Abstract
Prolonged immobility is associated with significant short- and long-term morbidities in critically ill adults and children. The majority of critically ill children remain immobilized while in the pediatric intensive care unit (PICU) due to limited awareness of associated morbidities, lack of comfort and knowledge on how to mobilize critically ill children, and the lack of pediatric-specific practice guidelines. The objective of this article was to develop consensus practice recommendations for safe, early mobilization (EM) in critically ill children. A group of 10 multidisciplinary experts with clinical and methodological expertise in physical rehabilitation, EM, and pediatric critical care collaborated to develop these recommendations. First, a systematic review was conducted to evaluate existing evidence on EM in children. Using an iterative process, the working document was circulated electronically to panel members until the group reached consensus. The group agreed that the overall goals of mobilization are to reduce PICU morbidities and optimize recovery. EM should therefore not be instituted in isolation but as part of a rehabilitation care bundle. Mobilization should not be delayed, but its appropriateness and safety should be assessed early. Increasing levels of physical activity should be individualized for each patient with the goal of achieving the highest level of functional mobility that is developmentally appropriate, for increasing durations, daily. We developed a system-based set of clinical safety criteria and a checklist to ensure the safety of mobilization in critically ill children. Although there is a paucity of pediatric evidence on the efficacy of EM, there is ample evidence that prolonged bed rest is harmful and should be avoided. These EM practice recommendations were developed to educate clinicians, encourage safe practices, reduce PICU-acquired morbidities, until future pediatric research provides evidence on effective rehabilitation interventions and how best to implement these in critically ill children.
Keywords: early mobilization, critically ill children, physiotherapy, practice guidelines
Introduction
Pediatric intensive care unit (PICU) mortality rates have decreased in the last decade, however, the proportion of children surviving their critical illness with significant functional morbidity is rising. 1 Prolonged immobility is an important predictor of poor functional outcome and the development of critical illness-acquired morbidities. 2 These morbidities, in turn, have important negative physical, neurocognitive, and mental health consequences in adults and pediatric survivors of critical illness, that can persist long after these patients leave the intensive care unit (ICU) setting. 3 4 Referred to collectively as the postintensive care syndrome, this phenomenon affects up to 69% ICU survivors, is often longlasting, negatively impacts patients' quality of life, and represents a significant burden not only to the health care system, but to society at large. 5 Post-PICU cognitive, psychologic, and functional sequelae is also increasingly recognized in critically ill children and their families. 6 As a result, there is tremendous growth of research evaluating interventions to prevent these critical illness sequelae. Minimizing sedation, facilitating spontaneous breathing, and promoting early rehabilitation have been shown to be feasible, safe, and improves patient outcomes, and are therefore now recommended as practice priorities amongst ICUs. 7 8 9 This approach, coupled with post-ICU follow-up and rehabilitation programs are increasingly adopted to optimize posthospital recovery in adult ICU survivors. 10
Unfortunately, pediatric research on ICU-based rehabilitation significantly lags behind adult evidence. 11 The majority of rehabilitation in critically ill children is nonmobility based. 12 13 14 Only 9.5% of children admitted to Canadian PICUs are mobilized early, within 48 hours of PICU admission. 12 Major barriers to mobilizing critically ill children include resource limitations (i.e., the lack of dedicated physical or occupational therapy staff), limited awareness of existing evidence, and the lack of practice guidelines specifically for the PICU population. 13 15 While clinicians agree that prolonged bed rest is inappropriate, many express safety concerns with mobilizing children. 15 Subsequently, there are diverse opinions regarding if, when and how to mobilize children in the PICU.
Mobility-based rehabilitation initiated early during critical illness and continued after discharge has been suggested to improve patient outcomes, particularly in adult ICU, and specific pediatric populations such as premature neonates, neurosurgical, cardiac surgical, and burns patients. 16 17 18 19 However, there are currently no published rehabilitation or physiotherapy practice guidelines specifically targeted to the general PICU population. The objective of this article was to develop clinical practice recommendations for safe, mobility-based rehabilitation in critically ill children.
Methods
A group of 10 multidisciplinary experts with either clinical and methodological expertise in physical rehabilitation, pediatric critical care and currently involved in research on early mobilization (EM) in critically ill patients were engaged to participate in developing clinical practice recommendations for the safe mobilization in PICU, using the Institute of Medicine framework. 20 Participants were all from tertiary care institutions and comprised of three pediatric intensivists, four physiotherapists, one nurse and research psychologist, one quality improvement nurse, and one advanced care practice nurse, from Canada ( n = 5), United States ( n = 4), and South Africa ( n = 1). Key principles agreed upon by the group were to define: (1) the goals of EM; (2) what constitutes mobilization; (3) appropriate timing for mobilization; (4) clinical criteria for determining mobilization readiness and safety, and (5) mobilization frequency and duration.
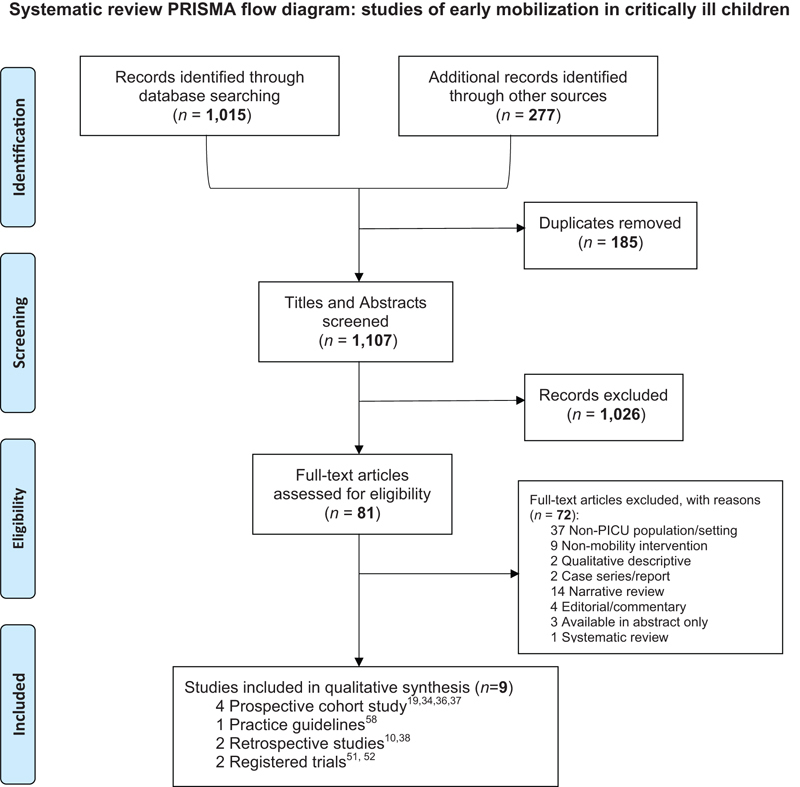
First, we conducted a systematic review of the literature. We searched PubMed, CINAHL, and EMBASE from inception to October 2016, for observational studies, clinical trials or clinical trial protocols, and practice guidelines focused on PICU-based mobility or physical therapy interventions conducted in the general PICU population aged younger than 18 years, published in full or in abstract in any language. We manually searched the National Institutes of Health (available at: http://clinicaltrials.gov), and the Evidence in Pediatric Intensive Care Collaborative (available at: http://epicc.mcmaster.ca) for additional eligible studies. We excluded adult trials, case series or case reports, systematic and narrative reviews, and studies focused on nonmobility interventions or chest physiotherapy alone. The results of our search are presented in the Appendix . We used this evidence to answer the clinical questions where possible and appropriate, however, where there was a paucity of pediatric evidence, we utilized adult ICU randomized trials, systematic reviews, and practice guidelines for additional safety data on EM. 21 22 23 24 25 26 27 We summarized the best level of evidence supporting our recommendations using the Oxford Centre of Evidence-Based Medicine (OCEBM) 2011 guidelines, where level 1 represents systematic review of randomized trials, level 2 represents randomized trial or observational study with dramatic effect, level 3 represents cohort studies, level 4 represents case series or case–control studies, and level 5 indicates mechanism-based reasoning. 28 We considered the strength and quality of the available evidence alongside potential benefits and harms when making our safe practice recommendations. Using an iterative process, the working document was circulated electronically to panel members until the group reached consensus, defined as 100% agreement. The consultation was sought from key stakeholders in the PICU and the subspecialty services whose patients may be cared for in the PICU such as neurosurgery, otolaryngology, orthopedic surgery, plastic surgery, and general surgery. We solicited their input through the respective division leaders, on contraindications, precautions, and appropriate levels of mobilization in their critically ill pediatric population. The guidelines were then piloted at a single center over a 12-month period (McMaster University), during which time informal feedback was obtained from bedside nurses, physicians, physiotherapists, and the subspecialty division leaders, on the sensibility and feasibility of the practice recommendations.
Results
The Goals of Early Mobilization: A Bundled Approach
Recommendation
The consensus group agreed that the overall goals of mobilization in critically ill children are to improve functional recovery and reduce the length of PICU and hospital stay. We, therefore, recommend that EM be instituted as a part of an “ABCDEFGH” rehabilitation care bundle:
A ttention to A nalgesia; A void oversedation; allow A wakening
Spontaneous B reathing trials
C hoice of sedation and analgesia
D elirium prevention, surveillance, and management
E arly mobilization and E xercise
F amily engagement and empowerment
G ood nutrition
H umanism
Rationale
Mobilization is a rehabilitation intervention to prevent critical illness-acquired morbidities, such as muscle weakness and deconditioning, while optimizing skin integrity, physical, and neurocognitive health, decrease the duration of advanced life-support and PICU length of stay, and ultimately to enhance functional recovery. Hence, mobilization strategies can only be effective if supported by a patient-centered care bundle. The ABCDEF bundle incorporates a set of evidence-based practices that address several emerging serious ICU-acquired morbidities such as ventilator pneumonia, weakness, delirium, and functional disability. 29 The use of such a bundle in critically ill adults can result in significant improvements in patient care and outcomes, 30 and is therefore recommended by the Society of Critical Care Medicine ICU Liberation Campaign (available at: www.iculiberation.org). Integrating these practices in the PICU may similarly reduce iatrogenic morbidities and improve outcomes and recovery in critically ill children, however, there is currently little pediatric evidence supporting this approach. Family-centered care is now considered “best practice” and essential for a child's recovery from critical illness. 31 Promoting family engagement and partnership in a rehabilitation care bundle increases awareness and positively impacts practice. 32 We added “G” for “Good nutrition” to this bundle, to emphasize that nutrition is a key component to optimizing functional recovery during critical illness. 33 We promote “H” for “Humanism,” as a reminder to clinicians of the negative effects of the critical care setting, and of the depersonalization of patients which is unfortunately now commonplace in our technology-dependent environment. 34 We recommend strategies to foster more personal and humane care, and to create an environment where healing and recovery are possible. 35
What Constitutes “Mobilization” in the Critically Ill Child: Graded Mobilization Activities and Goals
Recommendation
To optimize safe mobilization while minimizing the adverse events, we recommend that critically ill children progress through a range of graduated activities that are developmentally appropriate, individualized, and at its lowest level serves to prevent muscle wasting, and advances as the goals of care transition to achieving functional mobility and increasing muscle strength.
Rationale
There is level 1 evidence suggesting that compared with other interventions, exercise and mobility-based physical therapy is the most effective intervention in optimizing functional recovery in critically ill adults. 16 However, to date, there is only level 3 evidence describing mobilization interventions, and randomized trials underway in pediatrics. 14 21 36 37 38 39 40 These studies do not clearly define degrees of mobilization activities in the critically ill pediatric population. While ambulation and independent mobilization out of bed are often the endpoints in adults, this is often not feasible in children given the heterogeneous age, cognitive and baseline function of this population. The group, therefore, agreed that what constitutes “functional mobility” for a child should, therefore, be individualized and developmentally appropriate; this may vary from sitting tolerance in chronic wheelchair users to neurodevelopmental play in infants.
We developed taxonomy for physical therapy activities for the purpose of ensuring clarity, defining levels of mobility, identifying individualized patient goals, and facilitating consistency in language and documentation ( Table 1 ). The level of mobilization should be determined by the physiotherapist's clinical assessment of the patient in conjunction with input from other clinicians, as well as an assessment of safety. Given the heterogeneous population of children admitted to PICUs, we recommend that progressive mobilization goals should be individualized for each patient daily, corresponding to their clinical condition, developmental maturity, strength, and endurance. We have organized mobilization activities according to three levels of assistance required, that graduate from a minimum goal of preventing muscle wasting, maintaining range of motion, and optimizing circulatory flow (level 1), to mobility activities that enhance strength, endurance, balance, and functional mobility (levels 2 and 3; Table 2 ). Even passive mobilization has the potential to activate muscle contraction and has been shown to be beneficial. 41 As the level of assistance required improves over time, the activity goals may progress to encourage increasingly active patient participation, to achieve the highest level of physical activity that is safe, age appropriate, and functional for that patient. It is acknowledged that some patients have significant baseline functional limitations that may never allow them to progress to higher levels of activity. Hence, optimizing passive mobilization activities for those who require level 1 or maximum assistance to facilitate their recovery to baseline, and identifying what functional mobility for each patient is, should be individualized.
Table 1. Definitions of mobility and nonmobility interventions in critically ill children.
| Intervention | Description |
|---|---|
| Nonmobility | |
| Bed repositioning only | Activity restricted to passive position changes in bed |
| Respiratory or “chest physiotherapy” | Physical methods to improve: Ventilation and V/Q matching, breathing mechanics, respiratory muscle strength and airway secretions clearance, e.g., chest wall vibrations, percussion techniques, manual facilitation of chest wall movement, manual or ventilator hyperinflation, deep breathing exercises (including blowing bubbles and incentive spirometry), and inspiratory muscle training |
| Passive range of motion and stretching exercises | The therapist moves joints and stretches muscles through their full available range of motion to prevent or correct tightening of muscles or joints, which could lead to contracture formation |
| Mobility | |
| Active range of motion and stretching exercises (“AROM” or “AAROM”) Strengthening exercises |
Active movement of patient's limbs through an available range of joint motion. These movements can be independently done by patient (active ROM; “AROM”), active stretching (patient uses opposing muscle group to stretch affected group), or the patient may need assistance to complete the full available joint range (active-assisted ROM; “AAROM”) Exercises to place a load on muscles to achieve greater muscle strength, e.g., by a patient actively moving a weak limb against gravity; by the therapist providing manually graded resistance to movement; by applying tension to cycling on the ergometer |
| Neurodevelopmental play | Goal-directed activities to maintain or improve fine and gross motor development, muscle strength, thoracic mobility, coordination and balance for infants, and developmentally delayed children |
| Mobility device (e.g., in-bed cycling) | Activities are done with a device that facilitates functional limb movement, the range of motion, and strengthening, e.g., cycle ergometer. May be active or passive and executed in the supine patient. May be conducted in lower or upper limbs |
| Bed mobility | Functional activities are done while patient is recumbent in bed, but require the active participation of the patient; e.g., active or active-assisted repositioning in bed; rolling from side-to-side; and bridging (i.e., supine with pelvic or hip lifts), does not involve moving out of bed or over the edge of the bed |
| Transfers | These activities may be active or passive, may occur with varying degrees of caregiver assistance and supervision, or may be performed independently |
| Transfer from lying to sitting at edge of bed | Sitting at edge of bed, with or without caregiver support as needed |
| Transfer from bed to/from chair | Transfers from bed to chair, wheelchair or a neurochair, using a mechanical lift, sliding board, caregiver assistance through patient pivoting, stepping or shuffling to the chair/wheelchair or commode |
| Transfer from sitting to/from standing | The patient can get up from sitting to/from standing with supervision or assistance |
| Sitting tolerance | Patient tolerates transfers from bed to a bedside chair or wheelchair and can tolerate sitting tilted or upright, for periods of time (i.e., for at least 30 min) |
| Crawling | Crawling with/without assistance |
| Pregait activities | Exercises before ambulation, conducted with or without assistance, e.g., moving from seated to a standing position, weight shifting from foot to foot, stepping in place, and sideways stepping |
| Ambulation | Walking away from bed or chair (i.e., on each foot) with or without assistance from a therapist or a gait aid (e.g., walker) |
| Activities of daily living | For example, face washing, oral hygiene, dressing. May occur with varying degrees of caregiver assistance |
Abbreviations: AROM, active range of motion; AAROM, active assisted range of motion; ROM, range of motion; V/Q, ventilation/perfusion.
Note: Passive: No effort by the patient.
Assisted: Some active participation by the patient and with the help of a therapist or assistant.
Active: Some active participation (full to partial) by the patient with or without the help of a therapist.
Table 2. Activity goals.
| Level of assistance | Definition | Activity goals a | |
|---|---|---|---|
| 1 | Maximum |
|
|
| 2 | Moderate |
|
|
| 3 | Minimum |
|
|
Abbreviations: AROM, active range of motion; AAROM, active assisted range of motion; EOB, edge of bed; PROM, passive range of motion.
To be individualized, according to the patient's level of assistance required, the presence of precautions and functional level.
Appropriate Timing for Early Mobilization in Critically Ill Children
Recommendation
Critically ill children should be assessed for appropriate activity within 24 hours of PICU admission.
Rationale
Skeletal muscle wasting has been demonstrated to occur early and rapidly in adults in the first week of critical illness, and is more pronounced amongst those with multi- versus single organ failure. 42 The benefits of mobilization appear to be optimized with earlier initiation, while delays in mobilization are associated with increasing morbidity in adults. 16 However, a recent trial suggests that very EM within 24 hours specifically in adult stroke patients, is not recommended. 43 A recent meta-analysis that categorized “late” as greater than 7 days, and “early” as less than 7 days, reported conflicting results. While earlier studies demonstrated improved functional mobility with EM interventions, 44 45 more recent, larger trials have added controversy on its effect on longer term functional outcome and health-related quality of life in the adult population. 46 47 48 Potential sources of inconsistent findings in these trials to date include the delayed onset (i.e., 4–8 days from admission), duration and intensity of mobilization, and selected outcome measures of physical mobility and strength which are not necessarily predictive of “function.” Further pilot and ongoing trials seek to evaluate the “dosage, ” that is, the intensity and timing of EM, and a multiprong approach to “rehabilitation” in the adult population. 49 50 51
In the pediatric critical care setting, EM was defined by Wieczorek et al in their quality improvement project as within the first 3 days of critical illness. 38 Pediatric interventional studies enrolled children who were within 24 to 96 hours of fulfilling eligibility (level 3 evidence), 14 21 39 52 and ongoing registered trials define “early” as within 48 hours of critical illness, or when safety criteria are met following PICU admission. 37 53 Based on the current evidence, we were not able to determine the impact of time from admission to first mobilization session on functional outcomes, or clearly, define what constitutes “early” for mobility activities in critically ill children. Ongoing pediatric and adult trials will provide important information on the most appropriate timing and “dosage” of mobilization in critically ill patients in the future. 49 51 54 Our recommendations are therefore based on the strength of evidence that prolonged immobilization is harmful and should, therefore, be avoided. 42 55 56 We, therefore, emphasize that the timing of assessment for mobilization should be early, within the first 24 hours of admission, and that readiness be determined according to the clinical and safety criteria recommended below.
Criteria for Determining Early Mobilization Readiness and Safety
Recommendation
We recommend that the decision to initiate and advance mobility be individualized for each patient, guided by clinical judgment, and involve an interprofessional team that includes therapists who are knowledgeable in mobilizing patients, and the clinicians who have ultimate responsibility for decision-making in the patient's overall care.
Rationale
EM has consistently been shown to be safe in critically ill adults including those requiring vasoactive infusions, mechanical ventilation, and invasive indwelling devices. 24 50 57 Evidence on the safety of EM in critically ill children is derived from observational studies (level 3), 12 21 23 38 39 58 59 or are opinion based. 60 This evidence to date demonstrates that EM is safe and feasible in critically ill children receiving mechanical ventilatory support, invasive monitoring, sedative and vasoactive infusions. Based on these data, we developed a system-based set of clinical safety criteria that prioritizes maintaining cardiorespiratory and neurologic stability and preventing patient discomfort and device dislodgement ( Table 3 ). Conditions at highest risk of adverse events even during bed rest, therefore, constitute contraindications to any mobilization until more evidence is available. Patients with conditions listed as “precautions,” may be mobilized according to the level of assistance required, but to exercise caution particularly when there are specific considerations, for example, fresh postoperative patient, mechanical ventilation, muscle paralysis. We included “acute spinal cord injury” and “strict spinal precautions” as precautions, to remind clinicians when possible, it is important to continue to mobilize the patient's limbs while maintaining in-line spinal stabilization. Select pediatric patients may participate in active rehabilitation and ambulate while on venovenous extracorporeal membrane oxygenation, in the context of a well-organized multidisciplinary program. 23 59 There was no consensus agreement on threshold doses of vasoactive infusions or degree of invasive mechanical ventilator support for which mobilization is contraindicated, hence each case should be discussed individually, and precaution exercised during mobilization. As the clinical status of each critically ill patient is often dynamic, safety should be assessed before, and during each mobilization event. We developed a safety checklist for use before the initiation of mobilization ( Table 4 ), and a set of safety criteria for suspending or aborting mobility physical therapy ( Table 5 ).
Table 3. Contraindications and precautions to mobilization in critically ill children.
| Contraindications (Not safe to mobilize, bed repositioning only) | |
|---|---|
| Hemodynamic instability |
|
| Respiratory instability |
|
| Neurological instability |
|
| Surgical |
|
| Precautions (special care, resources, and attention are required during mobilization of these patients) | |
| Cardiovascular |
|
| Respiratory |
|
| Neurological/neurosurgical |
|
| Orthopedic/musculoskeletal |
|
| Other |
|
Abbreviations: CPP, cerebral perfusion pressure; ECG, electrocardiogram; IV, intravenous.
Table 4. Premobilization safety checklist (for patients with precautions present).
| No contraindications present |
| Precautions reviewed |
| PT/OT has assessed the patient and set target activity goal(s) |
| Activity order and goals reviewed with the team (i.e., health care team, family, and patient, where possible) |
| Personnel required for mobilization available, e.g., PT, RN, and RT in patients requiring respiratory support |
| Airway and lines secured, dressings intact |
| Patient's analgesia and comfort is optimized (target as determined by the medical team, using institutional guidelines) |
Abbreviations: MD, medical doctor; OT, occupational therapist; PT, physiotherapist; RN, registered nurse; RT, respiratory therapist.
Table 5. Safety and tolerance criteria for interrupting, altering, or aborting mobilization therapy.
| Cardiorespiratory instability |
|
| CNS |
|
| Skin, wound, and joints |
|
| Device |
|
| Patient |
|
Abbreviations: BP, blood pressure; CPP, cerebral perfusion pressure; HR, heart rate; ICP, intracranial pressure; RR, respiratory rate; Spo 2 , peripheral capillary oxygen saturation.
Note: Occurrence of these events prompt an interruption, rest as appropriate, and reassessment of ability to continue with the same mobility plan, or readjustment to another mobility type and level.
Mobilization Frequency and “Dosage”
Recommendation
The nature of mobilization activities should focus on achieving age-appropriate functional tasks, while the duration and frequency depend on the patient's underlying condition. We suggest a goal of at least 30 minutes, once a day or in divided intervals, with the aim of increasing duration, frequency, and/or intensity according to the child's tolerance, response, and individualized functional activity goals as outlined in Table 2 . Prescriptions for mobilization should be reassessed regularly, and be conducted in consultation with a qualified therapist. Therapists may prescribe a combination of activities such that the patient is mobilized as many times a day as possible as is safe. To facilitate this in a limited resource setting, where appropriate, therapists may engage bedside caregivers (i.e., nurses, family members) in patient mobilization activities.
Rationale
Duration and intensity of activity are relevant to adequate physical, motor, and cognitive growth. Around 60 minutes daily or 250 minutes a week of moderate to vigorous-intensity physical activity is recommended for healthy children, while 150 minutes a week is recommended in adults. 61 Recommendations in the setting of acute or chronic illness are variable. 62 The dose response or frequency of mobilization that is most efficacious in preventing morbidity and optimizing functional recovery in critically ill patients is currently unclear. 63 The evidence from adult trials suggests that a minimum of 30 and up to 60 minutes a day is safe. 48 49 63 64 Our review of the pediatric evidence revealed that novel interventions such as in-bed cycling have been safely instituted in the range of 10 to 30 minutes, once to twice per day (level 3). 21 36 37 54 There is currently no evidence regarding the intensity of mobilization that is ideal for all critically ill adults or children. We, therefore, graded intensity in this population according to whether an activity is passive, active-assisted or actively applied ( Table 2 ). There are benefits to passive mobilization in patients who cannot actively participate, such as the prevention of skeletal muscle atrophy, and the preservation of joint mobility and arterial function. 41 65 This is particularly relevant in children where the population is heterogeneous in age, cognitive and functional ability, and subsequently cannot always comply with activities.
We summarize our recommendations in Fig. 1 . We used a “traffic light” color-coded system: red to denote contraindications, amber to denote precautions and safety thresholds, and green to denote mobilization activities should proceed. In order and foster a collaborative team approach to operationalizing these EM recommendations, we encourage the following three steps and questions to be assessed for each patient, every day. Step 1: Is it safe to move the patient? Step 2: What is the activity goal and what is the safe level of activity for the patient? Step 3: When can we mobilize the patient , when the safety criteria are met? Feedback from the stakeholders during the pilot phase allowed us to assess the sensibility of the listed precautions and contraindications, and to determine if following such guidelines was feasible.
Fig. 1.

Early mobilization recommendations for critically ill children. We used a “traffic light” color-coded system: Red to denote contraindications, amber to denote precautions and safety thresholds, and green to denote mobilization activities should proceed. AAROM, active assisted range of motion; AROM, active range of motion; BP, blood pressure; CPP, cerebral perfusion pressure; EVD, external ventricular drain; Fio 2 , fraction of inspired oxygen; HR, heart rate; ICP, intracranial pressure; OT, occupational therapist; PROM, passive range of motion; PT, physiotherapist; WOB, work of breathing.
Discussion
Functional recovery is a patient-centered outcome and is increasingly identified as a priority in critically ill children. 66 Rehabilitation has become a part of the adult ICU paradigm, and EM is now recommended as part of usual practice for critically ill adults. 26 The National Institute for Health and Care Excellence clinical guidelines on rehabilitation after critical illness, identified the need for high-quality randomized controlled trials to determine the most effective rehabilitation strategy for critically ill patients. 67 Subsequently, there is tremendous interest in not only preventing critical illness-acquired morbidities, but optimizing physical and mental health, and functional recovery in adult and pediatric survivors of critical illness.
A key barrier to acute rehabilitation within the PICU is physician discomfort and knowledge on what is appropriate, safe, and timely in this population. 12 As a result, bed rest and prolonged immobility is the current standard in many PICUs. 12 14 These practice recommendations incorporate currently available prospective efficacy, safety, and feasibility evidence, and consensus expert opinion that promotes a safe, bundled approach with a goal of minimizing morbidity and optimizing functional recovery in critically ill children. They raise awareness of the risks associated with immobility, prompt PICU clinicians to screen and assess their patients early, and serve to enhance communication in a collaborative approach to patient-centered care, and encourage family engagement. We consider mobilization as therapy and a targeted goal and encourage scheduling rehabilitation into the daily goals of care for critically ill children. Our aim was to alleviate the apprehension around mobilizing critically ill children, and encourage the safe progression from the lowest level to higher levels of mobility as the patient gains strength and endurance. We, therefore, provide recommendations for advancing from passive to active mobilization, as our pediatric population is heterogeneous, and may have limited ability to actively participate in exercise at best. These recommendations serve as a guide and should always be used in the context of specific individualized patient considerations, and in conjunction with an interprofessional team.
The strengths of this article are that these practice recommendations were developed: (1) through the engagement of a multidisciplinary group of experts with clinical and methodological expertise in adult and pediatric rehabilitation; (2) guided by the Institute of Medicine framework for developing clinical practice guidelines; (3) supported by currently available evidence obtained through a systematic review of the literature; and (4) refined through an iterative process that engaged other clinician stakeholders. The process of piloting the guidelines allowed us to receive key feedback on the feasibility of its implementation. Also, it allowed us to refine safety criteria, and upgrade some contraindications to precautions when clinicians began to understand that it is safe and important to begin in-bed mobility even in children who were traditionally perceived as “too unstable to move” or on significantly advanced life support. We emphasize that our consensus recommendations are based on panel agreement of good practice statements; we therefore consciously chose not to apply the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology inappropriately, given the low quality of existing evidence. 68
There are several limitations to these recommendations. The most obvious are the paucity of pediatric evidence in this field. While our recommendations on safety are supported by prospective pediatric data, due to the lack of clinical trial evidence, we acknowledge that our recommendations on the timing and “dosage” of mobilization are therefore largely opinion based. We, therefore, supported our recommendations where possible with safety criteria from ongoing registered trials and evidence from adult trials. Until more pediatric-specific evidence emerges, we cannot make any recommendations as to which types of patients may benefit most from EM, nor if EM indeed improves outcomes in all critically ill children. These guidelines are targeted at a general medical-surgical PICU population, and not specific subgroups of critically ill children with unique rehabilitation needs. Our objective is to promote a culture of safety while guiding a goal-oriented collaborative approach to minimize critical illness-acquired morbidities and optimize functional recovery. Finally, while we recommend EM as only one component of a bundled approach to rehabilitation in critically ill children, our assessment of the evidence and practice recommendations focused only on mobilization, as this was the primary objective of this article. 69
Prolonged bed rest and immobilization is no longer an acceptable standard of practice because of clear evidence of harm. However, operationalizing the change in practice is challenging in the PICU, given the current level of evidence and the limitations described earlier. 70 To reduce PICU-acquired morbidities and promote functional recovery, a logical process is first to establish good practice recommendations focused on safety and promoting awareness, developed through available evidence and expert consensus, and subsequently, validate and/or modify these guidelines through research. Emerging trials of EM and rehabilitation interventions in children will inform the safety and feasibility of these recommendations. 53 54 Future research on the efficacy of EM on clinically relevant outcomes will allow us to update these recommendations as prospective evidence accumulates. High priorities for research in this area include how best to implement mobility-based rehabilitation in critically ill children, with respect to optimal timing, intensity, and duration; to determine if there are subgroups of patients that are at greatest risk in whom we should prioritize for EM, or indeed refrain from implementing EM; to determine whether there is incremental benefit when EM is administered together with the other components of a rehabilitation care bundle; supplemented by qualitative and quantitative research that will help us determine how best to administer rehabilitation in an interprofessional way, that includes patient and family engagement.
Conclusion
The objectives of these EM guidelines are to educate clinicians, encourage safe practices, reduce PICU-acquired morbidities, and promote functional recovery in critically ill children. They were developed from a growing need to ensure best possible practices for critically ill children in tandem with emerging evidence and to avoid suboptimal care because of a lack of knowledge, comfort, or high-level evidence. Though early recognition and resuscitation are the mainstays of initial treatment in critically ill patients when survival is our goal, as patients stabilize, our attention should turn to early rehabilitation and recovery , to improve survival outcomes.
Acknowledgments
The authors thank Dr. Sue Apkon for her thorough and thoughtful review of this article. The authors also thank Ms. Racquel Simpson and Dr. Samah Al-Harbi who conducted the literature search and data abstraction for the systematic review.
Authors' Contributions
K.C. conceived of the study and drafted and revised the article. K.C., R.S., and S.A. performed the systematic review. K.C., F.C., H.C., and C.N. drafted the tables and figures. All authors participated in the development of each of the practice recommendations. All authors contributed to the interpretation of results and reviewed and edited the article. All authors approved the final submitted version for publication.
Appendix.
References
- 1.Pollack M M, Holubkov R, Funai T et al. Pediatric intensive care outcomes: development of new morbidities during pediatric critical care. Pediatr Crit Care Med. 2014;15(09):821–827. doi: 10.1097/PCC.0000000000000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Needham D M, Davidson J, Cohen H et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med. 2012;40(02):502–509. doi: 10.1097/CCM.0b013e318232da75. [DOI] [PubMed] [Google Scholar]
- 3.Iwashyna T J, Ely E W, Smith D M, Langa K M. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–1794. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knoester H, Bronner M B, Bos A P. Surviving pediatric intensive care: physical outcome after 3 months. Intensive Care Med. 2008;34(06):1076–1082. doi: 10.1007/s00134-008-1061-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Desai S V, Law T J, Needham D M. Long-term complications of critical care. Crit Care Med. 2011;39(02):371–379. doi: 10.1097/CCM.0b013e3181fd66e5. [DOI] [PubMed] [Google Scholar]
- 6.Biagas K V, Hough R F.Post-intensive care syndrome: A look at PICU outcomes Pediatr Crit Care Med 201617111101. Doi: 10.1097/PCC.0000000000000975 [DOI] [PubMed] [Google Scholar]
- 7.Kayambu G, Boots R, Paratz J. Physical therapy for the critically ill in the ICU: a systematic review and meta-analysis. Crit Care Med. 2013;41(06):1543–1554. doi: 10.1097/CCM.0b013e31827ca637. [DOI] [PubMed] [Google Scholar]
- 8.Adler J, Malone D. Early mobilization in the intensive care unit: a systematic review. Cardiopulm Phys Ther J. 2012;23(01):5–13. [PMC free article] [PubMed] [Google Scholar]
- 9.Stiller K. Physiotherapy in intensive care: an updated systematic review. Chest. 2013;144(03):825–847. doi: 10.1378/chest.12-2930. [DOI] [PubMed] [Google Scholar]
- 10.Cuthbertson B H, Rattray J, Campbell M Ket al. The PRaCTICaL study of nurse led, intensive care follow-up programmes for improving long term outcomes from critical illness: a pragmatic randomised controlled trial BMJ 2009339b3723. Doi: 10.1136/bmj.b3723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bourgeois F T, Murthy S, Pinto C, Olson K L, Ioannidis J P, Mandl K D. Pediatric versus adult drug trials for conditions with high pediatric disease burden. Pediatrics. 2012;130(02):285–292. doi: 10.1542/peds.2012-0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choong K, Foster G, Fraser D D et al. Acute rehabilitation practices in critically ill children: a multicenter study. Pediatr Crit Care Med. 2014;15(06):e270–e279. doi: 10.1097/PCC.0000000000000160. [DOI] [PubMed] [Google Scholar]
- 13.Cremer R, Leclerc F, Lacroix J, Ploin D; GFRUP/RMEF Chronic Diseases in PICU Study Group.Children with chronic conditions in pediatric intensive care units located in predominantly French-speaking regions: Prevalence and implications on rehabilitation care need and utilization Crit Care Med 200937041456–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bybee J, Sorce L, Ciolino J, Bone M. Mobility practices in the PICU. Crit Care Med. 2015;43(12) 01:213–214. [Google Scholar]
- 15.Choong K, Koo K K, Clark H et al. Early mobilization in critically ill children: a survey of Canadian practice. Crit Care Med. 2013;41(07):1745–1753. doi: 10.1097/CCM.0b013e318287f592. [DOI] [PubMed] [Google Scholar]
- 16.Calvo-Ayala E, Khan B A, Farber M O, Ely E W, Boustani M A. Interventions to improve the physical function of ICU survivors: a systematic review. Chest. 2013;144(05):1469–1480. doi: 10.1378/chest.13-0779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shaklai S, Peretz R, Spasser R, Simantov M, Groswasser Z. Long-term functional outcome after moderate-to-severe paediatric traumatic brain injury. Brain Inj. 2014;28(07):915–921. doi: 10.3109/02699052.2013.862739. [DOI] [PubMed] [Google Scholar]
- 18.Creighton D E, Robertson C M, Sauve R S et al. Neurocognitive, functional, and health outcomes at 5 years of age for children after complex cardiac surgery at 6 weeks of age or younger. Pediatrics. 2007;120(03):e478–e486. doi: 10.1542/peds.2006-3250. [DOI] [PubMed] [Google Scholar]
- 19.Cameron E C, Maehle V, Reid J. The effects of an early physical therapy intervention for very preterm, very low birth weight infants: a randomized controlled clinical trial. Pediatr Phys Ther. 2005;17(02):107–119. doi: 10.1097/01.pep.0000163073.50852.58. [DOI] [PubMed] [Google Scholar]
- 20.Graham R J, Mancher M, Miller Wolman D, Greenfield S, Steinberg E, eds.Clinical Practice Guidelines We Can Trust. Committee on Standards for Developing Trustworthy Clinical Practice Guidelines Washington, DC: The National Academies Press; 2011 [PubMed] [Google Scholar]
- 21.Choong K, Chacon M, Walker R et al. In- bed mobilization in critically ill children: a safety and feasibility trial. J Pediatr Intensive Care. 2015;4(02):225–234. doi: 10.1055/s-0035-1563545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hollander S A, Hollander A J, Rizzuto S, Reinhartz O, Maeda K, Rosenthal D N. An inpatient rehabilitation program utilizing standardized care pathways after paracorporeal ventricular assist device placement in children. J Heart Lung Transplant. 2014;33(06):587–592. doi: 10.1016/j.healun.2013.12.009. [DOI] [PubMed] [Google Scholar]
- 23.Zebuhr C, Sinha A, Skillman H, Buckvold S. Active rehabilitation in a pediatric extracorporeal membrane oxygenation patient. PM R. 2014;6(05):456–460. doi: 10.1016/j.pmrj.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 24.Hodgson C L, Stiller K, Needham D Met al. Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults Crit Care 20141806658. Doi: 10.1186/s13054-014-0658-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Perme C, Chandrashekar R. Early mobility and walking program for patients in intensive care units: creating a standard of care. Am J Crit Care. 2009;18(03):212–221. doi: 10.4037/ajcc2009598. [DOI] [PubMed] [Google Scholar]
- 26.Berry A, Beattie K, Bennett J . New South Wales, Australia: Agency for Clinical Innovation NSW Government; 2014. Physical Activity and Movement: A Guideline for Critically Ill Adults. [Google Scholar]
- 27.Gosselink R, Bott J, Johnson M et al. Physiotherapy for adult patients with critical illness: recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on Physiotherapy for Critically Ill Patients. Intensive Care Med. 2008;34(07):1188–1199. doi: 10.1007/s00134-008-1026-7. [DOI] [PubMed] [Google Scholar]
- 28.Howick J, Chalmers I, Glasziou P http://www.cebm.net/index.aspx?o=5653 http://www.cebm.net/index.aspx?o=5653
- 29.Morandi A, Brummel N E, Ely E W. Sedation, delirium and mechanical ventilation: the ‘ABCDE’ approach. Curr Opin Crit Care. 2011;17(01):43–49. doi: 10.1097/MCC.0b013e3283427243. [DOI] [PubMed] [Google Scholar]
- 30.Balas M C, Vasilevskis E E, Olsen K M et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med. 2014;42(05):1024–1036. doi: 10.1097/CCM.0000000000000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Curley M A, Meyer E. Philadelphia, PA: WB Saunders Company; 2001. Caring practices: the impact of the critical care experience on the family; pp. 47–68. [Google Scholar]
- 32.Camden C, Shikako-Thomas K, Nguyen T et al. Engaging stakeholders in rehabilitation research: a scoping review of strategies used in partnerships and evaluation of impacts. Disabil Rehabil. 2015;37(15):1390–1400. doi: 10.3109/09638288.2014.963705. [DOI] [PubMed] [Google Scholar]
- 33.Skillman H E, Zebuhr C A. Optimal nutrition for acute rehabilitation in the PICU. J Pediatr Intensive Care. 2015;4(02):194–203. doi: 10.1055/s-0035-1563546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Verghese A. Culture shock–patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748–2751. doi: 10.1056/NEJMp0807461. [DOI] [PubMed] [Google Scholar]
- 35.Fontaine D K, Briggs L P, Pope-Smith B. Designing humanistic critical care environments. Crit Care Nurs Q. 2001;24(03):21–34. doi: 10.1097/00002727-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Abdulsatar F, Walker R G, Timmons B W, Choong K. “Wii-Hab” in critically ill children: a pilot trial. J Pediatr Rehabil Med. 2013;6(04):193–204. doi: 10.3233/PRM-130260. [DOI] [PubMed] [Google Scholar]
- 37.Choong K, Awladthani S, Khawaji A https://clinicaltrials.gov/ct2/show/NCT02358577?term=wEECYCLE&rank=1 https://clinicaltrials.gov/ct2/show/NCT02358577?term=wEECYCLE&rank=1
- 38.Wieczorek B, Ascenzi J, Kim Y et al. PICU Up!: Impact of a quality improvement program to promote early mobilization in critically ill children. Ped Crit Care Med. 2016;17(12):e559–e566. doi: 10.1097/PCC.0000000000000983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsuboi N, Nozaki H, Ishida Y et al. Early mobilization after pediatric liver transplantation. J Pediatr Intensive Care. 2016;6(01) doi: 10.1055/s-0036-1593387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Choong K, Tran N, Clark H, Cupido C, Corsi D. Acute rehabilitation in critically ill children. J Pediatr Intensive Care. 2012;1:183–192. doi: 10.3233/PIC-12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Phillips A A, Cote A T, Warburton D E. A systematic review of exercise as a therapeutic intervention to improve arterial function in persons living with spinal cord injury. Spinal Cord. 2011;49(06):702–714. doi: 10.1038/sc.2010.193. [DOI] [PubMed] [Google Scholar]
- 42.Puthucheary Z A, Rawal J, McPhail M et al. Acute skeletal muscle wasting in critical illness. JAMA. 2013;310(15):1591–1600. doi: 10.1001/jama.2013.278481. [DOI] [PubMed] [Google Scholar]
- 43.Bernhardt J, Langhorne P, Lindley R Iet al. Efficacy and safety of very early mobilisation within 24 h of stroke onset (AVERT): a randomised controlled trial Lancet 2015386(9988):46–55. [DOI] [PubMed] [Google Scholar]
- 44.Burtin C, Clerckx B, Robbeets C et al. Early exercise in critically ill patients enhances short-term functional recovery. Crit Care Med. 2009;37(09):2499–2505. doi: 10.1097/CCM.0b013e3181a38937. [DOI] [PubMed] [Google Scholar]
- 45.Schweickert W D, Pohlman M C, Pohlman A Set al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial Lancet 2009373(9678):1874–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Denehy L, Skinner E H, Edbrooke Let al. Exercise rehabilitation for patients with critical illness: a randomized controlled trial with 12 months of follow-up Crit Care 20131704R156. Doi: 10.1186/cc12835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morris P E, Berry M J, Files D C et al. Standardized rehabilitation and hospital length of stay among patients with acute respiratory failure: a randomized clinical trial. JAMA. 2016;315(24):2694–2702. doi: 10.1001/jama.2016.7201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moss M, Nordon-Craft A, Malone D et al. A randomized trial of an intensive physical therapy program for patients with acute respiratory failure. Am J Respir Crit Care Med. 2016;193(10):1101–1110. doi: 10.1164/rccm.201505-1039OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hodgson C L, Bailey M, Bellomo R et al. A binational multicenter pilot feasibility randomized controlled trial of early goal-directed mobilization in the ICU. Crit Care Med. 2016;44(06):1145–1152. doi: 10.1097/CCM.0000000000001643. [DOI] [PubMed] [Google Scholar]
- 50.Brummel N E, Girard T D, Ely E W et al. Feasibility and safety of early combined cognitive and physical therapy for critically ill medical and surgical patients: the Activity and Cognitive Therapy in ICU (ACT-ICU) trial. Intensive Care Med. 2014;40(03):370–379. doi: 10.1007/s00134-013-3136-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kho M E.CYCLE pilot randomized trial. ClinicalTrialsgov identifier: NCT02377830. Available at:https://clinicaltrials.gov/ct2/show/NCT02377830
- 52.Remonidini R, Valerio N, Barcellos P, do Prado C, Santos E.Early mobilization in Children under invasive and noninvasive positive pressure ventilation: Description and preliminary results of a new protocol. Abstract presented at: 2012 International Conference of the American Thoracic SocietyMay 18–23, 2012San Francisco, CA. Abstract A1832 [Google Scholar]
- 53.Fink E.RCT: Early rehabilitation protocol vs. usual care in pediatric ICU for children with acute brain injury. Clinicaltrialsgov identifier: NCT02209935. Available at:https://clinicaltrials.gov/ct2/show/NCT02209935
- 54.Choong K, Al-Harbi S, Alothani S
- 55.Kress J P, Hall J B. ICU-acquired weakness and recovery from critical illness. N Engl J Med. 2014;370(17):1626–1635. doi: 10.1056/NEJMra1209390. [DOI] [PubMed] [Google Scholar]
- 56.Lee C M, Fan E.ICU-acquired weakness: what is preventing its rehabilitation in critically ill patients? BMC Med 20121001115. Doi: 10.1186/1741-7015-10-115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bailey P, Thomsen G E, Spuhler V J et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med. 2007;35(01):139–145. doi: 10.1097/01.CCM.0000251130.69568.87. [DOI] [PubMed] [Google Scholar]
- 58.Jacobs B R, Salman B A, Cotton R T, Lyons K, Brilli R J. Postoperative management of children after single-stage laryngotracheal reconstruction. Crit Care Med. 2001;29(01):164–168. doi: 10.1097/00003246-200101000-00032. [DOI] [PubMed] [Google Scholar]
- 59.Turner D A, Cheifetz I M, Rehder K J et al. Active rehabilitation and physical therapy during extracorporeal membrane oxygenation while awaiting lung transplantation: a practical approach. Crit Care Med. 2011;39(12):2593–2598. doi: 10.1097/CCM.0b013e3182282bbe. [DOI] [PubMed] [Google Scholar]
- 60.Roeseler J, Sottiaux T, Lemiale V et al. Prise en charge de la mobilisation précoce en réanimation, chez l'adulte et l'enfant (électrostimulation incluse) Reanimation. 2013;22(02):207–218. [Google Scholar]
- 61.Canadian Society for Exercise Physiology. Canadian Physical Activity Guidelines; Canadian Sedentary Behaviour Guidelines. Available at:http://www.csep.ca/cmfiles/guidelines/csep_guidelines_handbook.pdf
- 62.Riner W F, Sellhorst S H. Physical activity and exercise in children with chronic health conditions. J Sport Health Sci. 2013;2(01):12–20. [Google Scholar]
- 63.Castro-Avila A C, Serón P, Fan E, Gaete M, Mickan S.Effect of early rehabilitation during intensive care unit stay on functional status: systematic review and meta-analysis PLoS One 20151007e0130722. Doi: 10.1371/journal.pone.0130722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kho M E, Martin R A, Toonstra A L et al. Feasibility and safety of in-bed cycling for physical rehabilitation in the intensive care unit. J Crit Care. 2015;30(06):14190–1.419E8. doi: 10.1016/j.jcrc.2015.07.025. [DOI] [PubMed] [Google Scholar]
- 65.Dirks M L, Hansen D, Van Assche A, Dendale P, Van Loon L J. Neuromuscular electrical stimulation prevents muscle wasting in critically ill comatose patients. Clin Sci (Lond) 2015;128(06):357–365. doi: 10.1042/CS20140447. [DOI] [PubMed] [Google Scholar]
- 66.Odetola F O. Outcomes research in the PICU. Pediatr Crit Care Med. 2014;1:107–116. [Google Scholar]
- 67.Lancaster G A. Pilot and feasibility studies come of age! Pilot Feasibil Studies. 2015;1(01):1–4. doi: 10.1186/2055-5784-1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Guyatt G H, Schünemann H J, Djulbegovic B, Akl E A. Guideline panels should not GRADE good practice statements. J Clin Epidemiol. 2015;68(05):597–600. doi: 10.1016/j.jclinepi.2014.12.011. [DOI] [PubMed] [Google Scholar]
- 69.Carcillo J A, Fields A I; American College of Critical Care Medicine Task Force Committee Members.Clinical practice parameters for hemodynamic support of pediatric and neonatal patients in septic shock Crit Care Med 200230061365–1378. [DOI] [PubMed] [Google Scholar]
- 70.Munkwitz M, Hopkins R O, Miller Iii R R, Luckett P M, Hirshberg E L. A perspective on early mobilization for adult patients with respiratory failure: Lessons for the pediatric population. J Pediatr Rehabil Med. 2010;3(03):215–227. doi: 10.3233/PRM-2010-0130. [DOI] [PubMed] [Google Scholar]


