Introduction
Central nervous system metastases are the most common adult tumors, frequently arising from primary tumors in the lung, breast, kidneys, and finally colon. They account for 13–39% of intracranial tumors. Transitional and urothelial cell carcinoma is a rare cause of brain metastasis with an ominous prognosis. Majority of the reported cases of intracranial metastasis from these lesions originated from bladder and upper urinary tract.
Here, we report a rare case of papillary urothelial carcinoma with Central nervous system metastasis. The patient recovered well after resection of brain lesion. The optimal method for the treatment of such metastasis in patients will also be discussed in this case report.
Case report
It is about a 50 year-old smoking man with no particular medical history who was admitted in the neurosurgery department for slow progress onset of holocranial headaches resistant to medical treatment and evovlving since more than 12 months with recently installation of vomiting and bilateral visual blur 3 days before his admission without epilepsia or another localization sign.
Neurological examination showed no motor palsy except a left facial hypoesthesia and right lateral homonymous hemianopia. The fundus examination was without abnormalities.
A CT scan was performed showing intra axial parieto-occipital lesion mesearing 45 mm of long axis which is hypodense and unenhanced in its center with thick enhanced wall and having intensely enhanced left anterolateral focal thickening. This lesion is surrounded by important edema with mass effect on cortical grooves and the left occipital horne of the homolateral ventricule (Fig. 1).
Fig. 1.
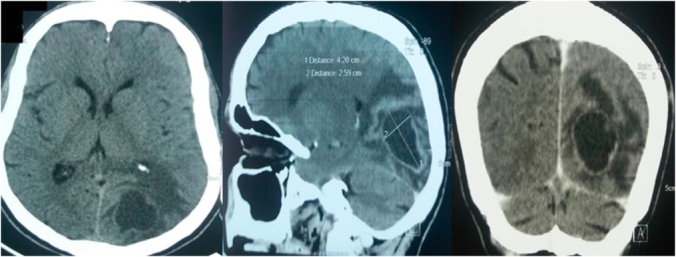
Brain CT scan showing intra axial parieto-occipital lesion mesearing 45 mm of long axis which is hypodense and unenhanced in its center with thick enhanced wall and having intensely enhanced left anterolateral focal thickening. This lesion is surrounded by important edema with mass effect on cortical grooves and the left occipiatal horne of the homolateral ventricule.
The MRIconfirmed the occipital inta axial lesion with fluid center hypo intense on T1 weighted image, which presents at the periphery a tissue component of variable thickness that intensely enhances measuring 31 * 23 * 49 mm. This lesion comes into contact with the superior sagittal sinus without thrombosis (Fig. 2).
Fig. 2.
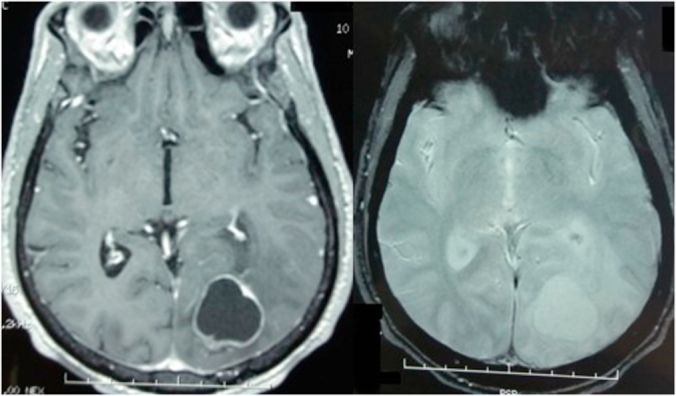
Brain MRI showing the occipital inta axial lesion with fluid center hypo intense on T1 weighted image, which presents at the periphery a tissue component of variable thickness that intensely enhances. This lesion comes into contact with the superior sagittal sinus without thrombosis.
The patient underwent a total remove of the lesion through a parieto-occipal bone flap. The lesion was friable and haemorrhagic with no obvious healthy boundaries.
The histopathological examination showed a proliferation of papillary structures centered by a conjonctivo-vascular axis and lined by several layers of cells of transitional appearance with nuclear atypies (Fig. 3a). The immunohistochemistry was positive for only cytokeratine 7 (Ck7) (Fig. 3b). This aspect is compatible for a metastasis of high grade urothelial papillary carcinoma.
Fig. 3.
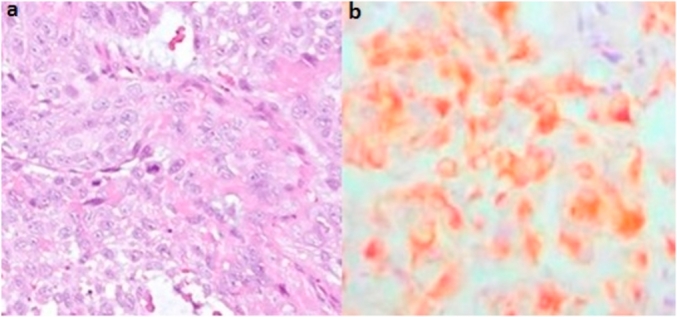
Proliferation of papillary structures centered by a conjonctivo-vascular axis and lined by several layers of cells of transitional appearance with nuclear atypies (hematoxylin-eosin × 200) (3.a). The immunohistochemistry was positive for only cytokeratine 7 (Ck7) (3.b).
The patient received full dose of radio and chemotherapy with good evolution after 39 months as he get rid of his intracranial hypertension syndrome except remaining of the right lateral homonymous hemianopia.
Discussion
Upper tract urothelial cancer (UTUC), arising from the urothelial lining of the urinary tract, accounts for about 5% of urothelial malignancies. They are relatively uncommon than urothelial cancers of the urinary bladder.1 UTUC progresses in several different ways including direct invasion, lymphatic spread, and hematogeneous metastases. Regional lymph nodes are commonly the initial site of metastasis, followed by migration to the liver, lung, and bone.2 Central nervous system metastasis is uncommon and rare in patients with urothelial carcinoma.3
In patients with theses brain metastasis, headache is the most common presenting symptom and occurs in approximately half of patients just like in our case. Focal neurologic dysfunction occurs in 20%–40% of patients and hemiparesis is the most common neurologic dysfunction. Our patient didn't have any palsy except the lateral homonymous hemianopia. The occipital lobe typically had the least number of metastases.
Based on the review of the literature, cerebral metastasis presented as one of the features in systemic progression of papillary urothelial carcinoma but it could occur in the patient with systemic control, and even as an initial manifestation4 just like our case. The interval from primary diagnosis to the cerebral metastasis was 0–69 months, and it generally developed within 3 years.
Contrast-enhanced MRI has been suggested as the modality of choice for the diagnosis of brain metastases because brain CT may underestimate the number of brain metastatic lesions.
Metastasectomy has been reported to improve the prognosis of patients with metastatic urothelial cancer. In patients with advanced stage, adjuvant chemotherapy has been suggested as an effective treatment modality with a high response rate. A combination of gemcitabine and cisplatin (GC) has demonstrated progression free and overall survival rates equal to those of M-VAC regimen, with a statistically lower incidence of adverse effects such as mucositis and neutropenia. GC is now considered a new standard chemotherapy regimen for advanced urothelial carcinoma.5 The main stay of treatment for multiple metastases was additionnal whole brain radiation therapy, which extends median survival from 1–2 months to 4–6 months in most series.
Because of the limited number of the case reports, the optimal treatment of urothelial cancer with brain metastasis is still unclear. However, our case report suggests resection of the metastatic lesion may benefit urothelial cancer patients with brain metastasis. This case report reminds us that brain metastasis should be considered in urothelial cancer patients with a headache or any ohther neurological dysfunction as it may inaugurate the whole pathology.
Conclusion
The metastases from the transitional papillary cell carcinoma of the renal pelvis to the brain are still rare. This possibility should always be kept in mind, while evaluating patients with metastatic disease to the brain. Due to availability of non-invasive treatment and newer less toxic chemotherapy, such patients can be managed in minimally morbid way.
Conflicts of interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
Contributor Information
Borni Mehdi, Email: borni.mehdi13@gmail.com.
Brahim Kammoun, Email: kammoun.brahim28@gmail.com.
Fatma Kolsi, Email: kolsineifar.fatma@gmail.com.
Mohamed Zaher Boudawara, Email: zaher.boudawara@rns.tn.
References
- 1.Jemal A., Siegel R., Ward E. Cancer statistics. Ca - Cancer J Clin. 2007;57:43–66. doi: 10.3322/canjclin.57.1.43. 2007. [DOI] [PubMed] [Google Scholar]
- 2.Johnson J.D., Young B. Demographics of brain metastasis. Neurosurg Clin N Am. 1996;7:337–344. [PubMed] [Google Scholar]
- 3.Forsyth P.A., Posner J.B. Headaches in patients with brain tumors: a study of 111 patients. Neurology. 1993;43:1678–1683. doi: 10.1212/wnl.43.9.1678. [DOI] [PubMed] [Google Scholar]
- 4.Davies B.J., Bastacky S., Chung S.Y. Large cerebellar lesion as original manifestation of transitional cell carcinoma of the bladder. Urology. 2003;62:749. doi: 10.1016/s0090-4295(03)00662-9. 10.1016/S0090-4295(03)00662-9. [DOI] [PubMed] [Google Scholar]
- 5.von der Maase H., Hansen S.W., Roberts J.T. J Clin Oncol. 2000 Sep;18(17):3068–3077. doi: 10.1200/JCO.2000.18.17.3068. [DOI] [PubMed] [Google Scholar]


