Abstract
Objective This study aims to evaluate the impact of early mobilization (EM) after pediatric liver transplantation in the pediatric intensive care unit (PICU).
Design A 14-month prospective before and after study.
Setting Multivalent PICU with 20 beds at a tertiary children's hospital.
Patients A total of 57 patients aged younger than 16 years who received liver transplantation and were admitted to the PICU after surgery.
Interventions EM project, a multifaceted framework for successful EM practice in the PICU focusing on a multidisciplinary team approach.
Measurements and Main Results Compared with the period before the implementation of the EM project, there was a significant increase in the proportion of patients who received physical therapy in the PICU (43 vs. 97%, p < 0.001). Also, there were greater median numbers of physical therapy per eligible patient (0 vs. 3, p < 0.001). Moreover, patients achieved higher functional mobility level within a shorter time. Length of intubation, PICU stay, and hospital stay were not significantly different. There were no adverse events or deaths.
Conclusion Using an EM project process, the proportion of patients who received physical therapy after liver transplantation increased. However, there was no difference in the length of PICU or hospital stay. Our findings indicated that EM for pediatric patients who received liver transplantation was well tolerated and safe.
Keywords: early mobilization, rehabilitation, pediatric intensive care unit, physical therapy
Introduction
Early mobilization (EM) for adults in the intensive care unit (ICU) can confer significant benefit in improving the quality of life, physical function, peripheral and respiratory muscle strength, as well as increasing ventilator-free days, and decreasing hospital and ICU stay. 1 2 3 4 5 6 A recent study showed that EM practices were present in 45% of the surveyed ICUs in the United States ( n = 227). 7 In contrast, rehabilitation practices for critically ill children in the pediatric intensive care unit (PICU) are not well characterized. Traditionally, the focus of PICU care is on the resuscitation and management of critical disease processes. As a result, critically ill children are often sedated and confined to bed for prolonged periods. 8 Immobilization and delayed rehabilitation could lead to negative emotional, behavioral, cognitive, and functional outcomes, which affect pediatric patients' quality of life. 8 9 10 11 EM in the PICU may positively impact the child's recovery from critical illness, but this has not been well studied. 4 At present, pediatric data to support the benefits of EM interventions are lacking, and there are few PICUs that introduce EM as a routine practice. A Canadian survey showed that only 3.4% of the institutions had local guidelines for EM for critically ill children. 9
Multiple barriers to integration of EM in the PICU have been reported. These include a lack of practice guidelines, the need for physician orders, conflicting perceptions regarding the safety and clinical thresholds of EM, and provider knowledge gaps in the benefits of mobilization for critically ill children. 9 These barriers also existed in our institution. To that end, we implemented an EM project to improve physical therapy services in our PICU. The goals of the before and after EM project were to increase the frequency of physical therapy consultations and treatments to improve patients' functional mobility in the PICU. Because the reasons why patients were admitted to the PICU were widely heterogeneous, we evaluated the EM project focusing on patients who received liver transplantation and were admitted to the PICU after surgery.
Materials and Methods
This is a prospective before and after study at the PICU of the National Center for Child Health and Development, which is a tertiary children's hospital in Tokyo, Japan. The unit is a multivalent PICU composed of 20 beds and staffed by attending physicians, fellows, and registered nurses (staff-to-patient ratio, 1:2). This study was approved by the ethics committee of our institution.
This EM project started in the spring of 2015 with increasing intensity. We set the 7-month EM period (June–December 2015) for evaluation of the EM project, during which EM in the PICU was implemented. We evaluated the EM project using a before and after design focusing on PICU patients receiving liver transplantation. To evaluate the effects of the EM project, the EM period is compared with the same 7-month pre-EM period in the prior year (June–December 2014). Thus, the “before” study period was 7 months (June–December 2014) and the “after” study period was 7 months (June–December 2015). There was a gap of 5 months in between the before and after study arm. This time was spent implementing the team and getting the members to be accustomed to the new practice of EM. We obtained consent for EM interventions from patients' parents at their admission to the PICU for the EM period.
Patients
We enrolled all patients aged younger than 16 years who received liver transplantation during pre-EM and EM periods, and were admitted to the PICU after surgery. The patients who needed intensive care in the PICU before the surgery were excluded. In both pre-EM and EM periods, we targeted prospective data collection including age at liver transplantation, weight, sex, preoperative disposition, types of donors, pediatric index of mortality 2, pediatric end-stage liver disease score, etiology, operation time, blood loss, graft recipient body weight, ABO types of recipient and donor, postoperative complications, the number of physical therapy consultations/treatments, functional mobility during a physical therapy in the PICU on each day, length of intubation, length of PICU stay, length of hospital stay, adverse events from EM, and mortality.
EM Project
The EM project was composed of the following eight elements:
1. Staffing changes
Before the EM project started, there were five physical therapists who had to cover all departments of the hospital. In April 2015, two new physical therapists working solely for the PICU were recruited.
2. Rehabilitation aids
We procured rehabilitation aids, including a walker, wheelchairs and toys, and used them during EM.
3. Team approach
Daily multidisciplinary meetings were held to promote communication among staff and coordination of physical therapy.
4. Education and training
Educational seminars on research on the ICU-acquired weakness and benefits of EM in the ICU were held. The seminars include summarizing and discussion of published findings. Training for nurses, physical therapists, and physicians was conducted to equip the staff with fundamental skills in rehabilitation, including positioning and range of motion exercise skills.
5. Changing ordering system of physical therapy
Before the EM project, rehabilitation therapy was ordered only when a PICU physician consulted a physiatrist. After the EM project, we added rehabilitation therapy to the standardized PICU admission orders, and changed the ordering system so that PICU physicians could order rehabilitation therapy directly. The ordering system is a computer order form. We had made it a routine practice (every patient had a physical therapy order) to improve the number of orders and the timelines.
6. Planning daily goals for every patient
A rehabilitation daily goal sheet for every patient was introduced. The sheets were shared among the unit members. Every morning, the allowed mobility level of each patient was discussed among team members and the daily goal of EM was determined within that level (e.g., the range of motion exercise on the first day, supine to sit on the second day, and sit at the edge of the bed on the third day). The usual daily goal for a ventilated patient was the range of motion exercise.
7. Developing safety-related guidelines
The exclusion criteria for EM by physical therapists in the PICU were hemodynamic instability, the day of thoracic or abdominal surgery, intracranial hypertension, and cervical spine instability. Thus, if the patient had no hemodynamic instability, we usually determined that the patient was ready for receiving EM on the next day of the liver transplantation surgery.
The criteria for temporary discontinuation of therapy were loosening the fixation or dislodgement of the devices (endotracheal tube, drainage tube, and so on), vital signs exceeding a threshold, and patients' unacceptability (complaining of pain and Richmond Agitation Sedation Score ≥ 2). 12 We defined the default vital signs threshold during EM according to the patient's age ( Table 1 ). After the problems that caused the discontinuation of the therapy were resolved and the vital signs recovered, we deemed that the patient was ready for reattempting EM. During EM, morphine bolus infusion was used for pain management, if necessary. For nonventilated patients, a single morphine bolus dose was 10 μg/kg. For ventilated patients, sedation agents such as midazolam and dexmedetomidine were also used continuously.
Table 1. Default vital signs threshold during early mobilization.
| Patient age | Vital signs | |||
|---|---|---|---|---|
| HR (/min) | sBP (mm Hg) | RR (/min) | Sp o 2 (%) | |
| < 3 mo | 120–170 | 60–90 | 25–70 | ≥ 95 |
| 3–5 mo | 120–160 | 70–90 | 25–65 | ≥ 95 |
| 6–11 mo | 110–150 | 70–90 | 20–60 | ≥ 95 |
| 1–2 y | 90–140 | 70–100 | 20–45 | ≥ 95 |
| 3–5 y | 80–110 | 75–120 | 15–30 | ≥ 95 |
| ≥ 6 y | 60–100 | 90–160 | 12–25 | ≥ 95 |
Abbreviations: HR, heart rate; RR, respiratory rate; sBP, systolic blood pressure.
8. Feedback
The information in every monthly rehabilitation report was disseminated to the unit members.
Statistical Analysis
Descriptive statistics were expressed as medians and interquartile ranges for continuous data, or absolute frequencies and percentage for categorical data. Bivariate comparisons between groups were performed using Mann–Whitney U test for continuous data, and Fisher exact test for categorical data. Cumulative incidence was demonstrated as one minus the Kaplan–Meier survival method. Comparisons between groups were performed using the Gray test. All analyses were performed using R version 3.2.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
All eligible PICU patients during the pre-EM and EM periods were included in the study, representing a total of 23 and 34 patients requiring 340 and 327 PICU patient-days, respectively. These patients represented approximately 4 and 5% of all PICU admissions during each period ( Fig. 1 ). The baseline characteristics between the two groups were not significantly different except for preoperative hospitalization ( Table 2 ). For all patients, the median length of intubation was 2 (range, 0–2) days, the median length of PICU stay was 9 (range, 7–13) days, and the median length of hospital stay was 45 (range, 37–63) days.
Fig. 1.
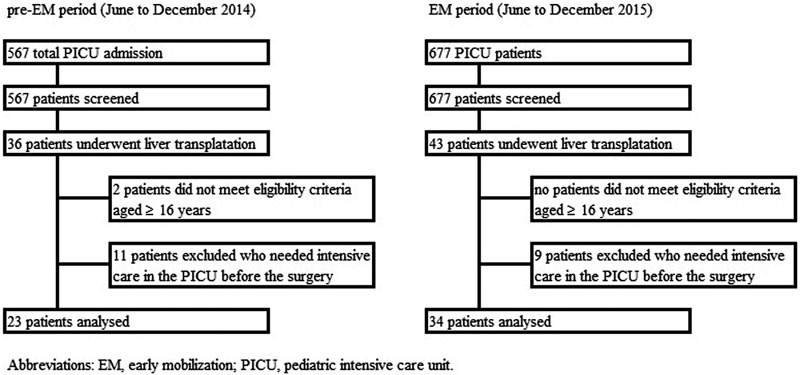
The trial profile. EM, early mobilization; PICU, pediatric intensive care unit.
Table 2. Baseline characteristics of patients.
| Baseline characteristics | Pre-EM period ( n = 23) |
EM period ( n = 34) |
p Value a |
|---|---|---|---|
| Age, median (IQR) (mo) | 13 (8–31) | 13 (7–74) | 0.776 |
| Weight, median (IQR) (kg) | 7.6 (6.8–11.6) | 9.2 (6.8–17.6) | 0.232 |
| Male | 11 (48) | 14 (41) | 0.786 |
| Preoperative hospitalization | 17 (74) | 33 (97) | 0.014 |
| Living donor | 23 (100) | 33 (97) | 1 |
| PIM 2 on PICU admission, median (IQR) (%) | 3.2 (1.3–4) | 3.2 (1.2–3.7) | 0.987 |
| PELD score, median (IQR) b | 10 (0–13) | 6 (0–12) | 0.619 |
| Etiology | |||
| Biliary atresia | 14 (61) | 15 (44) | 0.283 |
| Hepatoblastoma | 2 (9) | 1 (3) | 0.559 |
| Progressive familial intrahepatic cholestasis | 1 (4) | 4 (12) | 0.638 |
| Hepatic fibrosis | 1 (4) | 1 (3) | 1 |
| Fulminant hepatitis | 1 (4) | 1 (3) | 1 |
| Ornithine transcarbamylase deficiency | 3 (9) | 0.265 | |
| Carbamoyl phosphate synthetase deficiency | 2 (6) | 0.510 | |
| Citrullinemia | 2 (6) | 0.510 | |
| Others | 4 (17) | 5 (15) | 1 |
| Operative data | |||
| Operation time, median (IQR) (min) | 470 (424–592) | 467 (416–509) | 0.345 |
| Blood loss, median (IQR) (g) | 440 (265–750) | 498 (399–680) | 0.411 |
| GRBW, median (IQR) (%) | 2.9 (2.1–3.1) | 2.2 (1.5–3.3) | 0.433 |
| ABO-incompatible | 4 (17) | 6 (18) | 1 |
| Postoperative complications | |||
| Acute rejection | 12 (52) | 11 (32) | 0.173 |
| Bacteremia | 5 (22) | 2 (6) | 0.106 |
| Thromboembolism | 0 (0) | 0 (0) | |
Abbreviations: EM, early mobilization; GRBW, graft recipient body weight; IQR, interquartile range; PELD, pediatric end-stage liver disease; PICU, pediatric intensive care unit; PIM 2, pediatric index of mortality 2.
Note: Values are n (%) or as otherwise indicated.
Fisher exact and Mann–Whitney U tests were used to compare patient characteristics across the pre-EM and EM periods.
PELD score were calculated for 20 patients in pre-EM period and 23 patients in EM period younger than 12 years. Patients with hepatoblastoma or inborn errors of metabolism were excluded.
Outcomes
There was a significant increase in the proportion of patients who received physical therapy in the PICU, especially within the first 72 hours after transplantation ( Table 3 ). Moreover, the number of physical treatments per eligible patient and per eligible PICU day increased. The length of intubation, PICU stay, and hospital stay between the two groups were not significantly different. No adverse events or deaths were reported. Time from transplantation to the milestones achieved in each patient during PICU stay is summarized in Fig. 2 . Compared with patients in the pre-EM period, patients in the EM period could achieve the same milestones earlier. For example, the cumulative incidence of patients reaching the “supine to sit” level was higher in EM period than in pre-EM period ( Fig. 3 ).
Table 3. Outcomes.
| Outcome measure | Pre-EM period ( n = 23) |
EM period ( n = 34) |
p Value a |
|---|---|---|---|
| Consultations | |||
| Physical therapy | 13 (57) | 34 (100) | < 0.001 |
| Patient data | |||
| Received physical therapy in PICU | 11 (43) | 33 (97) | < 0.001 |
| Received physical therapy in PICU within first 72 h | 0 (0) | 22 (65) | < 0.001 |
| Number of treatments per patient, median (IQR) | 0 (0–1) | 3 (2–6) | < 0.001 |
| Number of treatments per day, median (IQR) | 0 (0–0.1) | 0.3 (0.3–0.5) | < 0.001 |
| Length of intubation, median (IQR) (d) | 2 (0–2) | 2 (0–2) | 0.779 |
| Length of PICU stay, median (IQR) (d) | 9 (8–14) | 8 (7–12) | 0.317 |
| Length of hospital stay, median (IQR) (d) | 45 (36–57) | 46 (38–65) | 0.770 |
| Adverse events from EM | 0 (0) | 0 (0) | |
| In-hospital death | 0 (0) | 0 (0) | |
Abbreviations: EM, early mobilization; IQR, interquartile range; PICU, pediatric intensive care unit.
Note. Values are n (%) or as otherwise indicated.
Fisher exact and Mann–Whitney U tests were used to compare patient characteristics across the pre-EM and EM periods.
Fig. 2.

Time from transplantation to milestones achieved in each patient during the PICU stay. One crossbar represents one patient. EM, early mobilization; PICU, pediatric intensive care unit.
Fig. 3.

Cumulative incidence of patients reaching the “supine to sit” level. Cumulative incidence was demonstrated as one minus the Kaplan–Meier survival method. Comparisons between groups were performed using the Gray test. EM, early mobilization; PICU, pediatric intensive care unit.
Discussion
In this prospective before and after study, we found that the EM project resulted in an increase in the proportion of patients who received physical therapy after liver transplantation. In addition, the patients in EM period could achieve the same milestones earlier than the patients in the pre-EM period. Thus, patient's quality of life was considerably improved during the same hospitalization period. However, these outcomes did not translate into any difference in the length of stay in the PICU or in hospital stay between the EM and pre-EM groups. We postulate that the reason for this was the small sample size of the study, other factors affecting the length of stay in the PICU or in the hospital, and the relatively low number of physical treatments per day even during the EM period. In our PICU, we have yet to introduce EM by physical therapists on weekends and public holidays. By a sample size calculation from this study (α error = 0.05, β error = 0.80), we estimated that approximately 900 patients would be needed to show a difference in the length of stay in the PICU. Thus, we concluded that a novel finding of this study was that EM for pediatric patients who received liver transplantation was well tolerated and safe.
A recently presented abstract examining the Studies of Pediatric Liver Transplantation database showed that among 25 centers, the high-performing institutions had a shorter mean length of postoperative intubation (2.7 days) compared with the other centers (6.5 days). The mean length of PICU stay and hospital stay were 5.5 and 15.3 days, respectively, in high-performing centers, and 10.8 and 25.4 days, respectively, in the others. 13 The length of intubation in our institution was near to high-performing centers. However, the length of PICU and hospital stay in our institution was longer than that in high-performing centers. A reason for this may be the difference between hospital types and health care systems in Japan and the United States.
An element of the EM project was the recruitment of two physical therapists working only for the PICU. As far as we know, this is the first report of PICU-only physical therapists, which also represents a major breakthrough in the EM implementation in our institution. Nonetheless, other factors were also needed to implement EM. Bakhru et al surveyed 687 ICUs in the United States with a response rate of 73% (500 ICUs), and proposed a framework for successful EM practice in the ICU based on processes associated with successful implementation. 7 The framework contains the following steps to EM: (1) team approach: multidisciplinary rounds to enhance communication and coordination of care; (2) explicit daily goals for each patient across disciplines (nursing, respiratory, therapy, pharmacy, and physicians); (3) standardize practice: utilize team-based protocols to achieve patient goals; (4) system for audit-feedback for performance improvement. To overcome the barriers for EM in our institution, we started the EM project which comprised eight elements that are consistent with Bakhru et al framework. To start EM, a significant transformation in “culture” was needed among the entire multidisciplinary PICU team.
Serious adverse events are uncommon in adult patients in the ICU due to EM. Previous studies reported that the incidence of adverse events during physical therapy in the ICU was lower than 5%. 14 15 16 17 In this study, no adverse events occurred during either the EM or pre-EM periods. Hodgson et al presented expert consensus and recommendations on the safety criteria for active mobilization of mechanically ventilated critically ill adults. 18 However, safety criteria for EM of critically ill children in the PICU are not available. In the EM project, we set out the exclusion criteria for EM by physical therapists in the PICU, as well as for temporary discontinuation of therapy. Moreover, to secure safety, we held multidisciplinary meetings every morning and chose patients who received EM therapy.
Limitations
This EM project has some limitations. First, given its design as a before and after study, the patients were not randomized to physical therapy interventions, nor were the outcomes evaluated in a blinded manner. Second, given the relatively small sample size and short duration of this EM project and its focus on homogenous patients receiving liver transplantation in a single PICU, the results may not be generalizable to other pediatric patients. Third, the relatively high staff-to-patient ratio may have been an enabling factor to introduce EM in our PICU. Further studies are needed to establish the new standard of EM care in the PICU.
Conclusion
Since the introduction of the structured and multifaceted EM project, the proportion of patients who received physical therapy after liver transplantation has increased. However, there were no differences in the length of PICU or hospital stay. Our findings indicated that EM for pediatric patients who received liver transplantation was well tolerated and safe.
Note
The authors Norihiko Tsuboi and Mureo Kasahara have received the grant from National Center for Child Health and Development (no. 27–1). For the remaining authors none were declared.
References
- 1.Needham D M, Korupolu R, Zanni J M et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil. 2010;91(04):536–542. doi: 10.1016/j.apmr.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Kayambu G, Boots R, Paratz J. Physical therapy for the critically ill in the ICU: a systematic review and meta-analysis. Crit Care Med. 2013;41(06):1543–1554. doi: 10.1097/CCM.0b013e31827ca637. [DOI] [PubMed] [Google Scholar]
- 3.Stiller K. Physiotherapy in intensive care: an updated systematic review. Chest. 2013;144(03):825–847. doi: 10.1378/chest.12-2930. [DOI] [PubMed] [Google Scholar]
- 4.Cameron S, Ball I, Cepinskas G et al. Early mobilization in the critical care unit: A review of adult and pediatric literature. J Crit Care. 2015;30(04):664–672. doi: 10.1016/j.jcrc.2015.03.032. [DOI] [PubMed] [Google Scholar]
- 5.Schweickert W D, Pohlman M C, Pohlman A Set al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial Lancet 2009373(9678):1874–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morris P E, Goad A, Thompson C et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36(08):2238–2243. doi: 10.1097/CCM.0b013e318180b90e. [DOI] [PubMed] [Google Scholar]
- 7.Bakhru R N, Wiebe D J, McWilliams D J, Spuhler V J, Schweickert W D. An Environmental Scan for Early Mobilization Practices in U.S. ICUs. Crit Care Med. 2015;43(11):2360–2369. doi: 10.1097/CCM.0000000000001262. [DOI] [PubMed] [Google Scholar]
- 8.Wieczorek B, Burke C, Al-Harbi A, Kudchadkar S R. Early mobilization in the pediatric intensive care unit: a systematic review. J Pediatr Intensive Care. 2015;2015(15):129–170. doi: 10.1055/s-0035-1563386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choong K, Koo K K, Clark H et al. Early mobilization in critically ill children: a survey of Canadian practice. Crit Care Med. 2013;41(07):1745–1753. doi: 10.1097/CCM.0b013e318287f592. [DOI] [PubMed] [Google Scholar]
- 10.Melnyk B M, Alpert-Gillis L, Feinstein N F et al. Creating opportunities for parent empowerment: program effects on the mental health/coping outcomes of critically ill young children and their mothers. Pediatrics. 2004;113(06):e597–e607. doi: 10.1542/peds.113.6.e597. [DOI] [PubMed] [Google Scholar]
- 11.Taylor A, Butt W, Ciardulli M. The functional outcome and quality of life of children after admission to an intensive care unit. Intensive Care Med. 2003;29(05):795–800. doi: 10.1007/s00134-003-1690-6. [DOI] [PubMed] [Google Scholar]
- 12.Ely E W, Truman B, Shintani A et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS) JAMA. 2003;289(22):2983–2991. doi: 10.1001/jama.289.22.2983. [DOI] [PubMed] [Google Scholar]
- 13.Kelly B, Englesbe M, Bucuvalas Jet al. Improving value after pediatric liver transplant: discharge practices of high-performing centers [abstract] Am J Transplant 201313054723237696 [Google Scholar]
- 14.Sricharoenchai T, Parker A M, Zanni J M, Nelliot A, Dinglas V D, Needham D M. Safety of physical therapy interventions in critically ill patients: a single-center prospective evaluation of 1110 intensive care unit admissions. J Crit Care. 2014;29(03):395–400. doi: 10.1016/j.jcrc.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 15.Zanni J M, Korupolu R, Fan E et al. Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care. 2010;25(02):254–262. doi: 10.1016/j.jcrc.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 16.Bourdin G, Barbier J, Burle J F et al. The feasibility of early physical activity in intensive care unit patients: a prospective observational one-center study. Respir Care. 2010;55(04):400–407. [PubMed] [Google Scholar]
- 17.Lee H, Ko Y J, Suh G Y et al. Safety profile and feasibility of early physical therapy and mobility for critically ill patients in the medical intensive care unit: Beginning experiences in Korea. J Crit Care. 2015;30(04):673–677. doi: 10.1016/j.jcrc.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 18.Hodgson C L, Stiller K, Needham D M et al. Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults. Crit Care. 2014;18(06):658. doi: 10.1186/s13054-014-0658-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


