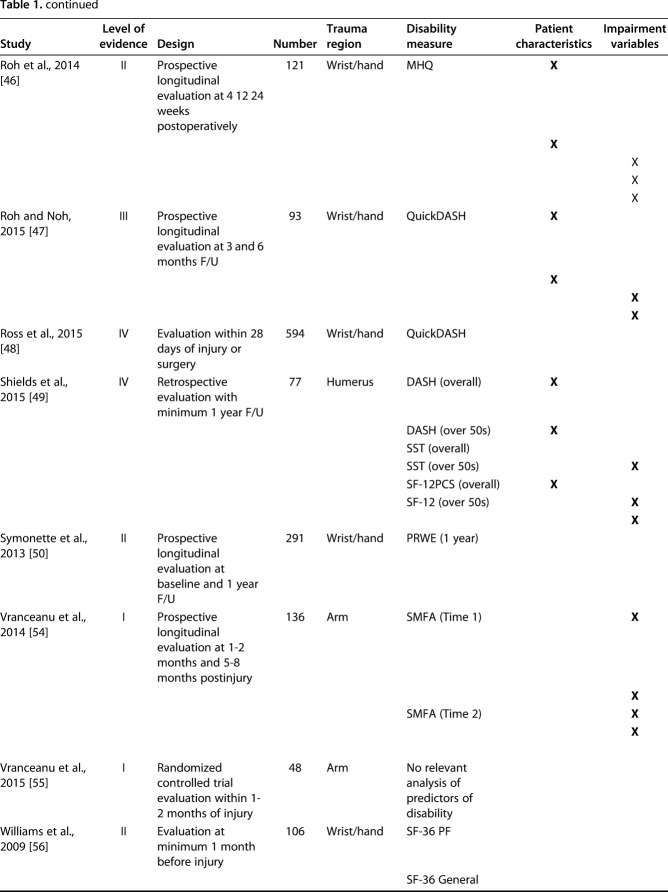
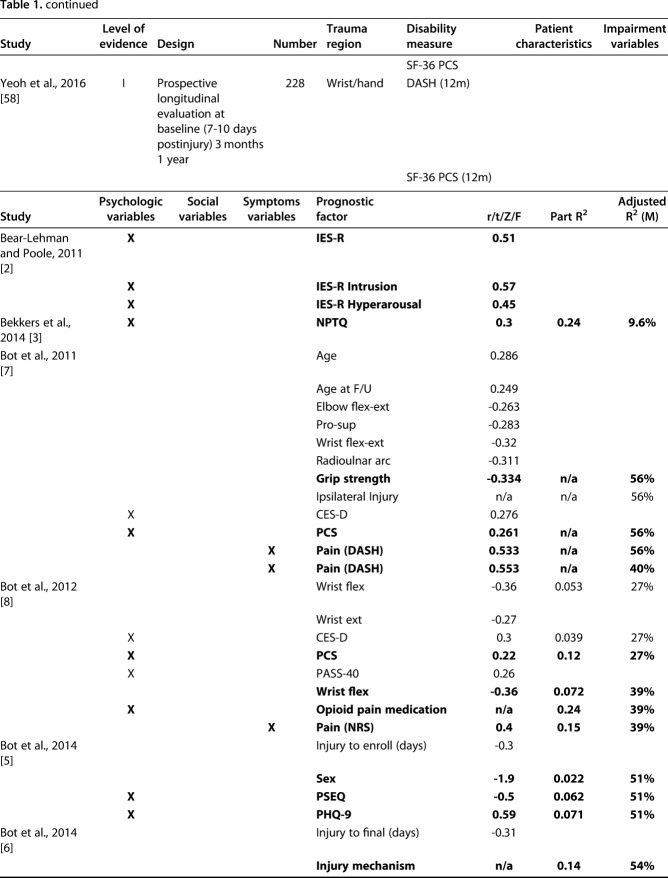
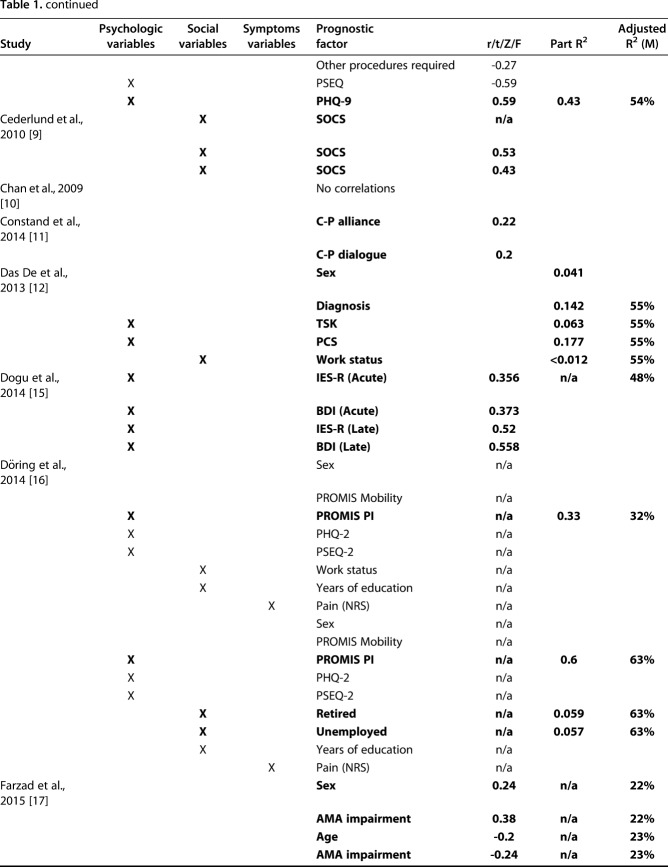
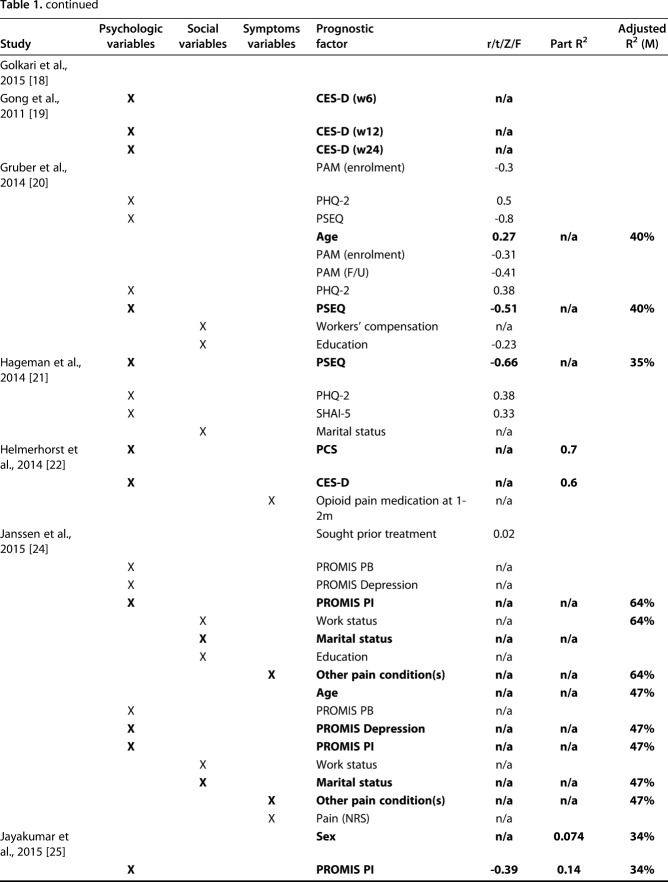
Table 1.
Study characteristics, PRO measures of disability, variables associated with disability, and key statistical data
Selection of Studies
The database search provided a total of 9339 citations and after adjusting for duplicates, 4385 remained. Of these, 1757 were excluded by criteria after title and abstract screening and a further assessment of eligibility through closer abstract and full-text review excluded 2544 articles. This resulted in 84 studies involving disability and associated factors related to any orthopaedic condition. Of these, 41 studies solely involved trauma conditions (n = 29 of 41 [71%]) or a combined cohort of trauma and nontrauma conditions (n = 12 of 41 [29%]) (Fig. 2).
Study Characteristics
Definition of Study Designs, Diagnoses, and Outcome Measures
Most studies were cross-sectional (n = 25 of 41 [61%]) with highly variable levels of evidence (Level I, n = 12 of 41 [29%]; Level II, n = 10 of 41 [24%]; Level III, n = five of 41 [12%]; Level IV, n = 14 of 41 [34%]) (Table 1). Cohort sizes ranged from five [42] to 839 [35]. “Wrist and hand” trauma was most frequently investigated (n = 21 of 41 [51%]) followed by injuries involving more than one upper limb region (n = 16 of 41 [39%]) and single studies involving each of the remaining areas (n = four of 41 [10%]; shoulder, humerus, elbow, and forearm). The most frequently used PROM for disability was the Quick Disabilities of the Arm, Shoulder and Hand (QuickDASH) (n = 17 of 41 [41%]) followed by the DASH (n = 16 of 41 [39%]) (Fig. 3). Participants included adults with a range of upper extremity conditions including injuries that ranged from soft tissue injuries to dislocations, subluxations, and fractures involving various regions of the arm treated with nonoperative and operative interventions.
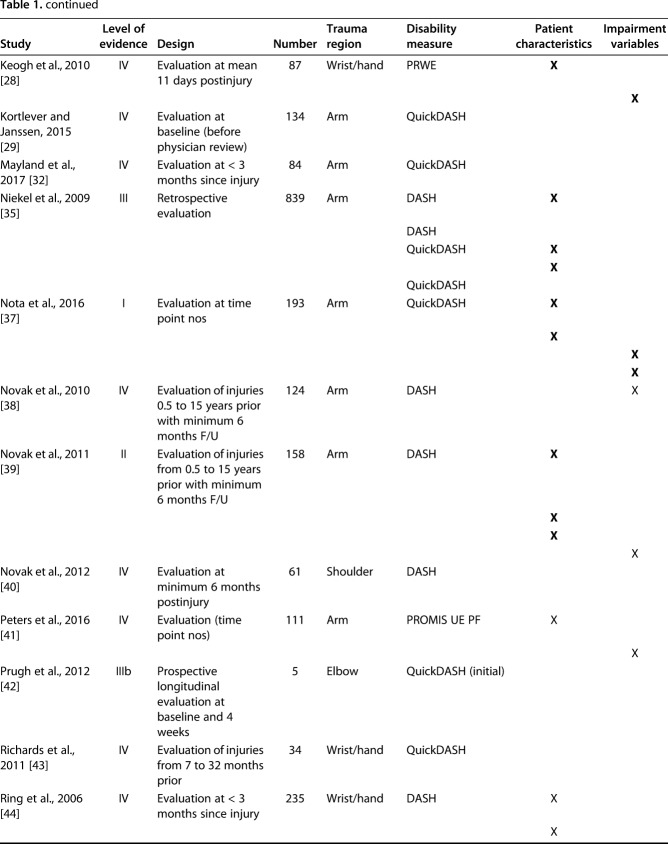
Fig. 3.
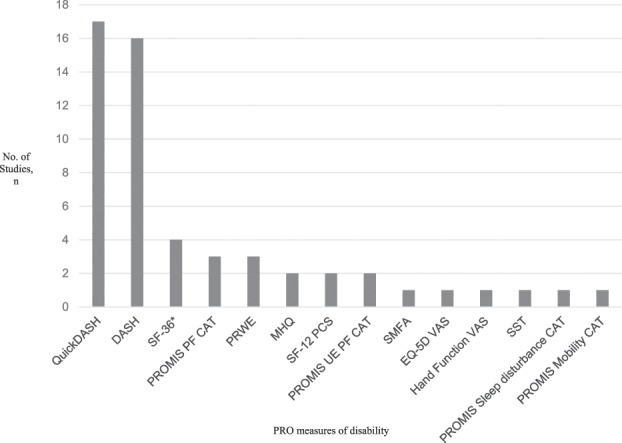
The distribution of PROMs used in the final inclusion study set is shown. QuickDASH = Quick Disabilities of the Arm, Shoulder and Hand; PROMIS = Patient Reported Outcome Measurement Information System; PF = Physical Function; CAT = Computer Adaptive Test; MHQ = Michigan Hand Questionnaire; PCS = Physical Component Summary Score; UE = upper extremity; SMFA = Short Musculoskeletal Functional Assessment; EQ-5D VAS = European Quality of Life Index; VAS = visual analog scale; SST = Simple Shoulder Test.
Quality Assessment
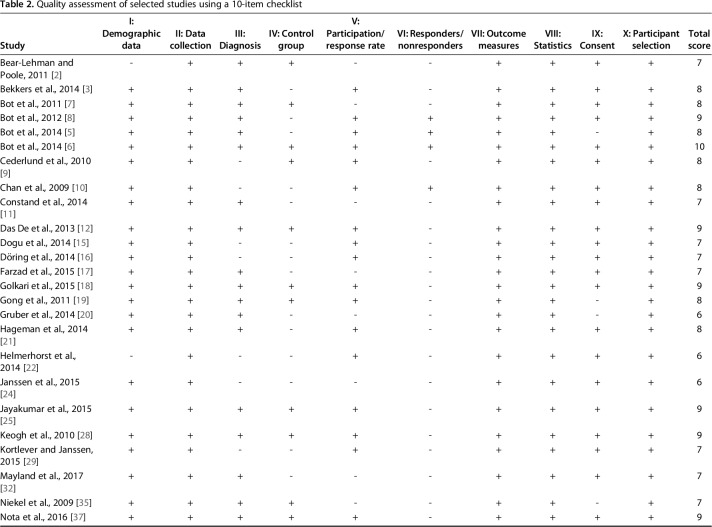
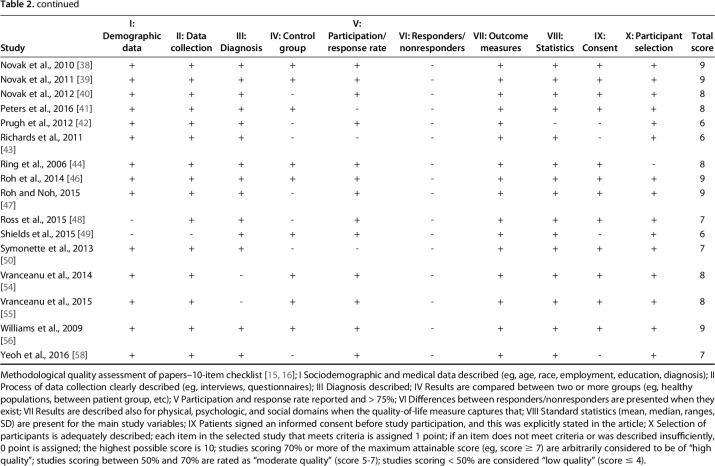
Of the 41 studies, 15% (n = 6) of studies had moderate quality and 85% (n = 35) had high quality (Table 2). All studies met the threshold total score of > 50% and were thus included in the subsequent strength of evidence evaluation.
Table 2.
Quality assessment of selected studies using a 10-item checklist
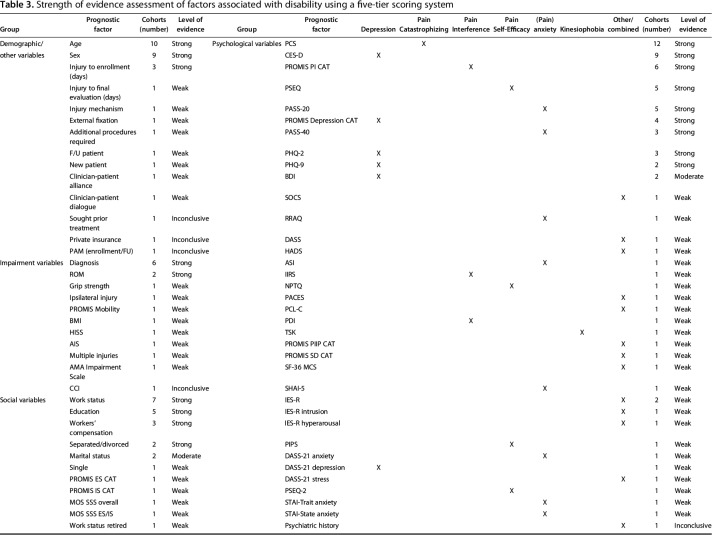
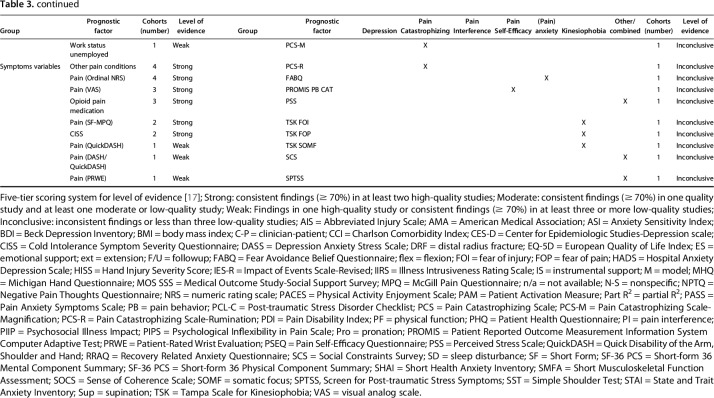
Overall Strength of Evidence
Heterogeneity of studies in terms of design, diagnoses, outcome measures utilized, and statistical analysis performed meant statistical pooling was not considered feasible or appropriate. A qualitative evaluation and best evidence synthesis was performed instead to summarize the strength of evidence for each variable (Table 3). Although there was strong evidence for a selection of psychologic, social, and symptomatic factors being associated with magnitude of disability (PROMs), a significant number of factors had weak or inconclusive findings. As expected, there were greater numbers of “strong” evidence classifications when interactions were assessed between prognostic variables and combined PROMs of disability.
Table 3.
Strength of evidence assessment of factors associated with disability using a five-tier scoring system
Other Methods
Strength of evidence for all prognostic variables associated with PROMs of disability was assessed using an established five-tier system that graded strength based on consistency of findings and quality of studies (Table 3) [1]. Positive findings from bivariate and multivariate analyses were utilized to determine the strength of evidence for interactions between variables and each PROM of disability as well as interactions between the variable and PROMs of disability combined. Statistical pooling was considered depending on the homogeneity of study populations, type of prognostic factors, and outcome measures. The overall level of consistency of factors associated with disability was based on observing statistically significant associations in multiple studies, considering the quality of these studies and strength of evidence assessment.
We analyzed studies clearing the screening phase (n = 2628) and calculated a percentage for outcome measurement categories represented within the articles and reported by year of publication (2000–2016). A starting year of 2000 was set to observe this trend because this was around the same time the WHO ICF was being introduced. During screening, we also observed unusual, conflicting, or inappropriate use of (1) terminology related to disability; and/or (2) outcome measures used to represent disability and its contributory factors. The authors agreed on classifying any relevant abstracts into these categories and documenting descriptive notes to inform a subclassification. The benchmarks were based on the WHO ICF definitions, which were used as a reference guide throughout this process, along with a classification of outcome measures into (1) objective, ie, clinician-based questionnaires; (2) subjective, ie, patient-reported outcome measures and scales; and (3) performance-based measures. None of the authors received any form of funding in relation to this work.
Results
Disability after upper extremity injury was most consistently associated with symptoms of depression (in 21 cohorts), pain catastrophizing (an exaggerated negative response to nociception in 13 cohorts), anxiety (negative cognitive, behavioral, and physiological response, with or without a relation to nociception [pain anxiety] in 11 cohorts), pain self-efficacy (confidence in the ability to cope despite pain in eight cohorts), and pain interference (the influence of pain in all aspects of life in seven cohorts) (Table 1). Other psychologic factors such as kinesiophobia (fear of movement), sense of coherence (a person’s capacity to cope in situations), nonadaptive pain thoughts, and stress after trauma also demonstrated associations with disability, but these were less consistent based on observations in fewer studies (Table 1), studies of poorer quality (Table 2), or factors that showed weaker strengths of evidence (Table 3).
Six of 14 studies that identified depression as a factor associated with the magnitude of disability also provided some form of clinical grading (range; minimal [19%-26%], mild [4%-17%], moderate [5%-17%], severe or major depression [6%-79%]) [15, 19, 22, 43, 56, 58]. Two of these studies reported patients with depressive symptoms (15% in one study, 29% in the other) and a diagnosis of posttraumatic stress disorder [43, 56]. Pain catastrophizing and pain are shown to be significant predictors of disability after distal radius fractures and both-bone fractures of the forearm in multivariable analysis [7, 8]. Pain intensity represented by the visual analog scale, ordinal numeric rating scale, pain-specific questionnaires, or subscales of patient-reported outcome instruments (eg, McGill Pain Questionnaire, Patient-Rated Wrist Evaluation [PRWE] pain subscale) demonstrated strong correlations with disability [7, 8, 28, 38, 39, 40, 43, 48]. Social factors associated with greater disability included lower education level [24], marital status (specifically being single [25], separated, divorced, or widowed [24, 37]), work/employment status (ie, being off work [24], unemployed [39], unemployed but able to work [16], unemployed and unable to work [37], retired [16]), and being involved in workers’ compensation or litigation claims [39] (Table 1). Constructs of social, emotional, and informational support were also found to be associated with disability in the longer term [37, 50]. Objective, clinician-based measures such as diagnosis, Hand Injury Severity Scoring System and American Medical Association impairment scale, and performance-based measures such as ROM (specifically wrist flexion after distal radius fractures) and grip strength were the only impairment-related variables shown to have an association with disability (Table 1). The strongest evidence was for diagnosis and ROM. Age and sex were the only consistent demographic factors influencing disability (n = 10 [24%] and n = 9 [22%], respectively). Specifically, being older [17, 20, 24, 35, 39, 46, 47, 49] and being female [5, 17, 25, 35, 54] were associated with greater disability (Table 1). A few longitudinal studies also identified disability itself at baseline or early postinjury as an influential factor of disability at a later stage [15]. In studies performing multivariable analysis with a PROM of disability as the response variable, various prognostic factors explained 10% to 63% of variance (Table 1).
We found a gradual increase in utilization of region or condition-specific PROMs and measures of psychologic and symptomatic factors from 2000 to 2016 (Fig. 4). Use of objective, clinician-based metrics and social factors remained relatively unchanged and use of generic health measures appeared to decline. Seventeen percent of studies (n = 454 of 2628) had cases of unclear, conflicting, or inappropriate terminology. For instance, terms such as functional disability, subjective disability, functional impairment, functional function, and subjective impairment were used without being clearly defined. None of these terms are specified in the WHO ICF, which provides a comprehensive definition of the terms disability and impairment. We accepted that many authors chose to use the terms QoL, function, and derivatives, including functional outcome, interchangeably with disability and so this was not considered an irregularity. Eleven percent of studies (n = 257 of 2628) involved misrepresentations of outcome measures related to disability. For example, one study described wrist accelerometry as a measure of disability when it is more specifically an automated, performance-based measure of impairment, similar to ROM and grip strength. Other instances included the use of PROMs as indicators of patient satisfaction and PROM scores to arbitrarily grade disability as mild, moderate, or severe without any scientific basis.
Fig. 4.
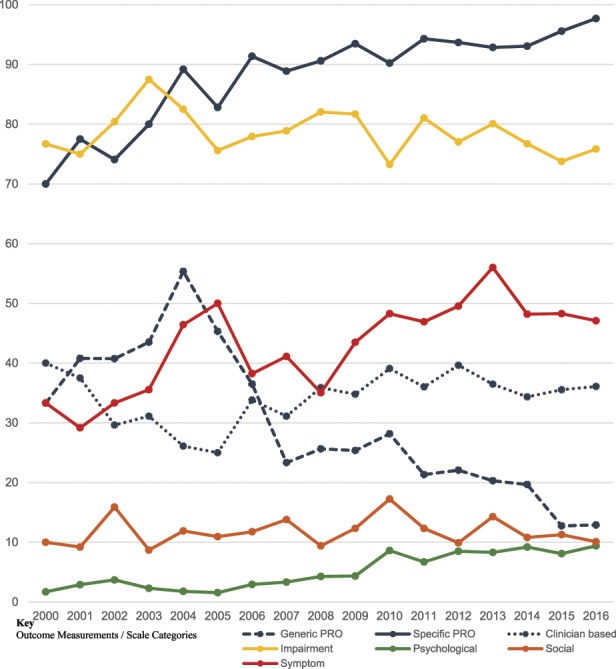
The annual percentage rate of outcome measurement categories is represented within all published orthopaedic upper extremity articles for year based on the systematic review search criteria (2000-2016).
Discussion
Defining factors associated with disability related to a health condition is integral to understanding the outcomes that matter to individuals and how we should consider their care. Although there is growing evidence for psychosocial factors being the key determinants of health after upper extremity injuries, there is lack of clarity regarding which psychosocial factors have the most consistent association with disability and how the language, conceptualization, and types of measures used to assess disability impact these associations in upper extremity injuries.
We conducted the first systematic review of all studies on upper extremity injury published until December 2016. We found that psychologic and social factors were more consistently associated with disability than factors related to impairment. We also observed a substantial number of irregularities in the use of outcome measurement tools and terminology related to disability despite clear guidelines provided by the WHO ICF framework.
This study has several limitations. First, during categorization of the outcome measures into psychologic, social, symptomatic, demographic, and impairment-related factors, it is conceivable that some measurements could fit into more than one of these categories. For example, emotional support (the perceived feelings of being cared for and being valued as a person) could be classed as a psychologic as well as a social factor. Although the constituents of these categories could be debated, a consensus was reached at the outset by our multidisciplinary team of authors and adhered to throughout the study. Second, a degree of selection bias may exist as a result of the broad scope of this review despite following a clear set of inclusion and exclusion criteria throughout the analysis. For instance, a proportion of studies may not have listed all their outcome measures in the abstract, leading to inadvertent exclusion. It was difficult to mitigate this with such a large study set. Third, although this study aimed to assess the association among a comprehensive range of factors with disability, it is dependent on the set of variables chosen by the investigators. It is possible that other determinants associated with disability were not captured and the group of factors selected in this study may not be exhaustive. Fourth, one must acknowledge that these conclusions are made on a broad range of studies with heterogeneous populations (two-thirds of studies involved trauma and nontraumatic conditions combined). Thus, we would recommend readers zone in on an area or factor of interest and consider the study characteristics, data, and populations to which the associations with disability are assigned. Finally, the generalizability of these findings could be questioned because most studies were conducted in US institutions. Cultural and societal differences between US populations and other parts of the world should be considered when interpreting findings.
Psychologic factors, specifically depression, pain catastrophizing, pain self-efficacy, pain interference, and pain anxiety, along with certain social factors (work, education, marital status) and pain intensity are consistently associated with the magnitude of disability. Impairment-related factors (such as diagnosis or ROM) are comparatively weak. Although psychologic factors impact disability prospectively even after controlling for impairment [33, 36], numerous studies indicate that a large amount of variance in disability remains unexplained. The contextual factors component of the WHO ICF, which is classified into environmental and personal factors, may account for some of this unexplained variance (Fig. 1) [57]. This could be tested by enlisting other forms of PROMs and evaluating their association with disability. For example, environmental factors include relationships and attitudes toward surrounding services, and personal factors include behavioral assets including confidence to cope. These could be quantified by patient experience ratings and patient activation measures, which aim to capture the knowledge, skills, and confidence an individual has in engaging with their own health and their healthcare providers.
Based on our findings, further studies should evaluate the potential impact of early assessment and treatment of psychosocial factors on recovery after upper extremity injury [15, 22, 56]. Interventions such as behavioral activation and cognitive-behavioral therapy (CBT) may counteract nonadaptive cognitions and behaviors, but are seldom used in orthopaedic patients. The single randomized controlled trial in this review found that a CBT-like skill-based intervention was feasible, acceptable, and effective in decreasing pain intensity and magnitude of disability [55]. Further clinical trials are required to assess the impact of mind-body skill-based coaching at different stages of recovery [18, 55]. Quality research in this area may not only provide further evidence to support treatment decision-making, but also a means of diminishing the stigma and shame that patients may experience during assessment of psychosocial factors. Notably, PROMs should only be used as guidance, not mandate, in screening patients and triggering therapies during the recovery trajectory to mitigate the risk of labeling patients with psychologic diagnoses and exposing vulnerabilities [46, 55].
This study also mapped the trends in the tools used to assess disability and inspected articles for variations in terminology describing aspects of disability. In the era of patient-centered care, it is not surprising that there is a relative increase in utilization of condition- and region-specific PROMs. A greater appreciation for psychologic factors may also be reflected by the gradual increase in measures of emotional health. The percentage of measures representing social factors, however, remained largely unchanged. An increasing recognition of the role played by social determinants on health may support the inclusion of a greater number of social factor variables in future work in this field such as nutritional status and housing. In terms of terminology related to disability and its components, and the outcome measures used to quantify them, one assumes there is sufficient understanding of terms before publishing scientific literature. The substantial proportion of abstracts exhibiting unclear, conflicting, and incorrect terminology in this study suggests otherwise. This observation was based on referencing terms against the WHO ICF, which provides a global standard for definitions related to disability and health. Although this framework is well established in healthcare research, it may be less familiar to the broader orthopaedic community given our findings [26, 53]. Disability reflects the interactions between impairment, activity limitations, and participation restrictions and contextual factors in relation to a health condition. It should be represented by PROMs of physical functioning at the level of tasks, broader acts, and roles [51]. Physical functioning represents a person’s capacity in certain situations and the ability to manage barriers to this functioning [57]. The term function is applied extremely liberally in clinical practice and research and often represented by a range of measures, often precluding a clear idea of what concept is being measured. Psychosocial factors and pain can be assessed using PROMs and ordinal or numeric rating scales, respectively. Impairment (pathophysiology) can be assessed using objective, clinician-based measures such as radiographic classification or performance-based measures such as grip strength. [51]. Orthopaedic institutions with global networks should consider standard setting for terms and tools related to disability after injuries. This may facilitate better comparisons between studies in this field. Much can be learned from extensive consensus-building work in the area of disability related to chronic pain [51]. A system of research has been endorsed where investigators are encouraged to assess (1) the capacity to physically function; (2) the impact of psychosocial, symptomatic, environmental, and personal stressors on this capacity; and (3) the ability of coping and adaptation to modify the relationship between capacity and actual performance [51]. Standard sets of validated patient-reported, clinician-based, and performance-based measures representing disability and its components are being developed to support such guidance [51].
Psychosocial factors are most consistently associated with the magnitude of disability after upper extremity injuries. Further studies should investigate the impact of early assessment and provision of interventions, eg, coping strategies, behavioral activation, CBT, and social support, during recovery on long-term PROMs. Intelligent comparison of disability outcomes in this field requires a level standardization in the tools to assess disability and the terminology used to communicate information related to disability. This should be a priority for orthopaedic institutions with networks capable of defining consensus-based standards and disseminating these recommendations internationally. This could be further consolidated at the policy level because the delivery of health care is becoming increasingly guided by patient-reported outcome data and measuring what matters to patients.
Footnotes
One of the authors (PJ) certifies that he received payments during the study period in the amount of less than USD 10,000 in personal fees as a consulting clinician from Johnson & Johnson, DePuy Synthes (New Brunswick, NJ, USA) outside the submitted work. One of the authors certifies that she (SL) received payments during the study period in the amount of less than USD 10,000 in personal fees as a consulting clinician/statistician from Pleuristem Inc (Tel Aviv, Israel) outside the submitted work. One of the authors (DR) certifies that he received payments in the amount of less than USD 10,000 in royalties from Skeletal Dynamics (Miami, FL, USA) and payments in the amount of less than USD 10,000 in personal fees from Wright Medical (Memphis, TN, USA), personal fees from Biomet (Warsaw, IN, USA), personal fees from Acumed (Hillsboro, OR, USA), personal fees from Illuminos (East Providence, RI, USA), personal fees as Deputy Editor for the Journal of Hand Surgery, personal fees as Deputy Editor for Clinical Orthopaedics and Related Research®, personal fees from universities and hospitals, and personal fees from lawyers outside the submitted work.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
This work was performed at The Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences, Oxford, UK.
References
- 1.Ariens GAM, van Mechelen Q, Bongers PM, Bouter LM. Physical risk factors for neck pain. Scand J Work Environ Health. 2000;26:7–19. [DOI] [PubMed] [Google Scholar]
- 2.Bear-Lehman J, Poole SE. The presence and impact of stress reactions on disability among patients with arm injury. J Hand Ther. 2011;24:89–94. [DOI] [PubMed] [Google Scholar]
- 3.Bekkers S, Becker SJE, Bossen JKJ, Mudgal CS, Ring D, Vranceanu AM. Relationships between pain misconceptions, disability, patient’s goals and interpretation of information from hand therapists. J Hand Ther. 2014;27:287–295. [DOI] [PubMed] [Google Scholar]
- 4.Bhandari M, Busse JW, Hanson BP, Leece P, Ayeni OR, Schemitsch EH. Psychological distress and quality of life after orthopedic trauma: an observational study. Can J Surg. 2008;51:15–22. [PMC free article] [PubMed] [Google Scholar]
- 5.Bot A, Bekkers S, Herndon J, Mudgal CS, Jupiter JB, Ring D. Determinants of disability after proximal interphalangeal joint sprain or dislocation. Psychosomatics. 2014;55:595–601. [DOI] [PubMed] [Google Scholar]
- 6.Bot AGJ, Bossen JKJ, Mudgal CS, Jupiter JB, Ring D. Determinants of disability after fingertip injuries. Psychosomatics. 2014;55:372–380. [DOI] [PubMed] [Google Scholar]
- 7.Bot AGJ, Doornberg JN, Lindenhovius ALC. Long-term outcomes of fractures of both bones of the forearm. J Bone Joint Surg Am. 2011;93:527–532. [DOI] [PubMed] [Google Scholar]
- 8.Bot AGJ, Mulders MAM, Fostvedt S. Determinants of grip strength in healthy subjects compared to that in patients recovering from a distal radius fracture. J Hand Surg. 2012;37:1874–1880. [DOI] [PubMed] [Google Scholar]
- 9.Cederlund RI, Ramel E, Rosberg H, Dahlin LB. Outcome and clinical changes in patients 3, 6, 12 months after a severe or major hand injury—can sense of coherence be an indicator for rehabilitation focus? BMC Musculoskelet Disord. 2010;11:286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan JCY, Ong JCY, Avalos G, Regan PJ, Mccann J, Groarke A, Kelly JL. Illness representations in patients with hand injury. J Plast Reconstr Aesthet Surg. 2009;62:927–932. [DOI] [PubMed] [Google Scholar]
- 11.Constand MK, Macdermid JC, Law M, Bello-Haas VD. Patient-centered care and distal radius fracture outcomes: a prospective cohort study analysis. J Hand Ther. 2014;27:177–184. [DOI] [PubMed] [Google Scholar]
- 12.Das De S, Vranceanu AM, Ring DC. Contribution of kinesophobia and catastrophic. J Bone Joint Surg Am. 2013;95:76–81. [DOI] [PubMed] [Google Scholar]
- 13.de Putter CE, Selles RW, Haagsma JA, Polinder S, Panneman MJM, Hovius SE, van Beeck EF. Health-related quality of life after upper extremity injuries and predictors for suboptimal outcome. Injury. 2014;45:1752–1728. [DOI] [PubMed] [Google Scholar]
- 14.de Putter CE, Selles RW, Polinder S, Panneman MJM, Hovius SER, van Beeck EF. Economic impact of hand and wrist injuries: health-care costs and productivity costs in a population-based study. J Bone Joint Surg Am. 2012;94:e56. [DOI] [PubMed] [Google Scholar]
- 15.Dogu B, Kuran B, Sirzai H. The relationship between hand function, depression, and the psychological impact of trauma in patients with traumatic hand injury. Int J Rehabil Res. 2014;37:105–109. [DOI] [PubMed] [Google Scholar]
- 16.Döring AC, Nota SPFT, Hageman MGJS, Ring DC. Measurement of upper extremity disability using the Patient-Reported Outcomes Measurement Information System. J Hand Surg. 2014;39:1160–1165. [DOI] [PubMed] [Google Scholar]
- 17.Farzad M, Asgari A, Dashab F, Layeghi F, Karimlou M, Hosseini SA, Rassafiani M. Does disability correlate with impairment after hand injury? Clin Orthop Relat Res. 2015;473:3470–3476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Golkari S, Teunis T, Ring D. Changes in depression, health anxiety, and pain catastrophizing between enrollment and 1 month after a radius fracture. Psychosomatics. 2015;56:652–657. [DOI] [PubMed] [Google Scholar]
- 19.Gong HS, Lee JO, Huh JK, Oh JH, Kim SH, Baek GH. Comparison of depressive symptoms during the early recovery period in patients with a distal radius fracture treated by volar plating and cast immobilisation. Injury. 2011;42:1266–1270. [DOI] [PubMed] [Google Scholar]
- 20.Gruber JS, Hageman M, Neuhaus V, Mudgal CS, Jupiter JB, Ring DC. Patient activation and disability in upper extremity illness. J Hand Surg. 2014;39:1378–1383.e3. [DOI] [PubMed] [Google Scholar]
- 21.Hageman M, Briet J, Oosterhoff T. The correlation of cognitive flexibility with pain intensity and magnitude of disability in upper extremity illness. J Hand Microsurg. 2014;6:59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Helmerhorst GTT, Vranceanu AM, Vrahas M, Smith M, Ring DC. Risk factors for continued opioid use one to two. J Bone Joint Surg Am. 2014;96:495–499. [DOI] [PubMed] [Google Scholar]
- 23.Hudak PL, Cole DC. Perspectives on prognosis of soft tissue musculoskeletal disorders. Int J Rehabil Res. 1998;21:29–40. [DOI] [PubMed] [Google Scholar]
- 24.Janssen S, ter Meulen D, Nota SPFT, Ring DC. Does verbal and nonverbal communication of pain correlate with disability? Psychosomatics. 2015;56:338–344. [DOI] [PubMed] [Google Scholar]
- 25.Jayakumar P, Overbeek CL, Ring DC. Relationship of age on enjoyment of physical activity in upper extremity illness. Hand. 2015;10:767–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jette AM. Toward a common language of disablement. J Gerontol A Biol Sci Med Sci. 2009;64:1165–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaske S, Lefering R, Trentzsch H, Driessen A, Bouillon B, Maegele M, Probst C. Quality of life two years after severe trauma: a single centre evaluation. Injury. 2014;45(Suppl 3):S100–105. [DOI] [PubMed] [Google Scholar]
- 28.Keogh E, Book K, Thomas J. Predicting pain and disability in patients with hand fractures: comparing pain anxiety, anxiety sensitivity and pain catastrophizing. Eur J Pain. 2010;14:446–451. [DOI] [PubMed] [Google Scholar]
- 29.Kortlever JTP, Janssen SJ. What is the most useful questionnaire for measurement of coping strategies in response to nociception? Clin Orthop Relat Res. 2015;473:3511–3518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kostanjsek N. Use of the International Classification of Functioning, Disability and Health (ICF) as a conceptual framework and common language for disability statistics and health information systems. BMC Public Health. 2011;11(Suppl 4):S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Levin PE, MacKenzie EJ, Bosse MJ. Improving outcomes: understanding the psychosocial aspects of the orthopaedic trauma patient. Instr Course Lect. 2014;63:39–48. [PubMed] [Google Scholar]
- 32.Mayland EC, Hay-Smith EJ, Treharne GJ. Recovery-related anxiety and disability following upper limb injury: the importance of context the importance of context. Disabil Rehabil. 2017;37:1753–1759. [DOI] [PubMed] [Google Scholar]
- 33.Menendez ME, Ring D. Disability versus impairment. J Hand Surg. 2014;39:1231. [DOI] [PubMed] [Google Scholar]
- 34.Moher D, Liberati A, Tetzlaff J. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Niekel MC, Lindenhovius ALC, Watson JB. Correlation of DASH and QuickDASH with measures of psychological distress. J Hand Surg. 2009;34:1499–1505. [DOI] [PubMed] [Google Scholar]
- 36.Nota SPFT, Bot AGJ, Ring D. Disability and depression after orthopaedic trauma. Injury. 2015;46:207–212. [DOI] [PubMed] [Google Scholar]
- 37.Nota SPFT, Spit SA, Oosterhoff TCH, Hageman MGJS, Ring DC, Vranceanu AM. Is social support associated with upper extremity disability? Clin Orthop Relat Res. 2016;474:1830–1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Novak C, Anastakis D, Beaton D. Relationships among pain disability, pain intensity, illness intrusiveness and upper extremity disability in patients with traumatic peripheral nerve injury. J Hand Surg Am. 2010;35:1633–1639. [DOI] [PubMed] [Google Scholar]
- 39.Novak CB, Anastakis DJ, Beaton DE. Biomedical and psychosocial factors associated with disability after peripheral nerve injury. J Bone Joint Surg Am. 2011;93:929–936. [DOI] [PubMed] [Google Scholar]
- 40.Novak CB, Anastakis DJ, Beaton DE. Cold intolerance after brachial plexus nerve injury. Hand. 2012;7:66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peters R, Menendez M, Mellema J, Ring D, Vranceanu AM. Sleep disturbance and upper-extremity disability. Arch Bone Jt Surg. 2016;4:35–40. [PMC free article] [PubMed] [Google Scholar]
- 42.Prugh J, Zeppieri G, George SZ. Impact of psychosocial factors, pain, and functional limitations on throwing athletes who return to sport following elbow injuries: a case series. Physiother Theory Pract. 2012;28:633–640. [DOI] [PubMed] [Google Scholar]
- 43.Richards T, Garvert DW, McDade E. Chronic psychological and functional sequelae after emergent hand surgery. J Hand Surg Am. 2011;36:1663–1668. [DOI] [PubMed] [Google Scholar]
- 44.Ring D, Kadzielski J, Fabian L. Self-reported upper extremity health status correlates with depression. J Bone Joint Surg Am. 2006;88:1983–1988. [DOI] [PubMed] [Google Scholar]
- 45.Roh YH, Kim KW, Paik N. How much are upper or lower extremity disabilities associated with general health status in the elderly? Clin Orthop Relat Res. 2012;470:3246–3252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Roh YH, Lee BK, Noh JH, Oh JH, Gong HS, Baek GH. Effect of anxiety and catastrophic pain ideation on early recovery after surgery for distal radius fractures. J Hand Surg. 2014;39:2258–2264.e2. [DOI] [PubMed] [Google Scholar]
- 47.Roh YH, Noh JH. To what degree do pain-coping strategies affect joint stiffness and functional outcomes in patients with hand fractures? Clin Orthop Relat Res. 2015;473:3484–3490. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 48.Ross C, Juraskova I, Lee H, Parkitny L, Stanton TR, Moseley GL, McCauley JH. Psychological distress mediates the relationship between pain and disability in hand or wrist fractures. J Pain. 2015;16:836–843. [DOI] [PubMed] [Google Scholar]
- 49.Shields E, Sundem L, Childs S, Maceroli M, Humphrey C, Ketz J, Gorczyca JT. Factors predicting patient-reported functional outcome scores after humeral shaft fractures. Injury. 2015;46:693–698. [DOI] [PubMed] [Google Scholar]
- 50.Symonette CJ, Macdermid J, Grewal R. Social support contributes to outcomes following distal radius fractures. Rehabil Res Pract. 2013;1:867250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Taylor AM, Phillips K, Patel KV, Turk DC, Dworkin RH, Beaton D, Witter J. Assessment of physical function and participation in chronic pain clinical trials: IMMPACT/OMERACT recommendations. Pain. 2016;157:1836–1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.van der Windt D, van der Heijden G. Systematic review of prognostic cohort studies on shoulder disorders. Pain. 2004;109:420–431. [DOI] [PubMed] [Google Scholar]
- 53.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. [DOI] [PubMed] [Google Scholar]
- 54.Vranceanu AM, Bachoura A, Weening A, Vrahas M, Smith RM, Ring D. Psychological factors predict disability and pain intensity after skeletal trauma. J Bone Joint Surg Am. 2014;96:e20. [DOI] [PubMed] [Google Scholar]
- 55.Vranceanu AM, Hageman M, Strooker J, Vrahas M, Ring D. A preliminary RCT of a mind body skills based intervention addressing mood and coping strategies in patients with acute orthopaedic trauma. Injury. 2015;46:552–557. [DOI] [PubMed] [Google Scholar]
- 56.Williams AE, Newman JT, Ozer K, Juarros A, Morgan SJ, Smith WR. Posttraumatic stress disorder and depression negatively impact general health status after hand injury. J Hand Surg Am. 2009;34:515–522. [DOI] [PubMed] [Google Scholar]
- 57.World Health Organization (Geneva) 2013. World Health Organization. How to use the ICF: A Practical Manual for Using the International Classification of Functioning. Available at: http://www.who.int/classifications/icf/en/. Accessed October 11, 2017.
- 58.Yeoh JC, Pike JM, Slobogean GP, Brien PJO, Broekhuyse HM, Lefaivre KA. Role of depression in outcomes of low-energy distal radius fractures in patients older than 55 years. J Orthop Trauma. 2016;30:228–233. [DOI] [PubMed] [Google Scholar]