Abstract
A 46 year old lady presented three weeks after an oesophagectomy for oesophageal carcinoma with increasing breathlessness and a large left-sided pleural effusion. Computed tomography (CT) scan of her thorax, abdomen and pelvis revealed a large left-sided and small right-sided pleural effusions, a pericardial effusion, ascites and intra-abdominal lymphadenopathy. The patient underwent both pericardial and pleural fluid drainage, however, unfortunately, deteriorated despite these interventions with increasing oxygen requirements requiring nasal high flow oxygen on the Intensive Care Unit. Her pleural and pericardial collections resolved with colchicine and later introduction of prednisolone over a period of 5 weeks. Polyserositis is well recognised after cardiac surgery, but such a dramatic complication after thoracotomy for non-cardiac surgery has as not previously been reported. The polyserositis may relate to the induction chemotherapy combined with surgery.
1. Case
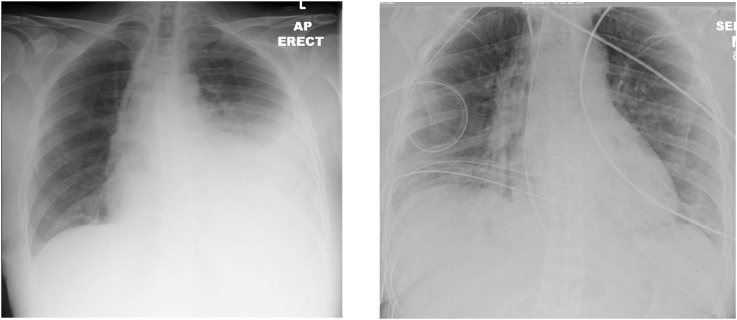
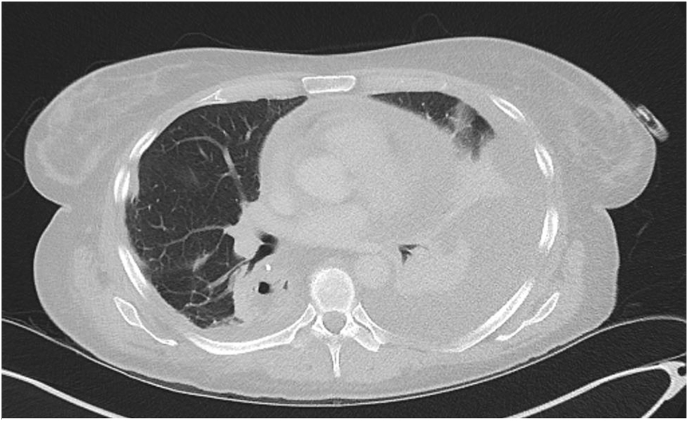
A 46 year old woman presented with 3 days increasing breathlessness 2 weeks after an open oesophagectomy for oesophageal adenocarcinoma, following pre-operative chemotherapy and radiotherapy. On examination, she was afebrile, saturations of 95% on room air, and had signs of a left pleural effusion. Chest radiograph (Fig. 1a) confirmed a significant left-sided pleural effusion and blood investigations showed serum albumin 18g/L and C-reactive protein of 70mg/L. CT scan of the chest confirmed a moderate left pleural effusion, a smaller right-sided pleural effusion, also a pericardial effusion and ascites. (Fig. 2). Fig. 1b is a chest radiograph of patient the day after her oesophagecomy demonstrating no evidence of a pleural effusion at this time.
Fig. 1.
a. Chest radiograph on admission showing large left-sided pleural effusion b. Chest radiograph day after surgery (2 weeks prior to CXR in Fig. 1a).
Fig. 2.
Admission CT thorax showing bilateral pleural effusions (left larger than right) with large pericardial effusion.
The initial working diagnosis was fluid accumulation secondary to a low protein state following surgery. Thoracocentesis of the left chest revealed straw-coloured non-chylous, exudative pleural fluid (pleural fluid glucose 5.5mmol/L, LDH 355U/L, pleural fluid protein 29g/L, serum protein 54g/L, triglycerides not checked given clinical appearance). She developed significant pleuritic chest discomfort after this procedure and became progressively more unwell that day with tachycardia, hypotension and increasing oxygen requirements. Urgent transthoracic echocardiography confirmed a significant pericardial effusion but good cardiac function. Therapeutic pericardiocentesis of 550ml blood-stained pericardial fluid was performed which improved her haemodynamic parameters. She was transferred to the Intensive Care Unit for nasal high flow oxygen.
Pleural and pericardial fluid culture was sterile and urinary pneumococcal and legionella antigen testing was negative. Pleural fluid cytology revealed mesothelial cells with normal and reactive features, scattered neutrophils and lymphocytes. Pericardial fluid also showed a mixed inflammatory cell population of polymorphs, lymphocytes and occasional macrophages and no malignant cells. Auto-immune profile was negative. Blood tests showed persistent inflammation (C-reactive protein 135mg/L) consistent with idiopathic polyserositis and colchicine (500 μg twice daily) was commenced. Broad spectrum antibiotics (5 day course of Piperacillin/tazobactam) had been administered although blood cultures were sterile.
Subsequently there was a gradual clinical and radiological improvement. Repeat echocardiography 3 days later reassuringly showed minimal pericardial fluid. 7 days after admission, and 4 days after initiation of colchicine, the patient no longer had any oxygen requirement and was discharged. CXR on discharge showed dramatic improvement in the right pleural effusion, but a small residual left pleural effusion remained.
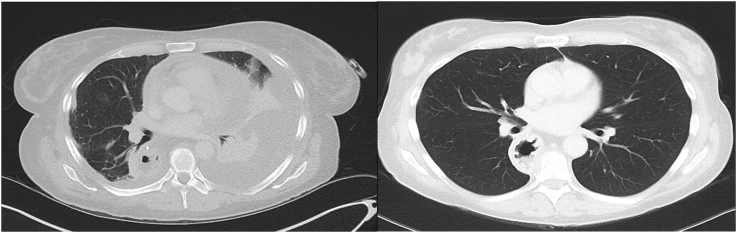
Review of the patient the following week revealed recurrence of a moderate free-flowing left-sided pleural collection and small right-sided effusion on CXR and ultrasound. Thoracocentesis of 1.3L was performed. She was commenced on corticosteroids given the re-accumulation despite a week of colchicine, (30mg prednisolone (0.5mg/kg)) for 1 month then weaning by 5mg/week alongside continuing 500 μg twice daily colchicine. Subsequent reviews showed gradual resolution of both pleural collections and 5 months later, a repeat CT thorax/abdomen/pelvis showed complete resolution of the effusions (Fig. 3). The patient was asymptomatic and had made a full recovery from this acute event. In total she received 3 months colchicine.
Fig. 3.
CT thorax (left image) shows bilateral pleural effusions and pericardial effusion on admission. CT thorax (right image) shows complete radiological resolution of the pleural and pericardial effusions on repeat imaging 5 months later.
2. Discussion
Pericardial and pleural effusions are recognised complications after cardiac surgery, with a reported incidence of 1%–2% [[1], [2], [3]]. However, there are no reports of life-threatening polyserositis occurring after oesophagectomy. Benign pericardial and pleural effusions have been reported in cases after oesophageal surgery, (especially chylous effusions related to thoracic duct trauma). Pericardial and pleural effusions occurring after radiotherapy for oesophageal cancer have been reported and a large case series does suggest that chemo-radiotherapy (CRT) is implicated in increasing the likelihood of such complications following oesophagectomy [4,5]. The risk of pleural and pericardial effusions may be twice and five-fold increased respectively with induction CRT compared to surgery alone with pericardial intervention in particular more frequently required after pre-operative CRT [6]. The underlying mechanism is likely related to direct toxicity to the mediastinum from radiotherapy in addition to chemotherapy potentially causing a protein-losing enteropathy, combined with disruption of lymphatic drainage by surgery [[7], [8], [9], [10]]. Our patient had more dramatic polyserositis requiring high level of anti-inflammatory treatment than has previously been reported. In addition, her last dose of chemoradiotherapy was 2 months prior to her surgery.
We employed a therapeutic strategy based on the literature for isolated pericarditis of colchicine and corticosteroids [11]. In absence of RCTs of therapies in idiopathic polyserositis, we would recommend colchicine as the initial treatment of choice with a low threshold for subsequent addition of moderate dose oral corticosteroids for at least a month, tapering according to response. Additionally, colchicine may have a role in the management of other forms of inflammatory pleural diseases.
Conflicts of interest
None of the authors have any conflicts of interests to declare with the writing of this case report.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2018.11.006.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Tsang T.S., Barnes M.E., Hayes S.N. Clinical and echocardiographic characteristics of significant pericardial effusions following cardiothoracic surgery and outcomes of echoguided pericardiocentesis for management: Mayo Clinic experience, 1979–1998. Chest. 1999;116:322–331. doi: 10.1378/chest.116.2.322. [DOI] [PubMed] [Google Scholar]
- 2.Ikäheimo MJ, Huikuri HV, Airaksinen KE, et al. Pericardial Effusion after Cardiac Surgery: Incidence, Relation to the Type of Surgery, Antithrombotic Therapy, and Early Coronarybypass Graft Patency. [DOI] [PubMed]
- 3.Sedaghat-Hamedani Post cardiac injury syndrome after initially uncomplicated CRT-D implantation: a case report and a systematic review. 2014;103(10):781–789. doi: 10.1007/s00392-014-0716-0. [DOI] [PubMed] [Google Scholar]
- 4.Ashikhmina . The annals of thoracic surgery; 2010. Pericardial Effusion after Cardiac Surgery: Risk Factors, Patient Profiles, and Contemporary Management. [DOI] [PubMed] [Google Scholar]
- 5.Fukada Pericardial and pleural effusions after definitive radiotherapy for esophageal cancer. J. Radiat. Res. 2012;53(3):447–453. doi: 10.1269/jrr.11194. [DOI] [PubMed] [Google Scholar]
- 6.Murthy Induction chemoradiotherapy increases pleural and pericardial complications after esophagectomy for cancer. J. Thorac. Oncol. 2009;(4):395–403. doi: 10.1097/JTO.0b013e318195a625. [DOI] [PubMed] [Google Scholar]
- 7.Lui Complications after esophagectomy for cancer: 53-year experience with 20,796 patients. World J. Surg. 2008;32(3):395–400. doi: 10.1007/s00268-007-9349-z. [DOI] [PubMed] [Google Scholar]
- 8.Ziarnik M. Chyle leak after esohageal surgery. Gastrointest. Surg. 2015:53–64. [Google Scholar]
- 9.Ferguson M.K., Celauro A.D., Prachand V. Prediction of major pulmonary complications after esophagectomy. Ann. Thorac. Surg. 2011;91:1494–1501. doi: 10.1016/j.athoracsur.2010.12.036. [DOI] [PubMed] [Google Scholar]
- 10.Merigliano S. Chylothorax complicating oesophagectomy for cancer: a place for early thoracic duct ligation. J. Thorac. Cardiovasc. Surg. 2000;119(3):453–457. doi: 10.1016/s0022-5223(00)70123-1. [DOI] [PubMed] [Google Scholar]
- 11.Imezio, Adler Treatment with aspirin, NSAIDs, corticosteroids and colchicine in acute and recurrent pericarditis. Heart Fail. Rev. 2012;18(3):355–360. doi: 10.1007/s10741-012-9328-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.