Abstract
Background
Pain-coping strategies and appraisals are responses to the pain experience. They can influence patient-reported and physical performance outcome measures in a variety of disorders, but the associations between a comprehensive profile of pain-coping responses and preoperative pain/function and physical performance measures in patients scheduled for knee arthroplasty have not been examined. Patients with moderate to high pain catastrophizing (a pain appraisal approach associated with an exaggerated focus on the threat value of pain) may represent an excellent study population in which to address this knowledge gap.
Questions/purposes
We asked the following questions among patients with high levels of pain catastrophizing who were scheduled for TKA: (1) Do maladaptive pain responses correlate with worse self-reported pain intensity and function and physical performance? (2) Do adaptive pain-coping responses show the opposite pattern? As an exploratory hypothesis, we also asked: (3) Do maladaptive responses show more consistent associations with measures of pain, function, and performance as compared with adaptive responses?
Methods
A total of 384 persons identified with moderate to high levels of pain catastrophizing and who consented to have knee arthroplasty were recruited. The sample was 67% (257 of 384) women and the mean age was 63 years. Subjects were consented between 1 and 8 weeks before scheduled surgery. All subjects completed the WOMAC pain and function scales in addition to a comprehensive profile of pain coping and appraisal measures and psychologic health measures. Subjects also completed the Short Physical Performance Battery and the 6-minute walk test. For the current study, all measures were obtained at a single point in time at the preoperative visit with no followup. Multilevel multivariate multiple regression was used to test the hypotheses and potential confounders were adjusted for in the models.
Results
Maladaptive pain responses were associated with worse preoperative pain and function measures. For example, the maladaptive pain-coping strategy of guarding and the pain catastrophizing appraisal measures were associated with WOMAC pain scores such that higher guarding scores (β = 0.12, p = 0.007) and higher pain catastrophizing (β = 0.31, p < 0.001) were associated with worse WOMAC pain; no adaptive responses were associated with better WOMAC pain or physical performance scores. Maladaptive responses were also more consistently associated with worse self-reported and performance-based measure scores (six of 16 associations were significant in the hypothesized direction), whereas adaptive responses did not associate with better scores (zero of 16 scores were significant in the hypothesized direction).
Conclusions
The maladaptive responses of guarding, resting, and pain catastrophizing were associated with worse scores on preoperative pain and performance measures. These are pain-related responses surgeons should consider when assessing patients before knee arthroplasty. TKA candidates found to have these pain responses may be targets for treatments that may improve postoperative outcome given that these responses are modifiable. Future intervention-based research should target this trio of maladaptive pain responses to determine if intervention leads to improvements in postsurgical health outcomes.
Level of Evidence
Level I, prognostic study.
Introduction
The prognostic role of pain-coping strategies and appraisals has been the focus of research in individuals with a variety of chronic pain conditions, but less so for persons undergoing TKA. Pain-coping strategies are a person’s responses to manage pain and its effects and include such strategies as resting, exercising, or asking for assistance. Pain-coping strategies are generally classified as adaptive strategies thought to result in better outcomes over time or maladaptive strategies thought to result in worse outcomes over time [20]. Pain-related beliefs or appraisals are a person’s thoughts regarding the pain. These can be classified as adaptive (self-efficacy beliefs about being able to manage pain) [4] or maladaptive (“catastrophizing” or excessively negative thoughts about pain) [41]. Research in other populations has shown that maladaptive coping strategies and pain-related appraisals tend to be more consistently associated with important outcomes than adaptive ones [16, 40], suggesting that it may be more useful to help patients decrease their use of maladaptive responses than to increase their use of adaptive ones.
The two most commonly used measures of pain-coping strategies are the Chronic Pain Coping Inventory (CPCI) [22] and the Coping Strategies Questionnaire [34]. Two commonly used measures of pain-related beliefs or appraisals are the Pain Catastrophizing Scale (PCS) [39] and the Arthritis Self-efficacy Scale (ASES) [28]. Pain-coping strategies and appraisals are important to study as potential prognostic indicators for persons with chronic pain, in part because they are modifiable. This provides an opportunity to intervene and potentially improve both short- and long-term outcomes. One prior study in patients undergoing TKA of which we are aware has examined associations between pain-coping strategies and related appraisals with patient-reported outcome measures (PROMs), but only for isolated coping or appraisal measures [1]. We found no studies that evaluated the extent to which a profile of pain coping and appraisal measures independently associates with preoperative measures of pain, function, and physical performance. This evidence gap is particularly important given the recent emphasis on performance-based outcomes as part of a comprehensive assessment [11]. A study examining these associations would provide evidence that could more fully inform surgeons of the most likely coping and appraisal targets for intervention before and after TKA.
Given these considerations, we analyzed data obtained from a sample of patients with moderate to high pain catastrophizing who were consented for TKA to determine if (1) maladaptive pain-coping strategies (such as guarding, resting, asking for assistance) and a pain-related appraisal (such as pain catastrophizing) were associated with worse preoperative self-reported pain intensity, function, and observed physical performance after adjustment for potential confounding variables; and if (2) adaptive pain-coping strategies and pain-related appraisals (including task persistence, exercise/stretch, coping self-statements, relaxation, seeking support, and pain self-efficacy beliefs) would show the opposite pattern. As an exploratory hypothesis, we also asked: (3) Do maladaptive responses show more consistent associations with measures of pain, function, and performance as compared with adaptive responses?
Patients and Methods
Study Design and Setting
The study was a prospective National Institutes of Health-funded randomized clinical trial (UM1AR062800, NCT01620983) conducted at five sites (Duke University, Durham, NC, USA; New York University Medical Center, New York, NY, USA; Virginia Commonwealth University, Richmond, VA, USA; Wake Forest University, Winston-Salem, NC, USA; and Southern Illinois University, Springfield, IL, USA). The purpose of the trial is to test the effectiveness of a telephone-based pain-coping skills training program in patients who report moderate to high levels of pain catastrophizing before surgery. Please see the published protocol for more information [31]. The current study is a cross-sectional study of baseline preoperative data collected during the trial. Patients were recruited and signed an institutional review board-approved consent form between January 2013 and June 2016. Only the preoperative baseline data were used to test the study hypotheses.
Participants
Patients were included if they (1) were aged 45 years or older; (2) had a diagnosis of osteoarthritis as confirmed by the surgeon; (3) had TKA scheduled between 1 week and 8 weeks after consent; (4) scored 16 or greater on the PCS [32], given that the primary study was designed to evaluate the efficacy of an intervention for reducing catastrophizing; and (5) were able to read and speak English. Patients were excluded if they (1) were scheduled for revision surgery; (2) underwent another arthroplasty within 6 months of the surgery of interest; (3) had a self-reported diagnosis of inflammatory arthritis (eg, rheumatoid arthritis, psoriatic arthritis); (4) were scheduled for bilateral TKA; (5) planned to undergo hip or knee arthroplasty within 6 months after the current knee arthroplasty; (6) scored 20 or greater on the depression screener (indicating severe clinical depression, which was judged to be a safety risk for the trial) [27]; and (7) scored 2 or less on the cognitive screener [6]. In general, we were interested in studying a sample of persons with knee osteoarthritis who had moderate to high pain catastrophizing and the patients indicating they had no scheduled arthroplasty procedures on other joints. In addition, they indicated they had no other arthroplasty surgeries in the 6 months before study participation. We also wanted to recruit persons who had normal cognitive function to assure sound data collection and we wanted to exclude persons with severe clinical depression leading to safety concerns during the trial. A total of 4043 patients were considered for screening. Of these, 551 declined to participate, 917 did not respond to requests to screen, 1976 did not meet one or more inclusion criteria, and 599 met all criteria. Of the 599 who met all criteria, 402 consented and 197 declined consent to participate. Of 402 patients who consented to participate, 18 had their surgery either canceled or delayed for medical reasons over the entire study period and were not included in the final sample. A total of 384 subjects participated.
Description of Experiment
Between 1 and 8 weeks before surgery, patients at each of the five sites were approached by the site coordinator and were informed about the purpose of the clinical trial. If patients were interested, they signed an institutional review board-approved consent form and then completed all required baseline data collection. All patients underwent either TKA (n = 367) or partial knee arthroplasty (n = 17). A total of 32 surgeons performed TKAs across the five sites and the total number of patients seen by each surgeon ranged from one to 54.
Outcome Measures of Interest at the Preoperative Visit
The PROMs were the WOMAC pain and the WOMAC function scales. WOMAC pain scores ranged from 0 to 20 with higher scores indicating greater pain with activity. The WOMAC function scale quantifies the extent of perceived difficulty with daily activities with scores ranging from 0 (no difficulty with activity) to 68 (extreme difficulty with all activity). Reliability and validity of the WOMAC have been repeatedly demonstrated for persons undergoing TKA [2, 3, 13].
The performance-based outcome measures were the Short Physical Performance Battery (SPPB) and the 6-minute walk test. The SPPB is a composite measure that includes balance tests, a 4-m walk gait speed test, and a single and repeated chair stand test [19]. The SPPB has been shown to be both reliable and valid for measuring physical performance-related deficits in persons with hip and knee osteoarthritis [7, 15, 19]. Scores on the SPPB range from 0 to 12 with higher scores equating to better physical performance. The 6-minute walk test is a reliable measure of actual walking endurance and when the SPPB and 6-minute walk test are combined with self-reported measures provides a comprehensive summary of PROMs and performance-based outcome measures [11, 25, 37].
Predictors
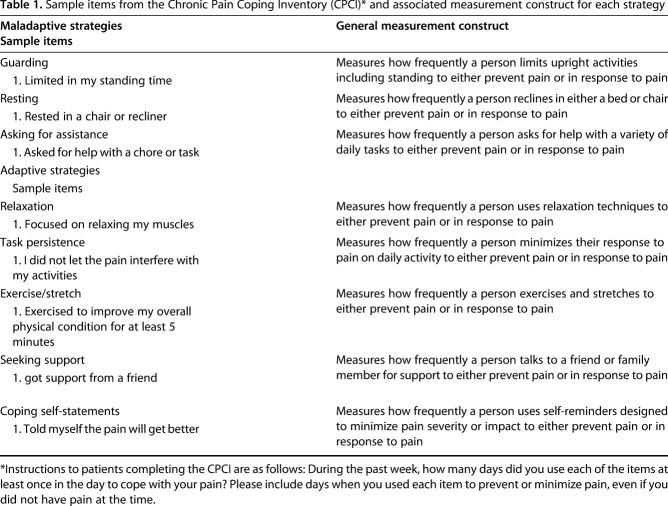
The pain-coping predictors were the subscale scores derived from the previously validated CPCI [22]. All two-item subscales from the CPCI were included in the analyses (Table 1). There are three maladaptive coping strategies (such as guarding, resting, and asking for assistance) and five adaptive coping strategies (like relaxation, task persistence, exercise/stretch, seeking support, and coping self-statements). Each subscale is scored from 0 to 14 with higher scores indicating higher use of each coping strategy in the previous week. Reliability and construct validity of each subscale have been supported [21].
Table 1.
Sample items from the Chronic Pain Coping Inventory (CPCI)* and associated measurement construct for each strategy
We used two pain-related appraisal measures, the PCS and the ASES. The PCS patient self-report instrument quantifies the extent to which a person amplifies their pain symptoms, feels helpless when experiencing pain, and ruminates about their pain experience. The PCS is a 13-item scale ranging from 0 (no pain catastrophizing) to 52 (most severe pain catastrophizing) [39]. Substantial research supports both the psychometric and prognostic importance of the PCS for patients undergoing TKA [32, 38, 39, 43]. The eight-item ASES is a validated measure of a patient’s beliefs in the ability to control pain and functional difficulty associated with arthritis [30]. Scores for the ASES range from 8 (lowest self-efficacy) to 80 (highest self-efficacy).
Potential Confounders
To account for other variables that may be associated with pain coping, appraisal, and PROMs or performance-based outcomes measures (that is, to reduce bias), we included measures of age, sex, race, body mass index (BMI), comorbidity, depression, and anxiety. Race was dichotomized to black subjects or all other subjects. BMI was recorded as kg/m2. We used the validated modified Charlson comorbidity index to quantify extent of comorbidity [23]. The previously validated Patient Health Questionnaire (PHQ-8) [27] and the Generalized Anxiety Scale (GAD-7) [26, 36] were used to quantify extent of depressive and anxiety symptoms, respectively. The PHQ-8 is scored from 0 to 24 and the GAD-7 is scored from 0 to 21 with higher scores indicating more severe depressive or anxiety symptoms.
Statistical Analysis
Multilevel multivariate multiple regression was used to examine the hypotheses. The selection of multilevel regression (that is, a random intercept model) accounted for cluster-based sampling of patients nested within surgeons. The choice of a multivariate analysis was motivated by a goal to estimate the effects of predictors on all four PROMs and performance-based outcome variables simultaneously. The regression analyses were run with the potential confounders included, which allowed us to estimate the effects of potential confounders on the prediction. The 6-minute walk test and the SPPB scores had 15% and 4% missing scores, respectively, either because the patient declined or because the patient was judged to be unsafe to perform the tests, whereas the WOMAC measures had no missing data. The full information maximum likelihood method was used to handle the missing data. We report standardized β coefficients for each model, which allows for direct comparison of each of the predictor variables in the models. Importantly, because this is a cross-sectional study, the predictor variables in our models are being used to identify predictors of outcome measures and not causes of these measures. MPlus (Version 7.4, https://www.statmodel.com/) was used to estimate the model and p < 0.05 indicated statistically significant associations.
Study Sample
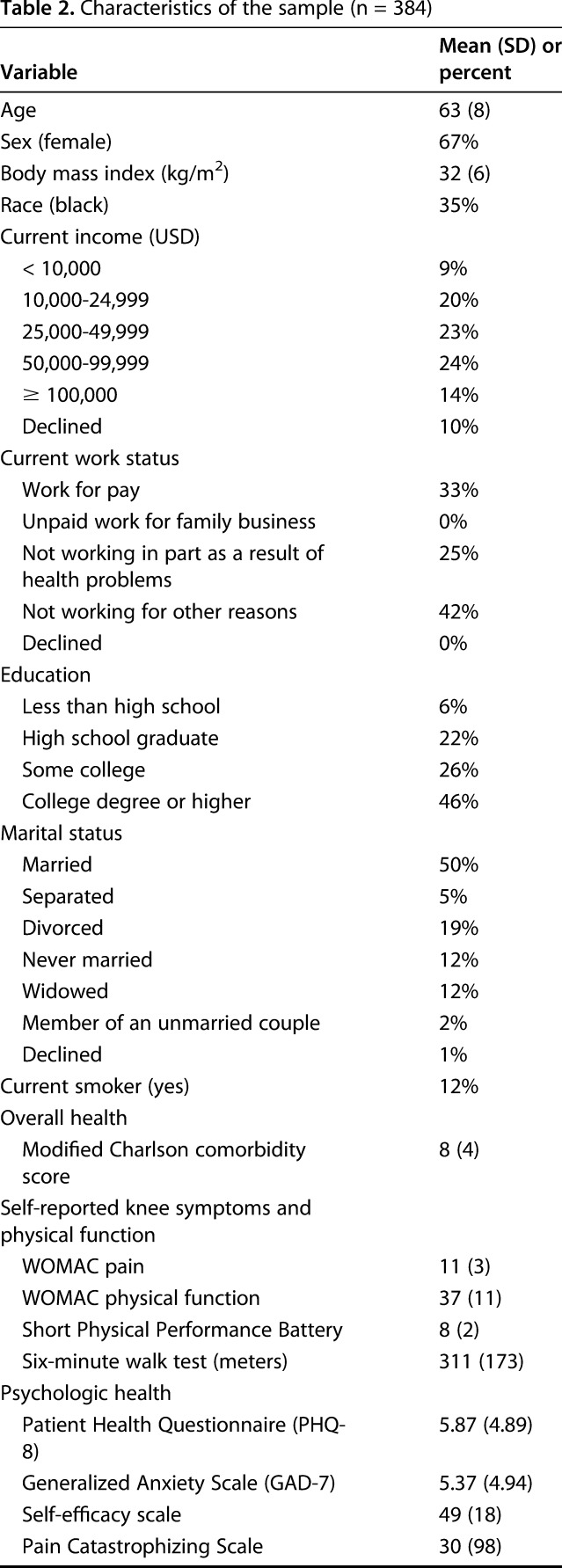
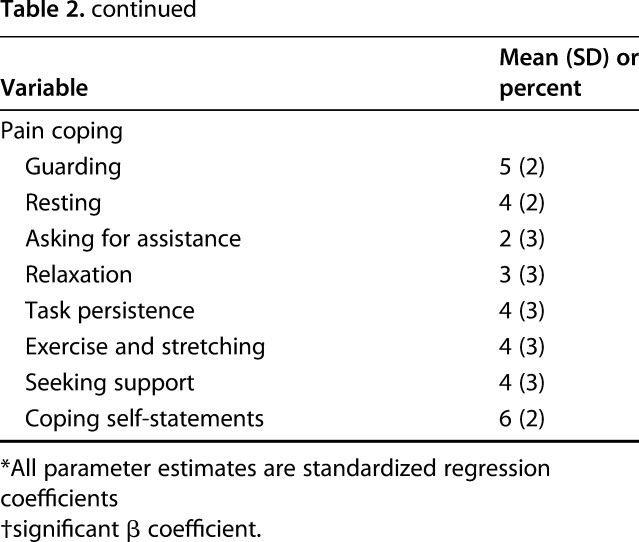
Characteristics of the sample demonstrate substantial variation across a variety of dimensions (Table 2).
Table 2.
Characteristics of the sample (n = 384)
Results
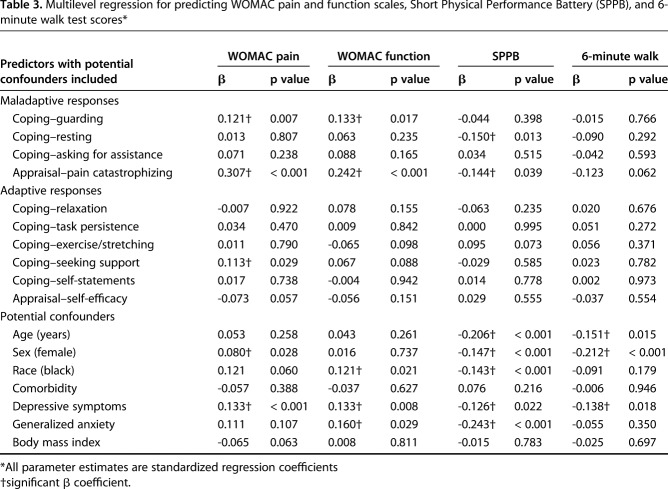
The maladaptive pain-coping strategy of guarding and the pain catastrophizing appraisal measures were positively associated with WOMAC pain scores such that higher guarding scores (β = 0.12, p = 0.007) and higher pain catastrophizing scores (β = 0.31, p < 0.001) were associated with worse WOMAC pain. Similar associations were found for WOMAC function scores (β = 0.13 for guarding and β = 0.24 for pain catastrophizing). These associations were present even after accounting for potential confounding variables. For physical performance outcome measures, the maladaptive pain-coping strategy of resting was negatively associated with SPPB scores (β = -0.15, p = 0.013) such that greater resting was associated with worse SPPB scores. Additionally, higher pain catastrophizing scores were associated with worse SPPB scores (β = -0.14, p = 0.039) after adjustment for potential confounding. These findings generally supported our hypotheses. All maladaptive pain-coping strategies and the pain catastrophizing appraisal measure are noted as “maladaptive responses,” whereas all adaptive pain-coping strategies and the self-efficacy appraisal measure are labeled “adaptive responses” in the statistical models analyzed (Table 3). Similar to partial correlation coefficients, the standardized β coefficients in multiple regression analysis are used as effect size indicators and are comparable. Using Cohen’s guidelines, standardized β coefficients indicate small effects when the coefficients approximate 0.1, moderate effects when it approximates 0.3, and large effects when the coefficient approximates 0.5 [9]. Applying this guideline to our study, all associations were small with the exception of associations between pain catastrophizing and WOMAC pain and function, which approximated a moderate effect size.
Table 3.
Multilevel regression for predicting WOMAC pain and function scales, Short Physical Performance Battery (SPPB), and 6-minute walk test scores*
The adaptive pain-coping strategy of seeking support was positively associated with baseline WOMAC pain scores (p = 0.029). That is, the higher the seeking support scores, the higher the WOMAC pain scores. However, the direction of this association was inconsistent with our hypothesis that higher adaptive coping responses would be associated with lower (that is, less) preoperative WOMAC pain or better WOMAC function scores. No other adaptive responses were negatively associated with WOMAC pain scores or WOMAC function scores nor was self-efficacy independently associated with the scores (Table 3).
Maladaptive responses generally were positively associated with self-reported and performance-based outcome measures, whereas adaptive coping strategies and appraisal scores were not associated with either WOMAC or performance-based scores in the hypothesized direction. These data are consistent with our exploratory hypothesis.
The adaptive coping strategies of relaxation, task persistence, exercise/stretching, coping self-statements, and self-efficacy appraisals did not predict any study measure score after adjusting for potential confounding variables. The maladaptive coping strategy, asking for assistance, also was not associated with any measure. Similarly, two covariates, BMI and comorbidity, were not related to study measures after adjustment for all other variables in the model.
Discussion
The study of pain-coping strategies and beliefs is important because these responses impact outcome measures for a variety of health conditions, and they are modifiable. There is thus the potential that these modifiable responses can be targets of interventions in those patients at risk for a poor outcome because of poor pain coping. We examined the association of a profile of both adaptive and maladaptive pain responses with self-reported baseline pain and functional scores in a sample of persons at particularly high risk for a poor outcome, those preparing for TKA with moderate to high levels of pain catastrophizing.
There are some limitations to our study. Our study was cross-sectional and we studied only persons who were screened into a planned randomized controlled trial (NCT01620983) and who had moderate to high levels of pain catastrophizing. This limits the potential generalizability of the findings to only patients with this symptom set. Furthermore, the restriction of range for pain catastrophizing scores attenuates the strength of the relationship between pain catastrophizing and other variables [14, 38, 43]. An additional important limitation is also related to the cross-sectional nature of the study design, where patients were tested at only one point in time. Although this allowed us to test specific hypotheses regarding the associations between pain-related coping and appraisals and measures of important function domains, the findings from such a design do not allow for inferences of causality. Association is only one of several criteria necessary for making a causal inference [8, 29]. Future longitudinal research and research using experimental designs (such as random assignment to interventions that target coping and appraisals for change) are needed to evaluate the extent to which pain coping and appraisals may be causally related to a subsequent change in function.
We identified a number of maladaptive responses to be associated with both PROMs and physical performance outcome measures. Both guarding and resting are related strategies that reflect a person’s hesitation to engage in physical activity. Both are also potentially modifiable. Thus, if patients were taught or encouraged to increase their activity and minimize time spent resting in response to pain, WOMAC pain and function scores could potentially be improved before surgery. Research is needed to test this possibility. The pain appraisal approach of pain catastrophizing was the only maladaptive response to be significantly associated with both WOMAC scores and physical performance. Consistent with a large body of research across a variety of chronic pain conditions [12], pain catastrophizing evidenced the most consistent association with preoperative measures among the four maladaptive approaches that we studied. Although pain catastrophizing has both trait and state-like qualities, pain-coping skills training has been shown to reduce pain catastrophizing in multiple studies [5, 24, 42] including persons with osteoarthritis [35]. These data support the need to evaluate the efficacy of treatments that target this appraisal for outcome effects in the TKA population.
We found only one adaptive coping strategy to be associated with WOMAC pain: the coping strategy of seeking support, which indicates the extent to which a person gets support from or talks to friends or family. However, the direction of the association found was opposite that hypothesized. More support-seeking was associated with higher (worse) WOMAC pain such that a 1-SD higher seeking-support strategy was associated with higher WOMAC pain scores by 0.11 SD, on average, after adjustment for confounding. Reasons for this association are unclear, but may be related to the cross-sectional nature of the data. That is, it is possible that patients with more pain seek social support as a way to help buffer the negative effects of that pain on their overall mood and function [17, 18], beneficial effects of which could not be detected in this study because outcomes subsequent to the coping responses were not assessed. It is also possible that although social support can have beneficial effects on psychologic function, some aspects of social support can have unintended negative effects as social reinforcers of pain and disability [10, 33].
As an exploratory hypothesis, we examined whether maladaptive responses, which we hypothesized would associate with worse scores on the preoperative measures tested, would demonstrate more consistent associations than adaptive responses, which we hypothesized would associate with better scores. Specifically, based on research in other pain populations [10, 33], we anticipated that responses to knee pain that were maladaptive would have a more consistent overall impact on both PROMs and physical performance-based outcome measures than adaptive responses. The data appear to support this hypothesis. None of the adaptive responses were associated with score measures in the hypothesized direction (that is, less pain, better function, and better performance), whereas three maladaptive responses were positively associated with self-reported pain and function as well as physical performance (worse pain and function). These data suggest the possibility that maladaptive responses may have a greater impact on pain and function before TKA relative to adaptive responses.
Guarding and resting, in addition to pain catastrophizing, were the maladaptive responses that were independently associated with worse preoperative WOMAC and physical performance measures, whereas adaptive coping responses were not related to better pain and functional scores in this sample of preoperative patients about to undergo TKA. Surgeons should consider assessing patients for guarding and resting responses to pain as well as pain catastrophizing given that these responses to pain associate with worse measures preoperatively, are modifiable, and could potentially impact outcome after surgery. Assessments of guarding and resting can be made quickly (in this study, this required only two items for each), and the PCS requires approximately 5 minutes for a patient to complete. In combination, these domains efficiently assess the most likely pain responses that could negatively impact postoperative recovery. Future research should focus on the prognostic benefit of measures of these three domains for identifying persons at risk for poor outcomes and for informing interventions designed to enhance recovery.
Acknowledgments
We acknowledge study staff and particularly the patients for their participation.
Footnotes
Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number UM1AR062800 and CTSA award No. KL2TR000057 from the National Center for Advancing Translational Sciences (DLR was Principal Investigator; DA, JS, RP, and LD were coinvestigators). One of the authors (MPJ) receives royalties when clinicians or researchers purchase or obtain a license to use one of the measures used in this study (the Chronic Pain Coping Inventory).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This trial was registered in ClinicalTrials.gov (NCT01620983).
This work was performed at Duke University, Durham, NC, USA; New York University Medical Center, New York, NY, USA; Virginia Commonwealth University, Richmond, VA, USA; Wake Forest University, Winston-Salem, NC, USA; and Southern Illinois University, Springfield, IL, USA.
References
- 1.Baert IA, Lluch E, Mulder T, Nijs J, Noten S, Meeus M. Does pre-surgical central modulation of pain influence outcome after total knee replacement? A systematic review. Osteoarthritis Cartilage. 2016;24:213–223. [DOI] [PubMed] [Google Scholar]
- 2.Bellamy N. The WOMAC Knee and Hip Osteoarthritis Indices: development, validation, globalization and influence on the development of the AUSCAN Hand Osteoarthritis Indices. Clin Exp Rheumatol. 2005;23:S148–S153. [PubMed] [Google Scholar]
- 3.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 4.Broderick JE, Junghaenel DU, Schneider S, Bruckenthal P, Keefe FJ. Treatment expectation for pain coping skills training: relationship to osteoarthritis patients' baseline psychosocial characteristics. Clin J Pain. 2011;27:315–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buhrman M, Nilsson-Ihrfeldt E, Jannert M, Strom L, Andersson G. Guided Internet-based cognitive behavioural treatment for chronic back pain reduces pain catastrophizing: a randomized controlled trial. J Rehabil Med. 2011;43:500–505. [DOI] [PubMed] [Google Scholar]
- 6.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771–781. [DOI] [PubMed] [Google Scholar]
- 7.Cecchi F, Molino-Lova R, Di IA, Conti AA, Mannoni A, Lauretani F, Benvenuti E, Bandinelli S, Macchi C, Ferrucci L. Measures of physical performance capture the excess disability associated with hip pain or knee pain in older persons. J Gerontol A Biol Sci Med Sci. 2009;64:1316–1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi HK, Seeger JD. Observational research in rheumatic disorders. Rheum Dis Clin North Am. 2004;30:685–699, v. [DOI] [PubMed] [Google Scholar]
- 9.Cohen J. Statistical Power: Analysis for the Behavioural Sciences. New York, NY, USA: Routledge; 1988. [Google Scholar]
- 10.Cunningham JL, Hayes SE, Townsend CO, Laures HJ, Hooten WM. Associations between spousal or significant other solicitous responses and opioid dose in patients with chronic pain. Pain Med. 2012;13:1034–1039. [DOI] [PubMed] [Google Scholar]
- 11.Dobson F, Hinman RS, Roos EM, Abbott JH, Stratford P, Davis AM, Buchbinder R, Snyder-Mackler L, Henrotin Y, Thumboo J, Hansen P, Bennell KL. OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthritis Cartilage. 2013;21:1042–1052. [DOI] [PubMed] [Google Scholar]
- 12.Edwards RR, Bingham CO, III, Bathon J, Haythornthwaite JA. Catastrophizing and pain in arthritis, fibromyalgia, and other rheumatic diseases. Arthritis Rheum. 2006;55:325–332. [DOI] [PubMed] [Google Scholar]
- 13.Escobar A, Quintana JM, Bilbao A, Arostegui I, Lafuente I, Vidaurreta I. Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthritis Cartilage. 2007;15:273–280. [DOI] [PubMed] [Google Scholar]
- 14.Forsythe ME, Dunbar MJ, Hennigar AW, Sullivan MJ, Gross M. Prospective relation between catastrophizing and residual pain following knee arthroplasty: two-year follow-up. Pain Res Manag. 2008;13:335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Freire AN, Guerra RO, Alvarado B, Guralnik JM, Zunzunegui MV. Validity and reliability of the short physical performance battery in two diverse older adult populations in Quebec and Brazil. J Aging Health. 2012;24:863–878. [DOI] [PubMed] [Google Scholar]
- 16.Geisser ME, Robinson ME, Riley JL., III Pain beliefs, coping, and adjustment to chronic pain: let's focus more on the negative. Pain Forum. 1999;8:161–168. [Google Scholar]
- 17.Ginting JV, Tripp DA, Nickel JC, Fitzgerald MP, Mayer R. Spousal support decreases the negative impact of pain on mental quality of life in women with interstitial cystitis/painful bladder syndrome. BJU Int. 2011;108:713–717. [DOI] [PubMed] [Google Scholar]
- 18.Goldberg GM, Kerns RD, Rosenberg R. Pain-relevant support as a buffer from depression among chronic pain patients low in instrumental activity. Clin J Pain. 1993;9:34–40. [DOI] [PubMed] [Google Scholar]
- 19.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. [DOI] [PubMed] [Google Scholar]
- 20.Haythornthwaite JA, Menefee LA, Heinberg LJ, Clark MR. Pain coping strategies predict perceived control over pain. Pain. 1998;77:33–39. [DOI] [PubMed] [Google Scholar]
- 21.Jensen MP, Keefe FJ, Lefebvre JC, Romano JM, Turner JA. One- and two-item measures of pain beliefs and coping strategies. Pain. 2003;104:453–469. [DOI] [PubMed] [Google Scholar]
- 22.Jensen MP, Turner JA, Romano JM, Strom SE. The Chronic Pain Coping Inventory: development and preliminary validation. Pain. 1995;60:203–216. [DOI] [PubMed] [Google Scholar]
- 23.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34:73–84. [DOI] [PubMed] [Google Scholar]
- 24.Keefe FJ, Shelby RA, Somers TJ, Varia I, Blazing M, Waters SJ, McKee D, Silva S, She L, Blumenthal JA, O'Connor J, Knowles V, Johnson P, Bradley L. Effects of coping skills training and sertraline in patients with non-cardiac chest pain: a randomized controlled study. Pain. 2011;152:730–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kennedy DM, Stratford PW, Wessel J, Gollish JD, Penney D. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord. 2005;6:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317–325. [DOI] [PubMed] [Google Scholar]
- 27.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114:163–173. [DOI] [PubMed] [Google Scholar]
- 28.Lorig K, Holman H. Arthritis Self-Efficacy Scales measure self-efficacy. Arthritis Care Res. 1998;11:155–157. [DOI] [PubMed] [Google Scholar]
- 29.Melhorn JM, Talmage JB, Ackerman WE, Hyman MH. AMA Guide to the Evaluation of Disease and Injury Causation. 2nd ed. Chicago, IL, USA: American Medical Association; 2014. [Google Scholar]
- 30.Mueller A, Hartmann M, Mueller K, Eich W. Validation of the arthritis self-efficacy short-form scale in German fibromyalgia patients. Eur J Pain. 2003;7:163–171. [DOI] [PubMed] [Google Scholar]
- 31.Riddle DL, Keefe FJ, Ang D, Saleh KJ, Dumenci L, Jensen MP, Bair MJ, Reed SD, Kroenke K. A phase III randomized three-arm trial of physical therapist delivered pain coping skills training for patients with total knee arthroplasty: the Kastpain protocol. BMC Musculoskelet Disord. 2012;13:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Riddle DL, Wade JB, Jiranek WA, Kong X. Preoperative pain catastrophizing predicts pain outcome after knee arthroplasty. Clin Orthop Relat Res. 2009;468:798–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Romano JM, Turner JA, Jensen MP, Friedman LS, Bulcroft RA, Hops H, Wright SF. Chronic pain patient-spouse behavioral interactions predict patient disability. Pain. 1995;63:353–360. [DOI] [PubMed] [Google Scholar]
- 34.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. [DOI] [PubMed] [Google Scholar]
- 35.Somers TJ, Blumenthal JA, Guilak F, Kraus VB, Schmitt DO, Babyak MA, Craighead LW, Caldwell DS, Rice JR, McKee DC, Shelby RA, Campbell LC, Pells JJ, Sims EL, Queen R, Carson JW, Connelly M, Dixon KE, Lacaille LJ, Huebner JL, Rejeski WJ, Keefe FJ. Pain coping skills training and lifestyle behavioral weight management in patients with knee osteoarthritis: a randomized controlled study. Pain. 2012;153:1199–1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. [DOI] [PubMed] [Google Scholar]
- 37.Stratford PW, Kennedy DM. Performance measures were necessary to obtain a complete picture of osteoarthritic patients. J Clin Epidemiol. 2006;59:160–167. [DOI] [PubMed] [Google Scholar]
- 38.Sullivan M, Tanzer M, Stanish W, Fallaha M, Keefe FJ, Simmonds M, Dunbar M. Psychological determinants of problematic outcomes following total knee arthroplasty. Pain. 2009;143:123–129. [DOI] [PubMed] [Google Scholar]
- 39.Sullivan MJL, Bishop S, Pivik J. The Pain Catastrophizing Scale: development and validation. Psych Assessment. 1995;7:524–532. [Google Scholar]
- 40.Tan G, Teo I, Anderson KO, Jensen MP. Adaptive versus maladaptive coping and beliefs and their relation to chronic pain adjustment. Clin J Pain. 2011;27:769–774. [DOI] [PubMed] [Google Scholar]
- 41.Taylor SS, Davis MC, Yeung EW, Zautra AJ, Tennen HA. Relations between adaptive and maladaptive pain cognitions and within-day pain exacerbations in individuals with fibromyalgia. J Behav Med. 2017;40:458–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Turner JA, Mancl L, Aaron LA. Short- and long-term efficacy of brief cognitive-behavioral therapy for patients with chronic temporomandibular disorder pain: a randomized, controlled trial. Pain. 2006;121:181–194. [DOI] [PubMed] [Google Scholar]
- 43.Vissers MM, Bussmann JB, Verhaar JA, Busschbach JJ, Bierma-Zeinstra SM, Reijman M. Psychological factors affecting the outcome of total hip and knee arthroplasty: a systematic review. Semin Arthritis Rheum. 2012;41:576–588. [DOI] [PubMed] [Google Scholar]