Abstract
Background
Symptom intensity and magnitude of limitations correlate with stress, distress, and less effective coping strategies. It is unclear if interventions to target these factors can be used to improve outcomes after distal radius fracture in either the short- or longer term.
Questions/purposes
(1) Are there any factors (including the use of a workbook aimed at optimizing psychological response to injury, demographic, radiographic, medical, or psychosocial) associated with improved Disabilities of the Arm, Shoulder and Hand (DASH) and Numerical Rating Scale pain (NRS pain) scores at 6 weeks after management of distal radius fracture? (2) Are any of these factors associated with improved DASH and NRS pain scores at 6 months after management of distal radius fracture?
Methods
We conducted a double-blind randomized controlled trial comparing a workbook designed to optimize rehabilitation by improving psychological response to injury using recognized psychological techniques (the LEARN technique and goal setting) versus a workbook containing details of stretching exercises in the otherwise routine management of distal radius fracture. Patients older than 18 years of age with an isolated distal radius fracture were recruited within 3 weeks of injury from a single academic teaching hospital between March and August 2016. During recruitment, 191 patients who met the inclusion criteria were approached; 52 (27%) declined participation and 139 were enrolled. Eight patients (6%) were lost to followup by 6 weeks. The remaining cohort of 129 patients was included in the analysis. DASH scores and NRS pain scores were recorded at 6 weeks and 6 months after injury. Multivariable regression analysis was used to identify factors associated with outcome scores.
Results
At 6 weeks after distal radius fracture, when compared with an information-only workbook, use of a psychologic workbook was not associated with improved DASH (workbook DASH: 38 [range, 21-48]; control DASH: 35 [range, 21-53]; difference of medians: 3; p = 0.949) nor NRS pain scores (workbook NRS: 3 [range, 1-5]; control NRS: 2 [range, 1-4]; difference of medians: 1; p = 0.128). Improved DASH scores were associated with less radial shortening (β = 0.2, p = 0.009), less dorsal tilt (β = 0.2, p = 0.035), and nonoperative treatment (β = 0.2, p = 0.027). Improved NRS pain scores were associated with nonoperative treatment (β = 0.2, p = 0.021) and no posttraumatic stress disorder (PTSD) (β = 0.2, p = 0.046). At 6 months, use of a psychologic workbook was not associated with improved DASH (workbook DASH: 11 [range, 5-28]; control DASH: 11 [range, 3-20]; difference of medians: 0; p = 0.367) nor NRS pain scores (workbook NRS: 1 [range, 0-2]; control NRS: 1 [range, 0-2]; difference of medians: 0; p = 0.704). Improved DASH score at 6 months was associated with having fewer medical comorbidities (β = 0.3, p < 0.001) and lower enrollment PTSD (β = 0.3, p < 0.011). Lower NRS pain scores at 6 months were associated with having fewer medical comorbidities (β = 0.2, p = 0.045), lower enrollment PTSD (β = 0.3, p = 0.008), and lower enrollment Tampa Scale for Kinesiophobia (β = 0.2, p = 0.042).
Conclusions
Our study demonstrates that there is no benefit from the untargeted use of a psychological workbook based on the LEARN approach and goal-setting strategies in patients with distal radius fracture. Future research should investigate if there is a subgroup of patients with a negative psychological response to injury that benefits from psychological intervention and, if so, how best to identify these patients and intervene.
Level of Evidence
Level II, therapeutic study.
Introduction
Distal radius fracture is a common injury. The majority of people recover well but a proportion have ongoing pain, stiffness, and functional limitation. Associations between these functional outcomes and injury characteristics, treatment methods, and radiographic outcomes are inconsistent. A deformed wrist is not always painful, stiff, and functionally limiting.
Patient stress, distress, and suboptimal coping strategies are associated with greater symptom intensity and magnitude of limitations in a variety of health conditions. Interventions that target psychologic factors improve outcomes for back pain, osteoarthritis, and myocardial infarction [7, 8, 19, 25, 45, 54]. However, the evidence regarding psychologic interventions after acute injury is limited.
The effectiveness of psychologic interventions is primarily mediated by their influence on self-efficacy: an individual’s confidence in their ability to perform a given behavior (eg, engagement with rehabilitation, performance of exercises, use of their arm, etc). Increased self-efficacy is associated with improved pain, disability, and functional outcome in a number of musculoskeletal conditions [14, 38, 46, 59]. The LEARN approach describes a stepwise method to affect change in self-efficacy: LEARN: L = learn exercise/activity; E = encourage or cue; A = address unpleasant symptoms; R = reinforcement from other’s experience/role model; and n = negate disability (say no to inability/promote confidence and a positive mindset; Fig. 1). It has been suggested as a template for developing interventions for use in distal radius fracture [15].
Fig. 1.
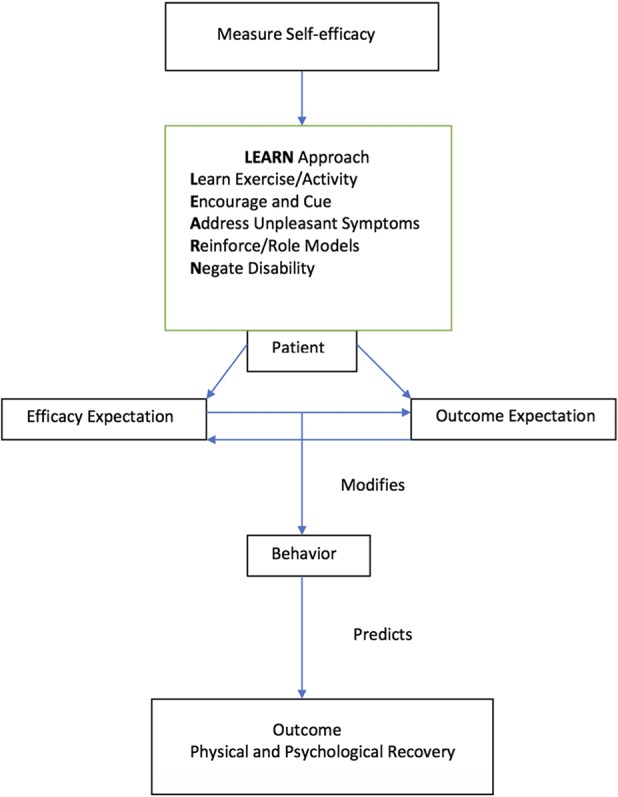
Diagram illustrating the LEARN approach to modifying self-efficacy.
There is potential for interventions that target psychologic factors such as self-efficacy to supplement routine orthopaedic care and improve outcomes. We developed and tested a psychologic workbook, which encompassed the LEARN approach, to supplement routine treatment of distal radius fractures in a fracture clinic setting. We wanted to assess the impact of such intervention on both short- and longer term recovery.
Study Questions
(1) Are there any factors (including the use of a workbook aimed at optimizing psychological response to injury, demographic, radiographic, medical, or psychosocial) associated with improved Disabilities of the Arm, Shoulder and Hand (DASH) and Numerical Rating Scale pain (NRS pain) scores at 6 weeks after management of distal radius fracture? (2) Are any of these factors associated with improved DASH and NRS pain scores at 6 months after management of distal radius fracture?
Patients and Methods
We conducted a double-blind randomized controlled trial comparing a psychologic workbook with an information-only workbook in the otherwise routine treatment of distal radius fracture. Patients were recruited from a single academic teaching hospital between March 2016 and August 2016 and followed up at 6 weeks and 6 months. The study population was inclusive because the treating hospital is the sole provider of orthopaedic care for the region. Ethical and clinical trial committees approved and authorized the work.
Patients with distal radius fracture were identified on presentation to the orthopaedic clinic. Diagnosis was made based on the presence of disruption of cortical bone in the distal one-third of the radius on radiographs of the wrist. The inclusion criteria were age 18 years and older; patients with isolated distal radius fracture undergoing management with manipulation and cast/cast alone/operative management; and recruitment within 3 weeks of injury. Exclusion criteria were cognitive impairment preventing informed consent or completion of questionnaires; non-English-speaking; open fracture; temporary residents unable to attend followup; patients with multiple fractures; undertaking injury compensation proceedings; illicit drug use; and a psychiatric diagnosis resulting in psychosis.
Fracture treatment was in line with hospital policy and independent from the study. After randomization, the patient was given a workbook and instructed on how to use it. Randomization was stratified based on age (older than 65 years:65 years and younger), gender (male:female), and treatment (operative:nonoperative). Patients were assigned to a group (A-H) based on these three criteria. Block randomization was then carried out within each group using a computer-generated sequence.
Study Intervention: Psychologic Workbook
The psychologic workbook was designed using the LEARN approach to change beliefs and behavior by improving self-efficacy (Fig. 1). The workbook comprised two parts: an information section and a goal diary. The book described exercises and activities that patients could undertake from the time of injury (L: learn exercises/activities). A progress diary was used to encourage progress (E: encourage and cue). Information regarding expectations, healthy eating, stretching exercises, pain management, stress reduction, and improving sleep was used to address unpleasant symptoms (A: address unpleasant symptoms) and was reinforced by describing the experiences of fictional patients in vignettes (R: reinforcement/role models). The book aimed to negate disability (N: negate disability) by using activities to focus on what individual patients were able to do rather than their activity limitations. Pain was normalized and safe movement encouraged at every opportunity.
The goal diary was designed to engage patients with all five components of the LEARN model through the inclusion of specific behavior change techniques [35]. It asked patients to set and write down three personal recovery goals specific to their lifestyle that they would work toward over a 6-week period. It then took the patient through planning a step-by-step approach to achieving these goals by utilizing learned activities described in the instructional book. It facilitated a weekly review of progress and allowed modification of the strategy if required.
Study Control: Information-only Workbook
Patients randomized into the control group received an information-only workbook. The information-only workbook contained details of a number of hand and wrist stretching exercises and advised the patient to begin work on these three times per day as soon as they felt able. Of note, these exercises were also included in the psychologic workbook. Both the psychologic intervention workbook and the information-only control workbook had matching covers to aid in blinding. Both treatment groups followed the same followup schedule and the guidelines for clinical care were the same in each group.
Patient Assessment and Outcome Measures
Demographic details, medical and psychiatric history, baseline radiographic parameters (radiocarpal alignment, dorsal tilt, radial shortening), injury and treatment characteristics, and psychologic scores (General Self-efficacy Scale [GSES], Pain Catastrophising Scale [PCS], Tampa Scale for Kinesiophobia [TSK], Hospital Anxiety and Depression Scale [HADS], Post Trauma Stress Disorder Civilian Checklist [PCL-C], Illness Perception Questionnaire–Revised [IPQR], Recovery Locus of Control [RLOC]) were measured at enrollment.
Six weeks after injury radiographic parameters, GSES, and patient-reported outcome measures (DASH score, NRS pain score, and SF-12) were measured.
Six months after injury, we measured wrist and finger motion and grip strength, recorded adverse events, and repeated GSES and outcome measures.
All measurements were taken by researchers not involved in the routine management of these patients and blinded to patient treatment group.
Assessment Tools
The GSES is a widely used 10-item measure of self-efficacy. Each item is scored from 1 to 4 giving a total score between 10 and 40 (10 low:40 high). It is used to assess self-confidence in ability to cope with difficult situations (perceived self-efficacy) [23, 48].
The PCS [50] is a 13-item measure of catastrophic thinking. Each item asks about the degree of agreement with a statement representative of catastrophic thinking; each item is scored 0 to 4, giving a total score between 0 and 52. Higher scores reflect higher levels of catastrophic thinking.
The TSK [27] is a 17-item measure of fear of movement associated with pain or reinjury. Each item is scored between 1 and 4, giving a scale range of 17 to 68; higher scores represent greater fear avoidance behavior.
Depression and anxiety were measured separately by the 14-item HADS [60]. Seven items measure each of depression and anxiety; items are scored 0 to 3, generating a total score between 0 and 21 for each (higher scores indicating more anxiety and depression). The HADS is designed to measure both facets of mood free from confounding with somatic symptoms.
The PCL-C is a 17-item measure of posttraumatic stress disorder (PTSD) symptoms based on the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition. Each question has five response options rated 1 to 5 giving a total score between 17 (low) and 85 (high). It is commonly used, valid, and reliable [13, 20]. To diagnose PTSD, symptoms must persist for > 3 months, but in the acute setting, the PCL-C can be used as an indicator of psychologic distress.
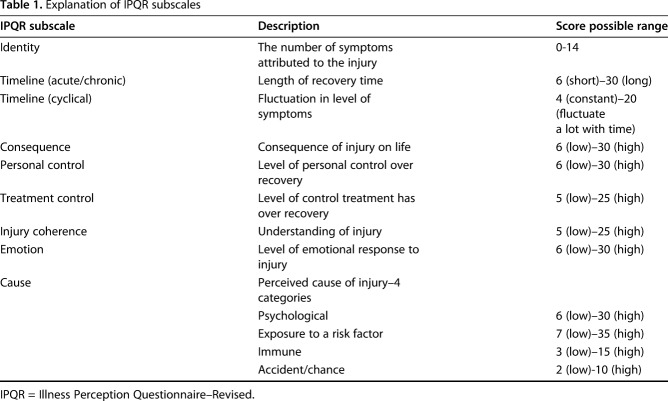
The IPQR is a nine-item measure of a patient’s perceptions of their illness/injury. Each item is assessed with a number of questions and is scored individually (Table 1) [29].
Table 1.
Explanation of IPQR subscales
The RLOC is designed to evaluate an individual’s beliefs about the control they have over recovery from a traumatic event [44]. It is comprised of nine items each scored 1 to 5, giving a total score range of 9 (high external locus) to 45 (high internal locus). “High external locus” refers to a belief that recovery is dependent on external factors with the patient’s own control in contrast to “high internal locus,” which refers to a mindset in which patients believe they have control over the recovery from and outcome of their injury. All scores used have been shown to be reliable and valid in populations similar to ours [2, 9, 17, 18, 22, 32, 36, 37, 41, 43, 43, 44, 51, 55].
The DASH score is responsive, reliable, and valid in patients with distal radius fracture and is widely used to assess outcomes in this group [26, 32]. It comprises 30 questions converted to a score out of 100 with a higher score representing greater disability [10, 21]. The NRS pain score was used to assess average pain intensity over the preceding week measured on an 11-point Likert scale from 0 (no pain) to 10 (worst pain imaginable).
All radiographic assessment was carried out by a single member of the research team (SG) using a picture archiving and communication system (Carestream, Version 11.40.1253; Carestream Health, Rochester, NY, USA). Posteroanterior (PA) and lateral radiographs of the wrist were taken in the standard manner. Carpal alignment was assessed on the lateral view by drawing a line along the long axis of the capitate and another along the long axis of the radius. If the lines intersected within the carpus, then radiocarpal alignment was maintained [34]. Ulnar variance (used as a measure of radial shortening) was measured on the PA view as the distance between two lines perpendicular to the long axis of the radius, one at the level of the radial articular surface and another at the distal end of the ulna [39]. Tilt was measured on the lateral view as the angle between a line perpendicular to the long axis of the radius and a line joining the most distal points of the volar and dorsal lips of the distal radius. Dorsal tilt was recorded as positive values and volar tilt as negative values [39]. Grip strength on both the injured and uninjured sides was measured in kilograms with a standard, adjustable handle Jamar dynamometer (Sammons Preston Rolyan, Bolingbrook, IL, USA) set to the second rung position, the optimal setting for measuring grip strength with this instrument [53], the elbow at 90° flexion, and the forearm in neutral rotation. The mean of three recordings was calculated and recorded as a percentage deficit relative to the strength of the contralateral hand. The deficit was adjusted to allow for dominance with a 10% increase in grip strength assumed for the dominant hand. The distance from the index fingernail tip to the palmar skin crease during maximal flexion was measured with a ruler in millimeters.
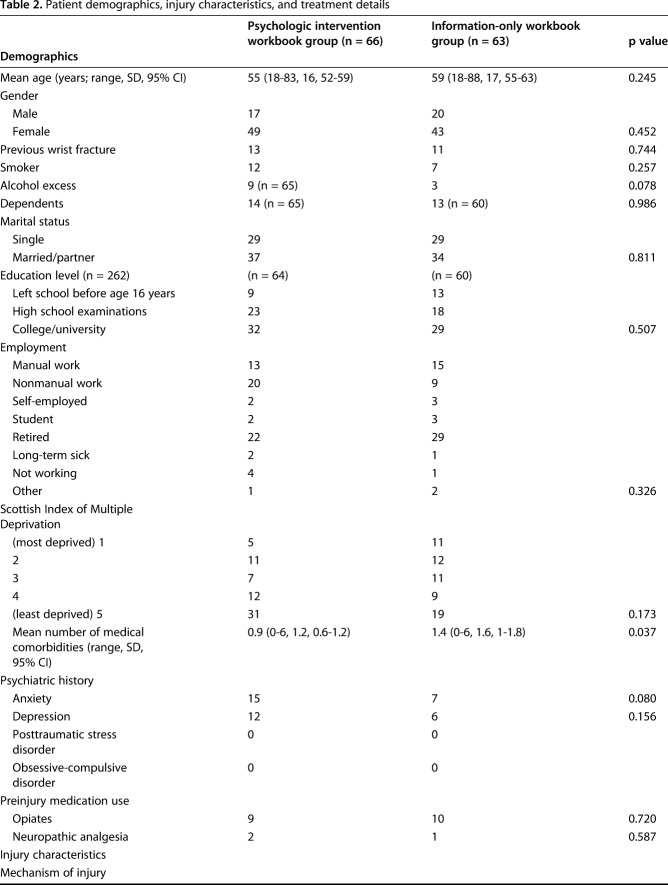
Patients
During recruitment, 191 patients who met the inclusion criteria were approached; 52 (27%) declined participation and 139 were enrolled. All 74 (100%) patients randomized to the psychologic workbook and 63 of 65 (97%) of patients randomized to the information-only workbook were given allocated treatment. Eight patients (6%) were lost to followup by 6 weeks. The remaining cohort of 129 patients was included in the analysis (66 in the psychologic workbook group and 63 in the information-only workbook group; Fig. 2).
Fig. 2.
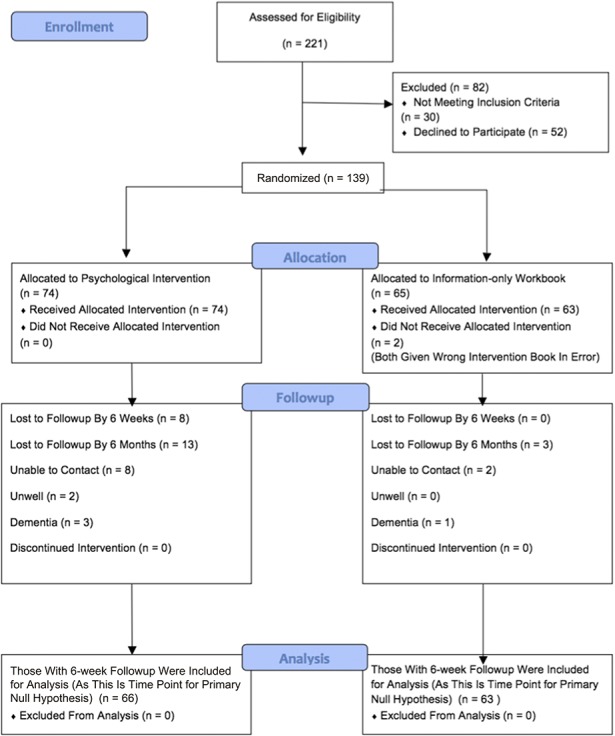
Flow diagram shows patients recruited to the trial.
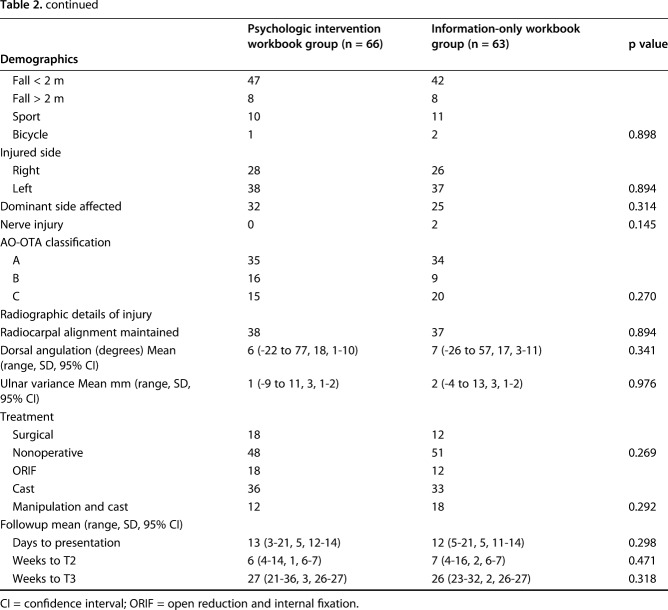
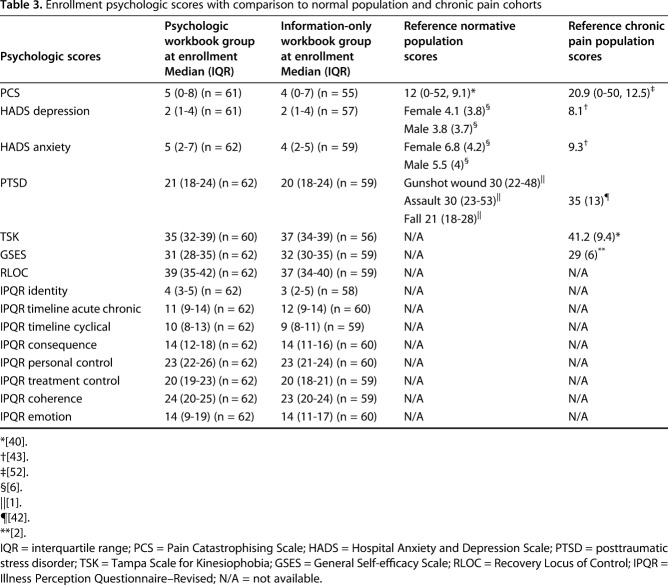
Demographics, injury and radiographic characteristics, treatment details, and enrollment psychologic scores in each treatment group were similar (Tables 2, 3). The enrollment psychologic scores of our study population were better than recognized population normal values (Table 3).
Table 2.
Patient demographics, injury characteristics, and treatment details
Table 3.
Enrollment psychologic scores with comparison to normal population and chronic pain cohorts
Statistical Analysis
The primary outcome measure was the DASH score. In a pilot study of 60 patients with distal radius fracture who were evaluated 8 weeks after injury, mean DASH score was 29 (SD 19). A sample size of 126 was estimated to provide power (90%) to identify a minimum difference between the psychologic workbook and the information-only workbook of 10 points (the recognized minimal clinically significant difference in DASH) with α set at 0.05. We anticipated a dropout rate of 10% and therefore aimed to enroll 139 patients.
Descriptive statistics were used to present demographic, comorbidity, injury, treatment, radiographic, and enrollment psychologic characteristics. We adhered to intention-to-treat principles. The response variables were DASH score and NRS pain score at 6 weeks and 6 months and grip strength at 6 months. The explanatory variables were age; number of medical comorbidities; Scottish Index of Multiple Deprivation quintile; injury to the dominant side; AO-OTA fracture group (A, B, or C); nerve injury; radiographic alignment at 6 weeks (radiocarpal alignment, radial shortening, dorsal tilt); surgical or nonoperative management; time to presentation and followup; psychologic measures (HADS, PCS, TSK, PCL-C, GSES, IPQR personal control, IPQR emotion, and RLOC); and workbook assignment. In bivariate analysis, outcomes were compared using median scores and Mann-Whitney U tests for nonparametric data and mean scores and independent-sample t-tests for parametric data. Missing data were completed with mean imputation. Spearman correlations, Mann-Whitney U tests, and Kruskal-Wallis tests were used for nonparametric data and Pearson correlations, t-tests, and analysis of variance for parametric data. Factors with p < 0.1 in bivariate analysis were entered into multivariable linear regression models to determine factors independently associated with each response variable. Where there was a correlation of > 0.7 between factors, the least clinically relevant was dropped from the model. We created three subgroups of patients based on recognized threshold scores on the enrollment psychologic scores (GSES < cohort median – 1 interquartile range, PCS > 16, HADS depression ≥ 8).
Results
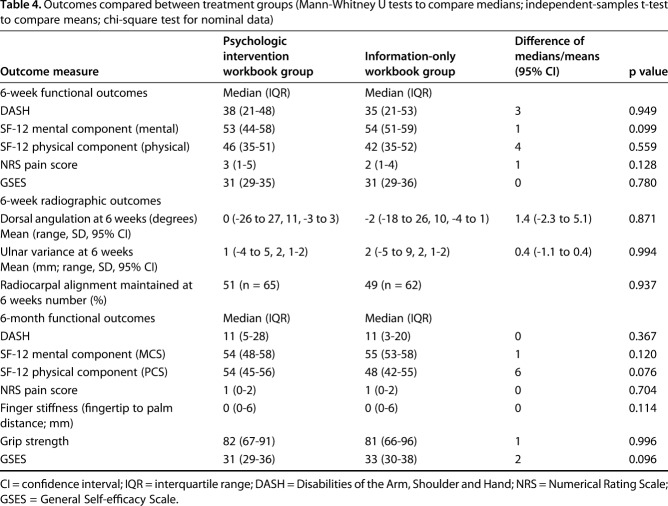
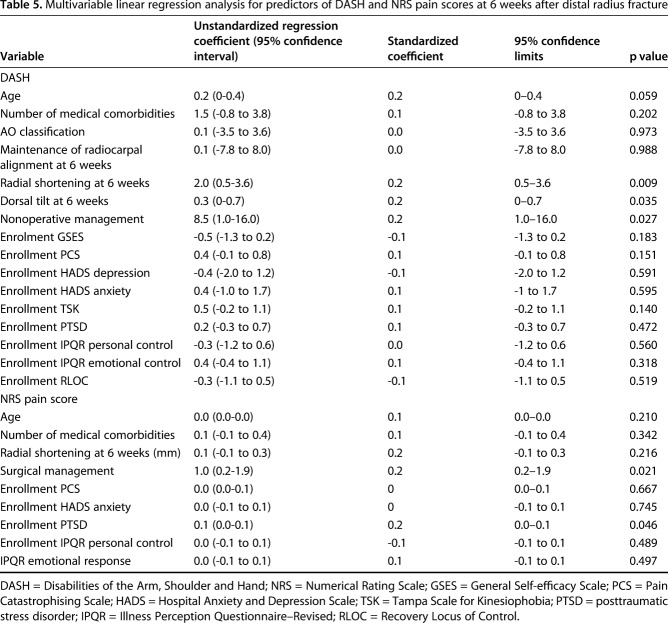
Six weeks after distal radius fracture, use of a psychological workbook was not associated with improved DASH (psychological workbook DASH: 38 [range, 21-48]; control DASH: 35 [range, 21-53]; difference of medians: 3; p = 0.949) nor NRS pain score (psychological workbook NRS pain score: 3 [range, 1-5]; control NRS pain score: 2 [range, 1-4]; difference of medians: 1; p = 0.128) when compared with the information-only workbook (Table 4). However, improved DASH scores were associated with less radial shortening (β = 0.2, p = 0.009), less dorsal tilt (β = 0.2, p = 0.035), and nonoperative treatment (β = 0.2, p = 0.027) and improved NRS pain score was associated with nonoperative treatment (β = 0.2, p = 0.021) and lower enrollment PTSD score (β = 0.2, p = 0.046) (Table 5).
Table 4.
Outcomes compared between treatment groups (Mann-Whitney U tests to compare medians; independent-samples t-test to compare means; chi-square test for nominal data)
Table 5.
Multivariable linear regression analysis for predictors of DASH and NRS pain scores at 6 weeks after distal radius fracture
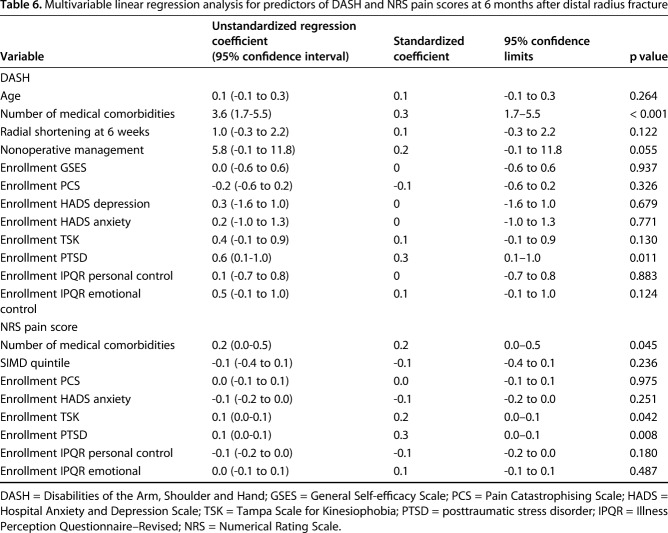
At 6 months, use of a psychological workbook was not associated with improved DASH (psychological workbook DASH score: 11 [range, 5-28]; control DASH score: 11 [range, 3-20]; difference of medians: 0; p = 0.367) nor NRS (psychological workbook NRS pain score: 1 [range, 0-2]; control NRS pain score: 1 [range, 0-2]; difference of medians: 0; p = 0.704) when compared with the information-only workbook (Table 4). However, improved DASH score was associated with having fewer medical comorbidities (β = 0.3, p < 0.001) and lower enrollment PTSD (β = 0.3, p = 0.011) and improved NRS pain score was associated with having fewer medical comorbidities (β = 0.2, p = 0.045), lower enrollment PTSD score (β = 0.3, p = 0.008), and lower enrollment TSK score (β = 0.2, p = 0.042) (Table 6).
Table 6.
Multivariable linear regression analysis for predictors of DASH and NRS pain scores at 6 months after distal radius fracture
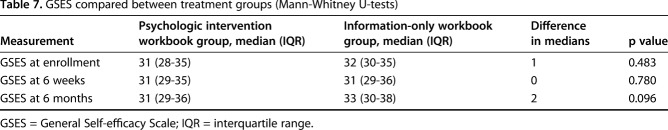
GSES did not differ between treatment groups at any time point (Table 7). As a result of the small number of cases in each subgroup, this could not be statistically analyzed.
Table 7.
GSES compared between treatment groups (Mann-Whitney U-tests)
Discussion
Self-efficacy is associated with recovery after acute orthopaedic trauma [4, 5, 11]. Psychologic interventions to teach effective coping strategies and change perceptions are associated with increased self-efficacy [33, 54] and reduced disability in musculoskeletal conditions [33]. This study represents an attempt to improve outcomes after fracture of the distal radius by bolstering self-efficacy using a LEARN approach [15]. We found that the use of a psychological workbook in addition to routine treatment of distal radius fracture did not reduce disability or symptom intensity compared with an information-only workbook in an inclusive cohort of patients with distal radius fracture whose baseline level of psychological distress was generally low.
This study had a number of limitations. First, patients were only followed up for 6 months. Patients can continue to improve for a year after injury, but we focused on early recovery because level of disability is most varied in this time period. Second, for unclear reasons, the psychologic workbook group had more patients from higher socioeconomic quintiles (less social deprivation) and more patients with a preinjury diagnosis of anxiety and depression. Stratified randomization was used to evenly distribute treatment type, age, and gender between the two treatment groups. Third, results should be extrapolated to other trauma populations with caution. The association among fracture site, injury severity, and psychological response to injury is unclear [3, 49, 56]. Psychological response may vary between patient groups with different fractures and severity of injury; thus, the utility of a psychological intervention may differ in these patient groups. Finally, we did not quantify engagement (how much time patients spent using workbooks); this was because this was an effectiveness rather than efficacy trial (the aim was to assess the intervention in a “real” fracture clinic setting rather than under “ideal” test conditions).
The use of a psychological workbook did not reduce short-term (6-week) disability or symptom intensity after distal radius fracture. The enrollment factors associated with outcome at this time point were radial shortening and dorsal tilt at 6 weeks and nonoperative management and level of psychological distress at enrollment. The limited associations between psychological factors and function and absence of improvement with the psychological workbook were unexpected in the context of other work. Prior studies found correlations of magnitude of limitations and symptom intensity with psychologic factors among patients recovering from distal radius fracture [30, 47]. There is work demonstrating that psychologic response to acute injury can be modified [28] and that goal-setting exercises can be effective [16]. A recent pilot randomized controlled trial in patients with acute musculoskeletal trauma demonstrated that disability, pain, and psychologic response to injury could be improved with psychological intervention [58]. This study differed from ours in a number of ways. The intervention in the pilot study was delivered face to face rather than in a workbook. However, there is evidence that interventions delivered remotely can be effective [8, 24]. Being a pilot study, it was underpowered; it also had a high attrition rate (50%) in the control group, which did not have a placebo intervention. Most importantly, the pilot study only included patients with high enrollment levels of depression and pain anxiety, whereas our study did not set inclusion criteria based on enrollment psychologic scores. Studies of psychological intervention in patients with back pain have shown that intervention is most effective in patients with poorer coping strategies [19, 25, 31]. Perhaps the psychological intervention would have been more effective if targeted to patients with relatively low self-efficacy or high levels of stress or distress. The association between surgical management and increased pain at 6 weeks is surprising because regardless of treatment method, the fracture should have united by this time and in the case of surgical management, the surgical wounds should have healed, creating a similar biomedical environment in both cases.
The use of a psychological workbook did not reduce longer term (6-month) disability or symptom intensity after distal radius fracture. The only enrollment factors associated with level of disability at this time were psychological distress and number of underlying medical comorbidities and the only factors associated with symptom intensity were kinesophobia, psychological distress, and number of underlying medical comorbidities. In a study of a mixed trauma population, high catastrophic thinking rather than psychologic distress was associated with higher disability at this time [57]. In other cohorts of patients who have undergone orthopaedic trauma, associations between psychologic distress and pain have been demonstrated [12], but fear and anxiety constructs (TSK) have been associated with disability rather than pain [57]. These results suggest that as time from injury increases, the influence of unrelated medical problems and psychosocial factors increases. It also highlights the difficulty identifying one single psychological scoring system that can reproducibly be associated with outcome that could be used to screen for patients with a negative response to injury.
Our study demonstrates that there is no benefit from the untargeted use of a psychological workbook based on the LEARN approach and goal-setting strategies in patients with distal radius fracture. Future research should investigate if there is a subgroup of patients with a negative psychological response to injury that benefit from psychological intervention and, if so, how best to identify these patients and intervene.
Acknowledgments
We acknowledge the statistical advice given by Dr Stephen Corson of the University of Strathclyde and thank all staff at the Scottish Orthopaedic Research Trust into Trauma (SORTiT) for their support and assistance with this study.
Footnotes
One of the authors (SG) has received funding from the Scottish Orthopaedic Research Trust into Trauma; he undertook this research during his term of employment. One of the authors (DR) has received grants from Skeletal Dynamics (Miami, FL, USA), other from Wright Medical (Memphis, TN, USA), personal fees from Biomet (Warsaw, IN, USA), personal fees from Acumed (Portland, OR, USA), other from Illuminos (Providence, RI, USA), personal fees as Deputy Editor for the Journal of Hand Surgery, personal fees as Deputy Editor for Clinical Orthopaedics and Related Research®, personal fees from universities and hospitals, and personal fees from lawyers, outside the submitted work.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
ClinicalTrial.gov registration number: NCT02720055
This work was performed at Royal Infirmary Edinburgh, Edinburgh, UK.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
References
- 1.Alarcon LH, Germain A, Clontz AS, Roach E, Nicholas DH, Zenati MS, Peitzman AB, Perry JL. Predictors of acute posttraumatic stress disorder symptoms following civilian trauma: highest incidence and severity of symptoms after assault. J Trauma Acute Care Surg. 2012;72:629. [DOI] [PubMed] [Google Scholar]
- 2.Barlow JH, Williams B, Wright C. The Generalized Self-Efficacy Scale in people with arthritis. Arthritis Care Res. 1996;9:189–196. [DOI] [PubMed] [Google Scholar]
- 3.Becher S, Smith M, Ziran B. Orthopaedic trauma patients and depression: a prospective cohort. J Orthop Trauma. 2014;28:e242–246. [DOI] [PubMed] [Google Scholar]
- 4.Bosse MJ, MacKenzie EJ, Kellam JF, Burgess AR, Webb LX, Swiontkowski MF, Sanders RW, Jones AL, McAndrew MP, Patterson BM, McCarthy ML, Travison TG, Castillo RC. An analysis of outcomes of reconstruction or amputation after leg- threatening injuries. N Engl J Med. 2002;347:1924–1931. [DOI] [PubMed] [Google Scholar]
- 5.Bot AGJ. Bekkers S, Herndon JH, Mudgal CS, Jupiter JB, Ring D. Determinants of disability after proximal interphalangeal joint sprain or dislocation. Psychosomatics. 2014;55:595–601. [DOI] [PubMed] [Google Scholar]
- 6.Breeman S, Cotton S, Fielding S, Jones GT. Normative data for the Hospital Anxiety and Depression Scale. Qual Life Res. 2015;24:391–398. [DOI] [PubMed] [Google Scholar]
- 7.Broadbent E, Ellis CJ, Thomas J, Gamble G, Petrie KJ. Further development of an illness perception intervention for myocardial infarction patients: a randomized controlled trial. J Psychosom Res. 2009;67:17–23. [DOI] [PubMed] [Google Scholar]
- 8.Burton AK, Waddell G, Tillotson KM, Summerton N. Information and advice to patients with back pain can have a positive effect. A randomized controlled trial of a novel educational booklet in primary care. Spine. 1999;24:2484. [DOI] [PubMed] [Google Scholar]
- 9.Burwinkle T, Robinson JP, Turk DC. Fear of movement: factor structure of the Tampa Scale of Kinesiophobia in patients with fibromyalgia syndrome. J Pain. 2005;6:384–391. [DOI] [PubMed] [Google Scholar]
- 10.Changulani M, Okonkwo U, Keswani T, Kalairajah Y. Outcome evaluation measures for wrist and hand—which one to choose? Int Orthop. 2008;32:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clay FJ, Newstead SV, McClure RJ. A systematic review of early prognostic factors for return to work following acute orthopaedic trauma. Injury. 2010;41:787–803. [DOI] [PubMed] [Google Scholar]
- 12.Clay FJ, Newstead SV, Watson WL, Ozanne-Smith J, Guy J, McClure RJ. Bio- psychosocial determinants of persistent pain 6 months after non-life-threatening acute orthopaedic trauma. J Pain. 2010;11:420–430. [DOI] [PubMed] [Google Scholar]
- 13.Conybeare D, Behar E, Solomon A, Newman MG, Borkovec TD. The PTSD Checklist—Civilian Version: reliability, validity, and factor structure in a nonclinical sample. J Clin Psychol. 2012;68:699–713. [DOI] [PubMed] [Google Scholar]
- 14.Costa Lda C, Maher CG, McAuley JH, Hancock MJ, Smeets RJ. Self-efficacy is more important than fear of movement in mediating the relationship between pain and disability in chronic low back pain. Eur J Pain. 2011;15:213–219. [DOI] [PubMed] [Google Scholar]
- 15.Dewan NJ, MacDermid C, Packham T. Role of self-efficacy based model of intervention: learn approach in rehabilitation of distal radius fracture. J Clin Densitom. 2014;17:428–429. [Google Scholar]
- 16.Evans L, Hardy L. Injury rehabilitation: a goal-setting intervention study. Res Q Exerc Sport. 2002;73:310–319. [DOI] [PubMed] [Google Scholar]
- 17.Feldman CH, Dong Y, Katz JN, Donnell-Fink LA, Losina E. Association between socioeconomic status and pain, function and pain catastrophizing at presentation for total knee arthroplasty. BMC Musculoskelet Disord. 2015;16:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.French DJ, France CR, Vigneau F, French JA, Evans RT. Fear of movement/(re)injury in chronic pain: a psychometric assessment of the original English version of the Tampa Scale for Kinesiophobia (TSK). Pain. 2007;127:42–51. [DOI] [PubMed] [Google Scholar]
- 19.George SZ, Fritz JM, Bialosky JE, Donald DA. The effect of a fear-avoidance- based physical therapy intervention for patients with acute low back pain: results of a randomized clinical trial. Spine. 2003;28:2551. [DOI] [PubMed] [Google Scholar]
- 20.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351:13–22. [DOI] [PubMed] [Google Scholar]
- 21.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder and Hand) corrected. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29:602. [DOI] [PubMed] [Google Scholar]
- 22.Hung M, Bounsanga J, Tang P, Chen W, Cheng C. The factor structure of the hospital anxiety and depression scale in orthopedic trauma patients. J Clin Med Res. 2015;7:453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jerusalem M, Schwarzer R. Self-efficacy as a resource factor in stress appraisal processes. In: Schwartzer R, ed. Self-efficacy: Thought Control of Action. Washington, DC, USA: Hemisphere; 1992:195–213. [Google Scholar]
- 24.Johnston M, Bonetti D, Joice S, Pollard B, Morrison V, Francis JJ, Macwalter R. Recovery from disability after stroke as a target for a behavioural intervention: results of a randomized controlled trial. Disabil Rehabil. 2007;29:1117–1127. [DOI] [PubMed] [Google Scholar]
- 25.Klaber Moffett JA, Carr J, Howarth E. High fear-avoiders of physical activity benefit from an exercise program for patients with back pain. Spine. 2004;29:1167. [DOI] [PubMed] [Google Scholar]
- 26.Kleinlugtenbelt YV, Nienhuis RW, Bhandari M, Goslings JC, Poolman RW, Scholtes VAB. Are validated outcome measures used in distal radial fractures truly valid? A critical assessment using the Consensus-based Standards for the selection of health Measurement Instruments (COSMIN) checklist. Bone Joint Res. 2016;5:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kori SH, Todd DD. Kinesophobia: a new view of chronic pain behavior. Pain Management. 1990;3:35–43. [Google Scholar]
- 28.Lee BO, Chien CS, Hung CC, Chou PL. Effects of an in-hospital nursing intervention on changing illness perceptions in patients with injury. J Adv Nurs. 2015;71:2540–2550. [DOI] [PubMed] [Google Scholar]
- 29.Leventhal H, Nerenz DR, Steele DJ. Illness representations and coping with health threats. In: Baum A, Taylor SE, Singer JE, eds. Handbook of Psychology and Health. Hillsdale, NJ, USA: Erlbaum; 1984:219–252. [Google Scholar]
- 30.Linton SJ, Buer N, Samuelsson L, Harms-Ringdahl K. Pain-related fear, catastrophizing and pain in the recovery from a fracture. Scand J Pain. 2012;1:38–42. [DOI] [PubMed] [Google Scholar]
- 31.Little P, Roberts L, Blowers H, Garwood J, Cantrell T, Langridge J, Chapman J. Should we give detailed advice and information booklets to patients with back pain? A randomised controlled factorial trial of a self-management booklet and doctor advice to take exercise for back pain. Spine. 2001;4:69–70. [DOI] [PubMed] [Google Scholar]
- 32.Lvgren A, Hellstrom K. Reliability and validity of measurement and associations between disability and behavioural factors in patients with Colles fracture. Physiother Theory Pract. 2012;28:188–197. [DOI] [PubMed] [Google Scholar]
- 33.Maddison R, Prapavessis H, Clatworthy M. Modeling and rehabilitation following anterior cruciate ligament reconstruction. Ann Behav Med. 2006;31:89–98. [DOI] [PubMed] [Google Scholar]
- 34.McQueen MM, Hajducka C, Court-Brown CM. Redisplaced unstable fractures of the distal radius: a prospective randomised comparison of four methods of treatment. J Bone Joint Surg Br. 1996;78:404–409. [PubMed] [Google Scholar]
- 35.Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46:81–95. [DOI] [PubMed] [Google Scholar]
- 36.Michopoulos I, Douzenis A, Kalkavoura C, Christodoulou C, Michalopoulou P, Kalemi G, Fineti K, Patapis P, Protopapas K, Lykouras L. Hospital Anxiety and Depression Scale (HADS): validation in a Greek general hospital sample. Ann Gen Psychiatry. 2008;7:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mounce C, Keogh E, Eccleston C. A principal components analysis of negative affect-related constructs relevant to pain: evidence for a three component structure. J Pain. 2010;11:710–717. [DOI] [PubMed] [Google Scholar]
- 38.Nahm ES, Barker B, Resnick B, Covington B, Magaziner J, Brennan PF. Effects of a social cognitive theory-based hip fracture prevention web site for older adults. Comput Inform Nurs. 2010;28:371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ng CY, McQueen MM. What are the radiological predictors of functional outcome following fractures of the distal radius? J Bone Joint Surg Br. 2011;93:145. [DOI] [PubMed] [Google Scholar]
- 40.Nicholas MK, Asghari A, Blyth FM. What do the numbers mean? Normative data in chronic pain measures. Pain. 2008;134:158–173. [DOI] [PubMed] [Google Scholar]
- 41.Osman A, Barrios F, Gutierrez P, Kopper B, Merrifield T, Grittmann L. The Pain Catastrophizing Scale: further psychometric evaluation with adult samples. J Behav Med. 2000;23:351–365. [DOI] [PubMed] [Google Scholar]
- 42.Pagé GM, Kleiman V, Asmundson GJG, Katz J. Structure of posttraumatic stress disorder symptoms in pain and pain-free patients scheduled for major surgery. J Pain. 2009;10:984–991. [DOI] [PubMed] [Google Scholar]
- 43.Pallant JF, Bailey CM. Assessment of the structure of the Hospital Anxiety and Depression Scale in musculoskeletal patients. Health Qual Life Outcomes. 2005;3:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Partridge C, Johnston M. Perceived control of recovery from physical disability: measurement and prediction. Br J Clin Psychol. 1989;28:53. [DOI] [PubMed] [Google Scholar]
- 45.Petrie KJ, Cameron LD, Ellis CJ, Buick D, Weinman J. Changing illness perceptions after myocardial infarction: an early intervention randomized controlled trial. Psychosom Med. 2002;64:580–586. [DOI] [PubMed] [Google Scholar]
- 46.Resnick B. Geriatric rehabilitation: the influence of efficacy beliefs and motivation. Rehabil Nurs. 2002;27:152. [DOI] [PubMed] [Google Scholar]
- 47.Roh YH, Lee BK, Noh JH, Oh JH, Gong HS, Baek GH. Effect of anxiety and catastrophic pain ideation on early recovery after surgery for distal radius fractures. J Hand Surg. 2014;39:2258–2264.e2. [DOI] [PubMed] [Google Scholar]
- 48.Schwartzer R, Jerusalem M. Generalized Self-Efficacy scale. In: Weinman J, Wright S, Johnston M, eds. Measures in Health Psychology: A User’s Portfolio. Causal and Control Beliefs. Windsor, UK: NFER-NELSON; 1995:35–37. [Google Scholar]
- 49.Starr AJ, Smith WR, Frawley WH, Borer DS, Morgan SJ, Reinert CM, Mendoza-Welch M. Symptoms of posttraumatic stress disorder after orthopaedic trauma. J Bone Joint Surg Am. 2004;86:1115. [DOI] [PubMed] [Google Scholar]
- 50.Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7:524–532. [Google Scholar]
- 51.Swinkels-Meewisse EJCM, Swinkels RAHM, Verbeek ALM, Vlaeyen JWS, Oostendorp RAB. Psychometric properties of the Tampa Scale for Kinesiophobia and the fear-avoidance beliefs questionnaire in acute low back pain. Man Ther. 2003;8:29–36. [DOI] [PubMed] [Google Scholar]
- 52.The Pain Catastrophising Scale User Manual. Available at: http://sullivan-painresearch.mcgill.ca/pdf/pcs/PCSManual_English.pdf. Accessed Jannuary 16, 2017.
- 53.Trampisch US, Franke J, Jedamzik N, Hinrichs T, Platen P. Optimal Jamar dynamometer handle position to assess maximal isometric hand grip strength in epidemiological studies. J Hand Surg. 2012;37:2368–2373. [DOI] [PubMed] [Google Scholar]
- 54.Trudeau KJ, Pujol LA, Das P, Mahapatra A, Wall R, Black RA, Zacharoff K. A randomized controlled trial of an online self-management program for adults with arthritis pain. J Behav Med. 2015;38:483–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Turk DC, Dworkin RH, Trudeau JJ, Benson C, Biondi DM, Katz NP, Kim M. Validation of the Hospital Anxiety and Depression Scale in patients with acute low back pain. J Pain. 2015;16:1012–1021. [DOI] [PubMed] [Google Scholar]
- 56.Vrahas MS, Crichlow RJ, Andres PL, Morrison SM, Haley SM. Depression in orthopaedic trauma patients. Prevalence and severity. J Bone Joint Surg Am. 2006;88:1927. [DOI] [PubMed] [Google Scholar]
- 57.Vranceanu A, Bachoura A, Weening A, Vrahas M, Smith RM, Ring D. Psychological factors predict disability and pain intensity after skeletal trauma. J Bone Joint Surg Am. 2014;96:e20. [DOI] [PubMed] [Google Scholar]
- 58.Vranceanu A, Hageman M, Strooker J, Ter Meulen D, Vrahas M, Ring D. A preliminary RCT of a mind body skills based intervention addressing mood and coping strategies in patients with acute orthopaedic trauma. Injury. 2015;46:552–557. [DOI] [PubMed] [Google Scholar]
- 59.Yip YB, Sit JWH, Fung KKY, Wong DYS, Chong SYC, Chung LH, Ng TP. Effects of a self-management arthritis programme with an added exercise component for osteoarthritic knee: randomized controlled trial. J Adv Nurs. 2007;59:20–28. [DOI] [PubMed] [Google Scholar]
- 60.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psych Scand. 1983;67:361–370. [DOI] [PubMed] [Google Scholar]