Abstract
Systemic capillary leak syndrome (SCLS) is a potentially life-threatening disorder characterized by distributive shock, hypoalbuminemia, and hemoconcentration. It is exceedingly rare in children with less than 20 cases reported to date. The underlying cause for this syndrome remains largely unknown and acute treatment has remained mainly supportive. Prophylaxis with intravenous immunoglobulin (IVIG) has been shown to successfully prevent further episodes in both adults and children. We present a case of a 2-year-old previously healthy male admitted to the pediatric intensive care unit with a clinical course consistent with SCLS. His shock was refractory to aggressive fluid and vasopressor support. Reversal of SCLS with IVIG given in the acute phase had been described in three adult subjects, and for this reason, the decision was made to administer IVIG. Within an hour of administration, hemodynamics stabilized and vasopressor support could be weaned. He has had no further episodes on prophylactic infusions of IVIG. Although the exact mechanism of IVIG in SCLS is unknown, it has proven to be an effective and safe prophylactic therapy, and in our patient, it drastically reversed the acute capillary leak. We suggest that IVIG should be considered as acute therapy in pediatric patients with refractory shock and a clinical course suggestive of SCLS.
Keywords: systemic capillary leak syndrome, intravenous immunoglobulin, hemoconcentration, hypoalbuminemia
Introduction
Systemic capillary leak syndrome (SCLS), also known as Clarkson's disease, was first reported in 1960 by Clarkson et al who described a patient presenting with cyclical edema and shock due to increased capillary permeability. The syndrome is a rare but potentially life-threatening disorder marked by recurrent, acute episodes of hypotension, generalized edema, hypoalbuminemia, and hemoconcentration. Although the exact pathogenesis remains unknown, SCLS appears to result from transient endothelial dysfunction and hyperpermeability causing a loss of plasma into the extravascular space. 1 2
Less than 300 cases of SCLS have been described in the literature. The syndrome is exceedingly rare in children, with less than 20 cases reported to date. In adults, SCLS is most commonly seen in middle-aged men, many of whom have a monoclonal gammopathy. In this population, infections do not appear to be an important trigger for episodes. In contrast, in children diagnosed with SCLS, monoclonal gammopathies have not been described and most acute episodes follow an infection, usually of viral origin. 3 4 The literature about SCLS in pediatric patients consists mainly of case reports, with the largest case series describing six patients. Cytokine profiles obtained in these children were found to have elevated levels of chemokine (C–C motif) ligand 2, interleukin-8, and tumor necrosis factor α (TNF-α), as compared with a control group of healthy children. The majority of them also had low complement levels (C3 and C4). 3 How this is related to the clinical picture of capillary leak is not completely understood, although it is known that cytokines and active component can both cause endothelial damage. A recently published study showed that endothelial cells in a pediatric patient with SCLS were hypersensitive to TNF-α (and lipopolysaccharide), with an exaggerated decrease in barrier function in response to stimulation. 5
Preventive treatments, including terbutaline, theophylline, or intravenous immunoglobulin (IVIG) have been shown to decrease or prevent further episodes in both adults and children. 3 6 7 Treatment in the acute phase, however, is mainly supportive with judicious fluid resuscitation and use of vasopressors. IVIG given in the acute phase has been described to dramatically reverse SCLS in a few adult cases but has not been extensively studied or described in children. 8
Case
We present a 2-year-old, previously healthy male, who was admitted with recurrent episodes of distributive shock following viral infections.
The patient first presented in shock with a 1-day history of vomiting and lethargy and required intraosseous needle placement, aggressive fluid resuscitation, and pediatric intensive care unit admission. Laboratory evaluation demonstrated positive influenza B viral antigen and elevated creatinine kinase, while bacterial blood and urine cultures were negative. He was discharged with a diagnosis of viral shock and myositis.
Three months later, the patient again presented in shock. The day prior to presentation, he had been seen in a primary care office due to fever, cough, and periorbital edema. He was prescribed amoxicillin for otitis media, dexamethasone for croup, and cetirizine for a possible allergic reaction. On the morning of admission, he was lethargic and had worsening periorbital edema. At an outside institution emergency department (ED), laboratory evaluation was remarkably only for an elevated hemoglobin (18.3 g/dL and hematocrit [Hct] of 51.8%) and low total protein (4.5 g/dL). He was treated for croup and dehydration before being transferred to our institution in stable condition. On arrival to our ED approximately 30 minutes later, he was lethargic, cyanotic, tachycardic, and hypotensive with severe periorbital edema. He required intubation and was treated per septic shock protocol with fluids and antibiotics. Laboratory evaluation showed hemoconcentration with a hemoglobin of 20 g/dL, Hct of 60%, and albumin of 0.7 g/dL. His inflammatory markers were not elevated. Over the course of the next few hours, he received further fluid resuscitation, required escalating doses of dopamine, epinephrine, and vasopressin, and was given stress dose hydrocortisone. Fluid resuscitation resulted in small but nonsustained improvement in hemodynamics. A bedside echocardiogram showed a pericardial effusion with possible tamponade physiology and a bedside pericardiocentesis was performed with immediate, however nonsustained, hemodynamic stability. He continued to require frequent isotonic crystalloid fluid boluses due to persistent hypotension despite aggressive vasopressor support.
Twelve hours after the admission, the decision was made to administer IVIG (2 g/kg) for possible SCLS. At the time of IVIG administration, the patient had received 250 mL/kg of isotonic crystalloids. At the completion of the IVIG infusion, his hemodynamics had stabilized and he received a last 10 mL/kg bolus of isotonic crystalloid fluids, after which no further resuscitation fluids were needed ( Fig. 1 ), and vasopressin, epinephrine, and dopamine infusions were weaned rapidly. Aggressive diuretic therapy was administered within 12 hours. The patient developed compartment syndrome of his lower extremity, a known complication of SCLS, and underwent a fasciotomy. Respiratory viral antigen testing was positive for human metapneumovirus. The patient was discharged home on hospital day 11 and remains in good health. He is being followed up in the infectious disease clinic where he receives monthly prophylactic treatment with IVIG (2 g/kg), which has been described previously in the literature, and he has had no further episodes to date.
Fig. 1.
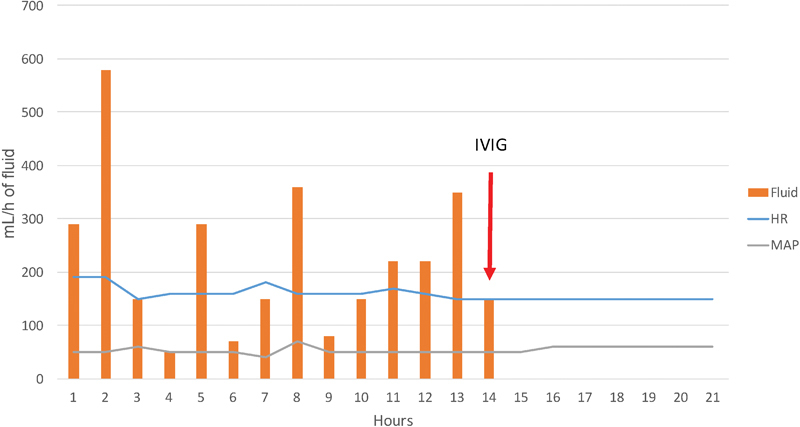
Massive fluid resuscitation was given until the time of IVIG administration, after which blood pressure stabilized and no further fluid boluses were needed. HR, heart rate; IVIG, intravenous immunoglobulin; MAP, mean arterial pressure.
Discussion
Due to its rare presentation, SCLS is likely under recognized. In children, the syndrome often presents in conjunction with viral infections and can be misdiagnosed as septic shock. Initial treatment is thus empiric, aimed at restoring hemodynamic stability. At the time of our patient's first presentation, he was presumed to have viral sepsis with septic shock and recovered with fluid resuscitation. During his second episode, however, he developed severe, treatment resistant, distributive shock that was nonresponsive to massive fluid resuscitation and several vasopressors. Administration of IVIG appeared to dramatically reverse his capillary leak and restore his hemodynamics. While further studies are needed to prove the causality of IVIG and reversal of capillary leak, the timing of IVIG administration to patient stability in our case strongly suggests a correlation.
Although there are some recommendations to use IVIG as preventive therapy for pediatric patients with SCLS, no recommendations for the acute phase exist. IVIG was reported by Lambert et al in 2008 as having drastically reversed SCLS in three adult patients, one patient with chronic SCLS and treatment-resistant peripheral edema and two patients with acute presentations and hypotensive shock. All three patients were alive and well maintained on prophylactic IVIG without further episodes several years later. 8
A few previous pediatric case reports on SCLS mention IVIG administration as part of the acute treatment. In three of them, it was part of a multitude of treatment approaches with favorable outcome; however, it is not clear what immediate effect the IVIG had. 9 10 11 One patient with a previous diagnosis of lymphoma was treated with clofarabine and developed SCLS, presumably as a side effect of the drug. He was treated with IVIG with reversal of the capillary leak. 12
The exact mechanism of IVIG in SCLS is not clear, as the pathogenesis of the syndrome itself remains unclear, but transient endothelial dysfunction seems to play a major role. There have been suggestions of abnormal cytokine and complement profiles as well as endothelial hyperreactivity in patients with SCLS. 3 5 IVIG is known to have several different immune modulatory properties, including interacting with antibodies, cytokines, and complement, and modulating autoreactivity, all of which may help in restore normal endothelial permeability.
Conclusion
In conclusion, pediatric SCLS is a very rare, potentially fatal, and likely underdiagnosed condition. The diagnosis should be considered in patients presenting in fluid-refractory hypovolemic or distributive shock, especially if accompanied by peripheral edema, hemoconcentration, or profound hypoalbuminemia. Although the exact mechanism remains unknown, IVIG has proven to be an effective and safe prophylactic treatment that prevents further episodes in both adult and pediatric patients. IVIG has also been reported to acutely reverse SCLS in adult subjects, may have played a role in acute improvement in previous pediatric cases, and drastically reversed the capillary leak in our patient. Despite the small sample size to date, we suggest that IVIG shows potential as an acute therapy to mitigate the hemodynamic compromise in acute episodes of shock due to SCLS and should be considered to reverse acute SCLS in pediatric patients.
Conflict of Interest None.
Note
The views expressed in this article are those of the authors and do not reflect the official policy of the Navy, Department of Defense, or U.S. Government.
References
- 1.Clarkson B, Thompson D, Horwith M, Luckey E H. Cyclical edema and shock due to increased capillary permeability. Am J Med. 1960;29:193–216. doi: 10.1016/0002-9343(60)90018-8. [DOI] [PubMed] [Google Scholar]
- 2.Druey K M, Greipp P R. Narrative review: the systemic capillary leak syndrome. Ann Intern Med. 2010;153(02):90–98. doi: 10.1059/0003-4819-153-2-201007200-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hsu P, Xie Z, Frith K et al. Idiopathic systemic capillary leak syndrome in children. Pediatrics. 2015;135(03):e730–e735. doi: 10.1542/peds.2014-2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perme T, Pokorn M, Markelj G et al. Two episodes of systemic capillary leak syndrome in an 8-year-old boy, following influenza A virus infection. Pediatr Infect Dis J. 2014;33(02):222–224. doi: 10.1097/INF.0000000000000029. [DOI] [PubMed] [Google Scholar]
- 5.Pierce R, Khokha M, Kluger M, Lavik J P, Pober J. Pediatric systemic capillary leak syndrome endothelial cells are hypersensitive to TNF-[alpha] and LPS. Crit Care Med. 2015;43(12):25–26. [Google Scholar]
- 6.Gousseff M, Arnaud L, Lambert M et al. The systemic capillary leak syndrome: a case series of 28 patients from a European registry. Ann Intern Med. 2011;154(07):464–471. doi: 10.7326/0003-4819-154-7-201104050-00004. [DOI] [PubMed] [Google Scholar]
- 7.Xie Z, Chan E C, Long L M, Nelson C, Druey K M. High-dose intravenous immunoglobulin therapy for systemic capillary leak syndrome (Clarkson disease) Am J Med. 2015;128(01):91–95. doi: 10.1016/j.amjmed.2014.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lambert M, Launay D, Hachulla E et al. High-dose intravenous immunoglobulins dramatically reverse systemic capillary leak syndrome. Crit Care Med. 2008;36(07):2184–2187. doi: 10.1097/CCM.0b013e31817d7c71. [DOI] [PubMed] [Google Scholar]
- 9.Kerketta J, Lodh M, Mandal K. Clarkson disease—systemic capillary leak syndrome in a 6-year-old girl: case report. Paediatr Int Child Health. 2015;35(02):160–163. doi: 10.1179/2046905514Y.0000000161. [DOI] [PubMed] [Google Scholar]
- 10.Iwasa T, Ohashi H, Kihira K et al. 10-year-old girl with life-threatening idiopathic systemic capillary leak syndrome: a case report. BMC Pediatr. 2014;14:137. doi: 10.1186/1471-2431-14-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karatzios C, Gauvin F, Egerszegi E P et al. Systemic capillary leak syndrome presenting as recurrent shock. Pediatr Crit Care Med. 2006;7(04):377–379. doi: 10.1097/01.PCC.0000227120.61949.FB. [DOI] [PubMed] [Google Scholar]
- 12.Kesik V, Atas E, Korkmazer N, Babacan O. Clofarabine associated capillary leak syndrome in a child with lymphoma successfully treated with intravenous immunoglobulin. J Cancer Res Ther. 2015;11(03):653. doi: 10.4103/0973-1482.138028. [DOI] [PubMed] [Google Scholar]


