Abstract
Background
In a typical osteoarthritic knee with varus deformity, distal femoral resection based off the worn medial femoral condyle may result in an elevated joint line. In a setting of fixed flexion contracture, the surgeon may choose to resect additional distal femur to obtain extension, thus purposefully raising the joint line. However, the biomechanical effect of raising the joint line is not well recognized.
Questions/purposes
(1) What is the effect of the level of the medial joint line (restored versus raised) on coronal plane stability of a TKA? (2) Does coronal alignment technique (mechanical axis versus kinematic technique) affect coronal plane stability of the knee? (3) Can the effect of medial joint-line elevation on coronal plane laxity be predicted by an analytical model?
Methods
A TKA prosthesis was implanted in 10 fresh frozen nonarthritic cadaveric knees with restoration of the medial joint line at its original level (TKA0). Coronal plane stability was measured at 0°, 30°, 60°, 90°, and 120° flexion using a navigation system while applying an instrumented 9.8-Nm varus and valgus force moment. The joint line then was raised in two steps by recutting the distal and posterior femur by an extra 2 mm (TKA2) and 4 mm (TKA4), downsizing the femoral component and, respectively, adding a 2- and a 4-mm thicker insert. This was done with meticulous protection of the ligaments to avoid damage. Second, a simplified two-dimensional analytical model of the superficial medial collateral ligament (MCL) length based on a single flexion-extension axis was developed. The effect of raising the joint line on the length of the superficial MCL was simulated.
Results
Despite that at 0° (2.2° ± 1.5° versus 2.3° ± 1.1° versus 2.5° ± 1.1°; p = 0.85) and 90° (7.5° ± 1.9° versus 9.0° ± 3.1° versus 9.0° ± 3.5°; p = 0.66), there was no difference in coronal plane laxity between the TKA0, TKA2, and TKA4 positions, increased laxity at 30° (4.8° ± 1.9° versus 7.9° ± 2.3° versus 10.2° ± 2.0°; p < 0.001) and 60° (5.7° ± 2.7° versus 8.8° ± 2.9° versus 11.3° ± 2.9°; p < 0.001) was observed when the medial joint line was raised 2 and 4 mm. At 30°, this corresponds to an average increase of 64% (3.1°; p < 0.01) in mid-flexion laxity with a 2-mm raised joint line and a 111% (5.4°; p < 0.01) increase with a 4-mm raised joint line compared with the 9-mm baseline resection. No differences in coronal alignment were found between the knees implanted with kinematic alignment versus mechanical alignment at any flexion angle. The analytical model was consistent with the cadaveric findings and showed lengthening of the superficial MCL in mid-flexion.
Conclusions
Despite a well-balanced knee in full extension and at 90° flexion, increased mid-flexion laxity in the coronal plane was evident in the specimens where the joint line was raised.
Clinical Relevance
When recutting the distal and posterior femur and downsizing the femoral component, surgeons should be aware that this action might increase the laxity in mid-flexion, even if the knee is stable at 0° and 90°.
Introduction
Joint stability is one of the primary components that determines a successful functional outcome after TKA. Instability has been identified as one of the major causes for early revision after TKA [36] and one under the direct control of the surgeon performing the procedure.
In contrast to alignment, joint stability remains a difficult parameter to quantify objectively. In most cases, joint stability is qualitatively assessed intraoperatively by the surgeon by manual varus and valgus and AP stress testing at 0° and 90°. The stability in the mid-flexion range frequently is not taken into account. During most activities of daily living, however, the knee is not only loaded near full extension but also in mid-flexion [29, 30], so stability throughout the mid-flexion range also should be considered during intraoperative testing. Failure to reproduce the required stability in the mid-flexion range can result in pain, an unstable feeling while walking, giving way, persistent synovitis, and even recurrent hemarthrosis [36]. During revision TKA, there is a tendency to raise the joint line owing to distal femoral bone loss. In the primary setting, the joint line also is frequently raised [6, 10, 28, 38]. This is partly the result of the surgical instrumentation of the procedure, which uses the worn distal femur as a reference. Failure to compensate for distal femoral bone loss will automatically result in a raised joint line. In addition, in the case of a fixed flexion contracture, resection of additional distal femoral bone is advocated by some surgeons [2, 25], which has been proven to increase maximal knee extension [7]. However, it is important to realize that a flexion contracture is not the consequence of distal femoral overgrowth. As a result, correcting the capsular-ligamentous contractures causing the extension deficit by additional bone resection might introduce new problems [7].
This link between the level of the joint line and coronal plane stability of the joint has been observed in previous studies, although the rationale for why joint line elevation would lead to mid-flexion instability remains unclear [7, 32].
We therefore asked: (1) What is the effect of the level of the medial joint line (restored versus raised) on coronal plane stability of a TKA? (2) Does coronal alignment technique (mechanical versus kinematic alignment affect coronal plane stability of the knee? (3) Can the effect of joint line elevation on coronal plane laxity be predicted by an analytical model?
Materials and Methods
The study protocol was approved by the local ethics committee.
Five fresh frozen full-body specimens (10 knees) were obtained by the human body donation program of the University of Leuven. There were three male and two female human donors between 55 and 85 years old at the time of death (Table 1). The specimens were stored at -18° C before the experiment.
Table 1.
Demographic variables of the specimens
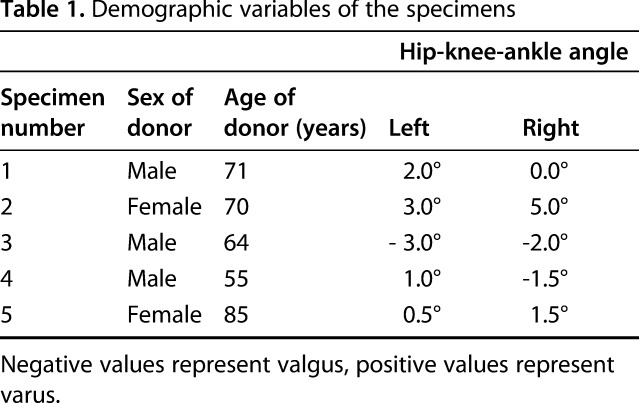
The full-body specimens were randomized to have the prosthesis implanted with mechanical alignment on one side and with kinematic alignment on the other. An online tool (Research Randomizer; https://www.randomizer.org) was used to perform randomization.
Before testing, the specimens were thawed for 48 hours at a room temperature of 20° C. Wet towels and water spraying prevented drying of the specimen throughout the experiment. Each knee (n = 10) was carefully checked for abnormalities during exposure, and a high-resolution photograph of the joint surfaces was taken. Exclusion criteria were previous surgery on the knee, abnormal AP or mediolateral ligamentous laxity, varus or valgus alignment greater than 6° as measured on the mechanical axis, or osteoarthritis (full thickness cartilage loss greater than 3 cm2 or the presence of osteophytes). These criteria were selected based on our intent to have as few outliers as possible in a limited number of cadaver knees and to minimize additional variables. No specimen had to be excluded.
An anterior midline incision was made followed by a standard subvastus arthrotomy. Two pins for the navigation frames were placed in the distal femur and proximal tibia, respectively, according to the manufacturer’s recommendations (BRAINLAB, Feldkirchen, Germany). The position of the femoral pins was chosen so that interference with closure of the joint capsule and with the extensor mechanism was avoided. Bony landmarks and joint surfaces were digitized with an optical localizer according to the manufacturer’s instructions (BRAINLAB). Resection of the anterior horn of the medial and lateral meniscus was necessary to reach the joint surfaces. The knee capsule was anatomically closed after performing the TKA. None of the specimens had a fixed flexion contracture greater than 10° as measured with the navigation software.
The reference planes as defined by the navigation software were: (1) coronal plane of the femur as the plane consisting of the center of the hip and the center of the two femoral condyles; (2) sagittal plane of the femur was perpendicular to the coronal plane, crossing the center of the knee; and (3) the axial plane of the femur was perpendicular to the two previous planes. The mechanical axis of the femur was defined as an axis crossing the center of the knee and the center of the hip and the mechanical axis of the tibia was defined as an axis running from the center of the proximal tibia to the center of the talus. The coronal plane of the tibia was defined by the medial and lateral points of intersection of the coronal plane of the femur with the proximal tibia in extension and the center of the talus. Any varus or valgus force applied was in the coronal plane of the tibia and directed perpendicular to the mechanical axis of the tibia.
At this stage, the natural joint laxity was measured by applying an instrumented varus and valgus stress moment at full extension, 30°, 60°, 90°, and 120° flexion. This was done in a standardized way by applying a 40-N pulling force moment measured by a digital force sensor connected to a stainless steel, threaded hook that was inserted through the anterior tibia 25 cm distal to the joint line [8]. This resulted in a standardized 9.8-Nm valgus or varus torque force. During the varus and valgus testing, rotation of the lower limb was prevented by applying counterforce on the femoral pins. Joint laxity was expressed as the sum of the maximum varus and valgus deviations measured under the applied stress.
Next, a posterior stabilized single-radius TKA prosthesis (Unity KneeTM; Corin Ltd, Cirencester, UK) was implanted using the navigation system. In all knees, the target for the medial distal and posterior medial femoral resection was 9 mm, because this equaled the implant thickness. As such, the medial joint line level was restored at its original level (TKA0 position).
The full-body specimens were randomized to have the TKA prosthesis implanted with neutral mechanical alignment on one side and with kinematic alignment principles on the other, both with the use of computer navigation. Mechanical alignment (five knees) was performed with a 0°-mechanical axis in coronal alignment as the target. This was done by a distal femoral cut and a proximal tibial cut perpendicular to the mechanical axis (Fig. 1A). In the axial plane, the femoral component was positioned in 3° external rotation relative to the posterior condylar line.
Fig. 1A-B.
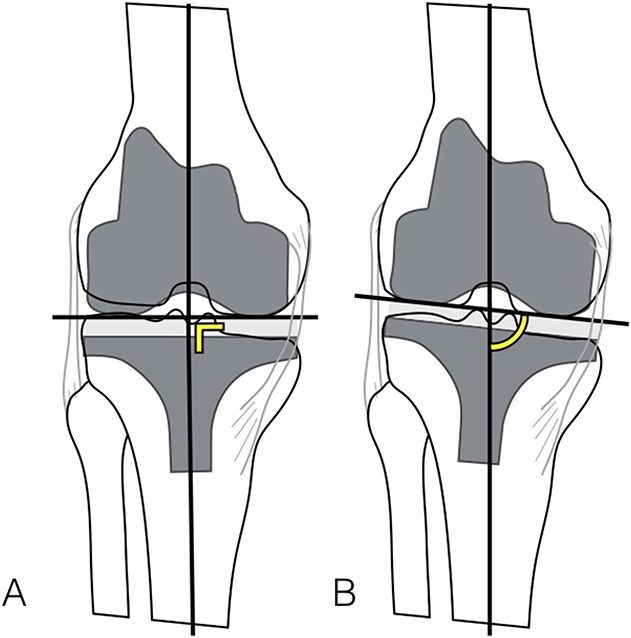
All TKA prostheses were implanted with restoration of the medial joint line. (A) In five knees the joint line was aligned perpendicular to the mechanical axis (mechanical alignment). (B) In the five other knees, the lateral joint line also was restored at its original level (kinematic alignment), thereby restoring the slight obliquity of the natural joint line. Yellow angle = perpendicular alignment; yellow arc = anatomic alignment.
Kinematic alignment (five knees) was performed by making the distal femoral and proximal tibial cuts parallel to the original distal femoral and proximal tibial joint surface, respectively. By doing this, the natural joint line obliquity was restored (Fig. 1B). In the axial plane, the femoral component was positioned parallel to the posterior condyles with no external rotation.
All femoral and tibial cuts were performed and verified with the navigation system. Adjustments were made when a deviation greater than 1° from the planning was measured in any plane. No soft tissue releases had to be performed. Soft tissue structures were meticulously protected with retractors during recutting. After recutting, ligament integrity was rechecked with the navigation software.
After closure of the knee capsule, the joint laxity measurements were repeated as described previously, with the most-stable trial components as assessed by navigation in place.
Next, the trial components were removed and 2 mm extra bone was removed from the distal and posterior femur with the use of the navigation software (TKA2 position). The knee stability in flexion and extension was maintained by using a 2-mm thicker polyethylene component. After closure of the knee capsule, the joint laxity measurements were repeated, as described previously, with the trial components in place. If stability of the trial component was insufficient, a definite component was cemented in place with the use of a polyester resin. This allowed stable fixation of the components and did not cause bone loss during removal of the component.
Next, an additional 2 mm (therefore 4 mm in total) of bone was removed from the distal and posterior femur with the use of the navigation system (TKA4 position). Knee stability in flexion and extension was again maintained by using a 2-mm thicker polyethylene component. After closure of the knee capsule, the joint laxity measurements were repeated, as described previously, with the trial components in place. Again, if the stability of the trial component was insufficient, a definitive component was cemented in place.
Development of the Analytical Model
Stability on the medial side of the knee primarily is provided by the superficial medial collateral ligament (MCL). Tightness and laxity of this ligament therefore directly relates to joint laxity in the coronal plane.
To predict the effect of medial joint line level changes on isometry of the superficial MCL, a simple two-dimensional analytical model was created. For this model, three basic assumptions were made. The first assumption is that the superficial MCL acts as an isometric ligament, meaning that the change in length of its fibers during ROM is minimal. The second assumption is that from a morphologic point of view, the shape of the posterior femoral condyles can be described as a circle. The third assumption is that the knee flexes and extends around a fixed axis of rotation, located at the center of these circular condyles.
In terms of the first assumption, it generally is accepted that a ligament can be considered isometric if the strain in the flexion arc remains less than 2% [43]. There are much data to support this statement. Using three-dimensional (3-D) digital image correlation, Luyckx et al. [31] showed that the central part of the superficial MCL was almost perfectly isometric between 15° and 90°, showing less than 0.3% strain. During the entire ROM, the maximum change of length of the whole superficial MCL was still minimal, averaging 1.7%. These data are consistent with the work of others [13, 43]. Victor et al. [43] reported a change in length of the proximal superficial MCL of 1 mm between 0° and 90° knee flexion. Ghosh et al. [13] found an average of 2 mm change in length between 0° and 110°. To be able to maintain its isometry throughout the ROM, the femoral insertion site of the superficial MCL coincides with the flexion and extension axis of the knee [11, 19, 45]. If this were not the case, elongation or slackening would occur during the flexion arc [11]. As the superficial MCL is the primary stabilizer against valgus stress, the concept of its isometry is crucial for knee stability as it reflects the ability of the ligament to stabilize the knee during the entire ROM [14, 15, 43].
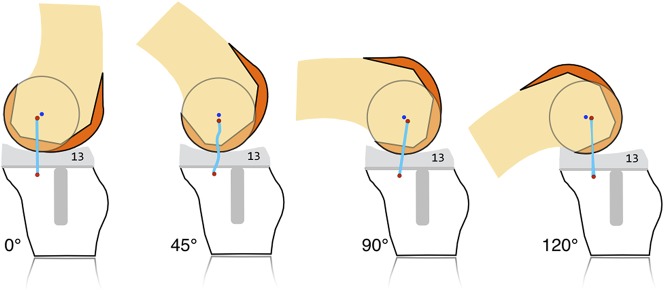
The second assumption is that from a morphologic point of view, the shape of the posterior femoral condyles can be described as a circle. This dates to 1836 when the Weber brothers were the first to describe the shape of the posterior condyles as a circle [46]. There are numerous more-recent studies showing that with the use of sophisticated 3-D imaging techniques, the shape of the femoral condyles can be described by best-fitting a circle, sphere, or cylinder in the posterior medial and lateral condyle (Fig. 2) [5, 8, 9, 19, 20]. Achieving the best fit possible to the articular surface in the posterior condyles corresponds to a flexion range of 10° to 160° [9, 20, 46].
Fig. 2A-C.
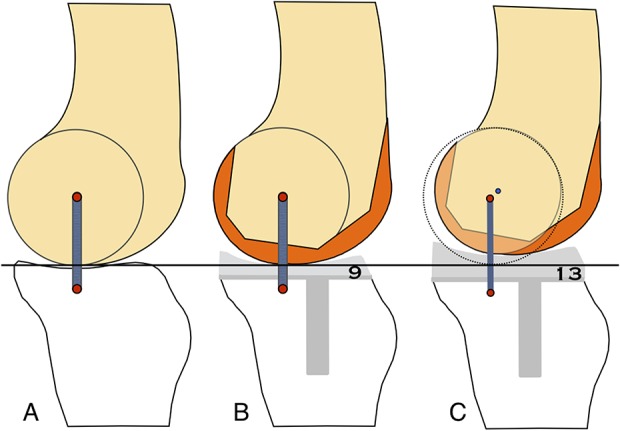
The schematics show the medial side of the knee in the sagittal plane. The femoral condyle is depicted as an “isometric” circle. The red dots indicate the femoral and proximal tibial insertion site of the superficial MCL. (A) On the femoral side, the insertion site of the superficial MCL coincides with the flexion and extension axis. (B) Restoration of the distal and posterior joint line after a single radius TKA reproduces the same flexion-extension axis. A 9-mm insert is used in the example. (C) The joint line is raised by using a 4-mm smaller femoral component in a 4-mm proximal position and a 4-mm thicker polyethylene insert (13 mm). The circle depicts the original level of the joint line. This causes a shift of the center of rotation to proximal and anterior (blue dot). This center no longer coincides with the femoral insertion site of the superficial MCL.
The third assumption is that the knee flexes and extends around a fixed axis of rotation, located at the center of these circular condyles. From a kinematic point of view, the knee historically was believed to rotate around a variable flexion and extension axis. It was referred to as a multiradius curve with an “instant center of rotation”, a theory that has been supported for almost 100 years [3, 12, 39, 44]. The problem created here was attributable to looking at a circle off-axis. A circle that is viewed along a line other than its axis will appear as an ellipse, thus leading to the conclusion of a multiradius curve [8]. Kinematic studies have shown that the knee flexes with a fixed axis of rotation [5, 19].
Regarding AP movement in the medial compartment, kinematic studies and in vivo weightbearing MRI studies have shown that in contrast to the passive situation, there is limited translation between 0° and 120° knee flexion [8, 16, 26, 27, 41, 42]. External rotation of the tibia during flexion allows the knee to function almost as a uniaxial hinge [16]. Therefore, kinematics of the medial femoral condyle can be described by a single and fixed center of rotation in the sagittal plane between 0o and 120° knee flexion.
Using a surface-derived approach and 3-D imaging, Eckhoff et al. [8] and Howell et al. [20] showed that the flexion and extension axis of the knee is fixed and passes through the center of a best-fit circle or cylinder in the posterior condyles. This assertion makes intuitive sense, as the axis is equidistant from the articular surface of the femur as it contacts the tibia from 15° to 115° flexion [9]. If the flexion and extension axis of the knee lies at some other location, the surfaces either would be pushed together or apart at various points in the flexion arc. Furthermore, stretching and contracting of the ligaments must occur to a greater extent the farther the flexion axis lies from the point equidistant from the surface.
Previous studies have shown the medial side of the knee as a relatively stable side with little tibiofemoral translation in the sagittal plane [26, 41]. Based on this knowledge, a simplified sagittal model of the knee, representing the section of the condyle as a circle (Fig. 2A), was created. Based on kinematic studies showing virtually no translation of the medial femoral condyle during the flexion arc between 0° and 90°, a single center of rotation in the sagittal plane can be accepted [8, 41, 42]. This means that we can assume that strain and tension in the superficial MCL will be identical after a single-radius TKA if a prosthesis with exactly the same surface geometry and size as the native knee is used. This will restore the center of rotation of the knee at its original spot (Fig. 2B). The experimental setting of TKA4 was modeled by fitting a 4-mm smaller femoral component with a 4-mm more-proximal position on the same knee. Stability was maintained by using a 4-mm thicker insert. As such, the joint line was raised by 4 mm (Fig. 2C), and consequently, a new center of rotation will be defined (the blue dot). With the assumption of a single functional flexion axis in the medial compartment, the effect of this joint line elevation can be calculated.
Statistical Analysis
An a priori power analysis with an α level of 0.05 showed a power of 0.85 to detect a difference of 3° in coronal plane stability between the mechanically and anatomically aligned TKAs and a power of 0.98 to detect a difference of 3° in coronal plane stability among the TKA0, TKA2, and TKA4 positions. All groups were compared using the Kruskal-Wallis test for comparison of more than two groups. Pairwise comparison was performed using the Wilcoxon rank-sum test. Probability values less than 0.05 are considered significant. All analyses were performed using JMP software Version 11.2 for Mac of the SAS System (SAS Institute Inc, Cary, NC, USA).
Results
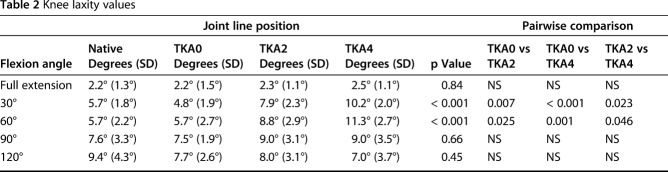
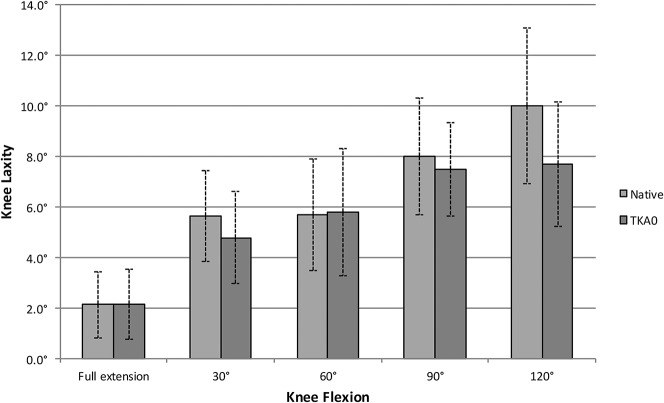
No differences, with the numbers available, were observed in coronal plane laxity between the native knee and the TKA performed with restoration of the medial joint line (TKA0) (Table 2). In both cases, mean coronal plane laxity generally increased as the knee went from extension to flexion (at 0°: 2.2° ± 1.3° versus 2.2° ± 1.5°; at 30°: 5.7° ± 1.8° versus 4.8° ± 1.9°; at 60°: 5.7° ± 2.2° versus 5.7° ± 2.7°; at 90° 7.6° ± 3.3° versus 7.5° ± 1.9°; at 120°: 9.4° ± 4.3° versus 7.7° ± 2.6°) (Fig. 3). This increase in laxity with flexion was significant with a probability less than 0.05 for all positions except for the 30° versus 60° position and the 90° versus 120° position.
Table 2.
Knee laxity values
Fig. 3.
Mean coronal plane joint laxity is presented for each flexion angle. Results for the native knee and the TKA with the restored medial joint line are shown (TKA0). No statistically significant differences were noted between the native knee and the TKA0 position. Error bars = SD.
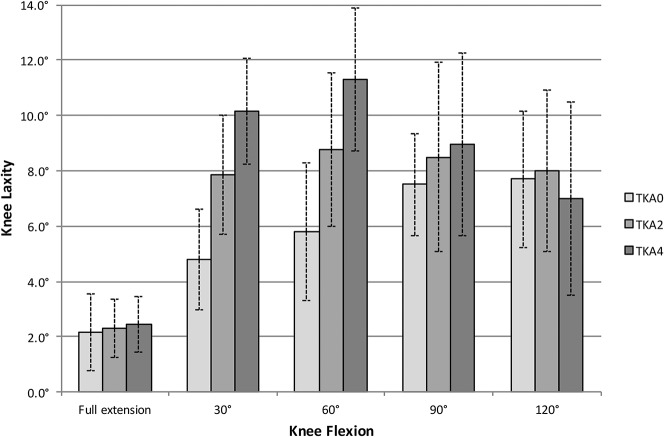
Despite that at 0° (2.2° ± 1.5° versus 2.3° ± 1.1° versus 2.5° ± 1.1°; p = 0.85) and 90° (7.5° ± 1.9° versus 9.0° ± 3.1° versus 9.0° ± 3.5°; p = 0.66) there was no difference in coronal plane laxity between the TKA0, TKA2, and TKA4 positions, an increased laxity at 30° (4.8° ± 1.9° versus 7.9° ± 2.3° versus 10.2° ± 2.0; p < 0.001) and 60° (5.7° ± 2.7° versus 8.8° ± 2.9° versus 11.3° ± 2.9°; p < 0.001) was observed when the medial joint line was raised by 2 and 4 mm respectively (Fig. 4).
Fig. 4.
Mean coronal plane joint laxity is presented for each flexion angle. Results for the TKA with the restored joint line (TKA0), the 2-mm (TKA2), and 4-mm (TKA4) raised joint lines are shown. No statistically significant differences were noted among the three groups in extension or at 90° and 120° flexion. However, significant increases in coronal plane laxity were noted at 30° and 60° flexion.
The first distal recut of +2 mm (TKA2) increased overall coronal plane laxity by on average 64% (3.1°) at 30° flexion (p < 0.01) and 51% (3.0°) at 60° flexion (p = 0.02) (Table 2). Performing a second +2-mm recut (TKA4) of the distal and posterior femur increased the mid-flexion laxity by 111% (5.4°; p < 0.01) at 30° and 95% (5.5°) at 60° flexion (p < 0.01) compared with the 9-mm baseline resection (TKA0) (Table 2).
No differences in terms of coronal plane laxity, with the numbers available, were found between the knees implanted with kinematic alignment versus mechanical alignment at any flexion angle.
The analytical model showed an equal length of the superficial MCL in full extension and at 90° flexion after raising and anteriorizing the joint line by 4 mm (Fig. 5). In the mid-flexion range (30°-60°), slackening of the superficial MCL of up to 2 mm was seen compared with the starting position. At 90° flexion, equal tension on the superficial MCL as in the 0° position was found. In deeper flexion (> 90°), progressive lengthening of the superficial MCL was seen.
Fig. 5.
Geometric models of the medial side of the knee are shown. The effect of a 4-mm smaller and 4-mm proximal femoral component with a 4-mm thicker insert (13 mm) on the superficial MCL isometry is shown. The models predicted equal tension on the superficial MCL in full extension and at 90° flexion strain and slackening as the knee rotates around a new center of rotation.
Discussion
The concept of mid-flexion instability remains poorly defined and understood. It was first introduced by Martin and Whiteside [32], who found a considerable increase in laxity in the mid-flexion range (30°-60°) by shifting the femoral component of a TKA prosthesis 5 mm proximal and 5 mm anterior. More recently, Cross et al. [7] found that raising the joint line during TKA to increase maximal extension caused substantial mid-flexion instability. Mid-flexion instability therefore was defined as instability in the mid-flexion range (30°-60°). Our current study would suggest that the definition of mid-flexion instability include the concept of instability in the mid-flexion range despite an equally balanced flexion and extension gap. That is, mid-flexion instability should be separated from other forms of coronal and sagittal plane instability, which are the consequence of a mismatch between the flexion and extension gap. Because most surgical routines only involve testing of stability in full extension and at 90° flexion, this type of instability frequently is overlooked. In a study using computer navigation, Yoon et al. [48] observed mid-flexion laxity in 36% of their patients during intraoperative TKA stability testing.
Our study has several limitations. First, all prostheses were cruciate substituting (posterior stabilized). The PCL is known to have an important effect on coronal plane stability. Removal is likely to affect stability in the mid-flexion range. Hino et al. [17] found more mid-flexion laxity in a TKA with a posterior stabilized versus a cruciate retaining prosthesis. However, it is crucial to take the level of the joint line into account. Surgeons using posterior stabilized prostheses in many cases will raise the joint line to compensate for the increase in flexion space resulting from cutting the PCL. The level of the joint line therefore is an important confounding variable for studies measuring coronal plane stability. By using computer navigation and a strict measured resection technique, we kept the medial joint line at its original level in all our specimens. Second, the native joint laxity was measured after resection of the anterior horn of the medial meniscus and lateral meniscus. Removal was needed to map the joint surface with the navigation software. Removal of the meniscus is known to have an effect on AP and rotational stability, but the effect on coronal plane stability is unknown [4, 33, 47]. Despite that only the anterior portion of the medial meniscus was removed and the body of the meniscus with its attachments to the deep MCL was left untouched, we cannot exclude an effect on coronal plane stability. Nevertheless, our results for native knee varus and valgus stability were comparable to those of others [23].
Numerous limitations apply here because we used a cadaver model in this study. In a cadaver model, it is not possible to know how dynamic forces (such as muscle contractions) or tissue scarring after surgery affect the degree of mid-flexion laxity in the in vivo situation. However, the purpose of our study was to evaluate the effect of joint line elevation on the static varus and valgus stabilizers of the knee and validate the simplified analytical model. This study serves as a proof of concept that raising the joint line leads to increased mid-flexion coronal plane laxity. An increase greater than 100% in passive laxity is likely to also affect dynamic stability. Other limitations related to this being a cadaveric study are the absence of knee osteoarthritis and the absence of deformity in the coronal plane in all knees. This limits direct conclusions related to severe osteoarthritic knees. However, the primary target of this study was better understanding of the biomechanics of coronal plane stability in the intact knee. This knowledge is essential before conclusions can be made regarding osteoarthritic knees. Tissue properties of a cadaveric knee might be different from living tissues. However, if fresh frozen tissue and only one freeze-thaw cycle is used, the effect on biomechanical properties is minimal. Finally, it is unknown what degree of joint laxity can be tolerated after TKA before clinical symptoms occur, which makes it difficult to draw conclusions regarding clinical importance. Moreover, the amount of laxity that is tolerated is likely subject-specific with wide variation throughout the population. Defining a threshold for clinical importance in terms of effect sizes therefore is difficult.
Finally, we need to address some limitations related to the analytical computer model itself. To make the model usable, certain simplifications (assumptions in the model) needed to be made. First the superficial MCL was considered a perfect isometric ligament. This is the case between 20° and 80° knee flexion, but in reality there is tensioning of the ligament toward terminal extension and slackening in deeper flexion. Second, the insertion site of the MCL was considered a point for purposes of modeling, although in reality, the superficial MCL inserts broadly, producing differential amounts tension in its anterior and posterior parts through the arc of motion. Third stability provided by the cruciate ligaments was not taken into account. However, despite these limitations, the model was able to predict the observed findings.
The most important finding of this study was that when the medial joint line was raised by 2 mm, there was an average increase of 64% in mid-flexion laxity. When the joint line was raised by 4 mm, the increase in mid-flexion laxity was, on average, 111%. When the joint line was restored at its original level, normal joint laxity throughout the ROM was seen. It would appear that restoration of the level of the medial joint line is an essential prerequisite for normal coronal plane stability in TKAs. The effect of joint line position on knee stability and ligament balance also was suggested by others. Hungerford et al. [22] stated: “ligament balance is principally a function of the femoral component and joint line positions relative to the femoral origins of the collateral and cruciate ligaments.” Although a 2-mm increase might seem minimal, it frequently is encountered during primary TKAs and its effect on coronal plane stability was found to be substantial. When the joint line is raised 4 mm, the mid-flexion joint laxity becomes even more pronounced. Raising the joint line by 4 mm may be encountered less frequently during primary TKA but is frequently seen in revision TKAs. Moreover, joint line changes of 4 mm or greater may be associated with an inferior clinical result [18, 34, 35, 37]. After primary TKA, functional outcome was improved when the joint line was kept at its original level [1], and some authors suggest that the explanation for association of an elevated joint line and inferior clinical results is the result of mid-flexion laxity [34].
We also sought to determine the effect of the alignment technique (mechanical versus kinematic) on the development of mid-flexion laxity during TKA. Full-body specimens were used with one alignment technique on one side and the other on the contralateral side, thus minimizing bias of interindividual variation. No effect of orientation of the joint line (mechanical versus kinematic) on coronal plane stability was found (Fig. 1). As the only difference between the two techniques in our study consists of the thickness of the lateral condylar resection (and thus orientation of the joint line), this means that restoration of the level of the medial joint line seems to be an essential prerequisite for normal joint laxity and is independent of the joint line orientation in the coronal plane. Discussion regarding the best orientation of the joint line in the coronal plane is ongoing. On average, the joint line is tilted in 3° varus. Mechanical alignment aims at a 0° joint line orientation, whereas in kinematic alignment the native joint line orientation is reproduced. Aside from the coronal plane, a surgeon advocating kinematic alignment also will restore the joint line in the axial plane by using 0° external rotation. From a conceptional point of view, kinematic alignment might be considered as resurfacing of the knee. Some believe that kinematic implantation of a TKA prosthesis best reproduces native knee stability and normal joint function [21], whereas others suggest that kinematic alignment is associated with an increased laxity in the mid-flexion range [24].
A mechanistic explanation for the link between the level of the joint line and joint stability is still lacking. The observed mid-flexion instability cannot be explained by the classic flexion and extension gap paradigm. We obtained a balanced flexion and extension gap in all knees, even after raising the joint line. Nevertheless, mid-flexion laxity was observed in the specimens with a raised joint line. Therefore, the flexion and extension gap paradigm is not sufficient to predict joint stability after TKA. In an attempt to provide more profound insight in the association between the level of the medial joint line and joint stability, we developed an analytical model. In the model, the effect of a 4-mm more-anterior and 4-mm more-proximal position of the joint line on the isometry of the superficial MCL was shown (Fig. 6). In mid-flexion, the superficial MCL insertion site was moved distally relative to the center of rotation, thereby causing slackening of the superficial MCL of up to 2 mm (Fig. 5). This is consistent with our data and data from previous studies [7, 33]. At 90° flexion, an equal length as in the 0° position was shown. The knee therefore would be considered balanced by most surgeons. In deeper flexion, proximal movement of the superficial MCL insertion site relative to the center of rotation caused elongation. This is also consistent with our data regarding strain in the superficial MCL after joint line elevation and reported data [11]. The value of our geometric model lies not in the prediction of absolute length changes of the superficial MCL, but in providing a qualitative explanation for the effect of joint line changes on joint stability. In contrast to the classic flexion and extension gap paradigm, it provides a new way of thinking about joint stability not only at 0° and 90° knee flexion, but throughout the full arc of motion.
Fig. 6.
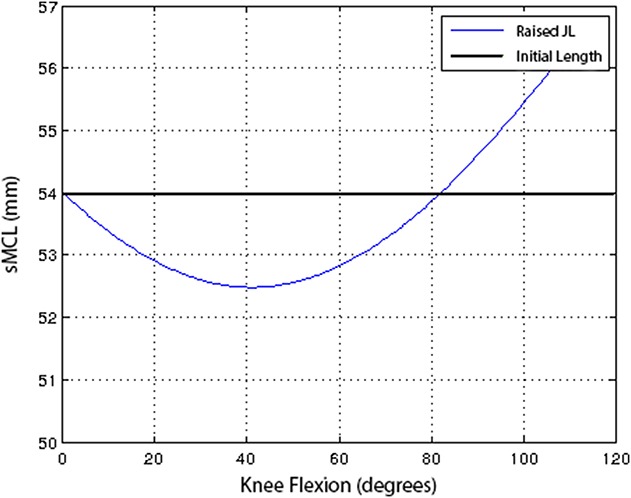
The length of the superficial MCL (sMCL) is represented as function of the ROM. Length changes were calculated based on the geometric model. The black line represents the isometric superficial MCL in the native knee. The effect of raising the joint line 4 mm and using a 4-mm smaller component is shown by the blue line. Slackening in the mid-flexion range and progressive lengthening in deeper flexion are seen. Slackening in the mid-flexion range and progressive lengthening in deeper flexion are seen. JL = joint line.
The collateral ligaments are recognized to be the primary joint stabilizers in the coronal plane and the concept of their isometry has been at the heart of models that describe normal knee motion [43]. To be able to maintain its isometry during knee flexion, the superficial MCL inserts at the tibiofemoral center of rotation [40, 45]. Restoration of this center of rotation with a single-radius TKA is known to reproduce normal joint stability [23]. Changes in joint line position with a single-radius TKA change the tibiofemoral center of rotation from its original position (Fig. 2). Because the femoral insertion site of the superficial MCL remains at the same spot, it will pivot around the new center of rotation during knee flexion and its isometric behavior will be changed (Fig. 5). The precise effect on the length change in the superficial MCL depends on the direction of the joint line change.
The results of our cadaveric research and the analytical model indicate that restoration of the medial joint line reproduces more-normal joint stability after TKA. Raising the joint line causes substantial mid-flexion laxity despite equal and well-balanced flexion and extension gaps. Further in vivo research on osteoarthritic knees is needed to prove that this concept does improve joint stability and clinical outcomes after TKA.
Acknowledgments
We thank Maarten Boonen MD and Jan Dauwe MD (both from the Department of Orthopaedic Surgery, University Hospitals Leuven) for help with the experiments. We thank BRAINLAB for providing us the navigation tools and Martin Bauer (BRAINLAB) for assistance with the experiments.
Footnotes
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that neither he or she, nor any member of his or her immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at University of Leuven campus KULAK (Kortrijk, Belgium).
References
- 1.Babazadeh S, Dowsey MM, Swan JD, Stoney JD, Choong PF. Joint line position correlates with function after primary total knee replacement: a randomised controlled trial comparing conventional and computer-assisted surgery. J Bone Joint Surg Br. 2011;93:1223–1231. [DOI] [PubMed] [Google Scholar]
- 2.Bellemans J, Vandenneucker H, Victor J, Vanlauwe J. Flexion contracture in total knee arthroplasty. Clin Orthop Relat Res. 2006;452:78–82. [DOI] [PubMed] [Google Scholar]
- 3.Blankevoort L, Huiskes R, De Lange A. Helical axes of passive knee joint motions. J Biomech. 1990;23:1219–1229. [DOI] [PubMed] [Google Scholar]
- 4.Chen L, Linde-Rosen M, Hwang SC, Zhou J, Xie Q, Smolinski P, Fu FH. The effect of medial meniscal horn injury on knee stability. Knee Surg Sports Traumatol Arthrosc. 2015;23:126–131. [DOI] [PubMed] [Google Scholar]
- 5.Churchill DL, Incavo SJ, Johnson CC, Beynnon BD. The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res. 1998;356:111–118. [DOI] [PubMed] [Google Scholar]
- 6.Cope MR, O’Brien BS, Nanu AM. The influence of the posterior cruciate ligament in the maintenance of joint line in primary total knee arthroplasty: a radiologic study. J Arthroplasty. 2002;17:206–208. [DOI] [PubMed] [Google Scholar]
- 7.Cross MB, Nam D, Plaskos C, Sherman SL, Lyman S, Pearle AD, Mayman DJ. Recutting the distal femur to increase maximal knee extension during TKA causes coronal plane laxity in mid-flexion. Knee. 2012;19:875–879. [DOI] [PubMed] [Google Scholar]
- 8.Eckhoff D, Hogan C, DiMatteo L, Robinson M, Bach J. Difference between the epicondylar and cylindrical axis of the knee. Clin Orthop Relat Res. 2007;461:238–244. [DOI] [PubMed] [Google Scholar]
- 9.Eckhoff DG, Bach JM, Spitzer VM, Reinig KD, Bagur MM, Baldini TH, Flannery NM. Three-dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg Am. 2005;87(suppl 2):71–80. [DOI] [PubMed] [Google Scholar]
- 10.Ensini A, Catani F, Biasca N, Belvedere C, Giannini S, Leardini A. Joint line is well restored when navigation surgery is performed for total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20:495–502. [DOI] [PubMed] [Google Scholar]
- 11.Feeley BT, Muller MS, Allen AA, Granchi CC, Pearle AD. Isometry of medial collateral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17:1078–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frankel VH, Burstein AH, Brooks DB. Biomechanics of internal derangement of the knee: pathomechanics as determined by analysis of the instant centers of motion. J Bone Joint Surg Am. 1971;53:945–962. [PubMed] [Google Scholar]
- 13.Ghosh KM, Merican AM, Iranpour F, Deehan DJ, Amis AA. Length-change patterns of the collateral ligaments after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20:1349–1356. [DOI] [PubMed] [Google Scholar]
- 14.Griffith CJ, LaPrade RF, Johansen S, Armitage B, Wijdicks C, Engebretsen L. Medial knee injury: Part 1: static function of the individual components of the main medial knee structures. Am J Sports Med. 2009;37:1762–1770. [DOI] [PubMed] [Google Scholar]
- 15.Grood ES, Noyes FR, Butler DL, Suntay WJ. Ligamentous and capsular restraints preventing straight medial and lateral laxity in intact human cadaver knees. J Bone Joint Surg Am. 1981;63:1257–1269. [PubMed] [Google Scholar]
- 16.Hill PF, Vedi V, Williams A, Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI. J Bone Joint Surg Br. 2000;82:1196–1198. [DOI] [PubMed] [Google Scholar]
- 17.Hino K, Ishimaru M, Iseki Y, Watanabe S, Onishi Y, Miura H. Mid-flexion laxity is greater after posterior-stabilised total knee replacement than with cruciate-retaining procedures: a computer navigation study. Bone Joint J. 2013;95:493–497. [DOI] [PubMed] [Google Scholar]
- 18.Hofmann AA, Kurtin SM, Lyons S, Tanner AM, Bolognesi MP. Clinical and radiographic analysis of accurate restoration of the joint line in revision total knee arthroplasty. J Arthroplasty. 2006;21:1154–1162. [DOI] [PubMed] [Google Scholar]
- 19.Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG. The axes of rotation of the knee. Clin Orthop Relat Res. 1993;290:259–268. [PubMed] [Google Scholar]
- 20.Howell SM, Howell SJ, Hull ML. Assessment of the radii of the medial and lateral femoral condyles in varus and valgus knees with osteoarthritis. J Bone Joint Surg Am. 2010;92:98–104. [DOI] [PubMed] [Google Scholar]
- 21.Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res. 2013;471:1000–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hungerford DS, Kenna RV, Krackow KA. The porous-coated anatomic total knee. Orthop Clin North Am. 1982;13:103–122. [PubMed] [Google Scholar]
- 23.Hunt NC, Ghosh KM, Blain AP, Athwal KK, Rushton SP, Amis AA, Longstaff LM, Deehan DJ. How does laxity after single radius total knee arthroplasty compare with the native knee? J Orthop Res. 2014;32:1208–1213. [DOI] [PubMed] [Google Scholar]
- 24.Incavo SJ, Schmid S, Sreenivas K, Ismaily S, Noble PC. Total knee arthroplasty using anatomic alignment can produce mid-flexion laxity. Clin Biomech. 2013;28:429–435. [DOI] [PubMed] [Google Scholar]
- 25.Insall JN, Binazzi R, Soudry M, Mestriner LA. Total knee arthroplasty. Clin Orthop Relat Res. 1985;192:13–22. [PubMed] [Google Scholar]
- 26.Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br. 2000;82:1189–1195. [DOI] [PubMed] [Google Scholar]
- 27.Johal P, Williams A, Wragg P, Hunt D, Gedroyc W. Tibio-femoral movement in the living knee: a study of weight bearing and non-weight bearing knee kinematics using “interventional” MRI. J Biomech. 2005;38:269–276. [DOI] [PubMed] [Google Scholar]
- 28.Kawamura H, Bourne RB. Factors affecting range of flexion after total knee arthroplasty. J Orthop Sci. 2001;6:248–252. [DOI] [PubMed] [Google Scholar]
- 29.Kettelkamp DB, Johnson RJ, Smidt GL, Chao EY, Walker M. An electrogoniometric study of knee motion in normal gait. J Bone Joint Surg Am. 1970;52:775–790. [PubMed] [Google Scholar]
- 30.Laubenthal KN, Smidt GL, Kettelkamp DB. A quantitative analysis of knee motion during activities of daily living. Phys Ther. 1972;52:34–43. [DOI] [PubMed] [Google Scholar]
- 31.Luyckx T, Verstraete M, De Roo K, Van Der Straeten C, Victor J. High strains near femoral insertion site of the superficial medial collateral ligament of the knee can explain the clinical failure pattern. J Orthop Res. 2016;34:2016–2024. [DOI] [PubMed] [Google Scholar]
- 32.Martin JW, Whiteside LA. The influence of joint line position on knee stability after condylar knee arthroplasty. Clin Orthop Relat Res. 1990;259:146–156. [PubMed] [Google Scholar]
- 33.Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010;38:1591–1597. [DOI] [PubMed] [Google Scholar]
- 34.Partington PF, Sawhney J, Rorabeck CH, Barrack RL, Moore J. Joint line restoration after revision total knee arthroplasty. Clin Orthop Relat Res. 1999;367:165–171. [PubMed] [Google Scholar]
- 35.Porteous AJ, Hassaballa MA, Newman JH. Does the joint line matter in revision total knee replacement? J Bone Joint Surg Br. 2008;90:879–884. [DOI] [PubMed] [Google Scholar]
- 36.Schroer WC, Berend KR, Lombardi AV, Barnes CL, Bolognesi MP, Berend ME, Ritter MA, Nunley RM. Why are total knees failing today? Etiology of total knee revision in 2010 and 2011. J Arthroplasty. 2013;28(8 suppl):116–119. [DOI] [PubMed] [Google Scholar]
- 37.Shoji H, Solomonow M, Yoshino S, D’Ambrosia R, Dabezies E. Factors affecting postoperative flexion in total knee arthroplasty. Orthopedics. 1990;13:643–649. [DOI] [PubMed] [Google Scholar]
- 38.Snider MG, MacDonald SJ. The influence of the posterior cruciate ligament and component design on joint line position after primary total knee arthroplasty. J Arthroplasty. 2009;24:1093–1098. [DOI] [PubMed] [Google Scholar]
- 39.Soudan K, Van Audekercke R, Martens M. Methods, difficulties and inaccuracies in the study of human joint kinematics and pathokinematics by the instant axis concept: example: the knee joint. J Biomech. 1979;12:27–33. [DOI] [PubMed] [Google Scholar]
- 40.Stoddard JE, Deehan DJ, Bull AM, McCaskie AW, Amis AA. The kinematics and stability of single-radius versus multi-radius femoral components related to mid-range instability after TKA. J Orthop Res. 2013;31:53–58. [DOI] [PubMed] [Google Scholar]
- 41.Victor J, Labey L, Wong P, Innocenti B, Bellemans J. The influence of muscle load on tibiofemoral knee kinematics. J Orthop Res. 2010;28:419–428. [DOI] [PubMed] [Google Scholar]
- 42.Victor J, Van Glabbeek F, Vander Sloten J, Parizel PM, Somville J, Bellemans J. An experimental model for kinematic analysis of the knee. J Bone Joint Surg Am. 2009;91(suppl 6):150–163. [DOI] [PubMed] [Google Scholar]
- 43.Victor J, Wong P, Witvrouw E, Vander Sloten J, Bellemans J. How isometric are the medial patellofemoral, superficial medial collateral, and lateral collateral ligaments of the knee? Am J Sports Med. 2009;37:2028–2036. [DOI] [PubMed] [Google Scholar]
- 44.Walker PS, Shoji H, Erkman MJ. The rotational axis of the knee and its significance to prosthesis design. Clin Orthop Relat Res. 1972;89:160–170. [PubMed] [Google Scholar]
- 45.Warren LF, Marshall JL, Girgis F. The prime static stabilizer of the medial side of the knee. J Bone Joint Surg Am. 1974;56:665–674. [PubMed] [Google Scholar]
- 46.Weber W, Weber E. Mechanik der menschilichen Gehwerkzeuge: eine anatomische-physiologische untersuchung. Göttingen, Germany: Dieterich; 1836. [Google Scholar]
- 47.Yammine K. Effect of partial medial meniscectomy on anterior tibial translation in stable knees: a prospective controlled study on 32 patients. BMC Sports Sci Med Rehabil. 2013;5:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yoon JR, Jeong HI, Oh KJ, Yang JH. In vivo gap analysis in various knee flexion angles during navigation-assisted total knee arthroplasty. J Arthroplasty. 2013;28:1796–800. [DOI] [PubMed] [Google Scholar]